Abstract
Sex development is a very complex biological event that requires the concerted collaboration of a large network of genes in a spatial and temporal correct fashion. In the past, much has been learned about human sex development from monogenic disorders/differences of sex development (DSD), but the broad spectrum of phenotypes in numerous DSD individuals remains a conundrum. Currently, the genetic cause of less than 50% of DSD individuals has been solved and oligogenic disease has been proposed. In recent years, multiple genetic hits have been found in individuals with DSD thanks to high throughput sequencing. Our group has been searching for additional genetic hits explaining the phenotypic variability over the past years in two cohorts of patients: 46,XY DSD patients carriers of NR5A1 variants and 46,XY DSD and 46,XX DSD with MAMLD1 variants. In both cohorts, our results suggest that the broad phenotypes may be explained by oligogenic origin, in which multiple hits may contribute to a DSD phenotype, unique to each individual. A search for an underlying network of the identified genes also revealed that a considerable number of these genes showed interactions, suggesting that genetic variations in these genes may affect sex development in concert.
Keywords: differences of sex development; DSD; oligogenicity; oligogenic disease; 46,XY DSD; 46,XX DSD; hypospadias; high throughput sequencing techniques; HTS
1. Introduction
Sex development is a very complex biological event that requires the concerted collaboration of a large network of genes in a spatial and temporal correct fashion [1]. In the past, much has been learned about human sex development from monogenic disorders/differences of sex development (DSD), but the broad spectrum of phenotypes in numerous DSD individuals remains a conundrum. Currently, the genetic cause of less than 50% of DSD individuals has been solved [2,3]. Oligogenic disease has been proposed. In fact, multiple genetic hits, which might not be deleterious by themselves, have been found in individuals with DSD [4,5,6,7,8,9,10,11,12,13,14].
Oligogenic inheritance is also currently discovered for several other disorders of the endocrine systems. For instance, in congenital hypogonadotropic hypogonadism (CHH) more than 25 causative genes are now considered to explain around 50% of the cases, and in at least 20% of cases disease-causing variants in two or more genes have been identified [15,16,17,18,19,20,21]. Similarly, in congenital hypothyroidism digenic [22,23] and polygenic [24] candidate-gene variants have been associated with the phenotypes [25].
2. Monogenic Inheritance in Humans with DSD
In humans, the DSD phenotypes manifesting discordances among sex chromosomes, gonadal and/or genital development are classified into three groups, namely sex chromosome DSD, 46,XX DSD or 46,XY DSD [26]. Additionally, for each of the 46,XX and 46,XY DSD groups, multiple gene and corresponding protein defects have been characterized. Animal models with the corresponding gene defects have generally been able to reproduce the human phenotype. Monogenic causes for both 46,XX and 46,XY DSD include genes regulating gonadal development, gonadal and/or adrenal steroidogenesis, genital ducts’ development, and target-cell responsiveness [2,3,27,28]. Clinical and biochemical phenotypes of DSD due to genetic defects, causing (a) a complete loss of protein function resulting in complete gonadal dysgenesis (CGD), (b) classical forms of defects of steroidogenesis (both gonadal and/or adrenal), and (c) hormone resistance, mostly relate directly to the underlying genetic defect, which is then typically monogenetic. Whenever possible, genetic family studies will confirm this type of inheritance.
Defects in genes regulating gonadal development and causing gonadal dysgenesis, either complete or partial, or gonadal sex reversal include a large groups of genes in 46,XY DSD (e.g., ARX, ATRX, CBX2, DAX1, DHH, DMRT1, EMX2, ESR2, FGFR2, GATA4, HHAT, MAP3K1, NR5A1, SOX9, SRY, TSPYL1, WNT4, WT1, ZFPM2, and ZNRF3) as well as in 46,XX DSD (e.g., BMP15, FGF9, FOXL2, NR2F2, NR5A1, NUP107, RSPO1, SOX3, SOX9, SOX10, SRY, and WNT4) [3,28]. Gene defects of steroidogenesis causing DSD include AKR1C2, AKR1C4, CYB5A, CYP11A1, CYP11B1, CYP17A1, CYP19A1, CYP21A2, DHCR7, HSD3B2, HSD17B3, POR, SRD5A2, and STAR [3,28]. Gene defects affecting gonadal ducts’ development comprise AMH in 46,XY and HOXA13 in 46,XX DSD [3,28]. Finally, hormone resistance syndromes causing monogenic forms of DSD are due to defects in genes AMHR, AR, ESR1, and LHCGR [3,28].
3. Digenic and Combined DSDs Described by Karyotyping and Single Candidate Gene Analyses
Patients carrying a digenic or combined DSD disease have been described even before the era of high throughput sequencing (HTS), when either the phenotype suggested the involvement of more than one gene defect or, incidentally, when an abnormal sex-chromosome karyotype is combined with an another gene defect [29,30,31,32,33,34,35].
Androgen receptor gene (AR) defects have occasionally been described in patients with a complete or partial androgen insensitivity syndrome (CAIS or PAIS) in whom sex chromosome analysis revealed a 47,XXY karyotype corresponding to a Klinefelter syndrome [29,30,31,32]. Similarly, a patient with a clinical and molecular diagnosis of familial male-limited precocious puberty due to an activating LHCGR mutation was demonstrated to have a 47,XXY karyotype upon detection of abnormally increased gonadotropin levels [33].
A 46,XY female DSD patient has been reported to combine AR and POR gene mutations causing a PAIS phenotype at birth, while clinical and biochemical phenotype at adrenarche suggested typical steroid anomalies of POR deficiency [34].
An adult 46,XY female DSD patient with primary amenorrhea, gonadal dysgenesis, bilateral gonadoblastoma, and dysgerminoma was first found to carry a missense SRY mutation, but later developed progressive focal segmental glomerular sclerosis and kidney failure. WT1 gene analysis revealed an intron 9 splice-site mutation and confirmed Frasier syndrome [35].
4. Oligogenic DSDs Described by High Throughput Sequencing (HTS)
In the past decade, high throughput sequencing (HTS) has changed the genetic approach in research and diagnostics. Whole-exome sequencing (WES) has led to the discovery of many new genes and has given insight into complex traits [36,37,38]. In addition, the HTS approach is discovering that some patients carry variants in more than one gene that may contribute to their phenotype.
Oligogenic DSD origin has been revealed either as a result of HTS directly or in a second approach, when the first candidate gene detected seemed not sufficient to explain the phenotype. Several recent studies demonstrate that many patients carry a gene variant likely responsible for the phenotype together with other variants in known or new candidate genes for DSD [4,5,6,7,8,9,10,11,12,13,14].
4.1. Digenic and Oligogenic Origin of DSD Revealed by HTS
In sex development, digenic inheritance has recently been suggested by WES analysis in a 46,XY DSD patient with gonadal dysgenesis (NR5A1 and MAP3K1 variants) [7] and in a family with a 46,XY DSD male (NR5A1 variant) and 46,XY DSD female (NR5A1 and TBX2 variants) [8] (Table 1).
Table 1.
