Abstract
BACKGROUND:
Deep venous thrombosis (DVT) is a prevalent complication of orthopedic surgery. According in many studies. The incidence of DVT may be up to 50% if thromboprophylaxis is not available.
AIM:
The objective of this study was to check the degree of disease, clinical characteristics and analyzed factors in vulnerabilities with lower-limp DVT after orthopedic surgery in a Vietnam teaching hospital.
METHODS:
Orthopedic patients who met criteria were recruited at our hospital between August 2017 and June 2018. Ultrasound was used to discovering lower-limp DVT in pre-surgery and 7 days after surgery in all patients.
RESULTS:
The incidence of DVT after orthopedic surgery was 7.2%. Patients with older age (> 60) have a risk of 2 times higher of DVT after surgery than normal people (p < 0.05). The incidence of postoperative DVT was higher in immobile individuals > 72 hours (p < 0.05). Patients with prolonged surgical time (>120 minutes) had a higher risk of postoperative DVT than non-surgical patients’ surgery (p < 0.05).
CONCLUSIONS:
DVT remains a common complication following orthopedic surgery. Older age, immobility status, and surgical time have been found to be risky factors for the development of postoperative lower-limp DVT in orthopedic patients.
Keywords: Deep Venous Thrombosis, Orthopedic, Frequency, Risk factor
Introduction
Deep vein thrombosis (DVT) occurs when blood clots are formed and cause partial or complete blockage of the veins, most commonly the lower-limb veins Complications can include pulmonary embolism (PE), as a result of a blood clot moving to the lungs, and syndrome after thrombosis. In the United States, DVT and PE caused up to 600,000 hospitalizations a year, approximately 50,000 deaths from PE [1].
Orthopedic surgeries, such as total hip arthroplasty (THA) and full knee joint surgery, are favorable conditions for the formation and development of the DVT. According to current reports, in the absence of thromboprophylaxis, the vein method used to detect DVT occurs in up to 50% of orthopedic patients, and PE is cause of death of about 1.7% of patients experience THA and about 2% of patients experience TKA. Even with prophylaxis, the likelihood of DVT in orthopedic surgery is 27% [2].
However, according to the literature, the clinical symptoms of DVT is mostly atypical, only suggestive [3]. Nguyen Van Dung conducted a study of clinical characteristics of DVT and found that leg pain occurs in 45.9% of patient with thrombosis and 48.4% of patients without thrombosis, while other symptoms such as swelling, leg numbness, warmth or redness are detected in these two groups. These signs and symptoms are easily confusing with those appearing postoperatively [4]. Similarly, Ker-Kan Tan et al., implemented hospital-based case-control study and indicated that presenting signs/symptoms relating to DVT such as leg pain, warmth, erythema and fever were not significantly different between groups [5].
We conducted this research to evaluate the incidence rate, clinical characteristics and risk factors for lower-limb DVT in patients undergoing major lower limb orthopedic surgery in our teaching Bach Mai hospital in Vietnam.
Materials and Methods
Study subjects
Patient Selection
To be included in the study, patients had to be adult (≥ 18 year of age) and had undergone one of surgical procedures including total hip arthroplasty, knee arthroplasty or repair of femur fracture, were received preoperative anticoagulant therapy with low-molecular-weight-heparin or oral rivaroxaban, and have ≥ 3 days of hospital stay after surgery. Patients who have been previously diagnosed and treated for lower extremity DVT were excluded from the study, as were patients with neurological diseases who did not have ability to co-operate and provide accurate information. All the patients were notified of the investigational nature of the research, provide oral acceptance before registration on to the study.
Time and Location
The research was proced from August 2017 to June 2018 in Bach Mai Hospital, Hanoi, Vietnam.
Methodology
Study Design: Cross-sectional descriptive examination.
Sample size and sampling method
Sample size
Method:
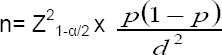
n: sample size for the study;
α: 95% confidence coefficient;
Z1-α/2= Zα/2 = 1,96;
p: incidence of DVT after orthopedic surgery, p = 0.4;
d: absolute error, d = 0.1;
The result of calculating the sample size is that n ≈ 92.2.
Therefore, the minimum sample size required for the study is 93 patients.
