Abstract
Purpose of Review
The purpose of this manuscript is to 1 define the features associated with borderline acetabular dysplasia and 2 review current status of diagnostic algorithms and treatment options for borderline dysplasia.
Recent Findings
Acetabular dysplasia is a common cause of hip pain secondary to insufficient coverage of the femoral head by the bony acetabulum. Historical classification of acetabular dysplasia has utilized the lateral center edge angle (LCEA); values above 25° are normal and below 20° are considered pathologic. Borderline dysplasia describes hips with LCEA between 20 and 25o; treatment of these patients is controversial.
Summary
While many studies utilize LCEA in classification of borderline dysplasia, isolated reliance on measurement of lateral femoral head coverage to define severity of undercoverage will continue to mislabel morphology. Thorough assessment of the characteristics of mild acetabular undercoverage is necessary for future studies, which will allow effective comparisons of results between hip arthroscopy and periacetabular osteotomy.
Keywords: Hip dysplasia, Acetabular dysplasia, Borderline hip, Mild hip dysplasia, Periacetabular osteotomy, Lateral center edge angle
Introduction
Acetabular dysplasia is a well-recognized cause of hip pain and dysfunction with an associated risk of developing osteoarthritis (OA) [4, 9, 13, 19]. In this condition, insufficient coverage of the femoral head by the acetabulum leads to excessive joint contact pressures and subsequent accelerated joint degeneration. Quantification of femoral head coverage is historically based on the lateral center-edge angle (LCEA), described by Wiberg in 1939 [55]. The magnitude of the LCEA has been linked to the progression of OA even in the absence of symptoms during early adulthood [39], with one study noting a 13% increased likelihood of developing OA for each 1° loss of lateral coverage below 28° [49].
Reorientation of the acetabulum is the standard treatment of symptomatic acetabular dysplasia, as it permits repositioning of the available weight-bearing cartilage into a functional position. The periacetabular osteotomy (PAO), first described by Ganz, has become the standard treatment of symptomatic acetabular dysplasia as it permits acetabular reorientation to optimize acetabular coverage while maintaining posterior column integrity [22]. Numerous studies have characterized the success of PAO in the treatment of acetabular dysplasia, typically in cases with a preoperative LCEA < 17°, at both intermediate and long-term follow-up [22, 32, 48, 52].
Incomplete characterization of the pathology of borderline hip dysplasia continues to cloud treatment strategies. While the LCEA is a commonly used measurement modality in classifying hip dysplasia, it can mischaracterize or underdiagnose the nature of certain forms of acetabular undercoverage or other underlying hip pathology. A number of other radiographic measurements have been described in the assessment of hip dysplasia. Additionally, cross-sectional imaging has become a useful adjunct in preoperative planning. The purpose of this review is to discuss the current status of diagnosis and treatment options for borderline hip dysplasia.
Borderline Dysplasia
What Is “Borderline” Dysplasia?
According to Wiberg’s original description, hips with LCEA below 20° were considered pathologic and hips with LCEA over than 25° were normal. Hips with LCEA between 20 and 25o were considered uncertain. This uncertainty has created confusion in the literature concerning the spectrum of acetabular dysplasia severity, and nonspecific terms such as mild dysplasia [21, 29, 33, 37, 44, 53] and borderline dysplasia [5, 6, 11, 12, 14, 15, 20, 24, 27, 40] have been interchangeably used to describe these hips. The majority of currently available literature on these hips come from hip arthroscopy studies, and the definitions of “mild” and “borderline” coverage have varied from as low as 16° to as high as 28° (Table 1). Only a select few studies considered other radiographic parameters, such as the Tonnis angle, Sharp angle, or anterior center edge angle (ACEA) [27, 30].
Table 1.
Classification of borderline acetabular dysplasia in orthopedic literature. LCEA, lateral center edge angle; ACEA, anterior center edge angle
| Study | Procedure | Dysplasia measurement |
|---|---|---|
| Byrd and Jones | Arthroscopy | LCEA 20–25° |
| Domb et al. | Arthroscopy | LCEA 18–25° |
| Dwyer et al. | Arthroscopy | LCEA 22–28° |
| Fukui et al. | Arthroscopy | LCEA 20–25° |
| Kalore and Janek | Arthroscopy | LCEA < 25°, Sharp angle < 40°, ACEA < 25° |
| Larson et al. | Arthroscopy | LCEA < 25°, Tonnis angle > 10° |
| Matsuda et al. | Arthroscopy | LCEA 16–24° |
| McCarthy and Lee | Arthroscopy | LCEA 22–28° |
| Nawabi et al. | Arthroscopy | LCEA 18–25° |
| Ricciardi et al. | Periacetabular osteotomy | LCEA 18–25° |
| McClincy et al. | Periacetabular osteotomy | LCEA 18–25° |
| Irie et al. | Periacetabular osteotomy | LCEA 15–24° |
| Bolia et al. | Arthroscopy | LCEA 20–25° |
| Mimura et al. | None | LCEA 20–24, Sharp Angle 42–45° |
| Maldonado et al. | Arthroscopy | LCEA 18–25° |
How Do We Treat Borderline Dysplasia?
While acetabular reorientation with PAO is the generally accepted treatment for “traditional” hip dysplasia (LCEA < 17), the ideal treatment of borderline dysplasia remains controversial. Surgical treatment of borderline dysplasia has been advocated both through addressing the bony (PAO) or intra-articular (hip arthroscopy) components of the pathology. Proponents of PAO tout its ability to address the structural deformity which gives rise to the associated soft tissue issues (labral tears, capsular attenuation, etc.), at the expense of a greater surgical exposure with a prolonged recovery and higher potential complications. Proponents of hip arthroscopy to address the effected capsular and intra-articular structures (labral repair, cam-type femoral deformity resection, capsular repair, and/or plication) tout the minimally invasive approach and its expedited recovery at the expense of leaving the acetabular bony pathology unchanged.
