Abstract
To test the role of neutralizing antibodies (nAbs) and receptor adaptation in interspecies transmission of influenza virus, two H5N1 strains, isolated from human and avian hosts, with four amino acid differences in hemagglutinin (HA) and seven HA mutations were studied. We found that a mutation at amino acid position 90 in the H5N1 HA, outside the receptor-binding domain (RBD), could simultaneously induce changes in the RBD conformation to escape from nAb binding and alter the receptor preference through long-range regulation. This mutation was deemed a “key event” for interspecies transmission. It is likely a result of positive selection caused by antibodies, allowing the original invasion by new species-specific variants. A mutation at amino acid position 160 in the RBD only induced a change in receptor preference. This mutation was deemed a “maintaining adaptation”, which ensured that influenza virus variants would be able to infect new organisms of a different species successfully. The mutation is the result of adaptation caused by the receptor. Our results suggest that continuing occurrence of these two types of mutations made the variants persist in the new host species.
Electronic supplementary material
The online version of this article (doi:10.1007/s00705-011-1056-2) contains supplementary material, which is available to authorized users.
Keywords: Influenza Virus, Sialic Acid, Avian Influenza, Avian Influenza Virus, Highly Pathogenic Avian Influenza
Introduction
Highly pathogenic avian influenza (HPAI) H5N1 infection represents a significant public-health risk in both poultry and humans. Lately, there has been much debate on whether avian H5N1 influenza virus can evolve into human H5N1 influenza viruses and result in major human pandemics. The recent global pandemic of swine influenza H1N1 virus further emphasizes the likelihood of an avian influenza pandemic. As a zoonotic disease, understanding the role of avian influenza virus evolution in interspecies transmission is essential for designing effective preventive measures [10].
Phylogenetic analysis has shown a strong association between viral variation and amino acid changes in the viral hemagglutinin (HA) [27]. Viral variation can be driven both by selective pressure by antibodies and receptor adaptation [25, 31]. The receptor of influenza virus consists of glycans terminated by sialic acid (SA) on the epithelial cell. Although a switch in the receptor specificity of avian influenza from Neu5Acα2-3Gal (α-2,3)-linked SA to Neu5Acα2-6Gal (α-2,6)-linked SA is considered a sign of evolution from avian to human host specificity [22, 31], antiviral neutralizing antibodies [1, 5, 8, 14, 15, 20, 22] were shown recently to be an important factor responsible for avian influenza virus variation during interspecies transmission. Evidence from the examination of infected human and avian serum samples also provides clues to the propensity of a virus to escape neutralization [12].
Small genetic changes sometimes have major effects on antigenicity [7, 16, 18, 30]. Here, we used natural H5N1 strains isolated from humans and birds with a panel of monoclonal antibodies (mAbs) to examine amino acid mutations and their impact on receptor adaptation and nAb reactivity. Two H5N1 strains, A/Bar-headed Goose/Qinghai/1/05 (QH) and A/Xinjiang/1/2006 (XJ), isolated from a bird and a human, respectively, with four amino acid difference in their HAs provided a good system for us to explore the mechanism of H5N1 to cross the species barrier. Based on sequence comparison, we generated seven QH HA mutants that mimicked the natural mutations. We also produced monoclonal antibodies against QH and XJ H5N1 HA. Using a panel of mAbs, we analyzed the binding and neutralization activities of these HA and HA mutants. We found that a mutation at aa 90 in the H5N1 HA, outside the receptor binding domain (RBD), could induce a conformational change of the RBD that allowed that virus to escape neutralization and, at the same time, change its receptor preference. This aa 90 mutation was deemed a “key event”, particularly during interspecies transmission, to break the species barrier. It was the result of positive selection caused by antibodies. A mutation at aa 160 in the RBD that only induces a change in receptor preference was deemed a “maintaining adaptation” to ensure that influenza virus variants would be able to successfully infect organisms of a different species. This was the result of an adaptation caused by the receptor. Our results suggest that the continuing occurrence of these two types of mutations made the variants persist in a new host species. Our observations provide insights on the pathway of viral evolution in interspecies transmission, which may also provide strategies to anticipate and address upcoming epidemics of avian influenza.
Materials and methods
HA genes and cells
Two HA genes (plasmids) of representative HPAI H5N1, A/Bar-headed Goose/Qinghai/1/05 (QH) (accession no. AAZ17522) and A/Xinjiang/1/2006 (XJ) (accession no. ACJ68614.1), were obtained from China Center for Disease Control and Chinese Academy of Sciences, respectively. 293T, MDCK, HeLa and DF-1 cells used in the pseudotype neutralization test were maintained in DMEM supplemented with 5% newborn calf serum (Sigma, St. Louis, MO) and antibiotics at 37°C in 5% CO2.
Expression of recombinant HA proteins
Briefly, Spodoptera frugiperda (Sf9) insect cells were propagated and maintained in Sf-900 II SFM (Gibco BRL). The HA ectodomain gene (from aa 17 to 532) was cloned into the transfer vector PacGP67b (BD Biosciences). The Sf9 cells were then co-transfected with the transfer vector and linearized baculovirus DNA (Invitrogen) to produce a recombinant baculoviruses containing the HA gene. The supernatant containing the virus was collected at 72 hours post-infection (PI). rHA proteins were expressed from the Sf-9 cells after 3 h PI. The supernatant from infected Sf-9 cells was collected and purified by Ni-NTA chromatography (GE Healthcare), using 6-His tags that had been added to the C-termini of the HA proteins. Western blotting using anti-His or anti-HA polyclonal antibodies was performed to confirm the rHA proteins.
