Abstract
BACKGROUND:
There has been a dramatic rise in the number of opioid prescriptions and opioid overdose deaths in the United States over the past 15 years. Misuse and abuse of opioids is also a growing public health concern in the United States. Medicaid enrollees are more likely to be prescribed opioids and are at higher risk of prescription drug overdose compared with non-Medicaid populations. Despite rising opioid drug overdose deaths in Georgia, prevalence of indicators for potential inappropriate prescribing practices has not been examined to date.
OBJECTIVE:
To examine trends in the general use of opioids and the prevalence of indicators for potential inappropriate opioid prescribing among the Georgia Medicaid population across various demographic characteristics over time.
METHODS:
This study used data from the Georgia individual Medicaid pharmacy claims database from 2009 to 2014. Data sample included 3,562,227 observations (patient prescriptions) representing 401,488 individuals. Outcome measures assessed the trends in the general use of opioids and the indicators of potential inappropriate prescribing practices by providers. These outcome measures were taken from previous expert panels and clinical guidelines (e.g., overlapping prescriptions of opioids, opioids and benzodiazepines, and opioids and buprenorphine/naloxone, as well as high daily doses of opioids). Analyses were stratified by gender, type of insurance (fee-for-service and managed care), age, and race/ethnicity.
RESULTS:
The average number of opioid prescriptions, average days supply of opioids per patient, and average daily dose of opioids per patient increased over time across all demographic categories with older, fee-for-service, male, and missing race groups experiencing higher use across all 6 years compared with their counterparts. A similar pattern was observed for average number of incidences of potential inappropriate prescribing of opioids in this population from 2009 to 2014. The percentage of Medicaid enrollees with at least 1 or more indicators of potential inappropriate prescriptions slightly increased from 17.17% to 18.21% during the study time frame. Moreover, the incidence rate of indicators for potential inappropriate prescribing of opioids also increased over time across all demographic groups, with the oldest age group (55-64 years) experiencing the largest increment. The incidence rate of potential inappropriate prescribing practices per patient increased more than 58% over the 6 years.
CONCLUSIONS:
The results of this study show that potentially inappropriate prescribing practices are common and are increasing over time in the Georgia Medicaid population across all demographic categories, with individuals who are listed in the missing race category, have fee-for-service plans, and are older experiencing the largest increments. These findings indicate that patients in certain demographic groups could be at higher risk for experiencing adverse health outcomes related to inappropriate prescribing of opioids. Further research is needed to explore which policy tools or interventions might be more effective in reducing inappropriate prescribing practices in this population.
What is already known about this subject
Inappropriate prescribing of opioids is associated with adverse health outcomes such as overdose deaths.
Medicaid populations are more likely to receive opioid prescriptions and are at higher risk of drug overdose compared with non-Medicaid populations.
What this study adds
This study examined trends in prevalence of indicators for potential inappropriate prescribing of opioids in the Georgia Medicaid population using patient demographic characteristics such as age, gender, race/ethnicity, and type of insurance.
Potentially inappropriate prescribing practices are common and are increasing over time in the Georgia Medicaid population across all demographic categories, with individuals enrolled in fee-for-service plans and in the older population group (aged 55-64 years) experiencing the largest increments.
As rates of opioid analgesic prescribing and deaths related to opioid overdose continue to rise in the United States, comprehensive strategies such as increasing access to naloxone and treatment for opioid use disorder (OUD), strengthening prescription drug monitoring programs, increasing oversight of pain management clinics, and requiring prescriber education focused on pain management and opioid prescribing must be implemented to reduce the harms associated with inappropriate prescribing of opioid analgesics. Inappropriate prescribing of opioids is defined as overlapping prescriptions of opioids, overlapping prescriptions of benzodiazepines and opioids, overlapping prescriptions of opioids and Suboxone (buprenorphine/naloxone); a high daily dose of opioids (100 morphine milligram equivalents [MMEs] or greater); and long-acting (LA)/extended release opioids for acute pain conditions. This is particularly true for the Medicaid population, which experiences high rates of opioid prescribing, opioid-related overdose deaths, and OUD.1,2
As of 2014, approximately 55 million Medicaid patients were enrolled in some type of managed care plan. While many states still offer services through traditional fee-for-service plans, a majority of enrollees receive care through Medicaid managed entities.3 This is true for Georgia as well. However, little information exists on trends in utilization of opioids and inappropriate prescribing of opioids by insurance type in Medicaid populations. Thus, examining differences in opioid prescribing by enrollment type may provide important insights to policymakers and prescribers on management approaches and prescription patterns.
Although a majority of Medicaid enrollees in states that have not opted to expand Medicaid are women and children, previous research suggests that men are at greater risk for opioid misuse, OUD, and death from overdose.2 In fact, a recent study of opioid-related deaths found that the rate of death for men was almost twice as high as the rate of death for women.4 Data also indicate that the gender gap in overdose deaths related to prescription opioids is closing and that patterns of potentially inappropriate prescribing of opioids vary by gender.2 One study of Medicaid enrollees in 12 states found that a higher percentage of men had 2 or more indicators of inappropriate use of opioids when compared with women (11.6% vs. 10.7%), and a higher percentage of men had 3 or more indicators of inappropriate use compared with women (6.0% vs. 4.7%). However, studies of patients with commercial insurance indicate that women are more likely to have indicators of potential inappropriate prescribing of opioid analgesics.5 Given these findings, it is also important to examine trends in opioid prescribing by gender.