Sampling method: Intentional sampling method by selecting patient according to the selection criteria in the study until the sample size is sufficient
Study Process
All patients who satisfy the criteria of study and agreed to attend in the examination were interviewed and collected data (demographic information, clinical and subclinical characteristics, surgical methods, thrombo-prophylaxis regimen), taken a blood sample to perform D-dimer levels before and after 3 days of surgery. Simultaneously, a Duplex ultrasonography of the lower limb veins was also excecuted to confirm the presentation of thrombi prior to surgery, since patients diagnosed with pre-existent DVT would be excluded from the study. After 7 days or in case of clinically suspected VTE post-operatively, patients were clinically checked-up and experienced Duplex ultrasonography of lower limb veins and were assessed using Caprini score in order to determine the diagnosis of DVT. After hospital discharge, patients were conducted to account to the reseach center promptly if any symptoms and evidences of DVT occurred at home, and were asked to visit for re-examination after 1 month or immediately when symptoms occurred.
Statistical Analysis
Consecutive variables were precented as mean ± standard deviation or median [range: min-max]. Besides, we conducted Student t test or the Wilcoxon Rank Sum test to appreciate distinction in mean or medians, respectively. Categorical data were compared using the chi-square or Fisher exact tests. Multivariate logistic regression was performed to identify risk factors independently interconnected with occurrence of post-operative DVT. Odds ratio (OR) and 95% confidence interval (CI) were computed using logistic regression. The α level for statistical significance for all test was set at 0.05. All analyses were performed using SPSS 23.0 and STATA 12.0.
Results
From August 2017 to June 2018, we enrolled 97 orthopedic surgical patients who meet criteria to be included in the study at Bach Mai Hospital. Mean age of study population was 61.1 ± 16.3 years old, with the lowest age of 25 and the highest of 95 years old. The proportion of men and women was 47.4% and 52.6%, respectively. All patients in the study did receive thromboprophylaxis, mainly with Rivaroxaban 10 mg/day (82.5%) or Enoxaparin 40 mg/day (13.4%), for average of 10-14 days, and possibly up to 35 days after surgery [26]. During follow-up, four patients presented major bleeding complications during Enoxaparin therapy, and Rivaroxaban was used alternatively in the following days.
Seven patients developed lower-limb DVT after surgery, and were compared versus those who did not (non-DVT group: n = 90). Patients with DVT were older than those without DVT (65.3 ± 7.3 vs. 60.8 ± 16.8 years, respectively). DVT was detected in 71.4% of patients aged 60-74 years. The distinction was not statistically considerably (p > 0.05). There were no gender differences between two subgroups. The prevalence of lower-limb DVT was mainly in the two types of surgery: 12.9% for knee arthroplasty and 4.8% for hip arthroplasty. Regarding to the clinical presentation of DVT in orthopedic patients, the rate of leg pain, erythema, swelling and limb numbness were respectively 100%, 83.6%, 57.1% and 28.6% in DVT patients, higher than those of non-DVT group (Table 1).
Table 1.
Essential characteristics of orthopedic inmates
| Characteristics | DVT group (n = 7) | Non-DVT group (n = 90) | p value |
|---|---|---|---|
| Age | |||
| 18-40 | 0 | 13 (14.4%) | P > 0,05 |
| 41-60 | 2 (28.6%) | 27 (30.0%) | |
| 61-74 | 5 (71.4%) | 31 (34.4%) | |
| ≥75 | 0 | 19 (21.2%) | |
| Mean age X ± SD (Min-Max) | 65.3 ± 7.3 (55-74) | 60.8 ± 16.8 (25-95) | |
| Gender | |||
| Male | 3 (42.9%) | 43 (47.8%) | P > 0.05 |
| Female | 4 (56.1%) | 47 (52.2%) | |
| Surgical procedures | |||
| Total hip replacement | 3 (4.8%) | 59 (95.2%) | P > 0.05 |
| Repair of femur fracture | 0 | 3 (100%) | |
| Total knee replacement | 4 (12.9%) | 27 (87.1%) | |
| Acetabular labral tear surgery | 0 | 1 (100%) | |
| Symptoms | |||
| Pain in one leg | 7 (100%) | 67 (74.4%) | > 0.05 |
| Erythema | 5 (83.6%) | 35 (38.9%) | > 0,05 |
| Swelling | 4 (57.1%) | 46 (51.1%) | > 0.05 |
| Limb numbness | 2 (28.6%) | 11 (12.2%) | > 0.05 |
| D-dimer test (mg/l FEU) | |||
| Before surgery | 2.39 ± 2.52 | 1.15 ± 1.38 | < 0.05 |
| After surgery | 6.13 ± 7.38 | 2.64 ± 2.31 | < 0.05 |
Table 2 summarizes the result of logistic regression used to analyze the association between post-operative lower-limb DVT and causative factors including age over 60, gender, smoking status, history of diabetes, previous major surgery, blood transfusion, immobilization > 72 hours and operative duration. Our analysis revealed that older age (> 60), immobilization (> 72 hours), and prolonged surgery (operation time > 120 min) were significantly associated to the high risk of DVT (p < 0.05). Particularly, the rate of post-operative lower-limb DVT was significantly higher in patients who were immobilized for ≥ 72 hours (20%), compared to those who weren’t (2.8%). Immobilization increased the risk of DVT by 8.8 times in orthopedic surgical patients (95% CI, 1.6-48.5). Patients with prolonged surgical time (≥ 120 min) had elevated overall rate for lower-limb DVT and greater risk of post-operative deep venous thromboembolism (OR = 28.67; 95% CI, 4.7-173.7) compared with patients having less than 120 minutes of surgical time.
