Abstract
Introduction
Michigan is one of three states that have implemented Health Risk Assessments (HRAs) for enrollees as a feature of its Medicaid expansion, the Healthy Michigan Plan. This study describes primary care providers’ (PCPs’) early experiences with completing HRAs with enrollees and examines provider- and practice-level factors that affect HRA completion.
Methods
All PCPs caring for ≥12 HMP enrollees (n=4,322) were surveyed from June to November 2015, with 2,104 respondents (55.5%). Analyses in 2016–2017 described provider knowledge, attitudes, and experiences with the HRA early in HMP implementation; multivariable analyses examined relationships of provider- and practice-level characteristics with HRA completion, as recorded in state data.
Results
Seventy-three percent of PCP respondents found HRAs very or somewhat useful for identifying and discussing health risks, although less than half (47.2%) found them very or somewhat useful for getting patients to change health behaviors. Most PCP respondents (65.3%) were unaware of financial incentives for their practices to complete HRAs. Nearly all PCPs had completed at least one HRA. The mean HRA completion rate (completed HRAs/number of HMP enrollees assigned to that PCP) was 19.6%; those who lacked familiarity with the HRA had lower completion rates.
Conclusions
Early in program implementation, HRA completion rates by PCPs were low and awareness of financial incentives limited. Most PCP respondents perceived HRAs to be very or somewhat useful in identifying health risks and about half of PCPs viewed HRAs as very or somewhat useful in helping patients to change health behaviors.
INTRODUCTION
Michigan received a Section 1115 waiver from the Centers for Medicare and Medicaid Services to expand Medicaid under the Affordable Care Act with cost sharing and healthy behavior incentives for beneficiaries. The Healthy Michigan Plan (HMP) began enrolling adults up to 138% of the Federal Poverty Level in April 2014.1 HMP enrollees are asked to complete a Health Risk Assessment (HRA) with questions on health characteristics and behaviors, and, in collaboration with their primary care provider (PCP), select healthy behaviors to pursue, such as getting an influenza vaccine or quitting smoking. Providers submit the HRA to the enrollee’s health plan, which forwards it to the state and can use the information to offer health programs to enrollees. The initial HRA form included a section for providers to document biometric data; this portion of the HRA was later removed.2 Primary care practices receive a financial incentive that varies by health plan: $15–$50 for each submitted HRA.3 Enrollees could receive a reduction in their cost sharing; early in implementation they could also receive $50 for completing the HRA.
Lack of provider knowledge of health behavior programs was a key reason for low participation rates in those programs among patients in Iowa’s Medicaid expansion.4 Few studies have examined how HRAs work in low-income or publicly insured populations,5–8 or the key role of providers.9–18 Michigan is one of three states that use a Section 1115 waiver to include HRAs; at least two other state Medicaid programs are awaiting HRA approval from the Centers for Medicare and Medicaid Services.19,20 As more states experiment with these risk assessments, understanding PCPs’ early experiences incorporating HRAs into practice could provide important insights. This mixed-methods study characterizes provider knowledge, attitudes, and experiences with the HRA early in HMP implementation, and analyzes relationships of provider-and practice-level characteristics with HRA completion.
METHODS
The details of PCP interviews and survey have been described previously.21 Briefly, 19 semi-structured interviews were conducted with PCPs from December 2014 to April 2015 to collect qualitative data on their attitudes and experiences. Interviewees included physicians (n=16) and non-physician practitioners (n=3) working in diverse practice types. Interviewees were asked about their knowledge of and experiences caring for patients with HMP coverage including changes in their practice. Interviews were audio-recorded and transcribed verbatim. These interviews informed survey design and provided quotes to illustrate common themes (Statistical Analysis section).
Study Sample
The cohort of PCPs was drawn in April 2015, 1 year after HMP implementation. HMP enrollment files in the Michigan Department of Health and Human Services (MDHHS) data warehouse identified all providers listed as the PCP for ≥12 HMP enrollees, which represents at least one enrollee per month during the first year of the program. This criterion was used to assure sampling of PCPs who had sufficient contact with HMP patients to respond to questions about their experiences with the HRA and other features of HMP. PCPs with <12 enrollees (n=2,813) were excluded yielding a population of 4,547 PCPs. After linking each National Provider Identifier with the Centers for Medicare and Medicaid Services National Plan and Provider Enumeration System data, the following were excluded: 161 PCPs with only a pediatric specialty, 35 PCPs with addresses >30 miles from the Michigan border, 25 PCPs with a National Provider Identifier that did not reflect an individual or active provider (20 organizational National Provider Identifier, four deactivated, one was invalid), and four physicians who were part of the HMP evaluation team. The surveyed cohort included the remaining 4,322 PCPs (3,686 physicians and 636 nurse practitioners and physician assistants) (Table 1).
Table 1.