Arthroscopic interventions to address the soft tissue pathology of borderline acetabular dysplasia have been described with variable success [4, 6, 15, 21, 26, 27, 30, 33, 40]. Several studies have shown good functional results of hip arthroscopy for the treatment of intra-articular pathology in patients with borderline dysplasia at short-term follow-up [6, 15, 26, 27, 40], while other studies noted inferior results of arthroscopy in patients with dysplasia [27, 30, 33]. A systematic review of hip arthroscopy in dysplastic patients noted a 14.1% revision rate and 9.5% rate of progression to total hip arthroplasty at an average of 29 months following hip arthroscopy [57••]. Two studies to date have focused specifically on outcomes of PAO in patients with LCEA between 18 and 25°, with improved patient reported outcomes and minimal complications at 1 year and 2 years postoperatively [34••, 46]. In the ANCHOR cohort, patients with “mild” dysplasia (LCEA > 15) did well following PAO but their improvements were not as significant as patients with more severe preoperative dysplasia [8].
Why Are We Failing?
The results of surgical outcomes for borderline dysplasia are variable at best. The unpredictability of results, especially with hip arthroscopy, may be attributable to a highly variable degree of acetabular morphology in patients with LCEA 18–25° when considering all radiographic measures of acetabular coverage. The LCEA is a reliable measure of lateral acetabular coverage, but is not a surrogate for the global morphology of the acetabulum. Other features of interest in these borderline hips include the anterior and posterior acetabular coverage, proximal femoral morphology, and rotational alignment of the proximal femur and acetabulum. All of these features should be evaluated and considered during the diagnostic evaluation of the symptomatic hip with borderline dysplasia, and better understanding of the global morphology of the hip may improve our surgical decision-making.
Imaging Evaluation of Borderline Dysplasia
Thorough imaging of non-arthritic hip disorders such as femoroacetabular impingement (FAI) and acetabular dysplasia are essential to develop appropriate treatment plans for these patients. The routine imaging evaluation typically begins with plain radiographs to develop an overall understanding of femoral and acetabular morphology. Ancillary imaging, such as CT and MRI are also frequently employed in these patients preoperatively to improve our understanding of the bony and soft tissue anatomy, respectively. With the increased utilization of ultrasound imaging for musculoskeletal pathology, its use will also likely expand in the diagnostic evaluation of hip pain. In the following sections, we will discuss each of these imaging modalities and note relevant measurements to aid in the evaluation of the borderline dysplastic hip.
Radiographs
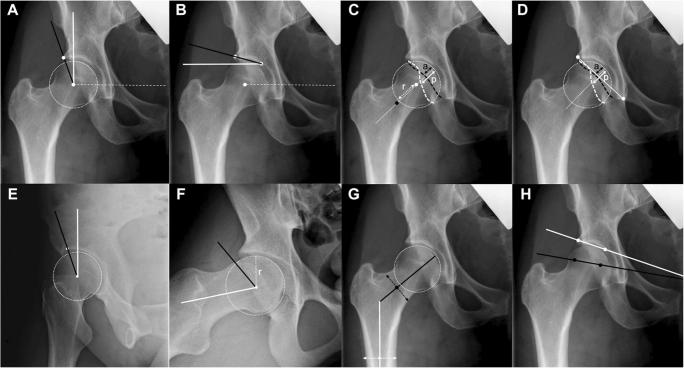
Plain radiographs remain the standard first-line imaging modality for the majority of non-arthritic hip disorders. Clohisy et al. have provided a comprehensive review of non-arthritic hip radiography, providing practical details on the acquiring and interpretation of hip radiographs [7]. The typical radiographic sequence obtained in these individuals includes an AP pelvis (with attention to proper positioning and alignment), 45o Dunn-lateral, and false profile views. With this group of radiographs, it is possible to thoroughly evaluate much of the proximal femoral and acetabular morphology. The characterization of hip pathology using radiographic measures continues to be an evolving field. Several measurements utilized are the femoral neck-shaft angle (FNSA) [3], alpha angle [1], lateral center edge angle (LCEA) [55], anterior/ventral center edge angle (ACEA), Tonnis roof angle [50], anterior wall index (AWI) and posterior wall index (PWI) [47], and the femoral-epiphyseal acetabular roof (FEAR) index [56]. The relevant radiographic features to review will be discussed in this section, and pictorial descriptions can be found in Fig. 1.
Fig. 1.
