Abstract
The current study examined the factor structure, measurement reliability, measurement invariance across genders, and latent gender mean differences, of a new Chinese translation of the Adult Eating Behavior Questionnaire (C-AEBQ) in a Chinese young adult sample (n = 1,068, 52.57% women). The associations between the appetitive traits assessed by the AEBQ and body mass index were also explored. The previously established eight-factor model of the AEBQ was supported in the present sample. The C-AEBQ had strong measurement invariance between genders. Cronbach’s alpha estimates of the eight subscales of the C-AEBQ ranged from 0.76 to 0.97, and the test–retest reliability coefficients of the subscales ranged from 0.50 to 0.77. The C-AEBQ had adequate convergent and divergent validity, as supported by the theoretically expected correlations between C-AEBQ and the Three-Factor Eating Questionnaire. Furthermore, Satiety Responsiveness, Slowness in Eating, and Food Fussiness were inversely associated with body mass index. Overall, the C-AEBQ appears to be a psychometrically sound instrument as a comprehensive measure for appetitive traits for Chinese young adults.
Keywords: Adult Eating Behavior Questionnaire (AEBQ), appetitive traits, obesity, validation, Chinese
Over several decades, rising levels of obesity has been a major public health concern worldwide (Arroyo-Johnson & Mincey, 2016; Williams, Mesidor, Winters, Dubbert, & Wyatt, 2015), including in China (Y. Wang, Mi, Shan, Wang, & Ge, 2007; Wu, 2006). In China, based on the findings from a large-scale nation-wide survey (i.e., the National Free Preconception Health Examination Project between 2010 and 2014; Y. He et al., 2016; Y. He et al., 2017), the prevalence of overweight (including obesity) was 33.8% for Chinese men aged 15- to 49-year-old (6.3% were obese) and 24.8% for Chinese women aged 20- to 49-year-old (4.8% were obese). Significant increasing trends in the prevalence of overweight and obesity were also revealed. Eating disorders are also a global public health concern (Erskine, Whiteford, & Pike, 2016; Hudson, Hiripi, Pope, & Kessler, 2007; Schmidt et al., 2016). Although eating disorders have been widely studied in Western societies, they have not received enough research attention in China. Based on the limited research concerning eating disorders in China, the prevalence of eating disorders has become increasingly similar to that of Western societies (Tong et al., 2014). For example, a large-scale survey in adolescents and young adults in China found a prevalence rate of 2.3% for endorsing full criteria of eating disorders (Chen & Jackson, 2008).
Obesity and Appetitive Traits
Obesity is usually the result of unbalanced energy intake and expenditure; that is, a sustained energy surplus resulting in weight gain over time (Hill, Wyatt, & Peters, 2012). Individuals’ energy intake is directly related to their eating behaviors, which are influenced by environment and culture (Ma, 2015), as well as by person-level factors such as eating behaviors (i.e., disordered eating symptoms and appetitive traits; Caran, Santana, Monteiro, & da Veiga, 2018; Wardle, & Carnell, 2009) and genetic risk that may or may not be mediated by eating behavior (Albuquerque, Stice, Rodríguez-López, Manco, & Nóbrega, 2015). Appetitive traits are individual differences in the tendency to increase or reduce food intake in response to internal and external stimuli (e.g., the presence of food or food-associated cues, physiological hunger/satiety, negative affect) and/or to the properties of available food (e.g., novelty, sensory properties; French, Epstein, Jeffrey, Blundel, & Wardle, 2012; Llewellyn & Fildes, 2017). Appetitive traits are early emerging and moderately to strongly heritable, but there is evidence that the response tendencies associated with appetitive traits are modifiable (Wardle & Carnell, 2009). If weight-related appetitive traits are identified by using validated instruments in a given population, interventions designed to modify these traits can be applied to affect individuals’ or larger groups’ weight status (Konttinen et al., 2015; Nagata, Garber, Tabler, Murray, & Bibbins-Domingo, 2018).
Eating Disorders and Appetitive Traits
In contrast to disordered eating symptoms, appetitive traits are distributed throughout the population, and their associated response tendencies are not inherently problematic or pathological. However, some appetitive traits appear to be risk factors for eating disorders, including binge eating (e.g., food responsiveness, emotional overeating, low levels of satiety responsiveness; Gianini, White, & Masheb, 2013) and avoidant/restrictive food intake disorder (e.g., food fussiness, often referred to as “picky eating” or “selective/neophobic eating,” satiety responsiveness, low levels of eating enjoyment; Zickgraf & Ellis, 2018; Zickgraf, Franklin, & Rozin, 2016). Furthermore, there are findings suggesting a higher prevalence of so-called “nonfat phobic anorexia” in Asian countries, and research on disordered eating behaviors not associated with intentional caloric restriction due to fear of fatness might be particularly relevant to the study of low-weight eating disorders in addition to obesity in this population (Pike & Dunne, 2015). Thus, there is a clear need to assess how appetitive traits are related to each other, and how appetitive traits, as nonproblematic characteristics of eating behaviors, contribute to the development of eating disorders.
The Current Study
Several eating-behavior-related self-report instruments have been validated in Chinese, including the Eating Disorder Examination-Questionnaire (Lian et al., 2017), the Eating Attitudes Test-26 (B.-Y. wang et al., 2015), the Three-Factor Eating Questionnaire (TFEQ; Shi, Kong, Chen, & Cheng, 2011), and the Night Eating Questionnaire (J. He, Ji, Zhang, & Fan, 2018). However, these measures either assess disordered eating symptoms as opposed to appetitive traits, or assess a limited number of appetitive traits that are associated with excessive, rather than inadequate, energy intake, and they do not measure eating behaviors associated with inadequate dietary variety (Zickgraf & Rigby, 2018). Thus, to date, there is no measure available for Chinese adults for assessing nonpathological appetitive traits associated with food selection and energy intake. To the best of our knowledge, the Adult Eating Behavior Questionnaire (AEBQ) is the most comprehensive measure currently available to assess adults’ self-reported appetitive traits (Hunot et al., 2016). Thus, we chose to translate the AEBQ for use to assess appetitive traits in Chinese adults.
The AEBQ was adapted from the Child Eating Behavior Questionnaire (CEBQ; Wardle, Guthrie, Sanderson, & Rapoport, 2001) by changing the response format of the CEBQ from parent-report to self-report, and the adapted items were discussed and further refined by a panel of experts in clinical psychology, behavioral science, and nutrition (Hunot et al., 2016). The AEBQ is aimed to assess eight adult appetitive traits and to explore the associations between appetitive traits and body mass index (BMI). The eight traits measured by the AEBQ include four food-approach traits (i.e., Hunger, Food Responsiveness, Emotional Overeating, and Enjoyment of Food), and four food-avoidance traits (Satiety Responsiveness, Emotional Undereating, Food Fussiness, and Slowness in Eating), which are consistent with the CEBQ (Hunot et al., 2016). In childhood, appetitive traits associated with increased food intake are consistently related to concurrent adiposity, and are prospectively related to weight gain. On the other hand, Satiety Responsiveness, Slow Eating, and Emotional Undereating are usually found to mitigate against weight gain/obesity, and in some cases, to be risk factors for underweight (e.g., Antoniou et al., 2016; Boswell, Byrne, & Davies, 2018; Koch & Pollatos, 2014; Llewellyn & Fildes, 2017). Because the AEBQ is relatively new, to date only two studies have explored its relationship with adiposity in nonclinical samples. In two adult samples from the United Kingdom and Australia, the food-approach traits (with the exception of Hunger) were shown to be positively correlated with BMI derived from self-reported weight and height, whereas the food-avoidance traits (with the exception of Food Fussiness) were negatively correlated with BMI (Hunot et al., 2016; Mallan et al., 2017).
