Abstract
Purpose of Review
Movement retraining in rehabilitation is the process by which a motor program is changed with the overall goal of reducing pain or injury risk. Movement retraining is an important component of interventions to address patellofemoral pain. The purpose of this paper is to review the methods and results of current retraining studies that are aimed at reducing symptoms of patellofemoral pain.
Recent Findings
The majority of studies reviewed demonstrated some improvement in patellofemoral pain symptoms and overall function. However, the degree of improvement as well as the persistence of improvement over time varied between studies. The greatest pain reduction and persistent changes were noted in those studies that incorporated a faded feedback design including between 8 and 18 sessions over 2–6 weeks, typically 3–4 sessions per week. Additionally, dosage in these studies increased to 30–45 min during later sessions, resulting in 177–196 total minutes of retraining. In contrast, pain reductions and persistence of changes were the least in studies where overall retraining volume was low and feedback was either absent or continual.
Summary
Faulty movement patterns have been associated with patellofemoral pain. Studies have shown that strengthening alone does not alter these patterns, and that addressing the motor program is needed to effect these changes. Based upon the studies reviewed here, retraining faulty patterns, when present, appears to play a significant role in addressing patellofemoral pain. Therefore, movement retraining, while adhering to basic motor control principles, should be part of a therapist’s intervention skillset when treating patients with PFP.
Keywords: Patellofemoral pain, Movement retraining, Gait retraining, Motor learning
Overview on a Physician’s Perspective on Retraining
Patellofemoral pain (PFP) is one of the most common lower extremity injuries in recreational athletes [1]. It has been reported that over one-third of runners will experience chronic knee pain [2, 3]. Additionally, having PFP as a young adult can serve as a risk factor for knee arthritis later in life [4, 5]. PFP often presents itself without any further radiologic or other imaging features. Appropriately, PFP has been described as “one of the most vexatious clinical challenges in rehabilitative medicine” [6].
The medical treatment for PFP is typically non-surgical. Non-steroidal anti-inflammatory medications (NSAIDs), acetaminophen, and other oral medications are considered for pain relief. While steroid injections have been traditionally offered, there is limited evidence for their success and compelling evidence suggests that both steroid and anesthetic are chondrotoxic [7]. Further, there is only limited evidence for alternative forms of injection including hyaluronic acid or use of orthobiological agents (such as platelet-rich plasma or regenerative medicine techniques).
Physical therapy is the mainstay treatment for PFP. This typically involves exercise in various forms, bracing, taping, foot orthotics, and a gradual return to sport. However, there are instances when this approach does not successfully resolve symptoms, especially once an athlete begins to increase their running volume or activity. The return of symptoms generates frustration for both the athlete and physician. When the standard approach has failed, it may be because the underlying cause of the problem has not been addressed. Emerging evidence suggests gait retraining provides an effective intervention in the management of PFP. When an athlete fails to see a resolution in symptoms, despite measured gains in strength and flexibility with physical therapy, they may be receptive to a gait retraining approach.
Gait retraining entails a significant time commitment. A new gait pattern places different demands on the body requiring adequate strengthening in preparation. The retraining phase can last 4–6 weeks followed by 2–3 months of habituation and gradual increase in mileage and overall activity. Therefore, deciding to take this approach requires some shared clinical decision-making as to the best time to begin a retraining program. Time in the season, upcoming planned competitions, and the state of injury in readiness all factor into when to start retraining program. The athlete needs to be counselled regarding anticipated time to habituation in order to reduce risk for future injury. Recreational runners and beginner athletes may be more receptive to make these changes. Professional athletes often have schedules that require faster return to competition not allowing for the time needed to alter and habituate to a new gait pattern. Unless they are taking time off for their injury, these athletes are likely to be less amenable to gait retraining and more appropriate for standard courses of physical therapy. Therefore, the physician plays an important role in deciding which athletes are most appropriate for a retraining intervention.
Introduction to Retraining
The biomechanical etiology of PFP is multifactorial in nature [8•]. However, one important underlying factor is the magnitude of patellofemoral joint stress. Running is a common activity in overground sports and has been the primary sport in which PFP and gait retraining have been studied. It has been reported that runners with PFP exhibit greater peak patellar stress compared with healthy runners [9•]. Elevated patellofemoral joint stress may be due to higher patellofemoral joint forces [10] which can result from higher ground reaction forces. These increased stresses may also be the result of altered hip and knee kinematics which can, in turn, reduce the patellofemoral joint contact area [9•, 11•]. Some of the abnormal movement patterns that have been associated with PFP include increased hip adduction, internal rotation, and contralateral pelvic drop [12•]. Thus, interventions may aim to either alter these movement patterns or reduce ground reaction forces during running to reduce patellofemoral joint stress.
The most common intervention approach to changing abnormal movement patterns is strengthening the muscles that control those aberrant movements. However, studies that have involved strengthening report persistent symptoms in long-term follow-ups. For example, 5.7 years following a strengthening intervention for individuals with PFP, it was reported 80% continued to have pain and 74% had to reduce their physical activity [13]. This begs the question as to why strengthening, as an isolated intervention, fails in the long term. In order to address this, Willy et al. randomized 40 asymptomatic individuals with increased hip adduction into a hip strengthening group and a control group [14]. The 6-week progressive strengthening program was directed at the hip abductors and external rotators. Despite the significant increase in strength of these muscles following the intervention, there were no reductions in hip adduction, internal rotation, or contralateral pelvic drop during running. These are common movement disorders associated with PFP [12•]. These results by Willy [14] and others [15] suggest that strengthening alone does not change a movement pattern. Strengthening may provide the capacity to move differently, but reprogramming of the motor pattern through movement retraining is needed to alter the way a person moves.
Movement retraining in rehabilitation is the process by which a motor program is changed with the overall goal of reducing pain or injury risk. This retraining requires that the individual has the capacity both in terms of range of motion and strength to achieve the new movement pattern, as well as the endurance for it to persist. These pre-requisites should be met before beginning a retraining program. There are a number of motor learning principles that need to be adhered to in order to retrain a motor pattern. One of the most important features of a retraining program is the provision of some type of feedback. Feedback can take on many forms such as visual, auditory, or haptic. This feedback allows the individual to make the connection between, for example, what they see as correct movement and what that movement feels like. The participant must be given adequate practice/dosage to reinforce this motor pattern [16]. Finally, the feedback should be gradually removed such that the learner relies on their own intrinsic cues (proprioception, kinesthesia) associated with the correct movement pattern [16, 17]. This is commonly referred to as a faded feedback design.
