Abstract
Background
The accuracy of any radiation therapy delivery is limited by target organ translocation and distortion. Bladder filling is one of the recognised factors affecting prostate translocation and distortion. The purpose of our study was to evaluate the effect of bladder volume on prostate translocation and distortion by using detailed three-dimensional prostate delineation on MRI.
Patients and methods
Fifteen healthy male volunteers were recruited in this prospective, institutional review board-approved study. Each volunteer underwent 4 different drinking preparations prior to imaging, with MR images acquired pre- and post-void. MR images were co-registered by using bony landmarks and three-dimensional contouring was performed in order to assess the degree of prostate translocation and distortion. According to changes in bladder or rectum distention, subdivisions were made into bladder and rectal groups. Studies with concomitant change in both bladder and rectal volume were excluded.
Results
Forty studies were included in the bladder volume study group and 8 in the rectal volume study group. The differences in rectal volumes yielded higher levels of translocation (p < 0.01) and distortion (p = 0.02) than differences in bladder volume. Moderate correlation of prostate translocation with bladder filling was shown (r = 0.64, p < 0.01). There was no important prostate translocation when bladder volume change was < 2-fold (p < 0.01). Moderate correlation of prostate distortion with bladder filling was shown (r = 0.61, p < 0.01).
Conclusions
Bladder volume has a minimal effect on prostate translocation and effect on prostate distortion is negligible. Prostate translocation may be minimalised if there is < 2-fold increase in the bladder volume.
Key words: prostate translocation, prostate distortion, gland deformation, bladder volume, magnetic resonance imaging, radiation therapy planning
Introduction
Prostate cancer is the commonest male non-cutaneous cancer worldwide, with its incidence continuing to increase due to an ageing population.1 Current American Urological Association guidelines for localized prostate cancer state that care options offered to patients should include active surveillance, external-beam radiation therapy, radical prostatectomy, brachytherapy and hormone therapy, with options being modulated according to baseline patient risk group.2, 3 Radiation therapy, either alone or in conjunction with hormonal therapy, is an effective and accepted care option across all risk groups.3
In radiation therapy, it is important to perform a secure delivery of high doses with dose minimization to adjacent organs at risk.4, 5 The accuracy of any radiation therapy is however limited by several factors, including set-up error, organ delineation, inter- and intra-fraction organ translocation, and target organ distortion.6 Rectal distension and, to a lesser extent, bladder filling have been found to be the principal causes of prostate translocation.4,7, 8, 9 Despite this, there is a lack of consensus regarding the optimal degree of bladder filling during radiation therapy, with recommendations encompassing a spectrum of an empty, partially full, comfortably full or full bladder.4, 8, 10, 11, 12, 13 Some studies have shown that radiation therapy with a full bladder protocol has distinct advantages in relation to dose load to both rectum and bladder.14, 15 However, a proportion of patients will struggle to maintain a full bladder protocol due to advanced age or urinary irritation, thus some authors favour an empty bladder protocol for reasons of patient comfort and the potential for improved volume reproducibility; despite initial concerns, such protocols have been shown to have a low radiation therapy bladder toxicity.15, 16
According to the literature there is only minimal effect of bladder filling on prostate translocation8,9,12,14,17,19, however, the methodology of these studies lacks standardization and their quantification methods may lack accuracy. Previous studies have reported on the prostatic mid-point or prostatic boarders as reference points of prostate translocation, but such a methodology may not fully account for prostate distortion and, by implication, changes in the target volume.10,14, 17 Although some studies have incorporated prostate three-dimensional (3D) contouring with computed tomography (CT)8, 12, CT is known to over-estimate prostate volume compared to magnetic resonance imaging (MRI).18, 19 Furthermore, detailed MRI information of prostate translocation and distortion is becoming increasingly important, with radiation therapy delivery systems that integrate MRI scanners for guidance being introduced into the clinic.20 Thus, the aim of our study was to evaluate the effect of bladder volume on prostate translocation and distortion by using detailed 3D prostate delineation on MRI.
Patients and methods
Study cohort
Fifteen healthy male volunteers were included in this prospective, institutional review board-approved study, with written informed consent obtained in all cases.