Oligogenic disorders/differences of sex development (DSDs) described by high throughput sequencing (HTS) techniques.
| First Gene | Other Genes | Zygosity | Variant Classification | Patient’s Phenotype | References | Method |
|---|---|---|---|---|---|---|
| NR5A1 | MAP3K1 | het/het | LP*/B | 46,XY DSD GD | Mazen et al., 2016 [7] | WES |
| NR5A1 | TBX2 | het/het | P/P | 46,XY DSD complete GD | Werner et al., 2017 [8] | WES |
| AR | HOXB6, MAMLD1 | hemi/het/hemi | P/P/LB* | 46,XY DSD | Kon et al., 2015 [4] | Gene panel |
| HSD3B2 | SRD5A2 | homo/het | P/P | 46,XY DSD | Kon et al., 2015 [4] | Gene panel |
| AR | SRD5A2 | hemi/homo | P/P | 46,XY DSD | Eggers et al., 2016 [5] | Gene panel |
| AR | HSD17B3, SOX9 | hemi/homo/het | P/P/VUS | 46,XY DSD | Eggers et al., 2016 [5] | Gene panel |
| AR | NR5A1, FGFR2 | hemi/het/het | P/LP/VUS | 46,XY DSD | Eggers et al., 2016 [5] | Gene panel |
| AR | ZFPM2 | hemi/het | LP/P | 46,XY DSD | Eggers et al., 2016 [5] | Gene panel |
| AR | WDR11 | hemi/het | P/VUS | 46,XY DSD | Eggers et al., 2016 [5] | Gene panel |
| MAP3K1 | WT1 | het/het | LP/VUS | 46,XY DSD | Eggers et al., 2016 [5] | Gene panel |
| MAP3K1 | WDR11 | het/het | LP/VUS | 46,XY DSD | Eggers et al., 2016 [5] | Gene panel |
| MAP3K1 | LHCGR | het/homo | VUS/VUS | 46,XY DSD | Eggers et al., 2016 [5] | Gene panel |
| ZFPM2 | MAP3K1 | 2xhet/het | LP/LP/VUS | 46,XY DSD | Eggers et al., 2016 [5] | Gene panel |
| NR5A1 | ZFPM2 | het/het | P/VUS | 46,XY DSD | Eggers et al., 2016 [5]; Robevska et al., 2018 [9] | Gene panel |
| ZFPM2 | GATA4 | het/het | LP/VUS | 46,XY DSD | Eggers et al., 2016 [5] | Gene panel |
| HSD3B2 | GNRHR | homo/homo | P/P | 46,XY DSD | Eggers et al., 2016 [5] | Gene panel |
| CHD7 | DHH | het/het | VUS/VUS | 46,XY DSD | Eggers et al., 2016 [5] | Gene panel |
| NR5A1 | SRD5A2 | het/het | P/P | 46,XY DSD | Robevska et al., 2018 [9] | Gene panel |
| AR | SOX9, POR | hemi/het/het | P/VUS/VUS | 46,XY DSD | Kolesinska et al., 2018 [10] | Gene panel |
| AR | CBX2 | hemi/het | VUS/VUS | 46,XY DSD | Kolesinska et al., 2018 [10] | Gene panel |
| AR | DMRT1 | hemi/het | VUS/VUS | 46,XY DSD | Kolesinska et al., 2018 [10] | Gene panel |
| AR | POR | hemi/het | P/VUS | 46,XY DSD | Kolesinska et al., 2018 [10] | Gene panel |
| AR | DHCR7 | hemi/het | P/VUS | 46,XY DSD | Kolesinska et al., 2018 [10] | Gene panel |
| HSD17B3 | CYP17A1 | comp het/het | P/P/VUS | 46,XY DSD | Kolesinska et al., 2018 [10] | Gene panel |
| HOXA13 | ARX | het/hemi | LP/VUS | 46,XY DSD | Kolesinska et al., 2018 [10] | Gene panel |
| AKR1C4 | AMH | het/het | VUS/VUS | 46,XY DSD | Kolesinska et al., 2018 [10] | Gene panel |
| GATA4 | LHCGR | het/het | VUS*/P | 46,XY DSD | Martinez de LaPiscina et al., 2018 [11] | Gene panel |
| GATA4 | LRP4 | het/het | VUS*/VUS | 46,XY DSD | Martinez de LaPiscina et al., 2018 [11] | Gene panel |
| NR5A1 | SRY, FGF10 | hemi/het | P/LP/VUS* | 46,XY DSD | Wang H et al., 2018 [12] | Gene panel |
| NR5A1 | CST9 | het/het | LP/VUS* | 46,XY DSD | Wang H et al., 2018 [12] | Gene panel |
| NR5A1 | CST9 | het/het | LP/LP* | 46,XY DSD | Wang H et al., 2018 [12] | Gene panel |
| NR5A1 | AR, MYH6 | het/hemi/het | LP/LP/VUS | 46,XY DSD | Wang H et al., 2018 [12] | Gene panel |
| NR5A1 | EGF | het/het | LP/VUS | 46,XY DSD | Wang H et al., 2018 [12] | Gene panel |
| NR5A1 | BMP2 | het/het | LP/LB | 46,XY DSD | Wang H et al., 2018 [12] | Gene panel |
| NR5A1 | SOX3 | het/hemi | LP/LP | 46,XY DSD | Wang H et al., 2018 [12] | Gene panel |
| NR5A1 | HSD17B3, WT1 | het/het/het | LP/VUS*/LP | 46,XY DSD | Wang H et al., 2018 [12] | Gene panel |
| SRD5A2 | PROKR2 | comp het/het | LP/P/LP | 46,XY DSD | Zhang W et al., 2019 [14] | Gene panel |
| AR | PROKR2 | hemi/het | LP/LP | 46,XY DSD | Zhang W et al., 2019 [14] | Gene panel |
| AR | TRIM17 | hemi/het | LP/LP | 46,XY DSD | Zhang W et al., 2019 [14] | Gene panel |
| NR5A1 | INHA | het/het | P*/VUS* | 46,XY DSD | Camats et al., 2018 [13] | WES |
| NR5A1 | AKR1C3, DOCK8, FSHR, NCOR1, POR | all het, NCOR1: 2xhet | P*/VUS*/VUS*/VUS*/VUS*/VUS*/VUS* | 46,XY DSD | Camats et al., 2018 [13] | WES |
| NR5A1 | CACNG4, FBLN2, NAV1, SMAD6, SRA1, ZDHHC11, ZFPM2 | all het | LP*/VUS*/VUS*/VUS*/LP*/LB*/VUS*/VUS* | 46,XY DSD | Camats et al., 2018 [13] | WES |
| NR5A1 | CHD7, DENND1A, GDNF, GLI2, SOX30 | all het | P*/VUS*/VUS*/LB*/B*/VUS* | 46,XY DSD | Camats et al., 2018 [13] | WES |
| MAMLD1 | CYP1A1, EVC, GRID1, NOTCH1, RET, RIPK4, ZBTB16 | all het, EVC: 2xhet, RIPK4: 2xhet | B*/VUS/VUS/VUS/VUS/LB/LP/VUS/VUS/VUS | 46,XY DSD | Flück et al., 2019 [6] | WES |
| MAMLD1 | RECQL4 | het/het | B*/VUS | 46,XY DSD | Flück et al., 2019 [6] | WES |
| MAMLD1 | GLI2, RECQL4 | het/het/het | LB*/VUS/LB | 46,XY DSD | Flück et al., 2019 [6] | WES |
| MAMLD1 | CDH23, COL9A3, MAML1, NOTCH1 | all het | LB*/P/VUS/VUS/LB | 46,XY DSD | Flück et al., 2019 [6] | WES |
| MAMLD1 | BNC2, FGF10, HSD3B2, IRX5, MAML2, NOTCH2 | all het | LB*/VUS/VUS/LP/VUS/VUS/VUS | 46,XY DSD | Flück et al., 2019 [6] | WES |
| MAMLD1 | ATF3, BNC2, CYP1A1, EYA1, FLNA, FRAS1, GLI3, HOXA13, IRX5, IRX6, MAML1, MAML3, NRP1, PROP1, PTPN11, WDR11 | all het, FLNA: hemi | LB*/VUS/VUS/VUS/VUS/LB/VUS/VUS/VUS/VUS/VUS/VUS/VUS/VUS/VUS/VUS/VUS | 46,XY DSD | Flück et al., 2019 [6] | WES |
| MAMLD1 | EVC, MAML3, NOTCH2, PPARGC1B, WDR11 | all het | LB*/VUS/VUS/VUS/VUS/VUS | 46,XY DSD | Flück et al., 2019 [6] | WES |
| MAMLD1 | CUL4B, DAPK1, EMX2, FREM2, IGFBP2, MAML2, MAML3, MYO7A, NOTCH1, PIK3R3, TGFBI, WNT9A, WNT9B | all het, CUL4B: hemi | LB/LB/VUS/VUS/LP/VUS/VUS/VUS/-/LP*/VUS/VUS/VUS/VUS/VUS | 46,XX POF | Flück et al., 2019 [6] | WES |
* variant classification revised in varsome/ACMG and HGMD (July 2019). GD: gonadal dysgenesis; homo: homozygous; het: heterozygous; hemi: hemizygous; B: benign; LB: likely benign; VUS: variant of uncertain significance; LP: likely pathogenic; P: pathogenic; WES: whole-exome sequencing.