Survey Respondent Characteristics
| Provider characteristics | n (%) |
|---|---|
| Sex | |
| Male | 1,165 (55.4) |
| Female | 939 (44.6) |
| Race | |
| White | 1,583 (79.3) |
| Black/African American | 93 (4.7) |
| Asian/Pacific Islander | 224 (11.2) |
| American Indian/Alaska Native | 10 (0.5) |
| Other | 86 (4.3) |
| Ethnicity | |
| Non-Hispanic/Latino | 1,978 (97.7) |
| Hispanic/Latino | 46 (2.3) |
| Provider type | |
| Physician | 1,750 (83.2) |
| Non-physician | 354 (16.8) |
| Specialty | |
| Family medicine | 1,123 (53.4) |
| Internal medicine | 507 (24.1) |
| Medicine‒Pediatrics | 67 (3.2) |
| General practice | 24 (1.1) |
| Obstetrics/Gynecology | 12 (0.6) |
| Nurse practitioner | 192 (9.1) |
| Physician’s assistant | 165 (7.8) |
| Other | 14 (0.7) |
| Board certification | 1,695 (81.6) |
| Yes | 1,695 (81.6) |
| No | 383 (18.4) |
| Years in practice | |
| <10 years | 520 (25.9) |
| 10‒20 years | 676 (33.7) |
| >20 years | 810 (40.4) |
| Practice characteristics | |
| ≤5 practitioners | 157 (57.5) |
| >6 practitioners | 855 (42.5) |
| Non-physician providers in practice | 1,275 (71.7) |
| Practice type | |
| Federally qualified health center | 311 (14.9) |
| University/Teaching hospital practice | 276 (13.1) |
| Non-teaching practice | 643 (30.7) |
| Predominant payer mix | |
| Private | 522 (27.4) |
| Medicaid/HMP | 686 (36.0) |
| Medicare | 645 (33.9) |
| Uninsured | 15 (0.8) |
| Mixed | 37 (1.9) |
| Location | |
| Non-urban | 520 (24.7) |
| Urban | 1,584 (75.3) |
HMP, Healthy Michigan Plan
Measures
The survey aimed to assess PCPs’ knowledge, attitudes, and experiences regarding the HRA. The survey included measures of PCP and practice characteristics and PCP experiences and perceptions drawn from prior national surveys. New items specific to HMP, including knowledge of the HRA, incentives for practices and patients, practice processes to complete and submit HRAs, and early experiences with HRAs, were developed from the PCP interviews and cognitively tested with PCPs.
The paper survey was mailed in June 2015 with a letter describing the project and the confidentiality of responses, a $20 bill, and paid-postage envelope. A fact sheet outlined HMP eligibility and program characteristics to help PCPs distinguish between HMP and traditional Medicaid coverage. Follow-up mailings were sent in August and September 2015 to non-respondents, and PCPs could complete an online version of the survey. Survey responses were supplemented with data from the MDHHS data warehouse, linked at the PCP level.
Statistical Analysis
Descriptive statistics characterized PCPs’ responses about their practices’ experience with completing HRAs. Bivariate relationships between practice characteristics and HRA experiences reported by respondents were assessed with Pearson chi-square tests. HRA completion rate was defined as the number of HRAs with PCP attestation in the data warehouse divided by the number of HMP enrollees per PCP. After conducting bivariate associations between PCP characteristics and survey responses and HRA completion rate, multivariable regression models further examined individual- and practice-level associations with HRA completion. Because the rate of HRA completion was non-normal, a two-part model was used first, using logistic regression to test the associations with any HRA completion, and linear regression with log link among PCPs who had at least one HRA completion (which excluded 132 PCPs with no HRA completions recorded). Finally, a generalized linear model with a gamma link was fitted including all PCP data. Predicted margins of HRA completion rates are presented from that analysis. Results were similar with both the two-part and generalized linear models. To address practice-level clustering where more than one PCP from a practice completed the survey, sensitivity analyses were performed for each regression model, adding practice ID as a random intercept in the model. Results from these analyses did not reveal any changes in significance or direction of associations. Quantitative analyses used Stata, version 14.
Semi-structured interviews were audio-recorded, transcribed, and coded iteratively by two or more researchers using grounded theory and standard qualitative analysis techniques, using Dedoose© software. As a government-mandated evaluation of a public program, this project was deemed exempt by the IRBs at the University of Michigan and the MDHHS.
RESULTS
Three of 19 PCP interviewees were nurse practitioners or physician assistants. Sixteen physicians included 14 in family medicine and two in internal medicine. Five interviewees had <10 years in practice, six had 10–20 years, and eight had >20 years. Five worked in Federally Qualified Health Centers (FQHCs), three in hospital-based practices, two in a free or low-cost clinic, seven in private practice, and two in rural health clinics.
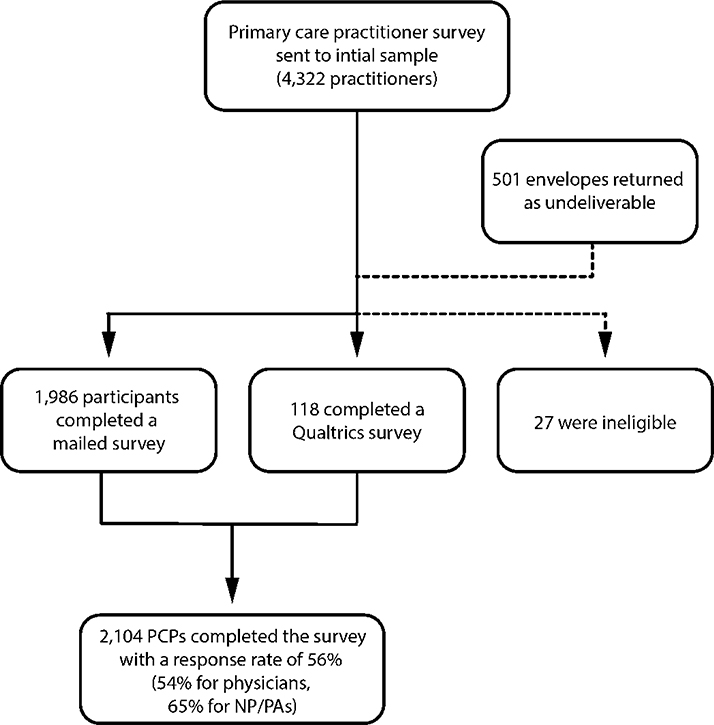
Of surveys sent to 4,322 PCPs (3,686 physicians and 636 nurse practitioners or physician assistants), 501 mailed surveys were returned as undeliverable. Of the remaining 3,821, a total of 27 PCPs were ineligible (e.g., retired, moved out of state) and 2,104 responded (1,986 mail, 118 online). The final response rate was 56% (54% for physicians, 65% for nurse practitioners/physician assistants) (Appendix Figure 2).
