Abstract
The aim of this retrospective study was to describe the epidemiology and spectrum of infections of admitted pediatric refugees and asylum seekers in a tertiary referral hospital in a high-income country in Europe. We identified recent refugees and asylum seekers < 18 years of age admitted to the University Children’s Hospital in Basel, Switzerland, in 2015. A retrospective analysis was performed using electronic patient records. We identified 105 admissions in 93 patients with a median age of 5.7 (IQR 2.6–14.5) years. Eritrea, Syria, and Afghanistan were the most frequent countries of origin. The median duration of admission was 4 (IQR 2–6) days with infections and elective surgical interventions being the most common reason (54.8 and 16.1%, respectively). Most infections were airway, skin, and gastrointestinal in 46.4, 20.2, and 11.9%, respectively. The prevalence of tropical infections was 11.9%. The main pathogens identified were influenza A virus (13.8%), Staphylococcus aureus (10.3%), and rhino/enterovirus (10.3%). Previous medical non-infectious conditions were recorded in 13%.
Conclusion: The study revealed a high burden of infections in admitted patients mostly caused by well-known pathogens prevalent also in the local population. Both tropical infections and pre-existing non-infectious conditions are also important in admitted patients. Better epidemiological data is required to optimize health care for this medically most vulnerable population in refugee crises.
|
What is Known: • Pediatric refugees and asylum seekers are the most vulnerable population in refugee crises. • Data on health concerns and needs in this population is scarce. |
|
What is New: • This is one of the first studies on the epidemiology of pediatric refugees and asylum seekers treated as inpatients in a European high-income country. • The high burden of infections is mostly caused by well-known pathogens prevalent also in the local population. |
Keywords: Europe, Children, Immigrant health, Refugee crisis, Unaccompanied refugee minor, Infections in refugees
Introduction
In 2015, the United Nations High Commissioner for Refugees (UNHCR) estimated that 24.5 million refugees and asylum seekers existed worldwide, of which 51% were younger than 18 years [23]. An estimated 12.4 million people were newly displaced due to conflict or persecution, equalling an average of 24 people every minute of 2015. Syria had become the largest source country, followed by Afghanistan and Somalia, together accounting for 54% of the global number of refugees and asylum seekers. These people were hosted mostly by neighboring countries like Turkey, Lebanon, and Jordan and only a fraction of them continued their way to Europe [24]. In 2015, approximately one million asylum seekers arrived by sea of which most (around 84%) landed in Greece, trying to subsequently make their way across the central and eastern Mediterranean routes to Western Europe, where Switzerland is one of the primary destination countries [7, 22–24].
In 2015, 39.5 thousand people applied for asylum in Switzerland, which was 66% more than the year before [21]. With this number, Switzerland counted for 3% of all asylum applications in Europe. The largest source country of asylum seekers in Switzerland in 2015 was Eritrea followed by Afghanistan and Syria. By the end of 2015, 12,548 (38%) asylum seekers had a reported age under 20 years and 2418 (7%) under 5 years [21]. The total number of people in the asylum-seeking process including accepted refugees and people with pending and preliminary decisions for asylum was 111,276 [21]. These numbers do not include individuals with irregular status, which are estimated to be between 100,000 and 300,000 [10].
Although there is increasing concern about the health of refugees and asylum seekers with national and supranational organizations including the World Health Organization (WHO) and medical aid charities underlining the importance of prioritizing health services, health care professionals in many countries have a limited understanding of the health concerns and needs in this patient group [9]. Most of the existing studies in the European Region focused on maternity and mental health and are limited by inconsistent definitions of refugees and asylum seekers [3]. Refugee and asylum-seeking children are at particular health risk, highlighted by data collected in 2015 in Croatia by Médecins Sans Frontières, showing that 25% of refugees and asylum seekers requiring medical services were under 5 years of age [4, 5]. Studies from Germany, Netherlands, and Switzerland showed that refugee and asylum-seeking children had higher rates of emergency room presentations and admissions, higher rates of infections like tuberculosis and intestinal parasites, and lower rates of vaccine coverage [11–13, 16, 19]. However, health data on asylum seekers and refugees in the European Region, particularly in pediatric populations, is very limited. A review performed in 2012 on the health of migrant children in Switzerland confirms that the literature on this topic is scarce [8].