The psychometric properties of the AEBQ as used in non-Western societies (e.g., China) have yet to be studied. Given some initial evidence for cross-cultural differences in the features of adult eating disorders and disordered eating behaviors (Cummins, Simmons, & Zane, 2005; Levinson & Brosof, 2016; Miller & Pumariega, 2001), potential cross-cultural differences in the features and possible correlates of nonproblematic eating behaviors are also of interest. For example, Chinese culture is considered to be characterized by collectivism, whereas Western societies are predominantly individualistic (Earley, 1989). It has been found that collectivism and individualism have influences on individual differences in self-control (J. B. Li, Vazsonyi, & Dou, 2018), with Chinese participants reporting higher behavioral self-control than their U.S. counterparts. Considering that self-control is closely related to eating behaviors, especially to those behaviors related to food-approach traits (e.g., emotional eating, binge eating, and loss of control overeating; J. He, Latner, Wu, & Fan, 2018; Keller, Hartmann, & Siegrist, 2016), it is possible that Chinese people might have lower levels of the four food-approach traits measured by the Chinese translation of the AEBQ (C-AEBQ). It is also possible that the level of Slowness in Eating of the C-AEBQ might be higher in Chinese compared with Western participants, as Chinese culinary culture regard slow eating as healthy and elegant (Counihan, & Van Esterik, 2012). For a better understanding of appetitive traits and the potential cultural differences in appetitive traits with obesity and eating disorders, there is a clear need to translate the AEBQ into Chinese and to examine the psychometric properties of the AEBQ as used in non-Western societies such as China.
Gender differences have been identified for certain appetitive traits (e.g., men showed lowers scores in Emotional Overeating; Zickgraf & Rigby, 2018). Therefore, it is important to examine whether differing item responses from men and women reflect true gender differences in typical levels of the measured traits, or whether they reflect differences in response tendencies or interpretation of the items (Milfont & Fischer, 2010). However, this information has not been included in the three published validation studies of the AEBQ. Thus, another aim of the current study was to test measurement invariance and latent mean differences of the AEBQ across gender groups.
Specifically, we hypothesized as follows: (1) The C-AEBQ would show similar factor structure as shown in previous studies, as appetitive traits appear to be relatively universal and highly genetically determined (Carnell & Wardle, 2009); (2) Due to the lack of previous invariance studies of the AEBQ, analyses of measurement invariance for the C-AEBQ were exploratory without specific hypothesis; (3) We expected to broadly replicate the pattern of C-AEBQ scale intercorrelations, and scale correlations with BMI, as shown in in previous Western samples. However, given the evidence that the expression of appetitive traits may be influenced by culture, we did not have specific hypotheses regarding whether these effects would have similar magnitudes to those found in Western samples (e.g., the United States, the United Kingdom, and Australia).
We had several additional hypotheses concerning convergent and divergent validity, which expanded on the previous AEBQ literature: (4) Cognitive restraint of the TFEQ would have weak or almost no relationship with the appetitive traits of C-AEBQ. This hypothesis was based on the consideration that cognitive restraint of TFEQ assesses the tendency to restrict food consumption in order to control weight, but appetitive traits do not involve intentional weight control behaviors; (5) Uncontrolled Eating on the TFEQ, which measures the tendency to experience loss of control after beginning to eat, would have positive correlations with food-approach subscales of the C-AEBQ, but negative correlations with food-avoidance subscales of the C-AEBQ; (6) Emotional Eating of the TFEQ, which measures the tendency to overeat to cope with emotions, would be strongly and positively correlated with Emotional Overeating of the C-AEBQ, but negatively correlated with Emotional Undereating of the C-AEBQ.
Method
Procedure and Participants
The participants of the current study were recruited from undergraduate populations in two Chinese universities in two provinces: Zhejiang (Southern China) and Liaoning (Northern China). The study protocol was approved by the Research and Development Administration Office of the university, and all participants provided informed consent. The final sample included 1,068 university students, with 506 and 562 university students from Zhejiang province and Liaoning province, respectively. There were no significant differences between the two samples in terms of the percentage of women (55.12% in Zhejiang vs. 51.02% in Liaoning, χ2 = 2.18, p = .14) and mean age (20.15 in Zhejiang vs. 20.08 in Liaoning, t = 1.17, p = .24). Thus, the two samples were combined and used in the subsequent data analyses. Of the total sample, self-reported weight and height measures were obtained for BMI calculation, and the participants’ BMI ranged from 14.30 to 36.89 kg/m2, with a mean (SD) of 21.11 (3.10) kg/m2, which is similar to the average BMI of 22.10 kg/m2 for Chinese young adults (i.e., mean age of 20 years; Zeng et al., 2014). Based on the cutoff values of BMI for Chinese adults (i.e., <18.5 for underweight, 18.5-23.9 for normal weight, 24-27.9 for overweight, and >28 kg/m2 for obese; Zhou, 2002), of the total sample, 19.8% were underweight, 63.3% were normal weight, 12.7% were overweight, and 3.3% were obese. To establish test–retest reliability for the C-AEBQ, a subsample of 101 participants retook the survey 4 weeks after the initial administration. All information from these participants was obtained using paper-pencil surveys.
Measures
Chinese Translation of the Adult Eating Behavior Questionnaire.
Based on the standard translation and back-translation procedures (Brislin, 1970), the English version of the AEBQ was first translated into Chinese based on collaborative efforts of three Chinese doctoral students in the area of health psychology with a high level of English proficiency. The back translation was then conducted by a fourth bilingual (English, Chinese) doctoral student in the area of clinical psychology who had no previous knowledge about the AEBQ. The back-translated version was then reviewed by the developer of the AEBQ. Based on the developer’s comments, relevant modifications were made such that the translated version better reflects the original version of the instrument. Afterward, the revised version was used in a focus group of 10 undergraduate students recruited from a class in health psychology. Based on students’ feedback, some minor language modifications were further made to improve the clarity of the translated version. The 35 items of the C-AEBQ was then finalized and used in subsequent research.
The Three-Factor Eating Questionnaire.
The TFEQ (Stunkard & Messick, 1985) is a widely used self-report questionnaire for assessing disordered eating behaviors. The Chinese version of the 18-question TFEQ (Shi et al., 2011) was used in the current study. The responses are measured on a Likert scale ranging from 1 (completely true) to 4 (completely false). The TFEQ-18 assesses 3 domains of eating behavior: Cognitive Restraint, Uncontrolled Eating, and Emotional Eating (The descriptions of the three domains were described in the hypotheses section). In the current study, the TFEQ-18 showed good reliability, with the Cronbach’s alpha for each dimension was 0.83, 0.86, and 0.92 for Cognitive Restriction, Uncontrolled Eating, and Emotional Eating, respectively.
Data Analysis
Data analyses in the current study were conducted via R version 3.5.0 (R Core Team, 2018). First, the total sample (N = 1,068) was randomly half-split to two approximately equal subsamples, with one being used for exploratory factor analysis (EFA) and their other for confirmatory factor analysis (CFA).
The Psych package version 1.8.4 (Revelle, 2014) was used to conduct EFA, with Oblimin rotation and the ordinary least squares estimator (Lee, Zhang, & Edwards, 2012). The EFA was based on nonparametric polychoric correlations, which is an appropriate approach for ordinal data from Likert-type scales (Baglin, 2014). The number of factors to retain was determined by using parallel analysis (Çokluk & Koçak, 2016). Factor loadings greater than 0.4 are considered adequate (Hair, Black, Babin, Anderson, & Tatham, 2010).
The factor structure derived from EFA was confirmed in the second half of the sample, using the R “lavaan” package version 0.6-2 (Rosseel, 2012). The mean- and variance-adjusted weighted least squares estimator was employed, which has been shown to be superior to other estimation methods for Likert-type rating scales (C.-H. Li, 2016). To evaluate model fit, we used the comparative fit index (CFI), Tucker–Lewis index (TLI), root mean square error of approximation (RMSEA), and standardized root mean square residual (SRMR). According to Hu and Bentler (1999), values of CFI and TLI greater than 0.90 are acceptable and values greater than 0.95 indicate good model fit; for RMSEA, a value less than 0.08 is acceptable and a value less than 0.05 is good; and for SRMR, a value less than 0.08 is acceptable and a value less than 0.06 is good.
