SARS (severe acute respiratory syndrome) was a new disease in the fall of 2002, which first occurred in Guangdong Province, China and spread to 29 countries with 8422 cases and 916 fatalities (1–3). After an unprecedented global public health effort, the epidemic was controlled within 7 mo of its original occurrence (4). The scientific effort demonstrated unusual international cooperation and was facilitated by electronic communication. Media coverage was incredibly accurate and provided worldwide pictures to augment scientific data. As of March 1, 2004, there were 1695 citations related to SARS in the medical literature. Of interest, however, is that of these citations only 0.1% are related to pediatric experiences. The purpose of this mini-review is to examine the unique pediatric aspects of SARS, to review the epidemiology of the SARS-CoV in regard to future epidemics, and to use the SARS experience as a model for future pandemics.
DISCUSSION
The first train of transmission of SARS occurred in Fosham City, Guangdong Province, China (2, 4). During the period from November 16, 2002, until February 9, 2003, there were 305 cases reported in Guangdong Province. SARS was spread to Hong Kong on February 22, 2003, by a patient from Guangdong Province who, before his hospitalization, stayed in the Metropole Hotel in Hong Kong for 1 d. Ten secondary cases occurred in hotel guests, and these infected persons led directly to tertiary cases in two Hong Kong hospitals and outbreaks in Singapore, Toronto, and Hanoi (5).
In March 2003, a novel coronavirus (SARS-CoV) (Fig. 1) was isolated from patients with SARS and subsequently sequenced (6–11). This virus was rapidly identified and characterized by a combination of classical virological methods and cutting-edge molecular biology. Electron microscopic examination of swabs and sputum specimens from affected patients revealed the presence of viral particles. Fortuitously, this newly identified agent replicated in Vero cells, in contrast to other human coronaviruses. Cytopathic effect was seen by 5–6 d after inoculation. In a technological Blitzkrieg, the genome was completely and rapidly sequenced by several laboratories. A low-stringency, random primer reverse transcription PCR method was used by Drosten et al. (8) to amplify short fragments of DNA using RNA recovered from culture supernatants as the template. This method, previously used to identify the human metapneumovirus, was successful again: 3 of 20 fragments identified showed homology to known coronavirus sequences. In a similar approach Marra et al. (7) began by the construction of random primed and oligo-dT primed cDNA library, beginning with viral RNA recovered from a highly purified virus preparation. These and other molecular tricks of the trade were used to rapidly establish complete sequences of the SARS-CoV. This was no small feat. Coronaviruses have the largest genomes (∼30,000 bases of positive-sense RNA) found in any RNA virus. These sequence data not only permitted the rapid development of highly specific diagnostic tests, but also helped in the epidemiologic tracking of the pandemic. Moreover, cataloging the genome from human cases assisted in the search for the origin of this disease, when viruses related to the SARS-CoV were identified in animals [Himalayan palm civets (Paguma larvata) and raccoon dogs (Nyctereutes procyonoides)] in a live animal market in Shenzhen, China (12). Viral genomes from nasal swabs from palm civets were 99.8% homologous to the human SARS CoV, and represented a distinct phylogenetic group from the human isolates. Moreover, early in the epidemic, open reading frame 8 sequences from human isolates were identical to those from palm civets, suggesting animal to human transmission. As the pandemic progressed, most human isolates contained a SARS-CoV sequence with a deletion of 29 nucleotides in this open reading frame. Signature sequences were also identified in the amino acid sequences of the spike protein, which is involved in the attachment of viral particles. It is unclear whether these changes represent adaptive mutation to replication in humans. However, coronaviruses, like other RNA viruses, mutate rapidly as a consequence of the error-prone nature of RNA polymerases and their characteristically short replicative life cycles. Thus, minor (perhaps inconsequential) mutations can emerge rapidly and persist as a founder effect. Despite the known high rate of recombination seen with other coronaviruses (13), there has been no evidence to date that this pandemic reflected the recombination of human and nonhuman coronaviruses, although this predilection could conceivably enhance the diversity of the SARS-CoV and result in a larger catastrophic pandemic.
Figure 1.
