Abstract
Purpose of Review
Anterior cruciate ligament (ACL) injury is one of the most common ligamentous injuries suffered by athletes participating in cutting sports. A common misperception is that ACL reconstruction can prevent osteoarthritis (OA). The goal of this paper is to review and discuss the contributing factors for the development of OA following ACL injury.
Recent Findings
There has been interesting new research related to ACL reconstruction. As understanding of knee biomechanics following ACL injury and reconstruction has changed over time, many surgeons have changed their surgical techniques to low anterior drilling to position their femoral tunnel in an attempt to place the ACL in a more anatomic position. Even with this change in the femoral tunnel position, 85% of knees following ACL reconstruction have abnormal tibial motion compared to contralateral non-injured knees. Studies have shown increases in inflammatory cytokines in the knee following ACL injury, and newer MRI sequences have allowed for earlier objective detection of degenerative changes to cartilage following injury. Recent studies have shown that injecting IL-1 receptor antagonist and corticosteroids can modulate the post-injury inflammatory cascade.
Summary
ACL reconstruction does not prevent the development of OA but can improve knee kinematics and reduce secondary injury to the cartilage and meniscus. Advancements in imaging studies has allowed for earlier detection of degenerative changes in the knee, which has allowed researchers to study how new interventions can alter the course of degenerative change in the knee following ACL injury.
Keywords: Anterior cruciate ligament, ACL reconstruction, Osteoarthritis
Introduction
Epidemiology of ACL Injury
Anterior cruciate ligament (ACL) rupture is a common injury suffered by athletes in sports that require quick pivoting and cutting, such as soccer, football, and skiing [1]. The incidence of ACL tears in the general population has been estimated at 0.8 per 1000 people, though this number is likely skewed by a higher prevalence in younger, more athletic populations [1, 2]. It is estimated that anywhere between up to 250,000 ACL ruptures occur annually in the USA alone, and the majority of injuries occur in people under the age of 30 [1–3].
From the moment of the initial ACL injury, the future health and function of the knee is profoundly affected. Roughly half of ACL-injured knees progress to osteoarthritis (OA) within 5–15 years after the initial injury, and at least a portion of this elevated risk of OA may be a result of trauma from the initial injury itself [4–6]. Patients electing to proceed with ACL reconstruction often do so with the goal of returning to sports that involve pivoting and cutting [7]. The Multicenter Orthopaedic Outcomes Network (MOON) group has reported that approximately 70% of athletes return to high-level sports after ACL reconstruction, with fear of reinjury and risk of further damage commonly cited as reasons for failure to do so [8]. ACL reconstruction enables patients to return to sport though it does not reliably alter the natural history of post-traumatic osteoarthritis (PTOA). Long-term studies demonstrate that around 50% of patients who undergo ACL reconstruction still develop OA within 12–14 years [9, 10].
With the high prevalence of ACL injuries and the young population affected by these injuries, it is important to understand the specific factors that may contribute to the elevated risk of OA after an ACL injury. The goal of this paper is to review the contributing factors for knee OA after ACL injury and how ACL reconstruction may influence these outcomes.
Debilitating Effects of Knee OA
Osteoarthritis is one of the most prevalent diseases in the USA and is the most common musculoskeletal disease. It is estimated that up to 67 million adults in the USA will be affected by OA by 2030 [11]. OA is characterized by a loss of articular cartilage, and is associated with osteophyte formation, subchondral bone changes, bone cysts, and synovitis and loss of joint space on radiographic evaluation [12]. Clinically, OA is often associated with pain, stiffness, and functional impairment [12]. A combination of patient symptoms and radiographic changes are used to make the clinical diagnosis of OA. In 2005, clinic visits for the primary diagnosis of OA were second only to those for hypertension. Health care costs attributed to OA constitute up to 3.5% of the national hospital bill in the USA, making it the fifth most expensive condition treated in 2008 [13].
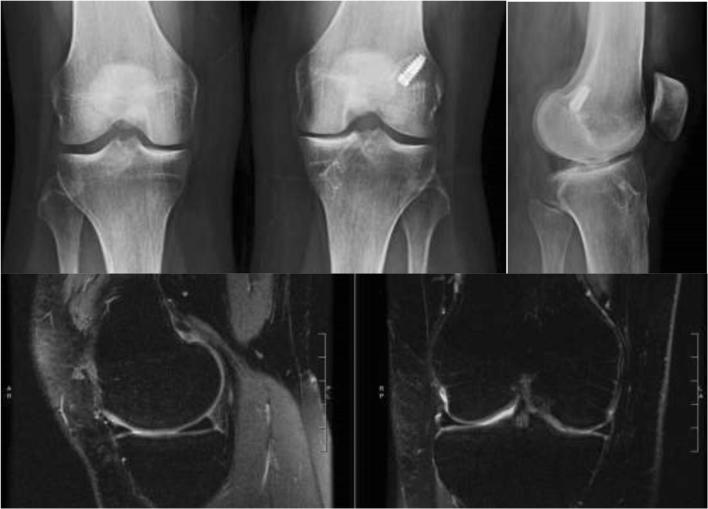
While the causes of OA are multifactorial, an estimated 12% of cases of symptomatic OA in the USA are attributed to PTOA [14]. One of the most common causes of knee PTOA is ACL injury [12, 15]. ACL tears most commonly occur in a younger, more active population, which is generally free of other risk factors for developing knee OA [16]. This injury can lead to a monumental change of the trajectory in the health of their injured knee. The prevalence of knee OA after an isolated ACL injury has been reported as up to 13% [17]. When associated with meniscal injuries, this rate increases up to 21 to 48% of patients [17]. Imaging and long-term studies have shown that changes in the articular cartilage occur in the medial compartment of the knee first [18], and long-term changes show that the medial compartment is more commonly affected than the lateral side (Fig. 1) [19].
