Abstract
Purpose of Review
The importance of both the static and dynamic stabilizers of the medial elbow for the throwing athlete has been demonstrated in recent studies. Furthermore, recent anatomic studies have demonstrated the insertion of the anterior bundle (UCL) to be more distal and elongated, which has implications for surgical reconstruction of the UCL. The purpose of this review is to highlight recent anatomic and biomechanical studies evaluating the anatomy and reconstructions of the medial elbow.
Recent Findings
Recent literature has highlighted the crucial role of the dynamic stabilizers in resisting valgus force, especially during the throwing motion. The dynamic stabilizers of the medial elbow include the flexor pronator mass, specifically the flexor carpi ulnaris (FCU) and flexor digitorum superficialis (FDS). The clinical importance of these findings cannot be under stated, as unrecognized dynamic stabilizer injury can lead to increased stress on a native or reconstructed UCL in the throwing athlete.
Summary
The medial ulnar collateral ligament complex of the elbow has a crucial role in providing both static and dynamic elbow stability. Most notably, the anterior bundle (UCL) provides the primary resistance to valgus and rotational stresses, especially during throwing motion. An understanding of the humeral and ulnar footprints and their relationships with surrounding structures is necessary to restore the native isometry of the medial complex of the elbow during UCL reconstruction. The flexor pronator musculature plays an essential role in dynamic stability, and the intimate relationship of the FCU and FDS with the ulnar insertion of the UCL should be considered to optimize recovery and outcomes with repair or reconstruction.
Keywords: Elbow, Medial ulnar collateral ligament, Anterior bundle, UCL reconstruction, Valgus stability, Biomechanics
Introduction
The medial elbow is composed of both static and dynamic stabilizers that provide restraint to valgus stress, especially during the throwing motion. The static osseous stabilizers include the radiocaptitellar (RC) and ulnohumeral (UH) articulations. These bony articulations provide stability under 20° and greater than 120° of elbow flexion and provide up to 2° of rotatory stability (RC). The medial ligamentous complex of the elbow is composed of the medial ulnar collateral ligament which is composed of anterior, posterior and oblique bundles. The anterior bundle (also known as the ulnar collateral ligament [UCL]) is the primary restraint to valgus force at the medial elbow and is composed of two separate bands: the anterior band, which is tight in extension, and the posterior bad, which is tight in flexion.
Historically, the dynamic stabilizers of the medial elbow have been less well studied than the static stabilizers. However, recent literature has highlighted the crucial role of the dynamic stabilizers in resisting valgus force, especially during the throwing motion [1••, 2, 3]. The dynamic stabilizers of the medial elbow include the flexor pronator mass, specifically the flexor carpi ulnaris (FCU) and flexor digitorum superficialis (FDS) [4, 5••, 6, 7]. These structures have been shown to be concomitantly injured in throwing athletes who have UCL injuries. The clinical importance of these findings cannot be understated, as unrecognized dynamic stabilizer injury can lead to increased stress on a native or reconstructed UCL in the throwing athlete.
Anatomy of the Medial Elbow Complex Static Stabilizers
The medial elbow collateral ligament complex is composed of three bundles, the anterior bundle, posterior bundle, and oblique bundle. The UCL is the primary static stabilizer to valgus stress on the medial elbow. It primarily acts to resist valgus and extension stress from 70 to 120° of elbow flexion. The posterior and oblique bundles have limited contribution to throwing elbow stability.
Figure 1 demonstrates the 3 bundles of the medial UCL complex and its musculotendinous relationships (Fig. 1).
Fig. 1.