In 46,XY patients with hypospadias, an oligogenic origin was also suggested by several HTS studies [4,5,9,10,11,12,14] (Table 1).
Kon et al. [4] analyzed 25 causative-candidate-susceptibility genes in 62 46,XY patients with non-syndromic and non-familial hypospadias. Causative mutations were described in seven patients (11.3%), with the AR gene accounting for the highest proportion (4/7) followed by SRD5A2, HSD3B2, and BCN2. In addition, four of these patients carried additional variants in other genes: one hemizygous AR patient carried heterozygous missense substitutions in HOXB6 and MAMLD1 and one patient with a homozygous missense mutation in HSD3B2 had an additional heterozygous missense variant in SRD5A2 that is reported to retain 3% of enzyme activity. The authors concluded that non-syndromic hypospadias may result from a digenic mechanism (Table 1).
Results from an analysis using a targeted DSD gene panel (including 64 known DSD and 967 candidate genes) described a total of 13 46,XY DSD patients who had more than one curated variant in diagnostic DSD genes [5]. Eight of these patients were classified as 46,XY DSD of unknown origin and five had hypospadias. Of the eight patients with 46,XY DSD of unknown origin, five had a known variant in the AR in combination with other DSD gene variants. Two patients had an additional pathogenic homozygous variant in SRD5A2 or HSD17B3, respectively, with the patient combining AR and HSD17B3 presenting a third variant in SOX9. Two other AR variant carriers had additional variants in a testis development gene, WDR11 and ZFPM2, the other one carried variants in NR5A1 and FGFR2. Three individuals had a pathogenic variant in a testis development gene (MAP3K1 or NR5A1) in combination with a less damaging DSD gene variant in WT1, LHCGR, or ZFPM2. Of the five patients with hypospadias, three were found to have a likely pathogenic variant in a testis development gene (MAP3K1 or ZFPM2) in combination with a variant of unknown significance (VUS) in an additional DSD gene (WDR11, MAP3K1, or GATA4), while one patient had two homozygous pathogenic variants (in HSD3B2 and in a CHH gene, GNRHR) and the last patient carried variants of unknown significance (VUS) in two genes of gonadal development (CHD7 and DHH) (Table 1).
In most cases with oligogenic inheritance, at least two of the genes were predicted to be pathogenic and/or contribute to the phenotype. Robevska et al. [9] analyzed the functional characteristics of NR5A1 gene variants and the phenotypes from 15 patients (most of them described in the study of Eggers et al. [5]). Two of these patients carried each an additional heterozygous variant in known 46,XY DSD genes, ZFPM2 [5] and SRD5A2. Whether these additional gene variants are able to modulate the NR5A1 patient phenotypes has been suggested by the authors. The patient carrying an additional ZFPM2 variant presented a more severe phenotype than another patient with the same NR5A1 variant (p.Arg84His) only; the heterozygous SRD5A2 variant (p.Arg227Gln) has been described in numerous patients with biallelic SRD5A2 mutations, but also as a monoallelic finding in patients with micropenis and/or hypospadias [9] (Table 1).
Kolesinska et al. [10] analyzed 37 DSD candidate genes and 21 CHH genes in 35 46,XY DSD patients; eight (23%) were found to carry gene variations in more than one candidate gene. To evaluate whether the DSD cohort was statistically enriched for oligogenicity, they compared the results to exome sequencing data from 247 male participants in the ‘Cohorte Lausannoise’ CoLaus control population. Variants in the 37 DSD-related genes were filtered for non-synonymous variants with a MAF <1.0%, including nonsense, splice-site (±6 base pairs) and missense variants found to be damaging in at least one of the two protein prediction programs, SIFT or MutationTaster. They found a statistical enrichment in oligogenic variants in their DSD cohort compared to CoLaus controls (23% vs. 2.5%; p = 0.0003). From these eight patients, five combined an AR gene defect with another monoallelic gene defect in either a gonadal dysgenesis gene (SOX9, CBX2, or DMRT1) or androgen synthesis gene (POR or DHCR7). Another patient was compound heterozygous for an androgen synthesis gene (HSD17B3) variant and a heterozygous variant in CYP17A1. Still, another patient combined two gonadal dysgenesis genes (HOXA13 and ARX), and one patient combined two heterozygous gene variants in the androgen synthesis gene (AKR1C4) and the genital duct development gene (AMH) (Table 1).
In a study on GATA4 [11], two 46,XY male DSD patients with cryptorchidism, micropenis, and hypospadias without cardiac defects were heterozygous for GATA4 missense variants located close to the GATA4 DNA-binding site, but both variants had wild-type functional activity in vitro. HTS analysis in these two patients revealed additional gene variants in the genes for LHCGR and LRP4, respectively, which are likely contributing to the DSD phenotype [11] (Table 1).
Furthermore, analysis of 70 Chinese patients with a 46,XY DSD phenotype (who could not be diagnosed according to the typical clinical phenotypes and routine candidate gene strategies; most patients presented with undervirilization, such as microphallus, variable degrees of hypospadias, and cryptorchidism) with a candidate gene panel (33 candidates and 47 genes involved in sexual differentiation and development) revealed that 19 out of 33 patients presented multiple (two or more) gene variants, a proportion significantly higher than the rate observed in 144 individuals from a control population [12]. The highest frequency of combined variants was detected in the genes for AR, SRD5A2 and NR5A1. Eighty percent (8 of 10) of patients carrying an heterozygous NR5A1 variant presented additional gene variants in SRY, FGF10, CST9, AR, MYH6, EGF, BMP2, SOX3, HSD17B3, or WT1 (Table 1). The authors concluded that multiple genetic lesions in some cases suggested that DSD is not a simple monogenic disorder and that a potential digenic or oligogenic pattern may underlie the pathological process [12].