Fig. 1.
XR and T2 weighted MRI showing early evidence of left knee medial wear and medial compartment breakdown following ACL reconstruction compared to the contralateral, non-injured knee
Though it is known that ACL injury leads to radiographic OA, the reported association between radiographic knee OA and symptomatic knee pain and function is inconsistent [20–22]. Øiestad et al. examined 210 patients who were 10–15 years from an ACL reconstruction and compared knee radiographs to KOOS outcome scores. The group found that patients with any radiographic knee OA had significantly increased symptoms compared with those without radiographic OA [23]. While radiographic OA may be an incidental finding, patients with a history of ligament reconstruction undergo TKA at a significantly younger age relative to patients without this prior surgical history. A total joint registry of over 1300 patients found that mean age of patients who had previous ligament reconstruction and underwent knee arthroplasty was 50.2 ± 9.1 compared to 59.9 ± 9.6 for those who did not have a ligament reconstruction [24]. Given that ACL injury is a leading cause of PTOA in a younger population, there has been growing interest to understand the pathophysiology of PTOA following ACL injury as well factors that may alter the natural history of the knee following ACL reconstruction.
Potential Pathophysiology for Post-Traumatic OA after ACL Injury
Mechanical Alterations/Neuromuscular Changes
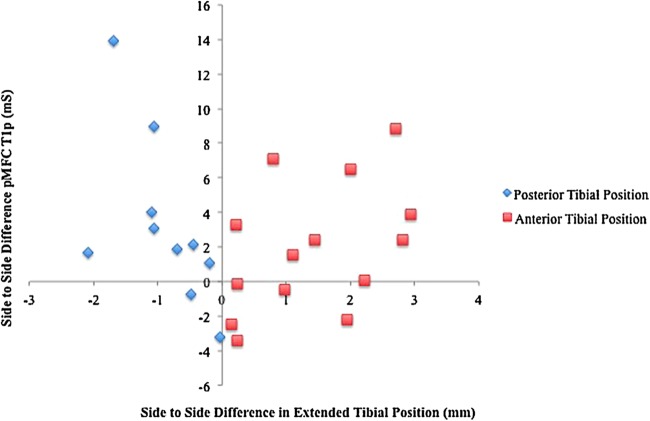
After ACL tear, a number of kinematic changes occur at the knee joint including an anterior shift of the tibia relative to the femur, increased anterior-posterior translation of the knee, increased internal rotation, and decreased external of the tibia during knee range of motion [1, 25]. Even after ACL reconstruction, which restores stability to the knee, an abnormal anterior position of the tibia has been linked with evidence of early degenerative cartilage changes as soon as 1 year after surgery, suggesting this persistence of abnormal kinematics may contribute to the development of PTOA (Fig. 2) [26]. Additionally, biomechanical studies have shown that 85% ACL reconstructed knees, as compared to the contralateral knees, have abnormal tibial rotation during the stance phase of gait [27]. Besides providing physical restraint, the ACL also serves an important role for proprioception within the knee. Disruption of the native ACL may impair the dynamic stabilizers of the knee, such as the quadriceps and hamstrings, in sensing joint positioning [28], which may contribute to knee instability. Though there is no single explanation, it is likely that a combination of these kinematic changes contributes to the finding that patients still develop early radiographic OA after ACL reconstruction.
Fig. 2.
Newer imaging modalities like T1ρ MRI can detect changes to the cartilage following ACL reconstruction. This figure shows the relationship between tibial position (x-axis) and changes in T1ρ MRI relaxation values (y-axis) following ACL reconstruction. Values on the left of the origin signify that the tibia has a more posterior position and the knee may be over-constrained, whereas values to the right of the origin show that the tibia is more anterior and suggests that the graft may be loose. Borrowed with permission from Zaid et al. [26]
Quadriceps atrophy and residual muscle weakness following knee injuries is another obstacle that arises after ACL injury. Due to ongoing neuromuscular deficits, less than half of patients with ACL tears were able to achieve normal strength levels as far out as 2–5 years after injury [29]. Quadriceps weakness following ACL surgery directly correlates with radiographic joint space narrowing in patients with PTOA [29]. Psychological factors following injury, such as pain and fear of reinjury, have also been shown to affect muscle activation patterns thus affecting joint stabilization [30]. It is likely that a combination of all these factors lead to an abnormal distribution of forces and torques across the knee, which alters cartilage contact forces [31]. These alterations can lead to changes in chondrocyte gene expression and thus changes in the structure and mechanical properties of the articular cartilage [32].
Inflammatory Response
Following ACL injury, it has been shown that numerous cytokine levels, such as TNF-a, IL-1B, and MMP-1 and MMP-13, immediately increase within the joint [33, 34]. TNF-a has been linked to an increase in the apoptotic caspase pathway within chondrocytes [32]. This finding is further corroborated by the increase in chondrocyte apoptosis seen in the days following initial injury [35]. While the levels of these cytokines slowly fall with time, ACL-deficient knees continue to demonstrate increased levels of inflammatory cytokines up to at least 1 year after injury [36, 37].
Mechanical activation of chondrocytes during injury has been shown to alter their gene expression leading to activation of degradative enzymes such as matrix metalloproteinases (MMPs) [32]. MMPs, in turn, contribute to the degradation of extracellular matrix (ECM) proteins such as glycosaminoglycans (GAGs) and collagen. These elevated levels of MMPs within the joint have been shown to persist long after the initial injury, thus causing continuous degeneration of GAGs and collagen up to 12 months afterwards [38, 39]. While chondrocytes have some ability to respond to injury, an ACL injury might cross a threshold where this catabolic cascade from MMPs overwhelms the regenerative capacity of chondrocytes. This may be yet another mechanism that contributes to the development of PTOA following ACL tear.