Slightly more than half of respondents (55.4%) were men and almost 80% self-identified as white (Table 1). Among respondents, 83.2% were physicians, although 71.7% had non-physician providers in their practice. About half identified their specialty as family medicine (53.4%) and a quarter (24.1%) as internal medicine. More than half (57.5%) were in practices with five or fewer providers; 14.9% practiced in FQHCs. Three quarters of PCP respondents (75.3%) practiced in urban settings, including 31.2% in the Detroit region. More than one third (36.0%) reported Medicaid/HMP as their predominant payer. Comparing the 2,104 respondents and 1,690 non-respondents revealed no significant differences in sex, age, number of affiliated Medicaid managed care plans, or practice in an FQHC. Non-respondents were more likely to have a rural practice and be internal medicine physicians.
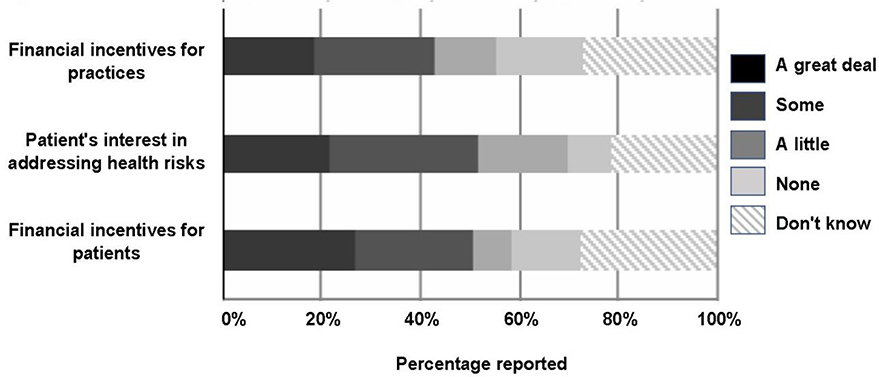
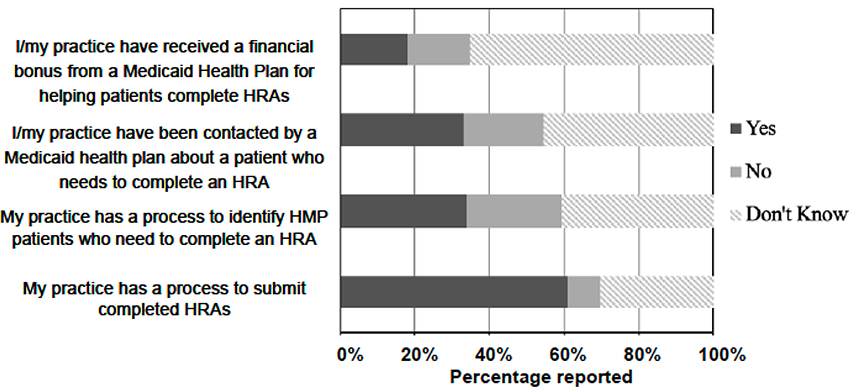
Most (61.2%) PCPs reported their practice had a process in place for submitting HRAs. One third (34.1%) reported their practice had a method of identifying patients who needed HRAs completed, while 40.7% did not know if their practice had a process for identifying patients who needed to complete an HRA (Appendix Figure 1). Nearly half (45.3%) did not know if they or their practice had been contacted by a health plan regarding HRA completion, and 65.3% did not know whether they or their practice had received a financial incentive for completing HRAs (Figure 1). PCPs were more likely to report their practice had a process to identify patients who needed to complete an HRA if their payer mix was predominantly uninsured (72.7%) or Medicaid (47.4%) compared with private (22.5%), Medicare (30.7%), or mixed (33.1%) (p<0.001), if they reported co-locating mental health within the previous year (47.5% vs 31.6% who did not report co-locating, p<0.001), or if they recalled they or their practice received an incentive for HRA completion (69.3% vs 26.4% for those who replied no or don’t know, p<0.001).
Figure 1.
Influence on primary care providers’ completion of Health Risk Assessments.
Notes: Not all survey questions were answered resulting in missing data. The number of responses per statement are as follows: My practice has a process to submit completed HRAs (n=2,041); My practice has a process to identify HMP patients who need to complete an HRA (n=2,042); I/my practice have been contacted by a Medicaid health plan about a patient who needs to complete an HRA (n=2,040); and I/my practice have received a financial bonus from a Medicaid health plan for helping patients complete HRAs (n=2,033).
