Abstract
BACKGROUND:
Keratoconus is an ectatic corneal disorder that can impair the visual acuity. Up to now, penetrating keratoplasty (PK) remains the most common surgical procedure to treat severe keratoconus. In Vietnam, most keratoconus patients come to visit doctor at severe stage and were treated by PK, so we conduct this study.
AIM:
To evaluate the results of PK for keratoconus in Vietnamese patients.
METHODS:
This was a retrospective study of 31 eyes with keratoconus who underwent PK in VNIO from January 2005 to December 2014.
RESULTS:
The average visual acuity was 0.86 ± 0.37 logMAR (20/145). In the group of patients without amblyopia, best spectacle-corrected visual acuity of 20/60 or better was recorded in 75.9% of eyes and 93.1% of eyes achieved a best corrected visual acuity with hard contact lenses of 20/40 or better. Mean postoperative corneal power was 43.8 ± 4.5D. Mean corneal astigmatism was 5.9 ± 2.7D. 94.6% of grafts remained clear. Posterior subcapsular cataract developed in 22.6% of eyes. Graft rejection was recognized in 12.9% of eyes.
CONCLUSION:
PK is an effective procedure with high rate of graft survival for keratoconus patients. However, patients should be aware of the necessary of optical correction to gain the best VA after surgery.
Keywords: Keratoconus, Penetrating keratoplasty, Donor-recipient disparity
Introduction
Keratoconus is a noninflammatory ectatic corneal disorder characterized by localized cornical protrusion owing to thinning of the corneal stroma. This condition can lead to high myopia, irregular astigmatism, and impairment of visual acuity (VA) [1]. The treatment of keratoconus depends on its severity, including spectacle, contact lens, intracorneal rings, collagen cross-linking and keratoplasty [2]. In recent years, deep anterior lamellar keratoplasty (DALK) has been selected to treat this disease as an alternative to PK by some surgeons [3], [4]. However, DALK is a difficult and long-time surgery, especially in patients with acute hydrops or corneal scar. Therefore, PK remains the most popular surgical procedure in the severe stage.
About 10-20% of keratoconus patients require PK for corneal scar, contact lens intolerance, or unsatisfaction with best-corrected visual acuity (BCVA) [1], [5]. Previous studies have noted that keratoconus is one of the common indications for corneal transplantation all over the world. The successful rate of PK for keratoconus is higher than other diseases. After 5 to 12 years, the graft survival rate is more than 90% [6], [7], [8].
In Vietnam, keratoconus is a rare disease and was well described in 2014 [9]. PK has been performed to treat patients with advanced keratoconus over the past fifteen years. This condition accounts for 1.4% of all PK operations [10]. This study was conducted to evaluate the outcomes of PK in Vietnamese patients with keratoconus.
Materials and Methods
All keratoconus patients who underwent PK at Vietnam National Institute of Ophthalmology (VNIO) between January 2005 and December 2014 were enrolled in this retrospective study.
PK surgeries were done under general anaesthesia. We used hand-held trephine to punch in the corneas. The host diameter ranged from 7.0 to 8.0 mm, and the donor diameter was same-size or 0.5 mm larger. The PK technique was 16-bite interrupted suture or a combined 8-bite interrupted suture and a 16-bite running suture. Postoperative treatment consisted of topical antibiotic and steroids 4 times per day. Steroids were tapered after one month and discontinued after 1 year.
Medical records were reviewed for demographic data, pre-and postoperative VA, keratometry, ocular conditions and general diseases associated with keratoconus, surgical technique, intraoperative and postporative complications such as graft rejection episodes, infection, trauma, and the requirement of glaucoma surgery or cataract surgery. After that, patients were recalled for the last follow-up examination. Patients who did not come for the last examination were excluded.
At the last follow-up examination, VA, BSCVA, and BCVA with hard contact lens were noted. The Icare tonometer was utilized to mesure the intraocular pressure. Patients were examined on the slit lamp to evaluate the graft clarity and other ocular conditions. Corneal topography was measured with the OPD-Scan III topographer. Two topographic indices were calculated and registered: average K-value and corneal astigmatism.
Statistical analysis
SPSS 16.0 was utilized to analysed the data. Chi-square test was applied to compare the difference of grouping variables. Fisher’s exact test was the alternative algorithm to Chi-square test when the number of data was small. We used t-test to compare continous variables.