There have been some early studies examining whether the inflammatory and catabolic cascade of events which occurs following a knee injury can be pharmacologically counteracted during the acute post-injury period. IL-1 levels are elevated following ACL injury, and its levels correlate with the severity of chondral damage [40]. Decreasing the levels of IL-1 may be a target of future therapies. To test this hypothesis, Kraus et al. conducted a small randomized controlled pilot study looking at the clinical effects of early aspiration of the knee and injection of IL-1 receptor antagonist (IL-1Ra) versus placebo [41]. The authors found that patients who received an early injection of IL-1Ra after injury had improved patient reported outcomes compared to those receiving placebo injections. Similarly, Lattermann et al. evaluated the effect of aspiration and injection with corticosteroids versus saline [42••]. There were no changes in patient reported outcomes, but there were significantly fewer collagen breakdown products following the corticosteroid injection relative to placebo. These early findings suggest that modulation of the initial inflammatory response after injury may have potential lasting effects on early knee cartilage degeneration.
Meniscal/Cartilage Insult at Time of Injury
During any injury to a joint, shear and compressive forces on the articular cartilage may create stress fractures through the cartilage matrix and as well as the underlying bone [43]. Unlike bone, articular cartilage lacks regenerative capacity which likely contributes to the development of PTOA following injury [44, 45]. One study assessing ankle fractures confirmed this finding [46]. Any intra-articular fracture in the ankle joint was found to lead to PTOA even if visually assessed anatomic joint reduction was achieved intra-operatively.
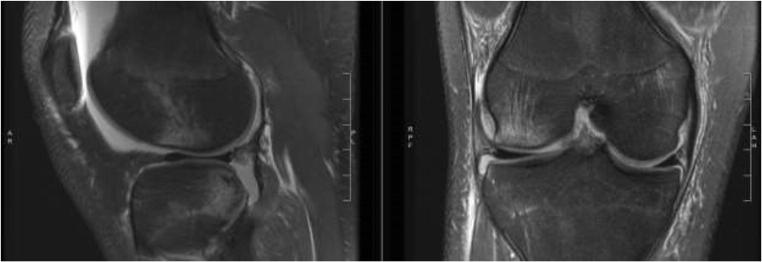
While most ACL tears are not associated with intra-articular fractures, the injury mechanism may still be traumatic enough to the joint to induce lasting cartilage damage. At the time of ACL injury, there is frequently an impaction injury with subchondral bone marrow edema, indicating load transmission through the articular cartilage. Typically, there may be bone marrow contusions at the posterolateral tibial plateau and the central aspect of the lateral femoral condyle due to the initial impact of the ACL injury (Fig. 3). The effects of this direct cartilage injury may persist even in the absence of visualizable injury at the articular cartilage. It has been reported though that the prevalence of cartilage injury following acute ACL injury is between 16 and 46% [47]. The true incidence of articular cartilage damage may be higher. Using MRI, it has been reported that up to 100% of knees imaged after ACL rupture had some evidence of cartilage damage after injury [48]. This immediate cartilage damage from the initial injury is not sufficient to account for development of PTOA following ACL tear. Most ACL tears have concomitant damage to the lateral tibial plateau and lateral femoral condyle, yet PTOA more commonly affects medial compartment in these patients.
Fig. 3.
T2 weighted MRI showing the typical bone bruise pattern for ACL tear with lateral femoral contusion, posterior lateral tibial contusion, and posterior lateral meniscus tear
In addition to cartilage damage following ACL injury, the meniscus is commonly affected. Large population-based studies of patients with ACL tears have shown the prevalence of meniscal tears to be between 47 and 61% [49, 50], with the timing of presentation following injury influencing the type of meniscal injury. Lateral meniscal injuries are more common in the acute setting. For patients who undergo arthroscopic evaluation and surgical treatment for their ACL tear and associated injuries within 8 weeks of injury, 69.4% have lateral meniscus injuries, 19.9% have medial and lateral meniscal injuries, and 10.8% have been found to have medial meniscal injuries [51]. The same study found a higher incidence of medial meniscus and medial and lateral meniscus injuries in patients undergoing surgery more than 8 weeks from injury [51]. This is likely because the medial meniscus acts as a secondary stabilizer to anterior translation and sees more stress in the ACL-deficient states, and therefore is more prone to injury.
Meniscal tear patterns are variable, and each type of tear has different clinical implications. Meniscal root injuries, defined as radial tears occurring within 1 cm of the posterior insertion sites of the meniscus, are important to recognize. Root tears cause an inability of the meniscus to resist hoop stresses leading to significantly increased tibiofemoral contact pressures [52], which may predispose knees to arthritic changes. Repair of medial and lateral meniscal root tears can have a dramatic effect on the long-term health of the knee. One study showed that 35% of patients with partial medial meniscectomy for root injury undergo TKA at 5 years following surgery, whereas no patients underwent TKA who had a medial meniscal root repair [53]. The lateral meniscal root is estimated to be injured in 7–12% of patients with ACL injury [54], and lateral meniscal root repair can restore tibiofemoral contact pressures [55]. A thorough understanding of associated meniscal injuries at the time of ACL injury, and how differences in management of these injuries affect the natural history of PTOA is important. Physicians should make every effort to restore the integrity of meniscal hoop stresses through meniscal repair and preserve meniscus, which may improve knee kinematics and may affect the onset of PTOA.
Can ACL Reconstruction Alter the Natural History of PTOA?