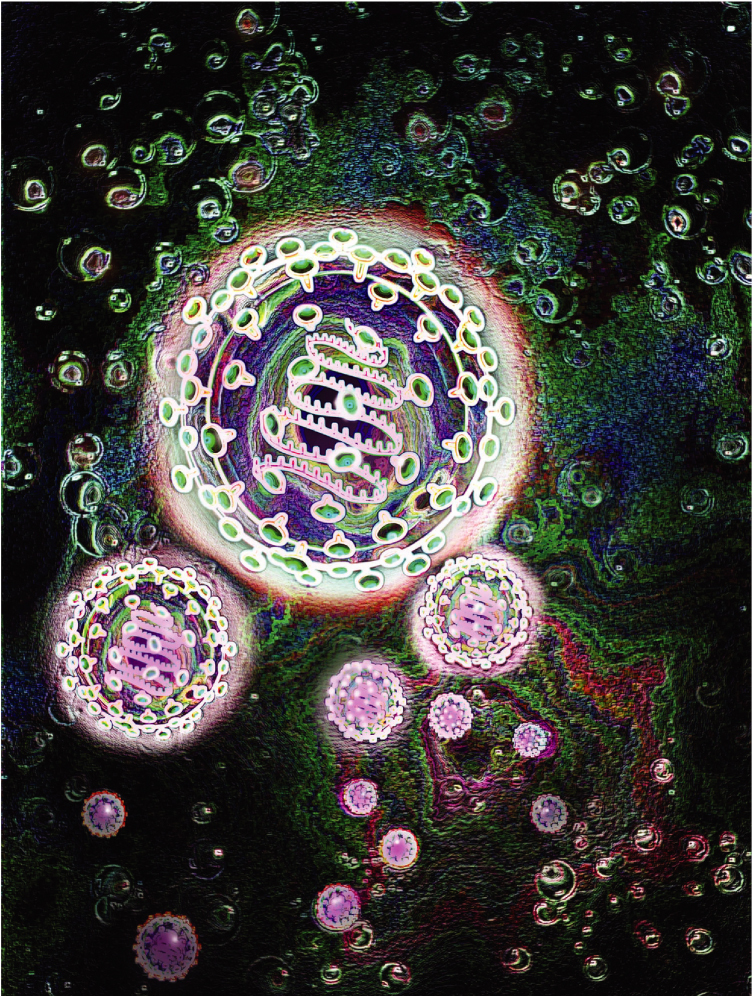
Illustration of SARS virus, a member of the Coronavirus family. The membrane and protein envelope (violet) surround a genome of single stranded RNA. The entire virus is surrounded by glycoproteins (orange) that suggest a corona or crown. © Jim Dowdalls /Photo Researchers, Inc.
Also of interest, in the investigation in the live animal market, was that 8 of 20 (40%) wild animal traders and 3 of 15 (20%) of those who slaughter the animals had antibody to the animal coronaviruses (12). In contrast, only 1 of 20 (5%) vegetable traders in the same market were seropositive, supporting the hypothesis that the SARS-CoV originated in these animals.
The epidemiology of SARS is both extremely interesting and frightening (2, 5, 14). As noted above, SARS spread to Hong Kong on February 22, 2003. The ten secondary cases associated with the Metropole Hotel lead to worldwide dissemination, which eventually involved 29 countries (5). How the 10 secondary cases acquired the disease at the Metropole Hotel is not known. Eight of the cases resided on the 9th floor, which was the same floor as the primary case. Since the index patient vomited in the hall of the 9th floor and this was subsequently cleaned by vacuuming, it is possible that an aerosol was created.
Of particular interest was the point source outbreak, which involved the Amoy Gardens housing complex, Kowloon Bay, Hong Kong (2, 3, 14). The primary case in this outbreak was a 33-y-old man who lived in Shenzhen. He had chronic renal disease and he frequently visited his brother in Amoy Gardens when he made visits to the Prince of Wales Hospital, where his renal disease was being treated. On March 14 and 19, 2003, he visited his brother who lived in a flat in Block E of the housing complex, which had 15 high-rise units (blocks). The patient had diarrhea at the time of his visits and used the toilet in his brother's unit. During the following month, 321 SARS cases occurred in Amoy Gardens, with 41% occurring in Block E residents. The peak of the outbreak occurred on March 24, 2003, and the Block E cases appeared earlier and showed a point-source-type distribution.
Subsequent study suggested that the secondary cases in Block E were due to aerosolization of contaminated sewage through floor vents when toilets were flushed and exhaust fans in bathrooms were switched on.