The purpose of this paper is to review the methods and results of current retraining studies that are aimed at reducing symptoms of PFP. The studies will be presented in three groups: studies aimed at changing kinematics during running, studies directed at altering temporospatial characteristics during running, and retraining studies of functional movements such as stair negotiation and single-leg squat. The paper will end with a summary of these studies, their application to the clinic, and finally recommendations for future retraining investigations.
Kinematic Retraining Studies of Running
Kinematic gait retraining refers to cueing and provision of feedback for specific changes in joint or segment orientations to reduce loading on the patellofemoral joint during running. To date, kinematic gait retraining for PFP has been focused on (a) reducing hip adduction, (b) transition from a rearfoot strike pattern to a forefoot strike pattern, and (c) adopting a more forward trunk lean. The first strategy targets the kinematic influences of patellofemoral joint contact area whereas the latter two retraining strategies aim to reduce patellofemoral joint contact force.
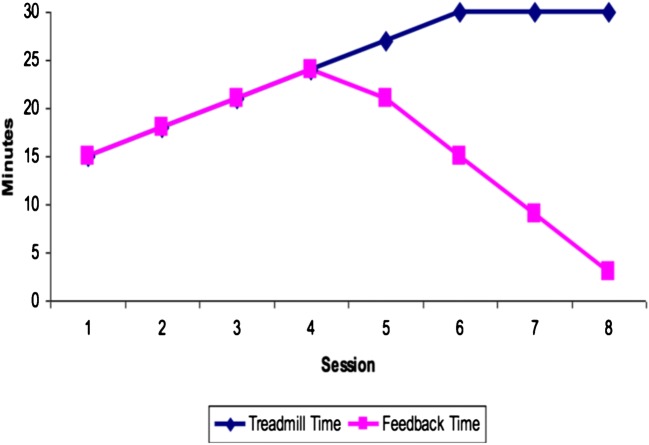
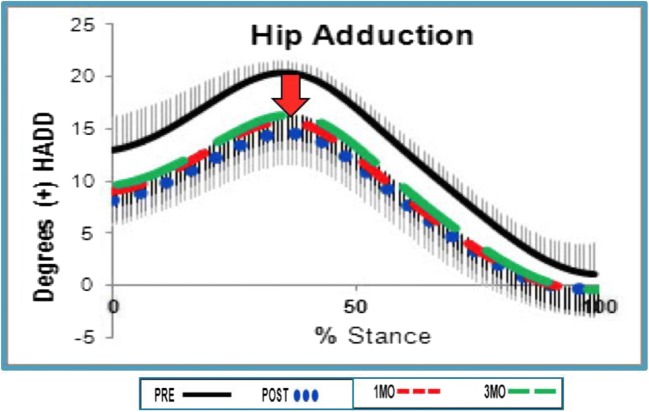
Female runners with PFP often demonstrate greater peak hip adduction [18–21] and hip internal rotation kinematics [22, 23] compared with uninjured female runners. While male runners with PFP demonstrate a different pattern of greater knee adduction, 17% of males demonstrate the female pattern of increased hip adduction [24], Increased hip adduction has been shown to increase lateral patellar tracking [25], leading to elevated lateral patellofemoral joint stress due to a reduction in patellofemoral contact area [26, 27]. Two case series of 10 participants with PFP and excessive hip adduction utilized visual feedback to improve hip mechanics. Noehren et al. [28] provided real-time feedback on the hip adduction angle during running over the course of 8 sessions of gait retraining. Sessions started at 15 min and increased to 30 min over the 8 sessions across 2 weeks. Feedback was provided on a video monitor placed in front of a treadmill that displayed the real-time kinematic curves of the runner’s hip adduction. The feedback was faded over the last four sessions (Fig. 1). The persistence of the biomechanical and clinical outcomes was assessed at a 1-month follow-up. In a similar investigation, Willy et al. [29] used a full-length mirror to provide visual feedback on hip adduction during running, given that mirrors are available in most clinics. These authors asked runners to increase the distance between their knees and point their patellae straight ahead by activating their gluteal muscles. Again, 8 sessions of faded feedback retraining were conducted over 2 weeks with results being measured post training and at 1- and 3-month follow-ups. Participants in studies by both Noehren et al. [28] and Willy et al. [29] demonstrated reductions in peak hip adduction, internal rotation, and contralateral pelvic drop during running (Fig. 2). They also reported improvements in pain (scored via visual analog scale) and function [28, 29]. These changes largely persisted for 1 month [28, 29] and 3 months [29] after the retraining periods (Fig. 3—Willy hip adduction curve). At 3 months, Willy et al. reported that hip adduction regressed by 2° from the post-test. While this change was not significant, it suggests there may have been some drift towards the baseline measure. However, pain levels remained at post-retraining levels [29].
Fig. 1.
Retraining schedule. Run time increases from 15 to 30 min over 8 sessions. Feedback is faded during the last 4 sessions
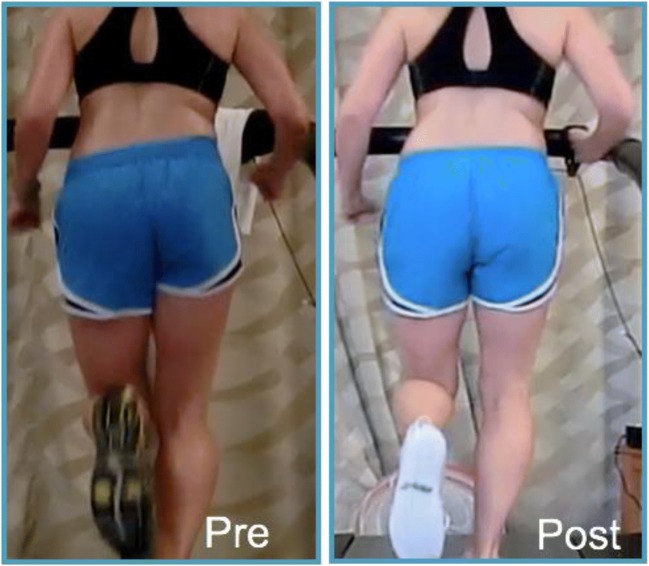
Fig. 2.
