Abstract
The history of Pediatric Infectious Diseases closely parallels the history of Pediatrics at least until the last century, because historically infections comprised the major causes of childhood morbidity and mortality, as they still do in the developing world. This history reviews developments in the field through the centuries and is writen so that it does not overlap the contribution to this series by Baker and Katz entitled ‘Childhood Vaccine Development in the United States.' Remarkable descriptions of selected pediatric infections existed long before the invention of printing, and early pediatric texts included many chapters devoted to various infections. Coincident with the establishment of pediatric organizations in America in the late 19th and early 20th Centuries, major attention was focused on diphtheria, infant diarrheal illnesses, tuberculosis, streptococcal infections and their complications, and other pediatric infections, and substantial progress was made. The American Pediatric Society (1888), the American Academy of Pediatrics (1930), the Society for Pediatric Research (1931), and the American Board of Pediatrics (1933) all contributed to the evolution of the discipline of Pediatric Infectious Disease, and numerous leaders of these organizations had significant infectious diseases interests. The establishment of the Pediatric Infectious Diseases Society, the Pediatric Infectious Diseases sub-board, and an accreditation process for training programs, as well as sub-specialty textbooks and journal, further validated the development of this specialty, particularly in North America. The many remaining challenges related to infectious diseases in children (including HIV, emerging infections, antimicrobial resistance, opportunistic infections, and infections in the developing world) insure the future of the specialty. The genomic era of medicine and the tools of molecular biology will lead to new insights into pathogenesis, diagnosis, and treatment of infections. Pediatric Infectious Diseases physicians can celebrate the past triumphs of the discipline and future achievements, all contributing to improved health for children.
Main
The earliest medical writers described illnesses that included infectious diseases that impacted children. These included Hippocrates' description of a mumps epidemic in the first book of the Epidemics; the descriptions by Celsus (1st Century, C.E.) of roundworms in children, pustules in young children, and apparently diphtheria; Oribasius' 4th Century writings on infant rashes, cough, coryza, draining ears, and siriasis (inflammation of the brain); Aetius' 6th Century discussion of fevers, eye inflammation, sneezing and catarrh, postdiphtheritic paralysis, and consumption of the spine; the works of Rhazes (∼860– ∼930), who distinguished smallpox from measles and noted the complications of these illnesses; and the 11th Century works of the prominent Arab physician Avicenna (Ibn Sina), who wrote on children's illnesses including tetanus, cough and catarrh, aphthae, ear drainage, seiriasis, fevers, pustules, throat inflammation, worms and diarrhea (flux) (1, 2). For the next almost 500 y, there were virtually no pediatric writings.
The invention of printing in the mid-15th Century revived learning, and the first printed work on diseases of children was published in 1472 by the Italian Paolo Bagellardo, including chapters on many common infections, including tinea capitis, otorrhea, ear abscess, cough, rheumatism and diarrhea (3). Two other similar books followed, that of Metlinger (German) in 1473 and of Roelans (Belgian) in 1483. Eucharius Roesslin (German) opened the 16th Century of pediatric texts with a text on midwifery and pediatrics, with reviews of the 35 most common ailments of children, including many infections, of course (2). The book by Leonellus Faventinus de Victoriis (Italian) was published posthumously in 1544 and included a chapter on aphthae and another on measles and smallpox. The first English-language pediatric book was published in 1544 by Thomas Phaer, “The Boke of Chyldren” and included chapters on Aposteme of the brayne (meningitis), Scalles of the heed, Styfnesse of the lymmes, Bloodshoten eyes [Kawasaki disease?], Diseases in the eares, Canker in the mouth, Quynsye or swelling of throte, Coughe, Feblenesse of the stomacke and vomiting, Fluxe of the belly (diarrhea), Wormes, Small pockes and measels, Fevers, and Consumpcion (1, 2). In 1553 Giovanne P. Ingrassias (Italian) differentiated scarlet fever (rossalia) from measles (1). Hieronymus Mercurialis (Italian) in 1583 published a pediatric text that mentioned the King's Evil (scrofulous glands) and included 10 chapters on worms (1). At the end of the 16th Century, understanding of disease in children had barely advanced beyond the theories and observations of the Greeks and Romans, restated by the Arab physicians, and clinical observation seemed of little value.
Significant advances, however, were made during the 17th Century. The works of Guillaume de Baillou (French) published in 1640 were important for the first detailed description of whooping cough as a distinct entity, as he described an epidemic in 1578, as well as rubeola and scarlet fever. Several important descriptions of diphtheria (morbo strangulatorio, angina puerorum) were made, with its epidemic nature highlighted by Johannes Sgambatus (Italian) in 1620, its pathologic anatomy in 1646 by Thomas Bartholin (Danish), who also commented on its contagious nature (1), and its method of killing children (paedanchone or child-throttling) by Marcus A. Severinus (Italian) in 1652.
The second English language pediatric book, published by Robert Pemell in 1653, included chapters on lice, scab and Itch, ulcers and sores in the head, pain and inflammation of the ears, oral ulcers, Feavers, small Pox and Measels, Rheums and cough, flux, Worms, inflammation of the Naval, and Saint Anthonie's fire (erysipelas or ergotism) (1, 2). The third English book appeared in 1664, written by J. Starsmare and included much the same topics but making the first mention in English of scrofula. Franciscus Sylvius de le Boe (Dutch) was a careful clinician and anatomist who published a book on diseases of infants in 1674 that included the usual topics. Sylvius is remembered best for the aqueduct of Sylvius and the sylvian fissure. Thomas Sydenham, the most respected English physician of the 17th Century, deserves mention here for his careful description of chorea (1686), his very detailed description of measles (1670), and his account of scarlet fever (1675), which surprisingly failed to mention pharyngitis. Thomas Willis, who described the circle of Willis, wrote a careful account of pertussis (chincough) in 1675 and said, “The plan of treatment which is usual in other varieties of cough is seldom of any use in this, which is the reason why old women and gypsies are consulted more often than doctors”(1).
Near the end of the 17th Century a small book on diseases of infants was published in London in 1689 by Walter Harris and became very popular, with 18 editions over 53 years. Harris also wrote an essay on venereal diseases, a treatise on plague, and in 1721 strongly advocated inoculation against smallpox (4). His comments about summer diarrhea of infants are described below.
In summary, the 17th Century was associated with a rebirth of medicine, and for the first time since Hippocrates clinical observations became important. Anatomists laid a foundation for morbid anatomy/pathology, and there was initial rejection of some of the ancient theories of disease (1). In the field of pediatric infectious diseases there was slow progress, but chorea, scarlet fever, scrofula, and pertussis had been recognized clearly as specific diseases.
PEDIATRIC INFECTIOUS DISEASES IN EARLY COLONIAL AMERICA
The history of pediatric infectious diseases (but not the medical specialty) in America predates the establishment of the United States. Colonial children were afflicted by many epidemic contagious diseases, and a number of very graphic descriptions have been recorded, many referred to in Thomas E. Cone's History of American Pediatrics (5).
Smallpox that affected children was described in 1629 on the Talbot, a ship en route from Gravesend, England, to New England. During the voyage, the Reverend Higginson wrote an account of his children who became ill with smallpox, including his young daughter who died at sea. Epidemics of smallpox, endemic in England through the 17th Century, were described in Massachusetts in 1633 and again in 1677, when about one-fifth of Boston's population succumbed to this scourge (5). The first American medical publication, a broadside on smallpox that discussed diagnosis and therapy, was written in 1677 by the pastor-physician Reverend Thomas Thacher (1620–1678) of Boston, who practiced part-time pediatrics (6).
Measles was recorded in Boston and Connecticut in 1657–1658 and again in 1687–1688, with many children afflicted but apparently relatively few deaths. Diphtheria, which was often confused clinically with scarlet fever, was associated with great mortality. The first recorded North American epidemic of diphtheria occurred in 1659 in Roxbury, MA, with subsequent probable outbreaks documented in 1686 in Virginia and 1689 in New London, CT. Scarlet fever, often mistaken for both measles and diphtheria, was first reported in the colonies by both John Marshall and Cotton Mather, who wrote of an epidemic in Boston from September to December, 1702. The next epidemic in New England did not occur until 1735. Whooping cough caused an extensive epidemic in 1659 in young children, but there are no records of subsequent epidemics until 1738 (5).
Summer diarrhea in infants was a very serious problem, with very high mortality rates. In England, Walter Harris (1647–1732), one of the earliest great “pediatrists” wrote in 1689 “From the Middle of July to about the Middle of September, the Epidemical Gripes of Children are so rife every Year, that more of them usually die in one Month, than in three or four at any other Time…”(4) In the colonies, John Josselyn in 1674 and John Marshall around 1700 wrote about children dying of bloody flux (dysentery) and fever (5).
EIGHTEENTH CENTURY (EUROPE)
The pace of progress regarding infectious diseases of children accelerated during the 18th Century, particularly with respect to prevention of smallpox by inoculation or variolation. Smallpox was an almost inevitable illness of childhood and was one of the most common causes of death because of its high mortality rate. It was reported, for example, to kill 10% of Swedish children yearly. Inoculation with matter from a smallpox subject was introduced into Western Europe from Constantinople around 1720, with limited mortality from the procedure and resulting immunity (1). Other advances were being made as well. Richard Wiseman (English), surgeon to King Charles II, wrote extensively about the King's Evil (scrofula) and mesenteric adenitis. Jean Astruc (French) in 1746 published an English edition of his lectures on diseases of children that included pertussis, infant diarrhea, worms, purulent lung disease, and scrofula. Astruc was among the first to emphasize the importance of a thorough and methodical clinical exam of children. John Fothergill (English) in 1748 published an important work on ulcerative pharyngitis, with descriptions of diphtheria and scarlet fever (1).