Production of monoclonal antibodies
We immunized 6-8-week-old female BALB/c mice using rHAs (1-50 μg) with Freund’s adjuvant (i.h.). After a final boost, the mice were sacrificed, the splenocytes were fused with sp2/0 cells, and the hybridoma cells were cultivated in DMEM supplemented with 5% newborn calf serum at 37°C in 5% CO2. Positive hybridoma clones identified by ELISA were subcloned twice and conserved in liquid nitrogen. A protein G column (GE Healthcare) was used to purify the mAbs from the supernatant.
Peptide synthesis
The following peptides were synthesized, including 11 5-6-aa peptides (P1-P11) and 4 19-aa peptides (Pa-Pd), and their sequences were derived from HA. All peptides were biotinylated by adding a biotin tag at the N-terminus for detection in later assays. Peptides were synthesized by the Academy of Military Medical Sciences, China. The purity of each peptide was 90%, as shown by high-performance liquid chromatography analysis.
Neutralization assay
Full-length HA and neuraminidase (NA) genes were used to produce HA-pseudotyped viruses. Briefly, all HA, and NA variants were cloned into the pcDNA3.1 V5His TOPO expression vector after being sequenced. Western blotting was used to confirm the expression of HA and NA in 293T cells. Three plasmids, pcDNA3.1-HA, pcDNA3.1-NA, and the backbone plasmid pNL4-3 encoding HIV gag-pol and a firefly luciferase reporter gene were introduced together into 293T cells to produce a pseudotype virus. Forty-eight hours post-transfection, viral supernatants were harvested for neutralization assay. Test antibodies at different dilutions were incubated with an adequate amount of HA pseudotype viruses for 30 min at room temperature (RT). The mixture was then applied to MDCK, HeLa or DF-1 cells in 96-well plates. The infection efficiency was quantified by measuring the luciferase activity in the target cells with an EG&G Berthold Microplate Luminometer LB 96V. All experiments with pseudovirus were performed in a P2 laboratory.
ELISA assay
rHAs were coated onto a polystyrene plate at 4°C overnight. The plate was blocked with 5% bovine serum albumin (BSA) (Sigma) at 37°C for 2 h. After washing the plate, the mAbs (1 μg/ml) were added, and the plate was incubated at 37°C for 1 h. After washing the plate, HRP-labeled secondary anti-mouse IgG (1:5000) (Sigma) was added, and the plate was incubated at 37°C for 1 h. OPD/H2O2 was added, color development was stopped by addition of H2SO4, and the plates were read at 450/630 nm. A competition ELISA assay was used to detect the blocking effect of peptides against mAbs. Coating HAs (2 μg/ml) were placed on a polystyrene plate (100 μl/well) and kept at 4°C overnight. Peptides at a concentration of 10 μg/ml were added, and the plate was incubated at 37°C for 1 hour (100 μl/well). The plate was then washed, mAbs (5 μg/ml) were added, and incubation was continued at 37°C for 1 hour.
A solid-phase binding assay with competing glycopolymers was performed as described in a previous report for evaluation of receptor affinity (3). Briefly, HA proteins (1 μg/ml) were allowed to attach overnight at 4°C in 96-well plates. BSA (5%) was used to block the plates for 2 h at 37°C. Neu5Acα2-6GalNAcα-PAA-biotin or Neu5Acα2-3GalNAcα-PAA-biotin (GlycoTech) was added to the wells at the indicated concentration for 1 h at 37°C. Horseradish peroxidase (HRP)-conjugated avidin (1:5000) was added to the wells for the final coloration. The extent of the binding effect of the polymers was determined by measuring avidin activity.
Statistics
An unpaired Student t-test was used for statistical analysis of differences between NmAbs in binding to HAs.
Results
Neutralization and binding activities of mAbs against QH and XJ H5N1 HAs
It is known that selection and adaptation during viral evolution can determine the amino acid changes that become stable and dominant in a specific host species. The QH and XJ H5N1 strains, isolated from a bird and a human, respectively, were utilized to investigate selection- and adaptation-dependent H5N1 influenza virus evolution. In 2005, an HPAI H5N1 (A/Bar-headedGoose/Qinghai/1/05(H5N1)) outbreak killed 6000 wild birds at Qinghai Lake, northwestern China [11]. Later that year, one infected human case caused by HPAI H5N1 (A/Xinjiang/1/2006(H5N1)) was reported in Xinjiang province, northwestern China. Since these two places are close in geography, the HA genes isolated from a wild bird and a human were strikingly similar, with only four amino acid differences. The 3-D structure of the HA with these four different amino acid changes was determined (Fig. 1A) [24]. Based on this structural information, we generated seven QH HA mutant pseudotype viruses and proteins with amino acid changes corresponding to XJ. These included A90V, A160T, I217L, I316V, VAL (A90V plus I217L), ATL (A160T plus I217L) and VTI (A90V plus A160T). The receptor-binding domain (RBD) of HA is comprised of an α-helix (190-helix) and two loops (130-loop and 220-loop), which function as the domain that recognize the receptor [24]. Three of the amino acids that differ between QH and XJ HA, located at aa 90, 160, and 217, were in or adjacent to the RBD. These amino acid changes may be related to the ability of avian influenza virus to break the species barrier. In this study, we focused on these three positions.
Fig. 1.