Measurement invariance across gender groups was assessed. Tests of configural invariance, metric invariance (or weak invariance), and scalar invariance (or strong invariance; van de Schoot, Lugtig, & Hox, 2012) were carried out for assessing progressively stronger measurement invariance. More specifically, configural invariance tests whether the basic model structure is invariant across groups. Metric invariance, while assuming configural invariance, tests whether factor loadings are invariant across groups. Finally, while assuming both configural and metric invariance, scalar invariance tests whether the intercepts of items are the same across groups (van de Schoot et al., 2012). According to previous literature (Chen, 2007; Cheung & Rensvold, 2002), ΔCFI <0.010 and ΔRMSEA < 0.015 indicate measurement invariance across different groups. After scalar invariance across the groups was shown, follow-up tests of latent mean differences across gender groups were conducted. In this analysis, the latent mean values are constrained to zero in one group and freely estimated for the other group, after which statistical significance of differences between the latent means are assessed (i.e., z greater than 1.96 means statistical significance at p = .05).
Cronbach’s alpha values based on polychoric correlations were calculated to assess internal consistency of the C-AEBQ, with Cronbach’s alpha greater than .70 being considered as adequate (Field, 2013). Test–retest reliability of the AEBQ was assessed using intraclass correlations (ICC; Shrout & Fleiss, 1979), with ICC values between 0.50 and 0.75 indicating moderate reliability and values greater than 0.75 indicating good reliability (Watkins & Portney, 2009). Because repeated measurements cannot be regarded as randomized samples, as recommended by Watkins and Portney (2009), the “two-way mixed effects” model was used for assessing ICC.
Convergent and divergent validity was measured by investigating Pearson correlation coefficients between the C-APEQ and the TFEQ. Furthermore, by using Pearson’s correlation, associations between the C-AEBQ and BMI were also explored. In addition, by using the R “cocor” package (Diedenhofen & Musch, 2015), statistical comparisons between certain correlations were also conducted.
Results
Exploratory Factor Analysis
Interpretation of the parallel analysis plot (Figure 1) supported a seven-factor solution, with the Hunger and Food Responsiveness items combined into a single scale (Hunger-Food Responsiveness). The EFA findings were in line with the EFA results found in the original development of the AEBQ (Hunot et al., 2016). EFA results showed that all the 35 items loaded on their intended factors, with 65% of the total variance explained. Item loadings are presented in Table 1.
Figure 1.
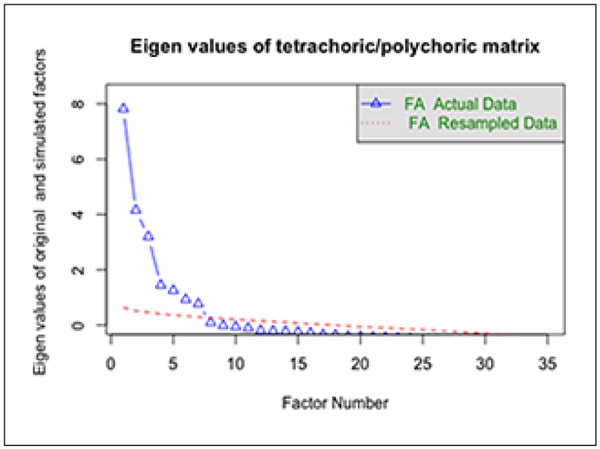
Parallel analysis (n = 534).
Table 1.
Factor Loadings of the C-AEBQ Based on EFA (n = 534).
| EUE | EOE | H-FR | SE | EF | FF | SR | |
|---|---|---|---|---|---|---|---|
| I eat less when I’m upset. | .96 | .01 | −.08 | .02 | .02 | .02 | −.01 |
| I eat less when I’m annoyed. | .93 | −.02 | .01 | .01 | 0 | .03 | −.01 |
| I eat less when I’m anxious. | .90 | −.02 | 0 | .01 | −.02 | .01 | −.02 |
| I eat less when I’m angry. | .87 | −.08 | −.01 | .01 | .02 | −.07 | .01 |
| I eat less when I’m worried. | .86 | −.06 | .05 | −.02 | 0 | −.04 | .02 |
| I eat more when I’m upset. | −.03 | .92 | −.02 | 0 | .02 | −.01 | 0 |
| I eat more when I’m anxious. | −.03 | .89 | .05 | −.03 | −.01 | −.07 | −.01 |
| I eat more when I’m worried. | −.06 | .87 | .01 | .03 | 0 | −.04 | −.03 |
| I eat more when I’m angry. | −.04 | .83 | .01 | −.05 | .07 | .08 | .06 |
| I eat more when I’m annoyed. | −.08 | .80 | .02 | .04 | .09 | −.01 | −.04 |
| I often feel hungry. | −.07 | −.01 | .79 | .06 | −.01 | −.02 | −.06 |
| I often feel so hungry that I have to eat something right away. | −.06 | 0 | .77 | .04 | −.02 | −.01 | .01 |
| I am always thinking about food. | −.06 | 0 | .69 | −.01 | .11 | −.02 | −.01 |
| Given the choice, I would eat most of the time. | .03 | .10 | .67 | .01 | .06 | .02 | −.05 |
| If I miss a meal, I get irritable. | .07 | .10 | .66 | −.01 | −.14 | .04 | −.03 |
| I often notice my stomach rumbling. | .06 | .06 | .62 | .05 | .06 | −.05 | .04 |
| If my meals are delayed, I get light-headed. | .07 | .19 | .56 | .16 | −.19 | .08 | −.01 |
| I often feel hungry when I am with someone who is eating. | .01 | −.04 | .50 | −.10 | .22 | −.01 | .06 |
| When I see or smell food that I like, it makes me want to eat. | −.11 | −.23 | .43 | −.05 | .40 | −.13 | .05 |
| I eat slowly. | .01 | −.01 | 0 | .90 | .02 | −.02 | .08 |
| I eat more and more slowly during the course of a meal. | .03 | .02 | .14 | .79 | −.06 | −.05 | .03 |
| I am often last at finishing a meal. | .10 | .11 | .10 | .78 | −.03 | .02 | .02 |
| I often finish my meals quickly.a | −.11 | −.15 | −.23 | .72 | .11 | .09 | −.09 |
| I enjoy eating. | .02 | .07 | 0 | .02 | .91 | 0 | −.02 |
| I love food. | .01 | .04 | −.07 | .01 | .88 | −.04 | −.03 |
| I look forward to mealtimes. | −.06 | .12 | .14 | −.02 | .67 | −.05 | −.08 |
| I am interested in tasting new food I haven’t tasted before.a | −.01 | −.01 | −.02 | −.04 | −.04 | .87 | .01 |
| I enjoy tasting new foods.a | −.08 | −.11 | −.02 | .02 | −.02 | .87 | −.03 |
| I refuse new foods at first. | .15 | .09 | .11 | .05 | .07 | .66 | .06 |
| I enjoy a wide variety of foods.a | −.02 | .15 | −.12 | −.01 | −.34 | .49 | −.02 |
| I often decide that I don’t like a food, before tasting it. | .13 | .04 | .16 | −.06 | .28 | .41 | .24 |
| I often get full before my meal is finished. | −.07 | −.09 | .02 | .06 | .03 | .01 | .80 |
| I get full up easily. | .06 | .07 | −.13 | −.03 | −.04 | 0 | .79 |
| I often leave food on my plate at the end of a meal. | −.09 | −.03 | .07 | .14 | −.11 | −.01 | .63 |
| I cannot eat a meal if I have had a snack just before. | .10 | .06 | 0 | −.04 | −.03 | .02 | .60 |
| Eigenvalue | 8.37 | 4.93 | 4.10 | 2.36 | 2.13 | 1.84 | 1.38 |
| Proportion of variance explained | .13 | .12 | .12 | .08 | .08 | .07 | .06 |
Note. C-AEBQ = Chinese translation of the Adult Eating Behavior Questionnaire; EFA = exploratory factor analysis; EUE = Emotional Undereating; EOE = Emotional Overeating; H = Hunger; FR = Food Responsiveness; SE = Slowness in Eating; EF = Enjoyment of Food; FF = Food Fussiness; SR = Satiety Responsiveness. Loadings greater than .30 are in bold type.