In a recent study of 130 Han Chinese 46,XY males with hypospadias of variable degrees (associated or not with other DSD signs and/or other system involvement), 105 genes were analyzed on a panel including genes involved in gonadal/urogenital development (55 well recognized genes), CHH (seven genes), syndromic DSD (four genes), and others (39 genes) [14]. Genetic variants were identified in 25 patients (19.21%): 13 (52%) in the SRD5A2 gene (compound heterozygous or homozygous), six (24%) in the AR gene (hemizygous), and six were heterozygous in other genes. Among them, gene variants in two different genes were only detected in three patients (12%): one compound heterozygous for SRD5A2 and one hemizygous for AR carried the same PROKR2 heterozygous mutation (p.W178S, previously reported in other Chinese patients), while another patient hemizygous for the AR gene carried a novel heterozygous TRIM17 mutation (Table 1). The authors concluded that polygenic inheritance in their population may be a rare genetic cause of hypospadias. In fact, this study detected a high proportion of monogenic 46,XY DSD causes (SRD5A2 and AR genes, with several mutations previously detected in the Han Chinese population), while no gene variants were detected in other candidate genes frequently found in other 46,XY DSD series such as NR5A1 and MAMLD1 [5,39,40].
4.2. HTS in a Second Approach to Detect Digenic or Oligogenic Origin of DSD
In 2012, we studied heterozygous NR5A1 gene variants detected in 10 DSD patients (nine 46,XY DSD and one 46,XX with primary ovarian insufficiency) in whom other DSD-causing genes such as AR, SRD5A2, and CYP17A1 were ruled out by Sanger sequencing [39]. While these gene variants were pathogenic in functional assays when tested alone, they acted similarly to wild-type when tested in heterozygote state together with the wild-type [39]. Thus, our study, similar to others [41,42,43,44], was not able to demonstrate a disease-causing effect leaving genotype–phenotype correlation for NR5A1 variants unsolved. Many patients with variants in NR5A1 have been described with broad phenotypes ranging from severe 46,XY DSD to unvirilized males with/without adrenal failure, 46,XX with ovarian insufficiency, 46,XX with ovotesticular DSD, and healthy carriers [45]. On the other hand, it has also been shown that SF-1 has an extraordinary network of regulators, modulators, and target genes [46,47,48].
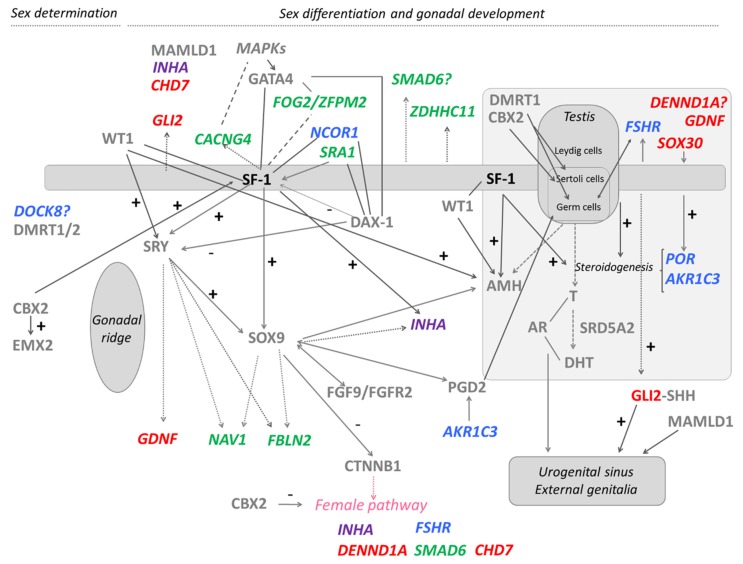
We therefore performed a WES analysis in four of these 46,XY DSD patients with heterozygous NR5A1 gene defects [13] in search for additional genetic hits explaining the phenotypic variability described in patients with NR5A1 mutations [45]. For specific bioinformatic analysis, candidate genes for DSD and genes related to NR5A1 were collected from the literature and databases including known and potential candidate genes. Included DSD-related genes were associated to DSD conditions in humans or rodent models or related to gonadal or sex development; and SF-1/NR5A1-related genes were associated to SF-1 regulation or modulation. An algorithm for data analysis based on these selected project-specific DSD- and SF-1/NR5A1-related genes led us to identify 19 potentially deleterious variants, one to seven per patient in 18 genes (e.g., AKR1C2, CACNG4, CHD7, DENND1A, DOCK8, FBLN2, FOG2/ZFPM2, FSHR, GDNF, GLI2, INHA, NAV1, NCOR1, POR, SMAD6, SOX30, SRA1, and ZDHHC11) [13]. Eight of these genes had been previously reported as DSD-causing in humans. Variants related to 46,XY DSD/CHH were found in genes CHD7, FOG2/ZFPM2, and SRA1, variants related to 46,XX DSD/CHH/primary ovarian insufficiency were found in CHD7, DENND1A, FSHR, GLI2, INHA, POR, and SRA1. Other identified gene variants (n = 7) in AKR1C3, DOCK8, NCOR1, FBLN2, NAV1, SMAD6, and GDNF were not previously related to sex development or gonadal function. By contrast, we also observed variants in genes CACNG4, ZDHHC11, and SOX30 that have been previously discussed as strong DSD candidates [46,49]. With respect to gene interactions with SF-1, nine of the detected genes have been previously shown to interact with SF-1/NR5A1 in functional studies [46,47,48,50,51]: five of them (FSHR, CACNG4, GLI2, SMAD6, and ZDHHC11) as targets of SF-1 [46,47,48], another three (NCOR1, SOX30 and SRA1) as regulators of SF-1 [47,50], and INHA as both SF-1 target and regulator [47]. From these data, we were able to construct a scheme of all hits within the landscape of currently known genes involved in male sex determination and differentiation (Figure 1). The results suggested that the broad phenotypes in heterozygous NR5A1 46,XY DSD subjects may be explained by an oligogenic mechanism, in which multiple hits may contribute to a DSD phenotype unique to each heterozygous SF-1/NR5A1 individual [13] (Figure 1).
Figure 1.
Additional genetic variants identified in four 46,XY patients with disordered/different sex development harboring heterozygous NR5A1/SF-1 disease-causing variants depicted with respect to the known pathways of male sex determination and differentiation. The scheme shows an overview of involved genes and their interrelationship. It emphasizes on SF-1, which seems to play an important role throughout all developmental processes (indicated by a thick line). Genes with variants identified by whole exome sequencing in the patients have specific colors. In violet: candidate gene in patient 1; in blue: candidate genes in patient 2; in green: candidate genes in patient 3; in red: candidate genes in patient 4; in grey: known genes involved in sexual development. Interrogation mark (?): function/timing/location is not clear; arrows: regulation/co-activation; dotted arrows: genes with binding regions for SF-1, SRY, and/or SOX9; lines: interaction/partnership; dashed lines: related genes, but thus far unclear how exactly; thick dashed arrows: hormone production. Modified from [13].