Table 2.
Risk factors of lower-limb DVT
| Risk factors | No. of patient with lower-limb DVT | Odd ratio | p value |
|---|---|---|---|
| Age > 60 | 5 (9.1%) | 2.0 (0.38-10.86) | < 0.05 |
| Female sex | 4 (7.8%) | 1.22 (0.26-5.8) | > 0.05 |
| Current smoker | 2 (12.5%) | 2.17 (0.4-12.0) | > 0.05 |
| Diabetes | 1 (9.1%) | 1.33 (0.1-12.3) | > 0.05 |
| Previous major surgery (1 month or more) | 2 (20.0%) | 4.1 (0.8-22.1) | > 0.05 |
| Blood transfusion | 4 (13.8%) | 3.5 (0.8-15.5) | > 0.05 |
| Immobilization > 72 hour | 5 (20.0%) | 8.8 (1.6-48.5) | < 0.05 |
| Operative time | 4 (50.0%) | 28.67 (4.7-173.7) | < 0.05 |
Discussion
Deep vein thrombosis is known to occur prevalently after surgery, particularly orthopedic surgery, and to be able result in PE, which can be fatal. Our study of 97 patients undergoing major orthopedic surgery reveals that the rate of DVT after orthopedic surgery was 7.2%. This finding is lower than the 40% found in the Vo Van Tam and Nguyen Vinh Thong’s study conducted in Cho Ray Hospital [6]. Moreover, Kim K et al reported 18%-24% incidence of deep vein thrombosis following total hip arthroplasty (THA) and an incidence of 20%-49% following total knee arthroplasty (TKA) [7]. Although these studies were similar in time and patient’s characteristics compared to our study, the patients of these studies did not receive pre-operative thromboprophylaxis while in our study it was provided to 100% of patients before surgery. Thus, the rates of DVT are higher than ours.
Regarding to the clinical characteristics of lower-limb DVT, no statistically considerably distinction was found between groups. The most found symptoms/signs were leg pain and erythema in DVT group. This suggests that these two symptoms may be indications that the patient may have had or be having lower-limb DVT. However, with the specificity of orthopedic surgery as the intervention in the limbs of the patient, so these symptoms can be confusing, difficult to identify. Author Nguyen Van Dung (2011) claimed that the clinical symptoms of lower-limb DVT are atypical, nonspecific and easy to confuse with other diseases [4]. Others such as swelling, numbness and paresthesia are somewhat related to the feeling of each patient, so there is a similarity between DVT and non-DVT patients.
Our study shows that preoperative and postoperative D-dimer test values were significantly higher in the DVT group than in the non-DVT group (p < 0.05). These values were also found similar after surgery. Si-dong Yang, et al., conducted study on D-dimer test and found the D-dimer in DVT group to be relatively greater than non-DVT group [8]. Hamidi S, et al., reported a difference in D-dimer levels after surgery between patients with and without DVT, with D-dimer cut-off point on day 3 post-operatively of 2.1 μg/mL for 100% sensitivity, 80.7% specificity and 100% negative diagnostic result [9]. Furthermore, Sudo A, et al., indicated the increase of D-dimer level statistically significant on day 4, 7, 10 and 14 after surgery, a value of 7.0 mg/L on day 4 is significant for the diagnosis of lower extremity DVT [10]. In case Duplex ultrasound images are negative, the addition of D-dimer test eliminates the risk of DVT and patient does not need to do second ultrasound test [11], [12]. Therefore, our findings are consistent with those of foreign authors.