Hip mechanics pre- and post-retraining. Note the reductions in hip adduction and contralateral pelvic drop following the retraining
Fig. 3.
Hip adduction reductions noted following retraining and at the 1- and 3-month follow-ups (Willy et al. 2012)
Transitioning to a forefoot strike pattern shifts some of the demand of the knee extensors to the plantar flexors [30], effectively reducing the patellofemoral joint stress. This transition can also eliminate the impact transient of the vertical ground reaction force, thereby reducing the vertical load rate. This load rate has been associated with PFP [31]. Three studies have used this forefoot strike transition to treat PFP. In a pilot study, 3 runners with PFP were provided real-time feedback from an insole sensor that provided an audible alarm when they landed on their heel [32]. The runners underwent 8 sessions of retraining over 2 weeks with a faded feedback design that incorporated a gradual reduction of audible feedback while run time increased. Post training, and at the 3-month follow-up, the runners exhibited lower vertical load rates and reduced knee pain and were able to return to the prior level of running. Using a randomized control design, Roper et al. [33] conducted a gait retraining program to transition to a forefoot strike in rearfoot strikers with PFP. Runners were randomized to either a retraining or a control group. Runners in the retraining group received both verbal and visual (via a mirror) feedback over the course of 8 retraining sessions, using a faded feedback design similar to Cheung et al. [29]. The control completed the same 8 sessions of treadmill running with a matched run time schedule [33], but without the verbal or visual feedback. Runners in the retraining group experienced large improvements in pain with 50% reductions in average patellofemoral joint stress during early stance phase. Importantly, the control group did not demonstrate reductions in knee pain at the conclusion of the sham intervention. Furthermore, these improvements persisted at the 30-day follow-up. Finally, dos Santos [34••] conducted a retraining study using faded verbal cuing to retrain six rearfoot strike runners with PFP to transition to a forefoot strike pattern. Following this retraining, patellofemoral joint stress was reduced by 27% and pain was reduced by 75% at the 6-month follow-up.
Adopting a forward trunk lean during running may also be a viable retraining strategy to reduce patellofemoral joint loads in individuals with PFP [35]. As part of the previously described study, dos Santos and colleagues [36••] instructed six runners with PFP to increase their forward lean. This was done by providing faded verbal cuing over 8 sessions. This approach resulted in a significant reduction in pain both at the post-training and at the 6 month follow-up. However, one concern with this study is that runners had relatively normal trunk lean at baseline (10.8°) which increased to 18° post training. This amount of trunk flexion might be considered excessive and may result in secondary negative consequences.
Spatiotemporal Retraining Studies of Running
Spatiotemporal retraining consists of altering a runner’s step rate/cadence to a set percentage above their baseline measurement [36••, 37, 38•]. This can be done easily using watch-based metronome applications and so is a simple intervention to employ. Studies have demonstrated that increasing step rate by 7.5–10% can acutely reduce peak hip adduction while also reducing the negative knee work by 27–34% [39, 40] and patellofemoral joint stress by 10–22% [41, 42]. Based upon these results in healthy individuals, increasing step rate has become one of the retraining interventions suggested for PFP.
Esculier and colleagues [37] conducted an RCT to compare gait retraining to increase cadence with education on load management and exercise targeting the hip and knee musculature. The study enrolled 69 participants, with 23 being allocated to one of three groups: education, education and exercise, and education with gait retraining. The gait retraining group underwent five 10-min treadmill sessions over 8 weeks. However, it should be noted that the retraining group was mixed with rearfoot and forefoot strikers. Rearfoot strike runners who were unable to increase their cadence were then cued to use a forefoot strike pattern and land softer. Neither structured nor faded feedback was provided. All three groups demonstrated small, but similar, improvements in outcomes, including pain and function leading the authors to conclude that education alone may be adequate for the treatment of PFP. However, given lack of structured and faded feedback, the validity of the retraining design is questioned. Additionally, it is unknown whether the small reductions in pain noted with the 3 interventions exceeded “wait and see” since a control group was not included.
Neal and colleagues [38•] conducted a feasibility study and recruited 10 participants with PFP for a gait retraining program that focused on increasing step rate by 7.5%. The program included 3 sessions a week for 6 weeks, with feedback provided using a metronome in a faded design. Participants experienced a significant reduction in average pain and improvement in function post-retraining. Worst pain scores improved from 6.8/10 to 2.9/10, which was a significant improvement but indicated continued dysfunction. Additionally, 3/10 participants were unable to increase step rate by 7.5%. This suggests that not all patients may be able to increase their step rates sufficiently to reduce their pain.
Bonacci et al. [36••] conducted a feasibility RCT to investigate the effect of a 6-week gait retraining program to increase cadence by 10%. Sixteen participants were recruited and randomized to either a foot orthoses or a gait retraining group. Participants in the gait retraining group performed 10 gait retraining sessions over 6 weeks to increase their cadence and were also issued minimalist shoes. This program transitioned runners from 50/50% walk/run to 100% running over the course of the 10 sessions, with metronome feedback provided in a faded feedback design. Participants then ran on their own for the following 6 weeks. Participants in the gait retraining group experienced an 81% reduction in pain at the 6-week follow-up. While increasing cadence has been shown to reduce patellofemoral joint loads by 10–22% [41, 42], Sinclair et al. [43] reported that wearing a minimalist shoe reduced these loads by approximately 9%. Thus, the combined use of the minimalist shoe with increasing cadence makes it difficult to discern the direct cause of the reduction in pain and improvement in function.
Finally, dos Santos et al. [34••] used verbal cuing and a metronome, in a faded feedback design over 8 sessions, to increase the cadence of six runners with PFP by 10%. These authors found that pain was not significantly reduced post training, but later demonstrated a significant reduction at the 6 month follow-up.
Functional Movement Retraining
In addition to the work conducted on running, there is emerging evidence supporting efficacy of functional movement retraining interventions for other functional tasks in participants with PFP. These studies include a mix of both randomized controlled trials (RCTs) and case series.
Baldon et al. [44] implemented an RCT comparing traditional quadriceps strengthening intervention with and without additional facilitation of improved motor control of the lower limb, pelvis, and trunk. Participants were instructed to perform all exercises with neutral frontal plane alignment and a forward trunk lean. Three sessions per week were completed for 8 weeks, supervised by a single physical therapist. Participants in the motor control group demonstrated significant improvements in 3D kinematics during a single-leg squat task. This included decreased ipsilateral trunk lean, hip adduction, knee abduction, and contralateral pelvic depression excursion. Both groups demonstrated a reduction in average pain (during the previous week) post-retraining and at 3-month follow-up. However, significantly greater improvements were noted for the motor control group at both time points.
