Abstract
Physical activity promotes positive effects on people's health, but most adolescents do not engage in sufficient physical activity to receive the benefits. Studies suggest that school-based interventions can be effective in increasing physical activity in adolescents. However, the literature is inconsistent on the effect size and the type of intervention. This paper presents the design of the SCHOOL IN ACTION program to increase physical activity engagement and healthy eating habits. The cluster randomized controlled trial was performed during a period of six months of intervention and 12 months of follow-up in adolescents from four Brazilian public schools. The theoretical model is based on health promoting schools and the social-ecological and self-determination theory. The action strategies were: improvement of exercises intensity during physical education classes and during lunch breaks; vegetable gardening experience; active breaks in non-physical education classes; counselling health to parents and adolescents and changes in the school environment to promote physical activity and healthy eating. Primary variables were physical activity and sedentary behavior (both assessed by accelerometers). Secondary variables were body composition (assessed by dual-energy x-ray absorptiometry) and eating habits (assessed by questionnaire and 3-day food recall). Questionnaires were used to assess other information related to life satisfaction, health behavior and socioeconomic information. Statistical analysis will follow the principles of intention-to-treat and will explore the composition data analysis and mediating factors of lifestyle-related behaviors. We propose that SCHOOL IN ACTION program will be effective to provide evidence to increase physical activity and food healthy habits in adolescents' students.
ClinicalTrials.gov registration: NCT03153176.
TRIAL STATUS: Follow-up and data analysis.
Keywords: Physical activity, School-based intervention, Lifestyle, Sedentary behavior, Adolescent, Mixed methods
1. Introduction
The problem of obesity among children and adolescents is alarming, with figures steadily increasing worldwide [1,2]. In the Brazilian school children population's case, a recent national survey found that 54.3% of adolescents between 12 and 17 years of age are physically inactive [3]. Most likely, the obesogenic environment including an unhealthy diet and physical inactivity exposures is responsible for most of this pandemic in western societies [4].
The literature have shown that moderate-to-vigorous physical activity (MVPA) promotes health benefits in school-age children and adolescents including, but not limited to, reducing risk factors for chronic diseases [5,6], improving quality of life [7], cognitive abilities and academic performance [8], as well as increasing cardiorespiratory fitness [9] and bone and muscle strengthening [10]. Even the physical activities of low intensity and duration may promote favourable changes in different anthropometric measures in obese [11,12] and younger girls [13] group. However, by increasing the intensity, additional gains could be obtained [10], especially to cardiometabolic and vascular parameters [12].
Physical education (PE) greatly contributes to daily MVPA. It is recommended that, at least, half of the time spent in PE classes should be spent engaging in MVPA so that health benefits for children and adolescents can be achieved [14,15]. Nevertheless, school-based intervention studies indicate that the average proportion of PE classes time spent engaging in MVPA is less than recommended for adolescents [16,17]. Other sources of activity may be required to reach adequate levels of MVPA. Evidence suggests that increasing both frequency and duration of physical activities during school time, for example during non-PE classes, recess or meal breaks may provide opportunities to efficiently achieve the recommended levels of MVPA amongst children and adolescents [18].
A recent systematic review showed that the effect of school-based programs on adolescents daily MVPA levels did not differ across gender or socio-economic status [19]. Several studies have indicated that interventions that include the whole school community, families [20,21], improved infrastructure to physical activity [22], and providing professional development course for PE teachers [22] have demonstrated to be more efficacious at improving MVPA levels and health outcomes of children and adolescents. Also, interventions that are evidence-based [23], and that incorporate appropriate behavioral change techniques [24] seem to be more effective at improving MVPA levels among children and adolescents. Despite this, often multicomponent interventions that incorporate the abovementioned components are rather scarce, particularly in South American countries.
This article presents the baseline data and protocol for implementation of a multicomponent school-based intervention (SCHOOL IN ACTION) to enhance physical activity levels and healthy eating habits among children and adolescents in Brazil. The intervention will be evaluated via the RE-AIM framework to expand the evaluation of the impact of health-promoting interventions to real-world conditions. The use of the five dimensions of RE-AIM (Reach, Effectiveness, Adoption, Implementation, and Maintenance) [25] will provide a concrete measure for the effectiveness of the actions implemented and the potential for maintenance the program.
2. Methods
2.1. Study design
The current study presents the method developed to be applied in a school-based intervention program in full-time public schools (two in the intervention group and two in the control group). The approach adopted was a mixed method, aiming to maximise the internal and external validity of the proposed methodology. In this approach, the following steps were considered: elaboration of the research plan (qualitative); implementation of the program (qualitative and quantitative) and analysis of results (qualitative and quantitative).
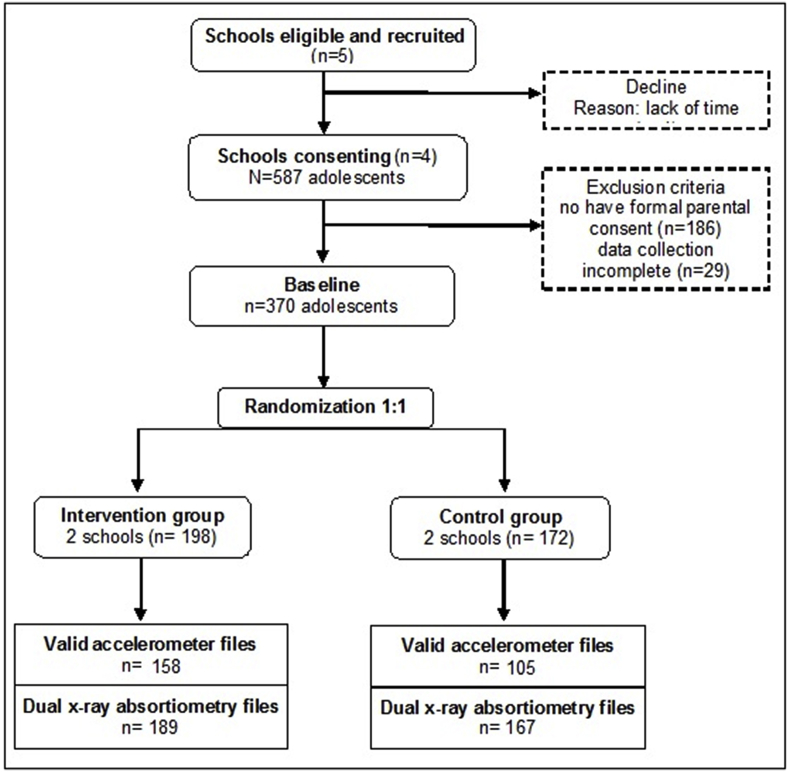
A randomized controlled trial (RCT) was conducted in a group of students from 6th and 7th years from primary school (aged 11–14 years). The design, application, and reporting of this cluster RCT followed the requirements of the Consolidated Standards of Reporting Trials (CONSORT) [26], and extension guidelines for cluster studies [27] (Fig. 1). The project was registered in the protocol of clinical trials of the National Institute of Health clinicaltrials.gov (Registration NCT03153176) and approved by the Committee of Ethics in Research with Human beings of the São Paulo State University, Presidente Prudente, São Paulo, Brazil (number 1.682.007).