Ascertaining the risk factor for progessive of DVT and PE is significant as this may help clinicians determine high risk patients and give them appropriate prophylaxis. In this study, we evaluate 8 factors for their role in causation or association with development of DVT after orthopedic surgery and found age over 60, immobility > hours and prolonged operative time (> 2 hours) to be significant risk factors.
Older age is commonly related to weak venous valve dinamic, vascular sclerosis and high blood viscousness. This factor associated with limited exercise after surgery, may result in lower limb DVT. In present research, age have been found to be significantly interconnected with an increase of venous thrombosis among orthopedic patients. Our result is consistent with that of Motohashi M which showed that age over 60 years significantly increased the risk of DVT by 3.91 times (p < 0.001) [13]. After surgery, patients often do not exercise in bed and spend a lot of time travelling on ambulant, thus they are at high baseline risk of venous thrombosis in the lower extremity. Our study confirms that postoperative immobilization over 72 hours was considerably interconnected with high risk of lower-limb DVT (OR = 8.8, p < 0.05). Our finding also accords with that of Bagiaria et al. [14]. In Virchow’s Triad describing the pathogenesis of venous thrombosis, one of the three factors are stasis of blood flow. Prolonged immobility can be conducive to this condition, leading to the genesis of blood clot in the lower-limb.
Table 2 shows that patients who had surgery time greater than 120 minutes increased the risk of DVT by 28.67-fold, which was statistically significant at p < 0.001. Bagiaria et al., suggested that a surgery performed for more than 2 hours will increase the risk of DVT by 4.318 times [14]. Besides, Kang J, et al., reported a 1.69 times higher risk in patient with prolonged operative time [15]. The finding of our study was surpassingly higher than those of the authors, perhaps because our sample size was 97 patients, which is much lower than that of Bagaria’s (147 patients) and Kang J’s (1025 patients). In an analysis of 611 patients who had undergone orthopedic surgery of lower extremities, Motohashi M et al. demonstrated that prolonged operation time (> 120 minute, OR = 4.52) was detected as factor that markedly impacted the occurrence of DVT in all patients. But in general, the more time the surgery take, the greater the risk for developing lower-limb DVT become [13].
In conclusion, DVT remains a common complication following orthopedic surgery. Our study conducted on 97 orthopedic surgical patients showed that the incidence of postoperative DVT was 7.2%. Common clinical symptoms are pain in one leg, swelling, paresthesia and skin color change. Old age, immobility status (> 72 hours) and prolonged operative time were associated with a higher risk of developing postoperative DVT after orthopedic surgery. Thus, plastic surgeons should carefully examine the risk factors of DVT before implementing major orthopedic surgeries and should remain aware of the likelihood of developing postoperative DVT in high-risk patients.
Acknowledgement
We would like to thank Bach Mai Hospital for providing favorable conditions to us to carry out this research. We are committed not to cause conflict of interests from research results. We would like to thank Ms. Hoang Thi Anh (Faculty of Biology, Hanoi National University of Education, Hanoi, Vietnam) checking and improving the English in the manuscript.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
Abbreviations: DVT: Deep vein thrombosis; PE: Pulmonary embolism; THA: Total hip arthroplasty; TKA: Total knee arthroplasty
Ethical Approval
This research was accepted by Ethical Review Board of Hanoi Medical University (Approval No. IRB 003121).
Informed Consent
Informed consents were collected from participating patient(s) for their anonymized information to be reported in the study.