Previous research indicates that rates of overdose death related to prescription opioids are higher among non-Hispanic whites compared with non-Hispanic blacks and Hispanics and among persons aged 25-54 years.2,4 A recent study of opioid-related deaths among Medicaid enrollees in Washington state found that the death rate was highest for enrollees aged 45-54 years, followed by those aged 35-44 years and 55-64 years.4 However, no previous studies have examined the distribution of potential inappropriate prescribing of opioids by age group.
Few studies have examined opioid prescribing in the Medicaid population.1,6,7 A study by Mack et al. (2015) used cross-sectional data from 2010 to investigate potential inappropriate prescribing and misuse of opioids among Medicaid enrollees in 12 states.1 This study only provides a snapshot of opioid prescribing in a single year. In addition, the study did not examine differences in opioid prescribing by Medicaid enrollment type, race/ethnicity, or age. Other studies relied on older data and did not examine potential inappropriate prescribing but rather focused on rates of opioid use for noncancer pain.6,7
Longitudinal data allow for a more nuanced understanding of potential inappropriate prescribing of opioids. Such data can be used to better target policies aimed at reducing inappropriate opioid prescribing and related harms. To address these gaps in the literature, this study examined trends in the use of opioids and the prevalence of potential inappropriate prescribing of opioids in the Georgia Medicaid population from 2009 to 2014 by using various demographic characteristics.
Methods Data
This study used individual pharmacy claims data from the Georgia Medicaid pharmacy claims database from 2009 to 2014. The study sample was restricted to individuals aged 18-64 years who received an opioid prescription (short- or long-acting extended release opioids) during the study period (4,220,791 patient prescriptions). Opioid prescriptions were identified using National Drug Code numbers, and the list of opioids included in the study was adapted from Jayawardhana et al. (2018).8 Similar to previous literature, individuals with cancer diagnoses were excluded from the study (657,429 patient prescriptions excluded).1,5 Cancer diagnoses were identified using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes 338.3, 140-172.9, 174-215.9, 217-229.10, and 235-239.9. After excluding any observations with quantities less than 1 (1,135 patient prescriptions excluded), the final study sample included 3,562,227 patient-prescription observations representing 401,488 individuals over the study period. It should be noted that about 8.6% of the individuals in the sample did not include race information for the study period, although they included information regarding age, gender, and insurance type. Therefore, a missing race category was created to include the individuals with this missing information in the analysis, which allowed us to examine whether the missing race group behavior differed from the other race groups in the data.
Measures
Indicators of general opioid use were presented using average days supply of opioids per patient, average daily dose of opioids per patient in MMEs, and average number of opioid prescriptions per patient across each year.
The indicators for potential inappropriate prescribing practices by providers were adapted following input from previous expert panels and using clinical guidelines and were measured using the following 5 indicators: (1) overlapping opioid prescriptions, defined as opioid prescriptions that overlap by 7 days or more; (2) overlapping opioid and benzodiazepine prescriptions, defined as opioid and benzodiazepine prescriptions that overlap by 7 days or more; (3) overlapping opioid and buprenorphine/naloxone prescriptions, defined as opioid and buprenorphine/naloxone prescriptions that overlap by 1 day or more; (4) LA/extended release opioids prescribed for acute pain; and (5) high daily doses of opioid prescriptions, defined as receiving more than 100 MMEs.9-13
Statistical Analysis
The trends in the general use of opioids were examined using average number of prescriptions per patient, average days supply of opioids per patient, and average daily dose of opioids per patient across each year. The trends in the prevalence of indicators for potential inappropriate prescribing practices by providers were analyzed using both number and proportions of Medicaid enrollees with inappropriate prescribing indicators, number of incidences of indicators for potential inappropriate prescriptions, and the incidence rate of such indicators per patient across each year. Since a patient could be present in the study sample across multiple years, the analyses were carried out at the patient-year level, and included 754,622 patient-year observations. The analyses were stratified by gender (male/female), type of insurance (fee-for-service or managed care), age groups (18-34, 35-44, 45-54, 55-64 years), and race/ethnicity (Hispanic, non-Hispanic white, non-Hispanic black, non-Hispanic other, and missing race) to understand the variations across these categories over time. All statistical analyses were conducted using Stata, version 14.2 (StataCorp, College Station, TX).
Results
The average number of opioid prescriptions received by Georgia Medicaid enrollees increased over time across all demographic categories (Figure 1). Among age groups, the largest increase was among those enrollees aged 55-64 years (66.1%), with enrollees aged 45-54 years ranking with the second highest increase (65.3%) when compared with other age groups between 2009 and 2014. Fee-for-service enrollees (60.4%) and male (53.3%) enrollees experienced the largest increases compared with managed care (28.1%) and female (39.8%) enrollees, respectively. Interestingly, the missing race group experienced the largest increase in average number of opioid prescriptions (64%) compared with other race/ethnicity groups during the study period. Non-Hispanic whites ranked second with the highest average number of opioid prescriptions per patient while non-Hispanic blacks ranked fourth across all years. However, the percentage increase in the average number of opioid prescriptions was larger among non-Hispanic blacks (41.5%) than among non-Hispanic whites (39.7%) from 2009 to 2014.
FIGURE 1.