Fig. 1.
Flow-chart of the School in Action cluster randomized controlled trial.
2.1.1. Reach, effectiveness, adoption, implementation and maintenance (RE-AIM)
The SCHOOL IN ACTION program involves a set of individual and organizational evidence-based intervention strategies based to promote the physical activity and obesity control of Brazilian's students. The evaluation model adopted was the RE-AIM [25] framework. The main purpose was to highlight the potential expansion of the intervention program as a public-school health policy that is applicable in similar contexts. Table 1 presents the research questions for each of the RE-AIM phases in the context of SCHOOL IN ACTION program:
Table 1.
Application of the RE-AIM model in the School in Action program.
| Dimension | Questions |
|---|---|
| Reach | What is the proportion and representativeness of public integral education schools during the study? What is the proportion and representativeness of the adolescents enrolled in the 6th and 7th year of secondary education in public integral education schools during the study? |
| Effectiveness | What is the impact of the program regarding on effectiveness in the primary and secondary variables of the study? What is the degree of satisfaction and usability of the program perceived by the school professionals, parents and students affected by the program? What is the relation between the result presented by the adolescent with the satisfaction and usability perceived by the key informants affected by the program? |
| Adoption | What is the proportion and representativeness of study participants (schoolchildren, teachers and parents), who started to adopt the program or some of the interventions developed? What is the proportion and representativeness of the adolescents enrolled in the 6th and 7th year of secondary education in the schools of integral education that would be reached? |
| Implementation | How faithful was the protocol performed as expected? |
| Maintenance | What is the representativeness and expansion of schools of integral education that gave continuity to the implemented intervention program? What is the representativeness of adolescent students enrolled in the 6th and 7th year of secondary education in the schools of integral education by the program? |
2.2. Setting and participants
The study was carried out in the city of Presidente Prudente, located in the western region of the State of São Paulo - Brazil. The population aged 10–14 years was, approximately, 15,305 people and schooling rates are of 97.8% [28]. In this region there are five schools included at Integral Education Program. National government policies prioritize implementation of programs in regions with greater social vulnerability, and thus, the school of Integral Education Program was started in peripheral neighbourhoods, with greater population in unfavourable economic conditions [29], and this are the most of our study population.
2.2.1. Primary school
Primary schools of integral education offer seven hours per day of studies that include in addition to the basic disciplines; preparatory activities for the workforce, the orientation of studies, elaboration of a life project, among other aspects [30]. Students can practice physical activities for 2 h a week in PE classes, which are taught by teachers with specific higher education qualifications. Authorization for the schools’ recruitment was made in August 2016 by the Regional Board of Education.
2.2.2. Students
The current project was directed to students enrolled in 2017, pertaining to the 6th and 7th year of primary school. In general, students live in the localities close to the school, since this is an established criterion for admission to enrolment [29]. All students in the selected schools were invited to participate in the program.
2.2.3. Recruitment procedures
Only primary schools of integral education were eligible to participate in the study. All five eligible schools in the city were contacted. The allocation of schools to the intervention or control group was made by randomization and performed by a research assistant that was not involved in the study.
The allocation was blinded to schools and after the allocation process, they received information about the research and were invited to partake in this study. At this stage, one school reported no interest in participating in the research. Finally, four eligible schools that showed interest were informed about their condition in the study and then formal consent form was sought.
Schools and students that refused to participate, as well as students whose parents did not sign the consent form, were also excluded from the study. Only for data analyses purposes, school-children with physical or motor limitations that compromised their participation in fitness assessment and/or presented with any mental or cognitive limitation that preclude them from filling the evaluation questionnaires, were also excluded.
2.3. Ethical and legal aspects
The project was approved by the Ethics Committee on Human Research of the São Paulo State University, Presidente Prudente, São Paulo, Brazil (number 1.682.007) and authorized by the Regional Board of Education (number 0248/1071/2016-DER PPR). The researchers visited each school to clarify the objectives and procedure of the research and to obtain the consent of the school board (principals, coordinators, and teachers). Subsequently, students were invited to participate in the research and received a meeting invitation to send to their parents. In a face-to-face meeting, the parents were informed about the study and were invited to sign the informed consent form, approving the child's participation in the study. At the end of each stage of the project, parents received a report of their child's assessment results with recommendations for improving health and living habits.
2.4. Intervention
The strategies of action in the SCHOOL IN ACTION program were planned one year before the intervention took place, which was then carried out in three stages. In the first stage, the research team investigated in the recent literature school-based interventions to promote physical activity and prevent obesity [6,18,31].
The second stage - diagnosis stage, involved exploration of knowledge, attitudes, and experiences of health promotion at a school level, with a focus on physical activity and nutrition. During this stage, participating children mapped their ideal environment in your neighbourhood and school that they perceived to promote physical activity. Participants also reported on the day-to-day activities at home and at school. School teachers reported on their previous knowledge on physical activity and health, and also on previous initiatives the school had used to promote the health of the students.
This diagnosis information associated to study of specific literature formed an evidence-based plan to promote physical activity and healthy eating among participating children and schools (third stage). The theoretical model and strategies of the intervention plan of School in Action program will be detailed below.
2.4.1. Theoretical model/theoretical framework
The SCHOOL IN ACTION program design was based on the socio-ecological model for health promotion [32,33], and the strategies adopted were guided by self-determination theory [34], social cognitive theory [35] and health promoting schools [36,37].
The socio-ecological model emphasizes the different levels of influence and aggregation of the interactions between the individual and the environment on the adoption of health-related behaviours [32,33]. This interaction constructs the individual-environment relationship. Thus, social groups and individuals can influence the environment and regulate habits and their own choices, leading to desired outcomes [38]. This interaction is also integrated in social cognitive theory [35] which seeks to understand how learning mechanisms, personal capacities, and environmental changes can influence health and direct positive changes in individual behavior. Either through interventions in health and social practices or public health policies.