The mid-18th Century saw the identification of varicella as a disease distinct from smallpox. François Boissier de Sauvages (French) in a 1760 book on diseases of children described what he thought was a variety of smallpox that he termed “la Vérole volante” or the fleeting variola (smallpox). The description is of varicella, which was very clearly distinguished as a separate illness by William Heberden the elder (English) in 1767 (1–3).
Nils Rosen von Rosenstein (Swedish) published a very important pediatric work in 1765, which was the most progressive and scientific book on pediatrics up to that time (1). It included a detailed description of a 1744 epidemic of scarlet fever, 14 varieties of infant diarrhea (obviously he was a splitter rather than a lumper), and also described varicella but considered it “the chrystalline or watery smallpox”(1). He described postscarletina dropsy with bloody urine (poststreptococcal nephritis) and had sufficient insight about pertussis to state that “The true cause of this disease must be some heterogeneous matter or seed which has a multiplicative power as is the case with smallpox… we find that it is communicated by infection and that a part of it is attracted by the breath down into the lungs.” Robert Whytt (Scottish) in 1768 published what some consider the finest clinical description of any disease to that time in his “Observations on the Dropsy in the Brain,” tuberculous meningitis, in which he detailed the three clinical stages of this disease as well as the autopsy findings (1).
Around this time Hugh Smith (English) importantly focused public attention upon the staggeringly high mortality rates among children. He showed that from 1762 to 1771 about two-thirds of children born in London died before the age of five years and that about 75% of the deaths occurred before two years of age (1, 2). At this time George Armstrong founded the first dispensary for children in 1769, which ultimately led to the establishment of children's hospitals. He published a work on the diseases most fatal to infants in 1767, and he wrote in detail about the treatment of the Chin-cough (pertussis).
Michael Underwood (English) was probably the most advanced 18th Century writer on the diseases of children (1). His treatise, first published in 1784, was reprinted in 17 editions until 1848. He provided the first description of sclerema and poliomyelitis and wrote about coryza maligna, which was either congenital lues or nasal diphtheria. Joseph Clarke (Irish) in 1789 described an outbreak of fatal “nine-day fits” among neonates (neonatal tetanus) at the Lying-in Hospital of Dublin. Hyacinthus Andreas (Spanish) had published an account of this condition at the end of the 17th Century (1).
It was in 1798 that Edward Jenner published his report of 23 years of observation and experimentation with the Variolae Vaccinae, or cowpox, to prevent smallpox. This proved much safer than the procedure of inoculation with smallpox matter (variolation) used earlier in the 18th Century, as described above.
At the end of the 18th Century, pediatrics was characterized by increased awareness of the value of children's lives, the beginning of institutions to provide medical care for children and the beginning of instruction of medical students in children's diseases. Additional important pediatric infectious diseases had been described, including tuberculous meningitis, varicella, neonatal tetanus, and poststreptococcal nephritis (1). Jenner's studies provided the means to prevent the great morbidity and mortality related to the dreaded smallpox.
EIGHTEENTH CENTURY (COLONIAL AMERICA)
Epidemic diseases were better described during the 18th Century in colonial America compared with the earlier period, and there was clear recognition of the impact of smallpox, diphtheria, scarlet fever, measles, influenza, tuberculosis and whooping cough, particularly upon children. A very severe New England epidemic of diphtheria in 1735–1740 killed more than 5000 individuals, mostly children, and was later called “the most horrible epidemic of a children's disease in American history”(7). Early accounts by Jabez Fitch (1736) of New Hampshire and Jonathan Dickinson (1740) described these events (2). Samuel Bard (1742–1821), Professor of Medicine at King's College, NY, in 1771 published an important book entitled Enquiry into the Nature, Cause and Cure of the Angina Suffocativa, or Sore Throat Distemper (8). This work about diphtheria emphasized its infective etiology, “drawn in by the breath of a healthy child,” and urged prevention by immediate removal of the young children in the family as soon as a first case appeared in a household. In 1736 William Douglass (1691–1752) of Boston provided what is considered the earliest complete description of scarlet fever, terming it angina ulcusculosa (5). In 1789, Dr. Benjamin Rush (1745–1813) described a widespread epidemic of scarlet fever (“scarlatina anginosa”) occurring in Philadelphia in 1783 and 1784, while pertussis was described in detail in 1776 by Lionel Chalmers (1715–1777) in An Account of the Weather and Diseases of South Carolina (9).
Dysentery (“bloody flux”) was emphasized as a serious and very common problem of children particularly in summer when Benjamin Rush wrote in detail about “cholera infantum” (and coined the term) in 1777 (10). Rush was the most influential American physician of his day and a signer of the Declaration of Independence, and he lectured and published regarding pediatric disorders, including cholera infantum and diphtheria (11). Cholera infantum, or summer diarrhea, appeared each year in epidemic form and emerged later as a particularly important problem for young children, as more crowded urban areas developed. In 1794 Rush also described a major epidemic of yellow fever in Philadelphia which killed about one-eighth of the population (5).
Particularly severe epidemics of measles were noted in 1688, 1713, 1740, 1758, and 1772. More than 900 children in Charleston, SC died in the 1772 epidemic alone (9). Cotton Mather's diary in 1713 recorded the death of his wife, the maid, his neonatal twins, and another child in his family within a 12-d period (5). This serves as a striking reminder about this now-preventable illness. Other primarily pediatric illnesses including thrush, mumps, tinea capitis, and worm infestations also were clearly described in the colonies of the 18th Century (5). In contrast to Europe, where smallpox was an endemic illness of childhood, in the colonies smallpox occurred in large epidemics with about 20-year periodicity and affected children as well as older susceptible individuals. This became an important issue during the Revolutionary War, when the troops of the Continental Army (but not the British forces) were ravaged by smallpox until General George Washington at Valley Forge decided to inoculate all susceptible troops. This act probably saved the war effort (12).
THE EARLY NINETEENTH CENTURY IN AMERICA
From 1800 to about 1870, the major causes of death in children were tuberculosis, diarrhea of infancy, bacillary dysentery, typhoid fever, and the highly contagious diseases of childhood, especially scarlet fever, diphtheria, and lobar pneumonia (5). Significant fluctuations occurred. For example, for the first three decades of the 19th Century, the severity of scarlet fever was less than observed previously but then around 1830 increased dramatically. By 1840 scarlet fever had become the leading cause of death among the infectious diseases of childhood in the U.S., Great Britain, and Europe (13). Changes in the virulence of prevalent Group A streptococcal strains would seem most likely responsible for such fluctuations, as seen in New York City, for example, where only 43 scarlet fever deaths were recorded from 1805–1822, but 4874 deaths by 1847 (14).
Reports about other pediatric infections also exist. In 1813 Nathan Smith of Lebanon, NH, founder of Dartmouth Medical School, successfully treated Joseph Smith (1805–1844), an unrelated 7-year-old boy, for osteomyelitis, removing bone from the left lower leg but avoiding amputation. Long-term drainage apparently occurred with discharge of 14 additional pieces of bone, and crutches were used by the child for more than three years. Joseph Smith, who retained a slight limp, later founded the Mormon church (11).
For a period of about 40 years, from 1813–1852, Eli Ives, the first U.S. medical school faculty appointee in pediatrics, lectured Yale medical students on the diseases of children. The surviving lecture notes show that these lectures included a number of infectious diseases topics as they impacted children (11). Also in the first half of the 19th Century, William Potts Dewees (1825), George Logan (1825), and John Eberle (1833) each published very early pediatric texts, each of which included sections on the infectious illnesses of children. Dewees of Philadelphia was an Adjunct Professor of Midwifery, and his text, the first truly comprehensive American pediatrics book, has more than 60 pages devoted to infections, including not only epidemic illnesses but also abscesses of the hip joint and ear, worms, and whitlow (paronychia) (15).
Epidemic spotted fever, or cerebrospinal meningitis, was described in detail by Elisha North (1771–1843), who reported the 1807 Connecticut outbreak of meningococcal infection (5). In 1834 William Wood Gerhard (1809–1872) provided the first American description of tuberculous meningitis (actually describing 30 children he saw in Paris), and in 1836 and 1837 he distinguished typhus from typhoid in children at the Pennsylvania Hospital. Gerhard also in 1834 was perhaps the first to record percussion and auscultation findings in pediatric pulmonary diseases (16). His Parisian training clearly exposed him to Laennec's critically important invention, the stethoscope (5).
NINETEENTH CENTURY IN EUROPE
Very substantial advances were made in European pediatrics, particularly with respect to infectious diseases, throughout the 19th Century. John Cheyne (Scottish, Irish) published a number of important works, including “The Pathology of the Membranes of the Larynx and Bronchia” in 1809, a description of the 1817–1819 Dublin fever epidemic, and three studies of cynanche trachealis (croup), and described Cheyne-Stokes respirations (3).
Pierre Bretonneau (French) described the contagious nature of typhoid fever (1819–1829) and of diphtheria (1826). He performed the first successful tracheostomy for diphtheria on July 1, 1825, on a child, Elizabeth de Puységur (3). In 1821 he distinguished typhoid from typhus clinically. The most important pediatric text of the early 19th Century was by Charles-Michel Billard (French). This 1828 work built upon that of Bichat and Laennec, who provided the initial scientific basis of medicine, and classified pediatric disorders (including infectious diseases) based not upon symptoms but upon pathologic lesions, i.e. upon autopsy findings (3). Armand Trousseau (French) performed the first tracheostomy in Paris (1831), described laryngeal tuberculosis, cutaneous and mucosal diphtheria, pediatric cholera, and he originated the technique of thoracentesis in pleurisy. Frédéric Rilliet (Swiss) wrote on typhoid in children (1840), epidemic measles (1847), mumps (1850), and cholera (1856). His text (1838–1843) with Antoine-Charles-Ernest Barthez (French) included classic descriptions of tuberculosis of the bronchial glands, bronchopneumonia, and chronic pleurisy.
