Abstract
Hypercytokinaemia is thought to contribute to highly pathogenic H5N1 influenza A virus disease. Glycyrrhizin is known to exert immunomodulatory and anti-inflammatory effects and therefore a candidate drug for the control of H5N1-induced pro-inflammatory gene expression. Here, the effects of an approved parenteral glycyrrhizin preparation were investigated on H5N1 virus replication, H5N1-induced pro-inflammatory responses, and H5N1-induced apoptosis in human monocyte-derived macrophages. Glycyrrhizin 100 μg/ml, a therapeutically achievable concentration, impaired H5N1-induced production of CXCL10, interleukin 6, and CCL5 and inhibited H5N1-induced apoptosis but did not interfere with H5N1 replication. Global inhibition of immune responses may result in the loss of control of virus replication by cytotoxic immune cells including natural killer cells and cytotoxic CD8+ T-lymphocytes. Notably, glycyrrhizin concentrations that inhibited H5N1-induced pro-inflammatory gene expression did not affect cytolytic activity of natural killer cells. Since H5N1-induced hypercytokinaemia is considered to play an important role within H5N1 pathogenesis, glycyrrhizin may complement the arsenal of potential drugs for the treatment of H5N1 disease.
Keywords: Glycyrrhizin, H5N1, Cytokines, Monocyte-derived macrophages
Introduction
Highly pathogenic H5N1 influenza A viruses are considered to be potential influenza pandemic progenitors [1–6]. As of March 4th 2010, 486 laboratory-confirmed cases of H5N1 infection have been reported in humans, resulting in 287 deaths, i.e. a mortality rate of 59% (http://www.who.int). The global mortality rate of the highly pathogenic pandemic 1918 H1N1 strain that caused the Spanish flu, the most severe modern influenza pandemic, was 2.5% [7]. At least for the first wave of an H5N1 pandemic, no sufficient amounts of adequate vaccines will be available [1–4, 6, 8, 9]. Therefore, antiviral therapy for influenza A viruses including highly pathogenic H5N1 virus strains remains of great importance for the first line defence against the virus [1–4, 6, 10].
The neuraminidase inhibitors oseltamivir and zanamivir as well as the adamantanes, amantadin and rimantadin, that interfere with the influenza M2 protein are licensed for the treatment of influenza [1–4, 6]. However, the use of both drug classes is limited by the emergence of resistant virus strains. In seasonal influenza strains, the majority of H3N2 viruses and a great proportion of H1N1 viruses in humans are now considered to be amantadine- and rimantadine-resistant [11–14]. Moreover, a drastic increase in oseltamivir-resistant H1N1 viruses has been reported during the 2007/2008 influenza season in the northern hemisphere [15–18]. Preliminary data from the United States predict a further rise for the 2008/2009 season, possibly resulting in more than 90% of the circulating H1N1 strains to be oseltamivir resistant [15].
H5N1 virus strains appear to be generally less sensitive to antiviral treatment than seasonal influenza A virus strains and treatment-resistant H5N1 strains emerge [1–4, 6, 19–22]. Moreover, parenteral agents for the treatment of seriously ill patients are missing. Glycyrrhizin, a triterpene saponine, is a constituent of licorice root. It has been found to interfere with replication and/or cytopathogenic effect (CPE) induction of many viruses including respiratory viruses, such as respiratory syncytial virus, SARS coronavirus, and influenza viruses [23–28]. Moreover, anti-inflammatory and immunomodulatory properties were attributed to glycyrrhizin [26]. The severity of human H5N1 disease has been associated with hypercytokinaemia (“cytokine storm”) [29, 30]. Delayed antiviral plus immunomodulator treatment reduced H5N1-induced mortality in mice [31]. Therefore, anti-inflammatory and immunomodulatory effects exerted by glycyrrhizin may be beneficial for treatment of H5N1.
Effects of H5N1 on macrophages are thought to contribute to H5N1 pathogenicity [5]. Alveolar macrophages have been described as H5N1 target cells in humans and in animal models [32–36]. Infection of macrophages with H5N1 results in a higher expression of pro-inflammatory cytokines than with seasonal influenza or pandemic H1N1/09 strains and this increased cytokine expression has been implicated to contribute to the unusual severity of H5N1 disease [37–39]. Therefore, we investigated the influence of the approved parenteral glycyrrhizin formulation stronger neo-minophagen C (SNMC) on H5N1 replication and H5N1-induced cytokine expression in human monocyte-derived macrophages (MDM).
Materials and methods
Drugs
Glycyrrhizin (Stronger Neo-Minophagen C) was obtained from Minophagen Pharmaceuticals Co., Ltd. (Tokyo, Japan).
Virus strains
The influenza strain A/Vietnam/1203/04 (H5N1) was received from the WHO Influenza Centre (National Institute for Medical Research, London, UK). The H5N1 influenza strain A/Thailand/1(Kan-1)/04 was obtained from Prof. Pilaipan Puthavathana (Mahidol University, Bangkok, Thailand).
Virus stocks were prepared by infecting Vero cells (African green monkey kidney; ATCC, Manassas, VA) and aliquots were stored at −80°C. Virus titres were determined as 50% tissue culture infectious dose (TCID50/ml) in confluent Vero cells in 96-well microtiter plates.