References
- 1.Prevention of venous thrombosis and pulmonary embolism NIH Consensus Development. JAMA. 1986;256(6):744–9. https://doi.org/10.1001/jama.256.6.744 PMid:3723773. [PubMed] [Google Scholar]
- 2.Kim YH, Oh SH, Kim JS. Incidence and natural history of deep-vein thrombosis after total hip arthroplasty. A prospective and randomised clinical study. J Bone Joint Surg Br. 2003;85(5):661–5. https://doi.org/10.1302/0301-620X.85B5.14012 PMid:12892186. [PubMed] [Google Scholar]
- 3.CB M, et al. Risk factors for clinically relevant pulmonary embolism and deep venous thrombosis in patients undergoing primary hip or knee arthroplasty. Anesthesiology. 2003;99:552–60. doi: 10.1097/00000542-200309000-00009. https://doi.org/10.1097/00000542-200309000-00009 PMid:12960538. [DOI] [PubMed] [Google Scholar]
- 4.Dung NV. Evaluation of Wells scales and serum D-dimer levels in the diagnosis of deep vein thrombosis. Hanoi Medical University Hospital, Hanoi. 2011 [Google Scholar]
- 5.Tan KK, Koh WP, Chao AK. Risk factors and presentation of deep venous thrombosis among Asian patients:a hospital-based case-control study in Singapore. Ann Vasc Surg. 2007;21(4):490–5. doi: 10.1016/j.avsg.2006.06.008. https://doi.org/10.1016/j.avsg.2006.06.008 PMid:17628265. [DOI] [PubMed] [Google Scholar]
- 6.Tam VV, Thong NV. Investigation of the frequency of deep vein thrombosis in the lower extremities in patients undergoing knee or hip replacement surgery. Ho Chi Minh Medical Journal. 2014;18(2):250–256. [Google Scholar]
- 7.Kim KI, et al. Thromboprophylaxis for Deep Vein Thrombosis and Pulmonary Embolism after Total Joint Arthroplasty in a Low Incidence Population. Knee Surg Relat Res. 2013;25(2):43–53. doi: 10.5792/ksrr.2013.25.2.43. https://doi.org/10.5792/ksrr.2013.25.2.43 PMid:23741698 PMCid:PMC3671115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang SD, Liu H, Sun YP, Yang DL, Shen Y, Feng SQ, Zhao FD, Ding WY. Prevalence and risk factors of deep vein thrombosis in patients after spine surgery:a retrospective case-cohort study. Scientific reports. 2015;5:11834. doi: 10.1038/srep11834. https://doi.org/10.1038/srep11834 PMid:26135271 PMCid:PMC448∦. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hamidi S, Riazi M. Cutoff Values of Plasma D-Dimer Level in Patients with Diagnosis of the Venous Thromboembolism after Elective Spinal Surgery. Asian Spine J. 2015;9(2):232–238. doi: 10.4184/asj.2015.9.2.232. https://doi.org/10.4184/asj.2015.9.2.232 PMid:25901235 PMCid:PMC4404538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sudo A, Wada H, Nobori T, Yamada N, Ito M, Niimi R, Hasegawa M, Suzuki K, Uchida A. Cut-off values of D-dimer and soluble fibrin for prediction of deep vein thrombosis after orthopaedic surgery. Int J Hematol. 2009;89(5):572–576. doi: 10.1007/s12185-009-0323-4. https://doi.org/10.1007/s12185-009-0323-4 PMid:19430861. [DOI] [PubMed] [Google Scholar]
- 11.SA L. Approach to the diagnosis and therapy of lower extremity deep vein thrombosis. 2014. www.Uptodate.com 2014 .
- 12.Working GJJ. Guidelines for the diagnosis, treatment and prevention of pulmonary thromboembolism and deep vein thrombosis. Circ J. 2011;75(5):1258–1281. doi: 10.1253/circj.cj-88-0010. https://doi.org/10.1253/circj.CJ-88-0010 PMid:21441695. [DOI] [PubMed] [Google Scholar]
- 13.Motohashi M, et al. Deep vein thrombosis in orthopedic surgery of the lower extremities. Ann Vasc Dis. 2012;5(3):328–333. doi: 10.3400/avd.oa.12.00049. https://doi.org/10.3400/avd.oa.12.00049 PMid:23555532 PMCid:PMC3595850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bagaria V. Incidence and risk factors for development of venous thromboembolism in Indian patients undergoing major orthopaedic surgery:results of a prospective study. Postgrad Med J. 2006;82(964):136–139. doi: 10.1136/pgmj.2005.034512. https://doi.org/10.1136/pgmj.2005.034512 PMid:16461477 PMCid:PMC2596707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kang J, Jiang X, Wu B. Analysis of Risk Factors for Lower-limb Deep Venous Thrombosis in Old Patients after Knee Arthroplasty. Chin Med J. 2015;128(10):1358–62. doi: 10.4103/0366-6999.156782. https://doi.org/10.4103/0366-6999.156782 PMid:25963358 PMCid:PMC4830317. [DOI] [PMC free article] [PubMed] [Google Scholar]