The transmissibility of the virus and human disease is a paradox. On the one hand, in the initial phases of the spread of SARS in Hong Kong, Singapore, and Toronto, a disproportionate number of health care workers became ill and apparent “superspreader” cases were noted (2–4, 6, 11, 14–18). In contrast, the secondary illness rate in households was only 15% in a Hong Kong study and 6% in a study in Singapore (19, 20). These household-contact rates are significantly less than occur with other respiratory infections such as pertussis and measles. With the exception of the Amoy Gardens outbreak and the secondary cases in the Metropole Hotel, most other instances of superspreading involved contact by hospital personnel who gave care and had contact with the primary cases without carrying out infection control precautions.
SARS spread rapidly around the world during March 2003 by infected persons who traveled by airplane. Surprising, there were relatively few secondary cases acquired by co-airline passengers (3, 21). Between February 23 and May 23, 2003, there were 40 known airline flights with symptomatic probable cases on board (3). A total of only 29 secondary cases have been linked to probable cases of SARS who traveled while symptomatic. However, on one flight from Hong Kong to Beijing with one symptomatic passenger, 22 of the 119 (18%) contacts became ill.
The incubation period of SARS is 2–10 d, with a median of 4–6 d (3). The attack rate in children is reported to be less than that of adults, but when consideration is given to the large number of nosocomial cases in original data sets, it appears that children have similar rates as adults.
Clinical disease in children is clearly less severe than disease in adults (2, 6, 17, 18, 22–33). Adolescents have illness similar to adults, but the case fatality rate in adolescents is significantly less. Although there is evidence that unrecognized infections occur, there is only one reported instance of a possible asymptomatic infection with the SARS-CoV (33).
Details of clinical illness in children have been presented from studies in Hong Kong, Singapore, Toronto, and Eastern Taiwan. The largest single experience occurred at the Princess Margaret Hospital in Hong Kong (25). The experience there was unique in that 31 (70.5%) of the hospitalized children were from the Amoy Gardens point-source outbreak. In a review of 62 pediatric patients seen in Toronto, Singapore, and Hong Kong, the following clinical findings were noted: fever, 100%; cough, 63%; rhinorrhea, 23%; myalgia, 18%; chills, 15%; and headache, 17% (32). In patients < 10 y of age, the most common findings when initially seen were fever and cough, whereas older children (≥10 y) also had headache, myalgia, sore throat, chills, and/or rigor. In this study, all cases categorized as probable SARS had abnormal chest radiographs or computerized tomography (CT). The most prominent radiographic findings were patchy infiltrates, opacities, and/or areas of consolidation. Multifocal lesions were seen in 23% of the radiographs. Hilar adenopathy, extensive pleural effusions, lung abscess, pneumatocele, or pneumothorax were not observed. On CT scan, unifocal or multifocal regions of consolidation and/or ground-glass opacities were observed throughout the lung fields.
The most striking laboratory finding is absolute lymphopenia. This occurs in nearly all pediatric patients. In one study, 57% of children had lymphopenia on presentation, and this frequency rose to 91% (28). The mean value was 0.9 ± 0.7 × 10−9/L. Other frequently abnormal laboratory findings include thrombocytopenia and elevated lactate dehydrogenase and creatinine phosphokinase.
The vast majority of children who were hospitalized with SARS were treated with i.v. or orally administered ribavirin. In Hong Kong, most children were also treated with steroids, whereas in Toronto none of the children received steroid treatment (25, 28, 29). Only a small number of children required oxygen supplementation and intensive care and, to our knowledge, no fatalities in children have occurred.
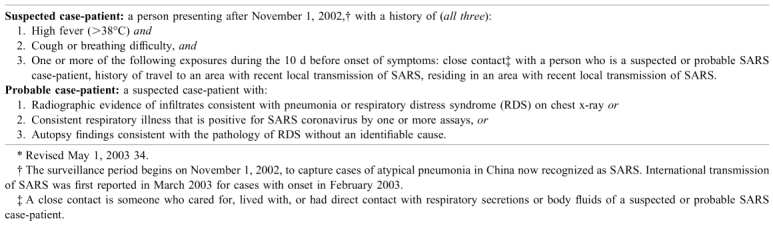
The initial diagnosis of SARS was based upon clinical and epidemiologic data. The World Health Organization SARS case definition is presented in the Table 1 (34). A revised U.S. surveillance case definition was published in December 2003 (35). Laboratory confirmation of a SARS-CoV infection can be determined by the demonstration of serum antibody by ELISA, isolation of the virus from a clinical specimen, or the detection of SARS-CoV RNA by a reverse transcription PCR assay (6, 36, 37).