Cells
Human monocytes were isolated from buffy coats of healthy donors, obtained from Institute of Transfusion Medicine and Immune Haematology, German Red Cross Blood Donor Center, Johann Wolfgang Goethe-University, Frankfurt am Main. After centrifugation on Ficoll (Biocoll)–Hypaque density gradient (Biochrom AG, Berlin, Germany), mononuclear cells were collected from the interface and washed with PBS. Then, monocytes were isolated using magnetically labelled CD14 MicroBeads (Miltenyi Biotec GmbH, Bergisch-Gladbach, Germany) following the manufacturer’s instructions. Monocytes were cultivated in IMDM supplemented with 10% pooled human serum, 100 IU/ml of penicillin, and 100 μg/ml streptomycin.
CD14+ monocytes were differentiated into monocyte-derived macrophages under stimulation with granulocyte/macrophage colony stimulating factor (GM-CSF, 500 U/ml) within 14 days. The identity of mature MDMs was confirmed by staining for CD14 (high expression in monocytes, low expression in macrophages), CD86 (low expression in monocytes, high expression in macrophages), CD11c (low expression in monocytes, high expression in macrophages), and HLA-DR (low expression in monocytes, high expression in macrophages) using flow cytometry. All antibodies were purchased from BD Biosciences (Heidelberg, Germany).
To confirm the phagocytotic activity of MDMs, cells were incubated with fluorescent latex beads (FluoSpheres, Invitrogen, Karlsruhe) and cellular fluorescence was examined (not shown).
Human peripheral blood mononuclear cells (PBMC) were isolated from the blood of healthy volunteers by Ficoll–Hypaque centrifugation. Freshly isolated PBMC were incubated for 2 h at 37°C to allow adherence of monocytes to the bottom of the culture flasks. The cell suspension was collected and natural killer (NK) cells were separated according to manufacturer’s protocol using the MACS NK cell isolation kit II (Miltenyi Biotec, Bergisch-Gladbach, Germany). The separated NK cells were treated with 100 U/ml recombinant human interleukin (IL)-2 (Cell Concepts, Umkirch, Germany) for 5 days. Flow cytometric analysis to determine purity of NK cells showed that more than 90% of the cells were CD56+CD3− (data not shown).
Flow cytometry
Antibodies directed against CD14 (Miltenyi Biotec, Bergisch-Gladbach, Germany), CD86, CD11c, and HLA-DR (all three BD Biosciences, Heidelberg, Germany) were used to detect protein expression in monocytes and MDMs by flow cytometry. Phycoerythrin (PE)-conjugated monoclonal antibodies (mAbs) directed against the NK cell surface receptors NKp30, NKp44, NKp46, NKG2D, and DNAM-1 were obtained from Miltenyi Biotec (Bergisch-Gladbach, Germany). PE-conjugated mAbs directed against perforin or granzyme B were purchased from Abcam (Cambridge, UK).
Cell viability assay
The cellular viability was assessed on confluent cell layers with CellTiter-Glo® Luminescent Cell Viability Assay (Promega GmbH, Mannheim, Germany) according to the manufacturers’ protocol. Cell viability was expressed as percentage of non-treated control.
Immune staining
Cells were fixed with 40:60 acetone/methanol for 15 min. For detection of influenza A nucleoprotein, the monoclonal antibody MsX Influenza A (Millipore, Molsheim, France) was used as primary antibody. As secondary antibody an Alexa Fluor 488 goat anti-mouse IgG (H&L) (Invitrogen, Eugene, Oregon, USA) was used (1 h incubation, 1:1,000 in PBS). Nuclei were stained using 4,6-diamidino-2-phenylindole (DAPI) (Sigma-Aldrich Chemie GmbH, Munich, Germany). Fluorescence was visualised using an Olympus IX 1 fluorescence microscope (Olympus, Planegg, Germany).
Cytopathogenic effect reduction assay
The cytopathogenic effect (CPE) reduction assay was performed as described before [40]. Confluent cell monolayers grown in 96-well microtitre plates were infected with influenza A strains in the presence or absence of the investigated agents. The virus-induced CPE was recorded at 24-h post-infection (p.i.) using an inverted light microscope.
Virus yield reduction assay
Infectious virus titres were determined as described before [40]. Briefly, MDMs were infected with influenza A (H5N1) at a multiplicity of infection (MOI, expressed as TCID50/ml) of 2 in MEM supplemented with 2% FBS, 100 IU/ml penicillin, and 100 μg/ml streptomycin. After 24 h, aliquots of the supernatants were taken and serial 10-fold dilution steps were performed. Infectivity was determined by endpoint dilution titration onto Vero cells in 96-well microtitre plates. Plates were incubated for 3–4 days and infectivity was analysed by virus-induced cytopathogenic effect. Virus titres were calculated by the method of Reed and Muench [41]. Virus titres in MDMs infected at MOI 2 were in the range of 104 TCID50/ml being clearly lower than titres detected in lung epithelial A549 cells being about 108 TCID50/ml, although in both cell types >90% of cells were infected 24-h post-infection.