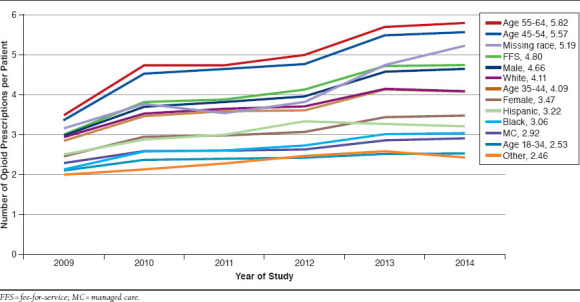
Average Number of Opioid Prescriptions per Patient by Insurance Type, Age, Gender, Race/Ethnicity and Year
Similarly, the average days supply of opioids per patient increased over time across all categories (Figure 2), with fee-for-service enrollees experiencing the largest increase (106.1%) across all groups from 2009 to 2014. Fee-for-service and male enrollees experienced higher average days supply of opioids per patient compared with managed care and female enrollees across all years. The percentage increase in average days supply of opioids per patient was also higher among males (91.3%) compared with females (77.3%), but it was much lower for managed care enrollees (54%) compared with fee-for-service enrollees (106.1%) during the study period. The oldest age group (55-64 years) experienced the highest average days supply of opioids per patient across all years while the second oldest age group (45-54 years) ranked second. The percentage increase in average days supply of opioids per patient from 2009 to 2014 was also higher among the oldest age group (99%), while the second oldest age group ranked second (97.9%). The missing race group experienced the highest average days supply of opioids per patient across all 6 years, while non-Hispanic whites ranked second and non-Hispanic blacks ranked fourth across all years (Figure 2). Similar to average number of prescriptions, the missing race group experienced the largest percentage increase in average days supply of opioids per patient (98.7%) among all race groups, while non-Hispanic blacks experienced the second largest increase (85.9%), Hispanics experienced the third largest increase (72.5%), and non-Hispanic whites ranked fourth (71.3%). The majority of the missing race group was female (64.5%), in the younger age group (18-34 years, 34.9%), and belonged to the fee-for-service payment model (83.9%).
FIGURE 2.
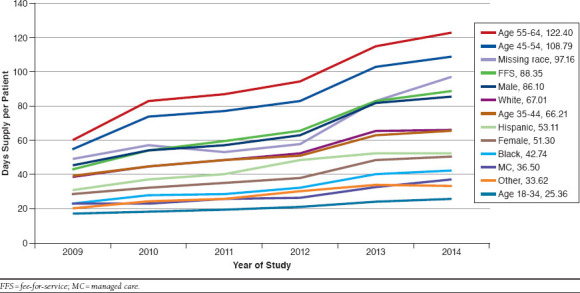
Average Days Supply of Opioids per Patient by Insurance Type, Age, Gender, Race/Ethnicity, and Year
The average daily dose of opioids per patient also increased over time across all categories (Figure 3), with the oldest age group (55-64 years) experiencing the largest increase (69.4%) from 2009 to 2014. Both the oldest age group (55-64 years) and the second oldest age group (45-54 years) experienced a higher average daily dose of opioids per patient compared with other age groups across all years. The missing race group experienced a higher average daily dose of opioids per patient across almost all years (except for 2011) compared with all other race groups. In addition, the missing race group also experienced the largest percentage increase in average daily dose of opioids (69.1%) compared with all other race groups from 2009 to 2014. While male and fee-for-service enrollees experienced a higher average daily dose of opioids per patient across all years compared with female and managed care enrollees, fee-for-service enrollees experienced the largest percentage increase (59.2%) from 2009 to 2014 compared with managed care (50.4%), male (56%), and female (52.3%) enrollees.
FIGURE 3.
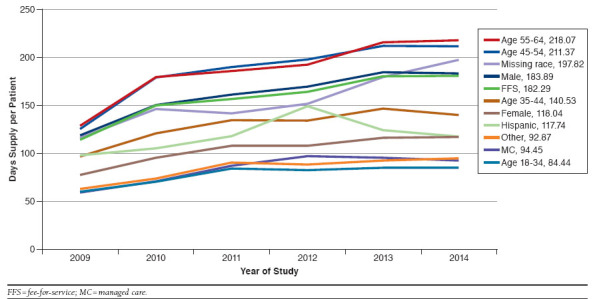
Average Daily Dose of Opioids per Patient by Insurance Type, Age, Gender, Race/Ethnicity, and Year
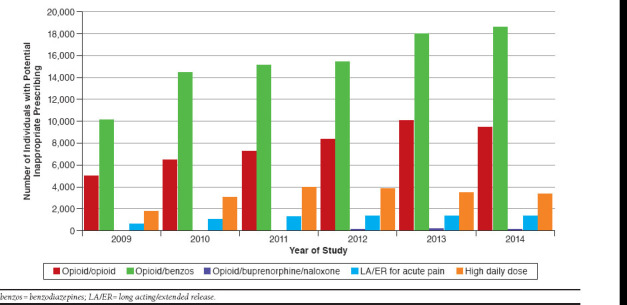
The average number of total incidences of potential inappropriate prescribing of opioids among Georgia Medicaid enrollees increased over time across all demographic categories (Figure 4), with non-Hispanic blacks experiencing the largest percentage increase (89.8%) from 2009 to 2014. While non-Hispanic blacks experienced the largest percentage increase from 2009 to 2014, the missing race group experienced a higher average number of incidences of potential inappropriate prescribing of opioids compared with all other race groups across all years. Both fee-for-service enrollees and male enrollees experienced a higher average number of incidences of potential inappropriate prescribing of opioids across all years compared with managed care and female enrollees, respectively. The average number of incidences of potential inappropriate prescribing of opioids was higher among the oldest age group (55-64 years) across all years, while that age group also experienced the largest percentage increase (73.8%) from 2009 to 2014 compared with all other age groups.