Results
From January 2005 to December 2014, there were 31 eyes of 28 keratoconus patients underwent PK. Mean age at the time of surgery was 20.4 ± 8.4 (range 8-58 yrs). There were 24 males (85.7%) and 4 females (14.3%) (p < 0.001). Preoperative VA of all patients was less than 20/200. Of all 31 eyes, 28 eyes (90.3%) had the VA less than count finger (CF) 3 m. Indications for PK involved corneal scar (54.8%), corneal hydrops (25.8%), unsatisfactory best corrected visual acuity (19.4%).
Recipient trephine size ranged from 7.0 to 8.0 mm. The most common host diameter was 7.0 mm (15 eyes). Donor-recipient disparity was 0.5 mm in 17 eyes (54,8%) and 0 mm in 14 eyes (45.2%). Suture technique was interrupted sutures in 28 eyes (90.3%) and combined sutures in 3 eyes (9.7%).
Visual Outcome
Of all 31 eyes, 2 eyes had amblyopia with the BCVA less than 20/200. The first patient was diagnosed keratoconus at the age of 2 years and underwent PK at 8 years old. His post-op BCVA was 20/160. The second patient had congenital cataract combined with nystagmus. He had undergone ECCE combined with IOL implantation 6 years before PK. At the last examination, the VA was CF 2.5 m and didn’t improve with pinhole. In the group of 29 eyes without amblyopia, mean UCVA and BSCVA at the last examination was 0.86 ± 0.37 logMAR (20/145) and 0.43 ± 0.18 logMAR (20/54) (p = 0.024), respectively. Hard contact lenses were fitted in 27 eyes, and the average BCVA was 0.09 ± 0.1 (20/25).
Table 1 show that the majority of patients had UCVA ranged from 20/200 to 20/60 (51.7%). Mean BSCVA at the final follow-up was at least 20/60 in 75.9% of the group without amblyopia. BCVA with hard contact lens of 20/40 or better was recorded in 27 eyes (93.1%) of this group including 14 eyes had BCVA of 20/25 or better.
Table 1.
Visual outcome at the last visit
| VA | UCVA | BSCVA | BCVA with HCL* | |
|---|---|---|---|---|
| < CF 3m | n | 2 | 0 | 0 |
| % | 6.9 | 0 | 0 | |
| CF 3m - < 20/200 | n | 5 | 0 | 0 |
| % | 17.2 | 0 | 0 | |
| 20/200 - < 20/60 | n | 15 | 7 | 0 |
| % | 51.7 | 24.1 | 0 | |
| 20/60 - < 20/40 | n | 7 | 12 | 0 |
| % | 24.1 | 41.4 | 0 | |
| ≥ 20/40 | n | 0 | 10 | 27 |
| % | 0 | 34.5 | 93.1 | |
| Total | n | 29 | 29 | 29 |
BCVA with HCL was not performed in 2 eyes of the non-amblyopia group, including 1 eye had corneal scar and 1 eye was being performed suture removal.
Refractive outcome
Corneal topography could not be measured in 2 eyes due to nystagmus and corneal scar. Mean keratometry of the remaining 29 eyes at the last visit was 43.8 ± 4.5D (range 32-52.25D). Of 29 eyes, 51.7% (15 eyes) had the keratometry in the normal range (40-44D). Corneal astigmatism was high with the average result of 5.9D (SD 2.7D, range 1-11.5D), and overall, 75.9% (22 eyes) had the corneal astigmatism more than 4D. There were 2 eyes had corneal astigmatism more than 10D. There were only 3 eyes (10.3%) had corneal astigmatism less than 2D.
Graft survival outcome
The rate of clear graft after PK was very high. A total of 94.6% (29 of 31 grafts) of the examined eyes had a clear graft. 1 eye had opaque graft after PK 43 months. 1 eye had corneal scar due to keratitis 1 month postoperatively.
Figure 1.