Rabelo et al. [45] conducted a similar RCT, assessing the effect of two interventions on a step down test in 34 women. The authors compared a traditional quadriceps and gluteal strengthening program with the same program with additional facilitation of improved motor control of the lower limb, pelvis, and trunk. Participants in the motor control group were instructed to correct these faults in their movement patterns during functional activities such as the single-leg squat and forward lunge. Three sessions per week were completed for 4 weeks, all of which were supervised by one of two physical therapists. Continual feedback was provided using both mirror and verbal cues. Both groups demonstrated reduced pain (measured using a numerical rating scale), but no differences between groups were noted for any of the follow-up points (4 weeks, 3 months, or 6 months). Those in the motor control group demonstrated a significant improvement in function at 3 months, reflected by a higher Kujala score. However, unlike with Baldon, this effect had washed out by the 6-month follow-up. Finally, there were no between-group differences in 3D kinematics during a step down task at any follow-up point. The superior results reported by Baldon et al. [44] may be due to the specificity of training. Their functional outcome test was a single-leg squat, the same task that was included in the motor retraining program. Willy and Davis [14] also identified improvements in a single-leg squat after a strengthening intervention that included single-leg squat training with verbal and visual feedback on alignment.
While RCTs are the strongest methodologic design, other types of studies have been used to examine the effect of retraining on functional activities. Salsich et al. [46•] conducted a feasibility study that involved twice-weekly sessions for 6 weeks. Twenty-five participants with PFP were provided with a variety of verbal and visual cues to ensure optimal kinematic alignment during functional tasks. These included single- and double-leg squats, ascending and descending stairs, and sitting and rising from a chair. The authors reported significant improvements in pain, function, and single-leg squat kinematics following the training. Liebbrandt and Louw [47•] used a comparable methodology to Salsich et al. [46•]. Eight participants with PFP (five females, three males) were provided with an individualized retraining program, to be completed four times per week for 6 weeks (one supervised, three independent sessions). The program was aimed at improving walking gait mechanics, squatting, and stair negotiation. Average pain was reduced by 3.6 points on a numerical rating scale (from 3.9 to 0.3) and seven out of the eight participants demonstrated improvement in their biomechanical outcomes during the functional activities. Finally, in a single case study of a female patient with PFP, Yemm and Krause [48] used functional retraining to reduce the frontal plane projection angle (i.e., hip adduction, internal rotation, knee valgus) during a single-leg step down. They provided mirror and verbal feedback continuously during 4 training sessions over 3 weeks. Immediately following the completion of the retraining period, PFP reduced from 4/10 to 1/10 and the frontal plane projection angle during the step down was reduced to normal. However, there was no follow-up to determine persistence of these changes.
Discussion
The results of the retraining studies for individuals with PFP are summarized in Table 1. The majority of these studies have been conducted in running and have focused on reducing hip adduction, increasing forward lean, transitioning to a forefoot strike pattern, and increasing cadence. A number of investigations have focused on improvement in functional activities such as walking, squatting, stair negotiation, and rising from a chair. Studies have all reported some improvements in mechanics, pain, and function. However, the degree of improvement was not consistent across studies.
Table 1.
Summary of narrative review for studies on movement retraining for patellofemoral pain
| Author/type | n | Age (years) | Sex | Protocol | Retraining time | Feedback type | Feedback frequency | Post-retraining follow-up | Biomechanical outcomes | Functional outcomes | VAS pain* pre (x/10) | VAS pain post (x/10) | VAS pain follow-up (x/10) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Running—kinematic FB | |||||||||||||
| Cheung and Davis 2011/case series | 3 | 26–32 | 3 F | 2 weeks, 8 sessions | Increasing 15–30 min | Pressure insole in heel | Continual first 4 sessions, then faded | 12 weeks | Loading rates reduced |
PF pain score reduced Kujala improved |
3.1 | 1.7 | 1.4 |
| Dos Santos et al. 2019/RCT (no true control) | 18 | 18–35 | 9 F, 9 M |
Control 2 weeks, 8 sessions |
Increasing 15–30 min | Verbal, metronome | Continual first 4 sessions, then faded | 24 weeks | Plant flex, Forward trunk lean increased | VAS-A reduced, AKPS improved | 5** | 2.5** | 1** |
| Noehren et al. 2011/case series | 10 | 18–35 | 10 F | 2 weeks, 8 sessions | Increasing 15–30 min | Kinematic curves for hip ADD | Continual first 4 sessions, then faded | 4 weeks | Pk HADD, HIR, Contr. Pelvic drop reduced, VALR and VILR reduced | VAS-R reduced, LEFS improved | 5.0 | 0.5 | 0.0 |
| Roper et al. 2016/RCT | 16 | 18–44 | 11 F, 5 M | 2 weeks, 8 sessions | Increasing 15–30 min | Mirror for foot strike pattern | Continual first 4 sessions, then faded | 4 weeks | Knee Add, PF Stress reduced | VAS-R reduced | 5.3 | 1 | 1 |
| Willy et al. 2012/case series | 13 | 18–35 | 13 F | 2 weeks, 8 sessions | Increasing 15–30 min | Mirror for hip ADD, IR | Continual first 4 sessions, then faded | 12 weeks | Hip Add, Int Rot and CPD reduced | VAS-R reduced, LEFS improved | 4.5 | 0.5 | 0.5 |
| Running—cadence FB | |||||||||||||
| Bonacci et al. 2018/RCT (no true control) | 16 | 18–40 | 12 F, 4 M | 6 weeks, 10 sessions | 20% weekly training vol. | Minimalist running shoes coupled with Metronome | Continual first 4 weeks, then faded | 6 weeks | Cadence increased | VAS-W reduced, AKPS improved | 1.8 | ---- | 0.4 |
| Esculier et al. 2017/RCT (no true control) | 69 | 18–45 | 43 F, 26 M | 8 weeks, 5 sessions | 10 min/session | Verbal instruction in FFS or cadence | Continual | 12 weeks | Cadence increased, AVLR and PFJ avg. load rate reduced | VAS-R reduced, KOS-ADLS improved | 6.1 | 3.5 | 2.5 |
| Neal et al. 2018/case series | 11 | 18–45 | 6 F, 4 M | 6 weeks, 18 sessions | Increasing 10–30 min | Metronome for cadence | Continual first 3 sessions, then faded | None | Pk Knee flex, Pk Hip add, Pk Hip Int Rot reduced, cadence increased | NPRS-A reduced | 3.0 | 0.9 | ---- |
