Abstract
Purpose
The aim of this study was to evaluate the combined effect of corticotomy and Low-Level Laser Therapy(LLLT) on the rate of orthodontic tooth movement.
Methods
A randomized split-mouth design for 16 female patients compared the rate of maxillary canine retraction using corticotomy combined with LLLT versus corticotomy only. The device used in the present study was an In-Ga-As semiconductor diode laser emitting at 940 nm (IR) with these parameters: 0.5 W/ cm2 power density, 5 J/cm2 Fluence, CW, 240 sec time irradiation, weekly for the first month and twice monthly for the next three months. Assessment of the rate of canine retraction was carried out via a series of dental models.
Results
A non-significant statistical rate of canine retraction was achieved by LLLT combined to corticotomy compared with the corticotomy technique alone.
Conclusion
Low-Level Laser Therapy combined to corticotomy could not achieve a higher rate of canine retraction compared to the golden standard corticotomy technique alone. No long-term adverse effects on the alveolar mucosa were detected following both techniques.
Keywords: Orthodontics, Rate of retraction, Low-Level Laser Therapy, Corticotomy
1. Introduction
Adult patients seeking orthodontic treatment often desire their treatment to be completed in a short period 1), and in adult patients, osteotomy of cortical bone or corticotomy decreases the treatment time because the resistance of the dense cortical bone to orthodontic tooth movement is reduced 2). In orthodontics, LLLT has been used to relieve pain associated with tooth movement, accelerate bone regeneration during rapid maxillary expansion, as well as faster the orthodontic tooth movement (OTM) 3, 4).
Orthodontic treatment always aims to achieve its esthetic and functional goals with the maximum benefits and the least side effects, and corticotomy, since its beginning in the last century, was considered a cornerstone in accelerating orthodontic tooth movement 5). With the introduction of LLLT in orthodontics, many investigators used it as a simpler, non-invasive alternative technique also to accelerate orthodontic tooth movement 6, 7, and 8). The aim of the present work was to combine the accelerator effect of both corticotomy and laser comparing them with the golden standard corticotomy alone in an attempt for more acceleration of orthodontic tooth movement assessed by the rate of maxillary canine retraction.
Corticotomy is defined as the osteotomy of the cortical bone, in adult patients, this technique reduces the treatment time because the resistance of the dense cortical bone to orthodontic tooth movement is reduced 9, 10). Transient localized demineralization/ remineralization occurs after corticotomy and that the demineralization of the alveolar bone over the root surfaces leaves the collagenous soft tissue matrix of the bone, which can be carried with the root surface and then remineralized following the completion of the orthodontic treatment, this process was called “bone matrix transportation 11).”
LLLT is one of the physical approaches to accelerate orthodontic tooth movement, it was claimed that soft laser is able to accelerate orthodontic tooth movement through its bio-stimulatory effect 4). LLLT and its bio-stimulation effect, occurred when the irradiated tissues showed local temperature increase not more than 1°C, the reason why this technique is termed low-level is that the optimum levels of energy density delivered are low when compared to other forms of laser therapy used for ablation, cutting, and thermally coagulating tissue 12), currently, LLLT, is also known as “cold laser”, “soft laser”, “bio-stimulation” or “photo bio-modulation” 12).
The effect of corticotomy and LLL in acceleration of tooth movement individually has been previously studied; but combing the effects of both corticotomy and laser therapy hasn't been attempted before and could have a synergistic effect on each other, moreover, the usage of LLLT combined with corticotomy may help to make use of the efficiency of laser in improving bone regeneration following corticotomy surgery 6).
The aim of this study was to evaluate the combined effect of corticotomy and LLLT on the rate of orthodontic tooth movement.
2. Methods
This was a split-mouth randomized clinical trial.
The sample of the present study consisted of 16 adult female patients with age ranged from 17 to 25 years representing the adult permanent dentition stage. The sample size was calculated using the G*Power program, University of Düsseldorf, Düsseldorf, Germany 13).
Medical and dental histories, as well as proper clinical examination, were carried out for all patients to confirm the match with the eligibility criteria using the diagnostic charts. Maxillary arch of each patient was divided randomly by a simple randomization technique generated by a computer into the right sides (intervention or comparator). Then, the left sides were automatically assigned to the alternative group. The start of orthodontic treatment and follow-up visits were performed at the orthodontic department clinic, by the principal operator. The latter clinic was equipped to perform minor dental surgical procedures. Group 1 was identified as the intervention group (Surgical corticotomy combined with LLLT), and group 2 was identified as the Comparator group (Surgical corticotomy alone).
2.1. All patients fulfilled the following eligibility criteria:
2.1.1. Inclusion criteria
-
1)
Class I or Class II (Angles' classification) malocclusion cases requiring 1st premolar extraction with moderate anchorage.
-
2)
Treatment mechanics that allowed an initial stage of leveling and alignment before extraction of the first premolars.