Item reverse coded.
Confirmatory Factor Analysis
CFA was used to test the fit of two models: The seven-factor structure derived from EFA and the eight-factor structure when the Hunger-Food Responsiveness scale was split into two factors (e.g., Hunot et al., 2016). CFA for the results for the correlated seven-factor correlated model showed good model fit, with χ2 = 1930.05 (degrees of freedom [df] = 539, p < .01), RMSEA = 0.07 (90% confidence interval [CI: 0.07, 0.08]), CFI = 0.98, TLI = 0.97, and SRMR = 0.08. The results of the eight-factor correlated model also indicated good model fit, with χ2 = 1700.30 (df = 532, p < .01), RMSEA = 0.07 (90% CI [0.06, 0.07]), CFI = 0.98, TLI = 0.98, and SRMR = 0.07. Using a model comparison approach, the Scaled Δχ2 = 133.76 (df = 7, p < .01) was statistically significant, suggesting that the eight-factor model has better fit for the data. Item loadings for the eight-factor model are showed in Table 2.
Table 2.
Factor Loadings of C-AEBQ Based on the Eight-Factor Model (n = 534).
| EUE | EOE | H | FR | SE | EF | FF | SR | |
|---|---|---|---|---|---|---|---|---|
| I eat less when I’m upset. | .96 | |||||||
| I eat less when I’m annoyed. | .95 | |||||||
| I eat less when I’m anxious. | .95 | |||||||
| I eat less when I’m angry. | .94 | |||||||
| I eat less when I’m worried. | .90 | |||||||
| I eat more when I’m upset. | .96 | |||||||
| I eat more when I’m anxious. | .94 | |||||||
| I eat more when I’m worried. | .95 | |||||||
| I eat more when I’m angry. | .85 | |||||||
| I eat more when I’m annoyed. | .86 | |||||||
| I often notice my stomach rumbling. | .69 | |||||||
| If I miss a meal, I get irritable. | .72 | |||||||
| I often feel so hungry that I have to eat something right away. | .76 | |||||||
| I often feel hungry. | .80 | |||||||
| If my meals are delayed, I get light-headed. | .61 | |||||||
| I often feel hungry when I am with someone who is eating. | .50 | |||||||
| Given the choice, I would eat most of the time. | .79 | |||||||
| I am always thinking about food. | .82 | |||||||
| When I see or smell food that I like, it makes me want to eat. | .56 | |||||||
| I eat slowly. | .91 | |||||||
| I eat more and more slowly during the course of a meal. | .88 | |||||||
| I am often last at finishing a meal. | .75 | |||||||
| I often finish my meals quickly.a | .61 | |||||||
| I enjoy eating. | .96 | |||||||
| I love food. | .88 | |||||||
| I look forward to mealtimes. | .84 | |||||||
| I enjoy tasting new foods.a | .93 | |||||||
| I am interested in tasting new food I haven’t tasted before.a | .93 | |||||||
| I refuse new foods at first. | .52 | |||||||
| I enjoy a wide variety of foods.a | .65 | |||||||
| I often decide that I don’t like a food before tasting it. | .22 | |||||||
| I often get full before my meal is finished. | .81 | |||||||
| I get full up easily. | .71 | |||||||
| I often leave food on my plate at the end of a meal. | .69 | |||||||
| I cannot eat a meal if I have had a snack just before. | .62 |
Note. C-AEBQ = Chinese translation of the Adult Eating Behavior Questionnaire; EUE = Emotional Undereating; EOE = Emotional Overeating; H = Hunger; FR = Food Responsiveness; SE = Slowness in Eating; EF = Enjoyment of Food; FF = Food Fussiness; SR = Satiety Responsiveness.
Item reverse coded.
One item (“I often decide that I don’t like a food, before tasting it”) in the eight-factor model belonging to the Food Fussiness scale had a relatively low loading (i.e., 0.22). Because the item had a high loading (i.e., 0.41) in EFA (see Table 1), and to maintain the integrity of the original AEBQ for future research in this population, the item was retained in subsequent analyses.
Reliability
Based on the total sample (N = 1,068), the Cronbach’s alpha coefficients for the eight C-AEBQ scales ranged from .76 (Food Responsiveness) to .97 (Emotional Undereating), with all greater than .70. In the subsample of 101 participants who took the survey again after 4 weeks, the intraclass coefficients ranged from 0.50 (Emotional Undereating) to 0.77 (Slowness in Eating), with all scales (except for Emotional Undereating) close to or greater than 0.70 (Table 3).
Table 3.
Cronbach’s Alpha (N = 1,068) and Intraclass Coefficients (n = 101) for the C-AEBQ.
| C-AEBQ scales | Cronbach’s alpha | Intraclass coefficients |
|---|---|---|
| Food-approach scales | ||
| H | .84 | 0.67 |
| FR | .76 | 0.74 |
| EOE | .96 | 0.65 |
| EF | .91 | 0.67 |
| Food-avoidance scales | ||
| SR | .79 | 0.70 |
| EUE | .97 | 0.50 |
| FF | .78 | 0.68 |
| SE | .86 | 0.77 |
Note. C-AEBQ = Chinese translation of the Adult Eating Behavior Questionnaire; H = Hunger; FR = Food Responsiveness; EOE = Emotional Overeating; EF = Enjoyment of Food; SR = Satiety Responsiveness; EUE = Emotional Undereating; FF = Food Fussiness; SE = Slowness in Eating.
Interfactor Correlations
Results indicated positive interfactor correlations among the four food-approach scales (Hunger, Food Responsiveness, Emotional Overeating, Enjoyment of Food) and among the four food-avoidance scales (Satiety Responsiveness, Emotional Undereating, Food Fussiness, and Slowness in Eating). Significant negative correlations (p < .05) were found between most combinations of food-avoidance and food-approach scales. The interfactor correlations of the C-AEBQ are shown in Table 4.
Table 4.
Description and Correlations Between Appetitive Traits (N = 1,068).
| C-AEBQ scales |
M | SD | Food-approach scales | Food-avoidance scales | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| H | FR | EOE | EF | SR | EUE | FF | SE | |||
| Food-approach scales | ||||||||||
| H | 2.67 | 0.81 | 1 | |||||||
| FR | 3.06 | 0.78 | .58** | 1 | ||||||
| EOE | 2.68 | 1.03 | .31** | .31** | 1 | |||||
| EF | 3.99 | 0.82 | .16** | .39** | .30** | 1 | ||||
| Food-avoidance scales | ||||||||||
| SR | 2.72 | 0.82 | .01 | −.05 | −.09** | −.19** | 1 | |||
| EUE | 3.08 | 1.06 | −.07* | −.08** | −.52** | −.13** | .16** | 1 | ||
| FF | 2.53 | 0.71 | −.01 | −.12** | −.04 | −.27** | .18** | .02 | 1 | |
| SE | 2.64 | 0.92 | .19** | .12** | .01 | −.01 | .21** | .07* | .02 | 1 |
Note. C-AEBQ = Chinese translation of the Adult Eating Behavior Questionnaire; H = Hunger; FR = Food Responsiveness; EOE = Emotional Overeating; EF = Enjoyment of Food; SR = Satiety Responsiveness; EUE = Emotional Undereating; FF = Food Fussiness; SE = Slowness in Eating.
p < .05.
p < .01.