Interviewees reflected that range
“I would have to say we have not really done a good job of accommodating it...it’s one of those, at the end of a visit, after-the-fact type of thing.…I’m thinking maybe one of the better ways to facilitate it is to actually ask the patient at the check-in, ‘Do they have any forms that need to be completed?’”
(Urban physician; large, hospital-based practice)
“I think the nurses help do it before I get in the room.”
(Rural physician, small private practice)
“Well, all of the plans are doing the health risk assessment, which is great and we’ve been able to set up a process here so that…If they’re patients that have been ours…we’re able to do the health risk assessment here with their first visit. If it’s a new patient, we do it at their second visit because we have some additional information that we can put into that to help set their goals.” (Urban physician, free/low-cost clinic)
The PCPs were typically involved in at least part of the process of HRA completion and discussion, although some just signed it.
“Eighty percent of the time I fill [the physician portion] out in the room with them, and then that leads to a conversation about some appropriate health screenings … whether or not we want to check their cholesterol or, ‘Okay, I’m just looking at your BMI here.’”
(Urban physician, FQHC)
Among PCP survey respondents, 79.4% reported completing at least one HRA with a patient; 43% of those reported completing more than ten (Appendix Table 1). About half of PCPs reported that financial incentives for patients (50.6%) or practices (42.9%) had some or a great deal of influence on completing HRAs. Slightly more than half of PCPs (51.6%) reported that patients’ interest in addressing health risks had some or a great deal of influence on PCPs’ completion of the HRA (Figure 1).
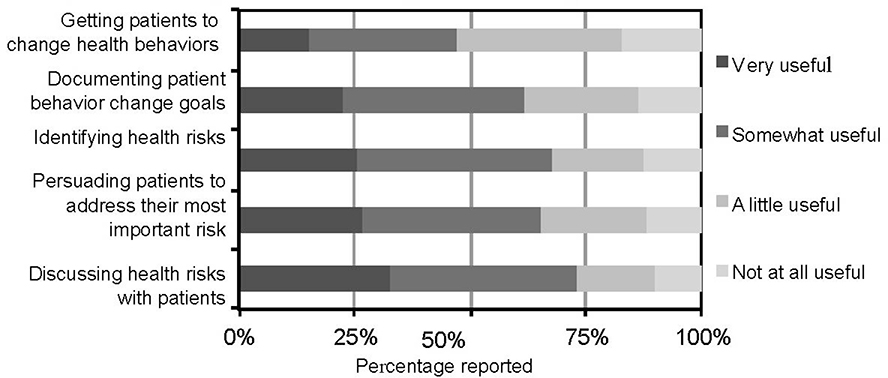
Most PCPs found HRAs very or somewhat useful for identifying and discussing health risks (73%), persuading patients to address their most important health risks (65.4%), and documenting behavior change goals (61.6%). About half (47.2%) found them very or somewhat useful for getting patients to change health behaviors (Figure 2).
Figure 2.
Primary care providers’ perceived utility of Health Risk Assessments.
Notes: Not all survey questions were answered resulting in missing data. The number of responses per statement are as follows: Getting patients to change health behaviors (n=1,828); Documenting patient behavior change goals (n=1,828); Identifying health risks (n=1,833); Persuading patients to address their most important health risk (n=1,826); and Discussing health risks with patients (n=1,821).
In Figure 3 in response to the question “How much influence do the following have on completion and submission of the Health Risk Assessment?”, the number of responses were as follows: “Financial incentives for patients” (n = 2046), “Patients’ interest in addressing health risks” (n = 2046), and “Financial incentives for practices” (n = 2044).
Many interviewed PCPs saw value in the completion of the HRA and discussion that it generated with patients.
“We usually will talk about strategies to improve their health. Usually with obesity, addressing some of the factors that may be contributing to obesity, cholesterol issues, and diabetes risk….Equally as high on the totem pole, I guess, would be tobacco use. We talk a lot about cessation, and I refer a lot of people over to Michigan Quitline as a result of us kind of sitting down and specifically talking about those kinds of areas of interest on the HRA forms.” (Urban physician assistant, FQHC)
“Having those tools to be able to help patients…do goal setting and move forward has been really helpful.”
(Urban physician, free/low-cost clinic)
Some PCPs saw little value in the HRA related to behavior change.
“So…Does this help me in a discussion with the patient? I don’t think so really whatsoever. Does it somehow tweak the patient that maybe they ought to get a flu shot this year? No. People either want it or they don’t want it. Like I said, filling out a questionnaire is not going to help them decide that kind of stuff, I don’t think.”
(Urban physician, free/low-cost clinic)
The mean HRA completion rate for surveyed PCPs was 19.6%. PCPs reporting private insurance as a dominant payer mix had slightly higher completion rates compared with those with a Medicaid predominant payer mix (21.3% vs 19.4%, p=0.05) (Table 2). PCPs practicing in urban settings had slightly lower completion rates that those practicing in other areas (19.7% vs 21.8%, p=0.02) (Table 2). A PCP was less likely to have recorded, in state data, any complete HRA (132 respondents) if their practice was located in an urban region (p=0.03), if Medicaid (p=0.05) or the uninsured (p=0.04) were the predominant payer, or if PCPs were a little or not familiar with completing HRAs (p<0.05) (Appendix Table 2).