-
3)
Normal shape and structure of maxillary canines, with no history of filling or root canal treatment.
-
4)
Patients with a healthy periodontal condition.
2.1.2. Exclusion criteria
-
1)
History of previous orthodontic treatment.
-
2)
History of hormonal disorder or syndrome.
-
3)
History of previous oral surgeries in upper arch.
-
4)
Cleft lip/palate or any other craniofacial anomalies.
-
5)
Drug therapy affecting orthodontic tooth movement, e.g. corticosteroids, hormonal therapy, NSAIDs.
-
6)
Chronic diseases e.g. liver or kidney diseases.
-
7)
Medical conditions that contraindicate surgeries, e.g. bleeding tendency and immune-compromised patients.
After a full explanation of the aim of the study, interventions and possible side effects, the patient's approval and written consent were given to either the patients and/or their guardians. This in-vivo study was carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans. Informed consent was signed by all patients who were enrolled in the study after full explanation of treatment stages and steps. Trial was registered in clinicaltrial.gov.
Random numbers were generated on a Computer using Microsoft Office Excel 2007 sheet by a person who was not involved in the clinical trial (MA). The concealed allocation was performed using a set of random numbers placed in sealed opaque envelopes. Each patient picked up a number that would represent the intervention side (laser+ corticotomy) performed either on the RT side or LT side and thus the opposing number would be the comparator side (corticotomy only). By calling (FS) who was accessible to the random table, the intervention which will be performed either on the LT or the RT side was revealed. At the time of intervention, the subject was allowed to choose one of the envelopes to detect her number in the randomization sequence and thus detect which was the intervention side.
All subjects included in the study received a straight wire appliance on their upper and lower arches excluding the upper first premolars; using Roth prescription 0.022 slot bracket system (Ormco-Mini 2000, USA). The metal brackets were bonded to all the teeth using orthodontic light-cured composite resin (Green gloo two-way color change adhesive, Ormco, USA). Ready-made molar bands with double buccal tubes were selected, fitted and cemented on the first molars using glass ionomer cement (Medicem glass ionomer, Promedica, USA). Trans-palatal arch was fabricated and soldered on maxillary molar bands for anchorage control. The upper archwires sequence used for initial leveling and alignment phase were 0.014 NiTi, 0.016” × 0.022” NiTi till 0.017” × 0.025” stainless steel wire was reached and leveling and alignment stage was completed. On the day of surgery, the upper archwire was removed, an alginate impression (Hydrogum, zhermack, Italy) was made to construct a dental model that would be used together with the follow-up models to measure the rate of canine retraction. Patients were referred to the Oral Surgery Department, for extraction of both maxillary 1st premolars.
Following extractions, buccal and palatal vestibular incision flaps design were planned. Lateral extensions of the flap were designed to extend from the mesial surface of the maxillary canine to the distal surface of the 2nd premolar. Scalpel blade (OdontoMed2011, USA) number 15c was used to make the bucco-labial incision. A full-thickness gingival muco-periosteal flap was elevated via a muco- periosteal elevator, and then the flap reflection was extended when possible beyond the root apex of the canine.
Surgical corticotomy was performed by the same surgeon for all patients. By using a conventional rotary high-speed motor (22000 to 27000 rpm) and a round bur number 2 (Verdent Ltd. Poland), ten to fifteen corticotomy perforations were made under copious saline irrigation, approximately 1–2 mm deep cortication's were made from the distal surface of the second premolar till the mesial surface of the canine surrounding the canine roots on both the buccal and palatal surfaces bilaterally for all the included subjects in the study (Figure 1). In the end, the flap was cautiously relocated and stitched with resorbable (5-0 Vicryl undyed 18” PS-2 cutting) by using the single interrupted method (Figure 2)
Figure 1:
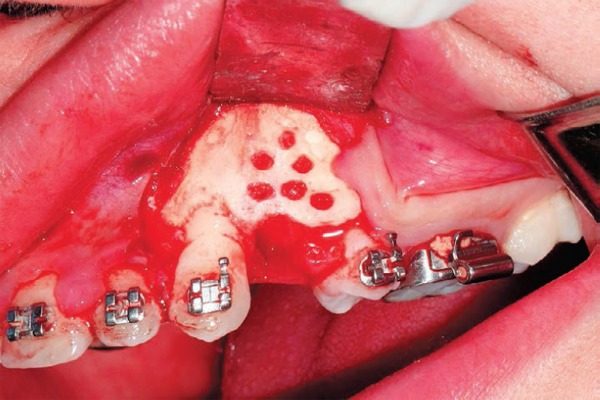
Decortication on the buccal surface.
Figure 2:

Flap cautiously relocated and stitched.