Tests of Measurement Invariance and Latent Mean Differences Across Gender
As shown in Table 5, the eight-factor model showed good model fit for both men and women. Next, tests for progressively stronger gender invariance conditions were conducted. Results showed that compared with the configural invariance model, the metric invariance model did not result in significantly decreased model fit (see Table 5), with ΔCFI = 0.001 and ΔRMSEA = 0.002, lower than the recommended cutoffs of 0.010 and 0.015, respectively. Furthermore, the scalar invariance model also did not result in a significantly decreased fit of the model over the metric invariance model (see Table 5), with ΔCFI = 0.000 and ΔRMSEA = 0.003. This finding suggests a lack of response bias between men and women and allows the comparisons of factor means across men and women.
Table 5.
Fit Indices for Gender Invariance Test (N = 1,068).
| Model | χ2 | df | CFI | TLI | RMSEA [90% CI] | SRMR | ΔCFI | ΔRMSEA |
|---|---|---|---|---|---|---|---|---|
| Men | 1263.62** | 532 | 0.988 | 0.987 | 0.054 [0.050, 0.058] | 0.057 | — | — |
| Women | 2207.82** | 532 | 0.969 | 0.965 | 0.080 [0.077, 0.084] | 0.076 | — | — |
| Configural invariance | 3455.79** | 1064 | 0.979 | 0.977 | 0.068 [0.066, 0.071] | 0.066 | — | — |
| Metric invariance | 3669.69** | 1091 | 0.978 | 0.976 | 0.070 [0.068, 0.073] | 0.070 | 0.001 | 0.002 |
| Scalar invariance | 3767.81** | 1188 | 0.978 | 0.978 | 0.067 [0.065, 0.070] | 0.067 | 0.000 | 0.003 |
Note. df = degrees of freedom; CFI = comparative fit index; TLI = Tucker–Lewis index; RMSEA = root mean square error of approximation
SRMR = standardized root mean square residual; CI = confidence interval; ΔCFI = change in CFI relative to the preceding model; ΔRMSEA = change in RMSEA relative to the preceding model.
p < .01.
Given the support for scalar invariance of the eight-factor model across men and women, we conducted a comparison of latent factor mean differences. Latent mean values for the eight factors were constrained to zero in the women and freely estimated for men. Results showed that there were significant latent mean differences on Emotional Undereating (z = 2.71, p < .01, d = 0.18), Hunger-Food Responsiveness (z = −3.71, p < .01, d = −0.27), Slowness in Eating (z = −2.94, p < .01, d = −0.21), Enjoyment of Food (z = −3.79, p < .01, d = −0.27), Satiety Responsiveness (z = −4.64, p < .01, d = −0.35). These findings indicated that women had lower latent scores in Emotional Undereating, but higher latent scores in Food Responsiveness, Slowness in Eating, Enjoyment of Food, and Satiety Responsiveness. There were no significant gender differences in Emotional Overeating (z = −1.28, p = .20, d = −0.09), Hunger (z = 1.26, p = .21, d = 0.09), or Food Fussiness (z = −0.61, p = .54, d = −0.04).
Associations With BMI
As shown in Table 6, contrary to our hypothesis, there were no statistically significant associations between the food-approach scales and participants’ BMI calculated by using self-reported height and weight. However, the food-avoidance scales (except for Emotional Undereating) had statistically significant (p < .01), and in the cases of Slowness in Eating and Satiety Responsiveness, small to moderate, negative associations with participants’ BMI. The correlation with Food Fussiness, while significant, was small. See Table 6 for unadjusted correlations and correlations adjusted for gender.
Table 6.
Correlations Between Appetitive Traits, BMI, and Disordered Eating Behaviors (N = 1,068).
| Food-approach scales | Food-avoidance scales | |||||||
|---|---|---|---|---|---|---|---|---|
| H | FR | EOE | EF | SR | EUE | FF | SE | |
| BMI (unadjusted) | −.05 | .01 | .01 | .03 | −.20** | .02 | −.08** | −.17** |
| BMI (adjusted for gender) | −.05 | .03 | .01 | .04 | −.18** | .01 | −.08** | −.16** |
| TFEQ-CR | .02 | .11** | .08** | −.02 | .08** | .05 | −.04 | 0 |
| TFEQ-UE | .48** | .52** | .40** | .17** | −.09** | −.21** | −.04 | .07* |
| TFEQ-EE | .34** | .30** | .56** | .07* | 0 | −.32** | .03 | .04 |
Note. BMI = body mass index; H = Hunger; FR = Food Responsiveness; EOE = Emotional Overeating; EF = Enjoyment of Food; SR = Satiety Responsiveness; EUE = Emotional Undereating; FF = Food Fussiness; SE = Slowness in Eating; TFEQ = Three-Factor Eating Questionnaire; CR = Cognitive Restraint; UE = Uncontrolled Eating; EE = Emotional Eating.
p < .05.
p < .01.
Associations With Disordered Eating Behaviors
Table 6 also shows the correlations between the C-AEBQ and the TFEQ. In line with the hypotheses, Cognitive Restraint showed negligible correlations with all subscales of the AEBQ. Uncontrolled Eating showed significant positive correlations with the four food-approach subscales of the C-AEBQ, with moderate-large effect sizes for Hunger, Food Responsiveness, and Emotional Overeating. Uncontrolled Eating also showed small negative correlations with Satiety Responsiveness (p < .01) and Emotional Undereating (p < .01), but negligible correlations with Food Fussiness and Slowness in Eating. TFEQ Emotional Eating had a strong and positive correlation with Emotional Overeating (p < .01), and a negative correlation with Emotional Undereating (p < .01). The correlation between Emotional Eating of the TFEQ and Emotional Overeating of the C-AEBQ was much higher than the correlations between Emotional Eating and other subscales of the C-AEBQ, with z ranging from 7.23 to 14.97 (all p < .01).
Discussion
The current study aimed to translate and evaluate the psychometric characteristics of this measure (i.e., factor structure, internal consistency, and measurement invariance and latent mean differences across gender) of the AEBQ in a sample from mainland China (C-AEBQ). Furthermore, the current study examined the convergent/divergent validity of AEBQ subscales, and it is the first study to examine the measurement invariance of the AEBQ and latent mean differences in appetitive traits across gender. Consistent with prior studies (Hunot et al., 2016; Mallan et al., 2017; Zickgraf & Rigby, 2018), an eight-factor structure separating the Hunger and Food Responsiveness scales appears to best represent appetitive traits in this non-Western sample. These two scales are intended to measure distinct phenomena that might be differentially associated with adiposity and eating behavior: Hunger is a measure of awareness of, and responsiveness to, physiological hunger cues, whereas Food Responsiveness is a measure of the tendency to feel subjective hunger and/or eat in response to food cues in the environment. The latter tendency has been associated with binge eating, weight gain, and cravings for high-calorie foods, whereas the associations between self-reported awareness of physiological hunger and eating behavior have not yet been explored (Burton, Smit, & Lightowler, 2007; Kakoschke, Kemps, & Tiggemann, 2015; Pinaquy, Chabrol, Simon, Louvet, & Barbe, 2003; van Strien, Herman, & Verheijden, 2012).
The interfactor correlation pattern among the eight subscales and internal reliability estimates (greater than 0.70) further support the construct validity and internal consistency reliability of the C-AEBQ (Hunot et al., 2016; Mallan et al., 2017; Zickgraf & Rigby, 2018). These findings confirmed the opposite directions of “food-approach” and “food-avoidance” measured by the C-APEQ.
Unlike in the three previous validation samples, the current findings did not show that Hunger was related to Emotional Undereating. Previously, Mallan et al. (2017) suggested that the correlation between Hunger and Emotional Undereating posed a challenge for the validity of the Hunger scale. Alternative hypotheses for their association have been proposed (Zickgraf & Rigby, 2018); however, this study’s inconsistent finding about the relationship (or lack thereof) between Hunger and Emotional Undereating compared and the unexpected positive correlation between Hunger and Slowness in Eating, raise further questions about the validity of the Hunger scale, particularly when used in young adult Chinese undergraduates.