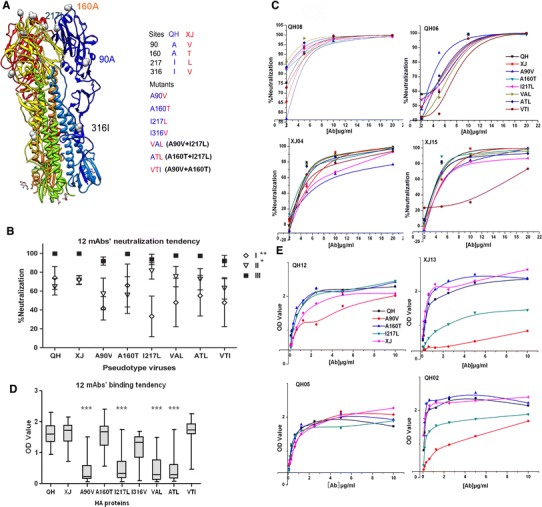
Neutralization and binding assays with QH and XJ H5N1 HAs. (A) The 3-D structure of the HA trimer (Protein Database [PDB] identifier 2IBX) [24] was used as an HA model to visualize the different aa positions in QH and XJ HA. Four different aa positions in QH and XJ HA and seven HA mutants are shown. (B) Neutralization by 12 mAbs in three groups is summarized in a dot-and-whiskers graph. **Group I vs. group III was P<0.01, while *group II vs. group III was P<0.05. (C) Dose-dependent neutralization assay carried out with four mAbs and eight HA pseudotype viruses. The neutralization activity of mAbs was calculated according to the following formula: (A-B)/A×100%. A represents the positive wells, which contained only pseudotype viruses. B represents the test wells, which contained a mixture of mAb and pseudotype viruses. (D) Twelve mAbs were used to measure the binding affinity to the HAs. ***A90V, I217L, VAL and ATL had significantly low binding to these mAbs (P<0.001). (E) Dose-dependent binding assay using four mAbs and five HA pseudotype viruses shown here as example. The ELISA assay was repeated more than three times. The neutralization assay was performed in triplicate. Results are the means of three similar experiments run in triplicate
To investigate the role of these mutants on interspecies transmission, we generated a series of monoclonal antibodies to QH and XJ HA proteins. We selected 12 mAbs according to their binding regions, which were identified by three approaches (Fig. S1). These mAbs were categorized into three groups according to the results of a competition assay using synthetic peptides (Table 1). Group I recognized the lateral part of HA. Group II recognized the tip of HA. Group III recognized a relatively large region of HA. Information about the selected mAbs is summarized in Table 2.
Table 1.
Synthetic peptides used in this study
| No. | Position | Peptide | Source |
|---|---|---|---|
| P1 | 87–91 | INPAN | QH |
| P2 | 87–91 | ANPAN | HK,AH |
| P3 | 87–91 | INPVN | XJ |
| P4 | 124–129 | SSWSDH | QH,XJ,AH |
| P5 | 124–129 | SSWSSH | HK |
| Pa | 145–163 | SSFFRNVVWLIKKNNAYPT | HK |
| Pb | 145–163 | SSFFRNVVWLIKKNNAYPT | QH |
| Pc | 145–163 | SSFFRNVVWLIKKNNTYPT | XJ |
| Pd | 145–163 | PSFFRNVVWLIKKNNTYPT | AH |
| P6 | 158–162 | NSTYP | Othera |
| P7 | 158–162 | NNAYP | QH,HK |
| P8 | 158–162 | NNTYP | XJ,AH |
| P9 | 214–219 | VPRIAT | Other |
| P10 | 214–219 | VPKIAT | QH,HK,AH |
| P11 | 214–219 | VPKLAT | XJ |
aThe most common sequence in other HA strains outside of China
Table 2.
Summary of mAbs used in this study
| mAb | Group | Epitopea | Amino acid positionb | |||
|---|---|---|---|---|---|---|
| 87–91 | 124–129 | 158–162 | 214–219 | |||
| QH02 | I | C | + | + | ||
| QH07 | I | C | + | + | ||
| QH12 | I | C | + | + | ||
| XJ04 | I | C | + | + | ||
| QH05 | II | L | + | |||
| XJ05 | II | C | + | + | ||
| XJ07 | II | C | + | + | ||
| XJ09 | II | L | + | |||
| XJ13 | II | C | + | + | ||
| XJ15 | II | L | + | |||
| QH06 | III | C | + | + | + | + |
| QH08 | III | C | + | + | + | |
a“C” and “L” in the epitope column stand for “conformational epitope” and “linearized epiotpe”, respectively
bThe amino acid positions in hemagglutinin where these mAbs bound when several synthetic peptides were in the indicated amino acid positions
The neutralization capability of 12 mAbs in these three groups is summarized in Fig. 1B. Neutralization by mAbs in group III was the strongest. Neutralization of XJ pseudotype virus by mAbs in group I was relatively strong, while neutralization of A90V and I217L pseudotype viruses by mAbs in group I was relatively weak. Next, we examined dose-dependent neutralization using four neutralizing mAbs (NmAbs) (Fig. 1C). Two NmAbs, QH08 and QH06 in group III, showed high neutralizing activities to all of these HA pseudotype viruses. Escape mutants were found against XJ04 and XJ15 in groups I and II: A90V could escape from XJ04, while VTI (A90V plus A160T) could escape from XJ15. We further analyzed the binding of 12 mAbs to HA and HA mutant proteins (Fig. 1D). A90V, I217L, VAL (A90V plus I217L), ATL (A160T plus I217L) HA mutant proteins had low binding to these mAbs. The dose-dependent binding of four mAbs whose binding regions were located near or in the receptor-binding domain are shown as examples (Fig. 1E). A90V and I217L showed weak binding to these mAbs, with the exception of QH05. Since only the QH05 binding site was a linear epitope in the RBD, and its binding avidity was not easily affected (Table 2), mutations at aa 90 and 217 must induce the conformational change of HA that decreases the binding avidity of mAbs whose binding sites are conformational epitopes.