Caspase activation
Caspase activation was measured using the Caspase-Glo 8, 9, or 3/7 assays (Promega, Mannheim, Germany) following the manufacturer’s instructions.
Real-time PCR
Total RNA was isolated from cell cultures using TRI reagent (Sigma-Aldrich, Munich, Germany). Real-time PCR for H5 was performed using described methods [42]. The following primers were used: sense 5′ ACG TAT GAC TAC CCG CAG TAT TCA G 3′; antisense 5′ AGA CCA GCY ACC ATG ATT GC 3′; probe 6-FAM-TCA ACA GTG GCG AGT TCC CTA GCA-TAMRA.
For the investigation of CXCL10 expression, the following primers were used: CXCL10, sense 5′ GAG CCT CAG CAG AGG AAC C, antisense 5′ GAG TCA GAA AGA TAA GGC AGC [43]. For the investigation of IL6 (Hs00174131_m1) and CCL5 (Hs00172575_m1) TaqMan Gene Expression Assays (Applied Biosystems, Darmstadt, Germany) were used.
Cytokine/Chemokine secretion
Cell culture supernatants were collected and frozen at −80°C. Cytokines/Chemokines were quantified by specific ELISA Duo Sets (R&D Systems GmbH, Wiesbaden, Germany) following the manufacturer’s instructions.
NK cell cytolytic activity
Cytotoxicity of NK cells was determined by a 4 h coupled luminescent method using the “aCella-Tox” kit (Cell Technology, Mountain View, CA, USA), as described [44]. K562 cells were used as target cells.
Measurement of interferon-γ (IFN-γ) production
As much as 2 × 104 K562 cells were cocultured with 2 × 105 NK cells for 24 h. NK cells alone or K562 cells were used as control. Supernatants were collected and tested for production of IFN-γ. The amounts of IFN-γ were determined using the Quantikine Human IFN-γ ELISA kit (R&D Systems, Wiesbaden, Germany) according to manufacturer’s protocol.
Results
Influence of glycyrrhizin on H5N1 replication in human monocyte-derived macrophages (MDM)
Glycyrrhizin concentrations up to 200 μg/ml did not affect macrophage viability (data not shown). Moreover, glycyrrhizin concentrations up to 200 μg/ml did neither reduce the number of H5N1-infected macrophages as indicated by nucleoprotein staining nor H5N1 titres (Fig. 1).
Fig. 1.
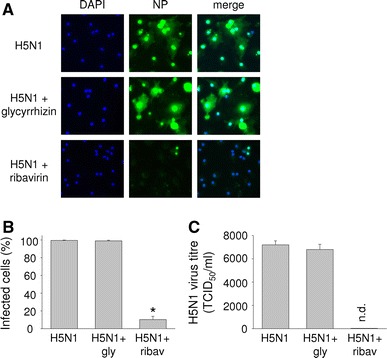
Influence of glycyrrhizin on H5N1-replication in human monocyte-derived macrophages (MDMs). a Representative pictures showing staining of nucleuses by DAPI (blue), H5N1 nucleoprotein (NP) (green), or merge of both stainings in H5N1 (MOI 2)-infected MDMs without treatment, with glycyrrhizin 200 μg/ml, or with ribavirin 40 μg/ml 24-h post-infection. Mock-infected cells did not show NP staining (not shown). b Fraction of H5N1 nucleoprotein-expressing cells in H5N1 (MOI 2)-infected MDMs without treatment, with glycyrrhizin (gly) 200 μg/ml, or with ribavirin (ribav) 40 μg/ml 24-h post-infection. No H5N1 nucleoprotein staining was detected in Mock-infected cells. *P < 0.05 relative to virus control. c Virus titres in H5N1 (MOI 2)-infected MDMs without treatment, with glycyrrhizin (gly) 200 μg/ml, or with ribavirin (ribav) 40 μg/ml 24-h post-infection. No virus titre was detected in mock-infected cells
Influence of glycyrrhizin on H5N1-induced apoptosis in human monocyte-derived macrophages (MDM)
Glycyrrhizin 100 μg/ml inhibited H5N1 A/Thailand/1(Kan-1)/04 (MOI 2)-induced caspase activation 24-h post-infection (Fig. 2). In non-infected cells, caspase activation was not affected by the investigated glycyrrhizin concentrations (not shown).
Fig. 2.
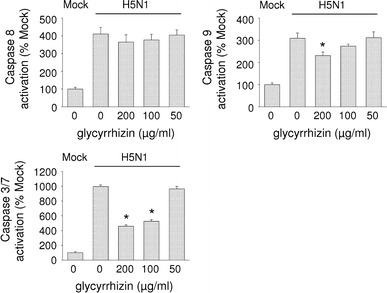
Influence of glycyrrhizin on H5N1-induced caspase activation in monocyte-derived macrophages (MDMs). Caspase activation was measured in non-infected (MOCK) or H5N1 A/Thailand/1(Kan-1)/04 (MOI 2)-infected glycyrrhizin-treated or non-treated MDMs 24-h post-infection. Glycyrrhizin treatment did not affect caspase activation in mock cells (not shown). *P < 0.05 relative to non-treated virus control
Influence of glycyrrhizin on H5N1-induced cytokine production in human monocyte-derived macrophages (MDM)
Glycyrrhizin 100 μg/ml interfered with H5N1 A/Thailand/1(Kan-1)/04 (MOI 2)-induced expression of the cytokines CXCL10, IL6, and CCL5 as determined 24-h post-infection by ELISA (Fig. 3a–c) and quantitative PCR (Fig. 3d). Glycyrrhizin did not influence cytokine expression in non-infected cells (not shown).