All safety precautions had been followed including eye protection glasses for both the patient and the operator. LLLT was started on the intervention side on the same day of surgery using Biolase (Epic 10 Console, Biolase, and Irvine, USA) Semi-conductor diode laser. After adjusting the device power/watt and intensity specifications according to the manufacturer instructions, the active laser tip was held in a perpendicular direction against the buccal mucosa and palatal mucosa respectively at the mid-root area of the canine. Total laser application time on the intervention side was 240 seconds for each patient divided equally between the buccal and palatal surfaces so that each surface received 120 seconds of irradiation distributed into 40 seconds each.
Laser application was performed by the principal operator throughout the study using the following parameters (Wavelength: 940 ± 10nm, Power density: 0.5 W/cm2, energy density: 5 J/cm2, continuous wave, and time for 240 seconds). The laser was applied according to the following laser time/line:
L1: On the first day of retraction.
L2: after one week.
L3: after two weeks.
L4: after three weeks.
Every 2 weeks until the end of the four months of the study time or full canine retraction.
Canine retraction was started on both sides at the same day of first premolars extraction and immediately after the completion of laser application and corticotomy procedure. The same arch wire (0.017 × 0.025 St St) was re-replaced in the upper arch, then a NiTi closed coil spring (Ormco, USA) was placed between the hook of the canine and the 1st molar band delivering a force of 150 g as measured by the force gauge.
Post-operative instructions were given to the patients as soft diet and strict oral hygiene instructions including regular brushing and the use of 0.02 chlorhexidine mouthwash for 1 week. Ice packs were prescribed during the first 12 hours, followed by hot fomentation for the next 48 hours. To control pain, Paracetamol (500 mg) was given as 1gm every 12 hours for 4 days. Patients were instructed to communicate with the doctor if they experienced too much swelling, bleeding or severe pain. Follow-up visits were scheduled every two weeks. At each follow-up visit, the force magnitude was checked using the same force gauge. Re-calibration of the coil springs were done when necessary to maintain 150 gms force delivery. An alginate impression for the upper arch was made every 4 weeks. The alginate impression was then poured within 15 minutes with dental stone to avoid dimensional instability. Finally, the dental cast was trimmed and labeled with the patient name, number and date.
Laser application was also applied according to the mentioned laser time/line of each patient on either the right or left sides of the upper arch depending on the randomized number picked up by the patient. The study time was continued for 4 months or completion of canine retraction on either side (T1, T2, T3, and T4) (Table 1). After 4 months of follow-up (Figure 3), the final dental model was made. During the study time, the patients received treatment in the opposing arch using the same type of brackets. Extraction or non-extraction conventional treatment in the lower arch was performed according to the treatment plan of each case separately. Any inferences during canine retraction were reported and adjusted during follow-up sessions.
Table 1: Patient timeline.
| Visit | Treatment performed | Model |
|---|---|---|
| First visit | • Clinical examination and full records including study model, photos, panorama and lateral Cephalometry. | yes |
| Lag phase | • Banding and bonding, levelling and alignment for the upper arch. | no |
| T0: Start of canine retraction | • Extraction of the upper 1st premolars. • Perform corticotomy bilaterally, insertion of 0.017″ × 0.025″ stainless steel arch wire. • Application of Low level laser on the intervention sides. • Start of canine retraction. | yes |
| T1: (1 month of canine retraction) | • Activation of canine retraction. | yes |
| T2: (2 months of canine retraction) | • Activation of canine retraction. | yes |
| T3: (3 months of canine retraction) | • Activation of canine retraction. | yes |
| T4: (4 months of canine retraction) | • Activation of canine retraction. | yes |
Figure 3:

Intra-oral side occlusal photograph (16 weeks of canine retraction).
The outcome of the study was to determine the effect of corticotomy combined with low-level laser therapy on the rate of canine retraction when compared to corticotomy alone.
Three-dimensional digital models were obtained by scanning the sequential stone models using a surface laser scanner. The incremental rate of canine retraction was then measured using the 3 shape program.
Total distance moved by the canines was assessed by superimposition of the pre-retraction and post-retraction digital models acquired. For each patient, upper impressions were taken just before canine retraction (T0) and every four weeks for 4 successive visits (T1, T2, T3, T4); therefore for each patient, five upper stone models were obtained (T0, T1, T2, T3, and T4). Each stone model (T0–T4) was then scanned using 3Shape R900 scanner14 (3Shape A/S, Copenhagen, Denmark), to obtain the stl. Format of the digital model. Using the attached 3 shape computer software (3-Shape Analyzer), the sequential digital models of each patient were superimposed and evaluated for canine distalization changes as described by El-Tamimy et al, 2016 14).
The oriented model at (T0) was the basic model on which all the successive models were superimposed. Using 3-point superimposition, model (T1) was superimposed on model (T0) where point localization was done on the two models in parallel. The points were selected on the right and left third rugae, which are stable palatal landmarks. Then model (T1) was superimposed to the model (T0). The procedure was repeated with the rest of follow up models until reaching the model at (T4).