Charles West (British) (1816–1898) was considered the greatest English “pediatrist” of the second half of the 19th Century. In 1852 he established the Children's Hospital in Great Ormand Street, London. His pediatric text of 1848, which went through seven editions and numerous translations, included outstanding descriptions of infantile tuberculosis and poliomyelitis and emphasized the importance of breast feeding in the prevention of infantile diarrhea. Johann Rehn (German) studied epidemic jaundice (infectious hepatitis) in children (1869), while his countryman Eduard Heinrich Henoch, a pupil of Schönlein, described abdominal purpura (Henoch-Schönlein purpura) in 1874.
Nil F. Filatoff (or Filatow) (Russian) published a series of lectures on the infectious diseases of children (1885–87), in which he described “scarlatinal rubella” termed “Fourth disease” or Filatoff-Dukes disease (3). Marie-Jules Parrot (French) described the pseudoparalysis of congenital syphilis (1872) that still bears his name (17). Jacques-Joseph Grancher (French) wrote extensively on tuberculosis (1872–1890) and pioneered isolation and antisepsis (Infection Control) at the Hôpital des enfants malades, Paris (1889–1890), housing infectious patients in wire cages and using surgical gowns for staff (3). Bernard-Jean-Antonin Marfan (French) wrote important works on pediatric typhoid (1894), peritonitis (1894), congenital infections (1897), infantile gastroenteritis (1900) and diphtheria (1905). Friedrich Bezold (German) in 1877 provided the first clear description of mastoiditis (18).
Henry Ashby (British) was a pediatrician and public health officer who led the movement in Britain to advocate for a pure milk supply during the 1890s and early 1900s. Sir Arthur Newsholme (British) in the late 19th Century and early 20th Century provided extremely important data related to changes in infant, child, and maternal mortality primarily due to infectious diseases, particularly rheumatic fever (1895), epidemic diphtheria (1898), and tuberculosis (1906) (3).
LATE NINETEENTH CENTURY
Beginnings of Organized Pediatrics in America
Before 1880, there was no organized group of physicians for children in the U.S. and, of course, no specific subspecialty fields within health care for children. The Section of Diseases of Children of the American Medical Association was organized in 1880 at a meeting of the AMA in Richmond, VA, with Abraham Jacobi chosen as president and Thomas Morgan Rotch as secretary (7, 19). Jacobi (1830–1919) was appointed Clinical Professor of Diseases of Children at Columbia University's College of Physicians and Surgeons in New York in 1870, after teaching as Professor of Infantile Pathology and Therapeutics at New York Medical College and then serving as Chief of Staff of the Nursery and Child's Hospital and teaching at the University Medical College in New York (3, 5). He was the first to teach medicine at the bedside (3). Jacobi is often called the “Father of American Pediatrics” and wrote extensively on a variety of pediatric problems, with his most frequent subjects related to infectious diseases, notably diphtheria. He advocated the use of boiled milk for infants (for nutritional reasons as well as to prevent the gastroenteritides). The inaugural issue of the AMA's American Journal of Obstetrics and Diseases of Women and Children in 1868, the first partially pediatric journal in the U.S., included an article on croup by Jacobi. Jacobi was an ardent social and political activist, striving to improve the circumstances of children.
Because the AMA group began to flounder and the membership of the Obstetrics and Gynecology Sections refused to allow pediatrics to form a separate section, a new group, the American Pediatric Society, the parent of organized pediatrics in the U.S., held an organizational meeting on September 18–20, 1888, at the Arlington Hotel in Washington D.C., with 14 physicians present (7, 19). Credit for forming the group is given to Job Lewis Smith (1827–1897) of Bellevue Medical School and William Booker (1844–1921) of Baltimore, the first Clinical Professor of the Diseases of Children at Johns Hopkins. Jacobi was elected the first President, and there were 43 founding members, predominantly from the Northeast, including William Osler, who later served as the fourth APS President (20). Four papers were scheduled to be presented (although it is not clear from the minutes that any of them in fact was presented), including “Treatment of Whooping Cough by Antipyrin” by L. Emmett Holt, Sr., of New York (21). Holt was Professor of Pediatrics at the New York Polyclinic Hospital and Attending Physician at Babies Hospital in New York. He was a Founder of the American Pediatric Society and served as President in 1898 and then again in 1923. Holt's presidential address in 1898 recapped his personal experiences with New York City children's hospitals, pointing out the discouraging 50% mortality for hospitalized infants and the very frequent nosocomial infections that occurred. He advocated care in the country, away from the crowded cities, during the summer months (21). This theme was echoed by Henry Koplik of New York, APS President in 1900, who reported the continued problem of summer diarrhea and recommended ambulatory care and a “colony or camping system” with care provided by live-in mothers (21).
Although it had improved somewhat compared with colonial times, the plight of children at the time of the founding of the American Pediatric Society in 1888 continued to be hazardous. Coincident with the Industrial Revolution, mortality rates had climbed substantially from early in the 19th Century to the later years of the 19th Century as major crowded urban areas developed. Life expectancy around 1888 was less than 50 years, infant mortality approached 200 per 1000 births, and neonatal mortality was about 50 per 1000 births (5, 21, 22). The infant mortality rate in 1880 in New York City, a particularly crowded urban area, was as high as 288 per 1000 live-born infants, primarily related to various infectious processes. Infectious diseases such as diarrhea, diphtheria, scarlet fever and tuberculosis dominated as the major causes of morbidity and mortality among children, and they had yet to be impacted by the just-emerging scientific base of medicine. The science of bacteriology, founded on the landmark discoveries of Louis Pasteur in Paris, Robert Koch in Berlin, and others in the early 1880s, had not yet impacted child health. Roentgen had not yet discovered x-rays. Biochemical analyses were not available for infants and children. Inadequate sanitation, impure water and unsafe milk supplies all contributed very significantly to the spread of infectious diseases among infants and children, and particularly to those living in the very crowded circumstances that promote transmission.
The early years of organized U.S. pediatrics were marked by a number of landmark advances in the diagnosis and treatment of infectious diseases of children, with substantial reduction in infant mortality rates, to 189/1000 live births in New York City in 1900, with rates as low as 147 in Chicago and as high as 311 in Biddeford, ME (5).
SCIENTIFIC PRESENTATIONS
The importance of infectious diseases to the relatively small number of founding members of the American Pediatric Society, a group of distinguished physicians who devoted much or all of their effort to the improvement of the health of children, is reflected by analysis of the topics of the papers presented at the early annual scientific meetings of APS. The first scientific meeting of the APS held in Washington on September 20, 1889, and the next day in the then-new Johns Hopkins Hospital included many presentations devoted to classic infectious diseases. These included two papers devoted to diphtheria, two elaborate bacteriologic studies of the stools in infant diarrhea (Booker isolated 19 bacterial varieties and Jeffries 28 different organisms), a paper on malaria in New York City, two papers related to infant feeding and prevention of infant diarrhea, and assorted case reports (7, 11). At least 46 of the 87 papers delivered at the first five annual scientific meetings (1889–1893) directly addressed infectious diseases topics, including diphtheria (8), diarrhea (7), scarlet fever and rheumatic fever (6), tuberculosis (6), pneumonia and empyema (6), typhoid fever (3), pertussis (2), lues (1), vulvo-vaginitis (1), malaria (1), and miscellaneous infections (5) (19). This dominance of the scientific agenda by infectious diseases topics attests to their extreme importance as the major causes of morbidity and mortality in childhood at the end of the 19th Century.
SPECIFIC INFECTIONS
Diphtheria.
Hippocrates had recognized the unfavorable implications of a sort of spiderweb (or membrane) in patients with tonsillar ulcers (2), and both Bard's 1771 contribution and the introduction of tracheostomy for laryngeal diphtheria in France in the 1820s have been noted (vide supra). Diphtheria was of particular concern at the early American Pediatric Society meetings, as the laryngeal form of the disease in that era was almost invariably fatal, despite the use of tracheostomy. The few years just before the founding of the APS and the early years of the organization represented a period of landmark advances in understanding the etiology of this illness and in the development of markedly improved treatment modalities. In 1884 Friedrich Loeffler proved that a specific bacterium was the etiologic agent of diphtheria. The introduction of the O'Dwyer intubation tube in 1885 received great attention because for the first time it enabled successful treatment of the suffocation that was associated with laryngeal diphtheria (23). Joseph O'Dwyer (1841–1898), Attending Physician at the New York Foundling Hospital, a facility for unwanted children, was a Founder of American Pediatric Society, and he served as President of APS in 1896 (19). O'Dwyer's 1896 presidential address reviewed his invention and experience with the intubation tube (7, 21).
At the 7th annual scientific meeting of the APS in 1895, papers from four groups regarding the dramatic, even revolutionary, effects of diphtheria antitoxin for therapy and prevention were presented. This led to the adoption of a formal resolution: “Resolved, that, in the opinion of the Society, the evidence thus far produced regarding the effects of diphtheria antitoxin, justifies its further and extensive trial”(7, 19). A committee was apparently appointed, as the 1896 annual meeting included a report from the American Pediatric Society's Collective Investigation of the Antitoxin Treatment of Diphtheria in Private Practice, chaired by L. Emmett Holt. This confirmed the spectacular results of the 1894 French report by Roux, Martin, and Chaillou from the Pasteur Institute in Paris. The 1897 meeting received a report from the Committee on Collective Investigation of the Antitoxin Treatment of Laryngeal Diphtheria in Private Practice, chaired by William P. Northrup (24). These clinical studies of diphtheria equine antitoxin represented the first pediatric investigations in the U.S. of a national scope. The four committee members analyzed 1704 cases of laryngeal diphtheria treated with antitoxin who were submitted by APS members and concluded that antitoxin lowered the necessity for intubation from 90% to 39% and the mortality rate from 73% to 27% in this severest form of diphtheria (24). The Schick test to assess susceptibility to diphtheria was introduced by Bela Schick in 1913. Emil von Behring of Germany, who initially discovered diphtheria toxin and developed the diphtheria antitoxin that was of such great interest and importance, was awarded the first Nobel Prize in Medicine in 1901 for this work.