The aim of this study is to describe the epidemiology of pediatric refugees and asylum seekers admitted to our institution and to detail the spectrum of diseases and management thereof.
Patients and methods
After arrival in Switzerland, asylum seekers are received at one of the reception and processing centers run by the State Secretariat for Migration. In 2015, the reception and processing center in Basel was the second largest in Switzerland with 8826 asylum applications [21]. Refugees and asylum seekers were hosted in six different locations in the cantons of Basel-Stadt and Basel-Land. The University of Basel Children’s Hospital (UKBB) receives referrals of children from the reception and processing center in Basel as well as from various cantonal accommodations and asylum centers in the cantons of Basel-Stadt, Basel-Land, and neighboring cantons. UKBB is the only pediatric hospital in the cantons of Basel-Stadt and Basel-Land and children from these two cantons are exclusively hospitalized at UKBB. Pediatric refugees and asylum seekers aged < 18 years and admitted between 1 January and 31 December 2015 were retrospectively identified using the hospital’s electronic health records.
As refugee status is not routinely recorded at our institution, the cases were identified through the cost bearer of the medical care being the State Secretariat for Migration and/or the residence of the patient being the reception and processing center in Basel and all known cantonal accommodations for asylum seekers of Basel-Land and Basel-Stadt. Additionally, all patients originating form the largest source countries of asylum seekers and refugees in Switzerland (Eritrea, Syria, Afghanistan, and Iraq) were also added to the dataset. Electronic medical records from all patients in the dataset were screened and patients were only included for further analysis if they fulfilled the following criteria: (i) recent refugee or asylum seeker defined as no previous presentations to our hospital before 2014, (ii) < 18 years of age, and (iii) resident in Switzerland. Patients claiming asylum for medical reasons were excluded from the final analysis. For patients included in the final analysis, data was extracted from the electronic medical record using a standard form which included country of origin, age, gender, admission and discharge date, department admitted to, diagnoses, any treatment prescribed, any pathogens detected, any laboratory tests performed, and vaccination status. Data analysis was performed using SPSS (IBM, version 24.0.0.1).
Results
We identified 206 cases of which 105 admissions in 93 patients were included in the final analysis (Fig. 1). Of those, 83 (89.2%) patients were admitted once, 8 (8.6%) twice, and 2 (2.2%) three times.
Fig. 1.
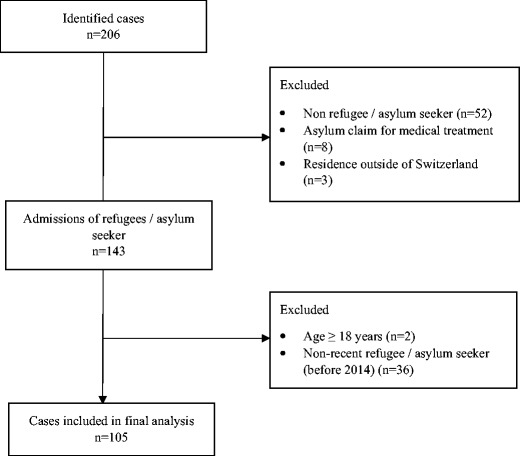
Cases included in the final analysis
The baseline characteristics of the patients are shown in Table 1. The median age of patients was 5.7 (IQR 2.6–14.5) years and 13% had previous medical conditions, such as congenital heart defects (3, 3.2%), congenital adrenal hyperplasia (2, 2.2%), and leukemia (2, 2.2%). Eritrea, Syria, and Afghanistan were the most frequent countries of origin with 30 (32.3%) originating from Sub-Saharan Africa, 29 (31.2%) from West Asia, 18 (19.4%) from Eastern Europe, and 16 (17.2%) from South Asia. Unaccompanied refugee minors originated from Eritrea (13, 72%), Afghanistan (3, 17%), and Somalia (2, 11%). The median age was 14.7 (IQR 4.4–15.8) years for patients originating from Eritrea, 5.5 (IQR 2.0–10.0) years for patients originating from Syria, and 8.9 (IQR 2.8–14.6) years for patients originating from Afghanistan. The median duration of admission was 4 (IQR 2–6) days and patients were most commonly admitted to the general pediatric department. The most common reason for admission was infection in 54.8%, followed by elective surgical interventions in 16.1%. A total of 105 admissions resulted in one, two, three, or four diseases diagnosed in 60 (57.1%), 24 (22.9%), 17 (16.2%), and 4 (3.8%).