FIGURE 4.
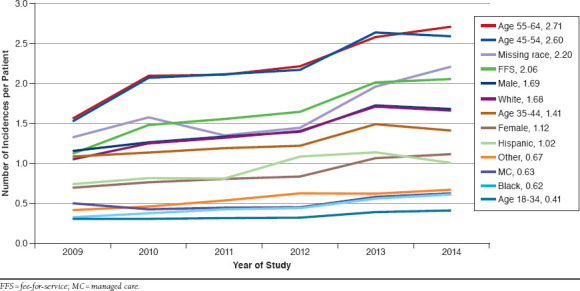
Average Number of Incidences of Indicators for Potential Inappropriate Prescriptions of Opioids per Patient by Insurance Type, Age, Gender, Race/Ethnicity and Year
The percentage of Medicaid enrollees with at least 1 or more indicators of potential inappropriate prescriptions slightly increased from 17.2% to 18.2% over the study period (Table 1). While the percentage of fee-for-service enrollees with at least 1 or more indicators of inappropriate prescriptions increased by 2.7% over the study period, the percentage of managed care enrollees with at least 1 or more indicators slightly decreased. Both percentages of male and female Medicaid enrollees with at least 1 or more indicators of inappropriate prescriptions increased over time, with male enrollees experiencing a higher percentage increase (1%) than female enrollees (0.8%). Among all age groups, the percentage of Medicaid enrollees with at least 1 or more indicators of potential inappropriate prescriptions increased among the older 2 age groups, with the oldest age group experiencing the largest percentage increase (2.7%), while it decreased for the younger 2 age groups. The percentage of Medicaid enrollees with indicators of potential inappropriate prescriptions was higher for the missing race group across all years compared with all other race groups, and the percentage increase over time was also higher among the missing race group (3.4%) compared with other race groups. The most common indicator of potential inappropriate prescriptions across all demographic groups and all years was opioid-benzodiazepine overlapping prescriptions, while opioid-opioid overlapping prescriptions ranked second. Results are shown in Appendix A (available in online article). While the number of individuals with opioid-benzodiazepine and opioid-opioid overlapping prescriptions increased from 2009 to 2014, the number of individuals with a high daily dose of opioids decreased from 2012 to 2014.
TABLE 1.
Individuals with at Least 1 or More Incidences of Inappropriate Prescribing Indicators by Demographic Characteristics and Year
| Demographic Group | Year of Study | Total | Mean (SD) | Range | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |||||
| Fee-for-service n = 318,496 | No. | 8,077 | 11,513 | 12,792 | 13,516 | 15,900 | 15,632 | 77,430 | 6.87 (8.60) | (1-137) |
| n | 34,112 | 51,784 | 55,701 | 57,256 | 60,437 | 59,206 | 318,496 | |||
| % | 23.68 | 22.23 | 22.97 | 23.61 | 26.31 | 26.40 | 24.31 | |||
| Managed care n = 436,126 | No. | 5,533 | 7,490 | 8,200 | 8,307 | 9,098 | 9,669 | 48,297 | 4.76 (6.13) | (1-109) |
| n | 45,161 | 75,726 | 78,863 | 78,393 | 78,273 | 79,710 | 436,126 | |||
| % | 12.25 | 9.89 | 10.40 | 10.60 | 11.62 | 12.13 | 11.07 | |||
| Male n = 151,728 | No. | 3,471 | 5,071 | 5,616 | 6,135 | 7,070 | 7,153 | 34,516 | 6.40 (8.30) | (1-115) |
| n | 15,040 | 24,112 | 26,201 | 27,475 | 29,213 | 29,687 | 151,728 | |||
| % | 23.08 | 21.03 | 21.43 | 22.33 | 24.20 | 24.09 | 22.75 | |||
| Female n = 602,894 | No. | 10,139 | 13,932 | 15,376 | 15,688 | 17,928 | 18,148 | 91,211 | 5.93 (7.61) | (1-137) |
| n | 64,233 | 103,398 | 108,363 | 108,174 | 109,497 | 109,229 | 602,894 | |||
| % | 15.78 | 13.47 | 14.19 | 14.50 | 16.37 | 16.61 | 15.13 | |||
| Age 18-34 (years) n = 424,818 | No. | 3,837 | 5,565 | 5,964 | 6,047 | 6,253 | 6,124 | 33,790 | 4.35 (6.23) | (1-109) |
| n | 44,586 | 76,434 | 78,710 | 77,175 | 75,190 | 72,723 | 424,818 | |||
| % | 8.61 | 7.28 | 7.58 | 7.84 | 8.32 | 8.42 | 7.95 | |||
| Age 35-44 (years) n = 134,457 | No. | 3,317 | 4,495 | 4,920 | 4,990 | 5,739 | 5,918 | 29,379 | 5.83 (7.37) | (1-137) |
| n | 14,079 | 21,679 | 22,974 | 23,738 | 25,061 | 26,926 | 134,457 | |||
| % | 23.56 | 20.73 | 21.42 | 21.02 | 22.90 | 21.98 | 21.85 | |||
| Age 45-54 (years) n = 105,419 | No. | 3,653 | 5,013 | 5,548 | 5,757 | 6,853 | 6,706 | 33,530 | 7.07 (8.57) | (1-106) |
| n | 11,742 | 16,582 | 18,163 | 18,773 | 20,017 | 20,142 | 105,419 | |||
| % | 31.11 | 30.23 | 30.55 | 30.67 | 34.24 | 33.29 | 31.81 | |||
| Age 55-64 (years) n = 89,928 | No. | 2,803 | 3,930 | 4,560 | 5,029 | 6,153 | 6,553 | 29,028 | 7.11 (8.56) | (1-121) |