Taken together, mutations at aa 90 and 217 of QH HA induced low neutralization, while mutations at aa 160, a potential glycosylation site, did not show a significant effect. Since aa 90 and 217 are located in the lateral section of HA, a change in conformation at the tip of these two HA mutants must occur, and this may be responsible for their weak binding to the antibodies tested. Furthermore, since the 130 loop has been identified as an important neutralizing epitope of HA [9, 13], mutations at aa 90 and 217 could affect neutralization through long-range modulation or an allosteric effect.
Neutralization inhibition and binding effect of blocking peptides on mAbs
In order to investigate which regions of HA containing aa 90, 160, 217 could affect the binding and neutralization of mAbs, the HAs were divided into four regions, aa 87-91, 124-129, 158-162, and 214-219, covering the functional HA regions. We performed a competition ELISA to test the effect of blocking peptides on binding and neutralization between mAbs and HAs. The fifteen peptides investigated are summarized in Table 1. We first tested the ability of the mAbs to bind to peptides P1-P11. We found that the inhibition of the peptides with aa 87-162 was relatively strong, suggesting that the majority of mAbs against QH and XJ H5N1 HA bind to this region (Fig. 2A). We also found that the peptides from around aa 217 were unable to inhibit antibodies against QH and XJ H5N1, so this site might be of little importance in the evolution of these two H5N1 strains. We also tested the affinity of these four HA regions containing mutated residues for binding to the mAbs. A mutation at aa 90 did not decrease the strong inhibition of P1, P2 and P3, indicating that the region around aa 90 had high binding affinity to mAbs in group I (Fig. 2B). The inhibition by P4 and P5 or by P6, P7 and P8 was significantly different, indicating that the changes at aa 124-129 or 159-162 could impact the binding affinity to mAbs in group II (Fig. 2B). Also, inhibition by P9, P10 and P11 was weak. These results indicated that the region around aa 90 was a potentially important target for responsive antibodies. In order to confirm the effect of the HA region containing aa 160 on binding and neutralization of mAbs, we used four 20-aa peptides to confirm the blocking effect of peptides around aa 144-163 (Fig. 2C). Only one aa change in these 20-aa peptides could affect their ability to block binding to QH or XJ HA. Thus, a mutation at aa 90 that could induce the conformational change of HA still retained high binding affinity to mAbs in group I. In contrast, a mutation at aa 160 that should not induce a conformational change affected its binding affinity to mAbs in group II.
Fig. 2.
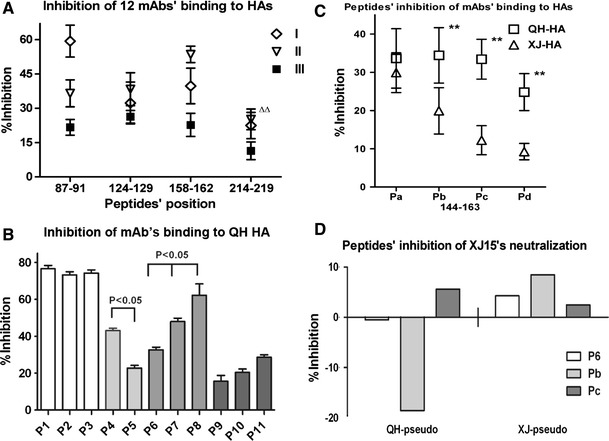
Blocking effect of peptides in neutralization and binding of mAbs and HAs. (A) Inhibition of 11 peptides in four regions against the binding of 12 mAbs in three groups and their corresponding HAs, summarized in a dot-and-whiskers graph. Statistical analysis was done using one-way ANOVA. ΔΔThe inhibition of peptides in aa 214-219 was significantly low (P<0.01). (B) Inhibition of binding of 11 individual peptides with mutated residues in QH HA to several mAbs. P1, P2, and P3 were detected using QH02; while P4 and P5 were detected using QH03; P6, P7, and P8, using QH05; and P9, P10, and P11, using QH12. The inhibition activity of peptides was calculated according to the following formula: (A-B)/A×00%. A represents positive wells without peptides. B represents the test wells containing blocking peptides. (C) Twenty-amino-acid peptides were used to block the binding of mAb to HAs. Numbers at the bottom of the abscissa indicate the aa position in HA. QH05 was used in this assay. An unpaired Students t-test was used for statistical analysis. The inhibition efficiency of Pb, Pc and Pd against the binding of QH05 to QH or XJ HA was significantly different (P<0.01). The inhibition of Pc was the strongest (P<0.01). The competition ELISA assay was repeated more than three times. Data are shown as the mean±s.d. of triplicate experiments. (D) The blocking effect of peptides on neutralization of XJ15 and QH or XJ pseudotype viruses was compared. If the peptide enhances neutralization, the inhibition percentage is a negative value
In order to investigate the effect of glycosylation of residue 160 on neutralization, the neutralizing mAb XJ15, with its binding region adjacent to aa 160, was studied (Fig. 2D). The neutralization of XJ15 against QH and XJ pseudotype viruses could be blocked by P6, Pb, and Pc. Pb and Pc, containing 19 amino acids and the 5 amino acids in P6, were used to confirm the result for P6. The blocking effect of Pb and Pc, with only one amino acid difference at aa 160, from Ala to Thr, was different. These results show that even one amino acid difference at aa 160 could affect neutralization, suggesting that glycosylation at aa 160 could play an important role in the process of viral binding and entry.