Table 1.
World Health Organization SARS case definitions*
At the present time, there are two key questions that relate to SARS: Will the disease reoccur? And, if it does, how should it be treated and can it be contained? This year, two laboratory confirmed cases of SARS have been identified in Guangong Province, China, and no secondary cases have occurred (38). Severe disease in humans who are infected with animal viruses are an ever-present danger. Although perhaps HIV infection is an exception, the only animal viruses that have caused pandemic human disease and continued human to human spread over periods of years are influenza A viruses. Other severe diseases acquired from animals such as rabies, Lassa fever, and Ebola hemorrhagic fever, all of which can be transmitted from person to person, have not resulted in sustained human disease. It would appear that the SARS-CoV should also be similarly grouped. The SARS pandemic of 2002–2003 had two initial events that led to its worldwide dissemination. In retrospect, it seems likely that aerosolization of the virus at the Metropole Hotel, Amoy Gardens, and perhaps in some nosocomial situations made the introduction of this virus different from experiences with Lassa and Ebola viruses.
However, concern has to be raised as to the possibility of a future genetic recombinant virus with the SARS-CoV and a human respiratory CoV such as OC43 or 229E strains. Because live animals and humans have close contact in Southern China and infections with human CoV are common, dual infection seems quite possible. However, this type of recombination among different groups of CoV has, to our knowledge, never been documented. Far more likely, however, is the occurrence of a recombinant between a strain of avian influenza (such as H5N1) and a circulating human strain (such as H3N2). From past experience it appears that an influenza pandemic will occur in the next few years. Hopefully, lessons learned from the international response to SARS will contribute to its control.
The pathophysiologic events in SARS are not clear. The illness in adults is biphasic and occasionally triphasic (6, 17, 18, 22–24, 39, 40). The biphasis illness is characterized by an initial febrile period, which is otherwise relatively symptom free, and then a period of respiratory symptoms, chills/rigor, and vomiting and diarrhea. Maximum virus shedding occurs during the second phase. About 15% of adults will have a third phase characterized by acute respiratory distress syndrome. Children in general have a single-phase disease and illness in adolescents is biphasic but generally less severe that that seen in older adults (2, 25, 28–32).
Initial therapy, which was developed on medical services, used both antiviral (ribavirin) and anti-inflammatory (steroids) treatment. The rationale for steroids was based on the perception that severe lung damage was occurring as a result of a “cytokine storm” (2). This thought was enhanced by the fact that illness in SARS was similar to illnesses in adults due to infection with avian influenza (H5N1). Laboratory studies with H5N1 virus in tissue culture noted the induction of proinflammatory cytokines (41). The most notable laboratory finding in SARS is the profound lymphopenia. Cui et al. (42) noted that CD4+ T cells were reduced in all patients, CD8+ cells in 87%, B-lymphocytes in 76%, and natural killer cells in 55% of patients. In patients who recover from SARS there is a rapid restoration of lymphocytes in peripheral blood (43).
SARS-CoV experimental infections in macaques suggest that pulmonary pathology is due to a direct viral effect on type 1 pneumocytes (44). At the present, when therapy of pediatric SARS patients is considered, it seems clear that there is no indication for routine treatment with steroids inasmuch as children in Toronto who did not receive steroids did equally well as those treated in Hong Kong with steroids. In regard to antiviral therapy, it is disappointing that no laboratory data have become available regarding the evaluation of ribavirin treatment (45). At the present time, the use of ribavirin either i.v. or orally is the standard of care. Laboratory studies have suggested that pegylated interferon-α and interferon-β might be useful therapeutic agents (44, 46). An uncontrolled study in adults in Toronto suggested that patients treated with interferon alfacon-1 plus steroids had more rapid recovery than patients treated with steroids alone (47).
Although it seems unlikely to us that pandemic infection with the SARS-CoV will ever occur, there has been considerable effort to develop a vaccine (48). To us, this seems ill advised for two reasons. First, if a reoccurrence of pandemic disease were to occur, it is likely, since its origin will be from an animal, that the new virus will be different from the present human SARS-CoV. Secondly, vaccines against known animal CoV have had varied results. Of particular concern in this regard is the possibility of enhanced SARS rather than protection. This has happened before in humans with other RNA viruses (measles and respiratory syncytial virus) and it has happened in the animal setting with a feline CoV vaccine (Denison MR, personal communication).