Radiographic features of the proximal femur and acetabulum relevant to the diagnostic evaluation of borderline dysplasia. a Lateral center-edge angle (LCEA): angle formed between a perpendicular line (white line) to the line that connects the center of the femoral heads (white dashed lines) and a line (black line) that connects the center of the femoral head to the most lateral point of the acetabular sourcil. b Tönnis angle: angle formed between a line (black line) drawn between the most lateral and most medial points of the acetabular sourcil and a parallel line (white line) to the line (white dashed line) connecting the center of the femoral heads. c Anterior wall index (AWI) and posterior wall index (PWI): the femoral neck axis (white dashed line) is drawn from the midpoint of the neck to the center of the femoral head. The radius (r) of the femoral head is drawn (dashed white arrow) in line with the axis of the femoral neck. The point at which the axis of the femoral neck passes through the anterior wall and the point at which the axis of the femoral neck passes through the posterior wall are marked. The AWI is calculated by dividing distance “a” (black arrow) by the radius of the femoral head. The PWI is calculated by dividing distance “p” (white arrow) by the radius of the femoral head. d Posterior to anterior wall (P/A) index: the most lateral aspect of the acetabulum and the most inferior point of the tear drop point are connected by a line (solid white line), and a perpendicular line (white dashed line) is drawn at its midpoint. The acetabular articular surface is marked (white dashed circle). The distances from the anterior (black arrow) and posterior (white arrow) walls to the acetabular articular surface are measured, and the P/A index is calculated as p/a. e Anterior center-edge angle (ACEA): in the false profile radiograph, the center of the femoral head is marked, and a longitudinal line (white line) passing through the center of the femoral head is drawn. The ACEA is the angle formed by this line and a line connecting the center of the femoral head to the most anterior point of the acetabular sourcil (black line). f Alpha angle: the femoral neck axis is drawn by connecting the center of the femoral neck to the center of the femoral head (solid white line). A perfect circle is drawn around the femoral head, and the radius of the femoral head is measured (dashed white line, distance “r”). The point at which the distance from the center of the head exceeds the radius of the femoral head is marked. The alpha angle is the angle formed by a line connecting the center of the femoral head to the point at which the distance from the center of the head exceeds the radius of the femoral head (black line) and the femoral neck axis (white line). g Femoral neck-shaft angle: angle formed between the axis of the femoral neck (black line) and the longitudinal axis of the femoral shaft (white line). The width of the femoral neck (black dashed line) and the width of the femoral shaft (white dashed line) are drawn. h Femoral epiphyseal acetabular roof (FEAR) index: angle formed between a line (black line) representing the physeal scar of the femoral head and a line connecting the most medial and lateral points of the acetabular sourcil (white line). (Reprinted with permissions [35])
LCEA
The lateral center edge angle (LCEA) is a radiographic assessment of lateral acetabular coverage in the frontal plane using an AP pelvis radiograph. Multiple methods of performing the measurement have been described. First described by Wiberg et al., the measurement is formed by a vertical line (or parallel to long axis of the body) starting from the center of the femoral head with a line to the most lateral point of the acetabular roof [55]. A LCEA value of greater than 20° (patients age 3–17) or 25° (adults) is considered “normal.” Values less than 15° (patients age 3–17) or 20° (adults) are considered pathologic [18]. Hips with LCEA between these value ranges (15–20° in children and adolescents and 20–25° in adults) are considered “intermediate” or “uncertain” and treatment strategies are controversial.
Tonnis Angle
The Tonnis angle, or the “acetabular roof angle of Tonnis” or the “acetabular index” attempts to quantify the acetabular sourcil, or the weight-bearing portion of the acetabular roof [50]. The measurement is performed using an AP pelvis radiograph and is formed between a horizontal line and a tangential line extending from the medial edge to the lateral edge of the sourcil. Values greater than 13° are considered abnormal. The medial edge of the sourcil can be difficult to distinguish in some patients. The modified Tonnis angle was described as an alternative method in cases where the medial edge was unclear; in this method, the vertex of the femoral head was used as the site of a parallel line to the horizontal plane [16]. The point at which this line contacted the acetabulum was used as the medial edge for the tangential line towards the lateral point of the sourcil. The Tonnis angle and modified Tonnis angles have been observed to have a high degree of correlation in cases without joint space narrowing and subluxation of the hip.
AWI/PWI
The anterior wall index (AWI) and posterior wall index (PWI) attempt to characterize acetabular pathomorphology by quantifying the anterior and posterior acetabular coverage [47]. The measurement is performed using AP pelvis radiographs; the first step is to make a best fitting circle around the femoral head. A line is then drawn down the center of the femoral neck intersecting the center of the circle for the femoral head. The distance along this line was recorded from the edge of the circle measuring to the femoral head to the edge of the anterior wall (A) or the posterior wall (P). The AWI and PWI is calculated by dividing the measurement of the anterior wall coverage (A) or posterior wall coverage (P) by the radius of the femoral head circle. The average AWI for a normal hip was 0.41 with 0.28 for dysplastic hips and 0.61 for deep acetabuli. The average PWI for a normal hip was 0.91 with 0.81 for dysplastic hips and 1.15 for deep acetabuli.
ACEA
The anterior/ventral center edge angle (ACEA) utilizes the false-profile radiograph to evaluate the anterior acetabular coverage of the femoral head. The angle is measured by a vertical line through the center of the femoral head and a second line through the center of the hip towards the most anterior aspect of the acetabular dome [31]. Values less than 20° are considered abnormal [10].
FNSA
The femoral neck-shaft angle (FNSA), first described by Muller [38], is performed to quantify the degree of coxa vara or coxa valga. It is performed by measuring the angle between the mid-point of the femoral neck and the long axis of the femoral shaft. Variability exists in the method of performing the FNSA; one recent study comparing methods of measurement reported the best results with forming the femoral neck line from the center of a best fit circle around the femoral head. Femoral version should be considered in performing this measurement, as rotational changes can change the apparent FNSA on AP pelvis radiographs [28].
Alpha Angle
A common measurement used to assess for cam deformity is the alpha angle [43]. The alpha angle attempts to quantify the degree at which the femoral head transitions from being spherical. It is measured from the AP pelvis and Dunn lateral radiographs by first drawing a best fitting circle around the femoral head. Using the marker from the center of the femoral head, one line is drawn through the center of the femoral neck. A second neck is drawn to the point at which the femoral head loses its sphericity. The angle created by these two lines is the alpha angle. The thresholds for diagnosing cam have been debated, with values ranging from 50 to 83° indicating moderate to severe cam [1].
FEAR Index
The femoral-epiphyseal acetabular roof (FEAR) index was developed to assess for pathologic behavior in borderline dysplastic hips [56]. Using standard AP pelvic radiographs, the central third portion of the physeal scar of the femoral head is identified, and the most medial and lateral points of the straight section are used to create a line. The second portion of the angle is defined by the most medial and lateral points of the acetabular sourcil. The FEAR index can be either positive (angle facing laterally with apex medially) or negative (angle facing medially with apex laterally). The initial investigation of this measurement reported that painful hips with a LCEA under 25° and FEAR index less than 5° are likely to be stable, supporting a diagnosis of FAI rather than instability.