Identification of receptor specificity of HA proteins and pseudotype viruses
We further investigated the role of these sites in HA in determining receptor specificity using sialic acid (SA)-binding and infection assays. The SA specificity of the different HAs was analyzed using a simplified glycan microarray method [29, 31]. Two major linkages between SA and the penultimate galactose residues of carbohydrate side chains are found in nature, Neu5Acα2-6Gal (α-2,6) and Neu5Acα2-3Gal (α-2,3). Different HAs have different recognition specificities for these linkages [19, 23]. In this study, Neu5Acα2-6GalNAcα-PAA-biotin and Neu5Acα2-3GalNAcα-PAA-biotin were used to study the receptor specificity of these HA proteins. As expected, QH-HA showed higher binding affinity for Neu5Acα2-3GalNAcα-PAA-biotin than Neu5Acα2-6GalNAcα-PAA-biotin, while XJ-HA had the opposite SA binding affinity pattern, preferentially recognizing the Neu5Acα2-6GalNAcα-PAA-biotin (Fig. 3A). The receptor specificity of H5N1 strains changed in the evolution process from avian to human, and this is attributed to antigenic drift. However, according to previous structural studies [23], the SA substituents and the HA residues around the RBD that are involved in recognition undergo low-affinity interactions. Between QH and XJ HAs, the binding affinity to three mutants did not differ significantly (Fig. 3A).
Fig. 3.
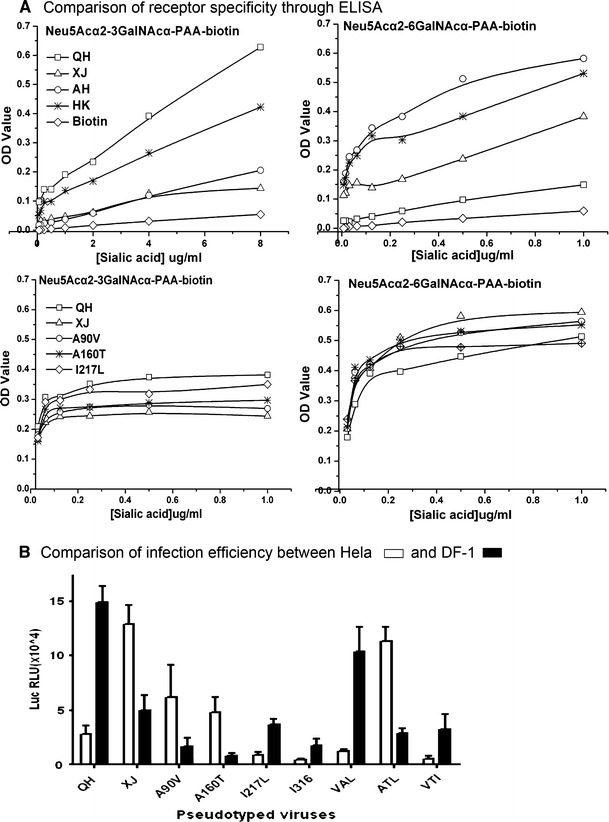
Receptor and species specificity assay for QH and XJ H5N1. (A) Two analogs of sialic acid, Neu5Acα2-6GalNAcα-PAA-biotin and Neu5Acα2-3GalNAcα-PAA-biotin, were used to determine the receptor specificity. Biotin was used as a negative control. The ELISA assay was repeated more than three times. (B) HeLa and DF-1 cells, from a human and a bird, respectively, were used to compare the infection efficiency of HA and HA mutant pseudotype viruses. Luciferase activities (raw light units [RLU]) of HeLa and DF-1 cells infected with nine HA pseudotype viruses are shown. Data are the mean ± s.d. of three similar experiments run in triplicate
Recently, several studies have suggested that different SAs on human and avian cells may not be the only major factor limiting the transmission of avian influenza viruses to humans [4]. The different glycan topology of the RBD between human and avian influenza viruses may also play a critical role in determining the species specificity [2]. In order to determine the role of glycans in receptor specificity, HeLa and DF-1 cells, which are from a human and a bird, respectively, were used to compare the efficiency of infection of these HA pseudotype viruses (Fig. 3B). As expected, QH pseudotype virus had high infection efficiency in DF-1 cells, while XJ pseudotype viruses had high infection efficiency in HeLa cells. Furthermore, mutations at aa 90 or 160 affected the ability of QH pseudotype virus to infect DF-1 cells. Interestingly, VAL (A90V plus I217L) and VTI (A90V plus A160T) could easily infect DF-1 cells, while ATL (A160T and I217L) could easily infect HeLa cells.
Amino acid 90 is on the side of the distal tip of the HA monomer on the membrane. That location makes it difficult to interact directly with SA receptors, while aa 160 is on the distal tip of the HA monomer on the membrane and therefore can easily make contact with SA receptors and antibodies. Both of these mutations could induce a change in SA binding and change the species tropism through different mechanisms (allosteric vs. direct).
Comparison of HA sequences circulating in nature
To confirm our experimental results, 103 human H5N1 HA genes and 70 avian H5N1 HA genes from 2006-2008 were analyzed for the frequency of amino acid changes at these positions (Table 3). For aa 90, the frequency of Thr was highest in human H5N1 strains, while Ala was highest in avian H5N1; for aa 160, Thr was highest in human H5N1, while Ala was highest in avian H5N1. The mutations at aa 90 and 160 from QH to XJ were consistent with viral evolution in the direction of avian to human. However, 217Leu and 316Val were not found in human H5N1, while only two strains of avian H5N1 with 217Ile and 100 strains of avian H5N1 HA genes with 316Ile appeared in more than 2000 H5N1 HA genes. These results suggest that the mutations in aa 90 and 160, but not 217 and 316, are important in QH and XJ H5N1 interspecies transmission. Our results also support this evolution pathway.