Contrary to our expectation, and inconsistent with previous validation studies of the AEBQ in general Western samples (Hunot et al., 2016; Mallan et al., 2017), none of the four food-approach scales were correlated with BMI. This finding suggests that there might be cultural differences between Chinese and Western populations in terms of how appetitive traits are related to BMI. A possible explanation for the lack of a relationship between food-approach traits and BMI in the current sample is that, in a culture of collectivism, Chinese people value self-control (J. B. Li et al., 2018), which might make them more resistant to the ubiquity of food-related cues in an obesogenic food environment, or to other nonphysiological eating triggers, including negative affect and reward seeking (Shmueli & Prochaska, 2009); as a result, the potential associations of food-approach traits with BMI are weakened by stronger self-control.
In line with the previous literature, significant and negative correlations were found between the three of the four food-avoidance scales (except for Emotional Undereating) and BMI. Specifically, these results indicate that participants with higher levels of Satiety Responsiveness, Food Fussiness, and Slowness in Eating tend to have lower BMI. This is consistent with a recent finding based on latent profile analyses identifying a class of U.S. adults with high levels of Food Fussiness, Slowness in Eating, and Satiety Responsiveness, and low levels of Enjoyment of Food, who were at significantly lower risk for overweight or obesity compared with members of all other profile groups (Ellis, Zickgraf, Galloway, Essayli, & Whited, 2018). Unlike other appetitive traits assessed by the AEBQ, Food Fussiness is not primarily related to energy intake, but rather to food choice. However, there is evidence that when Food Fussiness co-occurs with limited eating enjoyment and increased satiety responsiveness there might be additive effects leading to decreased caloric intake and protection against overweight/obesity. Furthermore, the correlation between Slowness in Eating and BMI was higher in the current study than those found in previous studies conducted in Western societies. A potential explanation for this finding is that, because slow eating is associated with politeness and sophistication in Chinese culture (Counihan & Van Esterik, 2012), this behavior, which also enhances the experience of satiety and is considered to be protective against overeating, may be more common, and therefore more likely to mitigate against overweight.
It is worth noting that the two emotion-related scales (i.e., Emotional Overeating and Emotional Undereating) showed trivial and nonsignificant correlations with BMI in the current study, which is inconsistent with the original development/validation study, where Emotional Overeating and Emotional Undereating showed the strongest correlations with BMI (Hunot et al., 2016). These scales might be more likely to be influenced by cultural differences than other AEBQ scales that measure traits more closely tied to physiology (e.g., Satiety Responsiveness; Johnson, 2013; Walker, Ibia, & Zigman, 2012). There have been numerous studies showing that individuals from Asian backgrounds (e.g., Chinese) are more likely to use suppression (or controlling emotions by not expressing them) to regulate their emotions than their peers from Western societies (Ford & Mauss, 2015). Thus, Chinese respondents in the current study might be less likely to act outwardly on emotions by expressing them through eating behavior, which could have weakened the associations between Emotional Overeating/ Emotional Undereating and BMI.
The current study also demonstrated that testing for gender differences on the C-AEBQ is methodologically valid. Latent mean difference tests showed that women had lower latent scores than men on Emotional Undereating but higher latent scores on Slowness in Eating and Satiety Responsiveness, which is consistent with Zickgraf and Rigby (2018). However, different from Zickgraf and Rigby (2018), we also found that women had higher scores in Food Responsiveness and Enjoyment of Food. Such discrepancies between the two studies could be a result of cultural differences (the United States vs. China) or the different characteristics of the samples used in the two studies (bariatric surgery-seeking patients vs. undergraduate students), or a combination of these two. Of the five traits with gender differences found in the current study, Slowness in Eating and Satiety Responsiveness were found to be associated with BMI; more research on gender differences is needed to understand whether weight-control interventions based on appetitive traits in a Chinese context may be further designed to be gender-specific.
Correlations between the C-AEBQ and the TFEQ provided support for the adequate validity of some subscales of the C-AEBQ. Specifically, as Cognitive Restraint of the TFEQ measures the tendency to restrict food consumption to control their weight, while no subscales of the C-AEBQ are developed involving the intention of weight control (Hunot et al., 2016), the negligible correlations between Cognitive Restraint and all subscales of the C-AEBQ supported the divergent validity of the C-AEBQ. Furthermore, Uncontrolled Eating of the TEFQ measures the tendency to experience loss of control overeating, which has been shown to have close relationships with food-approach traits (e.g., Emotional Overeating; Cornelis et al., 2014). Thus, the significant positive correlations between Uncontrolled Eating and the four food-approach subscales of the C-AEBQ supported the C-AEBQ’s convergent validity. Finally, as Emotional Eating of the TFEQ measures the tendency to overeat to cope with emotions, which is a similar construct to the Emotional Overeating of the C-AEBQ, our finding of the strongest and positive correlation between Emotion Eating and Emotional Overeating provided support for both convergent and divergent validity of the C-AEBQ, as the Emotional Eating showed lower correlations with other subscales of the C-AEBQ.
Limitations
Several limitations should be considered for interpreting the findings of the current study. First, the sample of the current work only included university students, which limits the generalizability of the findings of the current work to general adult populations or to clinical samples with obesity (i.e., Zickgraf & Rigby, 2018). It is possible that the psychometric properties of the C-AEBQ may differ across such different populations. Thus, future research is highly recommended to evaluate the performance of the C-AEBQ in general adult populations and in clinical samples. Moreover, as a cross-sectional study, caution is warranted in inferring about causal relationships between the appetitive traits and BMI found in the current work, and further studies are needed to confirm whether appetitive traits can affect individuals’ weight status. Three C-AEBQ traits were related to lower BMI, though the correlations are relatively low. However, considering the complex causes of obesity (Wright & Aronne, 2012), interventions targeting expression of appetitive traits might be used together with other interventions (e.g., dietary and physical activity interventions; Greaves et al., 2011). However, before designing interventions based on appetitive traits, the causal effects of appetitive traits on weight in the Chinese adult population should be investigated further. Finally, BMI was calculated based on participants’ self-reported height and weight, which has been demonstrated to be different from BMI calculated by using physically measured data in adults (Danubio, Miranda, Vinciguerra, Vecchi, & Rufo, 2008); thus, future studies may consider calculating BMI by using measured height and weight.
Conclusion
In summary, the current study showed that the C-AEBQ had an eight-factor model which demonstrated good reliability, convergent/divergent validity, and strong measurement invariance across gender groups. Overall, the C-AEBQ appears to be a reliable, convenient, and comprehensive measure of appetitive traits for Chinese young adults.