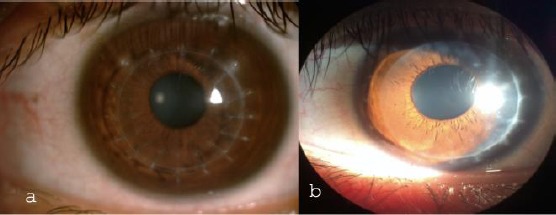
Clear grafts after PK (a.8.8yrs; b.27months)
Complications
Graft rejection was recorded in 4 eyes (12.9%). However, there was no case of graft rejection cause graft failure. Secondary glaucoma occurred in 2 eyes (6.5%) due to prolonged topical corticosteroid therapy to treat graft rejection.
Table 2.
Complications after PK
| Complication | n | Percentage (%) |
|---|---|---|
| Loose suture | 9 | 29.0 |
| Corneal neovascularization | 8 | 25.8 |
| Posterior subcapsular cataract | 7 | 22.6 |
| Graft rejection | 4 | 12.9 |
| Secondary glaucoma | 2 | 6.5 |
| Keratitis | 1 | 3.2 |
Of the 2 glaucoma eyes, 1 eye required trabeculetomy 10 months after PK because the IOP had not been controlled by 4 types of topical antiglaucoma eyedrops. There was 1 eye developed bacterial keratitis on the graft 1 month postoperatively, leading to graft failure due to corneal scar.
Figure 2.
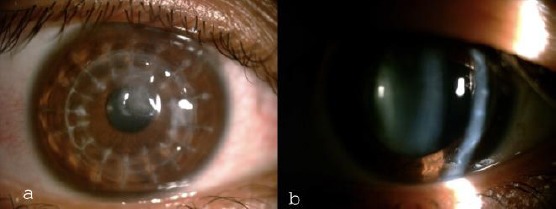
Complications after PK; A) Corneal scar; B) Posterior subcapsular cataract
Discussion
Keratoconus is a progressive disease characterized by paracentral or central thinning, and ectasia of the cornea. This disease often appears in the second decade of life and progresses at a variable rate. It causes severe myopia and irregular astigmatism. Keratoconus patients who underwent keratoplasty are very young because this disease often occurs at puberty.
In our study, most patients were male, which is similar to the results of some other authors [11], [12], [13]. The recent studies indicate that keratoconus is more common in men than women due to the combination of this disease and vernal conjunctivitis, a common disease in men [14]. Furthermore, this disease also progresses faster in men [15]. These findings contribute to explain that male patients tend to have to undergo keratoplasty than women.
Corneal scar was the leading indication for keratoplasty in our study, which account for the proportion of 54.8%. However, the main indication of surgery in Lim’s study was contact lens intolerance (51.6%) [8]. The indications for PK in patients with keratoconus vary greatly in different studies. In Vietnam, almost keratoconus patients were discovered in severe stage, and most of them have corneal scars [9]. Therefore, they could not be treated by hard contact lens, collagen cross-linking or intrastromal ring implantation. Penetrating keratoplasty was a good treatment for them.
Postoperative VA is the most important criteria when assessing the success of PK in terms of eye function. Before surgery, almost patients had VA less than CF 1 m. The average VA was 1.94 ± 0.14 logMAR. Postoperatively, the patients’ VA was improved significantly. The average UCVA was 0.86 ± 0.37 logMAR (20/145). The BCVA with hard contact lens of 29 eyes without amblyopia in our study was 20/27. This result is similar to the results of previous studies, with the BCVA ranged from 20/25 to 20/32 [7], [8], [11], [13].
For patients with PK, postoperative corneal astigmatism is still a big problem to overcome. Although the postoperative VA is improved significantly, most patients need to wear glasses or hard contact lens to gain the best VA. Wearing a hard contact lens is a non-surgical method, which is often selected to help patients achieve good VA after keratoplasty. It helps to correct corneal astigmatism and refractive deflection. In our study, the BSCVA of 22 non-amblyopia eyes (75.9%) was at least 20/60. 93.1% (27 eyes) of the non-amblyopia group had the BCVA of 20/40 or better with hard contact lens, including 14 eyes had BCVA of 20/25 or better.
Preoperative corneal refraction could not be measured in 26 eyes due to corneal scars, corneal hydrops and over-refraction. After surgery, there were 29 eyes which could be measured corneal topography with the average keratometry of 43.8 ± 4.5 D (range 32-52.25 D). Similar results were found in some previous studies [11], [16]. We could not measure topography in one eye with nystagmus and one eye with corneal scar.