Table 3.
The frequency of amino acids at indicated positions in H5N1 HAs isolated from humans and birds
| Frequency of occurrence (%) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Position | 90 | 128 | 159 | 160 | 217 | 316 | ||||||||
| aa | Ala | Val | Thr | Asp | Ser | Asn | Ser | Asp | Ala | Thr | Ile | Leu | Ile | Val |
| Human | 29.1 | 16.5 | 54.4 | 79 | 21 | 24.2 | 75.8 | 0 | 16.5 | 83.5 | 100 | 0 | 100 | 0 |
| Avian | 88 | 12 | 0 | 81 | 19 | 53 | 15 | 32 | 65 | 35 | 99 | 1 | 95 | 5 |
Discussion
Although there have been several research reports on changes in hemagglutinin receptor binding and neutralizing antibodies related to influenza virus evolution [6], our study further establishes the relationship between escape mutation and receptor adaptation. Two important factors determine the direction of viral variation: selective pressure by antibodies and receptor adaptation. A potential role of human nAbs in driving SARS-CoV evolution had been reported [25], and receptor adaptation as a driving force has also been suggested [31]. In the present study, two new observations related to the crucial factors involved in viral variation are presented. First, two mutations that are important for avian-to-human interspecies transmission were identified. Second, an evolution pathway from QH H5N1 to XJ H5N1 was outlined.
Two important mutations for avian influenza H5N1 HA identified in this study involved aa 90 and aa 160. A mutation at aa position 90 in the H5N1 hemagglutinin (HA), outside the receptor binding domain (RBD), could simultaneously induce a conformational change in the RBD that allowed escape from neutralization as well as a change in receptor preference through long-range regulation. A mutation at aa position 160 in the RBD only induced a change in receptor preference. Other research has also demonstrated that aa position 160 is essential for the receptor specificity [3]. From the results of this study, we could conclude that mutations distant from the RBD can induce a conformational change in the RBD to allow escape from nAbs and change the receptor preference simultaneously. These mutations are deemed “key events”, particularly during interspecies transmission, and they ensure that the original invasion is successful, i.e., the mutation at aa 90 on QH H5N1 HA. They are the result of positive selection caused by antibodies. Some mutations in the RBD could only induce a change in receptor preference, and these are deemed “maintaining adaptations” to ensure that the variants circulate in the new species, i.e., the mutation at aa 160 on QH H5N1 HA. They are the result of adaptation caused by the receptor. After global change of the tip of HA by the aa 90 mutation, and then the local readjustment of RBD by the aa 160 mutation, avian influenza virus would be more suitable for a mammal-like binding pocket, and this would make infection of humans successful. The continuing appearance of these two types of mutations make the variants persist in the new host species.
The interspecies transmission of QH H5N1 might start from the mutation at aa 90. The region adjacent to aa 90 of HA showed high binding affinity for mAbs. The location of antigen E of H3N2 HA was similar to the region containing aa 90 of avian influenza virus. A high-binding-affinity mAb to antigen E of H3N2 has been reported [21, 28]. To decrease lethality for the host, cytopathic viruses have to evolve to exhibit neutralizing determinants that are bound with high avidity by the available B-cell repertoire of higher vertebrates [5]. The region of position 90 possesses a high affinity for antibodies. It has been shown that antibodies with high binding affinity push viral variation to escape host immune clearance, and these mutants stimulate the host to produce nAbs with strong neutralization activity to keep the balance between virus and host. Furthermore, amino acid mutations at epitopes C and E of the HA of influenza A/H3N2 viruses may lead, on average, to an increase in the neutralization of the mutated viruses [17]. Position 90 of QH H5N1 is in epitope E of HA. High-binding-affinity antibodies to the region containing aa 90 push QH H5N1 variation to produce XJ H5N1, which can induce strong neutralizing antibodies.
Our results suggest an evolutionary pathway for HA from QH H5N1 to XJ H5N1. In this study, the mutation at aa 90 induced a conformational change in HA to influence the neutralization and binding capabilities of mAbs and its species tropism. The mutation at aa 160, which did not cause a conformational change in HA, changed the species tropism through the function of glycosylation, since this position is a glycosylation site. It was a strain similar to QH H5N1 that induced human infection in Xinjiang province. This epidemic might have been due to I217L or VAL (A90V plus I217L) mutants, because these types of mutations lose most binding to mAbs and induce a conformational change in HA without the species tropism change. A mutation at aa 217 can potentially occur in poultry or wild birds as well. After successful invasion, mutations at other positions are the result of virus-host interactions. Mutations at aa 90 and 160 were similar to the natural mutation induced by antigenic drift. H1N1 might use a similar evolutionary pathway and escape strategy to that of H5N1, since it belongs to the same group of influenza viruses, and its HA has similar structural characteristics [26].
In summary, we have investigated the neutralization, binding activity and specificity of contemporaneous strain-specific or multi-strain nAbs, stable circulating strains or their mutants, and their HA receptors. The results reveal two critical mutation points for the cross-species evolution of influenza viruses. The results also suggest a potential viral evolution pathway. This information can be utilized to design preventive measures for the next pandemic.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Fig. S1. Identification of epitopes of mAbs. (A) Native HA and denatured HA proteins were used to distinguish the conformational and linear epitopes of the mAbs used. (B) Peptide binding assays were performed to identify regions where mAbs bind. The amino acid positions of synthetic peptides are indicated. (C) Blocking effect of peptides against the binding of mAbs and their corresponding HAs. Groups labeled “no-P” served as positive controls, which included only the reaction between antibodies and HAs. Data are shown as the mean ± s.d. of triplicate experiments.