Magnetic resonance imaging
MRI examinations were carried out on a 3T MR750 magnet (General Electric Healthcare, Waukesha, WI, USA) using a 32-channel phased-array body coil. The protocol comprised: high-resolution axial T2-weighted (T2w) fast recovery fast spin echo (FRFSE) sequence, TR/TE of 3663/102 ms field-of-view (FOV) 22×22 cm2, slice thickness/gap 3.0/0.0 mm, in-plane resolution 0.85×0.57 mm, and 3 signal averages; sagittal T2w cube sequence, FOV 22×22 cm2, slice thickness/gap 2.0/0.0 mm, in-plane resolution 0.43×0.43 mm. MRI was performed on 4 consecutive days, with participants completing the following different preparations prior to imaging, with MR images acquired pre and post-void:
Preparation 1. Pass urine, no drinking 2 hours prior to scanning
Preparation 2. Pass urine, no drinking 1 hour prior to scanning
Preparation 3. Pass urine and drink 250 mL water 1 hour prior to scanning
Preparation 4. Pass urine and drink 500 mL water 1 hour prior to scanning
Computerised image analysis
The overall workflow diagram designed for MR image processing is depicted in Figure 1. Figure 1A represents the first phase of our procedure for the quantitative evaluation of the prostate translocation and distortion. For each study, the co-registration of the two MRI sequences was manually performed using ITK-SNAP in consensus with a board-certified uro-radiologist with 8-years’ experience in reporting prostate MRI studies – ITK-SNAP is a well-known medical image analysis framework based on the C++ Insight Toolkit (ITK) library. The registration was carried out in the sagittal plane according to bony landmarks (i.e., pelvic bones and lumbar spine) aiming to preserve the effects of soft-tissue deformation and movement.21, 22 The obtained affine transformation matrix (i.e., rigid-body transformations along with the scaling to take into account different FOVs) was then applied by means of advanced normalisation tools (ANTs).23, 24 For each pre-/post-void MRI scan pair for each of the four preparations, the pre-void scan (i.e., ‘moving’ volume) was co-registered in this way against the corresponding post-void scan (i.e., ‘fixed’ volume). Each co-registered image was then reformatted in the axial plane to allow for a more accurate and clinically relevant prostate delineation. The prostate was then manually delineated, by means of an in-house software tool, from the most inferior to the most superior location where the prostatic tissue could be clearly identified, excluding the seminal vesicles, according to the independently acquired high-resolution T2w FRFSE axial images.
Figure 1.
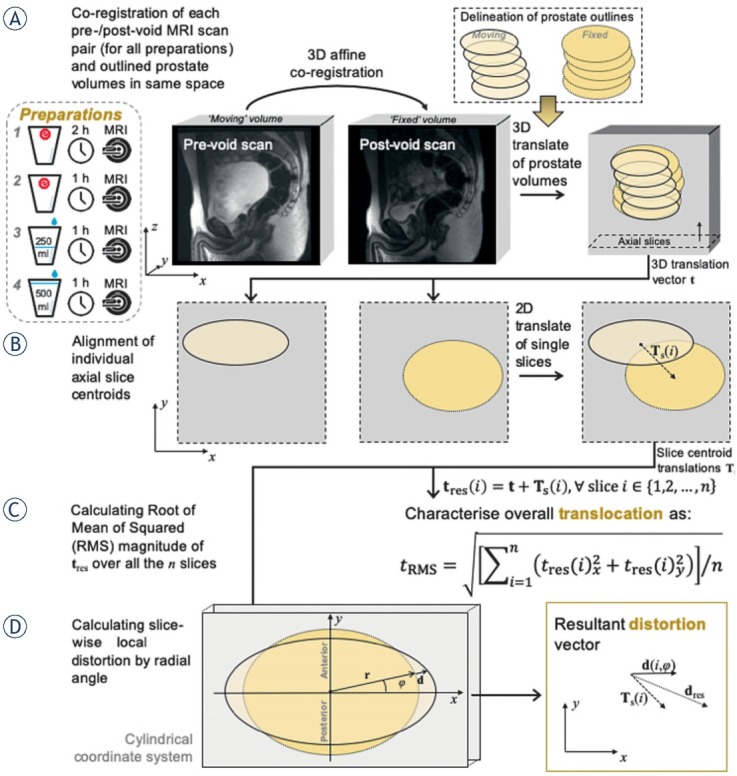
Overall scheme of the performed MR image analysis tasks. (A) 3D affine co-registration of each pre-void scan (‘moving’ volume) against the post-void scan (‘fixed’ volume). This operation is executed for all the four preparations described in the leftmost box. Subsequent manual delineation of the prostate on the two scans by using the axial reformatting. 3D rigid-body (translation alone t) volume alignment between the centres-of-mass of the two prostate glands under investigation. (B) For each slice, the volume sections are aligned so that their centroids are coincident (information stored in the ‘tree’ of slice centroid translations Ts). (C) Calculation of the RMS of the resultant translocation vector tres. (D) Computation of the resultant distortion vector dres, by considering also the subdivision of the axial plane into the anterior and posterior half-planes.