Cross Sectional Imaging
Obtaining information regarding anterior and posterior acetabular coverage, proximal femoral morphology, and rotational alignment of the femur and acetabulum is crucial in decision-making before potential surgical intervention in borderline hips. Three-dimensional (3D) imaging is a useful adjunct in the assessment and management of borderline hips. As the hip joint is a complex 3D structure, CT and MRI are able to provide additional details about specific anatomy and global morphology.
Ct
CT imaging is increasingly performed in the preoperative setting to characterize bony anatomy. The characterization of acetabular coverage in normal asymptomatic patients has been described, and several authors have previously characterized acetabular dysplasia on CT. Nepple et al. described a method of utilizing CT for determining variability in 3D acetabular deficiency and morphology [42••]. Also, by including cuts of the distal femur, CT enables precise calculation of both acetabular and femoral version [58]. Acetabular and femoral versions, and their combined relationship, impact the overall function of the hip and can predispose to either instability or impingement [17, 36]. Recent advancements have allowed for high quality CT imaging with much lower radiation exposure than previous testing [41].
MRI
MRI is the most commonly utilized non-invasive test for assessment of soft tissue structures in the assessment of the non-arthritic hip. In planning for surgical intervention, MRI can determine the presence of ligamentous, capsular, labral, tendinous, or osteochondral pathology. Alternative causes of hip pain, such as femoral neck stress fracture, avascular necrosis, or pigmented villonodular synovitis are also best evaluated with MRI. MRI arthrogram has been reported to have the best correlative results with arthroscopy, with labral tears having 92% sensitivity and 100% specificity [51]. However, one recent study suggested that non-arthrogramic hip MRI was a successful screening test for presence of labral tears, chondral defects, and ligamentum teres tears or synovitis [2]. In addition to providing details regarding intracapsular soft tissues, MRI also allows visualization of pericapsular structures. A small muscle overlying the anterior hip capsule called the iliocapsularis has been postulated as a secondary stabilizer of the hip capsule [54]. In dysplastic hips with deficient acetabular coverage, the iliocapsularis has been observed to be more prominent and hypertrophied. Conversely, the iliocapsularis is frequently diminutive and atrophied in stable hips with adequate acetabular coverage. Using MRI to define the iliocapsularis has been described as a useful preoperative decision-making tool in assessing hip stability in patients with borderline hip dysplasia [23]. MRI assessment of the iliocapsularis utilizes the axial T1-weighted image to define both the muscle morphology and degree of fatty infiltration at two points (4 cm below the AIIS and on first section inferior to the femoral head). Patients with deficient acetabular coverage were observed to have increased thickness, width, circumference, cross-sectional area, and partial volume of the iliocapsularis muscle and decreased fatty infiltration.
Imaging Clusters
We recently reviewed the comprehensive preoperative radiographic parameters of patients undergoing hip preservation surgery with “mild” or “borderline” dysplasia (LCEA 18–25°) at a tertiary referral center [35]. Ninety-nine patients underwent either hip arthroscopy or PAO over a 5-year period, and their preoperative imaging was reviewed for LCEA, Tonnis Angle, AWI/PWI, ACEA, FNSA, Alpha Angle (AP and Dunn views), and FEAR Index.
A cluster analysis was performed in an attempt to identify certain morphological groups within the overall patient cohort. We noted that males and females had fairly distinct morphologies, so sex-specific cluster analyses were performed. The cluster groups are presented in Table 2. Male patients showed 3 morphologic clusters: global impingement (high alpha angle on AP/Dunn and low PWI), focal impingement (high alpha angle on Dunn and low PWI), and isolated lateral acetabular insufficiency (low LCEA). Female patients also had 3 morphologic clusters: impingement (high alpha angle on AP/Dunn), anterolateral acetabular deficiency (low LCEA, low AWI, low ACEA, high FEAR), and isolated lateral acetabular insufficiency (low LCEA).
Table 2.
Male and female borderline acetabular dysplasia categories based upon radiographic parameters. AP, anteroposterior; LCEA, lateral center edge angle; ACEA, anterior center edge angle; AWI, anterior wall index
| Male borderline clusters | Female borderline clusters | |||||
|---|---|---|---|---|---|---|
| Global impingement | Focal impingement | Lateral deficiency | Cluster | Impingement | Anterolateral deficiency | Lateral deficiency |
| 35% | 40% | 25% | Incidence | 16% | 58% | 26% |
| Cam morphology on AP and Dunn | Cam morphology on Dunn | Normal proximal femur | Femoral morphology | Cam morphology on AP and Dunn | Normal proximal femur | Normal proximal femur |
| Superior acetabular retroversion and low LCEA | Superior acetabular retroversion and low LCEA | Isolated low LCEA | Acetabular morphology | Isolated low LCEA | Combed lower lateral (LCEA) and anterior (AWI, ACEA) coverage | Isolated low LCEA |
Using these patient clusters as a baseline, a reconsideration of the available literature is appropriate. Three patient clusters, two in males (global impingement and focal impingement) and one in females (impingement) had morphological features consistent with femoroacetabular impingement. These clusters were specifically targeted in the study by Nawabi et al., who described the outcomes of hip arthroscopy for cam resection and capsulolabral repair in patients with LCEA 18–25° [40]. They noted results comparable to those found in patients with normal acetabular coverage undergoing arthroscopic cam resection.
The anterolateral acetabular deficiency cluster in females showed numerous features of acetabular dysplasia. Not uncommonly, the borderline LCEA measurement was their most normal acetabular feature, and their anterior coverage was consistently suboptimal. A recent study noted that inadequate anterior acetabular coverage was predictive of poor outcomes following hip arthroscopy [25]. Two recent studies on PAO outcomes in patients with borderline dysplasia showed significant functional improvements with low rates of complications and failures at short-term follow-up [34, 45]. One of these studies noted that the majority of PAO patients had numerous radiographic features of dysplasia aside from LCEA measurement, and that anterior coverage was the most commonly deficient region [34••].