| Functional activities—walking, squatting, stair climbing | |||||||||||||
| Baldon et al. 2014/RCT (no true control) | 31 | 18–30 | 31 F | 8 weeks, 24 sessions | 90–120 min | Verbal instruction | Continual | 12 weeks | Trunk lean, Hip Add and Knee Abd reduced | VAS-W reduced, LEFS improved | 6.6 | 1.4 | 0.9 |
| Liebbrandt and Louw 2018/case series | 8 | 18–37 | 5 F, 3 M | 6 weeks, 6 sessions with PT, plus 18 home ex sessions | Not reported | Verbal | Continual | None | Knee flex, Ankle ROM and Hip Int Rot increased, | AKPS and LEFS improved in only 2 participants, NPRS-A decreased | 3.9 | 0.28 | --- |
| Rabelo et al. 2017/RCT (no true control) | 34 | 25.6 | 34 F | 4 weeks, 12 sessions | Increasing 40–60 min | Verbal, mirror | Continual | 24 weeks | Ipsilateral trunk lean increased | AKPS improved, NPRS-A decreased | 6.1 | 2.0 | 1.3 |
| Salsich et al. 2018/case series | 25 | 22 | 25 F | 6 weeks, 12 sessions, plus daily home ex | 45 min/session | Verbal, visual, tactile | Individualized schedule: continual initially, faded | 16 weeks | Hip add and med/lat rotation reduced, Knee med/lat rotation increased | VAS-C reduced, PSFS increased | 2.2 | 1.8 | 0.5 |
| Yemm and Krause 2015/case study | 1 | 19 | 1 F | 3 weeks, 4 sessions | Not reported | Verbal, mirror | Continual | None | Reduced medial collapse | VAS-C reduced | 6 | 1 | --- |
*VAS/NPRS pain descriptors—R, running pain; C, current pain; W, worst pain over past week; A, average pain over past week
**Estimated from graph
Studies that adhered to motor control principles, such as utilizing a faded feedback design and providing adequate dosage appeared to have the greatest effect. For example, the greatest pain reduction and persistent changes over time were noted in those studies that included between 8 and 18 sessions over 2–6 weeks, typically 3–4 sessions/week [28, 29, 32, 33]. Additionally, dosage in these studies increased to 30–45 min during later sessions, resulting in 177–196 total minutes of retraining. In contrast, pain reductions were the least in studies where overall retraining volume was low and feedback was either absent or continual. For instance, Esculier et al. [37] only utilized verbal cuing, without faded feedback and which was limited to 5 sessions, 10 min in length (50 total minutes of retraining) over 7 weeks. Post-training running pain was 3.5/10 in the retraining group compared with 0.5–1.0/10 in previous retraining studies [29, 33, 49], where a faded feedback design was used. Additionally, the retraining group remained symptomatic at the 20-week follow-up (running pain VAS = 2.5), suggesting that treatment dosage was inadequate. While the functional training studies did demonstrate improvements, most were conducted using non-structured feedback or verbal cuing with no feedback. Many of these functional retraining studies did not include a follow-up to determine whether changes persisted. It is plausible that even greater results may have been achieved using a faded feedback protocol [50].
There have been a number of retraining studies involving healthy runners that have focused on altering mechanics associated with PFP that can further inform clinical interventions. Futrell et al. [51•] conducted an RCT retraining study to compare transition to a forefoot strike pattern with increasing cadence by 7.5%. This study included a faded feedback protocol, as well as a 6-month follow-up. Another strength of this study was that a distraction test was used during all running assessments to reduce performance bias. The authors assessed the effect on vertical load rate and reported a 50% reduction in the forefoot strike group that persisted at the 6-month follow-up. In contrast, a small, but insignificant, reduction in vertical load rate was seen in the cadence group. In a more ecologically based study, Willy et al. [40] randomized 30 runners with high vertical load rates into a retraining or control group. The retraining group was trained to increase their cadence by 7.5% using self-controlled faded feedback from a wireless accelerometer and running watch over 8 outdoor running sessions. Runners in the retraining group reduced their load rates by 18% (and their hip adduction by approximately 3°). These studies together suggest that, while cadence may be effective, transitioning to a forefoot strike pattern may be the most effective way to reduce vertical load rates [34••, 51•].
Chan et al. have conducted the only retraining study of healthy individuals which includes a 1-year follow-up of injuries. The authors randomized 320 healthy runners into a control and retraining group [52••]. The retraining group was provided 8 sessions of faded feedback (over 2 weeks) on their vertical ground reaction force during treadmill running and asked to eliminate their impact peak by landing more softly. The control group did the same amount of running, but were given no instructions nor feedback. While the investigators did not measure the associated change in mechanics, transitioning to a forefoot strike pattern is the most effective way to eliminate the impact transient. Therefore, it is likely that many of the subjects used this strategy. The retraining group significantly reduced their vertical load rates, while the control group did not. More importantly, the retraining group experienced a 62% reduction in running-related injuries over the 1-year follow-up period [52••]. Interestingly, there was over a fourfold increase in the number of individuals experiencing PFP in the control group compared with the retraining group (4 vs 18). This suggests that this intervention had a preventative effect for PFP.
Tibial shock has also been used as feedback to reduce vertical load rates in healthy runners. Bowser and colleagues [53•] found a 32% reduction in tibial shock with an associated 25% reduction in vertical load rates following a 2-week, 8-session program using a faded feedback design. These reductions were maintained at the 1-, 6-, and 12-month follow-up, the longest retraining follow-up to date. Clansey et al. [54] also used tibial shock feedback as a means to reduce load rates. In contrast to Bowser, these authors conducted 6 20-min sessions over 3 weeks (2 sessions/week) providing continual feedback on tibial shock. They did note significant reductions of 31% for tibial shock and 18% for load rates post training. However, these changes did not persist at the 1-month follow-up, perhaps due to inadequate dosage and continual nature of the feedback.