Table 2.
Predicted HRA Completion Rates From GLM Regression
| Variable | Completion ratea (%) (95% CI) | p-value |
|---|---|---|
| PCP views of HRA | ||
| PCP familiarity with completing HRA | ||
| Very familiar | 23.3 (22.1, 24.4) | ‒ |
| Somewhat familiar | 18.2 (16.8, 19.5) | <0.001 |
| A little familiar | 17.0 (15.4, 18.6) | <0.001 |
| Not at all familiar | 13.7 (12.1, 15.2) | <0.001 |
| HRA useful for identifying health risks | ||
| Very useful | 18.9 (17.0, 20.9) | ‒ |
| Somewhat useful | 20.7 (19.4, 22.1) | 0.162 |
| A little useful | 20.5 (18.4, 22.6) | 0.357 |
| Not at all useful | 21.0 (16.8, 25.1) | 0.413 |
| HRA useful for discussing health risks | ||
| Very useful | 21.2 (18.8, 23.5) | ‒ |
| Somewhat useful | 19.8 (18.5, 21.1) | 0.334 |
| A little useful | 19.8 (17.5, 22.0) | 0.481 |
| Not at all useful | 20.5 (15.2, 25.8) | 0.841 |
| HRA useful for persuading patients to address risks | ||
| Very useful | 19.8 (17.6, 22.0) | ‒ |
| Somewhat useful | 19.8 (18.4, 21.1) | 0.986 |
| A little useful | 21.9 (19.7, 24.2) | 0.267 |
| Not at all useful | 19.6 (15.3, 24.0) | 0.951 |
| HRA useful for documenting patient behavior goals | ||
| Very useful | 18.5 (16.6, 20.5) | ‒ |
| Somewhat useful | 20.7 (19.3, 22.0) | 0.104 |
| A little useful | 20.8 (19.7, 22.6) | 0.145 |
| Not at all useful | 21.0 (17.5, 24.5) | 0.250 |
| HRA useful for getting patients to change behaviors | ||
| Very useful | 20.1 (17.0, 23.2) | ‒ |
| Somewhat useful | 20.7 (19.1, 22.2) | 0.761 |
| A little useful | 20.1 (18.8, 21.4) | 0.994 |
| Not at all useful | 19.8 (17.2, 22.5) | 0.900 |
| Provider and practice characteristics | ||
| Provider type | ||
| Non-physician | 21.0 (19.2, 22.8) | ‒ |
| Physician | 20.0 (19.2, 20.9) | 0.344 |
| Practice location | ||
| Non-urban | 21.8 (20.2, 23.3) | ‒ |
| Urban | 19.7 (18.8, 20.5) | 0.02 |
| Predominant payer mix | ||
| Private | 21.3 (20.0, 22.7) | ‒ |
| Medicaid | 19.4 (18.3, 20.6) | 0.05 |
| Medicare | 20.4 (18.7, 22.1) | 0.385 |
| Uninsured | 20.4 (12.7, 28.0) | 0.815 |
| Mixed | 19.2 (16.7, 21.7) | 0.171 |
Predicted HRA completion rates from GLM regression with gamma distribution. Link function was reciprocal and SEs calculated using the observed information matrix. Model predicts rate of completed HRAs using data warehouse records. Multivariate model was adjusted for all variables shown, as well as the number of HMP members assigned to the PCP.
PCP, primary care provider; HRA, health risk assessment; GLM, generalized linear model.
DISCUSSION
Approximately 18 months after the launch of the HMP, most PCPs had completed HRAs and reported value in doing so, with nearly three quarters reporting HRAs useful for identifying and discussing health risks, and nearly all having completed at least one HRA according to state records. A little less than half found them very or somewhat useful for getting patients to change health behaviors.
The role of frontline clinicians in health risk assessments has not been well studied.15 In one study, only one fifth of U.S. physician organizations routinely reported administering HRAs; information technology capacity and size and type of organization were associated with doing so.16 In the United Kingdom, uptake of the National Health Service Health Check, designed to address the high prevalence of cardiovascular disease among older adults, has been less than hoped, but has increased over time and seems to increased prescribing of statins.22 Studies have shown that HRAs are associated with positive health behavioral change if combined with individualized counseling and feedback.23,24 However, HRAs and promoting health behavior changes in patients can be challenging for PCPs, with time constraints commonly cited as a key factor.25–29 Importantly, the MDHHS streamlined the HRA form and submission process early in 2018 based on results of this survey and other feedback, which has improved completion rates.30 Lack of confidence in influencing health behaviors, lack of familiarity with the expectation and form, and incomplete integration of health risk assessment into practice processes also pose obstacles to broad uptake.
Practices with predominantly Medicaid or uninsured payer mixes were slightly less likely to have any completed HRAs, and practices with more privately insured patients had higher HRA completion rates. Although practices with more Medicaid patients could be expected to have greater familiarity with HMP and other Medicaid programs, well-resourced practices may be better positioned to quickly adopt new practices, or they may be more familiar with health risk assessments implemented by payers or employers. How payer mix relates to HRA completion is unclear and warrants further study.