For more detailed analyses, the prostate was subdivided into apex, mid-gland, and base sectors by dividing the whole prostate gland into thirds and into the anterior and posterior gland for assessing distortion directions in the axial plane. More details about the computational and physical concepts underlying our analysis are provided in Supplementary Material. Briefly, by exploiting the computational framework for prostate deformation assessment proposed by Gill et al., the two prostate outlines under investigation are aligned to their centres, the slice delineations of the ‘moving’ volume are then translated onto the ‘fixed’ reference system (Figure 1B).25 The ‘resultant translocation’ tres is then computed to characterise the global translocation of the prostate (Figure 1C). The Root Mean Square (RMS) value of the magnitude of the resultant translocation vector is calculated by averaging over all the slices. Finally, Figure 1d shows the ‘resultant distortion’ dres for evaluating the combined effects of both translational and local distortions; three examples of distortion maps, along with the corresponding fixed and moving volumes, are displayed in Figure 2.
Figure 2.
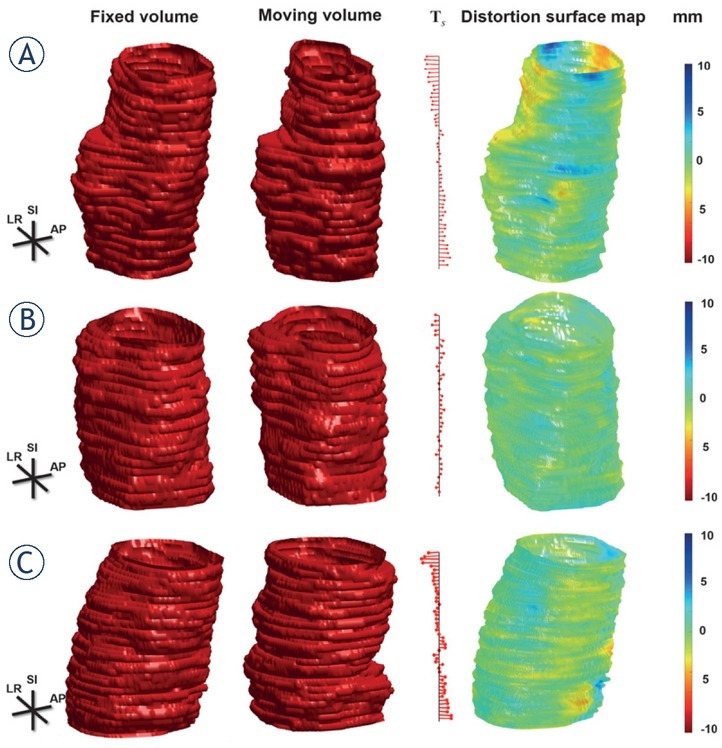
Example distortion maps of three MRI studies. (A) showing significant prostate translocation with significant base distortion in a study from the rectal group, (B) showing negligible prostate translocation and distortion in a study from the bladder group, and (C) showing significant prostate translocation but negligible prostate distortion in a study from the bladder group. The fixed and moving volumes are depicted in the first and second columns, respectively. In order to show the slice section difference as well as the local translation, the ‘tree’ of slice centroid translations Ts and the distortion surface map (along with the corresponding colour map expressed in mm) are shown in the third and fourth (fifth) columns, respectively.