| n | 8,866 | 12,815 | 14,717 | 15,963 | 18,442 | 19,125 | 89,928 | |||
| % | 31.62 | 30.67 | 30.98 | 31.50 | 33.36 | 34.26 | 32.28 | |||
| Hispanic n = 3,179 | No. | 53 | 87 | 91 | 113 | 101 | 96 | 541 | 5.60 (6.86) | (1-50) |
| n | 313 | 524 | 592 | 575 | 604 | 571 | 3,179 | |||
| % | 16.93 | 16.60 | 15.37 | 19.65 | 16.72 | 16.81 | 17.02 | |||
| Non-Hispanic, white n = 330,989 | No. | 9,256 | 12,443 | 12,993 | 12,853 | 13,845 | 13,558 | 74,948 | 6.37 (7.86) | (1-112) |
| n | 38,440 | 59,030 | 59,530 | 57,817 | 57,837 | 58,335 | 330,989 | |||
| % | 24.08 | 21.08 | 21.83 | 22.23 | 23.94 | 23.24 | 22.64 | |||
| Non-Hispanic, black n = 349,810 | No. | 3,262 | 4,800 | 5,644 | 5,854 | 6,962 | 6,962 | 33,484 | 5.01 (7.22) | (1-137) |
| n | 36,225 | 59,891 | 62,836 | 62,702 | 64,552 | 63,604 | 349,810 | |||
| % | 9.00 | 8.01 | 8.98 | 9.34 | 10.79 | 10.95 | 9.57 | |||
| Non-Hispanic, other n = 7,617 | No. | 82 | 124 | 128 | 149 | 145 | 169 | 797 | 5.47 (8.40) | (1-91) |
| n | 713 | 1,289 | 1,388 | 1,383 | 1,376 | 1,468 | 7,617 | |||
| % | 11.50 | 9.62 | 9.22 | 10.77 | 10.54 | 11.51 | 10.46 | |||
| Missing race n = 63,027 | No. | 957 | 1,549 | 2,136 | 2,854 | 3,945 | 4,516 | 15,957 | 6.84 (8.51) | (1-119) |
| n | 3,582 | 6,776 | 10,218 | 13,172 | 14,341 | 14,938 | 63,027 | |||
| % | 26.72 | 22.86 | 20.90 | 21.67 | 27.51 | 30.23 | 25.32 | |||
| Total N = 754,622 | No. | 13,610 | 19,003 | 20,992 | 21,823 | 24,998 | 25,301 | 125,727 | 6.06 (7.81) | (1-137) |
| n | 79,273 | 127,510 | 134,564 | 135,649 | 138,710 | 138,916 | 754,622 | |||
| % | 17.17 | 14.90 | 15.60 | 16.09 | 18.02 | 18.21 | 16.66 | |||
n = population; No. = number of individuals with inappropriate prescribing incidences; SD = standard deviation.
In addition to examining the number of individuals with indicators for potential inappropriate prescribing of opioids, we also examined the incidences of indicators for potential inappropriate prescribing of opioids, since an individual can experience multiple incidences during a given time period. The incidence rate of indicators for potential inappropriate prescribing of opioids increased over time across all demographic groups. Results are shown in Appendix B (available in online article). Fee-for-service and male enrollees experienced the largest increases in the incidence rate compared with managed care and female enrollees. The incidence rate was higher and quite close among the 2 older age groups (55-64 years and 45-54 years) across all years, while they also experienced higher increments in the incidence rate (1.14 and 1.06, respectively) from 2009 to 2014 compared with all other age groups. Among all race groups, incidence rate was higher among the missing race group across all years, and this group also experienced the largest increment in the incidence rate (0.87) over time compared with all other race groups.
Discussion: Given the high level of attention and scrutiny that has evolved in the United States associated with the prescribing of opioids, the finding that opioid utilization is continuing to increase in Georgia Medicaid enrollees is a concern. The average number of opioid prescriptions received by patients increased over time across all categories, yet this measure does not provide full insight into the nature of opioid use in this population. The increase in the number of opioid prescriptions may stem in part from prescribers attempting to work around policies limiting the quantity of opioids dispensed per prescription.
Specifically, greater numbers of opioid prescriptions might be written for smaller quantities of opioids per prescription to circumvent per prescription quantity limits. However, these results also confirm an increase in the average days supply, which compounds the issue of increasing numbers of opioid prescriptions. Further, and perhaps most significant from a clinical perspective, the average daily dose (MME) of opioids also increased. The implication of these trends (increased numbers of prescriptions, increased days supply, and increased daily dose) is that opioid use is increasing even with policy and societal pressure aimed at curbing marginal utilization.