At the present time, the most important factor in preventing a future epidemic or pandemic of SARS, as well as epidemics or pandemics with other new viruses, is sound public health policy and the use of standard infection control procedures. SARS gained a foothold because of an unusual event (probable aerosol dissemination), and the failure to recognize the problem and to initially use respiratory isolation procedures, and to use quarantine measures. In the United States in 2003 we were lucky because very few of the probable cases were actually infected with the SARS-CoV. In the spring of 2003, one of us surveyed a number of hospitals, including our own, and found that if a patient with SARS were to visit a clinic or emergency room, large numbers of persons would have been exposed before the problem was recognized. A further problem is that all hospitals built during the last 30 y and those being built today do not have the capacity to handle large numbers of patients who require respiratory isolation.
References
- 1.World Health Organization. 2002 Summary of probable SARS cases by onset of illness from 1 November 2002 to 31 July 2003. Available at: http://www.who.int/scr/sars/country/table2004_04_21/en/print.html
- 2.Hon E, Li A, Nelson EAS, Leung CW, Cherry JD. Textbook of Pediatric Infectious Diseases. 2003. Severe acute respiratory syndrome (SARS) pp. 2389–2393. [Google Scholar]
- 3.World Health Organization 2003 Consensus document on the epidemiology of severe acute respiratory syndrome (SARS). Global Health SecurityEpidemic Alert & Response11: 1–44
- 4.World Health Organization 2003 Severe acute respiratory syndrome (SARS). Report by the Secretariat EB113/33
- 5.Centers for Disease Control and Prevention 2003 Update: outbreak of severe acute respiratory syndrome—worldwide 2003. MMWR Morb Mortal Wkly Rep52: 241–248. [PubMed]
- 6.Peiris JS, Yuen KY, Osterhaus AD, Stöhr K. The severe acute respiratory syndrome. N Engl J Med. 2003;349:2431–2441. doi: 10.1056/NEJMra032498. [DOI] [PubMed] [Google Scholar]
- 7.Marra MA, Jones SJ, Astell CR, Holt RA, Brooks-Wilson A, Butterfield YS, Khattra J, Asano JK, Barber SA, Chan SY, Cloutier A, Coughlin SM, Freeman D, Girn N, Griffith OL, Leach SR, Mayo M, McDonald H, Montgomery SB, Pandoh PK, Petrescu AS, Robertson AG, Schein JE, Siddiqui A, Smailus DE, Stott JM, Yang GS, Plummer F, Andonov A, Artsob H, Bastien N, Bernard K, Booth TF, Bowness D, Czub M, Drebot M, Fernando L, Flick R, Garbutt M, Gray M, Grolla A, Jones S, Feldmann H, Meyers A, Kabani A, Li Y, Normand S, Stroher U, Tipples GA, Tyler S, Vogrig R, Ward D, Watson B, Brunham RC, Krajden M, Petric M, Skowronski DM, Upton C, Roper RL. The genome sequence of the SARS-associated coronavirus. Science. 2003;300:1399–1404. doi: 10.1126/science.1085953. [DOI] [PubMed] [Google Scholar]
- 8.Drosten C, Günther S, Preiser W, van der Werf S, Brodt HR, Becker S, Rabenau H, Panning M, Kolesnikova L, Fouchier RA, Berger A, Burguière AM, Cinatl J, Eickmann M, Escriou N, Grywna K, Kramme S, Manuguerra JC, Müller S, Rickerts V, Stürmer M, Vieth S, Klenk H-D, Osterhaus AD, Schmitz H, Doerr HW. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N Engl J Med. 2003;348:1967–1976. doi: 10.1056/NEJMoa030747. [DOI] [PubMed] [Google Scholar]
