Abstract
The effectiveness of acupuncture in the treatment of dry eye has been confirmed, but the association between acupoint selection and therapeutic effect has remained to be elucidated. In the present study, a systematic review and meta-analysis were performed to evaluate the effect of periocular acupoints and periocular acupoints plus body acupoints compared with AT for the treatment of dry eye disease (DED). The PubMed, Cochrane Library, Embase, Ovid, China National Knowledge Infrastructure and Chonqing VIP Information, Co., Ltd. databases were searched with entries until 10 July 2018 considered. Only randomized controlled trials (RCTs) were included. Meta-analyses were performed to compare the effects of acupuncture with those of conventional treatment (including AT or other non-acupuncture therapies). The primary outcomes, including tear break-up time (BUT), Schirmer's I test (SIT) result and Symptom scores were analyzed. Subgroup analysis was performed for periocular acupoints only and periocular acupoints plus body acupoints. A total of 12 studies comprising 900 participants were included. In the primary meta-analysis, a significant improvement in the BUT [n=1,209, weighted mean difference (WMD)=1.01, 95% CI: 0.56-1.84, P<0.00001], SIT result (n=1,107, WMD=1.98, 95% CI: 0.44-3.34, P<0.00001) and Symptom scores (n=402, WMD=-1.02, 95% CI: -1.33 to -0.72, P<0.00001) was obtained to evaluate the clinical efficacy of acupuncture and AT. Furthermore, periocular acupoints plus body acupoints were more effective in the treatment of DED. However, the total sample size of subjects with only periocular acupoints in the treatment of DED was too small to get any firm conclusions. Further large RCTs are warranted.
Keywords: acupoint selection, dry eye, meta-analysis, systematic review, acupuncture
Introduction
In 2017, the Tear Film and Ocular Surface Society International Dry Eye Workshop II revised the definition of dry eye disease (DED) and pointed out that its major pathology includes tear film instability, hyperosmolarity, ocular surface inflammation, damage and neurosensory abnormalities (1). Multiple risk factors for the development of dry eye have been repeatedly identified, including increasing age and female sex (particularly post-menopausal females) (2,3) long-term contact lens wear, (4) months after laser-assisted in situ keratomileusis (LASIK), (5) prolonged use of video display screens, (6,7) and exposure to dry environments (8). Due to the decrease of tear film stability and the high osmolarity of tears, patients may complain of burning, pricking, foreign bodies, tearing, eye fatigue and dryness (9,10).
DED has been one of the most common and prevalent eye disorders for which ophthalmological intervention is sought (11). Several studies have revealed that the prevalence of DED ranges from 2 to 50% in different regions of the world, with a higher incidence among older adults and females, particularly menopausal and post-menopausal females (4,12-14). With the excessive use of video display terminals (VDT), the number of patients with DED has consistently increased in recent years (15,16). As the population ages and the use of VDTs increases, the direct and indirect cost of managing DED exerts enormous pressure on the health care system (17). It has been reported that the annual economic burden of DED in the US is 55.4 billion dollars (18).
Belmonte and Gallar (19) reported that weakening of nerve stimulation function and a decrease in tear secretion produced corneal surface dryness. Decreased tear secretion, coupled with loss of epithelial cell viability, leads to a decrease in ocular surface neurotrophins. Nerve growth factor, a vital component of neurotrophins, is essential for the development and survival of sympathetic neurons. It also has a significant role in nutritional support after nerve injury (20). Tear evaporation has a crucial role in the pathogenesis of DED. It decreases the corneal temperature and repeatedly stimulates the cold-sensitive corneal nerves. Continuous long-term stimulation changes the function of thermal sensors to nociceptors (pain sensors) (21).
Acupuncture is widely known as one of the common forms of complementary and alternative medicine. A large number of randomized controlled trials (RCTs) and systematic reviews have indicated that acupuncture is effective in the treatment of various conditions, including vomiting, dental pain, chronic pain, lower back pain and eye disease (22-25). In addition, several systematic reviews have confirmed that acupuncture is effective for DED (26-28). Lee et al (26) reported that the effect of acupuncture on dry eye was better than that of artificial tears (AT) as indicated by the results of Schirmer's I test (SIT), tear break up time (BUT) test, response rate and corneal fluorescein staining (CFS). The study by Kim et al (27) is principally based on the analysis of results of SIT, BUT and Ocular Surface Disease Index (OSDI) (28), and confirmed that acupuncture was more effective than AT in the treatment of dry eye. Subgroup analysis was also performed to further prove the efficacy of acupuncture. Yang et al (29) indicated the effectiveness of acupuncture in the treatment of dry eye by comparing the results of SIT and the BUT prior to and after treatment. Acupuncture has been proven to promote the secretion of tears, relieve discomfort and improve visual function by modulating ocular surface inflammation in DED (30,31). However, to the best of our knowledge, no systematic summary of the therapeutic effect of multi-acupoint selection on DED has so far been provided. Therefore, a systematic review and meta-analysis were performed in the present study to evaluate the efficacy of periocular acupoints, as well as periocular acupoints plus body acupoints, with the latest literature on DED. On this basis, it was attempted to determine the optimal acupoints for acupuncture treatment of DED.
Materials and methods
Databases and search strategy
The PubMed, Cochrane Library, Embase, Ovid, China National Knowledge Infrastructure (CNKI), Chonqing VIP Information, Co., Ltd. (CQVIP) and Wanfang databases were searched from inception through to 10 July 2018. CNKI, CQVIP and Wanfang are Chinese databases. The following medical search terms were used: ‘dry eye’, ‘dry eye syndrome’, ‘ophthalmoxerosis’, ‘keratoconjunctivitis sicca’, ‘xerophthalmia’, ‘acupuncture’, ‘electroacupuncture’, ‘Gan Yan’ (DED), ‘Gan Yan Zheng’ (DED), ‘Zhen Jiu’ (acupuncture and moxibustion), ‘Zhen Ci’ (acupuncture) and ‘Dian Zhen’ (electroacupuncture). To identify additional articles, reference lists of selected reviews and studies were manually searched. There were no language restrictions.
Study selection
The two authors independently selected eligible studies and discussed any emerging inconsistencies amongst each other. The specific study inclusion criteria were as follows: i) RCTs of patients with DED; ii) acupuncture or electroacupuncture compared with several alternatives, including AT, other non-acupuncture therapies or conventional treatment; iii) acupuncture treatment combined with other interventions (including AT or other non-acupuncture therapies) and comparison with the other interventions; iv) outcomes included SIT results, BUT, Symptoms score, CFS and visual analogue scale (VAS); and v) full text available.
Studies fulfilling the following criteria were excluded: i) Participants with Sjögren's syndrome; ii) acupuncture combined with other treatments, including Chinese herbal, warming-promotion needling and moxibustion, including thunder-fire miraculous moxa; ii) control group treated with acupuncture therapy only or combined with other interventions (including AT or other non-acupuncture therapies); iv) animal studies or studies lacking a control group, or articles published as case reports, reviews, commentaries or letters.