Medial view of an elbow, demonstrating the 3 bundles of the medial ulnar collateral ligament complex. The relationships between the three bundles and the pronator teres (purple) and brachialis (yellow) muscles are also demonstrated. ABUCL (UCL) anterior bundle, FCU ulnar carpi ulnaris, FDS flexor digitorum superficialis, OBUCL oblique bundle, PBUCL posterior bundle
The origin of the UCL attaches 8.5 mm distal and 7.8 mm anterior to the medial epicondyle of the humerus [5••]. The surface area has been reported between 17.0 and 45.5 mm2 respectively [8••, 9•, 10]. This variation in footprint size may be attributed to differences in measurement technique, with the latter of the three studies measuring the footprint in the context of humeral tunnel placement during UCL reconstruction. The anterior position relative to the medial epicondyle is important to understand when considering UCL reconstruction, as posterior tunnel position is a common error and can decrease graft isometry and result in a graft which is overly tight in flexion [11••]. The insertion of the UCL, commonly referred to as the ulnar footprint, was historically thought insert directly on the sublime tubercle without distal extension [12]. However, more recent evidence has demonstrated an elongated, tapered insertion distally along the ulnar ridge [5••, 8••, 9•, 13••]. Based on the most recent studies, the mean surface area of the ulnar insertion of the UCL is 127.2 mm2 (range, 66.4–187.6 mm2) [4, 5••, 10, 12•, 14, 15••, 16•, 17]. The center of the footprint, which was historically thought to be at the apex of the sublime tubercle, has been demonstrated in recent studies to be distal to the center of the sublime tubercle, and average of 5.3 mm (1.5–7.6 mm) [5••, 8••], along the ulnar ridge, which is important to consider as we advance reconstruction techniques in attempt to reproduce native anatomy. (Fig. 2).
Fig. 2.
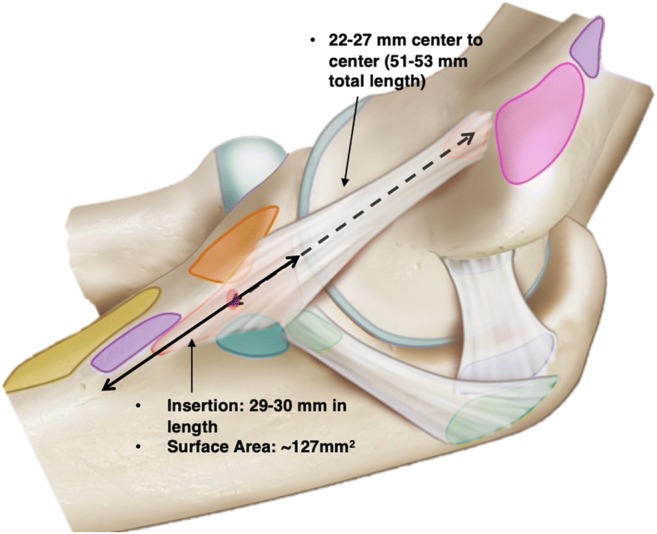
The UCL humeral footprint is 15/3 mm from the joint line, while its ulnar footprint is 5.8–7.8 mm from the joint line. The center of the ulnar footprint is 1.5–7.6 mm distal to the center of the sublime tubercle. The center to center length is 22–27 mm, with the overall length of the anterior band measuring 51–53 mm
There is significant heterogeneity in the literature regarding the true dimensions of the UCL. Based on the most recent studies, the mean length and width of the UCL are 31.9 mm (range, 21.1–53.9 mm) and 5.95 mm (range, 4.5–7.6 mm), respectively [4, 5••, 9•, 12, 14, 15••, 17, 18]. It should be highlighted that many of the reported lengths were measured from center of the humeral origin to the sublime tubercle, whereas more recent studies have measured total length from the humeral insertion to the more distal, tapered insertion along the ulnar ridge. The differences in total length and ulnar insertion surface area are likely due to the newly accepted more elongated, distal humeral insertion (Fig. 3).
Fig. 3.

Medial view of elbow demonstrating the more distal and elongated insertion of the UCL. More recent studies have demonstrated the ulnar footprint to be 29–30 mm in length and a surface area between 324 and 421 mm2
It must also be highlighted that the above lengths were obtained with the elbow in a static position. However, the UCL is not an isometric stabilizer but changes length throughout progressive elbow flexion. Studies have demonstrated a change of 2.8–4.8 mm as the elbow progresses from extension to full flexion [12, 19, 20].