Fig. 3.
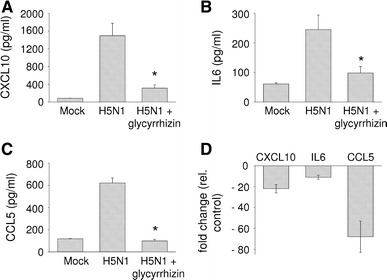
Influence of glycyrrhizin on H5N1-induced cytokine expression in monocyte-derived macrophages (MDMs). a–c Excretion of cytokines by non-infected MDMs (Mock) or H5N1 A/Thailand/1(Kan-1)/04 (MOI 2)-infected MDMs with or without glycyrrhizin (100 μg/ml) treatment 24-h post-infection determined by ELISA. Glycyrrhizin treatment did not affect cytokine excretion in mock cells (not shown). d Relative expression of cytokines at the mRNA level detected via real-time PCR. Glycyrrhizin treatment did not affect cytokine expression in mock cells (not shown). *P < 0.05 relative to non-treated virus control
Influence of glycyrrhizin on natural killer (NK) cell activity
While control of influenza A virus-induced hypercytokinaemia may be beneficial for disease outcome inhibition of the activity of cytotoxic cells that control virus replication like NK cells may be harmful. Therefore, we investigated the influence of glycyrrhizin on NK cell activity (Fig. 4). Glycyrrhizin concentrations up to 200 μg/ml did not influence NK cell viability (data not shown). In contrast to the antiviral drug ribavirin that had been shown before to inhibit NK cell activity [45], glycyrrhizin did not affect NK cell cytolytic activity (Fig. 4). In concordance, glycyrrhizin did neither interfere with the NK cell surface expression of the activating receptors NKG2D, NKp30, NKp44, NKp46, or DNAM-1 nor with the NK cell expression of IFN-γ, perforin, or granzyme B (data not shown).
Fig. 4.
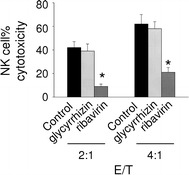
Influence of glycyrrhizin on natural killer (NK) cell cytolytic activity. A 4 h cytotoxicity assay against 5,000 K562 target cells was performed at indicated effector cell/target cell (E/T) ratios using glycyrrhizin (100 μg/ml)-, ribavirin (20 μg/ml)-treated, or non-treated (control) IL-2-activated NK cells. *P < 0.05 relative to non-treated virus control
Discussion
Here, we investigated the influence of glycyrrhizin on the replication of highly pathogenic H5N1 influenza A virus, on H5N1-induced apoptosis, and on H5N1-induced expression of pro-inflammatory cytokines in human MDMs as well as on NK cell activity. Notably, H5N1-induced cytokine expression was reduced by the investigated glycyrrhizin concentration of 100 μg/ml although H5N1 replication was not affected. Glycyrrhizin 100 μg/ml significantly inhibited expression of CXCL10, IL6, and CCL5 at the mRNA as well as at the protein level. Increased CXCL10 and IL6 levels were found in H5N1 patients and correlated with poor outcome [30]. Moreover, H5N1 induced significantly higher CCL5 levels in MDMs than seasonal H1N1 influenza strains [46]. Glycyrrhizin 100 μg/ml also significantly reduced H5N1-induced caspase activation.
After intravenous administration, achievable plasma concentrations of glycyrrhizin have been described to be about 100 μg/ml [47]. Therefore, the glycyrrhizin concentration found to be effective in reducing H5N1-induced pro-inflammatory gene expression in the present report is in the range of therapeutic plasma levels.
Experimental results had previously suggested that glycyrrhizin might be able to affect seasonal influenza A virus disease by antiviral and immunomodulatory effects [26, 27]. Mice were prevented from lethal H2N2 infection by glycyrrhizin although no influence on virus replication was detected. The mechanism was suggested to be induction of interferon-γ in T cells by glycyrrhizin [48]. In a recent report, glycyrrhizin reduced H3N2 titres in lung-derived cells [28]. The observed antiviral activity of glycyrrhizin was assumed to be mediated by an interaction with the cell membrane possibly resulting in reduced endocytotic activity and virus uptake. However, the investigated concentrations being ≥600 μg/ml were clearly above the range of therapeutic plasma levels and concentrations used by us. Therefore, it is hard to compare these results with those presented here. Also, the antiviral activity of glycyrrhizin may differ between seasonal or highly pathogenic H5N1 influenza A viruses. In addition, glycyrrhizin-mediated influences may vary between different cell types and our study reports for the first time on effects of glycyrrhizin on influenza viruses in macrophages.