Data extraction and risk of bias assessment
Two independent reviewers (QBW, N D) read the full texts of all selected articles and used a standardized collection form to extract the following content: First author name and year of publication, participant information, sample size, study selection (inclusion and exclusion criteria), treatment protocol (acupoints, duration, treatment sessions and frequency of treatment) and major outcome data (BUT, SIT results, Symptoms score, CFS, OSDI and VAS).
The risk-of-bias assessment of the included RCTs was independently performed according to the Cochrane Collaboration Tool (31). The following items were included in the risk-of-bias assessment: Random sequence generation, allocation concealment, blinding (participants and personnel, outcome assessment), incomplete outcome data, selective reporting and other biases (31). Two reviewers (QBW, ND) independently assessed the quality of the articles and discussed any emerging inconsistencies with a third reviewer (JJW).
Data synthesis and statistical methods
The statistical software Review Manager 5.3 for Windows (provided by the Cochrane Collaboration) was applied for data synthesis and statistical analysis. To evaluate the effect of acupoint selection on DED, the weighted mean difference (WMD) with 95% CIs were used to analyze subgroup continuous data. Heterogeneity in studies was assessed using the χ2 test and Higgins I2 test (32). A fixed-effect model was used for homogeneity (considered significant at P>0.1); a random-effect model was used for heterogeneity (P<0.1).
Results
Search results
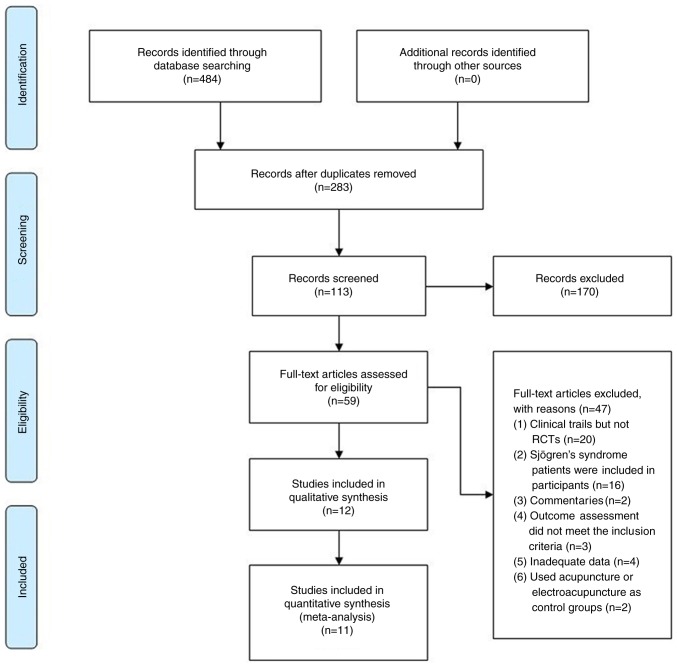
A total of 484 entries of potential relevance were identified from the database search. After excluding duplicate studies, screening of article titles and abstracts, 59 potentially relevant studies were retrieved. After reviewing the full texts, 47 studies were excluded for the following reasons: i) Clinical trials but not RCTs (n=20); ii) studies including patients Sjögren's syndrome as participants (n=16); iii) commentaries (n=2); iv) outcome assessment did not meet the inclusion criteria (n=3); v) inadequate data (n=4); vi) acupuncture or electroacupuncture used in the control groups (n=2). A flow diagram of the literature search and study selection process is presented in Fig. 1.
Figure 1.
Flow diagram of the study selection process. RCT, randomized controlled trial.
Study characteristics
A total of 12 studies with 900 participants were included in this review. A majority of the studies compared manual acupuncture with AT (33-43). An applied form of acupuncture was used in 4 of the studies, including 1 study using silver spike point electro-therapy (35), 1 study using electroacupuncture (44) and 2 studies using combined acupuncture at the phenomaxillary ganglia with acupoints (41,42). Participants in the study by Zeng et al (40) were patients who experienced DED for >1 month after LASIK. Furthermore, 2 studies focused on DED in post-menopausal or peri-menopausal females (38,43). Regarding the sensation of acupoints, 4 studies reported on de-qi (soreness, numbness, sensation of heaviness or swelling) associated with the needling (35,37,40,44). A total of 10 of the studies were performed in China (34-36,38-44). Detailed descriptions of the studies and the acupuncture treatments are provided in Tables I and II.
Table I.
Baseline characteristics of the randomized controlled trials included in the meta-analysis that investigated the effects of acupuncture in dry eye disease.
| First author (year) | Country | Sample sizea | Gender (M/F) | Mean age (range) | Duration (m or y)b | Treatment regime in intervention group | Treatment regime in control group | Major outcomes | (Refs.) |
|---|---|---|---|---|---|---|---|---|---|
| Nepp (1998) | Austria | 52 (30/22) | NA | NA | NA | Acupuncture | AT | BUT, SIT, drop frequency | (33) |
| Wang (2005) | China | 45 (15/15/15) | Intervention 1 (7/8) Intervention 2 (5/10) Control (5/10) | Intervention 1 51.7 (27-75) Intervention 2 51.8 (24-74) Control 51.5 (30-73) | Intervention 1 6m-10y Intervention 2 6m-10y Control 2m-10y | Acupuncture | AT | BUT, SIT, and CFS | (34) |
| Tseng (2006) | China (Taiwan) | 43 (17/17/9) | Intervention 1 (4/13) Intervention 2 (6/11) Control (6/3) | Intervention 1 52.24 Intervention 2 47.58 Control 51.33 | Intervention 1 2.65±1.80 y Intervention 2 3.24±3.17 y Control 4.00±3.35 y | Intervention 1: SSP + AT, Intervention 2: Acupuncture + AT | AT | BUT, SIT, VAS, overall score of eye condition | (35) |
| Shi (2012) | China | 68 (33/35) | Intervention (14/19) Control (16/19) | Intervention 47.4 (29-63) Control 51.4 (27-65) | NA | Acupuncture | AT | ST, BUT, tear lactoferrin concentration | (36) |
| Kim (2012) | South Korea | 150 (75/75) | Intervention (22/53) Control (19/56 | Intervention 47.95 Control 46.05 | NA | Acupuncture | AT | OSDI, VAS, BUT, SIT, QOL | (37) |
| Liao (2013) | China | 40 (0/40) | Intervention (0/20) Control (0/20) | Intervention 52.7 (45-55) Control 53.1 (45-55) | NA | Acupuncture + AT | AT | BUT, SIT, symptoms score, VRQOL | (38) |
| Nan (2014) | China | 60 (30/30) | Intervention (12/18) Control (13/17 | Intervention 48.57 (24-68) Control 47.56 (22-66) | Intervention 9.15 m (2 m-8 y) Control 10.55 m (3 m-9 y) | Eye acupuncture + AT | AT | ST, BUT, total score | (39) |
| Zeng (2014) | China | 52 (28/24) | Intervention (13/15) Control (11/13 | Intervention 33 (28-41) Control 31 (27-39) | Intervention 4-14 Control 6-18m | Acupuncture + AT | AT | BUT, SIT, FLS | (40) |
| Shang (2015) | China | 148 (72/76) | Intervention (40/32) Control (38/38 | Intervention 38 (24-61) Control 40 (21-64) | Intervention 4.3 y (3 m-19 y) Control 4.6y(2m-22y) | Acupuncture | AT | Symptoms score, VAS | (41) |
| Xiang (2016) | China | 88 (44/44) | Intervention (20/24) Control (16/28) | Intervention 34.27 (20-64) Control 36.11 (22-59) | Intervention 15.07 (3-48) m Control 13.30 (3-48) m | Acupuncture | AT | OSDI, BUT, SIT, FLS | (42) |
| Liu (2017) | China | 28 (14/14) | Intervention (0/14) Control (0/14) | Intervention 60.714 Control 60.786 | Intervention 3.857±3.225y Control 3.786±3.011y | Acupuncture + AT | AT | SIT, BUT, OSDI, scores of symptoms and signs, protein analysis | (43) |
| Huang (2013) | China | 126 (64/62) | Intervention (23/41) Control (20/42) | Intervention 42.32 (19-62) Control 41.18 (20-61) | Intervention 6.08 (1-15) m Control 5.17 (1-14) m | Electroacupuncture | AT | Symptoms score, BUT, SIT, FLS | (43) |
aSample size (number in intervention group/number in control group). NA, not available; AT, artificial tears; SIT, Schirmer's I test; BUT, tear break-up time; CFS, corneal fluorescein staining; OSDI, ocular surface disease index; VAS, Visual Analogue Scale; QOL, Quality of Life; VRQOL, vision-related quality of life; SSP, silver spike point; M, male; F, female; m, months; y, years.