ACL injury alone can lead to the development of knee OA regardless of whether a patient undergoes ACL reconstruction or conservative treatment. Recently, it has been reported that there is a 57% incidence of knee OA 14 years following ACL reconstruction, compared to an 18% incidence of knee OA in the contralateral knee [56]. In a 2014 meta-analysis, the relative risk (RR) of developing radiographic signs of moderate to severe osteoarthritis (Kellgren & Lawrence grade III or IV) was 3.84 (P < 0.0004), with 20.3% of ACL-injured knees with moderate or severe radiologic changes compared with 4.9% of uninjured contralateral knees at an average of 10 years. ACL-injured knees that did not undergo reconstruction had a significantly higher RR (RR, 4.98; P < 0.00001) of developing any grade of osteoarthritis compared with those treated with surgery (RR, 3.62; P < 0.00001) [57]. In a more recent meta-analysis, the prevalence of radiographic knee OA following ACL reconstruction at 5, 10, and 20 years after surgery was 11.3% (6.4–19.1%), 20.6% (14.9–27.7%), and 51.6% (29.1–73.5%), respectively [58••].
One common misperception is that ACL reconstruction prevents OA. Though ACL reconstruction does not prevent the eventual development of knee OA, one study suggested that it can delay its onset [56]. This is in contrast to other studies which have found an increased evidence of knee OA following ACL reconstruction compared to patients with chronic ACL tears treated conservatively [7]. Though ACL reconstruction may not prevent knee OA, it can reduce secondary injury to the meniscus and cartilage. Compared to a non-operative cohort of patients with ACL injuries, Chalmers et al. found that ACL reconstruction had an approximately twofold decreased need for secondary operation of meniscal surgery [59].
Meniscus and cartilage injuries alone can lead to the development of knee OA. Cross-sectional studies have demonstrated that regardless of their morphology, meniscus tears can predict the development of knee OA [60, 61]. Similarly, in early follow up, focal cartilage lesions have led to progression of knee OA [62]. In the setting of ACL injury, the status of the meniscus and the cartilage play a big role in the development of knee OA. At an average of 7.5 years following ACL reconstruction, 3% of patients with intact cartilage and menisci during ACL reconstruction had abnormal IKDC radiographic scores compared to 32% of patients with injury to both cartilage and menisci at the time of surgery [63]. At 10–15 years following ACL reconstruction, 80% of patients with combined ACL and meniscus or cartilage injuries developed knee OA compared to 62% with isolated ACL injury [64]. In the same cohort study, only 15% of contralateral uninjured knees developed knee OA. In a computer model used to estimate the timing of total knee arthroplasty and knee OA, Suter et al. found that the lifetime risk of symptomatic OA was 34% with combined ACL and meniscal injuries compared to 16% for isolated ACL injuries and 14% for uninjured controls [65]. Based on our current understanding, patients without ACL injury have the lowest risk for knee OA followed by isolated ACL injury, followed by combined injuries of the ACL and meniscus or cartilage.
There is some debate if the timing of ACL reconstruction following injury may also influence the eventual onset of knee OA. Jomha et al. followed 72 patients for 7 years following BTB ACL reconstruction and found that early reconstruction with meniscal preservation led to the lowest incidence of degenerative changes on radiographic follow up compared to delayed ACL reconstruction, or reconstruction with meniscus debridement [66]. These findings differ from findings from another cohort study by Harris et al. which showed that early ACL reconstruction led to a higher proportion of tibiofemoral radiographic OA (16 vs. 7%) compared to delayed ACL reconstruction [67]. Additionally, it has been shown that the subsequent risk of having a meniscus tear or undergoing TKA were no different between patients undergoing early ACL reconstruction compared to matched patients without ACL injury [68••]. Finally, early ACL reconstruction within 6 months of injury has a lower risk of concomitant meniscal surgery, and within 12 months of injury has a lower risk of concomitant cartilage injury [69].
Future Directions
There has been extensive research examining the effects of ACL reconstruction on the short-term and long-term health of the knee, but there is still work to be done. Much of our understanding related to PTOA following ACL injury comes from long-term follow up studies and retrospective studies of total joint registries and radiographic evaluation of knees decades after the initial injury. Though these studies have helped clinicians better understand the natural history of PTOA following knee injury, quantitative MRI imaging is allowing for earlier and more objective analysis of articular cartilage changes [70••]. By identifying changes in articular cartilage earlier in the disease process, clinicians may have the opportunity to intervene early and follow the effects of those interventions over time. As understanding of knee kinematics has changed, so has surgical technique. In a follow up survey study in 2014, low anterior femoral tunnel drilling was preferred by 47% of surgeon respondents, compared to 15% in a survey from 5 years previous. Additionally, the position of the tibial tunnel shifted anteriorly, and the femoral tunnel shifted posterior-superiorly [71]. As our understanding of ACL biomechanics improves, surgical techniques will continue to be refined to better re-create normal knee kinematics. Lastly, it will be exciting to see how injectable biologics and pharmaceuticals will affect the inflammatory cascade. What seems to be apparent is that prevention of injury, reduction of catabolic cytokines following injury, restoration of the normal kinematics of the knee, and preservation of meniscus and cartilage are all key factors in preserving the long-term health of the knee.
Conclusion
The final common pathway for end-stage, symptomatic knee OA is total knee arthroplasty. As many ACL injuries occur in a younger population, the ultimate goal in the care of these patients is to reduce the incidence of knee OA and eventual TKA. ACL injury alone leads to increased inflammatory markers in the knee which can influence the development of knee osteoarthritis, which cannot be reversed by ACL reconstruction. Additionally, mechanical alterations in ACL-injured patients may predispose patients to secondary chondral and meniscal injuries. Early ACL reconstruction versus late ACL reconstruction may have an effect on secondary injuries and may influence the onset of knee OA. Each of these areas likely contributes to the development of knee OA, and future research could focus identifying the exact inflammatory modulators that affect OA, while focusing on anti-inflammatory treatment. Additionally, as biomechanical research continues to focus on the knee and our surgical techniques improve, we continue to an improved understanding of how to restore normal knee kinematics with surgical treatments.