The landmarks and measurements were all recorded in their corresponding modules. A customized analysis was then created and saved to be used for all digital models. (Table 2 and 3) For each of the 5 superimposed successive digital models T0–T4 (obtained for one patient), landmarks were located on the 3D volume of each model then the desired measurements were all automatically generated using the saved analysis to measure the rate of canine retraction and anchorage loss. Landmark identification was done through two blinded assessors (N.A. and A.N) and an average of their measurements were considered for the statistical analysis. The sagittal distance from the canine cusp tip to the frontal plane was used to calculate the distance travelled by the canine in each month (rate of canine retraction) by subtracting the distance from the canine cusp tip to the frontal plane at that marks from that of the previous months till reaching the last model (T4) e.g.: Distance travelled by the right canine in the 1st month = [UR3 CT − FP (T1)] − [UR3 CT − FP (T0)].
Table 2: Landmarks used in the digital model analysis.
| Landmark abbreviation | Landmark definition |
|---|---|
| UR 3 CT (T0) | • The most incisal point on the upper right canine cusp tip in digital model (T0), (T1), (T2), (T3), and (T4). |
| UR 3 CT (T1) | |
| UR 3 CT (T2) | |
| UR 3 CT (T3) | |
| UR 3 CT (T4) | |
| UR 6 CT (T0) | • The most occlusal point on the mesiobuccal cusp tip of the upper right 1st molar in digital model (T0). |
| UR 6 CT (T4) | • Digital model (T4). |
| UL 3 CT (T0) | • The most incisal point on the upper left canine cusp tip in digital model (T0), (T1), (T2), (T3), and (T4). |
| UL 3 CT (T1) | |
| UL 3 CT (T2) | |
| UL 3 CT (T3) | |
| UL 3 CT (T4) | |
| UL 6 CT (T0) | • The most occlusal point on the mesiobuccal cusp tip of the upper left 1st molar in digital model (T0). |
| UL 6 CT (T4) | • Digital model (T4) respectively. |
Table 3: Measurements used in the digital model analysis.
| Measurement abbreviation | Measurement definition |
|---|---|
| UR 3 CT (T0) - FP | The sagittal distance (mm) between the upper right canine cusp tip and the frontal plane (FP) in digital model (T0), digital model (T1), digital model (T2), digital model (T3), digital model (T4) respectively. |
| UR 3 CT (T1) - FP | |
| UR 3 CT (T2) - FP | |
| UR 3 CT (T3) - FP | |
| UR 3 CT (T4) - FP | |
| UR 6 CT (T0) - FP | The sagittal distance (mm) between the mesiobuccal cusp tip of the upper right 1st molar and the frontal plane (FP) in digital model (T0) and digital model (T4) respectively. |
| UR 6 CT (T4) - FP | |
| UL 3 CT (T0) - FP | The sagittal distance (mm) between the upper left canine cusp tip and the frontal plane (FP) in digital model (T0), digital model (T1), digital model (T2), digital model (T3), digital model (T4) respectively. |
| UL 3 CT (T1) - FP | |
| UL 3 CT (T2) - FP | |
| UL 3 CT (T3) - FP | |
| UL 3 CT (T4) - FP | |
| UL 6 CT (T0) - FP | The sagittal distance (mm) between the mesiobuccal cusp tip of the upper left 1st molar and the frontal plane (FP) in digital model (T0) and digital model (T4) respectively. |
| UL 6 CT (T4) - FP | |
3. Results
The present study was conducted on 16 subjects; all females. The mean and standard deviation values for age were 21.5 ± 3.2 years old with a range of 17 to 25 years old. All patients had successfully completed the four months duration of the study except for 3 dropout patients who didn't continue the follow-up visits at the beginning of leveling and alignment phase of the orthodontic treatment that was substituted by another 3 patients who were full filling the same inclusion criteria of the study.
During the course of the study, there were no losses in the pre-intervention or in the final records derived from the dental models. No dropout visits were recorded regarding the monthly impression visits. As for the laser visits, nine patients missed their appointments in the third and fourth months that was recorded by date and was replaced by another consecutive visit.
No post-operative bleeding or infections were encountered in any of the patients. Two patients had an incidence of accidental retraction coil spring slippage which was re-attached within 2 days. All patients reported post-surgical swelling bilaterally following corticotomy that lasted from 4 to 6 days which was treated by following the post-surgical instructions regarding oral hygiene measures, medications (antibiotics and analgesics) and physical therapy (hot and cold packs) protocols.
At 1st month, intervention group showed statistically significantly lower mean rate of canine movement than comparator group. At 2nd as well as 3rd months, there was no statistically significant difference between the two groups. At 4th month, intervention group showed statistically significantly higher mean rate of canine movement than comparator group (Table 4).