Acknowledgments
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Albuquerque D, Stice E, Rodríguez-López R, Manco L, & Nóbrega C (2015). Current review of genetics of human obesity: From molecular mechanisms to an evolutionary perspective. Molecular Genetics and Genomics, 290, 1191–1221. [DOI] [PubMed] [Google Scholar]
- Antoniou EE, Roefs A, Kremers SPJ, Jansen A, Gubbels JS, Sleddens EFC, & Thijs C (2016). Picky eating and child weight status development: A longitudinal study. Journal of Human Nutrition and Dietetics, 29, 298–307. [DOI] [PubMed] [Google Scholar]
- Arroyo-Johnson C, & Mincey KD (2016). Obesity epidemiology worldwide. Gastroenterology Clinics, 45, 571–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baglin J (2014). Improving your exploratory factor analysis for ordinal data: A demonstration using FACTOR. Practical Assessment, Research & Evaluation, 19(5), 1–15. [Google Scholar]
- Boswell N, Byrne R, & Davies PS (2018). Eating behavior traits associated with demographic variables and implications for obesity outcomes in early childhood. Appetite, 120, 482–490. [DOI] [PubMed] [Google Scholar]
- Brislin RW (1970). Back-translation for cross-cultural research. Journal of Cross-Cultural Psychology, 1, 185–216. [Google Scholar]
- Burton P, Smit HJ, & Lightowler HJ (2007). The influence of restrained and external eating patterns on overeating. Appetite, 49, 191–197. [DOI] [PubMed] [Google Scholar]
- Caran LG, Santana DD, Monteiro LS, & da Veiga GV (2018). Disordered eating behaviors and energy and nutrient intake in a regional sample of Brazilian adolescents from public schools. Eating and Weight Disorders: Studies on Anorexia, Bulimia and Obesity, 23, 825–832. [DOI] [PubMed] [Google Scholar]
- Carnell S, & Wardle J (2009). Appetitive traits in children: New evidence for associations with weight and a common, obesity-associated genetic variant. Appetite, 53, 260–263. [DOI] [PubMed] [Google Scholar]
- Chen FF (2007). Sensitivity of goodness of fit indexes to lack of measurement invariance. Structural Equation Modeling, 14, 464–504. [Google Scholar]
- Chen H, & Jackson T (2008). Prevalence and sociodemographic correlates of eating disorder endorsements among adolescents and young adults from China. European Eating Disorders Review. The Professional Journal of the Eating Disorders Association, 16, 375–385. [DOI] [PubMed] [Google Scholar]
- Cheung GW, & Rensvold RB (2002). Evaluating goodness-of-fit indexes for testing measurement invariance. Structural Equation Modeling, 9, 233–255. [Google Scholar]
- Çokluk Ö, & Koçak D (2016). Using Horn’s parallel analysis method in exploratory factor analysis for determining the number of factors. Educational Sciences: Theory & Practice, 16, 537–551. [Google Scholar]
- Cornelis MC, Rimm EB, Curhan GC, Kraft P, Hunter DJ, Hu FB, & van Dam RM (2014). Obesity susceptibility loci and uncontrolled eating, emotional eating and cognitive restraint behaviors in men and women. Obesity, 22, e135–e141. doi: 10.1002/oby.20592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Counihan C, & Van Esterik P (Eds.). (2012). Food and culture: A reader. New York, NY: Routledge. [Google Scholar]
- Cummins LH, Simmons AM, & Zane NW (2005). Eating disorders in Asian populations: A critique of current approaches to the study of culture, ethnicity, and eating disorders. American Journal of Orthopsychiatry, 75, 553–574. [DOI] [PubMed] [Google Scholar]
- Danubio ME, Miranda G, Vinciguerra MG, Vecchi E, & Rufo F (2008). Comparison of self-reported and measured height and weight: Implications for obesity research among young adults. Economics & Human Biology, 6, 181–190. [DOI] [PubMed] [Google Scholar]
- Diedenhofen B, & Musch J (2015). cocor: A comprehensive solution for the statistical comparison of correlations. PLoS ONE, 10, e0121945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earley PC (1989). Social loafing and collectivism: A comparison of the United States and the People’s Republic of China. Administrative Science Quarterly, 34, 565–581. [Google Scholar]
- Ellis JM, Zickgraf HF, Galloway AT, Essayli JH, & Whited MC (2018). A functional description of adult picky eating using latent profile analysis. International Journal of Behavioral Nutrition and Physical Activity, 15, 109. doi: 10.1186/s12966-018-0743-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erskine HE, Whiteford HA, & Pike KM (2016). The global burden of eating disorders. Current Opinion in Psychiatry, 29, 346–353. [DOI] [PubMed] [Google Scholar]
- Field A (2013). Discovering statistics using IBM SPSS statistics: Thousand Oaks, CA: Sage. [Google Scholar]
- Ford BQ, & Mauss IB (2015). Culture and emotion regulation. Current Opinion in Psychology, 3, 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French SA, Epstein Leonard H., Jeffery Robert W., Blundell John E., & Wardle Jane. (2012). Eating behavior dimensions. Associations with energy intake and body weight. A review. Appetite, 59, 541–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gianini LM, White MA, & Masheb RM (2013). Eating pathology, emotion regulation, and emotional overeating in obese adults with binge eating disorder. Eating Behaviors, 14, 309–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greaves CJ, Sheppard KE, Abraham C, Hardeman W, Roden M, Evans PH, & Schwarz P (2011). Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health, 11, 119. doi: 10.1186/1471-2458-11-119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hair JF Jr., Black WC, Babin BJ, Anderson RE, & Tatham RL (2010). Multivariate data analysis (7th ed.). Upper Saddle River, NJ: Prentice Hall. [Google Scholar]
- He J, Ji F, Zhang X, & Fan X (2018). Psychometric properties and gender invariance of the simplified Chinese version of Night Eating Questionnaire in a large sample of mainland Chinese college students. Eating and Weight Disorders: Studies on Anorexia, Bulimia and Obesity, 24, 57–66. [DOI] [PubMed] [Google Scholar]
- He J, Latner JD, Wu W, & Fan X (2018). Measuring loss of control over eating in a Chinese context: Psychometric properties of the full and brief Chinese version of the loss of control over eating scale. Current Psychology. Advance online publication. doi: 10.1007/s12144-018-9976-6 [DOI] [Google Scholar]
- He Y, Pan A, Wang Y, Yang Y, Xu J, Zhang Y, . . . Yan D (2017). Prevalence of overweight and obesity in 15.8 million men aged 15-49 years in rural China from 2010 to 2014. Scientific Reports, 7, 5012. doi: 10.1038/s41598-017-04135-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He Y, Pan A, Yang Y, Wang Y, Xu J, Zhang Y, . . . Yan D (2016). Prevalence of underweight, overweight, and obesity among reproductive-age women and adolescent girls in rural China. American Journal of Public Health, 106, 2103–2110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill JO, Wyatt HR, & Peters JC (2012). Energy balance and obesity. Circulation, 126, 126–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu LT, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6, 1–55. [Google Scholar]
- Hudson JI, Hiripi E, Pope HG Jr., & Kessler RC (2007). The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry, 61, 348–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunot C, Fildes A, Croker H, Llewellyn CH, Wardle J, & Beeken RJ (2016). Appetitive traits and relationships with BMI in adults: Development of the Adult Eating Behaviour Questionnaire. Appetite, 105, 356–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson AW (2013). Eating beyond metabolic need: How environmental cues influence feeding behavior. Trends in Neurosciences, 36, 101–109. [DOI] [PubMed] [Google Scholar]
- Kakoschke N, Kemps E, & Tiggemann M (2015). External eating mediates the relationship between impulsivity and unhealthy food intake. Physiology & Behavior, 147, 117–121. [DOI] [PubMed] [Google Scholar]
- Keller C, Hartmann C, & Siegrist M (2016). The association between dispositional self-control and longitudinal changes in eating behaviors, diet quality, and BMI. Psychology & Health, 31, 1311–1327. [DOI] [PubMed] [Google Scholar]