Funding
No funding was received.
Compliance with Ethical Standards
Conflict of Interest
Edward C. Cheung and Marcus DiLallo declare that they have no conflict of interest. Brian T. Feeley reports he is a board or committee member of the American Orthopaedic Society for Sports Medicine and Orthopaedic Research Society and on the editorial or governing board for the Journal of Shoulder and Elbow Surgery and Current Reviews in Musculoskeletal Medicine. Drew A. Lansdown reports that he has research and educational support from Arthrex and Smith and Nephew and is a board or committee member of the Arthroscopy Association of North America.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on ACL: Risk Factors, Outcomes, Preventions
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Edward C. Cheung, Email: echeung@mednet.ucla.edu
Marcus DiLallo, Email: marcus.dilallo@ucsf.edu.
Brian T. Feeley, Email: brain.feeley@ucsf.edu
Drew A. Lansdown, Email: drew.lansdown@ucsf.edu
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
- 1.Carbone A, Rodeo S. Review of current understanding of post-traumatic osteoarthritis resulting from sports injuries. J Orthop Res. 2017;35(3):397–405. doi: 10.1002/jor.23341. [DOI] [PubMed] [Google Scholar]
- 2.Majewski M, Susanne H, Klaus S. Epidemiology of athletic knee injuries: a 10-year study. Knee. 2006;13(3):184–188. doi: 10.1016/j.knee.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 3.Hewett TE, Di Stasi SL, Myer GD. Current concepts for injury prevention in athletes after anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41(1):216–224. doi: 10.1177/0363546512459638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Segawa H, Omori G, Koga Y. Long-term results of non-operative treatment of anterior cruciate ligament injury. Knee. 2001;8(1):5–11. doi: 10.1016/s0968-0160(00)00062-4. [DOI] [PubMed] [Google Scholar]
- 5.Daniel DM, Lou SM, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of the ACL-injured patient. A prospective outcome study. Am J Sports Med. 1994;22(5):632–644. doi: 10.1177/036354659402200511. [DOI] [PubMed] [Google Scholar]
- 6.Kessler MA, Behrend H, Henz S, Stutz G, Rukavina A, Kuster MS. Function, osteoarthritis and activity after ACL-rupture: 11 years follow-up results of conservative versus reconstructive treatment. Knee Surg Sport Traumatol Arthrosc. 2008;16(5):442–448. doi: 10.1007/s00167-008-0498-x. [DOI] [PubMed] [Google Scholar]
- 7.Meuffels DE, Favejee MM, Vissers MM, Heijboer MP, Reijman M, Verhaar JAN. Ten year follow-up study comparing conservative versus operative treatment of anterior cruciate ligament ruptures. A matched-pair analysis of high level athletes. Br J Sport Med. 2009;43(5):347–351. doi: 10.1136/bjsm.2008.049403. [DOI] [PubMed] [Google Scholar]
- 8.Brophy RH, Schmitz L, Wright RW, Dunn WR, Parker RD, Andrish JT, et al. Return to play and future ACL injury risk after ACL reconstruction in soccer athletes from the Multicenter Orthopaedic Outcomes Network (MOON) group. Am J Sport Med. 2012;40(11):2517–2522. doi: 10.1177/0363546512459476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barenius B, Ponzer S, Shalabi A, Bujak R, Norlén L, Eriksson K. Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. Am J Sports Med. 2014;42(5):1049–1057. doi: 10.1177/0363546514526139. [DOI] [PubMed] [Google Scholar]
- 10.Lohmander LS, Östenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50(10):3145–3152. doi: 10.1002/art.20589. [DOI] [PubMed] [Google Scholar]
- 11.Hootman JM, Helmick CG. Projections of US prevalence of arthritis and associated activity limitations. Arthritis Rheum. 2006;54:226–229. doi: 10.1002/art.21562. [DOI] [PubMed] [Google Scholar]
- 12.Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med. 2007. [DOI] [PubMed]
- 13.Neogi T. The epidemiology and impact of pain in osteoarthritis. Osteoarthr Cartil. 2013;21(9):1145–1153. doi: 10.1016/j.joca.2013.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Suomalainen P, Järvelä S, Paakkala A, Kannus P, Järvinen M. Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective randomized study with 5-year results. Am J Sports Med. 2012;40(7):1511–1518. doi: 10.1177/0363546512448177. [DOI] [PubMed] [Google Scholar]
- 15.Louboutin H, Debarge R, Richou J, Selmi TAS, Donell ST, Neyret P, Dubrana F. Osteoarthritis in patients with anterior cruciate ligament rupture: a review of risk factors. Knee. 2009;16(4):239–244. doi: 10.1016/j.knee.2008.11.004. [DOI] [PubMed] [Google Scholar]
- 16.Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS. A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med. 2010;363(4):331–342. doi: 10.1056/NEJMoa0907797. [DOI] [PubMed] [Google Scholar]
- 17.Øiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37(7):1434–1443. doi: 10.1177/0363546509338827. [DOI] [PubMed] [Google Scholar]