Table 4: Mean, standard deviation (SD) values and results of Wilcoxon signed-rank test for the comparison between rates of canine movement in the two groups.
| Time | Intervention | Comparator | P-value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| 1st month | 0.81 | 0.58 | 1.16 | 0.67 | 0.019* |
| 2nd month | 1.04 | 0.61 | 0.82 | 0.36 | 0.064 |
| 3rd month | 1.83 | 1.00 | 2.01 | 1.37 | 0.968 |
| 4th month | 1.43 | 1.18 | 0.83 | 1.03 | 0.033* |
Significant at P ≤ 0.05
Descriptive statistics and results of comparison between total distances are presented in (Table 5). There was no statistically significant difference between total distances in the two groups.
Table 5: Descriptive statistics and results of paired t-test for the comparison between total distances in the two groups.
| Group | Mean | SD | Median | Minimum | Maximum | 95% CI |
P-value | |
|---|---|---|---|---|---|---|---|---|
| Lower bound | Upper bound | |||||||
| Intervention | 5.10 | 1.46 | 5.54 | 2.22 | 7.24 | 4.40 | 5.81 | 0.478 |
| Comparator | 4.85 | 1.55 | 4.84 | 2.82 | 7.42 | 4.11 | 5.60 | |
Significant at P ≤ 0.05
The total distance moved by the canine cusp tip was 5.10 ± 1.46mm/4 months in the intervention group, while in the comparator group was 4.85 ± 1.55 mm/4months. The mean difference of the anchorage loss by the mesio-buccal cusp tip of the upper 1st molar was higher in the comparator group than the intervention group by (0.46 ± 2.81 mm) which was statistically insignificant.
4. Discussion
The current study was a split-mouth randomized clinical trial, where one side was randomly allocated to surgical corticotomy combined with LLLT and the other side surgical corticotomy alone. A key advantage of the splitmouth design was the absence of the inter-subject variability, as the patient acted as her own control, resulting in a decrease in the number of participants required 6, 7, 15). Age for patient recruitment was selected to range from 17 to 25 years old, this range of age was decided to avoid any possible effects of growth changes on the results 6, 7, and 15). Canine retraction rate was assessed by taking the upper impression just before the start of canine retraction and every 4 weeks for 4 months. The incremental rate of canine retraction was then measured using the 3 shape program (3 Shape A/S, Copenhagen, Denmark). In order to prevent selection bias, the concealed allocation of both interventions, corticotomy combined with laser versus corticotomy only, to each side of the maxillary arch was done using sealed envelopes containing the computer- generated random number. Patient allocation was revealed only on the same day of application of interventions 6, 16, 17, 18).
The type of laser used in the present study was an In-Ga-As semiconductor diode laser. Laser parameters were adjusted to deliver a total energy of 5 J/cm2, administered on a weekly basis for the first month of canine retraction, followed by twice monthly for 3 months. Both, the laser energy dosage and the protocol of application were recommended by the manufacturer (Biolase Epic Console 10, Ivrine, USA) in order to attain bio-stimulatory effect and its accompanied acceleration of canine retraction. Reviewing the literature, vast heterogeneity was found in the administered energy dosage of LLLT to accelerate OTM. Although some authors used lower energy density ranging from 0.71, 5 and 8 J/ cm2 e.g. 7, 19) respectively. All previously mentioned authors used multiple point applications which were, on average, 5 on buccal and 5 on palatal sides, each was applied for 10 seconds. In the present work, the energy dosage (5 J/cm2) was delivered through a single application (240 seconds) via an active tip held against the buccal and palatal mucosa at the mid-root area of the canine.
Regarding the frequency of laser application 7, 19) used LLLT at 0, 3, 7 and 14 days, and they repeated the same frequency of application either after 21 days or 30 days respectively. Genc et al, 2013 added two applications to the previous protocol performing 6 applications applied once before the start of anterior teeth retraction as follows: 0, 3, 7, 14, 21 and 28 days 8). Doshi-Mehta & Bhad-Patil, 2012 used 4 applications in the 1st month followed by 2 applications per month until complete canine retraction 6). However, Dominguez et al, 2015 didn't follow that frequency of application and applied LLLT at each follow-up visit until the treatment was completed 20). In the present work, manufacturer recommendation of low-level laser for acceleration of OTM was followed. The justification of the use of the low level laser therapy in accelerating the rate of orthodontic movement was according to the conclusion reached by the systematic review done in 2017 by colson et al 21). They stated that comparing method to accelerate orthodontic tooth movement. The highest-level studies show that LLLT can accelerate orthodontic movements, but other research must be pursued. This review of the literature seems to suggest concentrating future research regarding the relationship between LLLT and orthodontic tooth movement on wavelengths in infrared radiation approximately 780–810 nm, with a fluency of approximately 5 J/cm2. Before drawing conclusions for orthodontic clinics, high quality trials are required to conclude about the long-term effects of LLLT and to give the optimal protocols 21).