Although financial incentives are often used to influence patient, clinician, and organizational behavior, several factors could potentially explain why PCPs did not view incentives as a strong motivator for HRA completion. First, at the time of this survey, most PCPs said they were not aware of receiving financial incentives for HRA completion. Second, the dollar amount of the incentives for PCPs to complete HRAs ($15–$50) may not have been large enough to encourage HRA completion. Prior research on financial incentives for providers to promote healthy behaviors has demonstrated mixed effects. One meta-analysis including trials on smoking cessation showed that financial incentives for providers had an effect on PCP behaviors, such as higher referral rates to counseling services, but had no effect on patient measures of cessation.31 A systematic review of diabetes trials conducted in the U.S. and other developed nations showed inconsistent effects of physician financial incentives on screening and improvement of HbA1c.32
Limitations
Self-reported survey data must be interpreted with some caution, because responses are susceptible to recall or social desirability bias.33 Results were from surveyed PCPs caring for at least 12 HMP enrollees, so they may not generalize to providers with fewer Medicaid patients. Because the survey occurred 15–18 months following implementation, these findings highlight early perspectives and experiences that may change over time, with greater experience with the HMP program and processes.
The HRA completion rate in Medicaid administrative data was lower than self-reported HRA completion, a difference that could be explained both by recall bias and by the possibility that HRA forms were not fully completed, or not submitted or received or recorded properly, perhaps due to the multistep process required to submit an HRA in the early years.
CONCLUSIONS
Eighteen months after the start of Michigan’s Medicaid expansion through the HMP, PCPs were often unaware of key aspects of the program’s HRA completion and submission process. Although financial incentives were available to both patients and providers, no more than half felt that these influenced HRA completion and a minority of PCPs believed that the HRA would lead to improved health behaviors.
Results highlight the challenges providers face when incorporating new aspects of Medicaid expansion into clinical practice in the early years of implementation and the need for policymakers to learn from clinicians before, during, and after program implementation, as the state of Michigan did.34 Medicaid managed care plans should also consider ways to improve engagement of PCPs and enrollees in HRAs, such as modifying financial incentives or promoting the potential for health improvement. Future research could assess how PCP understanding and experiences of the HRA have evolved, information that could be particularly important given completion of the HRA or a healthy behavior within the past year will be a requirement for continued enrollment for some HMP enrollees beginning in 2020.
ACKNOWLEDGMENTS
The University of Michigan Institute for Healthcare Policy and Innovation is conducting the evaluation required by the Centers for Medicare and Medicaid Services (CMS) of the Healthy Michigan Plan under contract with the Michigan Department of Health and Human Services (MDHHS). Data collected for this paper were funded by MDHHS and CMS for the purposes of the evaluation but do not represent the official views of either agency. The sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation of the manuscript; or the decision to submit the manuscript for publication.
Appendix Figure 1.
Primary care providers’ experiences with health risk assessments.
Appendix Figure 2.
Survey respondent participation.
Appendix Table 1.
Provider Experiences With Health Risk Assessments
| Variable | None | 1–2 | 3–10 | >10 |
|---|---|---|---|---|
| Approximately how many Health Risk Assessments have you completed with Healthy Michigan Plan Patients? (n=2,032) | 420 (20.7%) | 235 (11. 6%) | 503 (24.8%) | 874 (43.0%) |
| Almost always | Often | Sometimes | Rarely/never | |
| How often do your Healthy Michigan Plan patients bring in their Health Risk Assessment to complete at their initial office visit? (n=1,923) | 215 (11.2%) | 416 (21.6%) | 720 (37.4%) | 572 (29.7%) |
Appendix Table 2.
Predictors of Any HRA Completion by Provider and Practice Factors
| Variable | n | AOR (95% CI) | p-value |
|---|---|---|---|
| PCP familiarity with completing HRA | |||
| Very familiar | 928 | ‒ | |
| Somewhat familiar | 440 | 0.50 (0.20, 1.24) | 0.135 |
| A little familiar | 248 | 0.27 (0.10, 0.71) | 0.008 |
| Not at all familiar | 282 | 0.23 (0.07, 0.76) | 0.02 |
| HRA useful for identifying health risks | |||
| Very useful | 453 | ‒ | |
| Somewhat useful | 727 | 0.95 (0.27, 3.36) | 0.94 |
| A little useful | 347 | 3.41 (0.42, 27.75) | 0.251 |
| Not at all useful | 203 | 11.14 (0.35, 350.18) | 0.171 |
| HRA useful for discussing health risks | |||
| Very useful | 579 | ‒ | |
| Somewhat useful | 696 | 0.56 (0.13, 2.52) | 0.453 |
| A little useful | 288 | 0.04 (0.004, 0.485) | 0.01 |
| Not at all useful | 164 | 0.04 (0.004, 3.828) | 0.169 |
| HRA useful for persuading patients to address risks | |||
| Very useful | 464 | ‒ | |
| Somewhat useful | 674 | 2.95 (0.62, 14.06) | 0.174 |
| A little useful | 424 | 26.95 (2.87, 253.14) | 0.004 |
| Not at all useful | 229 | 8.34 (0.33, 210.86) | 0.198 |
| HRA useful for documenting patient behavior goals | |||
| Very useful | 391 | ‒ | |
| Somewhat useful | 683 | 0.71 (0.18, 2.84) | 0.628 |
| A little useful | 424 | 0.79 (0.14, 4.35) | 0.788 |
| Not at all useful | 229 | 1.32 (0.01, 17.34) | 0.835 |
| HRA useful for getting patients to change behaviors | |||
| Very useful | 267 | ‒ | |
| Somewhat useful | 551 | 1.03 (0.25, 4.19) | 0.963 |
| A little useful | 620 | 0.87 (0.19, 3.94) | 0.857 |
| Not at all useful | 284 | 0.28 (0.03, 2.50) | 0.257 |
| Provider type | |||
| Non-physician | 315 | ‒ | |
| Physician | 1,657 | 0.89 (0.40, 2.01) | 0.781 |
| Practice location | |||
| Non-urban | 488 | ‒ | |
| Urban | 1,484 | 0.39 (0.17, 0.93) | 0.03 |
| Predominant payer mix | |||
| Private | 610 | ‒ | |
| Medicaid | 640 | 0.42 (0.18, 0.99) | 0.05 |
| Medicare | 393 | 1.34 (0.54, 3.33) | 0.534 |
| Uninsured | 11 | 0.05 (0.003, 0.830) | 0.04 |
| Mixed | 133 | 0.71 (0.18, 2.84) | 0.628 |
Notes: The number of responses to each statement varies based on the PCP self-report. Adjusted logistic regression with ORs predicting any completion of HRA from data warehouse records. Multivariate model was adjusted for all variables shown, as well as the number of HMP members assigned to the PCP.