Bladder volume and rectal distention assessment
Bladder volumes were calculated by using whole volume segmentation on sagittal T2w cube sequence using an in-house tool developed in Matlab (Math Works, Natick, MA, USA).26 Relative bladder volume difference was defined as absolute volume difference divided by post-void bladder volume. Rectal distention was derived using maximum sagittal and axial dimensions (anal canal to peritoneal reflection), and subjectively scored following a previously reported 5-point Likert scale: 1 = no stool/gas, 2 = minimal, 3 = small amount, 4 = moderate, 5 = large amount of stool/gas.27
Group design
Bladder and rectal volumes are potential confounders that may alter prostate position, thus a division into two groups was performed according to any change or otherwise in rectal and/or bladder volume. Important change in rectal distention was based on the work of Villiers et al., where no effect on prostate translocation was demonstrated when rectal volume was <56 mL, equivalent to our baseline score of 2/5.10, 27 Thus, significant rectal distension was defined when an increase or decrease in scoring by ≥ 1 point was observed, however changes in rectal volume for a baseline score of < 2 were disregarded.10, 27 Significant bladder distension change was defined if there was ≥ 2 fold change of bladder volume. The inclusion into the bladder-change group required no significant change in rectal distension and, likewise, inclusion criterion into the rectal-change group mandated no significant bladder volume change. Studies with concomitant change in both bladder and rectal volume were excluded. The translocation cut off values of 3 mm and 5 mm were defined according to the values in the literature, as a tight planning of target volume (PTV) margin is needed for hypo-fractionation regimens in order to increase target dose whilst minimizing dose to the surrounding tissues.28, 29 Typically, a 3 mm to 5 mm PTV margin is recommended clinically to limit the dosimetric consequences of both intrafraction and interfraction motion.28, 29
Intra-observer repeatability
All prostate contouring was conducted by a single observer. After the primary prostate contouring, in order to assess intra-observer repeatability, a subset of 10 studies were randomly selected, and the prostate was re-contoured in a blinded fashion by the same observer at a separate sitting. We applied the same computerized image analysis methods devised for quantitatively evaluating the bladder volume effect on prostate translocation and distortion. In particular, the two prostate gland delineations, performed on the same MRI study by the same radiologist, were employed in place of the prostate volumes delineated on the pre-/post-void MRI scan pairs (concerning the four preparations investigated).
Statistics
Unpaired Student’s t-test was used to compare continuous variables between two groups. Analysis of variance (ANOVA) was used to compare translocation and distortion in between prostatic sectors. Post hoc comparisons were adjusted for multiplicity using Bonferroni correction. Pearson’s correlation coefficient (r) was calculated to evaluate correlation. Significance was set at p < 0.05. Statistical analysis was performed with SPSS v.17.0 (SPSS Inc., Chicago, IL, USA).
Results
Fifteen volunteers (mean age 35.9 years, median 34, range 27–53) completed the study. The average prostate volume was 39.1 ± 10.2 mL (range: 32.1–56.7). In one volunteer, the MRI protocol was incomplete, and in 19 studies significant rectal distension change was identified. Thus, a total of 40 scans were included into the bladder volume study group. For the 19 studies with significant rectal distension change, 8 did not have significant bladder volume change and formed the rectal volume study group.
Prostate translocation - Bladder group
The mean pre-void bladder volume was 237.3 ± 150.2 mL (range: 40.9–598.1), and mean average post-void volume 74.1 ± 46.4 mL (range: 32.9–203.4). The absolute difference in bladder volume change was 163.1 ± 126.1 mL (range: 8.0–515.9). The median value for rectal distension was 3 (range: 1–5). The mean average absolute change in rectal volume was 5.6 ± 6.2 mL (range: 0.0–30.2).