The World Health Organization establishes strategic lines of actions, which aim to create a healthier environment (physical and social) in schools [39]. This suggests that the WHO understands the potential of schools to utilize the social environment to create favourable to learning and cultural [39]. Studies [40,41] highlight that stimulating children and adolescents' sense of autonomy is key to enhancing motivation and promoting health. The theory of self-determination suggests that an intervention in accordance with the adolescent's intrinsic life goals will result in greater motivation for health change [34]. This is thought to generate greater satisfaction of the basic psychological needs (autonomy, competence, and relation), which are associated with well-being and quality of life [34].
2.4.2. Strategies
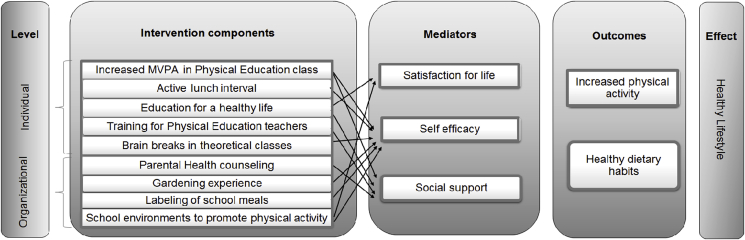
The SCHOOL IN ACTION program involved different evidenced based strategic actions to promote physical activity and healthy eating. These strategies were implemented during the intervention stage (one academic year). The strategies supported changes at the individual and organizational level. This was achieved by engaging participation among teachers, parents, and students. At the individual level, interventions were focused on the change in the components of lifestyle. At organizational level, the focus was on strategies that involve the context of social support and opportunities for the practice of physical activity within the school environment and during adolescent's free time (Fig. 2).
Fig. 2.
Theoretical Model School in Action program.
2.4.3. Individual level
-
1.
Development and monitoring of a physical exercise program in PE classes: To help increase MVPA levels during PE, all participants in the intervention group were exposed to six months of the exercise program during the first 10–15 min of PE classes. This included a warm-up activity with running and mini-circuit of functional training. The perceived exertion scale (BORG) was used to control the intensity of the activities during this component of the intervention [42]. The activities included in the program were based on the recommendations of high-intensity physical activities for adolescents [[43], [44], [45]].
-
2.
Physical activity during the lunch break: Equipment (i.e., balls, ropes, clubs, cones) was provided during the lunch break and supervised sports activities were held three times a week for six months (i.e., the duration of the intervention). Student participation was voluntary.
-
3.
Vegetable garden experience: for three months, the students went through the experience of growing vegetables in the school environment through the implementation of a vegetable garden. This experience provided contact with healthy and natural foods, with the purpose to promote improvement in the school menu and encourage the consumption of these foods among adolescents. The green leaves and vegetables produced in the vegetable garden were offered to students during school lunch time, and to parents during the final evaluation meeting.
-
4.
Students' healthy life project: in the first semester, students were provided with booklets containing information about lifestyle and positive attitudes towards physical activity and healthy diet. During the second semester, students were instructed to establish an objective, personal goals, and actions to improve their health-related lifestyle habits. This approach was reviewed and modified each semester, based on physical fitness data and new personal goals and objectives were established.
2.4.4. Organizational level
-
1.
Training and continuing education of PE teachers: four months before the intervention (September–December 2016), PE teachers participated in 20 h training with SCHOOL IN ACTION program's trainer. In these meetings, strategies were designed to increase the time in MVPA during PE classes. During these meetings, strategies to encourage the implementation of health actions in the school curriculum were also discussed.
-
2.
Program of active breaks during non-PE classes: the aim was to break up sitting time in the classroom by allowing the opportunity for around 5 min of physical activity. These active breaks involved simple body movements. Teachers and students were trained to conduct these active breaks. There were also posters available in class showing relaxation exercises, joint mobility exercises, and movement while standing exercises.
-
3.
Counselling to parents: three parent meetings were held during the intervention period, and newsletters related to lifestyle, healthy eating, and physical activity issues were given in each of those meetings. During these meetings, the parents were encouraged to promote changes in the domestic environment to stimulate habits of physical activity and healthy eating among all family members.
-
4.
Labeling of school meals: a team of nutritionists assessed the meal plan offered at school (breakfast, lunch and afternoon snack). A preparation of salty and sweet food was analyzed referring to the amount of salt or sugar and total calories. The labeling of the foods present in the school menu was elaborated, and a consumption recommendation per meal was specified, as well as the discrimination of the nutritional value of the food for each macronutrient (carbohydrate, protein, lipids, and minerals) present in the preparations. The menu was posted up on the wall of the school canteen and presented to the team of cookers.
-
6.
Changes in the environment and acquisition of material resources: the social area and less occupied spaces in the school were modified in order to encourage physical activity and healthy eating habits. Among the main environmental changes, we highlight the painting of games in the courtyards and corridors of the school; purchased a variety of sport equipment and teaching games which could be played during the lunch break; painting of the food pyramid in the cafeteria and establishing the school vegetable garden.
2.5. Control schools/control group
Participants in the control schools only participated in outcome assessment during the intervention time (i.e., baseline, 6-month and 12-months post-intervention). A condensed version of the program which included training of PE teachers, delivery of educational material and equipment kit (balls, cones, ropes, etc.) was offered to the control group after the 12-month intervention evaluations.
2.6. Outcome measures
Outcomes are measured during baseline (after parental consent and before intervention delivery), immediately after the conclusion of the intervention (6-months after to baseline) and after 6-months post intervention (12-months after to baseline). At baseline, all assessment was conducted by an experience researcher that was not involved in this study. This was done to ensure assessment procedure was blind to the researcher.
Participants completed questionnaires prior to start their physical assessments and to use an accelerometer. Self-report information that include health behavior related to physical activity, sedentary behavior and eating habits, as well their mediators’ factors (self-efficacy, confidence, barriers) was collected at baseline, post-intervention and follow-up. Confounding variables such as age, sex, ethnicity and socio-economic status [46] also be included on the questionnaire. Table 2 shows an overview of the distribution of outcomes across the primary and secondary level.
Table 2.