Tuberculosis and meningitis.
Tuberculosis was another very common and serious problem of childhood, and William Osler was very actively involved in its study before moving to Oxford, England, in 1905 to become the Regius Professor. Osler's commitment to pediatrics is apparent from his frequent participation in the APS meetings to discuss tuberculosis, pertussis, chorea and carditis, croup, peritonitis and other topics, as well as from the 10% of his writings which are on pediatric subjects. He was particularly interested in tuberculosis of childhood and presented a paper at the third APS meeting in 1891 on pulmonary tuberculosis in children, in which he divided it into acute, subacute, and chronic or protracted forms (20, 25), and another in 1893 that included autopsy findings (7). Papers on childhood tuberculosis were presented at virtually all of the APS scientific meetings during the early decades. Particularly noteworthy milestones included Walter Carr's 1912 presidential address that reported a 71% decline in extrapulmonary tuberculosis, the 1927 report by the Parisian Armand-de Lille of the diagnostic value of gastric aspirates in infants, the 1930 report by Bela Schick and colleagues on the BCG vaccination introduced three years earlier in France, Detroit's Joseph Johnston's discussion in 1936 of the evolution of pediatric TB to the adult type by endogenous reactivation, and the exciting initial report in 1947 by John Lyttle and colleagues from Los Angeles of the recovery of a patient with miliary TB after streptomycin treatment (7).
Meningitis, including the invariably fatal tuberculous meningitis, was also a common affliction of children in the late 19th Century. Abraham Jacobi wrote about meningitis that the U.S. “more than any other country has been invaded by this plague”(26). At the 1896 meeting of APS, August Caillé (1854–1935) presented a paper on “Tapping the vertebral canal in the lumbar region” and the following year a paper on “Local treatment for tubercular meningitis”(19). These were the first reports to the APS of diagnostic lumbar puncture, after it had been introduced by Quincke in 1891 as a treatment modality (2, 7). Two additional papers presented in 1896 discussed lumbar puncture in the subarachnoid space, which provided a scientific basis for studying meningitis, with measurement of sugar and protein, and a potential route of administering therapy, such as it was in the late 19th and early 20th Centuries (7).
Summer Diarrhea and the Milk Supply.
In addition to the introduction of intubation techniques and diphtheria antitoxin, an exceptionally important advance during the late 19th Century and early 20th Century was the result of efforts by concerned pediatricians and others to secure a safe and sanitary milk supply for infants (5). Nonbreast-fed infants experienced particularly high mortality rates, because much of the cow milk supply was “swill milk,” which came from cows fed only distiller's mash, housed in incredibly filthy conditions, without fresh air, exercise or hay, many of which were also infected by bovine tuberculosis (2, 5, 7, 22).
Job Lewis Smith, who was one of the first to differentiate rubella from rubeola and wrote several papers on neonatal tetanus, served as the second APS President in 1890, 18 years after he had written in his textbook that more than half of New York's infants who were spoon-fed (i.e. not nursed or wet-nursed) in the summer, died before fall (27). He strongly urged milk sterilization and wrote and spoke about the dangers of artificial infant feeding. Bacteriologic studies of milk began to establish a scientific basis for the association of impure milk with infant diarrheal illnesses, including the work of the pediatrician Escherich in 1886, Shiga in 1898, and Flexner in 1900. The genera Escherichia and Shigella (as well as the species Shigella flexneri) honor these pioneer bacteriologists. William D. Booker's major area of interest was summer diarrhea of infancy. He presented a paper at the first APS scientific meeting in 1889 on that topic (7), and he devoted his presidential address in 1901 to the early history of summer diarrhea in America from colonial times (21).
The problem of summer diarrhea and its increasingly clear relationship to contaminated milk in the urban poor was highlighted by the report of 1500 infant deaths per week in New York City during the hot weather summer months that were associated particularly with bottle feeding (28). Considerable attention of organized pediatrics was focused on this issue, particularly by Henry L. Coit (1854–1917), Smith, Rotch, Isaac Abt, Schick, and others, who advocated movement toward certified safe milk (5, 11). Coit began as early as 1887 to work tirelessly to ensure a safe milk supply for infants, after the death of his young son, by educating the public, lawmakers, and the medical community (5). He coined the term “Certified Milk” and established the first Medical Milk Commission in New Jersey (19). Henry Koplik (President of APS in 1900) established the first American clean milk depot in New York in 1889 (called Gouttes de Lait), and Thomas Morgan Rotch (a Founder of APS and President in 1891) organized the Walker-Gordon farms that led to the first milk laboratory for preparing safe milk formulas.
Pasteurization of milk by heating was introduced in Europe before 1890 (and had been used for wine since 1864!), and it was promoted particularly by Jacobi in the U.S. during the 1890s for its ability to prevent milk-borne infections. Many other academics preferred certification as an alternative to pasteurization, fearing that the latter would alter the chemical composition of milk and promote gastroenteritis. This proved wrong (29). Jacobi collaborated with the philanthropist Nathan Straus to establish pasteurization plants and milk stations for poor infants in New York beginning in 1893. A reduction in infant mortality of 65% was observed in just one year in the foundling hospital on Randall's Island after a pasteurization plant was established there by Straus (2, 5). However, it was not until 1908 that Chicago became the first city in the world to require pasteurization of milk, with many cities following thereafter (5). Controversy in this area was apparent early on, best exemplified perhaps by the resignation from the APS in 1892 of Arthur V. Meigs of Philadelphia, who argued vehemently against milk sterilization and who continued to reject the germ theory of disease until his death in 1912 (6, 21).
Thomas M. Rotch (1849–1914) was America's first full Professor of Pediatrics, appointed at Harvard in 1893. Rotch published a major textbook of pediatrics in 1896 as well as early reports of the value of the roentgen ray in pediatrics, in addition to his detailed studies of milk. Although extremely focused on the biochemical composition of milk, calculating in minute detail the precise amounts of protein, fat and sugar content of milk for infants, he also recognized the importance of a safe milk supply and worked to achieve that goal. The improved milk supply was complemented by studies, primarily at Johns Hopkins, by Holt, James Gamble, W. McKim Marriott, John Howland, and others, that led to understanding the roles of acidosis and dehydration in contributing to the mortality of infants and children with acute diarrhea. This led directly to effective rehydration and correction of electrolyte imbalances in such children with improved outcomes (25).
Scarlet Fever.
In the latter decades of the 19th Century, case-fatality rates for scarlet fever were very high, particularly in the youngest children. Holt's 1897 textbook, The Diseases of Infancy and Childhood, indicated the case-fatality rate to be as high as 55% in those under one year and 7% to 22% in those under three years (30). Wide year-year fluctuations were sometimes observed, with annual death rates during the decade of the 1850's, for example, from as low as 6/100,000 to a high of 272/100,000 population. Representative case-fatality rates during the latter years of the 19th Century were 12.3% in New York in 1889, 20% in 1886–1888 in Providence, RI, and 11.8% in Philadelphia in 1897 (21.8% for those 1–5 years old) (5). In addition to person-person spread of streptococcal infections including scarlet fever, contaminated milk was also shown to produce explosive epidemics of very acute streptococcal pharyngitis with high mortality. This provided an additional reason to support pasteurization of milk (7).
By the close of the 19th Century, scarlet fever had overtaken diphtheria as a cause of death, occurring with great frequency and often with high case-fatality rates. The 1894 pediatric text of Louis Starr (1849–1925) described scarlet fever as the most widely disseminated of the childhood exanthems and “the most dreaded of all the diseases of children.”(31)
Poliomyelitis.
Poliomyelitis, which was initially described in Underwood's first edition in 1784, was brought to general medical attention by Jacob von Heine (German). von Heine was a pioneer of orthopedics who published a classic monograph on infantile paralysis and its resultant deformities in 1840, and he recognized the spinal cord localization of the pathology (3). The classic French pediatric text of Rilliet and Barthez (1838–1843) provided an early account of polio, and Guillaume-Benjamin-Amand Duchenne (French) localized the lesion in polio to the anterior horn cells in 1855 (18). Later in the 19th Century, Oscar Medin (Swedish) first noted the epidemic character of polio when he observed an outbreak of 44 cases in Stockholm in 1887 (18). In 1894 a larger epidemic of 132 cases occurred in Rutland County, VT (5).
EARLY TWENTIETH CENTURY
From the turn of the century until about 1915, the pediatric community focused particularly upon major public health and welfare issues that adversely affected children, working particularly hard to improve the milk supply. Walter L. Carr's 1912 presidential address to the APS very clearly spelled out the impressive improvements in the health of children that had occurred during the early years of the 20th Century (7). Infant mortality in greater New York City declined 40% from 203/1000 live births in 1898 to 120 in 1911. As a consequence of the efforts to improve the milk supply, diarrheal deaths had declined 43%. Mortality from measles, scarlet fever, pertussis, and diphtheria had declined 54%, while that from acute respiratory disease including pneumonia fell 32%(7).