bDuration: median (range), mean ± SD, range.
Table II.
Details of acupuncture treatment characteristics of the randomized controlled trials included in the present meta-analysis.
| First author (year) | Acupoints | Treatment frequency | Therapeutic course | Duration of acupuncture (min) | Insertion depth | Needle type | De-qi | (Refs.) |
|---|---|---|---|---|---|---|---|---|
| Nepp (1998) | Periocular acupoints: GB 1, BL 2, EX-HN2; other acupoints: ST 5, LI 4, SI 3, LI 3, KI 6, TE 5 | Intervention: 1 time per week; Control: NA | Intervention: 10 weeks Control: NA | 30 | NA | NA | NA | (33) |
| Wang (2005) | Acupuncture 1: Heat ablaze and yin injury: LI 11, LI 4, SP 6, KI 3, ST 2, LI 20; Phlegm and blood | Intervention 1: Once in 2 days, 10 times/course, 10 days' rest after; | Intervention 1: 3 courses; Intervention 2: a course | 20-25 | NA | NA | NA | (34) |
| stasis: ST 2, SP 10, SP 9, ST 36, SP 6, ST 40; Acupuncture 2: BL 2, TE 23, GB 14, ST 1 | Intervention 2: Once in 2 days, 10 times/course, 10 days rest after a; course Control: 5 times a day | 3 courses; Control: 30 days | ||||||
| Tseng (2006) | Periocular acupoints: EX-HN5, TE 23, GB 14, ST 2; other acupoints: SP 6 | Intervention 1: Twice a week, 2-3 days apart; Intervention 2: Twice a week, 2-3 days apart; Control: NA | Intervention 1: 8 weeks; Intervention 2: 8 weeks; Control: NA | 20 | NA | Points on the face: No. 36 one-inch needles, the lower extremities: No. 32 two-inch needles | De-qi | (35) |
| Shi (2012) | Periocular acupoints: ST 1, BL 1, EX-HN 5, TE 23; other acupoints: GV 20, LI 4, ST 36 | Intervention: 3 times per week; Control: 3-4 times a day | Intervention: 3 weeks; Control: 3 weeks | 25 | NA | 40x0.25 mm disposable acupuncture needles | NA | (36) |
| Kim (2012) | Periocular acupoints: ST 1, BL 2, TE 23, GB 14, Ex 1, GV 23; other acupoints: GB 20, LI 4, LI 11 | Intervention: 3 times per week; Control: Use as required (at least once per day) | Intervention: 4 weeks; Control: 4 weeks | 20 | The acupuncture points at the face and head: 0.6 to 3 cm, and 3 to 4.5 cm for points of hand (LI 4) and arm (LI 11). | 0.20x30 mm disposable acupuncture needles | De-qi | (37) |
| Liao (2013) | Periocular acupoints: BL 1, ST 1, TE 23 penetrating EX-HN4; other acupoints: KI 3, LR 3, SP 6, ST 36 | Intervention: 1 time a day; Control: 4 times a day | Intervention: 14 days; Control: 14 days | 30 | NA | NA | NA | (38) |
| Nan (2014) | Eye acupuncture (liver area, gallbladder area, kidney area, spleen stomach area, upper jiao area) | Intervention: 1 time a day; Control: 5 times a day | Intervention: 20 days; Control: 20 days | 15-20 | Liver area and gallbladder area: 0.5 cun | 0.18x13 mm disposable acupuncture needles | NA | (39) |
| Zeng (2014) | Periocular acupoints: GB 1, BL 1, LI 20, BL 2, ST 2, EX-HN5; other acupoints: SP 6, SP 10, ST 36, KI 3 | Intervention: Acupuncture 1 time a day, Tears Naturale II 3 times a day, Refresh plus 1 time a day; Control: Tears Naturale II 3 times a day, Refresh Plus 1 time a day | Intervention: 10 days; Control: 10 days | NA | BL 1: 0.5 cun, GB 1: 0.7 cun | NA | De-qi | (40) |
| Shang (2015) | Periocular acupoints: phenomaxillary ganglia, BL 1, EX-HN5, ST 2 | Intervention: acupuncture 1 time per week; Control: AT 1 time a day | Intervention: 24 weeks; Control: 15 days | NA | Phenomaxillary ganglia: 55 mm | Phenomaxillary ganglia: 0.35x60 mm needles | De-qi | (41) |
| Xiang (2016) | Periocular acupoints: phenomaxillary ganglia, BL 2, Shangjingming (Extra), TE 23, ST 2 | Intervention: First week: Continuous acupuncture 5 times, and the rest 2 weeks: 3 times a week (1 time every other day); Control: AT 4 times a day | Intervention: 3 weeks; Control: 3 weeks | 30 | Phenomaxillary ganglia: 50 mm | Phenomaxillary ganglia: 0.25x60 mm, periocular acupoints: 0.25x25 mm | De-qi | (42) |
| Liu (2017) | Periocular acupoints: BL 1, BL 2, TE 23, EX-HN5, ST 2, ST 1; other acupoints: LI 4, GB 20, GV 20 | Intervention: Acupuncture three times a week, AT: NA; Control: NA | Intervention: 8 weeks; Control: 8 weeks | 30 | NA | NA | NA | (43) |
| Huang (2013) | Periocular acupoints: EX-HN5, ST 1, BL 1, BL 2, Ex-HN7; the acupoints: LU 7, GB 37, KI 3, LR 3; Ex-HN5 and ST 1 were connected to EA apparatus | Intervention: 1 time a day; Control: 4 times a day | Intervention: 30 times; Control: 30 times | 30 | NA | 40 mm disposable acupuncture needles | De-qi | (44) |
Total sample size (number in intervention group/number in control group); NA, not available/not specified; AT, artificial tears; EA, electroacupuncture.