Biomechanics of the Medial Elbow Complex Static Stabilizers
The primary biomechanical role of the UCL is to provide valgus stability of the elbow, especially in overhead throwing athletes. Morrey et al. [21] demonstrated that with an intact radial head, the UCL provides 31% and 54% of valgus stability at 0° and 90° of elbow flexion, respectively [12]. Moreover, the authors noted that an intact UCL allowed for only 3° of valgus opening in full extension and 2° of valgus opening in full flexion. Similar findings have been reported in a number of other studies, which have demonstrated 2 to 8° of valgus laxity with an intact UCL [4, 12, 18, 20, 21]. To quantify when the UCL has the most laxity with a loaded elbow, Safran et al. analyzed 12 cadaveric specimens with 2 Nm load applied to the elbow in 30° of flexion and reported 10.7° of valgus laxity with the forearm in neutral rotation [22••]. Callaway et al. expanded on these findings by loading the elbow with 2 Nm at 30° and 90° of flexion and reported a valgus laxity of 3.6° [23]. The former of these two studies did not quantify the amount of inherent valgus laxity specimens had prior to testing, which makes direct comparison of the two studies challenging. However, it is thought the amount of UCL valgus laxity is greatest at 30° of flexion [22••].
Several studies have sought to define the contribution of the UCL to valgus stability by sectioning the ligament in cadaveric models at different locations and measuring valgus angles during elbow range of motion. When the UCL is sectioned, the amount of valgus laxity increases until the secondary osseous stabilizers, ulnohumeral and radiocapitellar joints, engage [8••]. It has been demonstrated that the greatest valgus instability occurs with a deficient UCL and 90° of elbow flexion [23]. Furthermore, Callaway et al. demonstrated that there is a gradual increase in valgus laxity with progressive flexion through 30°, 60°, 90°, and 120° of flexion from 1.5 mm, 2.8 mm, 3.2 mm, and 3.0 mm, respectively [23]. Similar studies have reported a 150% increase in valgus instability following sectioning the UCL compared to elbows with an intact ligament [24]. Other studies have demonstrated the greatest valgus laxity to occur at 50 and 70° of flexion with sectioning of the mUCL [18, 25]. Taken together, these results demonstrate the vital role the UCL plays in providing valgus stability of the elbow, most notably in elbow flexion of at least 50°.
Anatomy of the Medial Elbow Complex Dynamic Stabilizers
The dynamic stabilizers of the elbow are made up of the flexor-pronator muscle complex that crosses the elbow joint. Specifically, the flexor digitorum superficialis (FDS), flexor carpi ulnaris (FCU), pronator teres (PT), and brachialis make up what is often referred to as the flexor-pronator mass. (Fig. 4).
Fig. 4.
a Cadaveric image demonstrating the contents and relationships of the flexor pronator mass. b Purple: pronator teres, two distinct attachments proximal to central flexor origin (CFO) and into CFO. Yellow: FCR inserts at the CFO. Blue: FDS attachment spans the anteromedial capsule and inserts at CFO. Red: Palmaris inserts at the CFO. Green: Humeral head of the FCU inserts at CFO
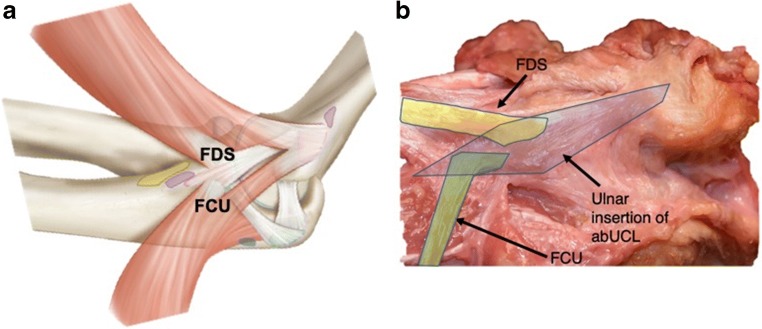
Of these structures, the FDS and FCU have been reported to play the most important roles in dynamic medial elbow stability [5••, 6, 7, 20]. The FDS inserts proximally on the humerus as part of the common flexor insertion, 4.4 mm posterior to the medial epicondyle [5••]. The common flexor insertion has been reported have an surface area of 127.9 mm2 (range, 89.5–166.3 mm2) [5••, 8••]. The FDS ulnar tendinous insertion is closely related to the UCL and has been reported to be overlapped with the UCL insertion for 46% of its total footprint, inserting 6.8 mm distal to the sublime tubercle of the ulna [5••]. The FCU inserts proximally at the common flexor insertion and has a similar ulnar insertion. The FCU ulnar insertion has been reported to be 1.9 mm posterior and 1.3 mm proximal the sublime tubercle and overlaps 21% of its total footprint on the UCL ulnar insertion [5••]. The FCU has been reported to have an ulnar insertion surface area of 20.2 mm2 [5••] (Fig. 5).