Acknowledgments
We thank Dr. Wenhui Li for his kind help in the pseudotype neutralization. This work is funded by National Institutes of Health (NIH) [grant numbers U19 AI051915-05S1].
Abbreviations
- HPAI
Highly pathogenic avian influenza
- HA
Hemagglutinin
- RBD
Receptor binding domain
- SA
Sialic acid
References
- 1.Burton DR. Antibodies, viruses and vaccines. Nature. 2002;2:706–713. doi: 10.1038/nri891. [DOI] [PubMed] [Google Scholar]
- 2.Chandrasekaran A, Srinivasan A, Raman R, Viswanathan K, Raguram S, Tumpey TM, Sasisekharan V, Sasisekharan R. Glycan topology determines human adaptation of avian H5N1 virus hemagglutinin. Nat Biotechnol. 2008;26:107–113. doi: 10.1038/nbt1375. [DOI] [PubMed] [Google Scholar]
- 3.Gao Y, Zhang Y, Shinya K, Deng G, Jiang Y, Li Z, Guan Y, Tian G, Li Y, Shi J, Liu L, Zeng X, Bu Z, Xia X, Kawaoka Y, Chen H. Identification of amino acids in HA and PB2 critical for the transmission of H5N1 avian influenza viruses in a mammalian host. PLoS Pathog. 2009;5:e1000709. doi: 10.1371/journal.ppat.1000709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guo CT, Takahashi N, Yagi H, Kato K, Takahashi T, Yi SQ, Chen Y, Ito T, Otsuki K, Kida H, Kawaoka Y, Hidari KI, Miyamoto D, Suzuki T, Suzuki Y. The quail and chicken intestine have sialyl-galactose sugar chains responsible for the binding of influenza A viruses to human type receptors. Glycobiology. 2007;17:713–724. doi: 10.1093/glycob/cwm038. [DOI] [PubMed] [Google Scholar]
- 5.Hangartner L, Zinkernagel RM, Hengartner H. Antiviral antibody responses: the two extremes of a wild spectrum. Nat Rev Immunol. 2006;6:231–241. doi: 10.1038/nri1783. [DOI] [PubMed] [Google Scholar]
- 6.Hensley SE, Das SR, Bailey AL, Schmidt LM, Hickman HD, Jayaraman A, Viswanathan K, Raman R, Sasisekharan R, Bennink JR, Yewdell JW. Hemagglutinin receptor binding avidity drives influenza A virus antigenic drift. Science. 2009;326:734–736. doi: 10.1126/science.1178258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.He Y, Li J, Jiang S. A single amino acid substitution (R441A) in the receptor-binding domain of SARS coronavirus spike protein disrupts the antigenic structure and binding activity. Biochem Biophys Res Commun. 2006;344:106–113. doi: 10.1016/j.bbrc.2006.03.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Karlsson Hedestam GB, Fouchier RA, Phogat S, Burton DR, Sodroski J, Wyatt RT. The challenges of eliciting neutralizing antibodies to HIV-1 and to influenza virus. Nat Rev Microbiol. 2008;6:143–155. doi: 10.1038/nrmicro1819. [DOI] [PubMed] [Google Scholar]
- 9.Khurana S, Suguitan AL, Jr, Rivera Y, Simmons CP, Lanzavecchia A, Sallusto F, Manischewitz J, King LR, Subbarao K, Golding H. Antigenic fingerprinting of H5N1 avian influenza using convalescent sera and monoclonal antibodies reveals potential vaccine and diagnostic targets. PLoS Med. 2009;6:e100049. doi: 10.1371/journal.pmed.1000049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kuiken T, Holmes EC, McCauley J, Rimmelzwaan GF, Williams CS, Grenfell BT. Host species barriers to influenza virus infections. Science. 2006;21:394–397. doi: 10.1126/science.1122818. [DOI] [PubMed] [Google Scholar]
- 11.Liu J, Xiao H, Lei F, Zhu Q, Qin K, Zhang XW, Zhang XL, Zhao D, Wang G, Feng Y, Ma J, Liu W, Wang J, Gao GF. Highly pathogenic H5N1 influenza virus infection in migratory birds. Science. 2005;309:1206. doi: 10.1126/science.1115273. [DOI] [PubMed] [Google Scholar]
- 12.Li Z, Ma C, Liu Z, He W. Serologic cross-reactivity among humans and birds infected with highly pathogenic avian influenza A subtype H5N1 viruses in China. Immunol Lett. 2011;135:59–63. doi: 10.1016/j.imlet.2010.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Luo W, Chen Y, Wang M, Chen Y, Zheng Z, Song H, Chen H, Guan Y, Ng MH, Zhang J, Xia N. Peptide mimics of a conserved H5N1 avian influenza virus neutralization site. Biochem J. 2009;419:133–139. doi: 10.1042/BJ20080083. [DOI] [PubMed] [Google Scholar]
- 14.Marasco WA, Sui J. The growth and potential of human antiviral monoclonal antibody therapeutics. Nature Biotechnol. 2007;25:1421–1434. doi: 10.1038/nbt1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martinez O, Tsibane T, Basler CF. Neutralizing anti-influenza virus monoclonal antibodies: therapeutics and tool for discovery. Int Rev Immunol. 2009;28:69–92. doi: 10.1080/08830180802593540. [DOI] [PubMed] [Google Scholar]