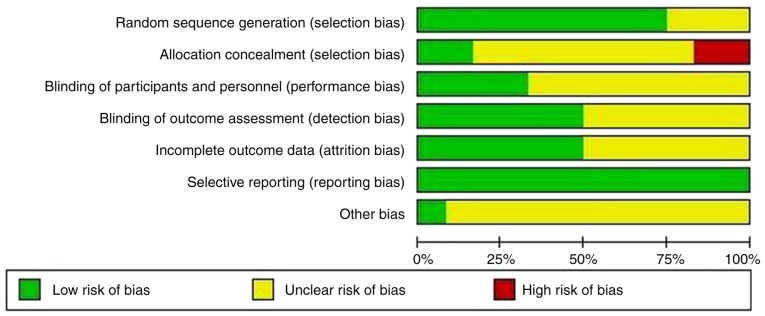
Risk-of-bias assessment
The results of the risk-of-bias assessment are summarized in Figs. 2 and 3. No serious risk of bias was detected. All studies included in the systematic review and meta-analysis mentioned randomization. Furthermore, 9 studies described the method of random sequence generation (using a random number Table or a computerized random-number generator) (34,36-42,44). Clear and adequate allocation concealment was performed in only two studies (35,37) and assessor blinding was used in six studies (33,36,37,41-43). Sufficient details of drop-out rates and reasons were described in six studies (35-39,41). Bias was suspected in two studies that did not mention the intervention time in the control group (33,35).
Figure 2.
Risk of bias graph.
Figure 3.
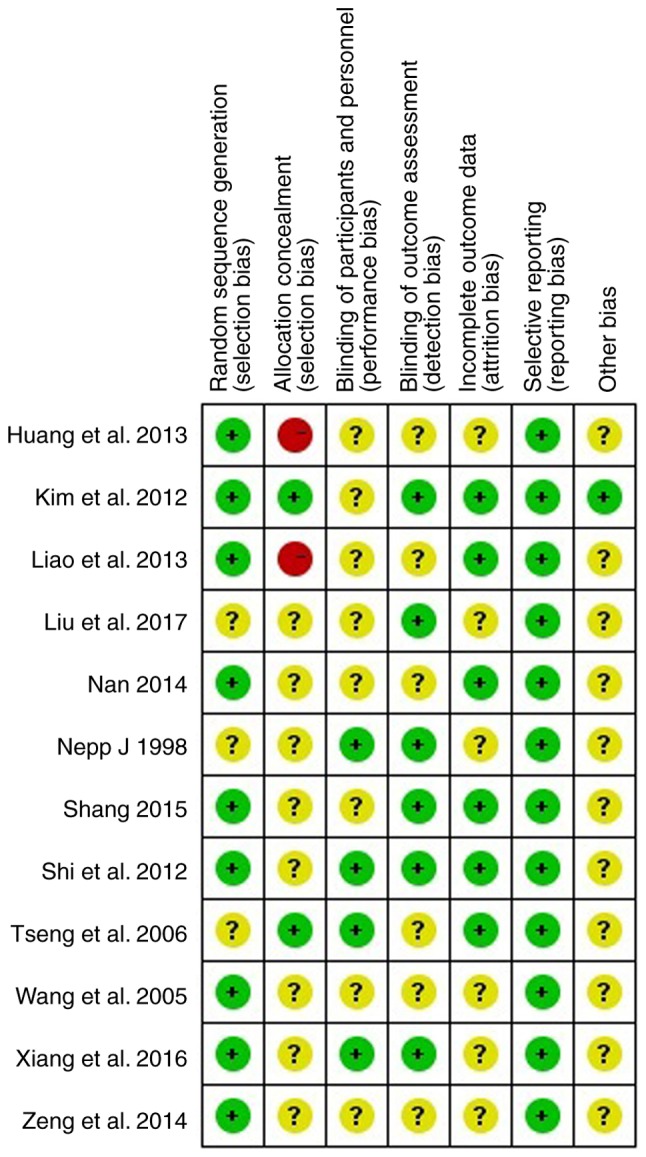
Risk of bias summary.
Meta-analysis for comparison between periocular acupoints and periocular acupoints plus body acupoints with AT
The study by Nepp et al (33) was excluded from the present meta-analysis, as it contained no detailed data except a graph. Therefore, the results of 11 of 12 studies were used to analyze BUT, SIT results and Symptoms score.
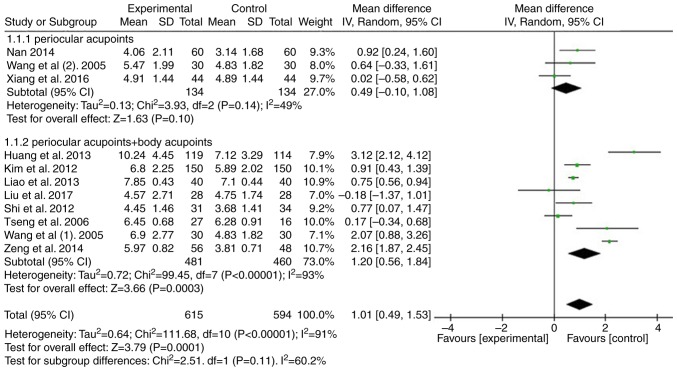
A total of 10 studies were analyzed to compare the effect of periocular acupoints or periocular acupoints plus body acupoints with those of AT in patients with DED in terms of the results of the BUT test (34-40,42-44). Compared with the AT group, significant improvement was identified among the acupuncture groups (n=1,209, WMD=1.01, 95% CI: 0.49-1.53, P=0.0001). Of note, subgroup analysis indicated no significant advantage of periocular acupoint intervention (P=0.10), but there was a significant difference in periocular acupoints plus body acupoint intervention (P=0.0003; Fig. 4).
Figure 4.
Forest plot for comparison of BUT between acupuncture and artificial tears. BUT, tear break-up time; IV, inverse variance; SD, standard deviation; df, degrees of freedom.