During the period from 1881 to 1914, the etiologic agents of more than 30 infectious diseases were identified (32). As microbiologic advances were made, American Pediatric Society meetings continued to include many papers related to epidemic infectious diseases including summer diarrhea, poliomyelitis, typhoid fever, gonococcal infection, and meningococcal meningitis. Increasingly large U.S. poliomyelitis epidemics occurred, primarily affecting children, for example in New York City in 1907, with almost 3000 cases and up to 12% mortality (7). This peaked in a 1916 epidemic in the Northeast with almost 30,000 cases and 6,000 deaths, many in the New York City area, leading to massive public anxiety and aggressive public health measures including quarantine and travel restrictions (5). Progress in understanding the etiology and pathogenesis of polio was made early in the 20th Century. In Vienna in 1909 Landsteiner and Popper transmitted polio to monkeys by intraperitoneal injection of spinal cord material from a child who died early in the course of polio. Also in 1909 Simon Flexner (of Shigella flexneri fame) and Paul Lewis in New York extended those studies to show transmission to monkeys also after s.c., i.v., or intracerebral routes of inoculation and produced disease using filtrates of nasopharyngeal washes from polio patients (5). Additional Flexner studies from 1910–1917 showed that sera from monkeys that recovered neutralized the infectivity of polio material, that intrathecal injection of convalescent sera within 24 h of inoculation prevented paralysis, that recovered monkeys were protected against subsequent inoculation, and that recovered human patient sera contained antibodies to the infectious agent (5). Great effort was devoted by several groups to use intrathecal administration of convalescent polio sera to treat children with acute poliomyelitis but this proved unhelpful (5). The development of the iron lung by Philip Drinker in the late 1920s was a noteworthy therapeutic advance for affected patients.
During the period from 1900 to 1915, the application of serum therapy to the management of diphtheria, meningococcal and streptococcal infections served as topics for many APS presentations (19). Jacobi's second APS presidential address, in 1906, was entitled “The Tonsil as a Portal for Microbic and Toxic Invasion,” while that of J. L. Morse in 1913 reviewed the high mortality of pertussis, especially in infants, and proposed stringent isolation (21). Specific therapy for congenital syphilis with salvarsan, introduced by Ehrlich two years earlier, was reported by LaFétra in 1912, with dramatic benefit (7). In his APS presidential address in 1923, L. Emmett Holt summarized the dramatic improvement in mortality in those less than five years old from infectious diseases in Manhattan and The Bronx from 1896–1897 to 1921–1922, with approximately an 80% decline in diarrheal deaths, diphtheria and croup, and 60% for pneumonia (33).
Over the next 2 decades (∼1915–1938), academic pediatricians and their research were focused particularly upon nutrition and the biochemistry of health and disease, which during this time somewhat eclipsed infectious disease concerns (21). Nevertheless, syphilis, tuberculosis, pertussis, measles, rheumatic fever, streptococcal infections, polio, and meningitis continued to interest those caring for children, as reflected by papers presented at the annual APS meetings. Active immunization against diphtheria using toxin and antitoxin was introduced by Alfred Hess in the U.S. in 1916 (7). At the end of this era, a particularly interesting paper was presented in 1937 by Francis Schwentker, who reported the treatment of meningococcal meningitis with s.c. and intrathecal para-aminobenzenesulfonamide (sulfanilamide) (7). The first use of an antimicrobial agent in the U.S. was by future APS President A. Ashley Weech, whose unsuccessful treatment of a physician's child with H. influenzae meningitis with the sulfanilamide-containing compound sulfachrysoidine in 1935 has been well documented (34, 35). The actual administration of this agent was by the Chief Resident at Babies Hospital in New York, F. Howell Wright, who later served as Chair of Pediatrics at the University of Chicago and President and Executive Secretary of the American Board of Pediatrics (35). During this era, several APS presidential addresses concerned infectious disease issues, including that by Linnaeus LaFétra in 1918 regarding the need for preventive measures against infectious diseases and rheumatic fever in children two to six years old; by Thomas S. Southworth in 1920 on the communicability of acute pneumonia and the need for isolation of such patients, as was done for tuberculosis patients; by L. Emmett Holt in 1923 highlighting the decline in infectious diseases, particularly diarrhea, diphtheria and acute respiratory disease (as discussed above); and by Henry F. Helmholtz in 1937 on infections of the renal parenchyma and the importance of stasis in predisposing to urinary tract infection (7, 19).
During this period the first pediatric department with several identified subspecialists was developed by Edwards A. Park at Johns Hopkins beginning in 1926. Under the previous leadership of John Howland from 1912–1926, there had not been any special clinics or pediatric subdepartments at Hopkins, with the exception of a clinic for the treatment of congenital syphilis. Curiously it was Lawson Wilkins, later known as the father of pediatric endocrinology, who initiated and organized the congenital syphilis clinic as an intern (25). As a discipline, infectious diseases did not figure as prominently as cardiology, endocrinology, neurology and other nascent subspecialty areas under Park's leadership. This theme was replicated in most other academic departments as subspecialization began to develop. A few exceptions were pediatricians known for their expertise in contagious diseases, some of whom were particularly interested in vaccine development. These included Bela Schick at Mt. Sinai and at Albert Einstein in New York, Hattie Alexander and Horace Hodes at Columbia University, Joseph Stokes at University of Pennsylvania, Russell Blattner at Baylor, William Bradford at Rochester, Amos Christie at Vanderbilt, Katherine Dodd at Vanderbilt and Cincinnati, Edith Lincoln at New York University, Louis Sauer at Evanston, IL, and John Zahorsky in St. Louis.
By 1938, when the American Pediatric Society was a half-century old, life expectancy had increased to over 60 years, infant mortality had declined to about 55/1000 and neonatal mortality to about 30/1000 (22). Sewage and sanitation had improved greatly, which along with much safer milk supplies had led to a marked fall in diarrheal illnesses of infancy. A few vaccines had been introduced, but antibiotic therapy was limited to the early use of sulfanilamide. At the 50th annual meeting of APS in 1938, the first held in conjunction with the young Society for Pediatric Research (SPR), important papers presented included that of Trask and Paul, reporting the isolation of poliovirus from nasal washes and stools of asymptomatic patients, several related to the pathogenesis of pertussis, that of Lyttle showing elevated ASO titers in acute glomerulonephritis, Hodes' report of an irradiated rabies vaccine, and Stokes' isolation of various strains of influenza virus. These works served as the prelude to the much more dramatic advances to come, related to the pathogenesis, diagnosis, and treatment of viral and bacterial infections of children (7).
NEW PEDIATRIC ORGANIZATIONS
Between 1930 and 1933, three new pediatric organizations emerged: the American Academy of Pediatrics in 1930, the Society for Pediatric Research in 1931, and the American Board of Pediatrics in 1933. The Eastern Society for Pediatric Research, organized in 1929, became a national organization (also including Mexico and Canada) called the Society for Pediatric Research (SPR) in 1931, with the goals to foster research in pediatrics and to serve the younger pediatric faculty (<45 years old), as the APS meetings were quite closed to junior investigators. The first meeting of the SPR was held in May, 1932, and since 1938 the APS and SPR have held joint meetings, with greater prominence of infectious diseases as a separate subspecialty in more recent years.
Presidents of SPR who have been associated with a particular interest in infectious diseases are shown in Table 1.
Table 1.
Presidents of the Society for Pediatric Research with Major Infectious Diseases Interests

The American Academy of Pediatrics (AAP) was founded in 1930 to promote the welfare of children. This occurred after the American Medical Association House of Delegates severely chastised the Pediatric Section of the AMA for taking pro-active stances favoring the Sheppard-Towner Act, which supported maternal and child health. Isaac Abt of Chicago became the first President of the AAP, which had 304 charter members and held its first meeting in Atlantic City, NJ, on June 12–13, 1931 (7). Early in its existence, the AAP declared its interest and involvement in infectious diseases issues. The AAP established a Special Committee on Prophylactic Procedures Against Communicable Diseases in 1933, chaired by Edward B. Shaw of San Francisco and including J.E. Gordon of Detroit and J.A. Toomey of Cleveland. This committee was disbanded after its report “Routine Measures for the Prophylaxis of Communicable Diseases” was published in The Journal of Pediatrics in April 1935 (36). This six-page report dealt with diphtheria, scarlet fever, typhoid fever, whooping cough, measles, smallpox, polio (3 lines), epidemic meningitis (1 line), mumps and chickenpox (4 lines), rabies, and tetanus. The Committee on Immunization Procedures was then established in 1936, with John A. Toomey as chair. Three years later the committee name was changed again to the Committee on Immunizations and Therapeutic Procedures for Acute Infectious Diseases, in 1953 it was modified again to the Committee on Control of Infectious Diseases, and then in 1969 to the Committee on Infectious Diseases, the current name, although it is now most commonly referred to as the Red Book Committee. Since 1938, this AAP committee has published a report every one to five years (every three years for the past five editions), which because of the color of its binding has been known as the Red Book for many editions. The 26th edition of this document, the closest thing to a Bible (albeit frequently revised) in the field of pediatric infectious diseases, was published in 2003. Chairs of the Committee on Infectious Diseases and editors of the committee reports (the Red Books) have included John A. Toomey, John R. Miller, Jr., Aims C. McGuinnes, Edward C. Curnen, Jr., Alex J. Steigman, Lewis L. Coriell, Franklin H. Top, Margaret H. D. Smith, Samuel L. Katz, Martha D. Yow, Vincent A. Fulginiti, Edward A. Mortimer, Jr., Jerome O. Klein, Philip A. Brunell, Georges Peter, Stanley A. Plotkin, Caroline B. Hall, Neal A. Halsey, John S. Abramson, Larry K. Pickering, and Margaret B. Rennels. In 1990 the AAP established the Section on Infectious Diseases, which has assumed major responsibility for developing educational infectious diseases programs for the general membership of the AAP. Chairs of the SOID have included David Lang, Stanford Shulman, and Ellen Wald.