PCP, primary care provider; HRA, health risk assessment.
Footnotes
No conflict of interest or financial disclosures were reported by any of the authors of this paper.
REFERENCES
- 1.Ayanian JZ. Michigan’s approach to Medicaid expansion and reform. N Engl J Med. 2013;369(19):1773–1775. 10.1056/nejmp1310910. [DOI] [PubMed] [Google Scholar]
- 2.Michigan Department of Health & Human Services . Healthy Michigan Plan: Updated Health Risk Assessment. www.michigan.gov/documents/mdhhs/HMP_HRA_FACT_SHEET_619607_7.pdf. Accessed August 26, 2019.
- 3.Michigan Primary Care Association . Health Risk Assessment (HRA) Instructions from Medicaid Health Plans. https://1pdf.net/download/healthy-michigan-plan-health-risk-assessment-hra-_58e4f30af6065dc0643631f8 Published July 8, 2014. Accessed June 14, 2018.
- 4.Askelson NM, Wright B, Bentler S, Momany ET, Damiano P. Iowa’s Medicaid expansion promoted healthy behaviors but was challenging to implement and attracted few participants. Health Aff (Millwood). 2017;36(5):799–807. 10.1377/hlthaff.2017.0048. [DOI] [PubMed] [Google Scholar]
- 5.Bradley CJ, Neumark D. Small cash incentives can encourage primary care visits by low-income people with new health care coverage. Health Aff (Millwood). 2017;36(8):1376–1384. 10.1377/hlthaff.2016.1455. [DOI] [PubMed] [Google Scholar]
- 6.Haisley E, Volpp KG, Pellathy T, Loewenstein G. The impact of alternative incentive schemes on completion of health risk assessments. Am J Health Promot. 2012;26(3):184–188. 10.4278/ajhp.100729-arb-257. [DOI] [PubMed] [Google Scholar]
- 7.Pham HH, Schrag D, Hargraves JL, Bach PB. Delivery of preventive services to older adults by primary care physicians. JAMA. 2005;294(4):473–481. 10.1001/jama.294.4.473. [DOI] [PubMed] [Google Scholar]
- 8.Seaverson ELD, Grossmeier J, Miller TM, Anderson DR. The role of incentive design, incentive value, communications strategy, and worksite culture on health risk assessment participation. Am J Health Promot. 2009;23(5):343–352. 10.4278/ajhp.08041134. [DOI] [PubMed] [Google Scholar]
- 9.Petersen LA, Simpson K, Pietz K, et al. Effects of individual physician-level and practice-level financial incentives on hypertension care: a randomized trial. JAMA. 2013;310(10):1042–1050. 10.1001/jama.2013.276303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mantzari E, Vogt F, Shemilt I, Wei Y, Higgins JPT, Marteau TM. Personal financial incentives for changing habitual health-related behaviors: a systematic review and meta-analysis. Prev Med (Baltim). 2015;75:75–85. 10.1016/j.ypmed.2015.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Redmond P, Solomon J, Lin M. Can incentives for healthy behavior improve health and hold down Medicaid costs? www.cbpp.org/research/can-incentives-for-healthy-behavior-improve-health-and-hold-down-medicaid-costs Published June 1, 2007. Accessed October 31, 2019.