Conclusions
The management of borderline dysplasia is an active controversy in the field of hip preservation. Much of the literature, up to this point, has isolated the definition of borderline dysplasia to the LCEA measurement. As awareness of the variable deformities present in acetabular dysplasia increases, isolated reliance on measurement of lateral femoral head coverage to define severity of undercoverage will continue to mislabel patients. Future studies should strive to more thoroughly define the characteristics of mild acetabular undercoverage, which will enable meaningful comparative effectiveness studies between hip arthroscopy and periacetabular osteotomy in the treatment of acetabular dysplasia in these patients. These studies can strive to help identify the patient subgroups to treat with either a hip arthroscopy or periacetabular osteotomy.
Compliance with Ethical Standards
Conflict of Interest
The authors declare no relevant conflicts of interest.
Human and Animal Rights
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Footnotes
This article is part of the Topical Collection on Pediatric Orthopedics
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
- 1.Agricola R, Heijboer MP, Bierma-Zeinstra SM, Verhaar JA, Weinans H, Waarsing JH. Cam impingement causes osteoarthritis of the hip: a nationwide prospective cohort study (CHECK) Ann Rheum Dis. 2013;72:918–923. doi: 10.1136/annrheumdis-2012-201643. [DOI] [PubMed] [Google Scholar]
- 2.Annabell L, Master V, Rhodes A, Moreira B, Coetzee C, Tran P. Hip pathology: the diagnostic accuracy of magnetic resonance imaging. J Orthop Surg Res. 2018;13:127. doi: 10.1186/s13018-018-0832-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boese CK, Dargel J, Oppermann J, Eysel P, Scheyerer MJ, Bredow J, Lechler P. The femoral neck-shaft angle on plain radiographs: a systematic review. Skelet Radiol. 2016;45:19–28. doi: 10.1007/s00256-015-2236-z. [DOI] [PubMed] [Google Scholar]
- 4.Byrd JW, Jones KS. Hip arthroscopy in the presence of dysplasia. Arthroscopy. 2003;19:1055–1060. doi: 10.1016/j.arthro.2003.10.010. [DOI] [PubMed] [Google Scholar]
- 5.Chaharbakhshi EO, Perets I, Ashberg L, Mu B, Lenkeit C, Domb BG. Do ligamentum teres tears portend inferior outcomes in patients with borderline dysplasia undergoing hip arthroscopic surgery? A match-controlled study with a minimum 2-year follow-up. Am J Sports Med. 2017;45:2507–2516. doi: 10.1177/0363546517710008. [DOI] [PubMed] [Google Scholar]
- 6.Chandrasekaran S, Darwish N, Martin TJ, Suarez-Ahedo C, Lodhia P, Domb BG. Arthroscopic capsular plication and labral seal restoration in borderline hip dysplasia: 2-year clinical outcomes in 55 cases. Arthroscopy. 2017;33:1332–1340. doi: 10.1016/j.arthro.2017.01.037. [DOI] [PubMed] [Google Scholar]
- 7.Clohisy JC, Carlisle JC, Beaule PE, Kim YJ, Trousdale RT, Sierra RJ, Leunig M, Schoenecker PL, Millis MB. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg (Am Vol) 2008;90(Suppl 4):47–66. doi: 10.2106/JBJS.H.00756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clohisy JC, Ackerman J, Baca G, Baty J, Beaule PE, Kim YJ, Millis MB, Podeszwa DA, Schoenecker PL, Sierra RJ, Sink EL, Sucato DJ, Trousdale RT, Zaltz I. Patient-reported outcomes of periacetabular osteotomy from the prospective ANCHOR cohort study. J Bone Joint Surg (Am Vol) 2017;99:33–41. doi: 10.2106/JBJS.15.00798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cooperman D. What is the evidence to support acetabular dysplasia as a cause of osteoarthritis? J Pediatr Orthop. 2013;33(Suppl 1):S2–S7. doi: 10.1097/BPO.0b013e3182770a8d. [DOI] [PubMed] [Google Scholar]
- 10.Crockarell JR, Jr, Trousdale RT, Guyton JL. The anterior centre-edge angle. A cadaver study. J Bone Joint Surg (Br) 2000;82:532–534. doi: 10.1302/0301-620x.82b4.10063. [DOI] [PubMed] [Google Scholar]
- 11.Cvetanovich GL, Levy DM, Weber AE, Kuhns BD, Mather RC, 3rd, Salata MJ, Nho SJ. Do patients with borderline dysplasia have inferior outcomes after hip arthroscopic surgery for femoroacetabular impingement compared with patients with normal acetabular coverage? Am J Sports Med. 2017;45:2116–2124. doi: 10.1177/0363546517702855. [DOI] [PubMed] [Google Scholar]
- 12.Domb BG, Stake CE, Lindner D, El-Bitar Y, Jackson TJ. Arthroscopic capsular plication and labral preservation in borderline hip dysplasia: two-year clinical outcomes of a surgical approach to a challenging problem. Am J Sports Med. 2013;41:2591–2598. doi: 10.1177/0363546513499154. [DOI] [PubMed] [Google Scholar]
- 13.Domb BG, Lareau JM, Baydoun H, Botser I, Millis MB, Yen YM. Is intraarticular pathology common in patients with hip dysplasia undergoing periacetabular osteotomy? Clin Orthop Relat Res. 2014;472:674–680. doi: 10.1007/s11999-013-3140-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Domb BG, Chaharbakhshi EO, Perets I, Yuen LC, Walsh JP, Ashberg L. Hip arthroscopic surgery with labral preservation and capsular plication in patients with borderline hip dysplasia: minimum 5-year patient-reported outcomes. Am J Sports Med. 2017;363546517743720. [DOI] [PubMed]