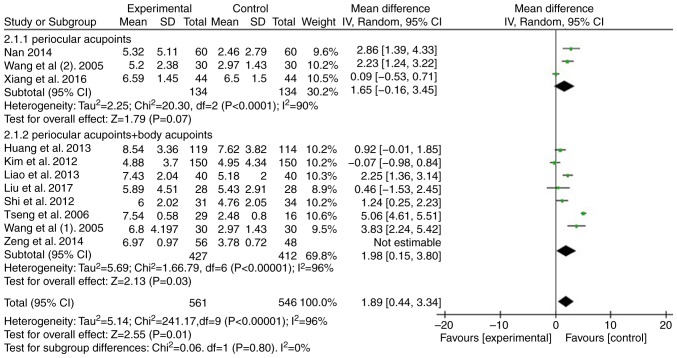
For the results of the SIT, 10 studies were used to compare the effect of periocular acupoints or periocular acupoints plus body acupoints with those of AT in patients with DED (34-40,42-44). Compared with the AT group, significant improvement was determined among the acupuncture groups (n=1,107, WMD=1.98, 95% CI: 0.44-3.34, P=0.01). The subgroup analysis indicated no significant difference in periocular acupoint intervention (P=0.07), but there was a significant difference in periocular acupoints plus body acupoints intervention (P=0.03; Fig. 5).
Figure 5.
Forest plot for comparison of SIT results between acupuncture and artificial tears. IV, inverse variance; SD, standard deviation; df, degrees of freedom; SIT, Schirmer's I test.
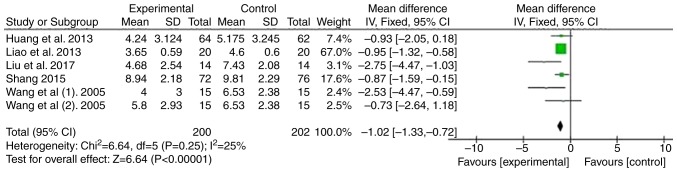
In addition, five studies were used to evaluate the Symptoms score (34,38,39,42,44). Compared with the AT group, the results indicated a significant difference among acupuncture groups (n=402, WMD=-1.02, 95% CI: -1.33 to -0.72, P<0.00001; Fig. 6).
Figure 6.
Forest plot for comparison of symptoms score between acupuncture and artificial tears. IV, inverse variance; SD, standard deviation; df, degrees of freedom.
Discussion
The purpose of the present systematic review and meta-analysis was to analyze the difference between each acupuncture modality group (periocular acupoints group and periocular acupoints plus body acupoints group) and the AT group. Although previous systematic reviews and meta-analyses have confirmed that acupuncture may effectively relieve DED (26-28), to the best of our knowledge, the present study was the first systematic review evaluating the therapeutic effects of multi-acupoint acupuncture on DED. In comparison with previous studies, stricter inclusion and exclusion criteria were adopted. After the selection process, the studies included were compared with those of the previous meta-analyses. Certain studies included in the previous meta-analyses were not included in the present study. The entire text of those studies was read and they were found unsuitable, principally because they included patients with Sjogren's syndrome and non-randomized controlled clinical trials. The present systematic review and meta-analysis initially included 11 RCTs comprising 848 patients with DED. The overall results indicated that acupuncture significantly improved the BUT, SIT results and Symptom scores compared with AT.
Although there are numerous predisposing factors and various clinical manifestations of DED, the major pathologies include hyperosmolarity, ocular surface inflammation and damage, tear film instability and neurosensory abnormalities (1). Tear film osmolarity has an important role in the pathogenesis of DED. It varies with the changes in internal and external factors, including body hydration, tear film stability, environmental conditions, blink interval, eyelid opening width and characteristics of tear film lipid layer (45). An increase in the osmolarity of the tear film is mainly caused by its excessive evaporation and reduced tear production (46-48). Exposure to tears with high osmolarity may lead to apoptosis of cells, loss of goblet cells, and dysfunction in corneal and conjunctival mucin expression. In addition, tear hyperosmolarity may activate a series of inflammatory events and contribute to further morphological changes in the cornea and conjunctiva. These changes may aggravate tear film instability and persistence of the condition (45,49,50).
In the theory of Traditional Chinese Medicine, acupoints are specific points that reflect the internal state of the body and regulate its function (51). The major purpose of acupoint stimulation includes the regulation of local and systemic effects. In the present study, the additional effect of stimulation of body acupoints in other parts of the body besides the periocular acupoints was examined, mainly for the purpose of distinguishing between the local therapeutic effects and remote sensing therapeutic effects. Histological investigations have confirmed that the local acupoints may be composed of the following parts: High-density nerve endings, high concentration of nerve and vascular elements, and mast cells, which have the function of perceiving stimuli (52). Zhang et al (53) proved that the skin resistance of acupoints in healthy individuals is significantly lower than that in non-acupoint areas. When the acupoints are stimulated, local biological molecules may be released, thus having a role in regulating the local effects (54). Studies have confirmed that acupuncture stimulates the afferent nerves of the skin and muscle at acupoints, and the somatic sensory information is then transmitted to the cerebral cortex and different nuclei of the brain stem and hypothalamus. At the same time, it may regulate the autonomic function of the body (55,56). Therefore, the combination of periocular acupoints and the body acupoints not only increases the local effects but also increases the local therapeutic effects but also increases the remote sensing therapeutic effects, which is more conducive to the treatment of dry eye.
Acupuncture therapy has a long history in the treatment of ophthalmic diseases. Systematic reviews have confirmed that acupuncture is effective in the treatment of myopia, amblyopia and optic atrophy (57-59). In recent decades, the use of acupuncture therapy for the treatment of DED has aroused interest and its efficacy has been actively explored (60). Although acupuncture treatment of dry eye has yielded encouraging results, rigorous clinical trials are required to confirm its therapeutic effect (26). Numerous studies have confirmed that acupuncture is useful for the treatment of dry eye, but the mechanism of action remains elusive. It is thought that acupuncture stimulates the lacrimal gland to secrete tears (61), promote corneal wound healing (62), reduce tension and reduce pain intensity or increase the pain threshold (63), regulate the autonomic nervous system and immune system (64,65), reduce local inflammatory response (43) and increase the flow velocity of the ophthalmic artery (66). Most of the acupuncture treatments for dry eye are based on the acupoints around the eyes, but there is no further research on the selection of acupoints. The most commonly used periocular acupoints include EX-HN5, BL1, GB1, BL2, ST1 and TE23.
Most clinicians still rely on conventional diagnostic tests, including the BUT test and SIT, for the diagnosis of DED (67). The measurement of tear film stability is usually performed by the BUT test (28), while the tear capacity is reflected by the SIT. Most patients seek ophthalmological intervention due to ocular discomfort. Although DED is usually diagnosed based on symptoms, there is no correlation between symptoms and signs of DED. The ability to quantify ocular surface symptoms helps to establish an additional medical assessment for dry eye. They have a critical guiding role in monitoring the development of DED and the prognosis after treatment (28). Therefore, in the present meta-analysis, the BUT, SIT results and Symptoms score were used as the outcome indexes, which may reflect the effect of acupuncture treatment from different angles. The present meta-analysis indicated that the BUT and SIT result of patients with DED exhibited statistically improvement in the acupuncture group, and the treatment effect of periocular acupoints plus body acupoints was more efficient than that using periocular acupoints only. At the same time, the present meta-analysis indicated that the symptoms score of patients with DED exhibited statistically improvement in the acupuncture group.