Table 1.
Baseline characteristics, countries of origin, and reasons for admission in 93 pediatric refugees/asylum seekers admitted in 2015
| n | %/IQR | |
|---|---|---|
| Baseline characteristics | ||
| Median age (years) | 5.7 | 2.6–14.5 |
| Female gender | 38 | 40.9 |
| Unaccompanied refugee minor | 18 | 19.4 |
| Previous medical condition | 13 | 14.0 |
| Vaccination status documented | 6 | 6.5 |
| Duration of admission (days) | 4 | 2–6a |
| Countries of origin | ||
| Eritrea | 26 | 28.0 |
| Syria | 22 | 23.7 |
| Afghanistan | 14 | 15.1 |
| Iraq | 7 | 7.5 |
| Macedonia | 5 | 5.4 |
| Serbia | 5 | 5.4 |
| Somalia | 3 | 3.2 |
| Kosovo | 2 | 2.2 |
| Albania | 1 | 1.1 |
| Bosnia and Herzegovina | 1 | 1.1 |
| Belarus | 1 | 1.1 |
| Serbia and Montenegro | 1 | 1.1 |
| Iran | 1 | 1.1 |
| Sri Lanka | 1 | 1.1 |
| Russia | 1 | 1.1 |
| Ethiopia | 1 | 1.1 |
| Turkey | 1 | 1.1 |
| Reasons for admission | ||
| Infection | 51 | 54.8 |
| Elective surgical interventionb | 15 | 16.1 |
| Traumac | 8 | 8.6 |
| Non-infectious gastrointestinal condition | 6 | 6.5 |
| Endocrine condition | 3 | 3.2 |
| Mental health condition | 3 | 3.2 |
| Neonatal condition | 2 | 2.2 |
| Neurological condition | 2 | 2.2 |
| Hematologic condition | 2 | 1.9 |
| Dermatologic condition | 1 | 1.1 |
aRange 1–95 days
bIncluding dental care (n = 8), tonsillectomy (n = 2), tumor resection (n = 2), percutaneous endoscopic gastrostomy (n = 1), hip reconstruction (n = 1), anterior cruciate ligament reconstruction (n = 1)
cIncluding minor head trauma (n = 5), laceration (n = 2), bone fracture (n = 1)
Overall, at least one infectious cause was the reason for 55 admissions, which was a single infection in 34 (61.8%) and two or three in 13 (23.6%) and 8 (14.5%) instances, respectively, resulting in 84 infection episodes (Fig. 2 and Table 2). The main sites of infection were airways, skin, and gastrointestinal tract in 46.4, 20.2, and 11.9%, respectively. Tropical infections (including malaria, schistosomiasis, and cutaneous diphtheria) accounted for 11.9% of infections. In 25 (45.5%) admissions due to infection, an antibiotic treatment was initiated. A pathogen was identified in 58 instances using culture, PCR, antigen/antibody test, or direct microscopy, of which 34 (58.6%) were viruses, 15 (25.9%) bacteria, 5 (8.6%) parasites, and 4 (6.9%) helminths (Table 3). In 13 (23.6%) admissions for infectious diseases, more than one microorganism was detected, and in 4 (4.8%) infections, more than one disease-causing microorganism was identified.
Fig. 2.
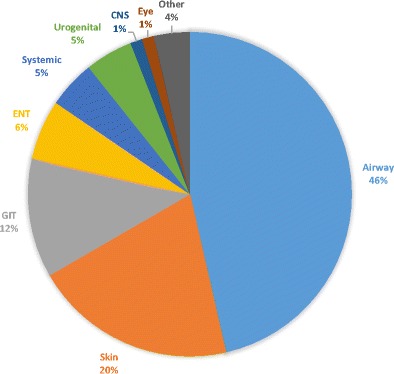
Sites of infection in 84 infections diagnosed in 55 admissions. CNS central nervous system, ENT ear, nose, and throat, GIT gastrointestinal tract
Table 2.