- 15.Evans PT, Redmond JM, Hammarstedt JE, Liu Y, Chaharbakhshi EO, Domb BG. Arthroscopic treatment of hip pain in adolescent patients with borderline dysplasia of the hip: minimum 2-year follow-up. Arthroscopy. 2017;33:1530–1536. doi: 10.1016/j.arthro.2017.03.008. [DOI] [PubMed] [Google Scholar]
- 16.Fa L, Wang Q, Ma X. Superiority of the modified Tonnis angle over the Tonnis angle in the radiographic diagnosis of acetabular dysplasia. Exp Ther Med. 2014;8:1934–1938. doi: 10.3892/etm.2014.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fabricant PD, Fields KG, Taylor SA, Magennis E, Bedi A, Kelly BT. The effect of femoral and acetabular version on clinical outcomes after arthroscopic femoroacetabular impingement surgery. J Bone Joint Surg (Am Vol) 2015;97:537–543. doi: 10.2106/JBJS.N.00266. [DOI] [PubMed] [Google Scholar]
- 18.Fredensborg N. The CE angle of normal hips. Acta Orthop Scand. 1976;47:403–405. doi: 10.3109/17453677608988709. [DOI] [PubMed] [Google Scholar]
- 19.Fujii M, Nakashima Y, Jingushi S, Yamamoto T, Noguchi Y, Suenaga E, Iwamoto Y. Intraarticular findings in symptomatic developmental dysplasia of the hip. J Pediatr Orthop. 2009;29:9–13. doi: 10.1097/BPO.0b013e318190a0be. [DOI] [PubMed] [Google Scholar]
- 20.Fukui K, Briggs KK, Trindade CA, Philippon MJ. Outcomes after labral repair in patients with femoroacetabular impingement and borderline dysplasia. Arthroscopy. 2015;31:2371–2379. doi: 10.1016/j.arthro.2015.06.028. [DOI] [PubMed] [Google Scholar]
- 21.Fukui K, Trindade CA, Briggs KK, Philippon MJ. Arthroscopy of the hip for patients with mild to moderate developmental dysplasia of the hip and femoroacetabular impingement: outcomes following hip arthroscopy for treatment of chondrolabral damage. Bone Joint J. 2015;97-B:1316–1321. doi: 10.1302/0301-620X.97B10.35303. [DOI] [PubMed] [Google Scholar]
- 22.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res. 1988:26–36. [PubMed]
- 23.Haefeli PC, Steppacher SD, Babst D, Siebenrock KA, Tannast M. An increased iliocapsularis-to-rectus-femoris ratio is suggestive for instability in borderline hips. Clin Orthop Relat Res. 2015;473:3725–3734. doi: 10.1007/s11999-015-4382-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hatakeyama A, Utsunomiya H, Nishikino S, Kanezaki S, Matsuda DK, Sakai A, Uchida S. Predictors of poor clinical outcome after arthroscopic labral preservation, capsular plication, and cam osteoplasty in the setting of borderline hip dysplasia. Am J Sports Med. 2018;46:135–143. doi: 10.1177/0363546517730583. [DOI] [PubMed] [Google Scholar]
- 25.Ibrahim MM, Poitras S, Bunting AC, Sandoval E, Beaule PE. Does acetabular coverage influence the clinical outcome of arthroscopically treated cam-type femoroacetabular impingement (FAI)? Bone Joint J. 2018;100-B:831–838. doi: 10.1302/0301-620X.100B7.BJJ-2017-1340.R2. [DOI] [PubMed] [Google Scholar]
- 26.Jayasekera N, Aprato A, Villar RN. Hip arthroscopy in the presence of acetabular dysplasia. Open Orthop J. 2015;9:185–187. doi: 10.2174/1874325001509010185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kalore NV, Jiranek WA. Save the torn labrum in hips with borderline acetabular coverage. Clin Orthop Relat Res. 2012;470:3406–3413. doi: 10.1007/s11999-012-2499-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kay RM, Jaki KA, Skaggs DL. The effect of femoral rotation on the projected femoral neck-shaft angle. J Pediatr Orthop. 2000;20:736–739. doi: 10.1097/00004694-200011000-00007. [DOI] [PubMed] [Google Scholar]
- 29.Lane NE, Lin P, Christiansen L, Gore LR, Williams EN, Hochberg MC, Nevitt MC. Association of mild acetabular dysplasia with an increased risk of incident hip osteoarthritis in elderly white women: the study of osteoporotic fractures. Arthritis Rheum. 2000;43:400–404. doi: 10.1002/1529-0131(200002)43:2<400::AID-ANR21>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 30.Larson CM, Ross JR, Stone RM, Samuelson KM, Schelling EF, Giveans MR, Bedi A. Arthroscopic management of dysplastic hip deformities: predictors of success and failures with comparison to an arthroscopic FAI cohort. Am J Sports Med. 2016;44:447–453. doi: 10.1177/0363546515613068. [DOI] [PubMed] [Google Scholar]
- 31.Lequesne M, de Seze False profile of the pelvis. A new radiographic incidence for the study of the hip. Its use in dysplasias and different coxopathies. Rev Rhum Mal Osteoartic. 1961;28:643–652. [PubMed] [Google Scholar]
- 32.Matheney T, Kim YJ, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg (Am Vol) 2009;91:2113–2123. doi: 10.2106/JBJS.G.00143. [DOI] [PubMed] [Google Scholar]
- 33.Matsuda DK, Gupta N, Khatod M, Matsuda NA, Anthony F, Sampson J, Burchette R. Poorer arthroscopic outcomes of mild dysplasia with cam femoroacetabular impingement versus mixed femoroacetabular impingement in absence of capsular repair. Am J Orthop (Belle Mead NJ) 2017;46:E47–E53. [PubMed] [Google Scholar]