More recently, we performed a WES study in eight DSD patients (seven 46,XY and one 46,XX) carrying sequence variation in MAMLD1 previously detected by Sanger sequencing [6]. Seven of eight MAMLD1 sequence variations did not show alterations in functional activity in vitro when compared to wild-type MAMLD1 and thus did not explain the DSD phenotype sufficiently [40]. So far, the role of MAMLD1 in sex development is controversial for several reasons, including that the same MAMLD1 variant may be present in healthy carriers and in 46,XY DSD patients with different severity of phenotypes [40]. We, therefore, hypothesized that MAMLD1 variants may also not suffice to explain the 46,XY DSD phenotype. WES data from these patients were obtained and filtered by an algorithm including disease-tailored lists of MAMLD1-related and DSD-related genes [6]. This analysis showed that patients harbored 1–16 variants in 1–16 genes together with their MAMLD1 variation. Fifty-five potentially deleterious variants in 41 genes were identified. Seventeen variants were reported in genes that had been previously associated with hypospadias (ATF3, BNC2, CYP1A1, EMX2, EYA1, FLNA, GLI3, GRID1, GLI2, BNC2, FGF10, HOXA13, HSD3B2, IRX5, IRX6, PPARGC1B, and WDR11), eight with cryptorchidism (BNC2, FLNA, RET, RECQL4, NRP1, PTPN11, RIPK4, and ZBTB16), and five with micropenis (ZBTB16, BNC2, EVC, FGF10, and RIPK4). Moreover, 16 identified genes had been previously described in other types of DSD (CUL4B, EMX2, FRAS1, FREM2, HSD3B2, NOTCH2, and NRP1) and/or were reported in different syndromes (CYP1A1, EVC, FRAS1, HOXA13, PTPN11, RECQL4, RET, RIPK4, and ZBTB16). In addition, 27 genes had been previously described in the context of sex or gonadal development (ATF3, BNC2, CDH23, COL9A3, DAPK1, EMX2, EVC, EYA1, FLNA, FRAS1, FREM2, GLI2, GLI3, HOXA13, IGFBP2, IRX5, MAML3, MYO7A, NOTCH1, NOTCH2, NRP1, PIK3R3, RET, RIPK4, TGFBI, WNT9A, and WNT9B). By contrast, only 13 genes (ATF3, DAPK1, EMX2, FLNA, FRAS1, FREM2, GLI3, IGFBP2, IRX5, MAML3, PIK3R3, WNT9A, and WNT9B) had been previously described in female gonadal development and 46,XX DSD and eight of them (DAPK1, EMX2, FREM2, IGFBP2, MAML3, PIK3R3, WNT9A, and WNT9B) were found in the 46,XX DSD patient (Table 1).
Nineteen of the 41 genes had been previously published in DSD panels (ATF3, BNC2, CUL4B, EVC, FLNA, FRAS1, FREM2, GLI3, HOXA13, HSD3B2, IRX5, NOTCH2, PROP1, PTPN11, RECQL4, RET, RIPK4, WDR11, ZBTB16). In addition, with this study we are adding 22 new candidate genes to the list of genes to consider in DSD (CDH23, COL9A3, CYP1A1, DAPK1, EMX2, EYA1, FGF10, GLI2, GRID1, IGFBP2, IRX6, MAML1, MAML2, MAML3, MYO7A, NOTCH1, NRP1, PIK3R3, PPARGC1B, TGFBI, WNT9A, and WNT9B).
A search for an underlying network comprising variants in the identified genes related to MAMLD1 revealed a considerable number of genes (n = 23) that showed interactions suggesting that genetic variations in these genes may affect sex development in concert. Interestingly, MAML3 (one variant in our 46,XX DSD patient) was found in a network related to female gonadal development [52]. Overall, three genes seemed prominent in the network analysis: NOTCH1/NOTCH2 and GLI3 (Figure 2) [6].
Figure 2.
Interaction network of DSD- and MAMLD1-related genes identified in DSD individuals harboring genetic variants in MAMLD1. The scheme depicts an overview of detected genes and their interrelationship. For the search for functional human partners, we used the Search Tool for the Retrieval of Interacting Genes/Proteins (STRING, http://string-db.org/). Nodes represent proteins. Filled nodes show proteins with known or predicted 3D structure. Empty nodes depict proteins with unknown 3D structure. Candidate genes are underlined. Known interactions correspond to curated databases (turquoise lines) and experimentally determined interactions (pink lines). Predicted interactions correspond to gene neighborhood (green lines), gene fusions (red lines), and gene co-occurrence (blue lines). Other interactions correspond to text mining (yellow lines), co-expression (black lines), and protein homology (violet lines). Reproduced from [6].
To summarize, results from the above studies have identified a digenic or oligogenic disorder in DSD mainly by combining mutations in genes involved more frequently in gonadal development (NR5A1, MAP3K1, ZFPM2, GATA4, CHD7, HOXA13, and MAMLD1 combined with other gonadal development genes), followed by the AR gene combined with gonadal development genes and less frequently with steroidogenesis genes.
5. Perspectives and Pitfalls
With the rapid evolution of HTS technology in terms of improving quality and diminishing costs, it is now conceivable that the best recommendable genetic diagnostic approach in 46,XY DSD patients and 46,XX DSD non-CAH patients is using a HTS technology [3]. In this perspective, although panels of candidate genes offer guaranteed coverage, candidate gene lists are growing fast and harnessing gene panels (even economically) is getting more and more difficult. Consequently, whereas gene panels become regularly outdated, WES allows the analysis of as many genes as wanted and affording re-analyses at any demand.
On the other hand, identification of “large” CNVs has been historically restricted to other (molecular) techniques such as array-CGH. This is also being solved nowadays in gene panels, as their robust coverage allows the detection of large deletions and duplications thanks to newly developed bioinformatic tools such as ExomeDepth [53]. Furthermore, some studies demonstrate that this analysis is already possible for WES, yet it needs some improvement [54].
Nevertheless, with the identification of more variants it becomes even more difficult to distinguish between what is contributing to the phenotype and what is not. This leads to discuss the difficulties of studying polygenic disorders. In this perspective, polygenic outcome has to face the following points:
(a) Algorithms of analysis including gene lists may enrich potentially deleterious variants that may ultimately not affect sex development, yet makes the analysis easier as the gene lists can be regularly updated. On the other hand, another possibility of analysis could be a “blind” analysis following the filtering criteria, yet without filtering by the gene lists. This would give the whole picture, but many other potentially affected genes indeed without any relationship with sex development or gonadal function may arise, making the outcome harder to understand. Maybe these two approaches could be done in parallel, to have a whole picture of the patient, mainly when the gene-list approach is not giving a “clue”.
(b) Bioinformatic network analysis can help in interpreting complex genetic data and put identified single candidate genes into a greater perspective to understand their possible role in DSD biology. There are some tools, such as STRING (https://string-db.org/), BioGRID (https://thebiogrid.org/), and databases that can help, yet we have to be cautious when using these networks, as they need expert eyes to interpret them.
(c) Biostatistics requires large sample sizes mostly not available in rare disorders such as DSD. Related to this, we would like to emphasize the need for multidisciplinary teams of medical specialists and researchers to implement multicenter collaborations by using well-accredited international registries such as the I-DSD Registry [55] and the European Reference Network for Rare Endocrine Diseases (EndoERN) [56].