There are significant limitations to some of the retraining studies to date. A number of these studies did not incorporate a control group, and thus, one cannot be sure that improved symptoms and function were not simply due to the passage of time. Some of the studies had very low participant numbers, limiting statistical power and making extrapolation of the results difficult. Furthermore, some studies addressed retraining mechanics that were not identified to be faulty. Retraining should be focused on subjects demonstrating the specific fault being addressed. For example, it is not advised to retrain runners to further increase their trunk lean or hip adduction if these mechanics are within normal limits. Teng and Powers noted a 7.4% decrease in patellofemoral joint stress when acutely increasing forward lean from an upright 4° forward lean to an average self-selected lean of 7° [55]. While patellofemoral joint stress reduced an additional 6% when flexing from 7 to 14°, this amount of lean might be considered excessive. Similarly, increasing cadence in runners with normal step rates should also be done with caution so as not to result in abnormally high turnover rates. Another limitation to these studies is that the majority involved female cohorts. While females are twice as likely to experience PFP compared with males, males still sustain this injury. Therefore, there is a need to further understand the effect of retraining on males with PFP. Adherence to motor control principles, such as adequate dosage and practice and faded feedback, is needed for true motor learning to occur. This adherence likely contributes to the persistence of the changes. Therefore, additional longer term follow-up studies (beyond 3–6 months) are needed to determine whether changes that are made with retraining truly persist.
In summary, faulty movement patterns have been associated with PFP. Studies have shown that strengthening alone does not alter these patterns, and that addressing the motor program is needed to effect these changes. Based upon the studies reviewed here, retraining faulty patterns, when present, appears to play a significant role in addressing PFP. Therefore, movement retraining, while adhering to basic motor control principles, should be part of a therapist’s intervention skillset when treating patients with PFP.
Compliance with Ethical Standards
Conflict of Interest
Irene S. Davis, Adam S. Tenforde, Bradley S. Neal, Jenevieve Roper, and Richard W. Willy declare that they have no conflict of interest.
Human and Animal Rights
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Footnotes
This article is part of the Topical Collection on Non-Operative Management of Anterior Knee Pain
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Smith BE, Selfe J, Thacker D, Hendrick P, Bateman M, Moffatt F, Rathleff MS, Smith TO, Logan P. Incidence and prevalence of patellofemoral pain: a systematic review and meta-analysis. PLoS One. 2018;13(1):e0190892. doi: 10.1371/journal.pone.0190892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kannus P, Natri A, Paakkala T, Jarvinen M. An outcome study of chronic patellofemoral pain syndrome. Seven-year follow-up of patients in a randomized, controlled trial. J Bone Joint Surg Am. 1999;81(3):355–363. doi: 10.2106/00004623-199903000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Lankhorst NE, Bierma-Zeinstra SM, van Middelkoop M. Factors associated with patellofemoral pain syndrome: a systematic review. Br J Sports Med. 2013;47(4):193–206. doi: 10.1136/bjsports-2011-090369. [DOI] [PubMed] [Google Scholar]
- 4.Utting MR, Davies G, Newman JH. Is anterior knee pain a predisposing factor to patellofemoral osteoarthritis? Knee. 2005;12(5):362–365. doi: 10.1016/j.knee.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 5.Thomas MJ, Wood L, Selfe J, Peat G. Anterior knee pain in younger adults as a precursor to subsequent patellofemoral osteoarthritis: a systematic review. BMC Musculoskelet Disord. 2010;11:201. doi: 10.1186/1471-2474-11-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wilk KE, Davies GJ, Mangine RE, Malone TR. Patellofemoral disorders: a classification system and clinical guidelines for nonoperative rehabilitation. J Orthop Sports Phys Ther. 1998;28(5):307–322. doi: 10.2519/jospt.1998.28.5.307. [DOI] [PubMed] [Google Scholar]
- 7.Jayaram P, Kennedy DJ, Yeh P, Dragoo J. Chondrotoxic effects of local anesthetics on human knee articular cartilage: a systematic review. PM R. 2019;11(4):379–400. doi: 10.1002/pmrj.12007. [DOI] [PubMed] [Google Scholar]
- 8.Powers CM, Witvrouw E, Davis IS, Crossley KM. Evidence-based framework for a pathomechanical model of patellofemoral pain: 2017 patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester, UK: part 3. Br J Sports Med. 2017;51(24):1713–1723. doi: 10.1136/bjsports-2017-098717. [DOI] [PubMed] [Google Scholar]
- 9.Liao T-C, Keyak JH, Powers CM. Runners with patellofemoral pain exhibit greater peak patella cartilage stress compared with pain-free runners. J Appl Biomech. 2018;34(4):298–305. doi: 10.1123/jab.2017-0229. [DOI] [PubMed] [Google Scholar]
- 10.Wille Christa M., Lenhart Rachel L., Wang Sijian, Thelen Darryl G., Heiderscheit Bryan C. Ability of Sagittal Kinematic Variables to Estimate Ground Reaction Forces and Joint Kinetics in Running. Journal of Orthopaedic & Sports Physical Therapy. 2014;44(10):825–830. doi: 10.2519/jospt.2014.5367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liao T-C, Powers CM. Tibiofemoral kinematics in the transverse and frontal planes influence the location and magnitude of peak patella cartilage stress: an investigation of runners with and without patellofemoral pain. Clin Biomech. 2019;62:72–78. doi: 10.1016/j.clinbiomech.2019.01.003. [DOI] [PubMed] [Google Scholar]