Subgroup analyses identified that men, older patients, and fee-for-service patients are at the greatest risk when considering the amount of opioids provided to patients. In addition to older patients and men being at higher risk, this finding is of interest because it is possible that structural differences in the payment system (fee-for-service vs. managed care) could be affecting utilization. In particular, fee-for-service may be imposing safety measures (e.g., formulary status, limits on the numbers of prescriptions, or quantity per prescription) at the point of payment to curb opioid utilization. In contrast, managed care plans may use these same methods but employ additional strategies for patient education or shared decision making. The comparative effectiveness of fee-for-service strategy versus managed care strategy needs further evaluation.
With respect to missing race utilization, nearly all patients with missing race information were in the fee-for-service (84%) payment system, and the majority were female (64.5%). In Georgia, patients who do not select a preference between managed care and fee-for-service are placed into fee-for-service plans by default. One explanation for higher utilization of fee-for-service plans is that these patients may be more ill and require more care. In the study sample, higher proportions of fee-for-service patients reported chronic pain (64%), acute pain (47%), and OUD (3%) conditions compared with managed care patients reporting chronic pain (44%), acute pain (37%), and OUD (1.7%) conditions, respectively. However, less than one third of these patients were in the oldest age group (55-64 years), indicating that it is the younger age group that is experiencing higher utilization of opioids among the missing race group. These findings are inconsistent with the idea that the oldest age group is the least healthy group of patients. The implication is that the potential inappropriate use of opioids is taking place among younger, female individuals within the fee-for-service payment system.
These results indicate the percentage of individuals with indicators of potential inappropriate prescribing and the incidence rate of indicators of potential inappropriate prescribing of opioids increased over the study period. It is reassuring to know that slightly more than 4 out of 5 patients using opioids experienced utilization that falls under appropriate use and accepted prescribing practices with an expected result of attainment of clinical goals and positive outcomes. However, this still leaves a substantial number of individuals whose use of opioids could result in undesirable utilization and adverse health outcomes. The indicators of inappropriate prescribing practices examined in this study have been linked to opioid-related adverse health outcomes such as increased health care utilization, increased emergency department visits, and overdose deaths.14,15 Given these results, there is certainly a large cohort of patients who could benefit from better utilization of opioids.
The results of this analysis of trends in opioid use revealed increased utilization and inappropriate prescribing with opioid prescriptions between 2009 and 2014, which is contrary to the desired effect of policies that were implemented in Georgia limiting opioid use over this time period. Georgia Medicaid implemented formulary policy changes in April 2013 limiting the number of opioid prescriptions that a patient could receive per month (from having no limits to a 5-prescription-per-month limit). The refill-too-soon rate changed from 75% days supply to 85% days supply, along with the blocking of concomitant use of opioids and buprenorphine/naloxone. Understanding utilization trends in opioid use is critical to evaluating the effect of policies implemented over the last several years that were designed to curb the inappropriate use of these potent medications. Further, this understanding may be useful feedback for policymakers in both revising existing policy and developing new policies.
The goals of any opioid policy limiting utilization should include a reduction in marginal (unnecessary) utilization of opioids and the number of incidences of inappropriate prescribing of these medications. The trends noted in this study revealed disparities between insurance type (managed care vs. fee-for-service), with fee-for-service exhibiting more undesirable utilization than managed care. Further, males experienced the greatest increases in undesirable utilization. This implies that participation in managed care Medicaid could improve outcomes over fee-for-service. Yet, fee-for-service is the default insurance type for patients who do not select managed care or who do not make a choice in Georgia Medicaid. In addition to the insurance type, structural differences in the provision of care need to be evaluated (or controlled for in future research) to fully assess the effect of insurance type on patient outcomes and undesirable utilization.
Given the trends noted here, in conjunction with the fact that policy changes limiting opioid use were implemented during this time period, we must begin to think about other ways to reduce undesirable utilization. Patient and provider education may help in the quest to reduce undesirable utilization. For patients with chronic pain, management by a pain specialist or appropriate counseling may be advised. In cases where de-prescribing is an option, it should be considered. At the minimum, more education for prescribers and dispensers regarding initiating opioid therapy and concomitant therapy should be engaged. In particular, pharmacists have been shown to effectively affect the de-prescribing of benzodiazepines.16 Pharmacists are the last checkpoint in the system, are easily accessible to patients, and may be able to play an important role in the de-prescribing of opioids as well.
Limitations
While this study presents several contributions to the literature, such as examining disparities in trends of potential inappropriate prescribing practices and the general use of opioids across various demographic characteristics (age, gender, race/ethnicity, and type of insurance), it also has some limitations that should be noted. This study focused only on the Georgia Medicaid population aged 18-64 years during the 2009-2014 time period. Therefore, caution should be used when generalizing these results for application to other states or the national stage. Further, as patient, prescriber, and other stakeholder awareness of the potential problems associated with opioid use increases, these trends may change. In addition, there could be systematic differences between the Medicaid enrollees in 2009 and 2014 that could affect opioid use in this analysis. This study used pharmacy claims data for the analysis that showed only filled prescriptions. However, actual consumption of these drugs may vary from the prescriptions filled. Moreover, use of ICD-9-CM codes to identify diagnoses has its own limitations, since the type of pain may not have been reported or coded accurately.