(d) Cell and animal models used in monogenic diseases are useful until a certain point: it is still feasible to study some gene variants and a discreet number of genes at the same time in the same model, but not in the case of “many” variants. Due to the complexity of sex development itself, a proper cell model has been searched for, for many years, to properly mimic patients’ phenotypes and study DSD-related candidate genes and role of candidate variants. Nowadays, new techniques based on cell reprograming and in vitro guided differentiation (from differentiated cells to pluripotent stem cells to redifferentiated cells again) open the field to adequate models for DSD in the near future to predict the role of candidate variants [57,58,59].
In summary, recent studies support the concept that the broad range of some DSD phenotypes may be due to digenic or oligogenic origin similarly to results described in other endocrine disorders such as CHH and congenital hypothyroidism. This is conceivable as sex developmental biology is complex and involves a vast network of genes. While some DSD phenotypes can be explained sufficiently by monogenetic defects, others may be caused by multiple minor hits in genetic networks. Whether these genes form clusters remains unknown until results of bigger cohorts of DSD individuals are studied.
Funding
This research was supported by the Beatriu de Pinós Fellowship 2014 BP-B 00145 (AGAUR, Catalonia, Spain), the Instituto de Salud Carlos III (www.isciii.es/; Madrid, Spain) Centro de Investigación Biomédica en Red de Enfermedades Raras (CIBERER; http://www.ciberer.es/) U-712 to N.C., and by the Swiss National Science Foundation (http://www.snf.ch) (320030-146127) to C.E.F.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Cools M., Nordenström A., Robeva R., Hall J., Westerveld P., Flück C., Köhler B., Berra M., Springer A., Schweizer K., et al. Caring for individuals with a difference of sex development (DSD): A Consensus Statement. Nat. Rev. Endocrinol. 2018;14:415–429. doi: 10.1038/s41574-018-0010-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alhomaidah D., McGowan R., Ahmed S.F. The current state of diagnostic genetics for conditions affecting sex development. Clin. Genet. 2017;91:157–162. doi: 10.1111/cge.12912. [DOI] [PubMed] [Google Scholar]
- 3.Audí L., Ahmed S.F., Krone N., Cools M., McElreavey K., Holterhus P.-M., Greenfield A., Bashamboo A., Hiort O., Wudy S.A., et al. Genetics in endocrinology: Approaches to molecular genetic diagnosis in the management of differences/disorders of sex development (DSD): Position paper of EU COST Action BM 1303 “DSDnet”. Eur. J. Endocrinol. 2018;179:261–267. [Google Scholar]
- 4.Kon M., Suzuki E., Dung V.C., Hasegawa Y., Mitsui T., Muroya K., Ueoka K., Igarashi N., Nagasaki K., Oto Y., et al. Molecular basis of non-syndromic hypospadias: Systematic mutation screening and genome-wide copy-number analysis of 62 patients. Hum. Reprod. 2015;30:499–506. doi: 10.1093/humrep/deu364. [DOI] [PubMed] [Google Scholar]
- 5.Eggers S., Sadedin S., van den Bergen J.A., Robevska G., Ohnesorg T., Hewitt J., Lambeth L., Bouty A., Knarston I.M., Tan T.Y., et al. Disorders of sex development: Insights from targeted gene sequencing of a large international patient cohort. Genome Biol. 2016;17:243. doi: 10.1186/s13059-016-1105-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Flück C.E., Audí L., Fernández-Cancio M., Sauter K.-S., Martinez de LaPiscina I., Castaño L., Esteva I., Camats N. Broad Phenotypes of Disorders/Differences of Sex Development in MAMLD1 Patients Through Oligogenic Disease. Front. Genet. 2019 doi: 10.3389/fgene.2019.00746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mazen I., Abdel-Hamid M., Mekkawy M., Bignon-Topalovic J., Boudjenah R., El Gammal M., Essawi M., Bashamboo A., McElreavey K. Identification of NR5A1 Mutations and Possible Digenic Inheritance in 46,XY Gonadal Dysgenesis. Sex. Dev. 2016;10:147–151. doi: 10.1159/000445983. [DOI] [PubMed] [Google Scholar]
- 8.Werner R., Mönig I., Lünstedt R., Wünsch L., Thorns C., Reiz B., Krause A., Schwab K.O., Binder G., Holterhus P.M., et al. New NR5A1 mutations and phenotypic variations of gonadal dysgenesis. PLoS ONE. 2017 doi: 10.1371/journal.pone.0176720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Robevska G., van den Bergen J.A., Ohnesorg T., Eggers S., Hanna C., Hersmus R., Thompson E.M., Baxendale A., Verge C.F., Lafferty A.R., et al. Functional characterization of novel NR5A1 variants reveals multiple complex roles in disorders of sex development. Hum. Mutat. 2018 doi: 10.1002/humu.23354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kolesinska Z., Acierno J., Faisal Ahmed S., Xu C., Kapczuk K., Skorczyk-Werner A., Mikos H., Rojek A., Massouras A., Krawczynski M.R., et al. Integrating clinical and genetic approaches in the diagnosis of 46,XY disorders of sex development. Endocr. Connect. 2018 doi: 10.1530/EC-18-0472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de LaPiscina I.M., de Mingo C., Riedl S., Rodriguez A., Pandey A.V., Fernández-Cancio M., Camats N., Sinclair A., Castaño L., Audi L., et al. GATA4 variants in individuals with a 46,XY Disorder of Sex Development (DSD) may or may not be associated with cardiac defects depending on second hits in other DSD genes. Front. Endocrinol. 2018;9:142. doi: 10.3389/fendo.2018.00142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang H., Zhang L., Wang N., Zhu H., Han B., Sun F., Yao H., Zhang Q., Zhu W., Cheng T., et al. Next-generation sequencing reveals genetic landscape in 46, XY disorders of sexual development patients with variable phenotypes. Hum. Genet. 2018 doi: 10.1007/s00439-018-1879-y. [DOI] [PubMed] [Google Scholar]
- 13.Camats N., Fernández-Cancio M., Audí L., Schaller A., Flück C.E. Broad phenotypes in heterozygous NR5A1 46,XY patients with a disorder of sex development: An oligogenic origin? Eur. J. Hum. Genet. 2018;26:749–757. doi: 10.1038/s41431-018-0202-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang W., Shi J., Zhang C., Jiang X., Wang J., Wang W., Wang D., Ni J., Chen L., Lu W., et al. Identification of gene variants in 130 Han Chinese patients with hypospadias by targeted next-generation sequencing. Mol. Genet. Genomic Med. 2019 doi: 10.1002/mgg3.827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pitteloud N., Durrani S., Raivio T., Sykiotis G.P. Complex genetics in idiopathic hypogonadotropic hypogonadism. Front. Horm. Res. 2010 doi: 10.1159/000312700. [DOI] [PubMed] [Google Scholar]