Fig. 5.
a Illustration and b cadaveric view of relationship of ulnar insertion of abUCL and the ulnar footprints of the FCU and FDS
The pronator teres inserts just proximal to the common flexor humeral insertion, 9.4 mm proximal from the medial epicondyle. The footprint of this humeral insertion has been reported to be 40.1 mm2 (range, 33–47 mm2) [5••]. The PT then courses distally to insert 14.5 mm distal to the sublime tubercle, which is 24.5 mm distal to the joint line. It should be highlighted the PT ulna insertion a thin tendinous structure that runs between the brachialis muscle and the anterior bundle of the UCL.
Biomechanics of the Medial Elbow Complex Dynamic Stabilizers
The biomechanics of the medial elbow dynamic stabilizers have been less well studied than the static stabilizers, but their importance for valgus stability, especially for the throwing athlete, has come to the forefront with more recent research. Morrey et al. was one of the earliest studies to describe the dynamic stabilizers of the medial elbow, when they demonstrated the importance of the anterior capsule in providing dynamic restraint to valgus instability [21]. More recent studies have performed cadaveric sectioning studies to characterize the roles of the FCU and FDS on dynamic elbow stability. Park et al. [7] used six cadaveric specimens with simulated complete mUCL tears. Elbows were tested at 30° and 90° of flexion and contraction of the FCU and FDS were observed. The authors reported that the largest correction in valgus angle was observed when the FCU and FDS contracted together at 30 and 60° of elbow flexion. In isolation, the FCU was observed to produce the greatest valgus correction angle, followed by isolated FDS contraction [7].
Lin et al. [6] performed a study with 8 cadaveric specimens to examine the contributions to valgus stability of each flexor-pronator mass muscle with a stress applied to the elbow. The authors reported that the FCU and FDS provided significant restraint to valgus stress at 45° and 90° of elbow flexion, with the FCU being the strongest restraint. The authors found that the PT did not provide significant restraint to valgus instability at any elbow flexion angles [6]. In a later study by Udall et al. [3], the authors not only reported similar findings with respect the flexor-pronator mass decreasing valgus angles in UCL deficient elbows but also noted that the PT provided additional restraint to valgus stress [3]. Finally, Remaley [26] et al. performed a surface EMG and high-speed videography study of 10 female collegiate pitchers to evaluate the activation pattern of forearm musculature during a throwing motion. The authors reported that during the release of the ball, with the arm in approximately the 6’o clock position, the FCU had the highest levels of activation compared to all other forearm muscles.
Taken together, the growing body of literature of the dynamic stabilizers of the medial elbow highlights the crucial roles of the FCU and FDS play in providing valgus stability in both the UCL intact and deficit elbow and the attention that should be directed towards the flexor-pronator mass during surgical intervention and/or rehabilitation.
Conclusion
The medial ulnar collateral ligament complex of the elbow has a crucial role in providing both static and dynamic elbow stabilities. Most notably, the anterior bundle (UCL) provides the primary resistance to valgus and rotational stresses, especially during throwing motion. An understanding of the humeral and ulnar footprints and their relationships with surrounding structures is necessary to restore the native isometry of the medial complex of the elbow during UCL reconstruction. The flexor pronator musculature plays an essential role in dynamic stability, and the intimate relationship of the FCU and FDS with the ulnar insertion of the UCL should be considered to optimize recovery and outcomes with repair or reconstruction.
Compliance with Ethical Standards
Conflict of Interest
Mark E Cinque MD, MS declares he has no conflict of interest.
Mark Schickendantz MD declares he has no conflict of interest.