THE POST-WAR BOOM YEARS
After World War II came the postwar boom, noteworthy for the expanded availability of federal research funds (especially from the National Institutes of Health), increasingly sophisticated research and technology, the development of vaccines against polio and measles, and the discovery of ever-more-active antibiotics and other anti-infectives, with the initial emergence of antibiotic resistance, e.g. penicillin-resistant S. aureus. The period from 1945 to about 1965 heralded the era of modern infectious diseases and coincided with the increasing trend to subspecialization within pediatrics and the development of full-time pediatric departments. Antimicrobial advances included the discoveries of streptomycin, isoniazid and then other agents to treat tuberculosis, as well as penicillin, chloramphenicol, streptomycin and other antibiotics for treatment of bacterial infections. Virtually universally fatal infections such as bacterial meningitis and endocarditis became amenable to therapy. American Pediatric Society presidential addresses during this period that dealt with infectious diseases topics included that by Jean V. Cooke in 1949 discussing the impact of specific therapy including antimicrobials upon the common contagious diseases and reviewing mortality statistics from 1930–1945; by Hugh McCulloch in 1952 on progress in prevention and treatment of rheumatic fever; by A. Ashley Weech in 1958 on milestones in scientific pediatrics, including the conquest of infectious diseases and the development of antibiotics; and by Joseph Stokes Jr. in 1959 regarding airborne infections and their prevention (7). This era was associated with the virtual elimination of congenital syphilis, early studies of bacterial resistance to antibiotics, improved methods of viral cultivation, but also large poliomyelitis epidemics.
The control of acute rheumatic fever and rheumatic heart disease was a consequence of the studies of Floyd Denny, Lewis Wanamaker, and others that proved that recurrent attacks could be prevented by antibiotic prophylaxis. Edith Lincoln's clinical studies of tuberculosis were classic. Hattie Alexander, President of APS in 1965, made great contributions to the improved understanding of the pathogenesis and treatment of H. influenzae infections. Other early postwar period pediatricians with special interests (clinical and/or research) in infectious diseases included Edward Curnen at Chapel Hill and Columbia, Heinz Eichenwald at New York Hospital and Dallas, Dorothy Horstman at Yale, Benjamin Kagan at UCLA, David Karzon at Buffalo, C. Henry Kempe at Colorado, Saul Krugman at New York University, Harris Riley at Oklahoma, Fred Robbins and Ed Mortimer at Case Western, Albert Sabin at Cincinnati, T. F. McNair Scott at University of Pennsylvania, Margaret Smith at Tulane, Martha Yow at Baylor, Alex Steigman at Louisville, Robert Ward at CHLA, Paul Wehrle at USC, Tom Weller at Harvard, Herb Wenner at Kansas City, Warren Wheeler at Ohio State and Kentucky, Henry Cramblett at Iowa and Ohio State, Robert McAllister at CHLA, and Harry Feldman at Syracuse.
THE DEVELOPMENT OF TRAINING PROGRAMS
In the 1950s National Institutes of Health training grants began to be available for support of physicians in subspecialty training, while other individuals obtained training at federal facilities including the Centers for Disease Control (including the Epidemic Intelligence Service Program), National Institutes of Health, and Walter Reed Institute. Some, including James Cherry and Jerome Klein, trained in the primarily adult program of Maxwell Finland at Boston City Hospital. By the late 1950s more formal Pediatric Infectious Diseases training programs were being established at the University of Minnesota (Lewis Wannamaker, Paul Quie), NY University (Saul Krugman, Edith Lincoln), University of Colorado (C. Henry Kempe), NY Hospital (Heinz Eichenwald), and Dallas (John Nelson). In the early 1960s programs were established at Wisconsin (James Cherry), Harvard and Boston University (Jerome Klein), Harbor UCLA (Joseph St. Geme, Jr.), CHLA (R. McAllister and Robert Ward), Miami (James Connor), Yale (Dorothy Horstmann), Harvard (Tom Weller, Frank Neva, Fred Robbins, Sam Katz), University of Pennsylvania (Joseph Stokes and T. F. McNair Scott), USC-LA County (Paul Wehrle), Johns Hopkins (Don Medeiros), Cleveland Metropolitan General (Edward Mortimer), Children's Hospital Boston (David Smith), and University of Florida (Elia Ayoub).
THE ERA OF SPECIALIZATION AND FRAGMENTATION
The period from 1966 to about 1985 has been termed the era of specialization and fragmentation of pediatrics by Howard Pearson (21). At the onset of this era, the 1966 program of the Society for Pediatric Research listed no Infectious Diseases subspecialty session per se but rather one session devoted to “Microbiology/Immunology” that included a handful of papers (out of the 101 in total that were presented) on topics that can be considered infectious diseases issues.
Several APS presidents during this era were closely linked to the emerging field of pediatric infectious diseases. (See Table 2). Warren Wheeler in 1972 in his presidential address discussed the epidemics of enteropathogenic E. coli 0111 in the 1930s and 1940s and those of S. aureus 80/81 in the 1950s, recommending surveillance to detect emergent bacterial “hot strains”(21). Saul Krugman, APS President in 1973, devoted his distinguished career to the field of infectious diseases, especially to the study of hepatitis viruses. Fred Robbins (1974) and Horace Hodes (1975) were each responsible for signal discoveries in virology, the former having received the Nobel Prize in 1954 with John Enders and Tom Weller for the development of tissue culture technology that led to viral vaccine production, and the latter devoting his life to investigations of viral gastroenteritis of infants and vaccine development (21). Margaret H. D. Smith (1977) worked tirelessly in the field of pediatric tuberculosis and advocated for social activism by organized pediatrics. C. Henry Kempe (1978) was instrumental in the eradication of smallpox, and Floyd Denny (1981) contributed to the understanding of group A streptococci and to the conquest of rheumatic fever. During this era, infections in the immunocompromised child began to emerge as an important clinical problem, as increasing numbers of cancer patients and other compromised patient populations were generated by improved treatment modalities (37), and these were accompanied by increasing numbers of opportunistic viral, fungal and bacterial infections requiring expert management.
Table 2.
Presidents of the American Pediatric Society with Major Infectious Diseases Interests

PEDIATRIC INFECTIOUS DISEASES ORGANIZATIONS
It was during this time that many subspecialty organizations within pediatrics were born, including the Pediatric Infectious Diseases Club. Formal organizations within the field of Pediatric Infectious Diseases emerged gradually as the subspecialty became more clearly defined and differentiated from the rest of Pediatrics during the 1960s and 1970s. In 1977–1978 Stanley Plotkin of Philadelphia led the establishment of the Pediatric Infectious Diseases Club, which held its first election of officers in 1982–1983. This Club evolved into the Pediatric Infectious Diseases Society (PIDS) in 1984, and it has grown into a very active organization to which the vast majority of those in the field belong. The Pediatric Infectious Diseases Society has established an effective partnership with the Infectious Diseases Society of America and with both the Section on Infectious Diseases and the Committee on Infectious Diseases of the American Academy of Pediatrics. Presidents of the Pediatric Infectious Diseases Society have included Stanley Plotkin, Walter Hughes, Jerome Klein, Phil Brunell, James Cherry, Caroline Hall, Carol Baker, Georges Peter, Larry Pickering, K. Lynn Cates, Sarah Long, Richard Jacobs, and Sheldon Kaplan.
THE MODERN ERA
The modern era, from about 1986 to the present, is the period of modern molecular biology and genomics, with advances based upon new diagnostic modalities such as DNA hybridization and sequencing, cloning, PCR, magnetic resonance imaging, PET scanning and many others. Laboratory techniques for research related to pediatric illnesses have used these and other increasingly sophisticated molecular methods. The elucidation of the first bacterial genome, that of Hemophilus influenzae, in 1995 heralded vast new opportunities to understand the pathogenesis of infectious diseases (38). Although many classic pediatric infectious disease disorders have virtually disappeared, new (or apparently new) clinical challenges such as opportunistic infections in the ever-increasing populations of immunocompromised patients, Lyme disease, Kawasaki disease, SARS and HIV/AIDS have emerged.
The onset of the AIDS epidemic in the early 1980s and the identification of HIV as its causative agent had a substantial impact upon the specialty of pediatric infectious diseases. Identifying perinatal vertical transmission risk factors, dealing with transfusion-associated HIV infection (particularly in the hemophiliac population), and determining the clinical, virologic and immunologic parameters of pediatric AIDS occupied the first decade or so of the pediatric AIDS experience. The landmark 1994 report of the Pediatric AIDS Clinical Trials Group Protocol 076 that demonstrated the marked effectiveness of zidovudine administered to pregnant women to prevent vertical transmission of HIV led to dramatic reduction in the number of perinatally infected children within several years in developed countries. In other areas of the world, where anti-retroviral therapy during pregnancy is not being utilized, vertical transmission of HIV continues unabated. In recent years, in the U.S., the field of pediatric AIDS has focused increasingly upon prevention and treatment of adolescent HIV infection as well as upon the highly effective multi-drug therapies.
Table 2 provides a listing of presidents of APS with major interests in infectious diseases issues. Recent APS presidents have included Sam Katz (1987), whose career has been devoted to vaccine development and implementation; Paul Quie (1988), a bacterial phagocytosis scholar; Vince Fulginiti (1992), who advanced the fields of prenatal infections and viral vaccinology; and Ralph Feigin (1998), an authority on meningitis and many other aspects of pediatric infectious diseases.
AWARDS
Nobel laureates.
Four members of the American Pediatric Society (including one Honorary member) have been awarded the Nobel Prize in Physiology and Medicine, and all of them were recognized for research related to infectious diseases and their prevention. In 1954, Thomas Weller, Frederick Robbins, and John Enders received the Nobel “for their discovery of the ability of poliomyelitis viruses to grow in cultures of various types of tissues.” Enders, a basic virologist, was elected to Honorary APS membership in 1962, and Weller and Robbins are full members. Additionally, D. Carleton Gajdusek received the 1976 Nobel “for discoveries concerning new mechanisms for the origin and dissemination of infectious diseases,” specifically for the study of kuru and slow virus infections.
Howland Award.