- 34.•• McClincy MP, Wylie JD, Kim YJ, Millis MB, Novais EN. Periacetabular osteotomy improves pain and function in patients with lateral center-edge angle between 18 degrees and 25 degrees, but are these hips really borderline sysplastic? Clin Orthop Relat Res. 2018; BACKGROUND: The treatment of mild or borderline acetabular dysplasia is controversial with surgical options including both arthroscopic labral repair with capsular closure or plication and periacetabular osteotomy (PAO). The degree to which improvements in pain and function might be achieved using these approaches may be a function of acetabular morphology and the severity of the dysplasia, but detailed radiographic assessments of acetabular morphology in patients with a lateral center-edge angle (LCEA) of 18° to 25° who have undergone PAO have not, to our knowledge, been performed. QUESTIONS/PURPOSES: (1) Do patients with an LCEA of 18° to 25° undergoing PAO have other radiographic features of dysplasia suggestive of abnormal femoral head coverage by the acetabulum? (2) What is the survivorship free from revision surgery, THA, or severe pain (modified Harris hip score [mHHS] < 70) and proportion of complications as defined by the modified Dindo-Clavien severity scale at minimum 2-year followup? (3) What are the functional patient-reported outcome measures in this cohort at minimum 2 years after surgery as assessed by the UCLA Activity Score, the mHHS, the Hip disability and Osteoarthritis Outcome Score (HOOS), and the SF-12 mental and physical domain scores? METHODS: Between January 2010 and December 2014, a total of 91 patients with hip pain and LCEA of 18° to 25° underwent a hip preservation surgical procedure at our institution. Thirty-six (40%) of the 91 patients underwent hip arthroscopy, and 56 hips (60%) were treated by PAO. In general, patients were considered for hip arthroscopy when symptoms were predominantly associated with femoroacetabular impingement (that is, pain aggravated by sitting and hip flexion activities) and physical examination showed a positive anterior impingement test with negative signs of instability (negative anterior apprehension test). In general, patients were considered for PAO when symptoms suggested instability (that is, pain with upright activities, abductor fatigue now aggravated by sitting) and clinical examinations demonstrated a positive anterior apprehension test. Bilateral surgery was performed in six patients and only the first hip was included in the study. One patient was excluded because PAO was performed to address dysplasia caused by surgical excision of a proximal femoral tumor associated with multiple epiphyseal dysplasia during childhood yielding a total of 49 patients (49 hips). There were 46 of 49 females (94%), the mean age was 26.5 years (± 8), and the mean body mass index was 24 kg/m (± 4.5). Radiographic analysis of preoperative films included the LCEA, Tönnis acetabular roof angle, the anterior center-edge angle, the anterior and posterior wall indices, and the Femoral Epiphyseal Acetabular Roof index. Thirty-nine of the 49 patients (80%) were followed for a minimum 2-year followup (mean, 2.2 years; range, 2–4 years) and were included in the analysis of survivorship after PAO, complications, and functional outcomes. Kaplan-Meier modeling was used to calculate survivorship defined as free from revision surgery, THA, or severe pain (mHHS < 70) at minimum 2 years after surgery. Complications were graded according to the modified Dindo-Clavien severity. Patient-reported outcomes were collected preoperatively and at minimum 2 years after surgery and included the UCLA Activity Score, the mHHS, the HOOS, and the SF-12 mental and physical domain scores. RESULTS: Forty-six of 49 hips (94%) had at least one other radiographic feature of dysplasia suggestive of abnormal femoral head coverage by the acetabulum. Seventy-three percent of the hips (36 of 49) had two or more radiographic features of hip dysplasia aside from a LCEA of 18° to 25°. The survivorship of PAO at minimum 2 years for the 39 of 49 (80%) patients available was 94% (95% confidence interval, 80%–90%). Three of 39 patients (8%) developed a complication. At a mean of 2.2 years of followup, there was improvement in level of activity (preoperative UCLA score 7 ± 2 versus postoperative UCLA score 6 ± 2; p = 0.02). Hip symptoms and function improved postoperatively, as reflected by a higher mean mHHS (86 ± 13 versus 64 ± 19; p < 0.001) and mean HOOS (386 ± 128 versus 261 ± 117; p < 0.001). Quality of life and overall health assessed by the physical domain of the SF-12 improved (47 ± 11 versus 39 ± 12; p < 0.001). However, with the numbers available, no improvement was observed for the mental domain of the SF-12 (52 ± 8 versus 51 ± 11; p = 0.881). CONCLUSIONS: Hips with LCEA of 18° to 25° frequently have other radiographic features of dysplasia suggestive of abnormal femoral head coverage by the acetabulum. These hips may be inappropriately labeled as "borderline" or "mild" dysplasia on consideration of LCEA alone. A more comprehensive imaging analysis in these hips by the radiographic features of dysplasia included in this study is recommended to identify hips with abnormal coverage of the femoral head by the acetabulum and to plan treatment accordingly. Patients with LCEA of 18° to 25° showed improvement in hip pain and function after PAO with minimal complications and low proportions of persistent pain or reoperations at short-term followup. Future studies are recommended to investigate whether the benefits of symptomatic and functional improvement are sustained long term.