Details of the 84 infections diagnosed in 55 admissions by site of infection
| n | % | |
|---|---|---|
| Airway | 39 | 46.4 |
| Infection of the upper airways | 13 | 15.5 |
| Influenza | 11 | 13.1 |
| Pneumonia | 10 | 11.9 |
| Wheezing episode | 4 | 4.8 |
| Laryngotracheitis | 1 | 1.2 |
| Skin | 17 | 20.2 |
| Skin abscess | 6 | 7.1 |
| Staphylodermia | 3 | 3.6 |
| Scabies | 3 | 3.6 |
| Cutaneous diphtheria | 2 | 2.4 |
| Pediculosis | 2 | 2.4 |
| Tinea corporis | 1 | 1.2 |
| GIT | 10 | 11.9 |
| Gastroenteritis | 8 | 9.5 |
| Hepatitis A | 1 | 1.2 |
| Hepatitis B | 1 | 1.2 |
| ENT | 5 | 6.0 |
| Acute otitis media | 4 | 4.8 |
| Sinusitis | 1 | 1.2 |
| Systemic | ||
| Malaria tertiana | 4 | 4.8 |
| Urogenital | ||
| Schistosomiasis | 4 | 4.8 |
| CNS | ||
| Bacterial meningitis | 1 | 1.2 |
| Eye | ||
| Bacterial conjunctivitis | 1 | 1.2 |
| Others | 3 | 3.6 |
| Polytopic viral infection | 2 | 2.4 |
| Fever without focus | 1 | 1.2 |
CNS central nervous system, ENT ear, nose, and throat, GIT gastrointestinal tract
Table 3.
Microorganisms identified using culture, PCR, antigen/antibody detection, or direct microscopy by frequency
| n | % | |
|---|---|---|
| Virus | 34 | 58.6 |
| Influenza A virus | 8 | 13.8 |
| Rhino/enterovirus | 6 | 10.3 |
| Parainfluenza virus | 5 | 8.6 |
| Influenza B virus | 3 | 5.2 |
| Rotavirus | 3 | 5.2 |
| Bocavirus | 2 | 3.4 |
| Coronavirus | 1 | 1.7 |
| Hepatitis A virus | 1 | 1.7 |
| Hepatitis B virus | 1 | 1.7 |
| Human metapneumovirus | 1 | 1.7 |
| Norovirus | 1 | 1.7 |
| Respiratory syncytial virus B | 1 | 1.7 |
| Adenovirus | 1 | 1.7 |
| Bacteria | 15 | 25.9 |
| Staphylococcus aureus | 6 | 10.3 |
| Streptococcus pyogenes | 4 | 6.9 |
| Corynebacterium diphtheriae | 2 | 3.4 |
| Neisseria meningitidis a | 2 | 3.4 |
| Mycoplasma pneumoniae | 1 | 1.7 |
| Parasite/helminth | 9 | 15.5 |
| Plasmodium vivax | 4 | 6.9 |
| Schistosoma sp b | 4 | 6.9 |
| Sarcoptes scabiei | 1 | 1.7 |
aSerotype W135 (n = 1), unknown serotype (n = 1)
b Schistosoma mansoni (n = 2), unspecified (n = 2)
In the majority of the patients (54, 58.1%), immunization status was not documented in our medical records, and in 33 (35.5%), the status was unknown. Only three (3.2%) of the patients received vaccinations during their hospitalizations. Infectious disease workup was performed in 22 (23.7%), mostly febrile, patients. The diseases most often investigated were human immunodeficiency virus (HIV), hepatitis C, malaria, hepatitis B, and tuberculosis, with 16 (72.7%), 10 (45.5%), 10 (45.5%), 9 (40.9%), and 7 (31.8%) cases, respectively.
A total of 62 (66.7%) patients had a full blood count performed and 19 (30.6%) were anemic, mostly with normocytic and normochromic erythrocytes (13, 68.4%). With 19 (20.4%) cases, anemia was the most frequent non-communicable condition in our population.
The second most common non-surgical reason for admission was non-infectious gastrointestinal conditions (6, 6.5%), with constipation reported in three cases. Admissions for endocrine conditions (3, 3.2%) were all due to type 1 diabetes mellitus; in two of the three cases, the condition was newly diagnosed. Three patients were admitted to our psychosomatic ward, one with anorexia nervosa, the other with posttraumatic stress disorder, and the last with recurrent emesis due to psychosocial stress. The two admissions for hematological conditions were leukemias; in both cases, the diagnosis was known before arrival in Switzerland. Two (2.2%) newborn infants were hospitalized in our neonatal unit, one for severe prematurity with a gestational age of 25 weeks and one for suspected child abuse. The neurological reasons for admission were generalized seizure and severe global development delay. The dermatological reason for hospitalization was an allergic reaction following a hymenoptera sting.