Conclusions
Opioid use and potentially inappropriate prescribing continues to increase in the Georgia Medicaid population—even with policies aimed at reducing marginal utilization. Men, older patients, and fee-for-service patients are at the greatest risk when considering the amount of opioids provided to patients. The problem of potentially inappropriate prescribing is concerning because while most patients using opioids experienced utilization that falls under appropriate use and accepted prescribing practices, nearly 1 in 5 did not, leaving a substantial number of individuals whose use of opioids could result in undesirable utilization and adverse health outcomes. Further research is needed to identify the effect on health outcomes of policies aimed at reducing marginal utilization of opioids and why differences in use of opioids may exist between fee-for-service and managed Medicaid insurance types.
APPENDIX A. Indicators of Potential Inappropriate Prescribing by Number of Individuals
APPENDIX B. Number of Incidences of Potential Inappropriate Prescribing Practices by Demographic Characteristics and Year
| Demographic Group | Year of Study | Total | ||||||
|---|---|---|---|---|---|---|---|---|
| 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |||
| Fee-for-service n = 318,496 | Number of incidences | 38,641 | 77,235 | 86,448 | 94,235 | 121,682 | 121,810 | 540,051 |
| n | 34,112 | 51,784 | 55,701 | 57,256 | 60,437 | 59,206 | 318,496 | |
| IRPP | 1.13 | 1.49 | 1.55 | 1.65 | 2.01 | 2.06 | 1.70 | |
| Managed care n = 436,126 | Number of incidences | 22,870 | 32,251 | 35,378 | 35,455 | 45,380 | 50,361 | 221,695 |
| n | 45,161 | 75,726 | 78,863 | 78,393 | 78,273 | 79,710 | 436,126 | |
| IRPP | 0.51 | 0.43 | 0.45 | 0.45 | 0.58 | 0.63 | 0.51 | |
| Male n = 151,728 | Number of incidences | 16,003 | 30,323 | 34,572 | 39,312 | 50,398 | 50,161 | 220,769 |
| n | 15,040 | 24,112 | 26,201 | 27,475 | 29,213 | 29,687 | 151,728 | |
| IRPP | 1.06 | 1.26 | 1.32 | 1.43 | 1.73 | 1.69 | 1.46 | |
| Female n = 602,894 | Number of incidences | 45,508 | 79,163 | 87,254 | 90,378 | 116,664 | 122,010 | 540,977 |
| n | 64,233 | 103,398 | 108,363 | 108,174 | 109,497 | 109,229 | 602,894 | |
| IRPP | 0.71 | 0.77 | 0.81 | 0.84 | 1.07 | 1.12 | 0.90 | |
| Age 18-34 (years) n = 424,818 | Number of incidences | 14,334 | 23,448 | 24,948 | 24,960 | 29,407 | 29,930 | 147,027 |
| n | 44,586 | 76,434 | 78,710 | 77,175 | 75,190 | 72,723 | 424,818 | |
| IRPP | 0.32 | 0.31 | 0.32 | 0.32 | 0.39 | 0.41 | 0.35 | |
| Age 35-44 (years) n = 134,457 | Number of incidences | 15,201 | 24,743 | 27,259 | 28,836 | 37,158 | 38,044 | 171,241 |
| n | 14,079 | 21,679 | 22,974 | 23,738 | 25,061 | 26,926 | 134,457 | |
| IRPP | 1.08 | 1.14 | 1.19 | 1.21 | 1.48 | 1.41 | 1.27 | |
| Age 45-54 (years) n = 105,419 | Number of incidences | 18,067 | 34,400 | 38,626 | 40,750 | 52,767 | 52,340 | 236,950 |
| n | 11,742 | 16,582 | 18,163 | 18,773 | 20,017 | 20,142 | 105,419 | |
| IRPP | 1.54 | 2.07 | 2.13 | 2.17 | 2.64 | 2.60 | 2.25 | |
| Age 55-64 (years) n = 89,928 | Number of incidences | 13,909 | 26,896 | 30,993 | 35,144 | 47,730 | 51,857 | 206,529 |
| n | 8,866 | 12,815 | 14,717 | 15,963 | 18,442 | 19,125 | 89,928 | |
| IRPP | 1.57 | 2.10 | 2.11 | 2.20 | 2.59 | 2.71 | 2.30 | |
| Hispanic n = 3,179 | Number of incidences | 233 | 430 | 476 | 624 | 685 | 580 | 3028 |
| n | 313 | 524 | 592 | 575 | 604 | 571 | 3,179 | |
| IRPP | 0.74 | 0.82 | 0.80 | 1.09 | 1.13 | 1.02 | 0.95 | |
| Non-Hispanic, white n = 330,989 | Number of Incidences | 44,319 | 74,716 | 79,880 | 80,661 | 99,510 | 98,154 | 477,240 |
| N | 38,440 | 59,030 | 59,530 | 57,817 | 57,837 | 58,335 | 330,989 | |
| IRPP | 1.15 | 1.27 | 1.34 | 1.40 | 1.72 | 1.68 | 1.44 | |
| Non-Hispanic, black n = 349,810 | Number of incidences | 11,900 | 23,089 | 26,901 | 28,563 | 37,894 | 39,589 | 167,936 |
| n | 36,225 | 59,891 | 62,836 | 62,702 | 64,552 | 63,604 | 349,810 | |
| IRPP | 0.33 | 0.39 | 0.43 | 0.46 | 0.59 | 0.62 | 0.48 | |
| Non-Hispanic, other n = 7,617 | Number of incidences | 303 | 601 | 749 | 862 | 859 | 986 | 4,360 |
| n | 713 | 1,289 | 1,388 | 1,383 | 1,376 | 1,468 | 7,617 | |
| IRPP | 0.42 | 0.47 | 0.54 | 0.62 | 0.62 | 0.67 | 0.57 | |
| Missing race n = 63,027 | Number of incidences | 4,756 | 10,650 | 13,820 | 18,980 | 28,114 | 32,862 | 109,182 |
| n | 3,582 | 6,776 | 10,218 | 13,172 | 14,341 | 14,938 | 63,027 | |
| IRPP | 1.33 | 1.57 | 1.35 | 1.44 | 1.96 | 2.20 | 1.73 | |
| Total N = 754,622 | Number of incidences | 61,511 | 109,486 | 121,826 | 129,690 | 167,062 | 172,171 | 761,746 |
| n | 79,273 | 127,510 | 134,564 | 135,649 | 138,710 | 138,916 | 754,622 | |
| IRPP | 0.78 | 0.86 | 0.91 | 0.96 | 1.20 | 1.24 | 1.01 | |
IRPP = incidence rate per patient; n = population.