- 35.McClincy MP, Wylie JD, Yen YM, Novais EN. Mild or borderline hip dysplasia: are we characterizing hips with lateral center-edge angle between 18° and 25° appropriately? Am J Sports Med. 2018; Publication Pending. [DOI] [PubMed]
- 36.McKibbin B. Anatomical factors in the stability of the hip joint in the newborn. J Bone Joint Surg (Br) 1970;52:148–159. [PubMed] [Google Scholar]
- 37.McWilliams DF, Doherty SA, Jenkins WD, Maciewicz RA, Muir KR, Zhang W, Doherty M. Mild acetabular dysplasia and risk of osteoarthritis of the hip: a case-control study. Ann Rheum Dis. 2010;69:1774–1778. doi: 10.1136/ard.2009.127076. [DOI] [PubMed] [Google Scholar]
- 38.Muller ME. Roentgen diagnosis of mechanical hip joint relationships. Radiol Clin. 1957;26:344–354. [PubMed] [Google Scholar]
- 39.Murphy SB, Ganz R, Muller ME. The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome. J Bone Joint Surg Am. 1995;77:985–989. doi: 10.2106/00004623-199507000-00002. [DOI] [PubMed] [Google Scholar]
- 40.Nawabi DH, Degen RM, Fields KG, McLawhorn A, Ranawat AS, Sink EL, Kelly BT. Outcomes after arthroscopic treatment of femoroacetabular impingement for patients with borderline hip dysplasia. Am J Sports Med. 2016;44:1017–1023. doi: 10.1177/0363546515624682. [DOI] [PubMed] [Google Scholar]
- 41.Nepple JJ, Clohisy JC. The dysplastic and unstable hip: a responsible balance of arthroscopic and open approaches. Sports Med Arthrosc Rev. 2015;23:180–186. doi: 10.1097/JSA.0000000000000096. [DOI] [PubMed] [Google Scholar]
- 42.Nepple JJ, Wells J, Ross JR, Bedi A, Schoenecker PL, Clohisy JC. Three patterns of acetabular deficiency are common in young adult patients with acetabular dysplasia. Clin Orthop Relat Res. 2017;475:1037–1044. doi: 10.1007/s11999-016-5150-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg (Br) 2002;84:556–560. doi: 10.1302/0301-620x.84b4.12014. [DOI] [PubMed] [Google Scholar]
- 44.Ricciardi BF, Fields KG, Wentzel C, Nawabi DH, Kelly BT, Sink EL. Complications and short-term patient outcomes of periacetabular osteotomy for symptomatic mild hip dysplasia. Hip Int. 2016;0. [DOI] [PubMed]
- 45.Ricciardi BF, Fields KG, Wentzel C, Kelly BT, Sink EL. Early functional outcomes of periacetabular osteotomy after failed hip arthroscopic surgery for symptomatic acetabular dysplasia. Am J Sports Med. 2017;45:2460–2467. doi: 10.1177/0363546517710011. [DOI] [PubMed] [Google Scholar]
- 46.Ricciardi BF, Fields KG, Wentzel C, Nawabi DH, Kelly BT, Sink EL. Complications and short-term patient outcomes of periacetabular osteotomy for symptomatic mild hip dysplasia. Hip Int. 2017;27:42–48. doi: 10.5301/hipint.5000420. [DOI] [PubMed] [Google Scholar]
- 47.Siebenrock KA, Kistler L, Schwab JM, Buchler L, Tannast M. The acetabular wall index for assessing anteroposterior femoral head coverage in symptomatic patients. Clin Orthop Relat Res. 2012;470:3355–3360. doi: 10.1007/s11999-012-2477-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year follow-up of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466:1633–1644. doi: 10.1007/s11999-008-0242-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Thomas GE, Palmer AJ, Batra RN, Kiran A, Hart D, Spector T, Javaid MK, Judge A, Murray DW, Carr AJ, Arden NK, Glyn-Jones S. Subclinical deformities of the hip are significant predictors of radiographic osteoarthritis and joint replacement in women. A 20 year longitudinal cohort study. Osteoarthr Cartil. 2014;22:1504–1510. doi: 10.1016/j.joca.2014.06.038. [DOI] [PubMed] [Google Scholar]
- 50.Tonnis D. Letter: congenital hip dysplasia: clinical and radiological diagnosis (author’s transl) Z Orthop Ihre Grenzgeb. 1976;114:98–99. [PubMed] [Google Scholar]
- 51.Toomayan GA, Holman WR, Major NM, Kozlowicz SM, Vail TP. Sensitivity of MR arthrography in the evaluation of acetabular labral tears. AJR Am J Roentgenol. 2006;186:449–453. doi: 10.2214/AJR.04.1809. [DOI] [PubMed] [Google Scholar]
- 52.Troelsen A, Elmengaard B, Soballe K. Medium-term outcome of periacetabular osteotomy and predictors of conversion to total hip replacement. J Bone Joint Surg (Am Vol) 2009;91:2169–2179. doi: 10.2106/JBJS.H.00994. [DOI] [PubMed] [Google Scholar]
- 53.Ueshima K, Takahashi KA, Fujioka M, Arai Y, Horii M, Asano T, Hirata T, Suehara H, Tanaka T, Kubo T. Relationship between acetabular labrum evaluation by using radial magnetic resonance imaging and progressive joint space narrowing in mild hip dysplasia. Magn Reson Imaging. 2006;24:645–650. doi: 10.1016/j.mri.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 54.Ward W. Timothy, Fleisch Isabelle-D??sir??e, Ganz Reinhold. Anatomy of the Iliocapsularis Muscle. Clinical Orthopaedics and Related Research. 2000;374:278–285. doi: 10.1097/00003086-200005000-00025. [DOI] [PubMed] [Google Scholar]
- 55.Wiberg G. Shelf operation in congenital dysplasia of the acetabulum and in subluxation and dislocation of the hip. J Bone Joint Surg (Am Vol) 1953;35-A:65–80. [PubMed] [Google Scholar]
- 56.Wyatt M, Weidner J, Pfluger D, Beck M. The femoro-epiphyseal acetabular roof (FEAR) index: a new measurement associated with instability in borderline hip dysplasia? Clin Orthop Relat Res. 2017;475:861–869. doi: 10.1007/s11999-016-5137-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yeung M, Kowalczuk M, Simunovic N, Ayeni OR. Hip arthroscopy in the setting of hip dysplasia: a systematic review. Bone Joint Res. 2016;5:225–231. doi: 10.1302/2046-3758.56.2000533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yoon RS, Koerner JD, Patel NM, Sirkin MS, Reilly MC, Liporace FA. Impact of specialty and level of training on CT measurement of femoral version: an interobserver agreement analysis. J Orthop Traumatol. 2013;14:277–281. doi: 10.1007/s10195-013-0263-x. [DOI] [PMC free article] [PubMed] [Google Scholar]