The present study indicated that the acupuncture group exhibited significant improvements in BUT, SIT result and Symptoms score compared with those in the control group. However, high heterogeneity was noted in the BUT (I2=91%) and SIT results (I2=96%). To reduce the heterogeneity of the present results, the studies were screened more strictly than in previous meta-analyses, excluding those studies on patients with Sjögren's syndrome and on acupuncture combined with other treatments, including moxibustion, Chinese herbal medicine, warming-promotion needling or thunder-fire miraculous moxa. However, the problem of high heterogeneity was not completely resolved. Different acupuncturists, different AT and the frequency of AT administration are important contributors to the high heterogeneity and affect the evaluation of the present results.
The present systematic review and meta-analysis has several limitations. The RCTs included in the present study exhibited a variation in acupuncture intervention programs (including acupoint selection, duration of treatment and course of treatment) and patient characteristics (including age, sex, ethnicity, environment and severity of DED). Due to insufficient data from RCTs, it was impossible to perform in-depth investigations of specific changes. Thus, individual patient data are required for future meta-analyses. Further limitations include the lack of standard protocols and the lack of high-quality RCTs. Only three studies reported on adverse reactions to acupuncture in the treatment of dry eye (36,37,40). Follow-up evaluation of acupuncture treatment for dry eye is necessary (37). Although the present study confirmed that acupuncture is more effective than AT, the latter has the advantage of being convenient to use, while needling is time-consuming and inconvenient for most patients with DED. A previous study indicated that the effect of acupuncture lasts longer than that of AT (37). Further large-cohort studies are required to confirm the long-term efficacy of acupuncture treatment.
In conclusion, the present meta-analysis revealed that in terms of BUT and SIT results, the effect of acupuncture is better than AT. However, due to the relatively small sample size, short treatment duration, lack of a sham-acupuncture control and insufficient observation of long-term efficacy, further large-sample RCTs are required to evaluate the efficacy of acupuncture in the treatment of DED.
Acknowledgements
Not applicable.
Funding
The present study was funded by the National Natural Science Foundation of China (grant no. 81774419).
Availability of data and materials
All data generated or analyzed during this study are included in this published article
Authors' contributions
Conception and design: WPG and QBW. Literature search and data extraction: QBW, WW, ND and JJW. Drafting of the manuscript: QBW and WW. Data interpretation and research supervision: WPG. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Craig JP, Nichols KK, Akpek EK, Caffery B, Dua HS, Joo CK, Liu Z, Nelson JD, Nichols JJ, Tsubota K, Stapleton F. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15:276–283. doi: 10.1016/j.jtos.2017.05.008. [DOI] [PubMed] [Google Scholar]
- 2.Sriprasert I, Warren DW, Mircheff AK, Stanczyk FZ. Dry eye in postmenopausal women: A hormonal disorder. Menopause. 2016;23:343–351. doi: 10.1097/GME.0000000000000530. [DOI] [PubMed] [Google Scholar]
- 3.Qiu X, Gong L, Sun X, Jin H. Age-related variations of human tear meniscus and diagnosis of dry eye with Fourier-domain anterior segment optical coherence tomography. Cornea. 2011;30:543–549. doi: 10.1097/ICO.0b013e3181fb84ea. [DOI] [PubMed] [Google Scholar]
- 4.Gayton JL. Etiology, prevalence, and treatment of dry eye disease. Clin Ophthalmol. 2009;3:405–412. doi: 10.2147/opth.s5555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Donnenfeld ED, Ehrenhaus M, Solomon R, Mazurek J, Rozell JC, Perry HD. Effect of hinge width on corneal sensation and dry eye after laser in situ keratomileusis. J Cataract Refract Surg. 2004;30:790–797. doi: 10.1016/j.jcrs.2003.09.043. [DOI] [PubMed] [Google Scholar]
- 6.Moon JH, Lee MY, Moon NJ. Association between video display terminal use and dry eye disease in school children. J Pediatr Ophthalmol Strabismus. 2014;51:87–92. doi: 10.3928/01913913-20140128-01. [DOI] [PubMed] [Google Scholar]
- 7.Nakamura S, Kinoshita S, Yokoi N, Ogawa Y, Shibuya M, Nakashima H, Hisamura R, Imada T, Imagawa T, Uehara M, et al. Lacrimal hypofunction as a new mechanism of dry eye in visual display terminal users. PLoS One. 2010;5(e11119) doi: 10.1371/journal.pone.0011119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iyer JV, Lee SY, Tong L. The dry eye disease activity log study. ScientificWorldJournal. 2012;2012(589875) doi: 10.1100/2012/589875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Terry MA. Dry eye in the elderly. Drugs Aging. 2001;18:101–107. doi: 10.2165/00002512-200118020-00003. [DOI] [PubMed] [Google Scholar]
- 10.Begley CG, Chalmers RL, Abetz L, Venkataraman K, Mertzanis P, Caffery BA, Snyder C, Edrington T, Nelson D, Simpson T. The relationship between habitual patient-reported symptoms and clinical signs among patients with dry eye of varying severity. Invest Ophthalmol Vis Sci. 2003;44:4753–4761. doi: 10.1167/iovs.03-0270. [DOI] [PubMed] [Google Scholar]
- 11.Craig JP, Nelson JD, Azar DT, Belmonte C, Bron AJ, Chauhan SK, de Paiva CS, Gomes JAP, Hammitt KM, Jones L, et al. TFOS DEWS II report executive summary. Ocul Surf. 2017;15:802–812. doi: 10.1016/j.jtos.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 12.McCarty CA, Bansal AK, Livingston PM, Stanislavsky YL, Taylor HR. The epidemiology of dry eye in Melbourne, Australia. Ophthalmology. 1998;105:1114–1119. doi: 10.1016/S0161-6420(98)96016-X. [DOI] [PubMed] [Google Scholar]
- 13.Lu P, Chen X, Liu X, Yu L, Kang Y, Xie Q, Ke L, Wei X. Dry eye syndrome in elderly Tibetans at high altitude: A population-based study in China. Cornea. 2008;27:545–551. doi: 10.1097/ICO.0b013e318165b1b7. [DOI] [PubMed] [Google Scholar]