Synthesis of the primary and secondary outcomes.
| Level | Variable | Efficacy Endpoint | Instrument | Unity |
|---|---|---|---|---|
| Primary | Physical activity | Change in MVPA from baseline to 6 and 12 months | Accelerometer | Total counts/Total minutes/Cut points Evenson |
| Questionnaire | Physical activity (domains, frequency, duration and intensity) | |||
| Logbook | Type of activity/Duration of PE class/Wake up time/Bedtime | |||
| Secondary | Body Composition | Change in body fat mass (total and segment) from baseline to 6 and 12 months | DXA | Fat mass/Lean mass/Bone mineral density/Bone mineral content |
| Anthropometry | Weight/Height/Head-cephalic height/Triceps cutaneous fold/Waist circumference/Hip circumference | |||
| Physical Fitness | Change in VO2max, muscular strength and flexibility from baseline to 6 and 12 months | Leger's 20-m run test | Minutes/Turns/Stages/VO2max | |
| Abdominals | Repetitions in 1 min | |||
| Horizontal jump test | Distance in meters | |||
| Hand Grip Dynamometer | Kilograms | |||
| Sit-and-reach test | Distance in centimeters | |||
| Eating habits | Change in total calories, consumption of sugary drinks, fruits and vegetables from baseline to 6 and 12 months | Questionnaire | Frequency of food (fruit, vegetables, sugary drinks) /consumption and family meals/3-day food recall |
|
| Sleep | Change in sleep time and quality from baseline to 6 and 12 months | Accelerometer | Total sleep time/Sleep efficiency/Sleep latency | |
| PSQI | Sleep quality |
All outcomes will be compared among control group. MVPA, moderate to vigorous physical activity; DXA, Dual-energy x-ray absorptiometry; PSQI, Pittsburg Sleep Quality Index.
2.6.1. Primary outcome
The primary endpoint is composite of physical activity level, based on time spend in MVPA measured after 6- and 12-months following baseline. The Chandler cut-off points [47] were used to categorize physical activity levels. MVPA will be analyzed by sum of daily minutes and correspondent percentage value. Thereby 24-h movement (physical activity, sedentary behavior, sleep) which was evaluated by accelerometers (GT3XE-Plus triaxial model, ActiGraph LLC, Pensacola, Fla, USA). The devices were configured to collect information within a period of 10 days recording the 24-h period. A minimum of 600 min of recording per day was considered for data validation [48]. The participants were instructed to use the accelerometer on the wrist of the non-dominant arm throughout the evaluation period. A self-reported questionnaire and a “logbook” was implemented to record participants daily routine when wearing accelerometer, include atypical activities (i.e. travel), PE class day, sports practice, physical activity during leisure time, sleep and awake time.
2.6.2. Secondary outcome
We hypothesize that School in Action program is effective to promote positive changes on MVPA (primary endpoint) and therefore included the following secondary endpoints: changes of body composition, physical fitness and another life style habits (eating behavior and sleep quality) assessed after 6- and 12-months following baseline (Table 2). Body composition was evaluated by means of the Dual-energy x-ray absorptiometry (DXA). This procedure spends approximately 10 min and the participant lie on the bed for scanning arm pass over in all body measuring bone, muscle and fat mass. Anthropometric measures of weight, height, triceps skinfold, waist, and hip circumferences were also calculated for the evaluation of physical growth and distribution of body fat.
The cardiorespiratory, musculoskeletal and motor skills tests utilized were selected as previous findings indicated sound reliability and validity properties [49,50]. Leger's 20-m run test [51] was used to measure the adolescents' cardiorespiratory fitness. The manual grip strength test, applied by Camry's hand-held dynamometer, the 1-min abdominal test, the horizontal jump test, and the Sit-and-reach for flexibility test were used to assess musculoskeletal and motor skills.
The sleep period was measured with accelerometers and the data were manually adjusted by the evaluator based on the first and the last moment of ten consecutive minutes or more in which the accelerometer was recorded 0 counts [52]. Mean scores were calculated for the analysis of total sleep time, sleep latency (wake-to-sleep transition), and sleep efficiency (percentage of sleep time in bed) for adolescents who obtained at least three nights of valid sleep measurements. In addition, the Pittsburgh Sleep Quality Index [53] was evaluated.
The dietary intake was evaluated by a 3-day food recall, the days were non-consecutive and one of them was during the weekend. This method provides information on the average habitual intake and makes it possible to evaluate the intake of macronutrients and the total daily calories consumed by the adolescent.
2.7. Potential mediator factors
Potential psychological mediators were measured using self-reported questionnaires based on self-determination theory [34]. After the school-interventions program we expect in regards to changes in quality of life [54], autonomy, self-efficacy, barriers and social support to reduce sedentary behavior, increase MVPA and consumption of fruits and vegetables.
2.8. Sample size calculation
A power calculation was applied to determine the sample size required to detect changes in the main outcomes (i.e., physical activity and adiposity). The sample size estimation was based on testing G Power 3.1.9.2 software was used to calculate the sample size, considering a statistical power of 80% and a significance level of 5% for comparison between means. The effect size was estimated from the mean and standard deviation results of pre- and post-intervention in the control and intervention groups of other studies with similar outcomes in the literature (Table 3).
Table 3.
Sample size calculation for primary and secondary outcomes based on effect size of previously interventions.
| Outucome | Author, year | Δ IG |
ΔCG |
Effect size | Power (%) | SL (%) | Sample size |
Drop-out (30%) |
||
|---|---|---|---|---|---|---|---|---|---|---|
| IG |
CG |
IG |
CG |
|||||||
| Mean(SD) | Mean(SD) | n | n | n | n | |||||
| PA (cpm) | Meyer, 2014 [55] | −185(191) | −227(182.5) | 0.4 | 80 | 5 | 102 | 102 | 133 | 133 |
| MVPA | Lindqvist, 2014 [56] | 4.9(28.9) | −25.4(23.0) | 1.2 | 80 | 5 | 14 | 14 | 18 | 18 |
| Body fat mass | Weeks, 2008 [57] | −699(2061) | −69(1408) | −0.4 | 80 | 5 | 100 | 100 | 130 | 130 |
| Sleep duration | Kredlow, 2015 [58] | – | – | 0.4 | 80 | 5 | 102 | 102 | 133 | 133 |
IG, intervention group; CG, control group; SL, significance level; SD, standard deviation; MVPA, moderate-to-vigorous physical activity; PA, physical activity; BMI, body mass index.
Sleep time and PA by (cpm) was the largest sample size required to achieve the outcomes of the study with a post-intervention sample size required of 102 subjects per arm. After allowing for a 30% drop-out, the a priori sample size required a minimum of 133 per arm (n = 266 subjects).
2.9. Statistical analysis
The procedures for data analysis will follow the guidelines of CONSORT in the presentation of results. Ordinary summary statistics were used to describe participants in the study on key demographic characteristics at baseline. The analysis of primary outcome of the study (i.e., percentage of time and total minutes spent in MVPA) will be performed using cluster analysis and compositional data analyses.
The geometric mean will be used to summarize daily time (%) across all 24-h lifestyle behaviors. Compositional analysis will be conducted making use of functions implemented in the R packages Compositions [59] and zCompositions [60]. This latter facilitated pre-processing of zero observations to be replaced by plausible small values using the log-ratio Expectation-Maximisation algorithm [61]. In this analyze, each participant's daily time use is considered as a composition [LIPA, MVPA, Sedentary time, sleep]. For each individual these components are scale to add up to 24 h. Participant's time use compositions are first expressed in isometric log-ratio (ilr) coordinates [62], used as explanatory variables representing the daily behavior composition in a linear regression model fitted to the different measures as a response (outcome) variables.