The John Howland Award of the American Pediatric Society “for distinguished service to Pediatrics” was initiated in 1952, and a number of Howland Awardees have been honored particularly for contributions to the conquest of infectious diseases of childhood. These include Bela Schick in 1954 for his studies of diphtheria, Harold K. Faber in 1956 for studies of poliomyelitis and pediatric history, Joseph Stokes Jr. in 1962 for his work on virology and poliomyelitis, Albert Sabin in 1974 for his creation of the oral attenuated poliomyelitis vaccine, Amos Christie in 1979 for research on histoplasmosis, C. Henry Kempe in 1980 for studies of smallpox and child abuse, Saul Krugman in 1981 for hepatitis and virology, Horace Hodes in 1982 for vaccine development and studies of viral gastroenteritis, Floyd Denny in 1995 for work related to rheumatic fever and Group A streptococci, and Sam Katz in 2000 for his unstinting efforts related to vaccines and their implementation.
E. Mead Johnson Awards.
The E. Mead Johnson Award of the Society for Pediatric Research was established in 1939 to honor research accomplishments in pediatrics. Awardees for research activities in the field of pediatric infectious diseases have included Rene Dubois (1941) for development of antibacterial agents, Albert Sabin (1941) for research into viral nervous system infections, David Bodian and Howard A. Howe (1942) for studies of the pathophysiology of poliomyelitis, Hattie Alexander (1943) for studies related to treatment of H. influenzae infections, Horace Hodes (1946) for studies of the transmission of Japanese B encephalitis, Paul Harper (1946) for studies of malaria in the South Pacific, Gertrude and Walter Henle (1950) for prevention of mumps, Seymour Cohen (1952) for research on bacteriophages, Fred Robbins and Thomas Weller (1953) for developing viral tissue culture, Margaret Smith (1953) for bacteriologic studies, C. Henry Kempe (1959) for smallpox vaccination studies, Richard T. Smith (1963) for neonatal infection and immunity, Robert Chanock (1964) for prevention of pediatric respiratory infections, Henry M. Meyer, Jr. and Paul D. Parkman (1967) for development of the attenuated rubella vaccine, Paul Quie (1971) for antibacterial host defense studies, Andre Nahimias (1974) for studies of in utero infections, John Robbins and David Smith (1975) for studies of prevention of H. influenzae infection, Robert Yolken (1989) for rapid viral diagnostic methods, Ann Arvin (1992) for pathogenetic and immunologic studies of herpes viruses, Margaret Hostetter (1995) for studies of the pathogenesis of candidiasis, and Elaine Tuomanen (1997) for mechanisms of bacterial pathogenesis.
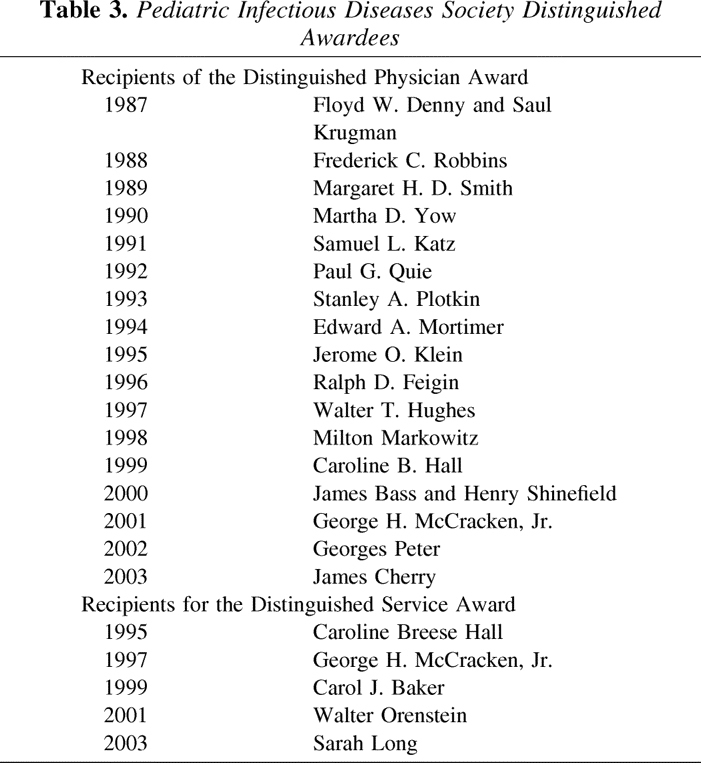
Pediatric Infectious Diseases Society Awards.
The Pediatric Infectious Diseases Society established two awards to honor distinguished physicians and distinguished service to the field. The former was established in 1987 and the latter first awarded in 1995. Recipients of the Distinguished Physician Award and the Distinguished Service Award of the Pediatric Infectious Diseases Society are shown in Table 3.
Table 3.
Pediatric Infectious Diseases Society Distinguished Awardees
OTHER ORGANIZATIONS
The first Committee on Rheumatic Fever of the American Heart Association was organized in 1940, with T. Duckett Jones (famous for his Jones Criteria proposed in 1944) serving as the first chair. Over the subsequent 63 years, this committee has expanded its scope to include infective endocarditis and Kawasaki disease, and its membership has been weighted heavily to include pediatric infectious diseases experts as well as cardiologists. In contrast to many other organizations, World War II actually accelerated the activities of this group because of the severity of rheumatic fever and rheumatic heart disease among both children and military recruits. The current title of this group is the Committee on Rheumatic Fever, Endocarditis and Kawasaki Disease of the Council on Cardiovascular Disease in the Young. Chairs of this committee with close connection to pediatric infectious diseases have included Maclyn McCarty, Lewis Wannamaker, Floyd Denny, Milton Markowitz, E. Kaplan, Adnan Dajani, Patricia Ferrieri, and Stanford Shulman.
The Infectious Diseases Society of America was established in 1962, and a number of Pediatric Infectious Diseases specialists have served with distinction in this organization. Pediatrician presidents of the IDSA have included Albert Sabin (1969), Dorothy Horstmann (1975), Floyd Denny (1980), Paul Quie (1985), Catherine Wilfert (2000), and Carol Baker (2001).
CERTIFICATION AND ACCREDITATION
The American Board of Pediatrics (ABP), which was founded in 1933, first certified general pediatricians in 1934. It then provided its first subspecialty certification in 1961 (cardiology). In May 1990 the ABP approved a proposal from the Pediatric Infectious Diseases Society to certify individuals in pediatric infectious diseases, and the ABP then applied to the American Board of Medical Specialties (ABMS). ABMS approved this application on March 21, 1991, and the ABP established the Sub-Board of Pediatric Infectious Diseases in 1991 (39). The initial certifying examination in pediatric infectious diseases was offered on November 15, 1994 with 607 candidates taking the examination and 493 passing (39). By 1998, after program applications were submitted and reviewed, a number of training programs for Pediatric Infectious Diseases fellows were accredited by the Accreditation Council for Graduate Medical Education (ACGME).
PUBLICATIONS
Several publications have been developed within the field of Pediatric Infectious Diseases, sponsored by various organizations. The AAP's Report of the Committee on Infectious Diseases (the Red Book) is mentioned above. The Pediatric Infectious Diseases Society organized the establishment of The Report on Pediatric Infectious Diseases, published by Churchill-Livingstone ten times yearly, beginning in January 1991. In 1998 The Report was changed to Concise Reviews of Pediatric Infectious Diseases and was incorporated within the monthly Pediatric Infectious Diseases Journal. The latter journal had been established in January 1982 by George McCracken and John Nelson and became the official journal of the Pediatric Infectious Diseases Society in 1995.
The publication of the first textbook in the field of pediatric infectious diseases in 1958 further validated the emerging subspecialty. This was Infectious Diseases of Children by Saul Krugman and Robert Ward. The eleventh edition of Krugman and Ward, edited by Anne Gershon, Peter Hotez, and Samuel Katz, was published in 2004. Additional textbooks followed more than a decade and a half later. Hugh Moffitt published Pediatric Infectious Diseases: A Problem Oriented Approach in 1975, with two subsequent editions, the third in 1988. The first edition of Jack Remington and Jerome Klein's Infectious Diseases of the Fetus and Newborn was published in 1976, with its fifth edition in 2001. The Textbook of Pediatric Infectious Diseases edited by Ralph Feigin and James Cherry appeared in 1981 and has become an encyclopedic two-volume work, the fifth edition being published in 2004. Current Therapy in Pediatric Infectious Diseases was published by John Nelson in 1986, with the third edition edited by Sheldon Kaplan in 1993. Hal Jenson and Robert Baltimore's Pediatric Infectious Diseases debuted in 1995, with a second edition published in 2002. Sarah Long, Larry Pickering, and Charles Prober published The Principles and Practice of Pediatric Infectious Diseases in 1997, with a second edition in 2003.
THE FUTURE OF PEDIATRIC INFECTIOUS DISEASES
The discipline of pediatric infectious diseases has a great many remaining challenges. These include the conquest of illnesses that affect children in the developing world, most notably HIV infection, tuberculosis and falciparum malaria, but also a wide array of other infections. Opportunistic infectious diseases that affect immunocompromised children will also continue to demand attention, and this host population will likely increase.
Medicine has entered the genomic era, and the quantity of genomic data available, both microbial and mammalian, is increasing at a phenomenal pace. This has had, and will continue to have, profound implications for the study and practice of pediatric infectious diseases. Since the elucidation of the H. influenzae genome with 1.8 million base pairs in 1995 (38), almost 100 bacterial genomes have become available, including that of Group A streptococcus (40) and other important human pathogens. The Group A streptococcal genome work was led by Joseph Ferretti, who trained at the University of Minnesota with Elia Ayoub and Lewis Wannamaker. Additionally, the Human Genome Project published drafts of the DNA sequence of Homo sapiens in 2001 (41, 42). These developments unlock the potential for significant advances with impact on all aspects of the field of pediatric infectious diseases. Pathogenesis of infections, new insights into the host-parasite relationship, mechanisms of host susceptibility and resistance, resistance to current and development of new anti-infective therapies, new vaccines, and the identification of new drug targets are some of the areas that will be impacted directly.