- 12.Carlfjord S, Lindberg M, Andersson A. Staff perceptions of addressing lifestyle in primary health care: a qualitative evaluation 2 years after the introduction of a lifestyle intervention tool. BMC Fam Pract. 2012;13:99 10.1186/1471-2296-13-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shaw RL, Pattison HM, Holland C, Cooke R. Be SMART: examining the experience of implementing the NHS Health Check in UK primary care. BMC Fam Pract. 2015;16:1 10.1186/s12875-014-0212-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu RR, Orlando LA, Himmel TL, et al. Patient and primary care provider experience using a family health history collection, risk stratification, and clinical decision support tool: a type 2 hybrid controlled implementation-effectiveness trial. BMC Fam Pract. 2013;14:111 10.1186/1471-2296-14-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Simpson V, Pedigo L. Nurse and physician involvement in health risk appraisals: an integrative review. West J Nurs Res. 2017;39(6):803–824. 10.1177/0193945916660341. [DOI] [PubMed] [Google Scholar]
- 16.Halpin HA, Mcmenamin SB, Schmittdiel J, et al. The routine use of health risk appraisals: results from a national study of physician organizations Am J Health Promot. 2005;20(1):34–38. 10.4278/0890-1171-20.1.34. [DOI] [PubMed] [Google Scholar]
- 17.Ahmad F, Skinner HA, Stewart DE, Levinson W. Perspectives of family physicians on computer-assisted health-risk assessments. J Med Internet Res. 2010;12(2):e12 10.2196/jmir.1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Luquis RR, Paz HL. Attitudes about and practices of health promotion and prevention among primary care providers. Health Promot Pract. 2015;16(5):745–755. 10.1177/1524839914561516. [DOI] [PubMed] [Google Scholar]
- 19.Contreary K, Miller R. Incentives to Change Health Behaviors: Beneficiary Engagement Strategies in Indiana, Iowa, and Michigan. www.mathematica-mpr.com/our-publications-and-findings/publications/incentives-to-change-health-behaviors-beneficiary-engagement-strategies-in-indiana-iowa-and-michigan. Published August 1, 2017. Accessed September 12, 2019.
- 20.Henry J Kaiser Family Foundation. Medicaid Waiver Tracker: Which States Have Approved and Pending Section 1115 Medicaid Waivers? [Google Scholar]
- 21.Goold SD, Tipirneni R, Kieffer E, et al. Primary care clinicians’ views about the impact of Medicaid expansion in Michigan: a mixed methods study. J Gen Intern Med. 2018;33(8):1307–1316. 10.1007/s11606-018-4487-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Robson J, Dostal I, Sheikh A, et al. The NHS Health Check in England: an evaluation of the first 4 years. BMJ Open. 2016;6(1):e008840 10.1136/bmjopen-2015-008840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stuck AE, Moser A, Morf U, et al. Effect of health risk assessment and counselling on health behaviour and survival in older people: a pragmatic randomised trial. PLoS Med. 2015;12(10):e1001889 10.1371/journal.pmed.1001889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Colkesen EB, Ferket BS, Tijssen JGP, Kraaijenhagen RA, van Kalken CK, Peters RJG. Effects on cardiovascular disease risk of a web-based health risk assessment with tailored health advice: a follow-up study. Vasc Health Risk Manag. 2011;7(1):67–74. 10.2147/vhrm.s16340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Geense WW, Van De Glind IM, Visscher TLS, Van Achterberg T. Barriers, facilitators and attitudes influencing health promotion activities in general practice: an explorative pilot study. BMC Fam Pract. 2013;14:20 10.1186/1471-2296-14-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rubio-Valera M, Pons-Vigués M, Martínez-Andrés M, Moreno-Peral P, Berenguera A, Fernández A. Barriers and facilitators for the implementation of primary prevention and health promotion activities in primary care: a synthesis through meta-ethnography. PLoS One. 2014;9(2):e89554 10.1371/journal.pone.0089554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dean CA, Arnold LD, Hauptman PJ, Wang J, Elder K. Patient, physician, and practice characteristics associated with cardiovascular disease preventive care for women. J Womens Health. 2017;26(5):491–499. 10.1089/jwh.2015.5613. [DOI] [PubMed] [Google Scholar]
- 28.Hooper LM, Epstein SA, Weinfurt KP, et al. Predictors of primary care physicians’ self-reported intention to conduct suicide risk assessments. J Behav Health Serv Res. 2012;39(2):103–115. 10.1007/s11414-011-9268-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aspy CB, Mold JW, Thompson DM, et al. Integrating screening and interventions for unhealthy behaviors into primary care practices. Am J Prev Med. 2008;35(5 suppl):S373–S380. 10.1016/j.amepre.2008.08.015. [DOI] [PubMed] [Google Scholar]
- 30.Michigan Department of Health and Human Services. Healthy Michigan Plan §1115 Demonstration Waiver Extension Request Amendment: Attachment B, Revised Healthy Behaviors Incentive Protocol. www.michigan.gov/documents/mdhhs/Attachment_B_-Revised_Healthy_Behaviors_Incentive_Protocol-Clean_632146_7.pdf. Accessed October 31, 2019.
- 31.Scott A, Sivey P, Ait Ouakrim D, et al. The effect of financial incentives on the quality of health care provided by primary care physicians. Cochrane Database Syst Rev. 2011;(9):CD008451 10.1002/14651858.cd008451.pub2. . [DOI] [PubMed] [Google Scholar]
- 32.Jackson T, Shields MD, Heaney LG, et al. The impact of financial incentives on the implementation of asthma or diabetes self-management: a systematic review. PLoS One. 2017;12(11):e0187478 10.1371/journal.pone.0187478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hunger M, Schwarzkopf L, Heier M, Peters A, Holle R. Official statistics and claims data records indicate non-response and recall bias within survey-based estimates of health care utilization in the older population. BMC Health Serv Res. 2013;13:1 10.1186/1472-6963-13-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Michigan Department of Health and Human Services. Medical Services Administration Bulletin: MI Marketplace Option and Healthy Michigan Plan Updates. www.michigan.gov/documents/mdhhs/MSA_18-05_615825_7.pdf. Published 2018. Accessed October 31, 2019.