Intention-to-treat linear mixed models using maximum likelihood estimation will be tested to verify the effect of the intervention between primary and secondary outcome measures between intervention and control group. Possible differences (group × time interactions) that can be change primary and secondary outcome will be calculated. These effects will be adjusted to baseline data and possible confounding variables (age, sex, maturation status and socioeconomic status) within baseline, post-intervention and follow-up period. The Consolidated Criteria for Qualitative Research Reports (COREQ) [63] will be used to evaluate the qualitative data of the study. Information on the perception, satisfaction, and evaluation of the intervention program, as well as the written responses and registration of the focus groups, will be evaluated through frequency and thematic grouping, through the NVIVO program, version 11.
3. Results
The baseline assessments were carried out during March–April of 2017. A total of four schools accepted to participate in the research. From the 587 eligible students in the 6th and 7th years of Primary school, 370 provided parental consent to participate and participated in the evaluations (63% recruitment rate). Almost all participants participated in the body composition evaluation by DXA (96.2%). Sample size reached on primary outcome of physical activity by valid accelerometer data was de 263 adolescents (71.1%) presented a power size of 50% to minutes of MVPA and 70% to percentage of MVPA at baseline data.
Table 4 present the baseline characteristics and outcomes measures in SCHOOL IN ACTION program. There were an approximately equal amount of male and female participants (male = 43%; females = 57%) and 86% of the families came from a low socioeconomic background. At baseline, there were no significant differences in demographic characteristics between intervention and control groups. There was a statistically significant difference between the intervention and control group only for counts per minute by accelerometer.
Table 4.
School in Action baseline characteristics and outcomes measures by group.
| All | Intervention | Control | p-value* | |
|---|---|---|---|---|
| Gender | 0.507 | |||
| Male | 161 | 83 (41,9) | 78 (45.3) | |
| Female | 209 | 115 (58.1) | 94 (54.7) | |
| Age in years | 11.72 ± 0.6 | 11.75 ± 0.7 | 11.69 ± 0.6 | 0.437 |
| Socioeconomic status | 0.760 | |||
| High | 43 | 25 (14.9) | 18 (13.6) | |
| Low | 257 | 143 (85.1) | 114 (86.40 | |
| Peak Height Velocity | −0.9 ± 1.9 | −0.8 ± 1.8 | −1.0 ± 1.9 | 0.263 |
| Counts per minute | 2434 ± 661 | 2356 ± 637 | 2556 ± 682 | 0.035 |
| MVPA (minutes) | 46.2 ± 27.5 | 47.4 ± 25.5 | 44.3 ± 30.4 | 0.384 |
| Sleep time (hours/day) | 7.9 ± 1.2 | 8.00 ± 1.1 | 7.7 ± 1.3 | 0.183 |
| Fat Mass (kg) | 14.8 ± 9.5 | 14.8 ± 9.0 | 14.8 ± 10.0 | 0.952 |
| Lean Mass(kg) | 29.4 ± 4.9 | 29.7 ± 5.0 | 29.2 ± 4.7 | 0.321 |
| BMI (kg/m2) | 20.8 ± 4.9 | 20.8 ± 4.8 | 20.7 ± 5.0 | 0.822 |
| BMC (g) | 1.8 ± 0.4 | 1.8 ± 0.4 | 1.7 ± 0.4 | 0.097 |
| BMD (g) | 1.0 ± 0.9 | 1.0 ± 0.1 | 1.0 ± 0.1 | 0.134 |
*p-value: difference between groups (p < 0.05). ±: standard deviation; mean and standard deviation to continuous variables, value and percentage to categorical variables. MVPA, moderate to vigorous physical activity; BMI, body mass index; BMC, bone mineral content; BMD, bone mineral density.
4. Discussion
This article describes the protocol of the intervention study SCHOOL IN ACTION which aim to test the effectiveness of an interdisciplinary and multidimensional intervention based on evidence to increase the engagement in MVPA physical activity among adolescents from public schools and low socioeconomic communities in Brazil. We proposed that the intervention would be effective in preventing and controlling obesity through increased physical activity, reduction of sedentary behavior, and encouragement of healthy eating habits of the adolescents.
Teachers and students participating in the program will benefit with increased opportunities to increasing physical activity and improve students lifestyles in daily school practice. Further accompanied by the subsequent increases in levels of physical activity and reduction in risky health behaviors among adolescents.
Teachers and parents were assigned with a crucial role as motivators and mentors to promote gains in the health of adolescents, since social support is a determining factor for behavioral change related to health and increased physical activity among young people [[64], [65], [66]]. One of the strengths of this program was the use of qualitative methodologies for the involvement of the school team since its inception, which allowed the intervention to incorporate both an experimental design based on scientific evidence and the social reality practicality of implementing an intervention. This is likely to increase the chances of sustainability of the program.
In this study, the aim was to assess the level of physical activity, sedentary behavior, sleep quality, and body composition, standing out as one of the first Brazilian studies with such methodological accuracy. The intervention strategies were based on the social-ecological theory [32,33], self-determination theory [34], social cognitive theory [35] and health promoting schools [36,37], which included specific practices for coping with each component of the studied lifestyle (physical activity, sedentary behavior and, eating habits). Studies have indicated that the best results for increasing physical activity in adolescents are sustained and multi-component interventions which are based in behavioral theories [23,24].
The long-term effects of the SCHOOL IN ACTION program intend to address core limitations in the literature for school-based interventions, particularly in the Brazilian context. This study prioritized the use of strategies applicable to the real context of everyday school life (theoretical lessons, PE classes, recreation and, parenting meetings) and educational policies.
Other noteworthy elements of this study were: the type of applied design, which involves not only the individual-level approach, but also the potential effect at the organizational level; the participatory process with end-users (teachers and students), which reduces the risk of low sustainability and maintenance of the program; the adoption of an evaluation model (RE-AIM) to provide a concrete dimension on the effectiveness of the actions implemented and the potential for program maintenance. Future studies could further explore the subgroup analysis that were identified, for example, the group of overweight adolescents, in view of the objective measure used and the model of the intervention of the program which could be directed to control body weight.
In conclusion, we expect the program components should be incorporated into school reality as part of the national educational curriculum to promote healthier schools. Training and supervision using online and face-to-face resources will be proposed so that successful and practical implementation can be ensured in adopting the program in other school structures. At the end of the study, manuals with intervention protocols and educational materials will be made available in the public domain as recommended by the Medical Research Council (MRC) [67] for other institutions who wish to implement a similar intervention.