During seasonal influenza epidemics, immunocompromised (very young or elderly) persons are mostly affected. In contrast, high death rates in healthy and completely immunocompetent individuals were reported to be characteristic for disease caused by the highly pathogenic pandemic 1918 H1N1 strain or by the recently isolated H5N1 strains [7]. These findings suggest that immune-mediated processes may contribute to highly pathogenic influenza A virus-caused pathology. Since H5N1-induced pro-inflammatory gene expression in macrophages is thought to contribute to H5N1 pathogenicity [5], anti-inflammatory effects of glycyrrhizin in H5N1-infected macrophages may be relevant for the H5N1 disease course. Although suppression of cytokine expression alone appears not to be sufficient to improve disease outcome [49–51], control of excessive inflammation was shown to exert beneficial effects in combination with antiviral treatment that reduces virus load. Significant improvements in survival rate, survival time, and inflammatory markers were reported for mice treated with a triple therapy containing zanamivir and immunomodulators including celecoxib, and mesalazine in comparison to zanamivir alone although zanamivir with or without immunomodulators reduced viral loads to a similar extent [31]. In this context, glycyrrhizin represents a potential additional treatment option that interferes with H5N1-induced expression of pro-inflammatory cytokines in macrophages.
Nevertheless, interference with H5N1-induced proinflammatory responses remains a double-edged sword [6]. On the one hand control of hypercytokinaemia at the right time point may improve disease outcome. On the other hand global inhibition of immune responses may also result in the loss of control of virus replication by cytotoxic immune cells including NK cells and cytotoxic CD8+ T-lymphocytes. In concordance, global immunosuppressants like corticosteroids failed to protect from lethal influenza virus infection [49]. The peroxisome proliferator-activated receptor γ agonist suppressed influenza A virus-induced expression of pro-inflammatory chemokines without affecting CD8+ cell cytotoxic activity and protected mice from lethal infection [52]. Also, antiviral drugs may interfere with cytotoxic cells that control virus replication as demonstrated for ribavirin that was shown to hamper NK cell cytolytic activity [45]. Therefore, the ability of glycyrrhizin to interfere with H5N1-induced hypercytokinaemia in concentrations that do not affect NK cell activity may further favour its use as complementary additional anti-influenza treatment option.
In conclusion, we show here that therapeutic concentrations of a clinically approved parenteral preparation of glycyrrhizin interfere with highly pathogenic H5N1 influenza A virus-induced pro-inflammatory gene expression in human MDMs without affecting NK cell activity that is known to be involved in the control of influenza A virus replication. Vaccines and antiviral agents will fail to meet global needs in the case of a severe influenza A virus pandemic [53]. Anti-inflammatory and immunomodulatory agents are important candidates as constituents of anti-influenza treatment strategies that may save lives in an influenza pandemic situation [53]. Therefore, glycyrrhizin may complement the arsenal of potential drugs for the treatment of H5N1-caused disease.
Acknowledgments
The work was supported by the EU grants SARS/FLU vaccine (proposal no. 512054), Chimeric Vaccines (proposal no. 512864), and Intranasal H5 vaccine (proposal no. 044512), by the Hilfe für krebskranke Kinder Frankfurt e.V. and by the Frankfurter Stiftung für krebskranke Kinder.
References
- 1.Cinatl J, Jr, Michaelis M, Doerr HW. The threat of avian influenza A (H5N1). Part I: epidemiologic concerns and virulence determinants. Med Microbiol Immunol. 2007;196:181–190. doi: 10.1007/s00430-007-0042-5. [DOI] [PubMed] [Google Scholar]
- 2.Cinatl J, Jr, Michaelis M, Doerr HW. The threat of avian influenza a (H5N1): part II: clues to pathogenicity and pathology. Med Microbiol Immunol. 2007;196:191–201. doi: 10.1007/s00430-007-0045-2. [DOI] [PubMed] [Google Scholar]
- 3.Cinatl J, Jr, Michaelis M, Doerr HW. The threat of avian influenza A (H5N1). Part III: antiviral therapy. Med Microbiol Immunol. 2007;196:203–212. doi: 10.1007/s00430-007-0048-z. [DOI] [PubMed] [Google Scholar]