With an average postoperative follow-up of 49.5 months, the rate of clear grafts was 94.6%. PK remains the main surgical procedure to treat severe keratoconus. The result of the other studies has shown that this is a high successful treatment method with the rate of clear grafts is about 95% after 2-5 years [8], [11], [17]. Although the cause of graft failure varies in different studies, the overall survival rate of the graft is still very high because the surgery is performed on the eye without inflammation and neo-vessel. In our study, the rate of graft rejection was 12.9% (4 eyes). Some studies of other authors shown the same result, which had the rate of graft rejection ranging from 4.3-31% [6], [18], [19], [20]. However, all cases of graft rejection were detected and treated promptly with topical and oral corticosteroids, so none of them led to graft failure.
In conclusion, keratoconus is a rare corneal degeneration that causes severe visual impairment. It usually occurs in young patients. In the severe stage, patients with keratoconus will require keratoplasty. PK is indicated for not only optical purpose for restoring VA, but also tectonic purpose for restoring the corneal integrity in terms of corneal thickness and shape. Patients with keratoconus can achieve good VA and a high rate of survival graft postoperatively. We propose that PK should be indicated in keratoconus patients with corneal scars. In some developing countries where advanced techniques as DALK or intracorneal ring implantation are not available, PK also should be considered in patients who have poor vision with spectacles or contact lens intolerance. However, some patients need to wear spectacles or hard contact lens to gain the best VA after PK.
Acknowledgement
We would like to acknowledge the support of all colleagues from Cornea Department and other colleagues from Vietnam National Institute of Ophthalmology.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
Ethics in Research
Research subjects voluntarily participate in the research, patients’ information is confidentiality. Research is only contributed to the vision of patients. Research subjects have the right to end the study at any time.
Informed Consent
All patients agreed and signed an informed consent form before surgeries.
References
- 1.Rabinowitz YS. Keratoconus. Survey of Ophthalmology. 1998;42(4):297–319. doi: 10.1016/s0039-6257(97)00119-7. https://doi.org/10.1016/S0039-6257(97)00119-7. [DOI] [PubMed] [Google Scholar]
- 2.Vazirani J, Basu S. Keratoconus:current perspective. Clinical Ophthalmology. 2013;7:2019–30. doi: 10.2147/OPTH.S50119. https://doi.org/10.2147/OPTH.S50119 PMid:24143069 PMCid:PMC3798205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kubaloglu A, Sari ES, Unal M. Long-term results of deep anterior lamellar keratoplasty for the treatment of keratoconus. Am J Ophathalmol. 2011;151(5):760–767. doi: 10.1016/j.ajo.2010.11.020. https://doi.org/10.1016/j.ajo.2010.11.020 PMid:21333267. [DOI] [PubMed] [Google Scholar]
- 4.MacIntyre R, et al. Long-term outcomes of deep anterior lamellar keratoplasty versus penetrating keratoplasty in Australian keratoconus patients. Cornea. 2014;33(1):6–9. doi: 10.1097/ICO.0b013e3182a9fbfd. https://doi.org/10.1097/ICO.0b013e3182a9fbfd PMid:24270676. [DOI] [PubMed] [Google Scholar]
- 5.Lass JH, et al. Clinical management of keratoconus A multicenter analysis. Ophthalmology. 1990;97(4):433–45. doi: 10.1016/s0161-6420(90)32569-1. https://doi.org/10.1016/S0161-6420(90)32569-1. [DOI] [PubMed] [Google Scholar]