- 18.Kumar D, Su F, Wu D, Pedoia V, Heitkamp L, Ma CB, et al. Frontal plane knee mechanics and early cartilage degeneration in people with anterior cruciate ligament reconstruction: a longitudinal study. Am J Sports Med. 2018;46(2):387–378. doi: 10.1177/0363546517739605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Seon JK, Song EK, Park SJ. Osteoarthritis after anterior cruciate ligament reconstruction using a patellar tendon autograft. Int Orthop. 2006. [DOI] [PMC free article] [PubMed]
- 20.Hannan MT, Felson DT, Pincus T. Analysis of the discordance between radiographic changes and knee pain in osteoarthritis of the knee. J Rheumatol. 2000;27(6):1513–1517. [PubMed] [Google Scholar]
- 21.Barker K, Lamb SE, Toye F, Jackson S, Barrington S. Association between radiographic joint space narrowing, function, pain and muscle power in severe osteoarthritis of the knee. Clin Rehabil. 2004;18(7):793–800. doi: 10.1191/0269215504cr754oa. [DOI] [PubMed] [Google Scholar]
- 22.Szebenyi B, Hollander AP, Dieppe P, Quilty B, Duddy J, Clarke S, Kirwan JR. Associations between pain, function, and radiographic features in osteoarthritis of the knee. Arthritis Rheum. 2006;54(1):230–235. doi: 10.1002/art.21534. [DOI] [PubMed] [Google Scholar]
- 23.Øiestad BE, Holm I, Engebretsen L, Risberg MA. The association between radiographic knee osteoarthritis and knee symptoms, function and quality of life 10-15 years after anterior cruciate ligament reconstruction. Br J Sports Med. 2011;45(7):583–588. doi: 10.1136/bjsm.2010.073130. [DOI] [PubMed] [Google Scholar]
- 24.Brophy RH, Gray BL, Nunley RM, Barrack RL, Clohisy JC. Total knee arthroplasty after previous knee surgery: expected interval and the effect on patient age. J Bone Jt Surg. 2014;96(10):801–805. doi: 10.2106/JBJS.M.00105. [DOI] [PubMed] [Google Scholar]
- 25.Andriacchi TP, Dyrby CO. Interactions between kinematics and loading during walking for the normal and ACL deficient knee. J Biomech. 2005;38(2):293–298. doi: 10.1016/j.jbiomech.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 26.Zaid M, Lansdown D, Su F, Pedoia V, Tufts L, Rizzo S, Souza RB, Li X, Ma CB. Abnormal tibial position is correlated to early degenerative changes one year following ACL reconstruction. J Orthop Res. 2015;33:1079–1086. doi: 10.1002/jor.22867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Scanlan SF, Chaudhari AMW, Dyrby CO, Andriacchi TP. Differences in tibial rotation during walking in ACL reconstructed and healthy contralateral knees. J Biomech. 2010;43(9):1817–1822. doi: 10.1016/j.jbiomech.2010.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reider B, Arcand MA, Diehl LH, Mroczek K, Abulencia A, Stroud CC, et al. Proprioception of the knee before and after anterior cruciate ligament reconstruction. Arthrosc J Arthrosc Relat Surg. 2003;19(1):2–12. doi: 10.1053/jars.2003.50006. [DOI] [PubMed] [Google Scholar]
- 29.Ageberg E, Thomeé R, Neeter C, Silbernagel KG, Roos EM. Muscle strength and functional performance in patients with anterior cruciate ligament injury treated with training and surgical reconstruction or training only: a two to five-year followup. Arthritis Rheum. 2008;59(12):1773–1779. doi: 10.1002/art.24066. [DOI] [PubMed] [Google Scholar]
- 30.Brewer BW, Cornelius AE, Sklar JH, Van Raalte JL, Tennen H, Armeli S, et al. Pain and negative mood during rehabilitation after anterior cruciate ligament reconstruction: a daily process analysis. Scand J Med Sci Sport. 2007;17(5):520–529. doi: 10.1111/j.1600-0838.2006.00601.x. [DOI] [PubMed] [Google Scholar]
- 31.Di Stasi SL, Logerstedt D, Gardinier ES, Snyder-Mackler L. Gait patterns differ between ACL-reconstructed athletes who pass return-to-sport criteria and those who fail. Am J Sports Med. 2013;41(6):1310–1318. doi: 10.1177/0363546513482718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kramer WC, Hendricks KJ, Wang J. Pathogenetic mechanisms of posttraumatic osteoarthritis: opportunities for early intervention. Int J Clin Exp Med. 2011;4(4):285–298. [PMC free article] [PubMed] [Google Scholar]
- 33.Irie K, Uchiyama E, Iwaso H. Intraarticular inflammatory cytokines in acute anterior cruciate ligament injured knee. Knee. 2003;10(1):93–96. doi: 10.1016/s0968-0160(02)00083-2. [DOI] [PubMed] [Google Scholar]
- 34.Haslauer CM, Elsaid KA, Fleming BC, Proffen BL, Johnson VM, Murray MM. Loss of extracellular matrix from articular cartilage is mediated by the synovium and ligament after anterior cruciate ligament injury. Osteoarthr Cartil. 2013;21(12):1950–1957. doi: 10.1016/j.joca.2013.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.D’Lima DD, Hashimoto S, Chen PC, Colwell CW, Lotz MK. Human chondrocyte apoptosis in response to mechanical injury. Osteoarthr Cartil. 2001;9(8):712–719. doi: 10.1053/joca.2001.0468. [DOI] [PubMed] [Google Scholar]
- 36.Edd SN, Giori NJ, Andriacchi TP. The role of inflammation in the initiation of osteoarthritis after meniscal damage. J Biomech. 2015;48(8):1420–1426. doi: 10.1016/j.jbiomech.2015.02.035. [DOI] [PubMed] [Google Scholar]