Whole prostate translocation of ≥ 5 mm was observed in 4/40 (10.0%) patients and ≥ 3 mm in 9/40 (22.5%) patients. Prostatic sector subdivision showed statistically significant differences in translocation between the base and apex (Table 1). Base translocation of ≥ 5 mm was observed in 5/40 (12.5%) patients and of ≥ 3 mm in 15/40 (37.5%) patients. Mid-base translocation of ≥ 5 mm was observed in 4/40 (10.0%) patients and ≥ 3 mm in 9/40 (22.5%) patients. Apex translocation of ≥ 5 mm was observed in 3/40 (7.5%) patients and of ≥ 3 mm in 4/40 (10.0%) patients. Figure 3A depicts prostate translocation plotted against bladder volume (pre-void, post-void, absolute difference). There was a significant difference when subdivision was made according to relative bladder volume difference. The group with ≥ 2-fold increase in bladder volume (N = 17) showed higher translocation values than the group with < 2-fold increase (N = 23) in bladder volume at 3.47 ± 2.21 mm versus 1.72 ± 0.65 mm, respectively (p < 0.01). The directions of prostatic translocation are shown in Figure 4. When plotting the prostate translocation against relative bladder volume difference, there was a moderate positive correlation (r = 0.64, p < 0.01) (Figure 3B), driven by prostate translocation in the antero-posterior (AP) direction, which was the only direction showing a significant difference.
Table 1.
Inter-group translocation comparison for whole gland and prostatic sectors
| Bladder group Mean ± SD (mm) |
Rectal group Mean ± SD (mm) |
p-value | |
|---|---|---|---|
| Whole gland | 2.46 ± 1.73 | 4.44 ± 1.74 | <0.01 |
| Apex | 1.86 ± 1.39 | 3.96 ± 1.92 | <0.01 |
| Mid-gland | 2.31 ± 1.83 | 4.46 ± 1.88 | <0.01 |
| Base | 2.98 ± 2.05 | 4.70 ± 1.85 | 0.03 |
Figure 3.
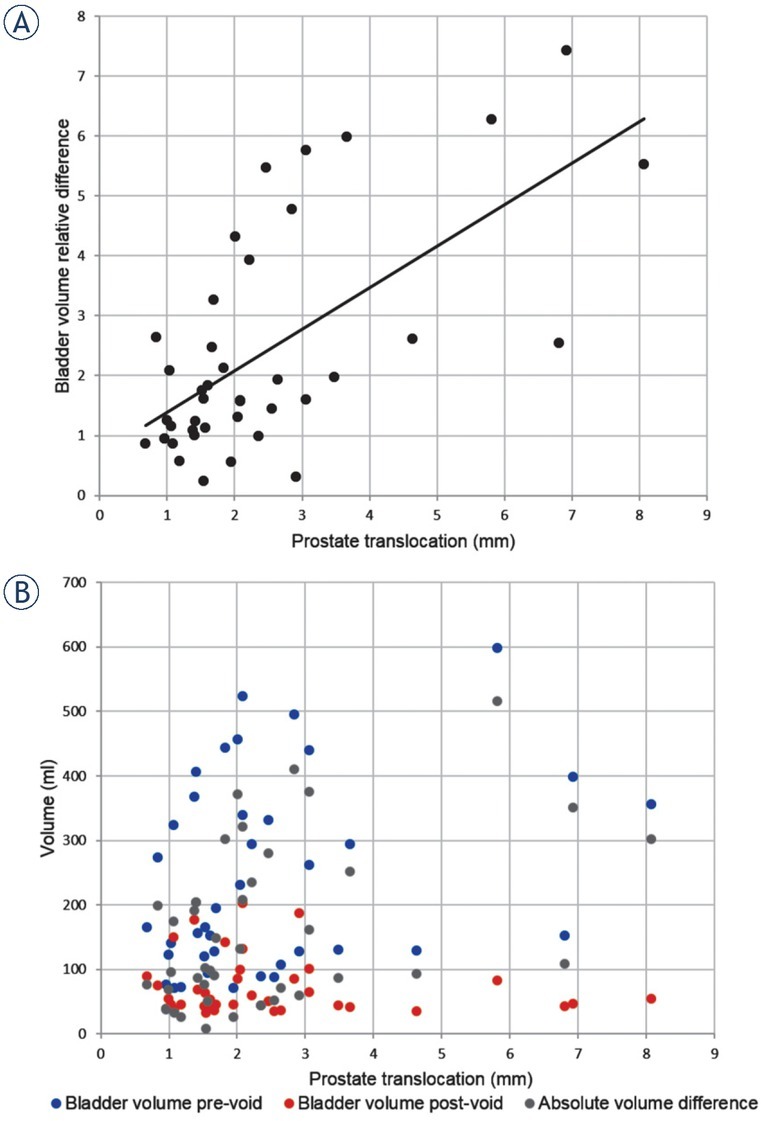
Prostate translocation plotted with relative bladder volume difference (r = 0.64, p < 0.01) (A). Prostate translocation plotted with bladder volumes (pre-void, post-void, absolute difference) (B).