Salvatore Frangiamore MD, MS declares he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Injuries in Overhead Athletes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Camp CL, Tubbs TG, Fleisig GS, Dines JS, Dines DM, Altchek DW, et al. The relationship of throwing arm mechanics and elbow varus torque: Within-Subject Variation for Professional Baseball Pitchers Across 82,000 Throws. Am J Sports Med. 2017;45:3030–3035. doi: 10.1177/0363546517719047. [DOI] [PubMed] [Google Scholar]
- 2.Dodson CC, Altchek DW. Ulnar collateral ligament reconstruction revisited: the procedure I use and why. Sports Health. 2012;4:433–437. doi: 10.1177/1941738112454649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Udall JH, Fitzpatrick MJ, McGarry MH, Leba TB, Lee TQ. Effects of flexor-pronator muscle loading on valgus stability of the elbow with an intact, stretched, and resected medial ulnar collateral ligament. J Shoulder Elb Surg. 2009;18:773–778. doi: 10.1016/j.jse.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 4.Alcid JG, Ahmad CS, Lee TQ. Elbow anatomy and structural biomechanics. Clin Sports Med. 2004;23(503–517):vii. doi: 10.1016/j.csm.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 5.Frangiamore SJ, Moatshe G, Kruckeberg BM, Civitarese DM, Muckenhirn KJ, Chahla J, et al. Qualitative and quantitative analyses of the dynamic and static stabilizers of the medial elbow: an anatomic study. The American Journal of Sports Medicine. 2018;46:687–694. doi: 10.1177/0363546517743749. [DOI] [PubMed] [Google Scholar]
- 6.Lin F, Kohli N, Perlmutter S, Lim D, Nuber GW, Makhsous M. Muscle contribution to elbow joint valgus stability. J Shoulder Elb Surg. 2007;16:795–802. doi: 10.1016/j.jse.2007.03.024. [DOI] [PubMed] [Google Scholar]
- 7.Park MC, Ahmad CS. Dynamic contributions of the flexor-pronator mass to elbow valgus stability. J Bone Joint Surg Am. 2004;86-a:2268–2274. doi: 10.2106/00004623-200410000-00020. [DOI] [PubMed] [Google Scholar]
- 8.Camp CL, Jahandar H, Sinatro AM, Imhauser CW, Altchek DW, Dines JS. Quantitative anatomic analysis of the medial ulnar collateral ligament complex of the elbow. Orthop J Sports Med. 2018;6:2325967118762751. doi: 10.1177/2325967118762751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dugas JR, Ostrander RV, Cain EL, Kingsley D, Andrews JR. Anatomy of the anterior bundle of the ulnar collateral ligament. J Shoulder Elbow Surg. 2007;16:657–660. doi: 10.1016/j.jse.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 10.Farrow LD, Mahoney AP, Sheppard JE, Schickendantz MS, Taljanovic MS. Sonographic assessment of the medial ulnar collateral ligament distal ulnar attachment. J Ultrasound Med. 2014;33:1485–1490. doi: 10.7863/ultra.33.8.1485. [DOI] [PubMed] [Google Scholar]
- 11.Lall AC, Beason DP, Dugas JR, Cain EL., Jr The effect of humeral and ulnar bone tunnel placement on achieving ulnar collateral ligament graft isometry: A Cadaveric Study. Arthroscopy. 2019;35:2029–2034. doi: 10.1016/j.arthro.2018.12.012. [DOI] [PubMed] [Google Scholar]
- 12.Morrey BF, An KN. Articular and ligamentous contributions to the stability of the elbow joint. Am J Sports Med. 1983;11:315–319. doi: 10.1177/036354658301100506. [DOI] [PubMed] [Google Scholar]
- 13.•• Erickson BJ, Fu M, Meyers K, Camp CL, Altchek DW, Coleman SH, et al. The middle and distal aspects of the ulnar footprint of the medial ulnar collateral ligament of the elbow do not provide significant resistance to valgus stress: a biomechanical study. Orthop J Sports Med. 2019;7, 2325967118825294 Purpose: The purpose of this study was to determine the contribution of each part of the UCL footprint to the elbow valgus stability provided by the UCL. It was hypothesized that the distal two-thirds of the ulnar UCL footprint would not contribute significantly to valgus stability provided by the UCL. Methods: Fifteen cadaveric arms were dissected to the capsuloligamentous elbow structures and potted. A servohydraulic load frame was used to place 5 N m of valgus stress on the intact elbow at 30°, 60°, 90°, and 120° of flexion. The UCL insertional footprint was measured and divided into thirds (proximal, middle, and distal). One-third of the UCL footprint was elevated off the bone (leaving the ligament in continuity), and