- 12.Neal BS, Lack SD, Lankhorst NE, Raye A, Morrissey D, van Middelkoop M. Risk factors for patellofemoral pain: a systematic review and meta-analysis. Br J Sports Med. 2019;53(5):270–281. doi: 10.1136/bjsports-2017-098890. [DOI] [PubMed] [Google Scholar]
- 13.Blond L, Hansen L. Patellofemoral pain syndrome in athletes: a 5.7-year retrospective follow-up study of 250 athletes. Acta Orthop Belg. 1998;64(4):393–400. [PubMed] [Google Scholar]
- 14.Willy RW, Davis IS. The effect of a hip-strengthening program on mechanics during running and during a single-leg squat. J Orthop Sports Phys Ther. 2011;41(9):625–632. doi: 10.2519/jospt.2011.3470. [DOI] [PubMed] [Google Scholar]
- 15.Snyder KR, Earl JE, O’Connor KM, Ebersole KT. Resistance training is accompanied by increases in hip strength and changes in lower extremity biomechanics during running. Clin Biomech (Bristol, Avon) 2009;24(1):26–34. doi: 10.1016/j.clinbiomech.2008.09.009. [DOI] [PubMed] [Google Scholar]
- 16.Winstein CJ, Pohl PS, Lewthwaite R. Effects of physical guidance and knowledge of results on motor learning: support for the guidance hypothesis. Res Q Exerc Sport. 1994;65(4):316–323. doi: 10.1080/02701367.1994.10607635. [DOI] [PubMed] [Google Scholar]
- 17.Winstein CJ. Knowledge of results and motor learning--implications for physical therapy. Phys Ther. 1991;71(2):140–149. doi: 10.1093/ptj/71.2.140. [DOI] [PubMed] [Google Scholar]
- 18.Noehren B, Hamill J, Davis I. Prospective evidence for a hip etiology in patellofemoral pain. Med Sci Sports Exerc. 2013;45(6):1120–1124. doi: 10.1249/MSS.0b013e31828249d2. [DOI] [PubMed] [Google Scholar]
- 19.Willson JD, Davis IS. Lower extremity mechanics of females with and without patellofemoral pain across activities with progressively greater task demands. Clin Biomech. 2008;23(2):203–211. doi: 10.1016/j.clinbiomech.2007.08.025. [DOI] [PubMed] [Google Scholar]
- 20.Dierks Tracy A., Manal Kurt T., Hamill Joseph, Davis Irene S. Proximal and Distal Influences on Hip and Knee Kinematics in Runners With Patellofemoral Pain During a Prolonged Run. Journal of Orthopaedic & Sports Physical Therapy. 2008;38(8):448–456. doi: 10.2519/jospt.2008.2490. [DOI] [PubMed] [Google Scholar]
- 21.Willy RW, Manal KT, Witvrouw EE, Davis IS. Are mechanics different between male and female runners with patellofemoral pain? Med Sci Sports Exerc. 2012;44(11):2165–2171. doi: 10.1249/MSS.0b013e3182629215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Souza RB, Powers CM. Predictors of hip internal rotation during running: an evaluation of hip strength and femoral structure in women with and without patellofemoral pain. Am J Sports Med. 2009;37(3):579–587. doi: 10.1177/0363546508326711. [DOI] [PubMed] [Google Scholar]
- 23.Souza RB, Powers CM. Differences in hip kinematics, muscle strength, and muscle activation between subjects with and without patellofemoral pain. J Orthop Sports Phys Ther. 2009;39(1):12–19. doi: 10.2519/jospt.2009.2885. [DOI] [PubMed] [Google Scholar]
- 24.Willy RW, Witvrouw E, Manal K, Davis IS. Are lower extremity mechanics different between male and female runners with patellofemoral pain syndrome? Med Sci Sport Exerc. 2012;44(11):2165–2171. doi: 10.1249/MSS.0b013e3182629215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Powers CM. The influence of abnormal hip mechanics on knee injury: a biomechanical perspective. J Orthop Sports Phys Ther. 2010;40(2):42–51. doi: 10.2519/jospt.2010.3337. [DOI] [PubMed] [Google Scholar]
- 26.Huberti HH, Hayes WC. Patellofemoral contact pressures. The influence of q-angle and tendofemoral contact. J Bone Joint Surg (Am Vol) 1984;66(5):715–724. doi: 10.2106/00004623-198466050-00010. [DOI] [PubMed] [Google Scholar]
- 27.Lee TQ, Morris G, Csintalan RP. The influence of tibial and femoral rotation on patellofemoral contact area and pressure. J Orthop Sports Phys Ther. 2003;33(11):686–693. doi: 10.2519/jospt.2003.33.11.686. [DOI] [PubMed] [Google Scholar]
- 28.Noehren B, Scholz J, Davis I. The effect of real-time gait retraining on hip kinematics, pain and function in subjects with patellofemoral pain syndrome. Br J Sports Med. 2010;45(9):691–696. doi: 10.1136/bjsm.2009.069112. [DOI] [PubMed] [Google Scholar]
- 29.Willy RW, Scholz JP, Davis IS. Mirror gait retraining for the treatment of patellofemoral pain in female runners. Clin Biomech. 2012;27(10):1045–1051. doi: 10.1016/j.clinbiomech.2012.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kulmala JP, Avela J, Pasanen K, Parkkari J. Forefoot strikers exhibit lower running-induced knee loading than rearfoot strikers. Med Sci Sports Exerc. 2013;45(12):2306–2313. doi: 10.1249/MSS.0b013e31829efcf7. [DOI] [PubMed] [Google Scholar]
- 31.Johnson CD, Outerleys J, Reilly JM, Tenforde AS, Davis IS. Increased ground reaction force load rates in runners with active patellofemoral pain. Med Sci Sports Exerc. 2019;51(supplement):438–439. doi: 10.1249/01.mss.0000561814.80487.cf. [DOI] [Google Scholar]
- 32.Cheung RT, Davis IS. Landing pattern modification to improve patellofemoral pain in runners: a case series. J Orthop Sports Phys Ther. 2011;41(12):914–919. doi: 10.2519/jospt.2011.3771. [DOI] [PubMed] [Google Scholar]
- 33.Roper JL, Harding EM, Doerfler D, Dexter JG, Kravitz L, Dufek JS, et al. The effects of gait retraining in runners with patellofemoral pain: a randomized trial. Clin Biomech (Bristol, Avon) 2016;35:14–22. doi: 10.1016/j.clinbiomech.2016.03.010. [DOI] [PubMed] [Google Scholar]
- 34.Dos Santos AF, Nakagawa TH, Lessi GC, Luz BC, Matsuo HTM, Nakashima GY, et al. Effects of three gait retraining techniques in runners with patellofemoral pain. Phys Ther Sport. 2019;36:92–100. doi: 10.1016/j.ptsp.2019.01.006. [DOI] [PubMed] [Google Scholar]
- 35.Teng Hsiang-Ling, Powers Christopher M. Sagittal Plane Trunk Posture Influences Patellofemoral Joint Stress During Running. Journal of Orthopaedic & Sports Physical Therapy. 2014;44(10):785–792. doi: 10.2519/jospt.2014.5249. [DOI] [PubMed] [Google Scholar]