Discussion
The results of the present study indicate a broad spectrum of health issues in refugee and asylum-seeking children and adolescents. Similar to other studies in this setting, infectious diseases were one of the main conditions requiring admission and treatment [12, 13, 16, 17]. Over half of the study population was admitted due to infection, one third of which localized in the airways. A high portion of infections was also found in a recent study in admitted asylum-seeking adults and children in the Netherlands, with 48% of infections predominantly caused by tropical diseases like malaria tertiana and tuberculosis [16]. In Germany, two recent studies on unaccompanied refugee minors showed a high prevalence of infections with approximately 20% of parasitic infections [12, 13].
A retrospective Swiss study including refugees and asylum seekers older than 15 years from the Middle East in an emergency department from 2011 to 2014 showed that the most common reasons for presentation were surgical (43%), followed by medical (37%) and psychiatric (16%). Amongst the group of medical reasons, acute infections were the most frequent reason of presentations (44%) [15].
Unlike other studies, we noticed a relatively low prevalence of tropical diseases with only a few cases of malaria and no intestinal parasitic infections [12, 13, 16, 17]. All cases of malaria originated from Eritrea which was the most frequent country of origin with endemic malaria in our population. Although malaria admission rates in Eritrea declined by over 75% between 2000 and 2014, neighboring Germany detected a sharp increase of Plasmodium vivax malaria in Eritrean migrants between 2014 and 2015 [20, 26]. The reason why we did not find any parasitic intestinal infections may have been the absence of routine screening procedures. Similarly, other screening tests for infections including schistosomiasis, HIV, and hepatitis B and C were not routinely performed but only if a clinical suspicion was present. Furthermore, it is likely that a certain selection of patients occurs in the refugee’s home country upon departure and during transit. Families with limited resources who can only afford to pay for one family member’s journey conceivably will select the healthiest individual with the highest chances to survive the journey.
The rate of anemia, the most frequent non-communicable condition in our population, was similar to a study recently in newly arrived refugees in Canada, in which 21% of children and women were anemic [18]. Since only two thirds of our patients had a full blood count performed, we are unable to determine the prevalence more accurately. However, this is certainly higher than in the local population with WHO estimated prevalence rate of anemia in Swiss preschool-age children of 6.3% [25].
Similar to other studies, a substantial group of our patients had pre-existing conditions including congenital adrenal hyperplasia, leukemia, or congenital heart defect [14]. Although this number is possibly biased by the fact that children with pre-existing conditions are more likely to be admitted to hospital, it underlines the complexity of health issues in the current migrant population.
In the majority of the patients, the immunization status was deemed incomplete. The retrospective collection of data does not allow us to determine whether this was due to a lack of immunization being performed in the country of origin, lack of immunization records, or lack of questioning and documentation of this fact by the clinician admitting the patient. Only a small proportion of patients received immunizations during their admission. Likely explanations include that the clinicians deemed immunizations to be deferred to a later time point in individuals admitted for infectious reasons and the fact that in Switzerland immunizations are usually performed by the primary health care provider. Importantly, the possibility of starting catch-up immunizations was commonly missed by the treating team.
The dense and difficult living conditions of asylum seekers increase the risk of transmission of highly contagious diseases, which may explain why the proportion of admissions due to influenza virus in our study was high. National recommendations for influenza vaccinations in children aim at individuals at risk: children with chronic diseases, pregnant women, or premature infants. Children that have close contact to individuals at risk or infants younger than 6 months are also advised to be immunized; however, health insurance only covers costs for the individuals at risk, and therefore, the majority of refugee and asylum-seeking children and adolescent remain unimmunized [6].
Unlike other studies which showed that mental health problems are an important issue with relatively high prevalence especially in unaccompanied minor refugees, in the present study, only few patients were admitted with mental health complaints [1, 3, 15]. A possible explanation is that many of those being treated for mental health issues are treated in outpatient settings and only a well-defined spectrum of severe cases is admitted. However, with no routine screening program for mental distress disorders in place for refugees in Switzerland, we must assume that a substantial rate of undetected mental health problems, especially in unaccompanied minors, has been missed.