- 16.Sykiotis G.P., Plummer L., Hughes V.A., Au M., Durrani S., Nayak-Young S., Dwyer A.A., Quinton R., Hall J.E., Gusella J.F., et al. Oligogenic basis of isolated gonadotropin-releasing hormone deficiency. Proc. Natl. Acad. Sci. USA. 2010 doi: 10.1073/pnas.1009622107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mitchell A.L., Dwyer A., Pitteloud N., Quinton R. Genetic basis and variable phenotypic expression of Kallmann syndrome: Towards a unifying theory. Trends Endocrinol. Metab. 2011;22:249–258. doi: 10.1016/j.tem.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 18.Miraoui H., Dwyer A.A., Sykiotis G.P., Plummer L., Chung W., Feng B., Beenken A., Clarke J., Pers T.H., Dworzynski P., et al. Mutations in FGF17, IL17RD, DUSP6, SPRY4, and FLRT3 are identified in individuals with congenital hypogonadotropic hypogonadism. Am. J. Hum. Genet. 2013;92:725–743. doi: 10.1016/j.ajhg.2013.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Boehm U., Bouloux P.M., Dattani M.T., de Roux N., Dode C., Dunkel L., Dwyer A.A., Giacobini P., Hardelin J.P., Juul A., et al. Expert consensus document: European Consensus Statement on congenital hypogonadotropic hypogonadism—Pathogenesis, diagnosis and treatment. Nat. Rev. Endocrinol. 2015;11:547–564. doi: 10.1038/nrendo.2015.112. [DOI] [PubMed] [Google Scholar]
- 20.Maione L., Dwyer A.A., Francou B., Guiochon-Mantel A., Binart N., Bouligand J., Young J. GENETICS IN ENDOCRINOLOGY: Genetic counseling for congenital hypogonadotropic hypogonadism and Kallmann syndrome: New challenges in the era of oligogenism and next-generation sequencing. Eur. J. Endocrinol. 2018 doi: 10.1530/EJE-17-0749. [DOI] [PubMed] [Google Scholar]
- 21.Amato L.G.L., Montenegro L.R., Lerario A.M., Jorge A.A.L., Junior G.G., Schnoll C., Renck A.C., Trarbach E.B., Costa E.M.F., Mendonca B.B., et al. New genetic findings in a large cohort of congenital hypogonadotropic hypogonadism. Eur. J. Endocrinol. 2019 doi: 10.1530/EJE-18-0764. [DOI] [PubMed] [Google Scholar]
- 22.Aycan Z., Cangul H., Muzza M., Bas V.N., Fugazzola L., Chatterjee V.K., Persani L., Schoenmakers N. Digenic DUOX1 and DUOX2 mutations in cases with congenital hypothyroidism. J. Clin. Endocrinol. Metab. 2017 doi: 10.1210/jc.2017-00529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Satoh M., Aso K., Ogikubo S., Yoshizawa-Ogasawara A., Saji T. Hypothyroidism caused by the combination of two heterozygous mutations: One in the TSH receptor gene the other in the DUOX2 gene. J. Pediatr. Endocrinol. Metab. 2015 doi: 10.1515/jpem-2014-0078. [DOI] [PubMed] [Google Scholar]
- 24.Watanabe Y., Bruellman R.J., Ebrhim R.S., Abdullah M.A., Dumitrescu A.M., Refetoff S., Weiss R.E. Congenital Hypothyroidism due to Oligogenic Mutations in Two Sudanese Families. Thyroid. 2019 doi: 10.1089/thy.2018.0295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Peters C., van Trotsenburg A.S.P., Schoenmakers N. DIAGNOSIS OF ENDOCRINE DISEASE: Congenital hypothyroidism: Update and perspectives. Eur. J. Endocrinol. 2018 doi: 10.1530/EJE-18-0383. [DOI] [PubMed] [Google Scholar]
- 26.Hughes I.A., Houk C., Ahmed S.F., Lee P. A; Lawson Wilkins Pediatric Endocrine Society/European Society for Paediatric Endocrinology Consensus Group Consensus statement on management of intersex disorders. J. Pediatr. Urol. 2006 doi: 10.1016/j.jpurol.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 27.Croft B., Ayers K., Sinclair A., Ohnesorg T. Review disorders of sex development: The evolving role of genomics in diagnosis and gene discovery. Birth Defects Res. Part C Embryo Today Rev. 2016 doi: 10.1002/bdrc.21148. [DOI] [PubMed] [Google Scholar]
- 28.Baetens D., Verdin H., De Baere E., Cools M. Update on the genetics of differences of sex development (DSD) Best Pract. Res. Clin. Endocrinol. Metab. 2019 doi: 10.1016/j.beem.2019.04.005. [DOI] [PubMed] [Google Scholar]
- 29.Girardin C.M., Deal C., Lemyre E., Paquette J., Lumbroso R., Beitel L.K., Trifiro M.A., Van Vliet G. Molecular Studies of a Patient with Complete Androgen Insensitivity and a 47,XXY Karyotype. J. Pediatr. 2009 doi: 10.1016/j.jpeds.2009.02.052. [DOI] [PubMed] [Google Scholar]
- 30.Akcay T., Fernandez-Cancio M., Turan S., Güran T., Audi L., Bereket A. AR and SRD5A2 gene mutations in a series of 51 Turkish 46,XY DSD children with a clinical diagnosis of androgen insensitivity. Andrology. 2014 doi: 10.1111/j.2047-2927.2014.00215.x. [DOI] [PubMed] [Google Scholar]
- 31.Batista R.L., Rodrigues A.S., Nishi M.Y., Feitosa A.C.R., Gomes N.L.R.A., Junior J.A.F., Domenice S., Costa E.M.F., De Mendonça B.B. Heterozygous Nonsense Mutation in the Androgen Receptor Gene Associated with Partial Androgen Insensitivity Syndrome in an Individual with 47,XXY Karyotype. Sex. Dev. 2017 doi: 10.1159/000468957. [DOI] [PubMed] [Google Scholar]
- 32.Acar S., Tuhan H., Bora E., Demir K., Onay H., Erçal D., Böber E., Abacı A. Identification of an AR mutation in klinefelter syndrome during evaluation for penoscrotal hypospadias. Hormones. 2017 doi: 10.14310/horm.2002.1741. [DOI] [PubMed] [Google Scholar]
- 33.Cornacchia M.A., Bhushan S., Arguello R. A Case of Familial Male-Limited Precocious Puberty in a Child With Klinefelter Syndrome. J. Endocr. Soc. 2018 doi: 10.1210/js.2018-00192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Idkowiak J., Malunowicz E.M., Dhir V., Reisch N., Szarras-Czapnik M., Holmes D.M., Shackleton C.H.L., Davies J.D., Hughes I.A., Krone N., et al. Concomitant mutations in the P450 oxidoreductase and androgen receptor genes presenting with 46,XY disordered sex development and androgenization at adrenarche. J. Clin. Endocrinol. Metab. 2010 doi: 10.1210/jc.2010-0058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hersmus R., van der Zwan Y.G., Stoop H., Bernard P., Sreenivasan R., Oosterhuis J.W., Brüggenwirth H.T., de Boer S., White S., Wolffenbuttel K.P., et al. A 46,XY female DSD patient with bilateral gonadoblastoma, a novel SRY missense mutation combined with a WT1 KTS splice-site mutation. PLoS ONE. 2012 doi: 10.1371/journal.pone.0040858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stessman H.A., Bernier R., Eichler E.E. A genotype-first approach to defining the subtypes of a complex disease. Cell. 2014 doi: 10.1016/j.cell.2014.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stark Z., Tan T.Y., Chong B., Brett G.R., Yap P., Walsh M., Yeung A., Peters H., Mordaunt D., Cowie S., et al. A prospective evaluation of whole-exome sequencing as a first-tier molecular test in infants with suspected monogenic disorders. Genet. Med. 2016 doi: 10.1038/gim.2016.1. [DOI] [PubMed] [Google Scholar]