- 4.Cinatl J, Jr, Michaelis M, Doerr HW. The threat of avian influenza A (H5N1). Part IV: development of vaccines. Med Microbiol Immunol. 2007;196:213–225. doi: 10.1007/s00430-007-0052-3. [DOI] [PubMed] [Google Scholar]
- 5.Maines TR, Szretter KJ, Perrone L, Belser JA, Bright RA, Zeng H, Tumpey TM, Katz JM. Pathogenesis of emerging avian influenza viruses in mammals and the host innate immune response. Immunol Rev. 2008;225:68–84. doi: 10.1111/j.1600-065X.2008.00690.x. [DOI] [PubMed] [Google Scholar]
- 6.Michaelis M, Doerr HW, Cinatl J., Jr Of chickens and men: avian influenza in humans. Curr Mol Med. 2009;9:131–151. doi: 10.2174/156652409787581565. [DOI] [PubMed] [Google Scholar]
- 7.Taubenberger JK, Morens DM. 1918 Influenza: the mother of all pandemics. Emerg Infect Dis. 2006;12:15–22. doi: 10.3201/eid1201.050979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hampson AW. Vaccines for pandemic influenza. The history of our current vaccines, their limitations and the requirements to deal with a pandemic threat. Ann Acad Med Singap. 2008;37:510–517. [PubMed] [Google Scholar]
- 9.Kieny MP, Fukuda K. The pandemic influenza vaccine challenge. Vaccine. 2008;26:D3–D4. doi: 10.1016/j.vaccine.2008.07.046. [DOI] [PubMed] [Google Scholar]
- 10.Sugrue RJ, Tan BH, Yeo DS, Sutejo R. Antiviral drugs for the control of pandemic influenza virus. Ann Acad Med Singap. 2008;37:518–524. [PubMed] [Google Scholar]
- 11.Deyde VM, Xu X, Bright RA, Shaw M, Smith CB, Zhang Y, Shu Y, Gubareva LV, Cox NJ, Klimov AI. Surveillance of resistance to adamantanes among influenza A(H3N2) and A(H1N1) viruses isolated worldwide. J Infect Dis. 2007;196:249–257. doi: 10.1086/518936. [DOI] [PubMed] [Google Scholar]
- 12.Saito R, Li D, Suzuki Y, Sato I, Masaki H, Nishimura H, Kawashima T, Shirahige Y, Shimomura C, Asoh N, Degawa S, Ishikawa H, Sato M, Shobugawa Y, Suzuki H. High prevalence of amantadine-resistance influenza a (H3N2) in six prefectures, Japan, in the 2005–2006 season. J Med Virol. 2007;79:1569–1576. doi: 10.1002/jmv.20946. [DOI] [PubMed] [Google Scholar]
- 13.Saito R, Suzuki Y, Li D, Zaraket H, Sato I, Masaki H, Kawashima T, Hibi S, Sano Y, Shobugawa Y, Oguma T, Suzuki H. Increased incidence of adamantane-resistant influenza A(H1N1) and A(H3N2) viruses during the 2006–2007 influenza season in Japan. J Infect Dis. 2008;197:630–632. doi: 10.1086/525055. [DOI] [PubMed] [Google Scholar]
- 14.Suzuki Y, Taira K, Saito R, Nidaira M, Okano S, Zaraket H, Suzuki H. Epidemiologic study of influenza infection in Okinawa, Japan, from 2001 to 2007: changing patterns of seasonality and prevalence of amantadine-resistant influenza A virus. J Clin Microbiol. 2009;47:623–629. doi: 10.1128/JCM.01760-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dharan NJ, Gubareva LV, Meyer JJ, Okomo-Adhiambo M, McClinton RC, Marshall SA, St George K, Epperson S, Brammer L, Klimov AI, Bresee JS, Fry AM. Infections with oseltamivir-resistant influenza A(H1N1) virus in the United States. JAMA. 2009;301:1034–1041. doi: 10.1001/jama.2009.294. [DOI] [PubMed] [Google Scholar]
- 16.Hauge SH, Dudman S, Borgen K, Lackenby A, Hungnes O. Oseltamivir-resistant influenza viruses A (H1N1), Norway, 2007–08. Emerg Infect Dis. 2009;15:155–162. doi: 10.3201/eid1502.081031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kramarz P, Monnet D, Nicoll A, Yilmaz C, Ciancio B. Use of oseltamivir in 12 European countries between 2002 and 2007—lack of association with the appearance of oseltamivir-resistant influenza A(H1N1) viruses. Euro Surveill. 2009;14:pii=19112. doi: 10.2807/ese.14.05.19112-en. [DOI] [PubMed] [Google Scholar]
- 18.Moscona A. Global transmission of oseltamivir-resistant influenza. N Engl J Med. 2009;360:953–956. doi: 10.1056/NEJMp0900648. [DOI] [PubMed] [Google Scholar]
- 19.Cheung CL, Rayner JM, Smith GJ, Wang P, Naipospos TS, Zhang J, Yuen KY, Webster RG, Peiris JS, Guan Y, Chen H. Distribution of amantadine-resistant H5N1 avian influenza variants in Asia. J Infect Dis. 2006;193:1626–1629. doi: 10.1086/504723. [DOI] [PubMed] [Google Scholar]
- 20.McKimm-Breschkin JL, Selleck PW, Usman TB, Johnson MA. Reduced sensitivity of influenza A (H5N1) to oseltamivir. Emerg Infect Dis. 2007;13:1354–1357. doi: 10.3201/eid1309.07-0164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.de Jong MD. H5N1 transmission and disease: observations from the frontlines. Pediatr Infect Dis J. 2008;27:S54–S56. doi: 10.1097/INF.0b013e3181684d2d. [DOI] [PubMed] [Google Scholar]