- 6.Niziol LM, et al. Long-term outcomes in patients who received a corneal graft for keratoconus between 1980 and 1986. Am J Ophathalmol. 2013;155(2):213–219. doi: 10.1016/j.ajo.2012.08.001. https://doi.org/10.1016/j.ajo.2012.08.001 PMid:23111176. [DOI] [PubMed] [Google Scholar]
- 7.Al-Mohaimeed MM. Penetrating Keratoplasty for Keratoconua:Visual and Graft Survival Outcomes. International Journal of Health Sciences. 2013;7(1):58–63. doi: 10.12816/0006023. https://doi.org/10.12816/0006023 PMid:23559907 PMCid:PMC3612418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lim L, Pesudovs K, Coster DJ. Penetrating keratoplasty for keratoconus:visual outcome and success. Ophthalmology. 2000;107(6):1125–31. doi: 10.1016/s0161-6420(00)00112-3. https://doi.org/10.1016/S0161-6420(00)00112-3. [DOI] [PubMed] [Google Scholar]
- 9.LêXuân, Cung T.K.M.H. Phạm Ngọc Đông,, Đặc âm lâm sàng bệnh giác mạc hình chóp. Tạp chíNghiên cứu Y học. 2014;88(3):49–54. [Google Scholar]
- 10.Phạm Ngọc Đông T.N.H., LêXuân Cung. Đặc lâm bệnh nhân được ghép giác mạc tại Bệnh viện Mắt Trung uong trong giai đoạn 2002-2011. Tạp chíNghiên c?u Y học. 2013;85(5):24–30. [Google Scholar]
- 11.Javadi MA, et al. Outcomes of penetrating keratoplasty in keratoconus. Cornea. 2005;24(8):941–6. doi: 10.1097/01.ico.0000159730.45177.cd. https://doi.org/10.1097/01.ico.0000159730.45177.cd PMid:16227837. [DOI] [PubMed] [Google Scholar]
- 12.Sharif KW, Casey TA. Penetrating keratoplasty for keratoconus:complications and long-term success. Br J Ophthalmol. 1991;75(3):142–6. doi: 10.1136/bjo.75.3.142. https://doi.org/10.1136/bjo.75.3.142 PMid:1826453 PMCid:PMC1042291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brierly SC, Izquierdo LJ, Mannis MJ. Penetrating keratoplasty for keratoconus. Cornea. 2000;19(3):329–32. doi: 10.1097/00003226-200005000-00014. https://doi.org/10.1097/00003226-200005000-00014 PMid:10832693. [DOI] [PubMed] [Google Scholar]
- 14.Abu Ameerh MA, Al Refai RM, Al Bdour MD. Keratoconus patients at Jordan University Hospital:a descriptive study. Clin Ophthalmol. 2012;6:1895–9. doi: 10.2147/OPTH.S38287. https://doi.org/10.2147/OPTH.S38287 PMid:23204831 PMCid:PMC350∧. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fan Gaskin, et al. The Auckland keratoconus study:Identifying predictors of acute corneal hydrops in keratoconus. Clinical and Experimental Optometry. 2013;96(2):208–213. doi: 10.1111/cxo.12048. https://doi.org/10.1111/cxo.12048 PMid:23432147. [DOI] [PubMed] [Google Scholar]
- 16.Troutman Richard C, Lawless Michael A. Penetrating Keratoplasty for Keratoconus. Cornea. 1987;6(4):298–305. doi: 10.1097/00003226-198706040-00013. https://doi.org/10.1097/00003226-19∂040-00013 PMid:3319412. [DOI] [PubMed] [Google Scholar]
- 17.Pramanik S, et al. Extended long-term outcomes of penetrating keratoplasty for keratoconus. Ophthalmology. 2006;113(9):1633–8. doi: 10.1016/j.ophtha.2006.02.058. https://doi.org/10.1016/j.ophtha.2006.02.058 PMid:16828503. [DOI] [PubMed] [Google Scholar]
- 18.Olson RJ, et al. Penetrating keratoplasty for keratoconus:a long-term review of result and complications. J Cataract Ref Surg. 2000;26:987–91. doi: 10.1016/s0886-3350(00)00430-2. https://doi.org/10.1016/S0886-3350(00)00430-2. [DOI] [PubMed] [Google Scholar]
- 19.Fukuoka S, et al. Extended long-term results of penetrating keratoplasty for keratoconus. Cornea. 2010;29(5):528–30. doi: 10.1097/ICO.0b013e3181c29705. https://doi.org/10.1097/ICO.0b013e3181c29705 PMid:20299971. [DOI] [PubMed] [Google Scholar]
- 20.Duman F, et al. Indications and Outcomes of Corneal transplantation in Geriatric Patients. Am J Ophathalmol. 2013;156(3):600–607. doi: 10.1016/j.ajo.2013.04.034. https://doi.org/10.1016/j.ajo.2013.04.034 PMid:23769195. [DOI] [PubMed] [Google Scholar]