Funding
This project was funded by the Public Education Improvement Program from The São Paulo Research Foundation - Brazil (FAPESP Process: 2016/09260).
This study was funded in part by the Coordination of Superior Level Staff Improvement – Brazil (CAPES Process: 88881.187941/2018–01).
Acknowledgements
The authors thank the SCHOOL IN ACTION team (research, school teachers, parents, and students), Prof. Ph. D. Mario Betti for the orientations about the Physical Education Curriculum of the State of São Paulo, and National Institutes of Health (NIH) who assisted in the donation of accelerometers.
References
- 1.World Health Organization (WHO) Obesity and overweight. 2018. http://www.who.int/mediacentre/factsheets/fs311/en/ accessed 29 October 2019.
- 2.Han J.C., Kimm S.Y.S. Childhood obesity-2010: progress and challenges. Lancet. 2010;375(9727):1737–1748. doi: 10.1016/S0140-6736(10)60171-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cureau F.V., Silva T.L.N., Bloch K.V., Fujimori E., Belfort D.R., B Carvalho K.M., Leon E.B., Vasconcelos M.T., Ekelind U., Schaan B.D. ERICA: leisure-time physical inactivity in Brazilian adolescents. Rev. Saude Publica. 2016;50(Suppl 1):4s. doi: 10.1590/S01518-8787.2016050006683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization (WHO) Ending childhood obesity. 2017. https://www.who.int/iris/handle/10665/259349 accessed 22 March 2018.
- 5.Simon C., Kellou N., Dugas J., Platat C., Copin N., Schweitzer B., Hausser F., Bergouignan A., Lefai E., Blanc S. A socio-ecological approach promoting physical activity and limiting sedentary behavior in adolescence showed weight benefits maintained 2.5 years after intervention cessation. Int. J. Obes. 2014;38(7):936–943. doi: 10.1038/ijo.2014.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Demetriou Y., Sudeck G., Thiel A., Horner O. The effects of school-based physical activity interventions on students' health-related fitness knowledge: a systematic review. Educ. Res. Rev. 2015;16:19–40. [Google Scholar]
- 7.Wu X.Y., Han L.H., Zhang J.H., Luo S., Hu J.W., Sun K. The influence of physical activity, sedentary behavior on health-related quality of life among the general population of children and adolescents: a systematic review. PLoS One. 2017;12(11) doi: 10.1371/journal.pone.0187668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mura G., Vellante M., Nardi A.E., Machado S., Carta M.G. Effects of school-based physical activity interventions on cognition and academic achievement: a systematic review. CNS Neurol. Disord. - Drug Targets. 2015;14(9):1194–1208. doi: 10.2174/1871527315666151111121536. [DOI] [PubMed] [Google Scholar]
- 9.Minatto G., Barbosa Filho V.C., Berria J., Petroski E.L. School-based interventions to improve cardiorespiratory fitness in adolescents: systematic review with meta-analysis. Sport. Med. 2016;46(9):1273–1292. doi: 10.1007/s40279-016-0480-6. [DOI] [PubMed] [Google Scholar]
- 10.Janssen I I., Leblanc A.G. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int. J. Behav. Nutr. Phys. Act. 2010;(7):40. doi: 10.1186/1479-5868-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fuzeki E., Engeroff T., Banzer W. Health benefits of light-intensity physical activity: a systematic review of accelerometer data of the national health and nutrition examination survey (nhanes) Sport. Med. 2017;47(9):1769–1793. doi: 10.1007/s40279-017-0724-0. [DOI] [PubMed] [Google Scholar]
- 12.García-Hermoso A., Ramírez-Vélez R., Saavedra J.M. Exercise, health outcomes, and pædiatric obesity: a systematic review of meta-analyses. J. Sci. Med. Sport. 2019;22(1):76–84. doi: 10.1016/j.jsams.2018.07.006. [DOI] [PubMed] [Google Scholar]
- 13.Dowd K.P., Harrington D.M., Hannigan A., Donnelly A.E. Light-intensity physical activity is associated with adiposity in adolescent females. Med. Sci. Sport. Exerc. 2014;46(12):2295–2300. doi: 10.1249/MSS.0000000000000357. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention National center for chronic disease prevention and health promotion, division of adolescent and school health, strategies to improve the quality of physical education. 2010. www.cdc.gov/healthyschools/pecat/quality_pe.pdf Accessed date: 23 October 2015.
- 15.Association for Physical Education Health Position. 2015. http://www.afpe.org.uk/physical-education/wp-content/uploads/afPE_Health_Position_Paper_Web_Version.pdf Paper 2015. accessed 11 April 2017. [Google Scholar]
- 16.Hollis J.L., Williams A.J., Sutherland R., Campbell E., Nathan N., Wolfenden L., Morgan P.J., Lubans D.R., Wiggers J. A systematic review and meta-analysis of moderate-to-vigorous physical activity levels in elementary school physical education lessons. Prev. Med. 2016;86:34–54. doi: 10.1016/j.ypmed.2015.11.018. [DOI] [PubMed] [Google Scholar]
- 17.Hollis J.L., Sutherland R., Williams A.J., Campbell E., Nathan N., Wolfenden L., Morgan P.J., Lubans D.R., Gillham K., Wiggers J. A systematic review and meta-analysis of moderate-to-vigorous physical activity levels in secondary school physical education lessons. Int. J. Behav. Nutr. Phys. Act. 2017;14(1) doi: 10.1186/s12966-017-0504-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dobbins M., Husson H., DeCorby K., LaRocca R.L. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst. 2013;2:CD007651. doi: 10.1002/14651858.CD007651.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Love R., Adams J., van Sluijs E.M.F. Are school-based physical activity interventions effective and equitable? A meta-analysis of cluster randomized controlled trials with accelerometer-assessed activity. Obes. Rev. 2019;20(6):859–870. doi: 10.1111/obr.12823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barbosa Filho V.C., Minatto G., Mota J., Silva K.S., Campos W., Lopes A.S. Promoting physical activity for children and adolescents in low- and middle-income countries: an umbrella systematic review. Prev. Med. 2016;88:115–126. doi: 10.1016/j.ypmed.2016.03.025. [DOI] [PubMed] [Google Scholar]
- 21.World Health Organization (WHO) Regional Office for Europe, Health Evidence Network, what is the evidence on school health promotion in improving health or preventing disease and, specifically, what is the effectiveness of the health promoting schools approach? 2006. http://www.euro.who.int/__data/assets/pdf_file/0007/74653/E88185.pdf accessed 15 October 2015.