- 36.Bonacci J, Hall M, Saunders N, Vicenzino B. Gait retraining versus foot orthoses for patellofemoral pain: a pilot randomised clinical trial. J Sci Med Sport. 2018;21(5):457–461. doi: 10.1016/j.jsams.2017.09.187. [DOI] [PubMed] [Google Scholar]
- 37.Esculier JF, Bouyer LJ, Dubois B, Fremont P, Moore L, McFadyen B, Roy JS. Is combining gait retraining or an exercise programme with education better than education alone in treating runners with patellofemoral pain?A randomised clinical trial. Br J Sports Med. 2018;52(10):659–666. doi: 10.1136/bjsports-2016-096988. [DOI] [PubMed] [Google Scholar]
- 38.Neal BS, Barton CJ, Birn-Jeffrey A, Daley M, Morrissey D. The effects & mechanisms of increasing running step rate: a feasibility study in a mixed-sex group of runners with patellofemoral pain. Phys Ther Sport. 2018;32:244–251. doi: 10.1016/j.ptsp.2018.05.018. [DOI] [PubMed] [Google Scholar]
- 39.Heiderscheit BC, Chumanov ES, Michalski MP, Wille CM, Ryan MB. Effects of step rate manipulation on joint mechanics during running. Med Sci Sports Exerc. 2011;43(2):296–302. doi: 10.1249/MSS.0b013e3181ebedf4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Willy RW, Buchenic L, Rogacki K, Ackerman J, Schmidt A, Willson JD. In-field gait retraining and mobile monitoring to address running biomechanics associated with tibial stress fracture. Scand J Med Sci Sports. 2016;26(2):197–205. doi: 10.1111/sms.12413. [DOI] [PubMed] [Google Scholar]
- 41.Lenhart RL, Thelen DG, Wille CM, Chumanov ES, Heiderscheit BC. Increasing running step rate reduces patellofemoral joint forces. Med Sci Sports Exerc. 2014;46(3):557–564. doi: 10.1249/MSS.0b013e3182a78c3a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Willson JD, Sharpe R, Meardon SA, Kernozek TW. Effects of step length on patellofemoral joint stress in females with and without patellofemoral pain. Clin Biomech. 2014;29:243–247. doi: 10.1016/j.clinbiomech.2013.12.016. [DOI] [PubMed] [Google Scholar]
- 43.Sinclair J. Effects of barefoot and barefoot inspired footwear on knee and ankle loading during running. Clin Biomech (Bristol, Avon) 2014;29(4):395–399. doi: 10.1016/j.clinbiomech.2014.02.004. [DOI] [PubMed] [Google Scholar]
- 44.Baldon Rde M, Piva SR, Scattone Silva R, Serrao FV. Evaluating eccentric hip torque and trunk endurance as mediators of changes in lower limb and trunk kinematics in response to functional stabilization training in women with patellofemoral pain. Am J Sports Med. 2015;43(6):1485–1493. doi: 10.1177/0363546515574690. [DOI] [PubMed] [Google Scholar]
- 45.Rabelo N, Costa LOP, Lima BM, Dos Reis AC, Bley AS, Fukuda TY, et al. Adding motor control training to muscle strengthening did not substantially improve the effects on clinical or kinematic outcomes in women with patellofemoral pain: a randomised controlled trial. Gait Posture. 2017;58:280–286. doi: 10.1016/j.gaitpost.2017.08.018. [DOI] [PubMed] [Google Scholar]
- 46.Salsich GB, Yemm B, Steger-May K, Lang CE, Van Dillen LR. A feasibility study of a novel, task-specific movement training intervention for women with patellofemoral pain. Clin Rehabil. 2018;32(2):179–190. doi: 10.1177/0269215517723055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Leibbrandt DC, Louw QA. Targeted functional movement retraining to improve pain, function, and biomechanics in subjects with anterior knee pain: a case series. J Sport Rehabil. 2018;27(3):218–223. doi: 10.1123/jsr.2016-0164. [DOI] [PubMed] [Google Scholar]
- 48.Yemm B, Krause DA. Management of a patient with patellofemoral pain syndrome using neuromuscular training in decreasing medial collapse: a case report. Physiother Theory Pract. 2015;31(3):221–229. doi: 10.3109/09593985.2014.982233. [DOI] [PubMed] [Google Scholar]
- 49.Noehren B, Scholz J, Davis I. The effect of real-time gait retraining on hip kinematics, pain and function in subjects with patellofemoral pain syndrome. Br J Sports Med. 2011;45(9):691–696. doi: 10.1136/bjsm.2009.069112. [DOI] [PubMed] [Google Scholar]
- 50.Wulf G, Shea C, Lewthwaite R. Motor skill learning and performance: a review of influential factors. Med Educ. 2010;44(1):75–84. doi: 10.1111/j.1365-2923.2009.03421.x. [DOI] [PubMed] [Google Scholar]
- 51.• Futrell EE, Gross KD, Reisman D, Mullineaux DR, Davis IS. Transition to forefoot strike reduces load rates more effectively than altered cadence. J Sport Health Sci. 2019. 10.1016/j.jshs.2019.07.006This RCT in healthy individuals compared the reduction of vertical load rates, often associated with patellofemoral pain between two retraining groups. One was retrained to increase their cadence, while the other transitioned to a forefoot strike pattern. Both of these retraining strategies are used as an intervention for runners with patellofemoral pain.
- 52.Chan ZYS, Zhang JH, Au IPH, An WW, Shum GLK, Ng GYF, et al. Gait retraining for the reduction of injury occurrence in novice distance runners: 1-year follow-up of a randomized controlled trial. Am J Sports Med. 2018;46(2):388–395. doi: 10.1177/0363546517736277. [DOI] [PubMed] [Google Scholar]
- 53.Bowser BJ, Fellin R, Milner CE, Pohl MB, Davis IS. Reducing impact loading in runners: a one-year follow-up. Med Sci Sports Exerc. 2018;50(12):2500–2506. doi: 10.1249/MSS.0000000000001710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Clansey AC, Hanlon M, Wallace ES, Nevill A, Lake MJ. Influence of tibial shock feedback training on impact loading and running economy. Med Sci Sports Exerc. 2014;46(5):973–981. doi: 10.1249/MSS.0000000000000182. [DOI] [PubMed] [Google Scholar]
- 55.Teng HL, Powers CM. Sagittal plane trunk posture influences patellofemoral joint stress during running. J Orthop Sports Phys Ther. 2014;44(10):785–792. doi: 10.2519/jospt.2014.5249. [DOI] [PubMed] [Google Scholar]