- Koch A, & Pollatos O (2014). Interoceptive sensitivity, body weight and eating behavior in children: A prospective study. Frontiers in Psychology, 5, 1003. doi: 10.3389/fpsyg.2014.01003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konttinen H, Llewellyn C, Wardle J, Silventoinen K, Joensuu A, Männistö S, . . . Perola M (2015). Appetitive trats as behavioural pathways in genetic susceptibility to obesity: A population-based cross-sectional study. Scientific Reports, 5, 14726. doi: 10.1038/srep14726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee C-T, Zhang G, & Edwards MC (2012). Ordinary least squares estimation of parameters in exploratory factor analysis with ordinal data. Multivariate Behavioral Research, 47, 314–339. [DOI] [PubMed] [Google Scholar]
- Levinson C, & Brosof L (2016). Cultural and ethnic differences in eating disorders and disordered eating behaviors. Current Psychiatry Reviews, 12, 163–174. [Google Scholar]
- Li C-H (2016). Confirmatory factor analysis with ordinal data: Comparing robust maximum likelihood and diagonally weighted least squares. Behavior Research Methods, 48, 936–949. [DOI] [PubMed] [Google Scholar]
- Li JB, Vazsonyi AT, & Dou K (2018). Is individualism-collectivism associated with self-control? Evidence from Chinese and U.S. samples. PLoS ONE, 13, e0208541. doi: 10.1371/journal.pone.0208541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lian G, Chen J, Huang Y, Kang Q, Huang J, Yanling H, & Xiao Z (2017). Validity and reliability of the Chinese version of the Eating Disorder Examination Questionnaire 6.0 in female patients with eating disorders. Chinese Mental Health Journal, 31, 350–355. [Google Scholar]
- Llewellyn CH, & Fildes A (2017). Behavioural susceptibility theory: Professor Jane Wardle and the role of appetite in genetic risk of obesity. Current Obesity Reports, 6, 38–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma G (2015). Food, eating behavior, and culture in Chinese society. Journal of Ethnic Foods, 2, 195–199. [Google Scholar]
- Mallan KM, Fildes A, de la Piedad Garcia X, Drzezdzon J, Sampson M, & Llewellyn C (2017). Appetitive traits associated with higher and lower body mass index: Evaluating the validity of the Adult Eating Behaviour Questionnaire in an Australian sample. International Journal of Behavioral Nutrition and Physical Activity, 14, 130. doi: 10.1186/s12966-017-0587-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milfont TL, & Fischer R (2010). Testing measurement invariance across groups: Applications in cross-cultural research. International Journal of Psychological Research, 3, 111–121. doi: 10.21500/20112084.857 [DOI] [Google Scholar]
- Miller MN, & Pumariega AJ (2001). Culture and eating disorders: A historical and cross-cultural review. Psychiatry: Interpersonal and Biological Processes, 64, 93–110. [DOI] [PubMed] [Google Scholar]
- Nagata JM, Garber AK, Tabler JL, Murray SB, & Bibbins-Domingo K (2018). Prevalence and correlates of disordered eating behaviors among young adults with overweight or obesity. Journal of General Internal Medicine, 33, 1337–1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pike KM, & Dunne PE (2015). The rise of eating disorders in Asia: A review. Journal of Eating Disorders, 3, 33. doi: 10.1186/s40337-015-0070-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinaquy S, Chabrol H, Simon C, Louvet JP, & Barbe P (2003). Emotional eating, alexithymia, and binge-eating disorder in obese women. Obesity Research, 11, 195–201. [DOI] [PubMed] [Google Scholar]
- R Core Team. (2018). R: A language and environment for statistical computing (version 3.5.0). Vienna: R Foundation for Statistical Computing. [Google Scholar]
- Revelle W (2014). psych: Procedures for psychological, psychometric, and personality research. Evanston, IL: Northwestern University. [Google Scholar]
- Rosseel Y (2012). Lavaan: An R package for structural equation modeling and more: Version 0.5-12 (BETA). Journal of Statistical Software, 48(2), 1–36. [Google Scholar]
- Schmidt U, Adan R, Böhm I, Campbell IC, Dingemans A, Ehrlich S, . . . Himmerich H (2016). Eating disorders: The big issue. Lancet Psychiatry, 3, 313–315. [DOI] [PubMed] [Google Scholar]
- Shi M, Kong F, Chen H, & Cheng D (2011). Applicability of Three-Factor Eating Questionnaire among Chinese women undergraduates. Chinese Journal of Clinical Psychology, 19, 737–739. [Google Scholar]
- Shmueli D, & Prochaska JJ (2009). Resisting tempting foods and smoking behavior: Implications from a self-control theory perspective. Health Psychology, 28, 300–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout PE, & Fleiss JL (1979). Intraclass correlations: Uses in assessing rater reliability. Psychological Bulletin, 86, 420–428. [DOI] [PubMed] [Google Scholar]
- Stunkard AJ, & Messick S (1985). The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. Journal of Psychosomatic Research, 29, 71–83. [DOI] [PubMed] [Google Scholar]
- Tong J, Miao S, Wang J, Yang F, Lai H, Zhang C, … & Hsu LG (2014). A two-stage epidemiologic study on prevalence of eating disorders in female university students in Wuhan, China. Social psychiatry and psychiatric epidemiology, 49, 499–505. [DOI] [PubMed] [Google Scholar]
- van de Schoot R, Lugtig P, & Hox J (2012). A checklist for testing measurement invariance. European Journal of Developmental Psychology, 9, 486–492. [Google Scholar]
- van Strien T, Herman CP, & Verheijden MW (2012). Eating style, overeating and weight gain: A prospective 2-year follow-up study in a representative Dutch sample. Appetite, 59, 782–789. [DOI] [PubMed] [Google Scholar]
- Walker AK, Ibia IE, & Zigman JM (2012). Disruption of cue-potentiated feeding in mice with blocked ghrelin signaling. Physiology & Behavior, 108, 34–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang B-Y, Chen J-Z, Liu Y, Liu J, Guo T, & Tieli VEC (2015). Validity and reliability of the Chinese Version of the Eating Attitudes Test in Chinese college students. Chinese Mental Health Journal, 29, 150–155. [Google Scholar]
- Wang Y, Mi J, Shan X, Wang QJ, & Ge K (2007). Is China facing an obesity epidemic and the consequences? The trends in obesity and chronic disease in China. International Journal of Obesity, 31, 177–188. [DOI] [PubMed] [Google Scholar]
- Wardle J, & Carnell S (2009). Appetite is a heritable phenotype associated with adiposity. Annals of Behavioral Medicine, 38(Suppl. 1), S25–S30. [DOI] [PubMed] [Google Scholar]
- Wardle J, Guthrie CA, Sanderson S, & Rapoport L (2001). Development of the children’s Eating Behaviour Questionnaire. Journal of Child Psychology and Psychiatry, 42, 963–970. [DOI] [PubMed] [Google Scholar]
- Watkins MP, & Portney L (2009). Foundations of clinical research: Applications to practice. Upper Saddle River, NJ: Prentice Hall. [Google Scholar]
- Williams EP, Mesidor M, Winters K, Dubbert PM, & Wyatt SB (2015). Overweight and obesity: Prevalence, consequences, and causes of a growing public health problem. Current Obesity Reports, 4, 363–370. [DOI] [PubMed] [Google Scholar]
- Wright SM, & Aronne LJ (2012). Causes of obesity. Abdominal Radiology, 37, 730–732. [DOI] [PubMed] [Google Scholar]
- Wu Y (2006). Overweight and obesity in China: The once lean giant has a weight problem that is increasing rapidly. British Medical Journal, 333, 362–363. doi: 10.1136/bmj.333.7564.362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng Q, He Y, Dong S, Zhao X, Chen Z, Song Z, . . . Wang Y (2014). Optimal cut-off values of BMI, waist circumference and waist: height ratio for defining obesity in Chinese adults. British Journal of Nutrition, 112, 1735–1744. [DOI] [PubMed] [Google Scholar]
- Zhou BF (2002). Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults: Study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomedical and Environmental Sciences, 15, 83–96. [PubMed] [Google Scholar]
- Zickgraf Hana F., & Ellis Jordan M. (2018). Initial validation of the nine item avoidant/restrictive food intake disorder screen (nias): A measure of three restrictive eating patterns. Appetite, 123, 32–42. [DOI] [PubMed] [Google Scholar]
- Zickgraf HF, Franklin ME, & Rozin P (2016). Adult picky eaters with symptoms of avoidant/restrictive food intake disorder: Comparable distress and comorbidity but different eating behaviors compared to those with disordered eating symptoms. Journal of Eating Disorders, 4, 26. doi: 10.1186/s40337-016-0110-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zickgraf HF, & Rigby A (2018). The Adult Eating Behaviour Questionnaire in a bariatric surgery-seeking sample: Factor structure, convergent validity, and associations with BMI. European Eating Disorders Review, 27, 97–104. doi: 10.1002/erv.2628 [DOI] [PMC free article] [PubMed] [Google Scholar]