- 37.Harkey MS, Luc BA, Golightly YM, Thomas AC, Driban JB, Hackney AC, Pietrosimone B. Osteoarthritis-related biomarkers following anterior cruciate ligament injury and reconstruction: a systematic review. Osteoarthr Cartil. 2015;23(1):1–12. doi: 10.1016/j.joca.2014.09.004. [DOI] [PubMed] [Google Scholar]
- 38.Wei L, Fleming BC, Sun X, Teeple E, Wu W, Jay GD, Elsaid KA, Luo J, Machan JT, Chen Q. Comparison of differential biomarkers of osteoarthritis with and without posttraumatic injury in the Hartley guinea pig model. J Orthop Res. 2010;28(7):900–906. doi: 10.1002/jor.21093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yang KGA, Saris DBF, Verbout AJ, Creemers LB, Dhert WJA. The effect of synovial fluid from injured knee joints on in vitro chondrogenesis. Tissue Eng. 2006;12(10):2957–2964. doi: 10.1089/ten.2006.12.2957. [DOI] [PubMed] [Google Scholar]
- 40.Marks PH, Donaldson MLC. Inflammatory cytokine profiles associated with chondral damage in the anterior cruciate ligament-deficient knee. Arthrosc J Arthrosc Relat Surg. 2005;21:1342–1347. doi: 10.1016/j.arthro.2005.08.034. [DOI] [PubMed] [Google Scholar]
- 41.Kraus VB, Birmingham J, Stabler TV, Feng S, Taylor DC, Moorman CT, et al. Effects of intraarticular IL1-Ra for acute anterior cruciate ligament knee injury: a randomized controlled pilot trial ( NCT00332254) Osteoarthr Cartil. 2012;20:271–278. doi: 10.1016/j.joca.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 42.Lattermann C, Jacobs CA, Proffitt Bunnell M, Huston LJ, Gammon LG, Johnson DL, et al. A multicenter study of early anti-inflammatory treatment in patients with acute anterior cruciate ligament tear. Am J Sports Med. 2016;45(2):325–333. doi: 10.1177/0363546516666818. [DOI] [PubMed] [Google Scholar]
- 43.Falah M, Nierenberg G, Soudry M, Hayden M, Volpin G. Treatment of articular cartilage lesions of the knee. Int Orthop. 2010;35(5):621–630. doi: 10.1007/s00264-010-0959-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ichiba A, Kishimoto I. Effects of articular cartilage and meniscus injuries at the time of surgery on osteoarthritic changes after anterior cruciate ligament reconstruction in patients under 40 years old. Arch Orthop Trauma Surg. 2009;129(3):409–415. doi: 10.1007/s00402-008-0786-4. [DOI] [PubMed] [Google Scholar]
- 45.Keays SL, Newcombe PA, Bullock-Saxton JE, Bullock MI, Keays AC. Factors involved in the development of osteoarthritis after anterior cruciate ligament surgery. Am J Sports Med. 2010;38(3):455–463. doi: 10.1177/0363546509350914. [DOI] [PubMed] [Google Scholar]
- 46.Etter C, Ganz R. Long-term results of tibial plafond fractures treated with open reduction and internal fixation. Arch Orthop Trauma Surg. 1991;110(6):277–283. doi: 10.1007/BF00443458. [DOI] [PubMed] [Google Scholar]
- 47.Brophy RH, Zeltser D, Wright RW, Flanigan D. Anterior cruciate ligament reconstruction and concomitant articular cartilage injury: incidence and treatment. Arthrosc J Arthrosc Relat Surg. 2010;26(1):112–120. doi: 10.1016/j.arthro.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 48.Potter HG, Jain SK, Ma Y, Black BR, Fung S, Lyman S. Cartilage injury after acute, isolated anterior cruciate ligament tear: immediate and longitudinal effect with clinical/MRI follow-up. Am J Sports Med. 2012;40(2):276–285. doi: 10.1177/0363546511423380. [DOI] [PubMed] [Google Scholar]
- 49.Granan LP, Inacio MCS, Maletis GB, Funahashi TT, Engebretsen L. Intraoperative findings and procedures in culturally and geographically different patient and surgeon populations: an anterior cruciate ligament reconstruction registry comparison between Norway and the USA. Acta Orthop. 2012;83(6):577–582. doi: 10.3109/17453674.2012.741451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ahldén M, Samuelsson K, Sernert N, Forssblad M, Karlsson J, Kartus J. The Swedish national anterior cruciate ligament register: a report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med. 2012;40(10):2230–2235. doi: 10.1177/0363546512457348. [DOI] [PubMed] [Google Scholar]
- 51.Hagino T, Ochiai S, Senga S, Yamashita T, Wako M, Ando T, Haro H. Meniscal tears associated with anterior cruciate ligament injury. Arch Orthop Trauma Surg. 2015;135(12):1701–1706. doi: 10.1007/s00402-015-2309-4. [DOI] [PubMed] [Google Scholar]
- 52.Kamatsuki Y, Furumatsu T, Fujii M, Kodama Y, Miyazawa S, Hino T, et al. Complete tear of the lateral meniscus posterior root is associated with meniscal extrusion in anterior cruciate ligament deficient knees. J Orthop Res. 2018. [DOI] [PubMed]
- 53.Chung KS, Ha JK, Yeom CH, Ra HJ, Jang HS, Choi SH, et al. Comparison of clinical and radiologic results between partial meniscectomy and refixation of medial meniscus posterior root tears: a minimum 5-year follow-up. Arthrosc J Arthrosc Relat Surg. 2015. [DOI] [PubMed]
- 54.West RV, Kim JG, Armfield D, Harner CD. Lateral meniscal root tears associated with anterior cruciate ligament injury: classification and management (SS-70) Arthrosc J Arthrosc Relat Surg. 2004;20:e32–e33. [Google Scholar]