Doshi-Mehta & Bhad-Patil, in 2012 conducted a split-mouth randomized clinical trial (RCT) with a sample size of 20 patients (8 females and 12 males, mean age 12–23y), they confirmed that there is increase in the rate of OTM following low level laser therapy (LLLT) 6). Authors concluded that varying the wavelength with a reasonable dose in the target zone leads to obtaining the desired biological effect and achieves a reduction in the orthodontic treatment time 7, 16, and 22). Aboul-Ela et al, 2011 in a splitmouth RCT investigated the effect of the corticotomy procedure on the rate of orthodontic tooth movement. In their study, 13 adult patients requiring extraction of upper first premolars were recruited. It was concluded that canine retraction rate on the control side was 2 times greater after two months from surgery, then reduced to 1.6 times by third month and 1.06 more by the fourth month 15).
A systematic review conducted by Kalemaj et al, 2015, concluded that there was some evidence that LLLT could slightly accelerate orthodontic tooth movement in spite of the fact that these results were not significant and the effect estimated was not clinically relevant. The findings showed that corticotomy procedure increased the rate of orthodontic tooth movement (2.3 times) in the 1st months, the effect of the procedure on the cumulative tooth movement was quite controversial, ranging from non-significant to highly significant. Consequently, the authors concluded that corticotomy could accelerate orthodontic tooth movement, whereas long-term effects were questionable 23). Thus, no firm conclusions could be drawn about the benefits of corticotomy in everyday practice 23). In another systematic review and meta-analysis regarding the effectiveness of minimally invasive surgical procedures in speeding up orthodontic tooth movement in humans. Despite the reported greater OTM with the minimally invasive surgical procedures compared to the conventional method by 0.65 and 1.41 mm for the first and second months respectively, the authors summed up their review by stating that the included studies were graded as having unclear risk of bias, thus the efficacy of these procedures were only supported by limited low-quality evidence 24).
From the author's point of view, the use of laser treatment in combination with corticotomy instead of comparing corticotomy alone with laser alone as an intervention was that corticotomy has already proved itself as a significant technique for accelerating orthodontic tooth movement in literature review 23). On the other hand, laser is still a controversy intervention that will be under- estimated if compared to corticotomy, that's why our active comparator was corticotomy compared to the intervention which is corticotomy combined with laser to validate better the laser efficiency in relation to corticotomy surgical treatment.
In the present study, the start of canine retraction was performed on the same day of first premolar extraction. As for surgical decortications, it was performed at the buccal and palatal cortical plate of bone in the form of cortical perforations using a rotary round bur size 2 similar to Farid et al, 2014 23). Decortications were performed around the root of the maxillary canine and into the edentulous area of the future canine movement similar to Aboul-Ela et al, 2011 15). In the present work, the decortication procedure was done using conventional rotary instrument because several RCTs (Rossini et al., 2016; Shoreibah et al., 2012) and systematic review (Hoogeveen et al., 2014) advocated the effectiveness of the former technique in accelerating orthodontic tooth movement. A recent experimental study done by (Farid et al., 2014) concluded that a faster orthodontic tooth movement (1.6 times faster) was achieved by the rotary decortication when compared to the piezo-surgical cuts.
The force for canine retraction was chosen to be 150g delivered via NiTi coil springs. This force magnitude was advocated by Barlow & Kula, 2008 2), who, in a systematic review, concluded that 200g didn't offer any benefit in the rate of canine retraction compared to 150g. The same magnitude and manner of force application for canine retraction were used by 6, 7, 15). Virtual study models are as reliable as plaster models (gold standard), exhibiting high accuracy, reliability, and reproducibility 17).
In the present study, at the 1st month, the intervention group showed a statistically significantly lower mean rate of canine movement than the comparator group. At 2nd as well as 3rd months, there was no statistically significant difference between the two groups. At 4th month, the intervention group showed a statistically significantly higher mean rate of canine movement than the comparator group as measured on the digital models. In conclusion, the intervention side showed a statistically insignificant higher rate of canine retraction after 4 months of treatment than the comparator side with a mean rate of 1.27 mm/month while the comparator side was 1.20 mm/month with a mean difference between the two groups 0.07 mm/month which was clinically insignificant. This could be explained by; at the first month in both groups there was an increase in the rate of orthodontic tooth movement as a result of the temporary regional acceleratory phenomenon (RAP) effect of corticotomy, where on the cellular and on the molecular level, corticotomy procedure increased osteoclastic and osteoblastic activity creating a state of increased bone turnover that diminished after the first month. The daily canine retraction rate on the control side was 2 times greater after two months from surgery, then reduced to 1.6 times by third and 1.06 more by the fourth month 15). However in this study, the accelerated rate of orthodontic tooth movement was lower in the intervention group than the comparator group at the first month following corticotomy, that deceleration of orthodontic tooth movement on the intervention side could be due to the healing effect of LLLT that might have reduced the osteoclastic activity and expression of RANK and RANKL and consequently reducing the rate of tooth movement 1). At the second and third months, both groups showed an equivalent rate of tooth movement. At the fourth month, the accelerator effect of corticotomy was reduced and only the bio-stimulatory effect of LLLT continued increasing the rate of canine retraction.