- 14.Hashemi H, Khabazkhoob M, Kheirkhah A, Emamian MH, Mehravaran S, Shariati M, Fotouhi A. Prevalence of dry eye syndrome in an adult population. Clin Exp Ophthalmol. 2014;42:242–248. doi: 10.1111/ceo.12183. [DOI] [PubMed] [Google Scholar]
- 15. Golden MI, Fries PL and Patel BC (Eds): Dry eye syndrome. StatPearls Publishing, Treasure Island, FL, 2019. [PubMed] [Google Scholar]
- 16.Rossi GCM, Scudeller L, Bettio F, Pasinetti GM, Bianchi PE. Prevalence of dry eye in video display terminal users: A cross-sectional Caucasian study in Italy. Int Ophthalmol. 2019;39:1315–1322. doi: 10.1007/s10792-018-0947-6. [DOI] [PubMed] [Google Scholar]
- 17.Miljanović B, Dana R, Sullivan DA, Schaumberg DA. Impact of dry eye syndrome on vision-related quality of life. Am J Ophthalmol. 2007;143:409–415. doi: 10.1016/j.ajo.2006.11.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yu J, Asche CV, Fairchild CJ. The economic burden of dry eye disease in the United States: A decision tree analysis. Cornea. 2011;30:379–387. doi: 10.1097/ICO.0b013e3181f7f363. [DOI] [PubMed] [Google Scholar]
- 19.Belmonte C, Gallar J. Cold thermoreceptors, unexpected players in tear production and ocular dryness sensations. Invest Ophthalmol Vis Sci. 2011;52:3888–3892. doi: 10.1167/iovs.09-5119. [DOI] [PubMed] [Google Scholar]
- 20.Sacchetti M, Lambiase A. Neurotrophic factors and corneal nerve regeneration. Neural Regen Res. 2017;12:1220–1224. doi: 10.4103/1673-5374.213534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Belmonte C, Brock JA, Viana F. Converting cold into pain. Exp Brain Res. 2009;196:13–30. doi: 10.1007/s00221-009-1797-2. [DOI] [PubMed] [Google Scholar]
- 22.Vickers AJ, Vertosick EA, Lewith G, MacPherson H, Foster NE, Sherman KJ, Irnich D, Witt CM, Linde K. Acupuncture Trialists' Collaboration: Acupuncture for chronic pain: Update of an individual patient data meta-analysis. J Pain. 2018;19:455–474. doi: 10.1016/j.jpain.2017.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kaptchuk TJ. Acupuncture: Theory, efficacy, and practice. Ann Intern Med. 2002;136:374–383. doi: 10.7326/0003-4819-136-5-200203050-00010. [DOI] [PubMed] [Google Scholar]
- 24.Manheimer E, White A, Berman B, Forys K, Ernst E. Meta-analysis: Acupuncture for low back pain. Ann Intern Med. 2005;142:651–663. doi: 10.7326/0003-4819-142-8-200504190-00014. [DOI] [PubMed] [Google Scholar]
- 25.Smith JR, Spurrier NJ, Martin JT, Rosenbaum JT. Prevalent use of complementary and alternative medicine by patients with inflammatory eye disease. Ocul Immunol Inflamm. 2004;12:203–214. doi: 10.1080/092739490500200. [DOI] [PubMed] [Google Scholar]
- 26.Lee MS, Shin BC, Choi TY, Ernst E. Acupuncture for treating dry eye: A systematic review. Acta Ophthalmol. 2011;89:101–106. doi: 10.1111/j.1755-3768.2009.01855.x. [DOI] [PubMed] [Google Scholar]
- 27.Kim BH, Kim MH, Kang SH, Nam HJ. Optimizing acupuncture treatment for dry eye syndrome: A systematic review. BMC Complement Altern Med. 2018;18(145) doi: 10.1186/s12906-018-2202-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wolffsohn JS, Arita R, Chalmers R, Djalilian A, Dogru M, Dumbleton K, Gupta PK, Karpecki P, Lazreg S, Pult H, et al. TFOS DEWS II diagnostic methodology report. Ocul Surf. 2017;15:539–574. doi: 10.1016/j.jtos.2017.05.001. [DOI] [PubMed] [Google Scholar]
- 29.Yang L, Yang Z, Yu H, Song H. Acupuncture therapy is more effective than artificial tears for dry eye syndrome: Evidence based on a meta-analysis. Evid Based Complement Alternat Med. 2015;2015(143858) doi: 10.1155/2015/143858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang X, Liu Z, Ding W, Zhang J, Shi H, Zhu W. Efficacy and safety of acupuncture at a single BL1 acupoint in the treatment of moderate to severe dry eye disease: Protocol for a randomized, controlled trial. Medicine (Baltimore) 2018;97(e10924) doi: 10.1097/MD.0000000000010924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA. Cochrane Bias Methods Group; Cochrane Statistical Methods Group: The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343(d5928) doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Higgins JP and Green S: Cochrane Handbook for Systematic Reviews of Interventions: Cochrane Book Series 2008. [Google Scholar]
- 33.Nepp J, Wedrich A, Akramian J, Derbolav A, Mudrich C, Ries E, Schauersberger J. Dry eye treatment with acupuncture. A prospective, randomized, double-masked study. Adv Exp Med Biol. 1998;438:1011–1016. [PubMed] [Google Scholar]
- 34.Wang ZL, He HQ, Huang D, Shi CG. Effect of integral syndrome differentiation acupuncture on the tear film stability in the patient of xerophthalmia. Zhongguo Zhen Jiu. 2005;25:460–463. (In Chinese) [PubMed] [Google Scholar]
- 35.Tseng KL, Liu HJ, Tso KY, Woung LC, Su YC, Lin JG. A clinical study of acupuncture and SSP (silver spike point) electro-therapy for dry eye syndrome. Am J Chin Med. 2006;34:197–206. doi: 10.1142/S0192415X0600376X. [DOI] [PubMed] [Google Scholar]
- 36.Shi JL, Miao WH. Effects of acupuncture on lactoferrin content in tears and tear secretion in patients suffering from dry eyes: A randomized controlled trial. Zhong Xi Yi Jie He Xue Bao. 2012;10:1003–1008. doi: 10.3736/jcim20120909. (In Chinese) [DOI] [PubMed] [Google Scholar]
- 37.Kim TH, Kang JW, Kim KH, Kang KW, Shin MS, Jung SY, Kim AR, Jung HJ, Choi JB, Hong KE, et al. Acupuncture for the treatment of dry eye: A multicenter randomised controlled trial with active comparison intervention (artificial teardrops) PLoS One. 2012;7(e36638) doi: 10.1371/journal.pone.0036638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liao L, Wei Q, Gong X. Effects of nourishing liver and kidney by acupuncture for vision related quality of life in perimenopausal women with dry eye. J Trad Chin Ophthalmol. 2013;23:403–406. [Google Scholar]
- 39. Nan H: Clinical Observation of 60 Cases of Dry Eye Syndrome by the Treatment of Eye Acupuncture Combining the ArtifiCiaI Tears: Hubei University of Chinese Medicine; 2014. [Google Scholar]
- 40.Zeng Z, Ma Q, Song C, Xia H. Clinical observation on 28 cases of dry eye after LASIK treated by acupuncture and artificial tear. Hunan J Trad Chin Med. 2014;30:105–107. [Google Scholar]