- 55.LaPrade CM, Jansson KS, Dornan G, Smith SD, Wijdicks CA, LaPrade RF. Altered tibiofemoral contact mechanics due to lateral meniscus posterior horn root avulsions and radial tears can be restored with in situ pull-out suture repairs. J Bone Jt Surg. 2014;96(6):471–479. doi: 10.2106/JBJS.L.01252. [DOI] [PubMed] [Google Scholar]
- 56.Mihelic R, Jurdana H, Jotanovic Z, Madjarevic T, Tudor A. Long-term results of anterior cruciate ligament reconstruction: a comparison with non-operative treatment with a follow-up of 17-20 years. Int Orthop. 2011;35(7):1093–1097. doi: 10.1007/s00264-011-1206-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ajuied A, Wong F, Smith C, Norris M, Earnshaw P, Back D, Davies A. Anterior cruciate ligament injury and radiologic progression of knee osteoarthritis: a systematic review and meta-analysis. Am J Sports Med. 2014;42(9):2242–2252. doi: 10.1177/0363546513508376. [DOI] [PubMed] [Google Scholar]
- 58.Cinque ME, Dornan GJ, Chahla J, Moatshe G, LaPrade RF. High rates of osteoarthritis develop after anterior cruciate ligament surgery: an analysis of 4108 patients. Am J Sports Med. 2018;46(3):2011–2019. doi: 10.1177/0363546517730072. [DOI] [PubMed] [Google Scholar]
- 59.Chalmers PN, Mall NA, Moric M, Sherman SL, Paletta GP, Cole BJ, et al. Does ACL reconstruction alter natural history?: a systematic literature review of long-term outcomes. J Bone Jt Surg. 2014;96(4):292–300. doi: 10.2106/JBJS.L.01713. [DOI] [PubMed] [Google Scholar]
- 60.Englund M, Guermazi A, Lohmander SL. The role of the meniscus in knee osteoarthritis: a cause or consequence? Radiol Clin N Am. 2009. [DOI] [PubMed]
- 61.Englund M, Guermazi A, Roemer FW, Aliabadi P, Yang M, Lewis CE, Torner J, Nevitt MC, Sack B, Felson DT. Meniscal tear in knees without surgery and the development of radiographic osteoarthritis among middle-aged and elderly persons: the multicenter osteoarthritis study. Arthritis Rheum. 2009;60(3):831–839. doi: 10.1002/art.24383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Houck Darby A., Kraeutler Matthew J., Belk John W., Frank Rachel M., McCarty Eric C., Bravman Jonathan T. Do Focal Chondral Defects of the Knee Increase the Risk for Progression to Osteoarthritis? A Review of the Literature. Orthopaedic Journal of Sports Medicine. 2018;6(10):232596711880193. doi: 10.1177/2325967118801931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Shelbourne KD, Gray T. Results of anterior cruciate ligament reconstruction based on meniscus and articular cartilage status at the time of surgery: five- to fifteen-year evaluations. Am J Sports Med. 2000;28(4):446–452. doi: 10.1177/03635465000280040201. [DOI] [PubMed] [Google Scholar]
- 64.Øiestad BE, Holm I, Aune AK, Gunderson R, Myklebust G, Engebretsen L, et al. Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: a prospective study with 10 to 15 years of follow-up. Am J Sports Med. 2010;38(11):2201–2210. doi: 10.1177/0363546510373876. [DOI] [PubMed] [Google Scholar]
- 65.Suter LG, Smith SR, Katz JN, Englund M, Hunter DJ, Frobell R, Losina E. Projecting lifetime risk of symptomatic knee osteoarthritis and total knee replacement in individuals sustaining a complete anterior cruciate ligament tear in early adulthood. Arthritis Care Res. 2017;69(2):201–208. doi: 10.1002/acr.22940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Jomha Nadr M., Borton David C., Clingeleffer Amanda J., Pinczewski Leo A. Long Term Osteoarthritic Changes in Anterior Cruciate Ligament Reconstructed Knees. Clinical Orthopaedics and Related Research. 1999;358:188–193. [PubMed] [Google Scholar]
- 67.Harris K, Driban JB, Sitler MR, Cattano NM, Hootman JM. Five-year clinical outcomes of a randomized trial of anterior cruciate ligament treatment strategies: an evidence-based practice paper. J Athl Train. 2015;50(1):110–112. doi: 10.4085/1062-6050-49.3.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sanders TL, Kremers HM, Bryan AJ, Fruth KM, Larson DR, Pareek A, et al. Is anterior cruciate ligament reconstruction effective in preventing secondary meniscal tears and osteoarthritis? Am J Sports Med. 2016;44(7):1699–1707. doi: 10.1177/0363546516634325. [DOI] [PubMed] [Google Scholar]
- 69.de Campos GC, Nery W, Teixeira PEP, Araujo PH, Alves W de M. Association between meniscal and chondral lesions and timing of anterior cruciate ligament reconstruction. Orthop J Sport Med. 2016;4(10). [DOI] [PMC free article] [PubMed]
- 70.Amano K, Li AK, Pedoia V, Koff MF, Krych AJ, Link TM, et al. Effects of surgical factors on cartilage can be detected using quantitative magnetic resonance imaging after anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45(5):1075–1084. doi: 10.1177/0363546516677794. [DOI] [PubMed] [Google Scholar]
- 71.Budny J, Fox J, Rauh M, Fineberg M. Emerging trends in anterior cruciate ligament reconstruction. J Knee Surg. 2017;30(1):63–69. doi: 10.1055/s-0036-1579788. [DOI] [PubMed] [Google Scholar]