- 38.Wright C.F., FitzPatrick D.R., Firth H.V. Paediatric genomics: Diagnosing rare disease in children. Nat. Rev. Genet. 2018 doi: 10.1038/nrg.2017.116. [DOI] [PubMed] [Google Scholar]
- 39.Camats N., Pandey A.V., Fernández-Cancio M., Andaluz P., Janner M., Torán N., Moreno F., Bereket A., Akcay T., García-García E., et al. Ten novel mutations in the NR5A1 gene cause disordered sex development in 46,XY and ovarian insufficiency in 46,XX individuals. J. Clin. Endocrinol. Metab. 2012;97:E1294–E1306. doi: 10.1210/jc.2011-3169. [DOI] [PubMed] [Google Scholar]
- 40.Camats N., Fernández-Cancio M., Audí L., Mullis P.E., Moreno F., González Casado I., Pedro López-Siguero J., Corripio R., De La Vega J.A.B., Blanco J.A., et al. Human MAMLD1 gene variations seem not sufficient to explain a 46,XY DSD phenotype. PLoS ONE. 2015;10:e0142831. doi: 10.1371/journal.pone.0142831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Biason-Lauber A., Schoenle E.J. Apparently normal ovarian differentiation in a prepubertal girl with transcriptionally inactive steroidogenic factor 1 (NR5A1/SF-1) and adrenocortical insufficiency. Am. J. Hum. Genet. 2000;67:1563–1568. doi: 10.1086/316893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kohler B., Lin L., Ferraz-de-Souza B., Wieacker P., Heidemann P., Schroder V., Biebermann H., Schnabel D., Gruters A., Achermann J.C. Five novel mutations in steroidogenic factor 1 (SF1, NR5A1) in 46,XY patients with severe underandrogenization but without adrenal insufficiency. Hum. Mutat. 2008;29:59–64. doi: 10.1002/humu.20588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Reuter A.L., Goji K., Bingham N.C., Matsuo M., Parker K.L. A novel mutation in the accessory DNA-binding domain of human steroidogenic factor 1 causes XY gonadal dysgenesis without adrenal insufficiency. Eur. J. Endocrinol. 2007;157:233–238. doi: 10.1530/EJE-07-0113. [DOI] [PubMed] [Google Scholar]
- 44.Tajima T., Fujiwara F., Fujieda K. A novel heterozygous mutation of steroidogenic factor-1 (SF-1/Ad4BP) gene (NR5A1) in a 46, XY disorders of sex development (DSD) patient without adrenal failure. Endocr. J. 2009;56:619–624. doi: 10.1507/endocrj.K08E-380. [DOI] [PubMed] [Google Scholar]
- 45.Fabbri-Scallet H., Sousa L.M., Maciel-Guerra A.T., Guerra-Júnior G., Mello M.P. Mutation update for the NR5A1 gene involved in DSD and infertility. Hum. Mutat. 2020 doi: 10.1002/humu.23916. [DOI] [PubMed] [Google Scholar]
- 46.Ferraz-de-Souza B., Lin L., Shah S., Jina N., Hubank M., Dattani M.T., Achermann J.C. ChIP-on-chip analysis reveals angiopoietin 2 (Ang2, ANGPT2) as a novel target of steroidogenic factor-1 (SF-1, NR5A1) in the human adrenal gland. FASEB J. 2011;25:1166–1175. doi: 10.1096/fj.10-170522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schimmer B.P., White P.C. Minireview: Steroidogenic factor 1: Its roles in differentiation, development, and disease. Mol. Endocrinol. 2010;24:1322–1337. doi: 10.1210/me.2009-0519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hoivik E.A., Lewis A.E., Aumo L., Bakke M. Molecular aspects of steroidogenic factor 1 (SF-1) Mol. Cell. Endocrinol. 2010;315:27–39. doi: 10.1016/j.mce.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 49.Han F., Dong Y., Liu W., Ma X., Shi R., Chen H., Cui Z., Ao L., Zhang H., Cao J., et al. Epigenetic regulation of sox30 is associated with testis development in mice. PLoS ONE. 2014;9:e97203. doi: 10.1371/journal.pone.0097203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Xu B., Yang W.-H., Gerin I., Hu C.-D., Hammer G.D., Koenig R.J. Dax-1 and Steroid Receptor RNA Activator (SRA) Function as Transcriptional Coactivators for Steroidogenic Factor 1 in Steroidogenesis. Mol. Cell. Biol. 2009 doi: 10.1128/MCB.01010-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kelly V.R., Hammer G.D. LRH-1 and Nanog regulate Dax1 transcription in mouse embryonic stem cells. Mol. Cell. Endocrinol. 2011;332:116–124. doi: 10.1016/j.mce.2010.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jameson S.A., Natarajan A., Cool J., DeFalco T., Maatouk D.M., Mork L., Munger S.C., Capel B. Temporal transcriptional profiling of somatic and germ cells reveals biased lineage priming of sexual fate in the fetal mouse gonad. PLoS Genet. 2012;8:e1002575. doi: 10.1371/journal.pgen.1002575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Plagnol V., Curtis J., Epstein M., Mok K.Y., Stebbings E., Grigoriadou S., Wood N.W., Hambleton S., Burns S.O., Thrasher A.J., et al. A robust model for read count data in exome sequencing experiments and implications for copy number variant calling. Bioinformatics. 2012 doi: 10.1093/bioinformatics/bts526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Marchuk D.S., Crooks K., Strande N., Kaiser-Rogers K., Milko L.V., Brandt A., Arreola A., Tilley C.R., Bizon C., Vora N.L., et al. Increasing the diagnostic yield of exome sequencing by copy number variant analysis. PLoS ONE. 2018 doi: 10.1371/journal.pone.0209185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ali S., Lucas-Herald A., Bryce J., Ahmed S. The Role of International Databases in Understanding the Aetiology and Consequences of Differences/Disorders of Sex Development. Int. J. Mol. Sci. 2019 doi: 10.3390/ijms20184405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hiort O., Cools M., Springer A., McElreavey K., Greenfield A., Wudy S.A., Kulle A., Ahmed S.F., Dessens A., Balsamo A., et al. Addressing gaps in care of people with conditions affecting sex development and maturation. Nat. Rev. Endocrinol. 2019 doi: 10.1038/s41574-019-0238-y. [DOI] [PubMed] [Google Scholar]
- 57.Ruiz-Babot G., Balyura M., Hadjidemetriou I., Ajodha S.J., Taylor D.R., Ghataore L., Taylor N.F., Schubert U., Ziegler C.G., Storr H.L., et al. Modeling Congenital Adrenal Hyperplasia and Testing Interventions for Adrenal Insufficiency Using Donor-Specific Reprogrammed Cells. Cell Rep. 2018 doi: 10.1016/j.celrep.2018.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rodríguez Gutiérrez D., Eid W., Biason-Lauber A. A Human Gonadal Cell Model From Induced Pluripotent Stem Cells. Front. Genet. 2018 doi: 10.3389/fgene.2018.00498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rodríguez Gutiérrez D., Biason-Lauber A. Pluripotent Cell Models for Gonadal Research. Int. J. Mol. Sci. 2019;20:5495. doi: 10.3390/ijms20215495. [DOI] [PMC free article] [PubMed] [Google Scholar]