- 22.Nguyen DH, Nguyen HH, Nguyen TV, Nguyen TM, Trinh TM, Nguyen QT, Van Dinh T, Shimbo T, Takahashi Y, Kato Y, Kawana A, Akita S, Kudo K. Human infection with highly pathogenic avian influenza virus (H5N1) in northern Vietnam, 2004–2005. Emerg Infect Dis. 2009;15:19–23. doi: 10.3201/eid1508.090270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cinatl J, Jr, Morgenstern B, Bauer G, Chandra P, Rabenau H, Doerr HW. Glycyrrhizin, an active component of liquorice roots, and replication of SARS-associated coronavirus. Lancet. 2003;361:2045–2046. doi: 10.1016/S0140-6736(03)13615-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cinatl J, Jr, Michaelis M, Hoever G, Preiser W, Doerr HW. Development of antiviral therapy for severe acute respiratory syndrome. Antiviral Res. 2005;66:81–97. doi: 10.1016/j.antiviral.2005.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang XQ, Li HY, Liu XY, Zhang FM, Li X, Piao YA, Xie ZP, Chen ZH, Li X. The anti-respiratory syncytial virus effect of active compound of Glycyrrhiza GD4 in vitro. Zhong Yao Cai. 2006;29:692–694. [PubMed] [Google Scholar]
- 26.Asl MN, Hosseinzadeh H. Review of pharmacological effects of Glycyrrhiza sp. and its bioactive compounds. Phytother Res. 2008;22:709–724. doi: 10.1002/ptr.2362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fiore C, Eisenhut M, Krausse R, Ragazzi E, Pellati D, Armanini D, Bielenberg J. Antiviral effects of Glycyrrhiza species. Phytother Res. 2008;22:141–148. doi: 10.1002/ptr.2295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wolkerstorfer A, Kurz H, Bachhofner N, Szolar OH. Glycyrrhizin inhibits influenza A virus uptake into the cell. Antivir Res. 2009;83:171–178. doi: 10.1016/j.antiviral.2009.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Beigel JH, Farrar J, Han AM, Hayden FG, Hyer R, de Jong MD, Lochindarat S, Nguyen TK, Nguyen TH, Tran TH, Nicoll A, Touch S, Yuen KY. Avian influenza A (H5N1) infection in humans. N Engl J Med. 2005;353:1374–1385. doi: 10.1056/NEJMra052211. [DOI] [PubMed] [Google Scholar]
- 30.de Jong MD, Simmons CP, Thanh TT, Hien VM, Smith GJ, Chau TN, Hoang DM, Chau NV, Khanh TH, Dong VC, Qui PT, Cam BV, Hado Q, Guan Y, Peiris JS, Chinh NT, Hien TT, Farrar J. Fatal outcome of human influenza A (H5N1) is associated with high viral load and hypercytokinemia. Nat Med. 2006;12:1203–1207. doi: 10.1038/nm1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zheng BJ, Chan KW, Lin YP, Zhao GY, Chan C, Zhang HJ, Chen HL, Wong SS, Lau SK, Woo PC, Chan KH, Jin DY, Yuen KY. Delayed antiviral plus immunomodulator treatment still reduces mortality in mice infected by high inoculum of influenza A/H5N1 virus. Proc Natl Acad Sci USA. 2008;105:8091–8096. doi: 10.1073/pnas.0711942105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van Riel D, Munster VJ, de Wit E, Rimmelzwaan GF, Fouchier RA, Osterhaus AD, Kuiken T. H5N1 virus attachment to lower respiratory tract. Science. 2006;312:399. doi: 10.1126/science.1125548. [DOI] [PubMed] [Google Scholar]
- 33.Deng R, Lu M, Korteweg C, Gao Z, McNutt MA, Ye J, Zhang T, Gu J. Distinctly different expression of cytokines and chemokines in the lungs of two H5N1 avian influenza patients. J Pathol. 2008;216:328–336. doi: 10.1002/path.2417. [DOI] [PubMed] [Google Scholar]
- 34.Liem NT, Nakajima N, Le Phat P, Sato Y, Thach HN, Hung PV, San LT, Katano H, Kumasaka T, Oka T, Kawachi S, Matsushita T, Sata T, Kudo K, Suzuki K. H5N1-infected cells in lung with diffuse alveolar damage in exudative phase from a fatal case in Vietnam. Jpn J Infect Dis. 2008;61:157–160. [PubMed] [Google Scholar]
- 35.Chen Y, Deng W, Jia C, Dai X, Zhu H, Kong Q, Huang L, Liu Y, Ma C, Li J, Xiao C, Liu Y, Wei Q, Qin C. Pathological lesions and viral localization of influenza A (H5N1) virus in experimentally infected Chinese rhesus macaques: implications for pathogenesis and viral transmission. Arch Virol. 2009;154:227–233. doi: 10.1007/s00705-008-0277-5. [DOI] [PubMed] [Google Scholar]
- 36.Kwon YK, Lipatov AS, Swayne DE. Bronchointerstitial pneumonia in guinea pigs following inoculation with H5N1 high pathogenicity avian influenza virus. Vet Pathol. 2009;46:138–141. doi: 10.1354/vp.46-1-138. [DOI] [PubMed] [Google Scholar]
- 37.Cheung CY, Poon LL, Lau AS, Luk W, Lau YL, Shortridge KF, Gordon S, Guan Y, Peiris JS. Induction of proinflammatory cytokines in human macrophages by influenza A (H5N1) viruses: a mechanism for the unusual severity of human disease? Lancet. 2002;360:1831–1837. doi: 10.1016/S0140-6736(02)11772-7. [DOI] [PubMed] [Google Scholar]