References
- 1.Mack KA, Zhang K, Paulozzi L, Jones C. Prescription practices involving opioid analgesics among Americans with Medicaid, 2010. J Health Care Poor Underserved. 2015;26(1):182-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Prescription opioid overdose data . August 1, 2017. Available at: https://www.cdc.gov/drugoverdose/data/overdose.html. Accessed June 28, 2018.
- 3.Henry J. Kaiser Foundation. Total Medicaid managed care enrollment. Report 2016. Available at: https://www.kff.org/medicaid/state-indicator/total-medicaid-mc-enrollment/?. Accessed June 28, 2018.
- 4.Garg RK, Fulton-Kehoe D, Franklin GM. Patterns of opioid use and risk of opioid overdose death among Medicaid patients. Med Care. 2017; 55(7):661-68. [DOI] [PubMed] [Google Scholar]
- 5.Liu Y, Logan JE, Paulozzi LJ, Zhang K, Jones CM. Potential misuse and inappropriate prescription practices involving opioid analgesics. Am J Manag Care. 2013;19(8):648-58. [PubMed] [Google Scholar]
- 6.Braden JB, Fan MY, Edlund MJ, Martin BC, DeVries A, Sullivan MD. Trends in use of opioids by noncancer pain type 2000-2005 among Arkansas Medicaid and HealthCore enrollees: results from the TROUP study. J Pain. 2008;9(11):1026-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sullivan MD, Edlund MJ, Fan MY, Devries A, Brennan Braden J, Martin BC. Trends in use of opioids for non-cancer pain conditions 2000-2005 in commercial and Medicaid insurance plans: the TROUP study. Pain. 2008;138(2):440-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jayawardhana J, Abraham AJ, Young HN, Perri M. Opioids in Georgia Medicaid: gender and insurance disparities in utilization and potential inappropriate prescribing practices. J Pharm Health Serv Res. 2018;9(2):101-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.White AG, Birnbaum HG, Rothman DB, Katz N. Development of a budget-impact model to quantify potential cost savings from prescription opioids designed to deter abuse or ease of extraction. Appl Health Econ Health Policy. 2009;7(1):61-70. [DOI] [PubMed] [Google Scholar]
- 10.Goldberg GA, Kim SS, Seifeldin R, Haberman M, Robinson D Jr. Identifying suboptimal management of persistent pain from integrated claims data: a feasibility study. Manag Care. 2003;12(8 Suppl Improving pain):8-13. [PubMed] [Google Scholar]
- 11.Parente ST, Kim SS, Finch MD, et al. Identifying controlled substance patterns of utilization requiring evaluation using administrative claims data. Am J Manag Care. 2004;10(11 Pt 1):783-90. [PubMed] [Google Scholar]
- 12.Utah Department of Health. Utah clinical guidelines on prescribing opioids for treatment of pain . 2009. Available at: http://health.utah.gov/prescription/pdf/guidelines/final.04.09opioidGuidlines.pdf. Accessed June 28, 2018. [DOI] [PubMed]
- 13.Agency Medical Directors’ Group. Interagency guideline on opioid dosing for chronic non-cancer pain: an educational aid to improve care and safety with opioid therapy, 2010 update . Available at: http://www.agencymeddirectors.wa.gov/files/opioidgdline.pdf. Accessed July 17, 2018.
- 14.Florence CS, Zhou C, Luo F, Xu L. The economic burden of prescription opioid overdose, abuse, and dependence in the United States, 2013. Med Care. 2016;54(10):901-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Vital signs: overdoses of prescription opioid pain relievers—United States , 1999-2008. MMWR Morb Mortal Wkly Rep. 2011;60(43):1487-92. [PubMed] [Google Scholar]
- 16.Tannenbaum C, Martin P, Tamblyn R, Benedetti A, Ahmed S. Reduction of inappropriate benzodiazepine prescriptions among older adults through direct patient education: the EMPOWER cluster randomized trial. JAMA Intern Med. 2014;174(6):890-98. [DOI] [PubMed] [Google Scholar]