This result was opposite to other studies as 6, 16). Sousa et al, 2011 explained the latter deceleration on the laser side by assuming a probable systemic effect of the LLL 16). They suggested that laser would increase phagocytosis of leukocytes present at the irradiated area, which might be transferred to other non-irradiated areas by humoral substances. Reviewing the literature, there was no similar study comparing the LLLT combined with corticotomy versus corticotomy as the golden standard, regarding both rates and a total distance of canine retraction. Our results denote that LLLT combined with corticotomy with the previously mentioned dosage and frequency might have the same stimulatory effect of the corticotomy alone procedure on OTM.
One of the limitations of the current study was the absence of a control conventional orthodontic retraction group within the same study which could have helped to confirm the effectiveness of both interventions in accelerating orthodontic tooth movement. However, this was not applicable while performing the split-mouth study design. A second limitation was that long-term effects on pain, periodontal health, and bone density were not studied. No statistically significant difference was found between both interventions as regards the total distance traveled by the maxillary canine at the end of the 4-month study. Similarly, the rate of canine retraction recorded every 4 weeks follow up period showed a statistically non-significant difference on both intervention sides.
5. Conclusions
Within the limitation of this study, the following can be concluded, Low-Level Laser Therapy combined to corticotomy could not achieve a higher rate of canine retraction compared to the golden standard corticotomy technique alone. In addition, no long-term adverse effects on the alveolar mucosa were detected following both techniques.
6. Conflicts of interest
The authors declare no conflicts of interest. This is a self-funded randomized controlled clinical trial. Ethical approval and clinical trial registry on clinicaltrial.gov (Registry number: NCT03906084)
References
- 1: Atlan Altan B. A., Sokucu O., Ozkut M. M., Inan S. Metrical and histological investigation of the effects of low-level laser therapy on orthodontic tooth movement. Lasers in Medical Science. 2012: 27(1); 131-1401. 10.1007/s10103-010-0853-2. [DOI] [PubMed] [Google Scholar]
- 2: Barlow M., Kula K. Factors influencing efficiency of sliding mechanics to close extraction space: a systematic review. Orthodontics & Craniofacial Research. 2008: 11(2); 65-73. 10.1111/j.1601-6343.2008.00421.x. [DOI] [PubMed] [Google Scholar]
- 3: Fujita S., Yamaguchi M., Utsunomiya T., Yamamoto H., Kasai K. Low-energy laser stimulates tooth movement velocity via expression of RANK and RANKL. Orthodontics & Craniofacial Research. 2008: 11(3); 143-155. 10.1111/j.1601-6343.2008.00423.x. [DOI] [PubMed] [Google Scholar]
- 4: Limpanichkul W., Godfrey K., Srisuk N., Rattanayatikul C. Effects of low-level laser therapy on the rate of orthodontic tooth movement. Orthodontics & Craniofacial Research. 2006: 9(1); 38-43. 10.1111/j.1601-6343.2006.00338.x. [DOI] [PubMed] [Google Scholar]
- 5: Hoogeveen E. J., Jansma J., Ren Y. Surgically facilitated orthodontic treatment: a systematic review. American Journal of Orthodontics and Dentofacial Orthopedics. 2014: 145(4 Suppl); S51-64. 10.1016/j.ajodo.2013.11.019. [DOI] [PubMed] [Google Scholar]
- 6: Doshi-Mehta G., Bhad-Patil W. A. Efficacy of low-intensity laser therapy in reducing treatment time and orthodontic pain: a clinical investigation. American Journal of Orthodontics and Dentofacial Orthopedics. 2012: 141(3); 289-297. 10.1016/j.ajodo.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 7: Cruz D.R., Kohara E.K., Ribeiro M.S., Wetter N.U. Effects of low-intensity laser therapy on the orthodontic movement velocity of human teeth: a preliminary study. Lasers in Surgery and Medicine. 2004: 35(2); 117-120. 10.1002/lsm.20076. [DOI] [PubMed] [Google Scholar]
- 8: Genc G., Kocadereli I., Tasar F., Kilinc K., El S., Sarkarati B. Effect of low-level laser therapy (LLLT) on orthodontic tooth movement. Lasers in Medical Science. 2013: 28(1); 41-47. 10.1007/s10103-012-1059-6. [DOI] [PubMed] [Google Scholar]
- 9: Ziegler P, Ingervall B. A clinical study of maxillary canine retraction with a retraction spring and with sliding mechanics. Am J Orthod Dentofacial Orthop. 1989; 95(42):99-106. [DOI] [PubMed] [Google Scholar]