- 9.Rota PA, Oberste MS, Monroe SS, Nix WA, Campagnoli R, Icenogle JP, Peñaranda S, Bankamp B, Maher K, Chen MH, Tong S, Tamin A, Lowe L, Frace M, DeRisi JL, Chen Q, Wang D, Erdman DD, Peret TC, Burns C, Ksiazek TG, Rollin PE, Sanchez A, Liffick S, Holloway B, Limor J, McCaustland K, Olsen-Rasmussen M, Fouchier R, Günther S, Osterhaus AD, Drosten C, Pallansch MA, Anderson LJ, Bellini WJ. Characterization of a novel coronavirus associated with severe acute respiratory syndrome. Science. 2003;300:1394–1399. doi: 10.1126/science.1085952. [DOI] [PubMed] [Google Scholar]
- 10.Ksiazek TG, Erdman D, Goldsmith CS, Zaki SR, Peret T, Emery S, Tong S, Urbani C, Comer JA, Lim W, Rollin PE, Dowell SF, Ling AE, Humphrey CD, Shieh WJ, Guarner J, Paddock CD, Rota P, Fields B, DeRisi J, Yang JY, Cox N, Hughes JM, LeDuc JW, Bellini WJ, Anderson LJ, SARS Working Group A novel corona-virus associated with severe acute respiratory syndrome. N Engl J Med. 2003;348:1953–1966. doi: 10.1056/NEJMoa030781. [DOI] [PubMed] [Google Scholar]
- 11.Holmes KV, Enjuanes L. Virology. The SARS coronavirus: a postgenomic era. Science. 2003;300:1377–1378. doi: 10.1126/science.1086418. [DOI] [PubMed] [Google Scholar]
- 12.Guan Y, Zheng BJ, He YQ, Liu XL, Zhuang ZX, Cheung CL, Luo SW, Li PH, Zhang LJ, Guan YJ, Butt KM, Wong KL, Chan KW, Lim W, Shortidge KF, Yuen KY, Peiris JS, Poon LL. Isolation and characterization of viruses related to the SARS coronavirus from animals in southern China. Science. 2003;302:276–278. doi: 10.1126/science.1087139. [DOI] [PubMed] [Google Scholar]
- 13.Lai MMC. Recombination in large RNA viruses: coronaviruses. Semin Virology. 1996;7:381–388. doi: 10.1006/smvy.1996.0046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Department of Health 2003 Outbreak of severe acute respiratory syndrome (SARS) at Amoy Gardens, Kowloon Bay, Hong Kong, main findings of the investigation. Available at: http://www.info.gov.hk/info/ap/pdf/amoy_e.pdf
- 15.Centers for Disease Control and Prevention 2003 Severe acute respiratory syndrome—Singapore, 2003. MMWR Morb Mortal Wkly Rep52: 405–413. [PubMed]
- 16.Centers for Disease Control and Prevention 2003 Cluster of severe acute respiratory syndrome cases among protected health-care workers—Toronto, Canada, April 2003. MMWR Morb Mortal Wkly Rep52: 433–436. [PubMed]
- 17.Hsu L-Y, Lee C-C, Green JA, Ang B, Paton NI, Lee L, Villacian JS, Lim PL, Earnest A, Leo YS. Severe acute respiratory syndrome (SARS) in Singapore: clinical features of index patient and initial contacts. Emerg Infect Dis. 2003;9:713–717. doi: 10.3201/eid0906.030264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee N, Hui D, Wu A, Chan P, Cameron P, Joynt GM, Ahuja A, Yung MY, Leung CB, To KF, Lui SF, Szeto CC, Chung S, Sung JJ. A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med. 2003;348:1986–1994. doi: 10.1056/NEJMoa030685. [DOI] [PubMed] [Google Scholar]
- 19.Goh DL, Lee BW, Chia KS, Heng BH, Chen M, Ma S, Tan CC. Secondary household transmission of SARS, Singapore. Emerg Infect Dis. 2004;10:232–234. doi: 10.3201/eid1002.030676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lau JT, Lau M, Kim JH, Tsui HY, Tsang T, Wong TW. Probable secondary infections in households of SARS patients in Hong Kong. Emerg Infect Dis. 2004;10:235–243. doi: 10.3201/eid1002.030626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Olsen SJ, Chang HL, Cheung TY, Tang AF, Fisk TL, Ooi SP, Kuo HW, Jiang DD, Chen KT, Lando J, Hsu KH, Chen TJ, Dowel SF. Transmission of severe acute respiratory syndrome on aircraft. N Engl J Med. 2003;349:2416–2422. doi: 10.1056/NEJMoa031349. [DOI] [PubMed] [Google Scholar]