- 22.Ribeiro I.C., Parra D.C., Hoehner C.M., Soares J., Torres A., Pratt M., Legetic B., Malta D.C., Matsudo V., Ramos L.R., Simoes E.J., Brownson R.C. School-based physical education programs: evidence-based physical activity interventions for youth in Latin America. Glob. Health Promot. 2010;17(2):5–15. doi: 10.1177/1757975910365231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hoor G.A., Plasqui G., Schols A.M.W.J., Kok G. Development, implementation, and evaluation of an interdisciplinary theory- and evidence-based intervention to prevent childhood obesity: theoretical and methodological lessons learned. Front Public Health. 2017;5:352. doi: 10.3389/fpubh.2017.00352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Owen M.B., Curry W.B., Kerner C., Newson L., Fairclough S.J. The effectiveness of school-based physical activity interventions for adolescent girls: a systematic review and meta-analysis. Prev. Med. 2017;105:237–249. doi: 10.1016/j.ypmed.2017.09.018. [DOI] [PubMed] [Google Scholar]
- 25.Antikainen L., Ellis R. A RE-AIM evaluation of theory-based physical activity interventions. J. Sport Exerc. Psychol. 2011;33(2):198–214. doi: 10.1123/jsep.33.2.198. [DOI] [PubMed] [Google Scholar]
- 26.Schulz K.F., Altman D.G., Moher D., CONSORT Group CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Ann. Intern. Med. 2010;152(11):726–732. doi: 10.7326/0003-4819-152-11-201006010-00232. [DOI] [PubMed] [Google Scholar]
- 27.Campbell M.K., Piaggio G., Elbourne D.R., Altman D.G. CONSORT Group, Consort 2010 statement: extension to cluster randomised trials. BMJ. 2012;345 doi: 10.1136/bmj.e5661. [DOI] [PubMed] [Google Scholar]
- 28.Instituto Brasileiro de Geografia e Estatistica (IBGE) Censo Demográfico. 20102010 https://cidades.ibge.gov.br/brasil/sp/presidente-prudente/panorama [Google Scholar]
- 29.Ministério da Educação (MEC) Plano Nacional da Educação 2014-2024. 2014. http://www.observatoriodopne.org.br/uploads/reference/file/439/documento-referencia.pdf accessed 29 October 2017.
- 30.Secretaria de Educação do Estado de São Paulo Diretrizes do programa de Ensino integral. 2014. http://www.educacao.sp.gov.br/a2sitebox/arquivos/documentos/342.pdf accessed 12 December 2016.
- 31.Hatfield D.P., Chomitz V.R. Increasing children's physical activity during the school day. Current Obesity Reports. 2015;4(2):147–156. doi: 10.1007/s13679-015-0159-6. [DOI] [PubMed] [Google Scholar]
- 32.Naylor P.J., Nettlefold L., Race D., Hoy C., Ashe M.C., Higgins J.W., McKay H.A. Implementation of school based physical activity interventions: a systematic review. Prev. Med. 2015;72:95–115. doi: 10.1016/j.ypmed.2014.12.034. [DOI] [PubMed] [Google Scholar]
- 33.Stokols D., Allen J., Bellingham R.L. The social ecology of health promotion: implications for research and practice. Am. J. Health Promot. 1996:247–251. doi: 10.4278/0890-1171-10.4.247. 0(4) [DOI] [PubMed] [Google Scholar]
- 34.Sallis J.F., Owen N., Fisher E. Ecological models of health behaviour. In: Glanz K., Rimer B.K., Viswanath K., editors. Health Behavior and Health Education: Theory, Research, and Practice. fifth ed. Jossey-Bass; San Francisco: 2015. pp. 43–64. [Google Scholar]
- 35.Deci E.L., Ryan R.M. The “what” and “why” of goal pursuits: Human needs and the self-determination of behaviour. Psychol. Inq. 2000;1194:227–268. [Google Scholar]
- 36.Bandura A. Health promotion by social cognitive means. Health Educ. Behav. 2004;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 37.Langford R., Bonell C.P., Jones H.E., Pouliou T., Murphy S.M., Waters E., Komro K.A., Gibbs L.F., Magnus D., Campbell R. The WHO Health Promoting School framework for improving the health and well-being of students and their academic achievement. Cochrane Database Syst. Rev. 2014;16(4):CD008958. doi: 10.1002/14651858.CD008958.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McAlister A.L., Perry C.L., Parcel G.S. How individuals, environments, and health behaviors interact: social cognitive theory. In: Glanz K., Rimer B.K., Viswanath K., editors. Health Behavior and Health Education: Theory, Research, and Practice. fourth ed. Jossey-Bass; San Francisco: 2008. pp. 169–188. [Google Scholar]
- 39.International Union for Health Promotion and education (IUHPE) 2010. http://www.iuhpe.org/images/PUBLICATIONS/THEMATIC/HPS/Evidence-Action_ENG.pdf accessed 12 December 2016.