the elbow was retested at the same degrees of flexion. This was repeated until the entire UCL footprint on the ulna was sectioned. Each elbow was randomized for how the UCL would be sectioned (sectioning the proximal, then middle, and then distal third or sectioning the distal, then middle, and then proximal third). Ulnohumeral joint gapping (millimeters) was recorded with a 3-dimensional motion capture system using physical and virtual markers. Two-group comparisons were made between each sectioned status versus the intact condition for each flexion angle. Results: When the UCL was sectioned from distal to proximal, none of the ligaments failed prior to complete sectioning. When the UCL was sectioned from proximal to distal, 3 of the 6 ligaments failed after sectioning of the proximal third, while 2 more failed after the proximal and middle thirds were sectioned. Of the specimens with the distal third of the ligament sectioned first, no significant differences were found between intact, distal third cut, and distal plus middle thirds cut at all flexion angles. Conclusion: The middle and distal thirds of the insertional footprint of the UCL on the ulna did not significantly contribute to gap resistance at 5 N m of valgus load. The proximal third of the footprint is the primary resistor of valgus load. [DOI] [PMC free article] [PubMed]
- 14.Beckett KS, McConnell P, Lagopoulos M, Newman RJ. Variations in the normal anatomy of the collateral ligaments of the human elbow joint. J Anat. 2000;197(Pt 3):507–511. doi: 10.1046/j.1469-7580.2000.19730507.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eygendaal D, Valstar ER, Sojbjerg JO, Rozing PM. Biomechanical evaluation of the elbow using roentgen stereophotogrammetric analysis. Clin Orthop Relat Res. 2002:100–5. [DOI] [PubMed]
- 16.Farrow LD, Mahoney AJ, Stefancin JJ, Taljanovic MS, Sheppard JE, Schickendantz MS. Quantitative analysis of the medial ulnar collateral ligament ulnar footprint and its relationship to the ulnar sublime tubercle. Am J Sports Med. 2011;39:1936–1941. doi: 10.1177/0363546511406220. [DOI] [PubMed] [Google Scholar]
- 17.Regan WD, Korinek SL, Morrey BF, An KN. Biomechanical study of ligaments around the elbow joint. Clin Orthop Relat Res. 1991:170–9. [PubMed]
- 18.Floris S, Olsen BS, Dalstra M, Sojbjerg JO, Sneppen O. The medial collateral ligament of the elbow joint: anatomy and kinematics. J Shoulder Elb Surg. 1998;7:345–351. doi: 10.1016/S1058-2746(98)90021-0. [DOI] [PubMed] [Google Scholar]
- 19.Armstrong AD, Ferreira LM, Dunning CE, Johnson JA, King GJ. The medial collateral ligament of the elbow is not isometric: an in vitro biomechanical study. Am J Sports Med. 2004;32:85–90. doi: 10.1177/0363546503258886. [DOI] [PubMed] [Google Scholar]
- 20.Bryce CD, Armstrong AD. Anatomy and biomechanics of the elbow. Orthop Clin North Am. 2008;39:141–154, v. doi: 10.1016/j.ocl.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 21.Morrey BF, An KN. Functional anatomy of the ligaments of the elbow. Clin Orthop Relat Res. 1985:84–90. [PubMed]
- 22.Safran M, Ahmad CS, Elattrache NS. Ulnar collateral ligament of the elbow. Arthroscopy. 2005;21:1381–1395. doi: 10.1016/j.arthro.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 23.Callaway GH, Field LD, Deng XH, Torzilli PA, O'Brien SJ, Altchek DW, Warren RF. Biomechanical evaluation of the medial collateral ligament of the elbow. J Bone Joint Surg Am. 1997;79:1223–1231. doi: 10.2106/00004623-199708000-00015. [DOI] [PubMed] [Google Scholar]
- 24.Mullen DJ, Goradia VK, Parks BG, Matthews LS. A biomechanical study of stability of the elbow to valgus stress before and after reconstruction of the medial collateral ligament. J Shoulder Elb Surg. 2002;11:259–264. doi: 10.1067/mse.2002.122622. [DOI] [PubMed] [Google Scholar]
- 25.Sojbjerg JO, Ovesen J, Nielsen S. Experimental elbow instability after transection of the medial collateral ligament. Clin Orthop Relat Res. 1987:186–90. [PubMed]
- 26.Remaley DT, Fincham B, McCullough B, Davis K, Nofsinger C, Armstrong C, et al. Surface electromyography of the forearm musculature during the windmill softball pitch. Orthop J Sports Med. 2015;3:2325967114566796. doi: 10.1177/2325967114566796. [DOI] [PMC free article] [PubMed] [Google Scholar]