- 38.Guan Y, Poon LL, Cheung CY, Ellis TM, Lim W, Lipatov AS, Chan KH, Sturm-Ramirez KM, Cheung CL, Leung YH, Yuen KY, Webster RG, Peiris JS. H5N1 influenza: a protean pandemic threat. Proc Natl Acad Sci USA. 2004;101:8156–8161. doi: 10.1073/pnas.0402443101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Woo PC, Tung ET, Chan KH, Lau CC, Lau SK, Yuen KY. Cytokine profiles induced by the novel swine-origin influenza A/H1N1 virus: implications for treatment strategies. J Infect Dis. 2010;201:346–353. doi: 10.1086/649785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Geiler J, Michaelis M, Naczk P, Leutz A, Langer K, Doerr HW, Cinatl J., Jr N-acetyl-L-cysteine (NAC) inhibits virus replication and expression of pro-inflammatory molecules in A549 cells infected with highly pathogenic H5N1 influenza A virus. Biochem Pharmacol. 2010;79:413–420. doi: 10.1016/j.bcp.2009.08.025. [DOI] [PubMed] [Google Scholar]
- 41.Reed LI, Muench H. A simple method of estimating fifty per cent endpoints. Am J Hyg. 1938;27:493–497. [Google Scholar]
- 42.Michaelis M, Geiler J, Klassert D, Doerr HW, Cinatl J., Jr Infection of human retinal pigment epithelial cells with influenza A viruses. Invest Ophthalmol Vis Sci. 2009;50:5419–5425. doi: 10.1167/iovs.09-3752. [DOI] [PubMed] [Google Scholar]
- 43.Osawa Y, Iho S, Takauji R, Takatsuka H, Yamamoto S, Takahashi T, Horiguchi S, Urasaki Y, Matsuki T, Fujieda S. Collaborative action of NF-kappaB and p38 MAPK is involved in CpG DNA-induced IFN-alpha and chemokine production in human plasmacytoid dendritic cells. J Immunol. 2006;177:4841–4852. doi: 10.4049/jimmunol.177.7.4841. [DOI] [PubMed] [Google Scholar]
- 44.Ogbomo H, Hahn A, Geiler J, Michaelis M, Doerr HW, Cinatl J., Jr NK sensitivity of neuroblastoma cells determined by a highly sensitive coupled luminescent method. Biochem Biophys Res Commun. 2006;339:375–379. doi: 10.1016/j.bbrc.2005.11.025. [DOI] [PubMed] [Google Scholar]
- 45.Ogbomo H, Michaelis M, Altenbrandt B, Doerr HW, Cinatl J., Jr A novel immunomodulatory mechanism of ribavirin in suppressing natural killer cell function. Biochem Pharmacol. 2010;79:188–197. doi: 10.1016/j.bcp.2009.07.026. [DOI] [PubMed] [Google Scholar]
- 46.Zhou J, Law HK, Cheung CY, Ng IH, Peiris JS, Lau YL. Differential expression of chemokines and their receptors in adult and neonatal macrophages infected with human or avian influenza viruses. J Infect Dis. 2006;194:61–70. doi: 10.1086/504690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.van Rossum TG, Vulto AG, Hop WC, Schalm SW. Pharmacokinetics of intravenous glycyrrhizin after single and multiple doses in patients with chronic hepatitis C infection. Clin Ther. 1999;21:2080–2090. doi: 10.1016/S0149-2918(00)87239-2. [DOI] [PubMed] [Google Scholar]
- 48.Utsunomiya T, Kobayashi M, Pollard RB, Suzuki F. Glycyrrhizin, an active component of licorice roots, reduces morbidity and mortality of mice infected with lethal doses of influenza virus. Antimicrob Agents Chemother. 1997;41:551–556. doi: 10.1128/aac.41.3.551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Salomon R, Hoffmann E, Webster RG. Inhibition of the cytokine response does not protect against lethal H5N1 influenza infection. Proc Natl Acad Sci USA. 2007;104:12479–12481. doi: 10.1073/pnas.0705289104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Droebner K, Reiling SJ, Planz O. Role of hypercytokinemia in NF-kappaB p50-deficient mice after H5N1 influenza A virus infection. J Virol. 2008;82:11461–11466. doi: 10.1128/JVI.01071-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ehrhardt C, Ludwig S. A new player in a deadly game: influenza viruses and the PI3K/Akt signalling pathway. Cell Microbiol. 2009;11:863–871. doi: 10.1111/j.1462-5822.2009.01309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Aldridge JR, Jr, Moseley CE, Boltz DA, Negovetich NJ, Reynolds C, Franks J, Brown SA, Doherty PC, Webster RG, Thomas PG. TNF/iNOS-producing dendritic cells are the necessary evil of lethal influenza virus infection. Proc Natl Acad Sci USA. 2009;106:5306–5311. doi: 10.1073/pnas.0900655106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fedson DS. Confronting the next influenza pandemic with anti-inflammatory and immunomodulatory agents: why they are needed and how they might work. Influenza Other Respir Viruses. 2009;3:129–142. doi: 10.1111/j.1750-2659.2009.00090.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