We noticed two major demographic differences between the groups of the three most frequent countries of origin: 50% of the patients originating from Eritrea were unaccompanied refugee minors, compared to 21% of the patients originating from Afghanistan and none from Syria. Accordingly, patients from Eritrea and Afghanistan were older than patients coming from Syria. This corresponds to observations from other studies that young Syrian children often arrive in families compared to Afghans and Eritreans often arriving as unaccompanied teenagers.
Several limitations exist in the present study. First, we only included patients admitted to the hospital, and therefore, our data is not generalizable to the general pediatric population of refugees and asylum seekers in Switzerland. Second, the reliance on retrospective electronic health records inevitably presents potential sources of reporting bias. Third, no routine screening tests for frequent conditions, such as enteric parasites, have been performed, as during the study period no hospital or national guidance existed for screening of refugees and asylum seekers, and therefore, their prevalence could not be analyzed [2]. Another important limiting factor is that many of our patients were only admitted several months after their arrival in Switzerland, which may not reflect their initial health status.
Conclusion
The study revealed a high burden of infections in admitted patients mostly caused by pathogens prevalent also in the local population. Both tropical infections and pre-existing non-infectious conditions are also important in admitted patients. Better epidemiological data is required to optimize health care for this medically most vulnerable population in refugee crises.
Abbreviations
- CNS
Central nervous system
- ENT
Ear, nose, and throat
- GIT
Gastrointestinal tract
- HIV
Human immunodeficiency virus
- UNHCR
United Nations High Commissioner for Refugees
- UKBB
University of Basel Children’s Hospital
- WHO
World Health Organization
Authors’ contributions
Christian Pohl: Conceived the study, performed data analysis, drafted the initial manuscript, and approved the final manuscript as submitted.
Ines Mack: Conceived the study, reviewed the manuscript, and approved the final manuscript as submitted.
Torsten Schmitz: Conceived the study, reviewed the manuscript, and approved the final manuscript as submitted.
Nicole Ritz: Conceived the study, supervised analysis, reviewed and revised the manuscript, and approved the final manuscript as submitted.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval/informed consent
Due to the retrospective, descriptive study design no patient consent was obtained. The study was approved by the ethics committee northwest/central Switzerland (EKNZ:2017-01585).
Contributor Information
Christian Pohl, Email: christian.pohl@ukbb.ch.
Ines Mack, Email: ines.mack@ukbb.ch.
Torsten Schmitz, Email: torsten.schmitz@ukbb.ch.
Nicole Ritz, Phone: +41 61 704 12 12, Email: nicole.ritz@unibas.ch.
References
- 1.Bean TM, Eurelings-Bontekoe E, Spinhoven P. Course and predictors of mental health of unaccompanied refugee minors in the Netherlands: one year follow-up. Soc Sci Med. 2007;64:1204–1215. doi: 10.1016/j.socscimed.2006.11.010. [DOI] [PubMed] [Google Scholar]
- 2.Bernhard S, Büttcher M, Heininger U, Ratnam S, Relly C. Guidance for testing and preventing infections and updating immunisations in asymptomatic refugee children and adolescents in Switzerland. Paediatrica. 2016;27:1–8. [Google Scholar]
- 3.Bradby H, Humphris R, Newall D, Phillimore J (2015) Public health aspects of migrant health: a review of the evidence on health status for refugees and asylum seekers in the European Region. WHO [PubMed]
- 4.Catchpole M, Coulombier D (2015) Refugee crisis demands European Union-wide surveillance! Eur Secur. 10.1086/520454 [DOI] [PubMed]
- 5.Escobio F, Echevarria J, Rubaki S, Viniczai V. Health assistance of displaced people along the Balkan route. Lancet. 2015;386:2475. doi: 10.1016/S0140-6736(15)01240-4. [DOI] [PubMed] [Google Scholar]