- 22.Booth CM, Matukas LM, Tomlinson GA, Rachlis AR, Rose DB, Dwosh HA, Walmsley SL, Mazzulli T, Avendano M, Derkach P, Ephtimios IE, Kitai I, Mederski BD, Shadowitz SB, Gold WL, Hawryluck LA, Rea E, Chenkin JS, Cescon DW, Poutanen SM, Detsky AS. Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. JAMA. 2003;289:2801–2809. doi: 10.1001/jama.289.21.JOC30885. [DOI] [PubMed] [Google Scholar]
- 23.Lew TW, Kwek TK, Tai D, Earnest A, Loo S, Singh K, Kwan KM, Chan Y, Rim CF, Bek SL, Kor AC, Yap WS, Chelliah YR, Lai YC, Goh SK. Acute respiratory distress syndrome in critically ill patients with severe acute respiratory syndrome. JAMA. 2003;290:374–380. doi: 10.1001/jama.290.3.374. [DOI] [PubMed] [Google Scholar]
- 24.Peiris JS, Chu CM, Cheng VC, Chan KS, Hung IF, Poon LL, Law KI, Tang BS, Hon TY, Chan CS, Chan KH, Ng JS, Zheng BJ, Ng WL, Lai RW, Guan Y, Yuen KY, HKU/UCH Study Group Clinical progression and viral load in a community outbreak of coronavirus-associated SARS pneumonia: a prospective study. The Lancet. 2003;361:1767–1772. doi: 10.1016/S0140-6736(03)13412-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Leung CW, Kwan YW, Ko PW, Chiue SS, Loung PY, Fong NC, Lee LP, Hui YW, Law HK, Wong WH, Chan KH, Peiris JS, Lim WW, Lau YL, Chiu MC 2004 Severe acute respiratory syndrome in children. Pediatrics (in press) [DOI] [PubMed]
- 26.Shek CC, Ng PC, Fung GP, Cheng FW, Chan PK, Peiris MJ, Lee KH, Wong SF, Cheung HM, Li AM, Hon EK, Yeung CK, Chow CB, Tam JS, Chiu MC, Fok TF. Infants born to mothers with severe acute respiratory syndrome. Pediatrics. 2003;112:e254. doi: 10.1542/peds.112.4.e254. [DOI] [PubMed] [Google Scholar]
- 27.Ng PC, Lam CW, Li AB, Wong CK, Cheng FW, Leung TF, Hon EK, Chan IH, Li CK, Fung KS, Fok TF. Inflammatory cytokine profile in children with severe acute respiratory syndrome. Pediatrics. 2004;113:e7–e14. doi: 10.1542/peds.113.1.e7. [DOI] [PubMed] [Google Scholar]
- 28.Chiu WK, Cheung PC, Ip PL, Sugunan VK, Luk DC, Ma LC, Chan BH, Lo KL, Lai WM. Severe acute respiratory syndrome in children: experience in a regional hospital in Hong Kong. Pediatr Crit Care Med. 2003;4:279–283. doi: 10.1097/01.PCC.0000077079.42302.81. [DOI] [PubMed] [Google Scholar]
- 29.Bitnun A, Allen U, Heurter H, King SM, Opavsky MA, Ford-Jones EL, Matlow A, Kitai I, Tellier R, Richardson S, Manson D, Babyn P, Read S, other members of the Hospital for Sick Children SARS Investigation Team Children hospitalized with severe acute respiratory syndrome-related illness in Toronto. Pediatrics. 2003;112:e261. doi: 10.1542/peds.112.4.e261. [DOI] [PubMed] [Google Scholar]
- 30.Sit SC, Yau EK, Lam YY, Ng DK, Fong NC, Hui YW, Cheng WF, Leung CW, Chiu MC. A young infant with severe acute respiratory syndrome. Pediatrics. 2003;112:e257. doi: 10.1542/peds.112.4.e257. [DOI] [PubMed] [Google Scholar]
- 31.Fong NC, Kwan YW, Hui YW, Yuen LK, Yau EK, Leung CW, Chiu MC. Adolescent twin sisters with severe acute respiratory syndrome (SARS) Pediatrics. 2004;113:e146–e149. doi: 10.1542/peds.113.2.e146. [DOI] [PubMed] [Google Scholar]
- 32.Babyn PS, Chu WC, Tsou IY, Wansaicheong GK, Allen U, Bitnum A, Chee TS, Cheng FW, Chiu MC, Fok TF, Hon EK, Gahunia HK, Kaw GJ, Khong PK, Leung CW, Li AM, Manson D, Metreweli C, Ng PC, Read S, Stringer DA. Severe acute respiratory syndrome (SARS): chest radiographic features in children. Pediatr Radiol. 2004;34:47–58. doi: 10.1007/s00247-003-1081-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee HK, Tso EY, Chau TN, Tsang OT, Choi KW, Lai TS. Asymptomatic severe acute respiratory syndrome-associated coronavirus infection. Emerg Infect Dis. 2003;9:1491–1492. doi: 10.3201/eid0911.030401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.World Health Organization 2003 Case definitions for surveillance of severe acute respiratory syndrome (SARS). Available at: http://www.who.int/csr/sars/casedefinition/en/print.html