- 40.Smith J.J., Morgan P.J., Plotnikoff R.C., Dally K.A., Salmon J., Okely A.D., Finn T.L., Babic M.J., Skinner G., Lubans D.R. Rationale and study protocol for the ‘Active Teen Leaders Avoiding Screen-time’ (ATLAS) group randomized controlled trial: an obesity prevention intervention for adolescent boys from schools in low-income communities. Contemp. Clin. Trials. 2014;37(1):106–119. doi: 10.1016/j.cct.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 41.Lonsdale C., Lester A., Owen K.B., White R.L., Peralta L., Kirwan M., Diallo T.M.O., Maeder A.J., Bennie A., MacMillan F., Kolt G.S., Ntoumanis N., Gore J.M., Cerin E., Cliff D.P., Lubans D.R. An internet-supported school physical activity intervention in low socioeconomic status communities: results from the Activity and Motivation in Physical Education (AMPED) cluster randomised controlled trial. Br. J. Sports Med. 2019;53:341–347. doi: 10.1136/bjsports-2017-097904. [DOI] [PubMed] [Google Scholar]
- 42.Borg G.A. Psychological bases of perceived exertion. Med. Sci. Sport. Exerc. 1982;14(5):377–381. [PubMed] [Google Scholar]
- 43.Kilka B., Jordan C. High-intensity circuit training using body weight: maximum results with minimal investment, ACSMs Health Fit. J. 2013;17(3):8–13. 2013. [Google Scholar]
- 44.Giannaki C.D., Aphamis G., Tsouloupas C.N., Ioannou Y., Hadjicharalambous M. An eight week school-based intervention with circuit training improves physical fitness and reduces body fat in male adolescents. J. Sports Med. Phys. Fitness. 2016;56(7–8):894–900. [PubMed] [Google Scholar]
- 45.Schmidt D., Anderson K., Graff M., Strutz V. The effect of high-intensity circuit training on physical fitness. J. Sports Med. Phys. Fitness. 2016;56(5):534–540. [PubMed] [Google Scholar]
- 46.Associação Brasileira de Geografia e Estatística (ABEP) 2016. Critério de Classificação Econômica Brasil.http://www.abep.org/new/criterioBrasil.aspx accessed 12 March 2016. [Google Scholar]
- 47.Chandler J.L., Brazendale K., Beets M.W., Mealing B.A. Classification of physical activity intensities using a wrist-worn accelerometer in 8–12-year-old children. Pediatr Obes. 2016;11(2):120–127. doi: 10.1111/ijpo.12033. [DOI] [PubMed] [Google Scholar]
- 48.Migueles J.H., Cadenas-Sanchez C., Ekelund U., Delisle N.C., Mora-Gonzalez J., Lof M., Labayen I., Ruiz J.R., Ortega F.B. Accelerometer data collection and processing criteria to assess physical activity and other outcomes: a systematic review and practical considerations. Sport. Med. 2017;47(9):1821–1845. doi: 10.1007/s40279-017-0716-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ruiz J.R., Castro-Piñero J., España-Romero V., Artero E.G., Ortega F.B., Cuenca M.M., Jimenez-Pavón D., Chillón P., Girela-Rejón M.J., Mora J., Gutiérrez A., Suni J., Sjöström M., Castillo M.J. Field-based fitness assessment in Young people: the ALPHA health-related fitness test battery for children and adolescents. Br. J. Sports Med. 2011;45(6):518–524. doi: 10.1136/bjsm.2010.075341. [DOI] [PubMed] [Google Scholar]
- 50.Cvejic D., Pejovic T., Ostojic S. Assessment of Physical Fitness in Children and Adolescents, Series: Phys. Educ. Sport. 2013;11(2):135–145. [Google Scholar]
- 51.Barnett A., Chan L.Y.S., Bruce I.C. A preliminary study of the 20-m multistage shuttle run as a predictor of peak VO2 in Hong Kong Chinese students, Pediatr. Exerc. Sci. 1993;5(1):42–50. [Google Scholar]
- 52.Cole R.J., Kripke D.F., Gruen W., Mullaney D.J., Gillin J.C. Automatic sleep/wake identification from wrist activity. Sleep. 1992;15(5):461–469. doi: 10.1093/sleep/15.5.461. [DOI] [PubMed] [Google Scholar]
- 53.Buysse D.J., Reynolds C.F., 3rd, Monk T.H., Berman S.R., Kupfer D.J. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 54.Gilman E.R., Huebner S., Laughlin E.J. A first study of the multidimensional students' life satisfaction scale with adolescents. Soc. Indic. Res. 2000;52(2):135–160. [Google Scholar]
- 55.Meyer U., Schindler C., Zahner L., Ernst D., Hebestreit H., van Mechelen W., Brunner-La Rocca H.P., Probst-Hensch N., Puder J.J., Kriemler S. Long-term effect of a school-based physical activity program (KISS) on fitness and adiposity in children: a cluster-randomized controlled trial. PLoS One. 2014;9(2):1–10. doi: 10.1371/journal.pone.0087929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lindqvist A.K., Mikaelsson K., Westerberg M., Gard G., Kostenius C. Moving from idea to action: promoting physical activity by empowering adolescents, health promot. In Pract. 2014;15(6):812–818. doi: 10.1177/1524839914535777. [DOI] [PubMed] [Google Scholar]
- 57.Weeks B.K., Young C.M., Beck B.R. Eight months of regular in-school jumping improves indices of bone strength in adolescent boys and girls: the POWER PE study. J. Bone Miner. Res. 2008;23(7):1002–1011. doi: 10.1359/jbmr.080226. [DOI] [PubMed] [Google Scholar]
- 58.Kredlow M.A., Capozzoli M.C., Hearon B.A., Calkins A.W., Otto M.W. The effects of physical activity on sleep: a meta-analytic review. J. Behav. Med. 2015;38(3):427–449. doi: 10.1007/s10865-015-9617-6. [DOI] [PubMed] [Google Scholar]
- 59.van den Boogaart K.G., Tolosana-Delgado R. “compositions”: A unified R package to analyze compositional data. Comput. Geosci. 2008;34(4):320–338. [Google Scholar]
- 60.Palarea-Albaladejo J., Martín-Fernández J.A. zCompositions - R package for multivariate imputation of left-censored data under a compositional approach. Chemometr. Intell. Lab. Syst. 2015;143:85–96. [Google Scholar]
- 61.Palarea-Albaladejo J., Martín-Fernández J.A. A modified EM alr-algorithm for replacing rounded zeros in compositional data sets. Comput. Geosci. 2008;34(8):902–917. [Google Scholar]
- 62.Pawlowsky-Glahn V., Egozcue J.J., Tolosana-Delgado R. John Wiley & Sons; 2015. Modeling and Analysis of Compositional Data. [Google Scholar]
- 63.Tong A., Sainsbury P., Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care. 2007;19(6):349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 64.Kwon S., Janz K.F., Letuchy E.M., Burns T.L., Levy S.M. Parental characteristic patterns associated with maintaining healthy physical activity behavior during childhood and adolescence. Int. J. Behav. Nutr. Phys. Act. 2016;13:58. doi: 10.1186/s12966-016-0383-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Jaeschke L., Steinbrecher A., Luzak A., Puggina A., Aleksovska K., Buck C., Burns C., Cardon G., Carlin A., Chantal S., Ciarapica D., Condello G., Coppinger T., Cortis C., De Craemer M., D'Haese S., Di Blasio A., Hansen S., Iacoviello L., Issartel J., Izzicupo P., Kanning M., Kennedy A., Ling F.C., Napolitano G., Nazare J.A., Perchoux C., Polito A., Ricciardi W., Sannella A., Schlicht W., Sohun R., MacDonncha C., Boccia S., Capranica L., Schulz H., Pischon T. Socio-cultural determinants of physical activity across the life course: a ‘Determinants of Diet and Physical Activity’ (DEDIPAC) umbrella systematic literature review. Int. J. Behav. Nutr. Phys. Act. 2017;14(1):173. doi: 10.1186/s12966-017-0627-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wilk P., Clark A.F., Maltby A., Smith C., Tucker P., Gilliland J.A. Examining individual, interpersonal, and environmental influences on children's physical activity levels. SSM - Population Health. 2018;4:76–85. doi: 10.1016/j.ssmph.2017.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Craig P., Dieppe P., Macintyre S., Michie S., Nazareth I., Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. Int. J. Nurs. Stud. 2013;50(5):587–592. doi: 10.1016/j.ijnurstu.2012.09.010. [DOI] [PubMed] [Google Scholar]