Utilization of DNA microarray analysis as well as new methodologies of proteonomics will facilitate new insights into the characterization of gene expression during health as well as in disease states, with identification of new antimicrobial targets and identification of infectious disease risk factors for individuals.
Additionally, the field of pediatric infectious diseases will be impacted for the foreseeable future by issues related to the threat of bioterrorism and the public health response to this threat. This includes the renewal of smallpox immunization in the U.S. as well as focus upon prevention and treatment of anthrax and other potential bioterrorism threats. The unexpected appearance of new infectious diseases (e.g. severe acute respiratory syndrome - SARS) highlights the potential for previously unknown agents to emerge as major threats, and the discipline must learn whether they can cause congenital infection, transfusion-associated infection, and if they particularly target vulnerable populations such as children.
Pediatric infectious disease physicians can rightfully celebrate the past triumphs of their discipline and should anticipate future outstanding achievements, all of which contribute directly and indirectly to improved health for children.
Post-Script.
This history of the development of the field of Pediatric Infectious Diseases in the United States has been written so that it does not overlap the contribution of Baker and Katz entitled “Childhood Vaccine Development in the United States”(43). Therefore, it includes little if any information related to the highly successful development and implementation of vaccines for children that have been so instrumental in improving the health of children. Rather, this history is focused upon infectious diseases of children per se and upon the development of the subspecialty.
Acknowledgements
The author wishes to acknowledge the American Pediatric Society and its Council for stimulating and supporting the activities of the workgroup on History, chaired by Drs. Laurence Finberg and E. Richard Stiehm, which resulted in this manuscript. The author also acknowledges the significant editorial contributions of his mentor Dr. Elia M. Ayoub and of Dr. Jerome O. Klein, Dr. James D. Cherry and Dr. Ben Z. Katz, as well as the reviewers for the journal.
Footnotes
This is the eighth article in our series on the history of pediatric specialties. Dr. Shulman describes the history of infectious diseases over the centuries. Many of these major killers of children were conquered by research that led to understanding the causes of these diseases and eventually to establishing means of prevention and treatment. Dr. Shulman also describes the organizations and publications that have furthered the development of treatment, research and education in this specialty. The future of this field includes the challenges of understanding and treating infectious diseases in immunocompromised children and in developing countries where infectious disease is still a major killer.
References
- 1.Still GF 1931 The History of Paediatrics. Oxford University Press, London
- 2.Colón AR, Colón PA 1999 Nurturing Children, a History of Pediatrics. Greenwood Press, Westport
- 3.Abt AF 1965 Abt-Garrison History of Pediatrics. WB Saunders, Philadelphia
- 4.Harris W 1689 De Morbis Acutis Infantum. Samuel Smith, London
- 5.Cone TE Jr 1979 History of American Pediatrics. Little Brown, Boston
- 6.Thacher T 1677 A brief Rule to Guide the Common-People of New England How to Order Themselves and Theirs in the Small Pocks or Measles. Boston, John Foster
- 7.Faber HK, McIntosh R 1966 History of the American Pediatric Society, 1887–1965. McGraw-Hill, New York
- 8.Bard S 1771 Enquiry into the Nature, Cause and Cure of the Angina Suffocativa or Sore Throat Distemper. S Inslee, New York
- 9.Chalmers L 1776 An Account of the Weather and Diseases of South Carolina. E and S Dilly, London
- 10.Rush B 1777 An Inquiry into the Cause and Cure of Cholera Infantum. Prichard and Hall, Philadelphia
- 11.Pearson HA. Oski's Pediatrics, 3rd Ed. 1999. History of pediatrics in the United States; pp. 2–7. [Google Scholar]
- 12.Fenn E 1999 Pox Americana: The Great Smallpox Epidemic of 1775–1782. Hill and Wang, New York [PubMed]
- 13.Creighton C 1891–1894 A History of Epidemics in Britain, Vol. 2. Cambridge University Press, Cambridge
- 14.Rosen G. The History and Conquest of Common Diseases. 1954. Acute communicable diseases. [Google Scholar]
- 15.Dewees WP 1825 A Treatise on the Physical and Medical Treatment of Children. Carey and Lea, Philadelphia
- 16.Gerhard WW. On the pneumonia of children. Am J Med Sci. 1834;14:328–346. doi: 10.1097/00000441-183408000-00003. [DOI] [Google Scholar]
- 17.Shulman ST. Parrot's pseudoparalysis. Am J Dis Child. 1970;120:243–244. doi: 10.1001/archpedi.1970.02100100144022. [DOI] [PubMed] [Google Scholar]
- 18.Garrison FH 1929 History of Medicine, 4th ed. WB Saunders, Philadelphia
- 19.Sherman DH, Aldrich CA, Bonar BE, Carr WL, McCulloch H (eds) 1938 Semi-Centennial Volume of the American Pediatric Society, 1888–1938. G Banta Publishing Co, Menasha
- 20.McGovern JP, Davison WC. Osler and children. JAMA. 1969;210:2241–2244. doi: 10.1001/jama.1969.03160380055013. [DOI] [PubMed] [Google Scholar]
- 21.Pearson HA 1988 The Centennial History of the American Pediatric Society, 1888–1988. Yale University Printing Service, New Haven
- 22.Denny FW. Infectious diseases and the last 100 years in the American pediatric society. Pediatr Res. 1990;27:S49–S54. doi: 10.1203/00006450-199006001-00013. [DOI] [PubMed] [Google Scholar]
- 23.English PC. Diphtheria and theories of infectious disease: centennial appreciation of the critical role of diphtheria in the history of medicine. Pediatrics. 1985;76:1–9. [PubMed] [Google Scholar]
- 24.Northrup WP, O'Dwyer J, Holt LE, Adams SS. The American pediatric society's report of the collective investigation of the antitoxin treatment of laryngeal diphtheria in private practice. Trans Am Pediatr Soc. 1897;9:32–38. [Google Scholar]
- 25.Harvey AM. The first full-time academic department of pediatrics: the story of the Harriet Lane Home. Johns Hopkins Med J. 1975;137:21–47. [PubMed] [Google Scholar]
- 26.Jacobi A 1905 The history of cerebro-spinal meningitis in America. Trans Med Soc State NY pp 89–98, discussion 113–116
- 27.Smith JL 1872 A Treatise on the Diseases of Infancy and Childhood, 2nd ed. HC Lea, Philadelphia
- 28.Baker SJ 1939 Fighting for Life. Macmillan, New York
- 29.Meckel R 1990 Save the Babies: American Public Health Reform and the Prevention of Infant Mortality, 1850–1929. Johns Hopkins University Press, Baltimore
- 30.Holt LE 1897 The Diseases of Infancy and Childhood. Appleton, New York
- 31.Starr L (ed) 1894 An American Text-Book of the Diseases of Children by American Teachers. FJ Rebman, London
- 32.Nichols BL, Ballabriga A, Kretchmer N (eds) 1991 History of Pediatrics 1850–1950. Raven Press, New York
- 33.Holt LE. A retrospect and a forecast. Trans Am Pediatr Soc. 1923;35:9. [Google Scholar]
- 34.Forbes GB, Forbes GM. A historical note on chemotherapy of bacterial infections. Am J Dis Child. 1970;119:6–11. doi: 10.1001/archpedi.1970.02100050008003. [DOI] [PubMed] [Google Scholar]
- 35.Carithers H. The first use of an antibiotic in America. Am J Dis Child. 1974;128:207–211. doi: 10.1001/archpedi.1974.02110270081016. [DOI] [PubMed] [Google Scholar]
- 36.Report of Special Committee on Prophylactic Procedures Against Communicable Diseases. 1935 J Pediatr6: 586–591
- 37.Pearson HA. History of pediatric hematology oncology. Pediatr Res. 2002;52:979–992. doi: 10.1203/00006450-200212000-00026. [DOI] [PubMed] [Google Scholar]
- 38.Fleischmann RD, Adams MD, White O, Clayton RA, Kirkness EF, Kerlavage AR, Bult CJ, Tomb JF, Dougherty BA, Merrick JM. Whole-genome random sequencing and assembly of Haemophilus influenzae Rd. Science. 1995;269:496–512. doi: 10.1126/science.7542800. [DOI] [PubMed] [Google Scholar]
- 39.Butzin DW, Guerin RO, Long SS. The first certifying examination in pediatric infectious diseases. Pediatr Infect Dis J. 1998;17:161–163. doi: 10.1097/00006454-199802000-00018. [DOI] [PubMed] [Google Scholar]
- 40.Ferretti JJ, McShan WM, Ajdic D, Savic DJ, Savie G, Lyon K, Primeaux C, Sezate S, Suvorov AN, Kenton S, Lai HS, Lin SP, Qian Y, Jia HG, Najar FZ, Ren Q, Zhu H, Song L, White J, Yuan X, Clifton SW, Roe BA, McLaughlin R. Complete genome sequence of an M1 strain of Streptococcus pyogenes. Proc Natl Acad Sci USA. 2001;98:4658–4663. doi: 10.1073/pnas.071559398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Venter JC, Adams MD, Myers EW, Li PW, Mural RJ, Sutton GG, Smith HO, Yandell M, Evans CA, Holt RA. The sequence of the human genome. Science. 2001;291:1304–1351. doi: 10.1126/science.1058040. [DOI] [PubMed] [Google Scholar]
- 42.International Human Genome Sequencing Consortium 2001 Initial sequencing and analysis of the human genome. Nature409: 860–921 [DOI] [PubMed]
- 43.Baker P, Katz S 2004 Childhood vaccine development in the United States. Pediatr Res ( in press) [DOI] [PubMed]