- 35.Centers for Disease Control and Prevention 2003 Update: influenza activity—United States, 2003-04 season. MMWR Morb Mortal Wkly Rep52: 1197–1202. [PubMed]
- 36.Chan KH, Poon LL, Cheng VC, Guan Y, Hung IF, Kong J, Yam LY, Seto WG, Yuen KY, Peiris JS. Detection of SARS coronavirus in patients with suspected SARS. Emerg Infect Dis. 2004;10:294–299. doi: 10.3201/eid1002.030610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jernigan JA, Low DE, Helfand RF. Combining clinical and epidemiologic features for early recognition of SARS. Emerg Infect Dis. 2004;10:327–333. doi: 10.3201/eid1002.030741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hong Kong Government Information Centre 2004 Two SARS cases confirmed in Guangdong. http://www.info.gov.hk/gia/genereal/200401/17/0117172.htm. Accessed 3/21/04
- 39.Low DE, McGeer A. SARS— one year later. N Engl J Med. 2003;349:2381–2382. doi: 10.1056/NEJMp038203. [DOI] [PubMed] [Google Scholar]
- 40.Mazzulli T, Farca GA, Poutanen SM, Willey BM, Low DE, Butany J, Asa SL, Kain KC. Severe acute respiratory syndrome-associated coronavirus in lung tissue. Emerg Infect Dis. 2004;10:20–24. doi: 10.3201/eid1001.030404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cheung CY, Poon LL, Lau AS, Luk W, Lau YL, Shortridge KF, Gordon S, Guan Y, Peiris JS. Induction of proinflammatory cytokines in human macrophages by influenza A (H5N1) viruses: a mechanism for the unusual severity of human disease? Lancet. 2002;360:1831–1837. doi: 10.1016/S0140-6736(02)11772-7. [DOI] [PubMed] [Google Scholar]
- 42.Cui W, Fan Y, Wu W, Zhang F, Wang J-Y, Ni A-P. Expression of lymphocytes and lymphocyte subsets in patients with severe acute respiratory syndrome. Clin Infect Dis. 2003;37:857–859. doi: 10.1086/378587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Li T, Qiu Z, Zhang L, Han Y, He W, Liu Z, Me X, Fan H, Lu W, Xie J, Wang H, Deng G, Wang A. Significant changes of peripheral T lymphocyte subsets in patients with severe acute respiratory syndrome. J Infect Dis. 2004;189:648–651. doi: 10.1086/381535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Haagmans BL, Kuiken T, Martina BE, Fouchier RA, Rimmlezwaan GF, Van Amerongen G, Van Riel D, De Jong T, Itamura S, Chang KH, Tashiro M, Osterhaus AD. Pegylated interferon-α protects type 1 pneumocytes against SARS corona-virus infection in macaques. Nat Med. 2004;10:290–293. doi: 10.1038/nm1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhaori G. Antiviral treatment of SARS: can we draw any conclusions? CMAJ. 2003;169:1165–1166. [PMC free article] [PubMed] [Google Scholar]
- 46.Cinatl J, Morgenstern B, Bauer G, Chandra P, Rabenau H, Doerr HW. Treatment of SARS with human interferons. Lancet. 2003;362:293–294. doi: 10.1016/S0140-6736(03)13973-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Loutfy MR, Blatt LM, Siminovitch KA, Ward S, Wolff B, Lho H, Pham DH, Deif H, LaMere EA, Chang M, Kain KC, Farcas GA, Ferguson P, Latchford M, Levy G, Dennis JW, Lai EK, Fish EN. Interferon alfacon-1 plus corticosteroids in severe acute respiratory syndrome: a preliminary study. JAMA. 2003;290:3222–3228. doi: 10.1001/jama.290.24.3222. [DOI] [PubMed] [Google Scholar]
- 48.Marshall E, Enserink M. Caution urged on SARS vaccines. Science. 2004;303:944–946. doi: 10.1126/science.303.5660.944. [DOI] [PubMed] [Google Scholar]