Figure 4.
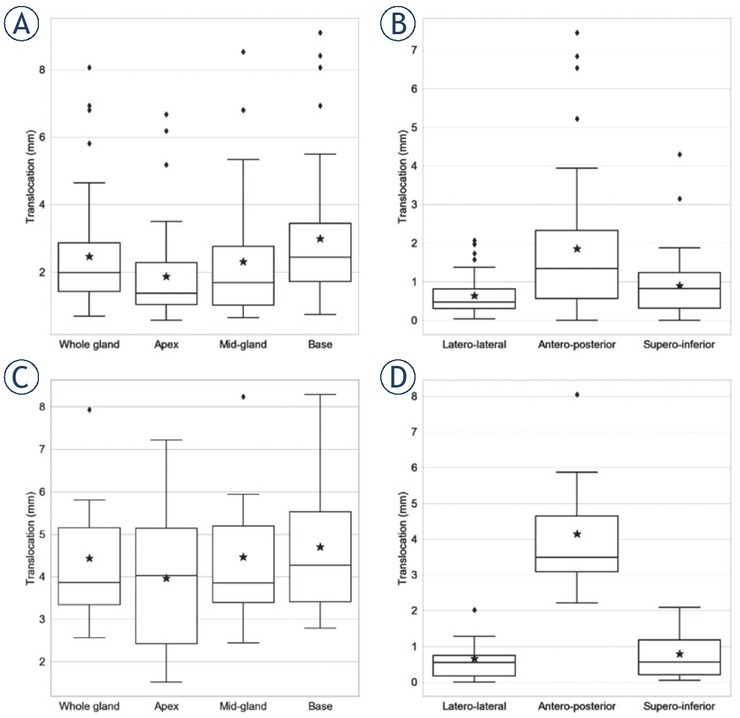
Translocation in the bladder group according to the prostatic sectors (A) and directions of translocation (B). Translocation in the rectum group according to the prostatic sectors (C) and directions of translocation (D). Each boxplot shows a black solid line and a grey star marker that denote the median and mean values, respectively.
Prostate translocation - Rectal group
Within the rectal group, the mean pre-void bladder volume was 84.4 ± 11.9 mL (range: 67.7– 99.0), and post-void bladder volume was 55.3 ± 9.9 mL (range: 38.8–70.9). The absolute difference in bladder volume change was 29.1 ± 14.7 mL (range: 8.2–48.0). On the pre-void study, the median value for rectal distension was 3 (range: 1–5) and on the post-void study the median value was 4 (range: 3–5). The average absolute difference in rectal change was 36.3 ± 19.7 mL (range: 14.5–77.5). Whole prostate translocation of ≥ 5 mm was observed in 2/8 (25.0%) patients and ≥ 3 mm in 7/8 (87.5%) of patients. There was no significant difference in translocation between the prostatic sectors (Table 1, Figure 4). Base translocation of ≥ 5 mm was observed in 4/8 (50.0%) patients and of ≥ 3 mm in 6/8 (75.0%) patients. Mid-gland translocation of ≥ 5 mm was observed in 3/8 (37.5%) patients and of ≥ 3 mm in 6/8 (75.0%) patients. Apex translocation of ≥ 5 mm was observed in 3/8 (37.5%) patients and of ≥ 3 mm in 6/8 (75.0%) patients. No correlation was found when plotting rectal volume against prostate translocation. Studies within the rectal group demonstrated significantly higher degrees of whole gland prostate distortion compared to the bladder group (Table 1).