- 16.Nakajima S, Nakajima K, Nobusawa E, Zhao J, Tanaka S, Fukuzawa K. Comparison of epitope structures of H3HAs through protein modeling of influenza A virus hemagglutinin: mechanism for selection of antigenic variants in the presence of a monoclonal antibody. Microbiol Immunol. 2007;51:1179–1187. doi: 10.1111/j.1348-0421.2007.tb04013.x. [DOI] [PubMed] [Google Scholar]
- 17.Ndifon W, Wingreen NS, Levin SA. Differential neutralization efficiency of hemagglutinin epitopes, antibody interference, and the design of influenza vaccines. PNAS. 2009;106:8701–8706. doi: 10.1073/pnas.0903427106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nelson MI, Holmes EC. The evolution of epidemic influenza. Nature. 2007;8:196–205. doi: 10.1038/nrg2053. [DOI] [PubMed] [Google Scholar]
- 19.Nicholls JM, Chan MC, Chan WY, Wong HK, Cheung CY, Kwong DL, Wong MP, Chui WH, Poon LL, Tsao SW, Guan Y, Peiris JS. Tropism of avian influenza A (H5N1) in the upper and lower respiratory tract. Nat Med. 2007;13:147–149. doi: 10.1038/nm1529. [DOI] [PubMed] [Google Scholar]
- 20.Pinschewer DD, Perez M, Jeetendra E, Bächi T, Horvath E, Hengartner H, Whitt MA, de la Torre JC, Zinkernagel RM. Kinetics of protective antibodies are determined by the viral surface antigen. J Clin Invest. 2004;114:988–993. doi: 10.1172/JCI22374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shih AC, Hsiao TC, Ho MS, Li WH. Simultaneous amino acid substitutions at antigenic sites drive influenza A hemagglutinin evolution. PNAS. 2007;104:6283–6288. doi: 10.1073/pnas.0701396104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shinya K, Ebina M, Yamada S, Ono M, Kasai N, Kawaoka Y. Avian flu: influenza virus receptors in the human airway. Nature. 2006;440:435–436. doi: 10.1038/440435a. [DOI] [PubMed] [Google Scholar]
- 23.Skehel JJ, Wiley DC. Receptor binding and membrane fusion in virus entry: the Influenza hemagglutinin. Annu Rev Biochem. 2000;69:531–569. doi: 10.1146/annurev.biochem.69.1.531. [DOI] [PubMed] [Google Scholar]
- 24.Stevens J, Blixt O, Tumpey TM, Taubenberger JK, Paulson JC, Wilson IA. Structure and receptor specificity of the hemagglutinin from an H5N1 influenza virus. Science. 2006;312:404–410. doi: 10.1126/science.1124513. [DOI] [PubMed] [Google Scholar]
- 25.Sui J, Aird DR, Tamin A, Murakami A, Yan M, Yammanuru A, Jing H, Kan B, Liu X, Zhu Q, Yuan QA, Adams GP, Bellini WJ, Xu J, Anderson LJ, Marasco WA. Broadening of neutralization activity to directly block a dominant antibody-driven SARS-coronavirus evolution pathway. PLoS Pathog. 2008;4:e1000197. doi: 10.1371/journal.ppat.1000197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sui J, Hwang WC, Perez S, Wei G, Aird D, Chen LM, Santelli E, Stec B, Cadwell G, Ali M, Wan H, Murakami A, Yammanuru A, Han T, Cox NJ, Bankston LA, Donis RO, Liddington RC, Marasco WA. Structural and functional bases for broad-spectrum neutralization of avian and human influenza A viruses. Nat Struct Mol Biol. 2009;16:265–273. doi: 10.1038/nsmb.1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Suzuki Y. Natural selection on the influenza virus genome. Mol Biol Evol. 2006;23:1902–1911. doi: 10.1093/molbev/msl050. [DOI] [PubMed] [Google Scholar]
- 28.Takematsu K, Fukuzawa K, Omagari K, Nakajima S, Nakajima K, Mochizuki Y, Nakano T, Watanabe H, Tanaka S. Possibility of mutation prediction of influenza hemagglutinin by combination of hemadsorption experiment and quantum chemical calculation for antibody binding. J Phys Chem B. 2009;113:4991–4994. doi: 10.1021/jp810997c. [DOI] [PubMed] [Google Scholar]
- 29.Totani K, Kubota T, Kuroda T, Murata T, Hidari KI, Suzuki T, Suzuki Y, Kobayashi K, Ashida H, Yamamoto K, Usui T. Chemoenzymatic synthesis and application of glycopolymers containing multivalent sialyloligosaccharides with a poly (L-glutamic acid) backbone for inhibition of infection by influenza viruses. Glycobiology. 2003;13:315–326. doi: 10.1093/glycob/cwg032. [DOI] [PubMed] [Google Scholar]
- 30.Yang ZY, Wei CJ, Kong WP, Wu L, Xu L, Smith DF, Nabel GJ. Immunization by avian H5 influenza hemagglutinin mutants with altered receptor binding specificity. Science. 2007;317:825–828. doi: 10.1126/science.1135165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yamada S, Suzuki Y, Suzuki T, Le MQ, Nidom CA, Sakai-Tagawa Y, Muramoto Y, Ito M, Kiso M, Horimoto T, Shinya K, Sawada T, Kiso M, Usui T, Murata T, Lin Y, Hay A, Haire LF, Stevens DJ, Russell RJ, Gamblin SJ, Skehel JJ, Kawaoka Y. Haemagglutinin mutations responsible for the binding of H5N1 influenza A viruses to human-type receptors. Nature. 2006;444:378–382. doi: 10.1038/nature05264. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