- 10: Mohammad Tizini, Ghosn Ibrahim. Retraction of the upper maxillary incisors with corticotomy-facilitated orthodontics and mini-implants. The Saudi Journal for Dental Research 2014: 5; 146-151. [Google Scholar]
- 11: Ramachandra Prabhakar M.K., Karthikeyan R., Saravanan K.S., Kannan M.R., Arun Raj. Anterior maxillary intrusion and retraction with corticotomy-facilitated orthodontic treatment and burrstone three Piece intrusive arch. J Clin Diagn Res. 2013; 7(12): 3099-3101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12: Reza F, Katayoun K. Laser in Orthodontics. Principles in contemporary Orthodontics. 1994. p. 129-80. [Google Scholar]
- 13: Kansal A., Kittur N., Kumbhojkar V., Keluskar K. M., Dahiya P. Effects of low-intensity laser therapy on the rate of orthodontic tooth movement: A clinical trial. Dental Research Journal. 2014: 11(4); 481-488. [PMC free article] [PubMed] [Google Scholar]
- 14: El-Timamy A.M., El-Sharaby F.A., Eid F. H., Mostafa Y. A. Three-dimensional imaging for indirect-direct bonding. American Journal of Orthodontics and Dentofacial Orthopedics. 2016: 149(6); 928-931. 10.1016/j.ajodo.2015.12.009. [DOI] [PubMed] [Google Scholar]
- 15: Aboul-Ela S. M. B. E.-D., El-Beialy A. R., El-Sayed K. M. F., Selim E. M. N., El-Mangoury N. H., Mostafa Y. A. Miniscrew implant-supported maxillary canine retraction with and without corticotomy-facilitated orthodontics. American Journal of Orthodontics and Dentofacial Orthopedics. 2011: 139(2); 252-259. 10.1016/j.ajodo.2009.04.028 [DOI] [PubMed] [Google Scholar]
- 16: Sousa M. V. da S., Scanavini M. A., Sannomiya E. K., Velasco L. G., Angelieri F. Influence of low-level laser on the speed of orthodontic movement. Photomedicine and Laser Surgery. 2011: 29(3); 191-196. 10.1089/pho.2009.2652. [DOI] [PubMed] [Google Scholar]
- 17: Rossini G., Parrini S., Castroflorio T., Deregibus A., Debernardi C. L. Diagnostic accuracy and measurement sensitivity of digital models for orthodontic purposes: A systematic review. American Journal of Orthodontics and Dentofacial Orthopedics. 2016: 149(2); 161-170. 10.1016/j.ajodo.2015.06.029 [DOI] [PubMed] [Google Scholar]
- 18: Shoreibah E. A., Ibrahim S. A., Attia M. S., Diab M. M. N. Clinical and radiographic evaluation of bone grafting in corticotomy-facilitated orthodontics in adults. Journal of the International Academy of Periodontology. 2012: 14(4); 105-113. [PubMed] [Google Scholar]
- 19: Youssef M., Ashkar S., Hamade E., Gutknecht N., Lampert F., Mir M. The effect of low-level laser therapy during orthodontic movement: a preliminary study. Lasers in Medical Science. 2008: 23(1); 27- 33. 10.1007/s10103-007-0449-7. [DOI] [PubMed] [Google Scholar]
- 20: Dominguez A., Gomez C., Palma J. C. Effects of low-level laser therapy on orthodontics: rate of tooth movement, pain, and release of RANKL and OPG in GCF. Lasers in Medical Science. 2015: 30(2); 915-923. 10.1007/s10103-013-1508-x. [DOI] [PubMed] [Google Scholar]
- 21: Fromont-Colson C., Marquez-Diaz M., Badran Z. Laser Dent Sci. 2017: 1; 47 https://doi.org/10.1007/s41547-017-0010-3. [Google Scholar]
- 22: Sonesson M., De Geer E., Subraian J., Petren S. Efficacy of low-level laser therapy in accelerating tooth movement, preventing relapse and managing acute pain during orthodontic treatment in humans: a systematic review. BMC Oral Health. 2016: 17(1); 11. 10.1186/s12903-016-0242-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23: Kalemaj Z., Debernard I.C.L., Buti J. Efficacy of surgical and non-surgical interventions on accelerating orthodontic tooth movement: a systematic review. European Journal of Oral Implantology. 2015: 8(1); 9-24. [PubMed] [Google Scholar]
- 24: Alfawal A. M. H., Hajeer M. Y., Ajaj M. A., Hamadah O., Brad B. Effectiveness of minimally invasive surgical procedures in the acceleration of tooth movement: a systematic review and meta-analysis. Progress in Orthodontics. 2016: 17(1); 33. 10.1186/s40510-016-0146-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25: Farid K. A., Mostafa Y. A., Kaddah M. A., El-Sharaby F. A. Corticotomy-facilitated orthodontics using piezosurgery versus rotary instruments: an experimental study. Journal of the International Academy of Periodontology. 2014: 16(4); 103-108. [PubMed] [Google Scholar]