- 41.Shang XJ. Therapeutic observation of acupuncture at phenomaxillary ganglia for dry eye syndrome. Shanghai J Acu Mox. 2015;9:870–872. (In Chinese) [Google Scholar]
- 42.Xiang S, Jiang X, Li Y, Dou R. The efficacy of acupuncture at phenomaxillary ganglion and periocular acupiont for the treatment of dry eye. J Zhejiang Univ Trad Chin Med. 2016;40:730–734. (In Chinese) [Google Scholar]
- 43.Liu Q, Liu J, Ren C, Cai W, Wei Q, Song Y, Yu J. Proteomic analysis of tears following acupuncture treatment for menopausal dry eye disease by two-dimensional nano-liquid chromatography coupled with tandem mass spectrometry. Int J Nanomedicine. 2017;12:1663–1671. doi: 10.2147/IJN.S126968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Huang R, Wu X, Li D. Observation on therapeutic effect of acupuncture on dry eye. Chin J Information on TCM. 2013;20:67–68. (In Chinese) [Google Scholar]
- 45.Bron AJ, de Paiva CS, Chauhan SK, Bonini S, Gabison EE, Jain S, Knop E, Markoulli M, Ogawa Y, Perez V, et al. TFOS DEWS II pathophysiology report. Ocul Surf. 2017;15:438–510. doi: 10.1016/j.jtos.2017.05.011. [DOI] [PubMed] [Google Scholar]
- 46.Li Y, Liu H, Zeng W, Wei J. Edaravone protects against hyperosmolarity-induced oxidative stress and apoptosis in primary human corneal epithelial cells. PLoS One. 2017;12(e0174437) doi: 10.1371/journal.pone.0174437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gilbard JP, Rossi SR, Heyda KG. Tear film and ocular surface changes after closure of the meibomian gland orifices in the rabbit. Ophthalmology. 1989;96:1180–1186. doi: 10.1016/s0161-6420(89)32753-9. [DOI] [PubMed] [Google Scholar]
- 48.Xie Y, Wang L. Correlation between tear osmolarity and the dry eye severity. Chinese J Experimental Ophthalmology. 2012;30:1022–1025. (In Chinese) [Google Scholar]
- 49.Cong C, Bi H, Wen Y. Research advance of the pathogenesis and treatment of dry eye. Guoji Yanke Zazhi (Int Eye Sci) 2012;12:464–467. (In Chinese) [Google Scholar]
- 50.Baudouin C, Aragona P, Messmer EM, Tomlinson A, Calonge M, Boboridis KG, Akova YA, Geerling G, Labetoulle M, Rolando M. Role of hyperosmolarity in the pathogenesis and management of dry eye disease: Proceedings of the OCEAN group meeting. Ocul Surf. 2013;11:246–258. doi: 10.1016/j.jtos.2013.07.003. [DOI] [PubMed] [Google Scholar]
- 51.Melzack R, Stillwell DM, Fox EJ. Trigger points and acupuncture points for pain: Correlations and implications. Pain. 1977;3:3–23. doi: 10.1016/0304-3959(77)90032-x. [DOI] [PubMed] [Google Scholar]
- 52.Li F, He T, Xu Q, Lin LT, Li H, Liu Y, Shi GX, Liu CZ. What is the Acupoint? A preliminary review of Acupoints. Pain Med. 2015;16:1905–1915. doi: 10.1111/pme.12761. [DOI] [PubMed] [Google Scholar]
- 53.Zhang WB, Jeong DM, Lee YH, Lee MS. Measurement of subcutaneous impedance by four-electrode method at acupoints located with single-power alternative current. Am J Chin Med. 2004;32:779–788. doi: 10.1142/S0192415X04002351. [DOI] [PubMed] [Google Scholar]
- 54.Wang Y, Yin LM, Xu YD, Lui YY, Ran J, Yang YQ. The research of acupuncture effective biomolecules: Retrospect and prospect. Evid Based Complement Alternat Med. 2013;2013(608026) doi: 10.1155/2013/608026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Andersson S, Lundeberg T. Acupuncture-from empiricism to science: Functional background to acupuncture effects in pain and disease. Med Hypotheses. 1995;45:271–281. doi: 10.1016/0306-9877(95)90117-5. [DOI] [PubMed] [Google Scholar]
- 56.Takahashi T. Mechanism of acupuncture on neuromodulation in the gut-a review. Neuromodulation. 2011;14:8–12. doi: 10.1111/j.1525-1403.2010.00295.x. [DOI] [PubMed] [Google Scholar]
- 57.Zhi FY, Liu J, Ma XP, Hong J, Zhang J, Zhang D, Zhao Y, Wu LJ, Yang YT, Wu DY, et al. Manual acupuncture for optic atrophy: A systematic review and meta-analysis. Evid Based Complement Alternat Med. 2019;2019(1735967) doi: 10.1155/2019/1735967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wei ML, Liu JP, Li N, Liu M. Acupuncture for slowing the progression of myopia in children and adolescents. Cochrane Database Syst Rev. 2011;(CD007842) doi: 10.1002/14651858.CD007842.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yan X, Zhu T, Ma C, Liu A, Dong L, Wang J. A meta-analysis of randomized controlled trials on acupuncture for amblyopia. Evid Based Complement Alternat Med. 2013;2013(648054) doi: 10.1155/2013/648054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lin T, Gong L, Liu X, Ma X. Fourier-domain optical coherence tomography for monitoring the lower tear meniscus in dry eye after acupuncture treatment. Evid Based Complement Alternat Med. 2015;2015(492150) doi: 10.1155/2015/492150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gong L, Sun X, Chapin WJ. Clinical curative effect of acupuncture therapy on xerophthalmia. Am J Chin Med. 2010;38:651–659. doi: 10.1142/S0192415X10008123. [DOI] [PubMed] [Google Scholar]
- 62.Müller LJ, Marfurt CF, Kruse F, Tervo TM. Corneal nerves: Structure, contents and function. Exp Eye Res. 2003;76:521–542. doi: 10.1016/s0014-4835(03)00050-2. [DOI] [PubMed] [Google Scholar]
- 63.Nepp J, Tsubota K, Goto E, Schauersberger J, Schild G, Jandrasits K, Abela C, Wedrich A. The effect of acupuncture on the temperature of the ocular surface in conjunctivitis sicca measured by non-contact thermography: Preliminary results. Adv Exp Med Biol. 2002;506:723–726. doi: 10.1007/978-1-4615-0717-8_102. [DOI] [PubMed] [Google Scholar]
- 64.Bäcker M, Grossman P, Schneider J, Michalsen A, Knoblauch N, Tan L, Niggemeyer C, Linde K, Melchart D, Dobos GJ. Acupuncture in migraine: Investigation of autonomic effects. Clin J Pain. 2008;24:106–115. doi: 10.1097/AJP.0b013e318159f95e. [DOI] [PubMed] [Google Scholar]
- 65.Kavoussi B, Ross BE. The neuroimmune basis of anti-inflammatory acupuncture. Integr Cancer Ther. 2007;6:251–257. doi: 10.1177/1534735407305892. [DOI] [PubMed] [Google Scholar]
- 66.Zhu C. Effect of acupuncture on visual system and its mechanism. Heilongjiang Med J. 2005;29:744–5. [Google Scholar]
- 67.Pflugfelder SC, Solomon A, Stern ME. The diagnosis and management of dry eye: A twenty-five-year review. Cornea. 2000;19:644–649. doi: 10.1097/00003226-200009000-00009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article