- 6.Federal Office of Public Health FOPH (2016) Swiss influenza pandemic plan
- 7.International Organization for Migration (IOM) (2016) Mixed migration flows in the Mediterranean and beyond—2015 annual report
- 8.Jaeger FN, Hossain M, Kiss L, Zimmerman C. The health of migrant children in Switzerland. Int J Public Health. 2012;57:659–671. doi: 10.1007/s00038-012-0375-8. [DOI] [PubMed] [Google Scholar]
- 9.Jakab Z (2015) Population movement is a challenge for refugees and migrants as well as for the receiving population http://www.euro.who.int/en/health-topics/health-determinants/migration-and-health/news/news/2015/09/population-movement-is-a-challenge-for-refugees-and-migrants-as-well-as-for-the-receiving-population
- 10.Longchamp C, Aebersold M, Rousselot B, Ratelband-Pally S (2005) Sans Papiers in der Schweiz: Arbeitsmarkt, nicht Asylpolitik ist entscheidend. 1–68
- 11.Manzano S, Suter S. La santé des enfants requérants d’asile à Genève. Med Hyg (Geneve) 2002;60:360–362. [Google Scholar]
- 12.Marquardt L, Krämer A, Fischer F, Prüfer-Krämer L. Health status and disease burden of unaccompanied asylum-seeking adolescents in Bielefeld, Germany: cross-sectional pilot study. Trop Med Int Heal. 2015;21:210–218. doi: 10.1111/tmi.12649. [DOI] [PubMed] [Google Scholar]
- 13.Mockenhaupt FP, Barbre KA, Jensenius M, Larsen CS, Barnett ED, Stauffer W, Rothe C, Asgeirsson H, Hamer DH, Esposito DH, Gautret P, Schlagenhauf P (2016) Profile of illness in Syrian refugees: a geosentinel analysis, 2013 to 2015. Eur Secur. 10.2807/1560-7917.ES.2016.21.10.30160 [DOI] [PMC free article] [PubMed]
- 14.Nicolai T, D M, Fuchs O, von Mutius E (2015) Caring for the wave of refugees in Munich. N Engl J Med 150923140040009. doi: 10.1056/NEJMp1512139 [DOI] [PubMed]
- 15.Pfortmueller CA, Schwetlick M, Mueller T, Lehmann B, Exadaktylos AK. Adult asylum seekers from the middle east including Syria in central Europe: what are their health care problems? PLoS One. 2016;11:1–11. doi: 10.1371/journal.pone.0148196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ravensbergen SJ, Lokate M, Cornish D, Kloeze E, Ott A, Friedrich AW, van Hest R, Akkerman OW, de Lange WC, van der Werf TS, Bathoorn E, Stienstra Y. High prevalence of infectious diseases and drug-resistant microorganisms in asylum seekers admitted to hospital; no carbapenemase producing Enterobacteriaceae until September 2015. PLoS One. 2016;11:e0154791. doi: 10.1371/journal.pone.0154791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Redditt VJ, Graziano D. Health status of newly arrived refugees in Toronto, Ont part 1: infectious diseases. Can Fam Physician. 2015;61:e303–e309. [PMC free article] [PubMed] [Google Scholar]
- 18.Redditt VJ, Janakiram P, Graziano D, Rashid M. Health status of newly arrived refugees in Toronto, Ont part 2: chronic diseases. Can Fam physician Médecin Fam Can. 2015;61:e310–e315. [PMC free article] [PubMed] [Google Scholar]
- 19.Ritz N, Brinkmann F, Garcia BS, Tebruegge M, Kampmann B. Tuberculosis in young refugees. Lancet. 2015;386:2475–2476. doi: 10.1016/S0140-6736(15)01241-6. [DOI] [PubMed] [Google Scholar]
- 20.Roggelin L, Tappe D, Noack B, Addo MM, Tannich E, Rothe C (2016) Sharp increase of imported Plasmodium vivax malaria seen in migrants from Eritrea in Hamburg. Germany Malar J doi. 10.1186/s12936-016-1366-7 [DOI] [PMC free article] [PubMed]
- 21.State Secretariat for Migration (SEM) (2016) Schweiz-Asylstatistik:2015
- 22.United Nations High Commisioner for Refugees (UNHCR) (2015) Europe’s refugee emergency response update #16
- 23.United Nations High Commissioner for Refugees (UNHCR) (2016) Global Report 2015
- 24.United Nations High Commissioner for Refugees (UNHCR) (2016) Global Trends 2015
- 25.World Health Organization (WHO) (2008) Worldwide prevalence on anaemia 1993–2005
- 26.World Health Organization (WHO) (2015) World Malaria Report 2015