Prostate distortion
Important differences were observed between the groups, with the rectal group showing higher levels of prostate distortion (Table 2). Similarly, important differences were observed between the groups in the degree of posterior whole gland distortion (Table 2). In the bladder group the maximum prostate distortions for whole gland, base, mid-gland and apex were 9.0 mm, 9.0 mm, 9.0 mm and 8.3 mm, respectively. In the rectal group the maximum prostate distortions for whole gland, base, mid-gland and apex were 10.1 mm, 9.5 mm, 10.1 mm and 6.6 mm, respectively. When plotting the whole gland distortion, there was a moderate positive correlation for relative bladder volume difference (r = 0.61, p < 0.01), but not for the rectum volume difference.
Table 2.
Prostate distortion expressed as mean and distortion values of the 90th percentile
| Bladder group |
Rectal group |
||||
|---|---|---|---|---|---|
| Mean ± SD (mm) | 90th percentile ± SD (mm) | Mean ± SD (mm) | 90th percentile ± SD (mm) | p-value | |
| Whole gland | 1.40 ± 0.36 | 2.55 ± 0.62 | 1.71 ± 0.33 | 3.20 ± 0.56 | 0.02 |
| Apex | 1.42 ± 0.53 | 2.44 ±0.80 | 1.46 ± 0.31 | 2.53 ± 0.43 | 0.80 |
| Mid-gland | 1.19 ± 0.27 | 2.19 ± 0.50 | 1.61 ± 0.41 | 2.90 ± 0.67 | <0.01 |
| Base | 1.61 ± 0.46 | 2.84 ± 0.80 | 2.01 ± 0.5 | 3.73 ± 0.83 | 0.02 |
| Whole gland, anterior | 1.41 ± 0.35 | 2.56 ± 0.60 | 1.59 ± 0.30 | 2.91 ± 0.50 | 0.14 |
| Whole gland, posterior | 1.40 ± 0.37 | 2.54 ± 0.65 | 1.82 ± 0.35 | 3.36 ± 0.61 | <0.01 |
Intra-observer reproducibility
High reproducibility was observed with only minimal discrepancies. The reliability measurements for the translocation direction were 0.08 ± 0.07 mm (range: 0.00–0.27) in the latero-lateral (LL) direction; 0.11 ± 0.07 mm (range: 0.00–0.27) in the AP direction and 0.4 ± 0.03 mm (range: 0.00–0.10) in the supero-inferior (SI) direction. Whole gland RMS translocation reproducibility and distortion reproducibility are noted in Supplementary Table.
Discussion
The results of our study suggest that bladder volume has only a minimal effect on prostate translocation and its effect on prostate distortion is negligible. Furthermore, it appears that prostate translocation may be minimised if there is a <2-fold increase in the bladder volume. Previous studies evaluated the effect of bladder volume on prostate translocation and distortion, typically utilizing CT for assessment.7, 8, 9 CT is known to over-estimate prostate volume by up to 35% compared to MRI, with MRI providing better differentiation of prostatic anatomy, particularly the posterior border, prostate apex and base-seminal vesicle interface.18, 19 In our study, detailed MRI prostate delineation on axial slices with sub-millimetre in-plane resolution was performed to more accurately quantify the degree of prostate translocation and distortion secondary to changes in bladder or rectal volumes, using a previously devised computational framework.25
Bladder volume has generally been reported to have a weak association with prostate translocation.7, 8, 10 In our study moderate correlation of prostate translocation with bladder filling was shown in the AP direction. Villeirs et al. described a considerable increase in prostate translocation in the superior-inferior direction with bladder volumes above 300 mL.10 The results of our study show that inter-fractional fluctuations of bladder volume should ideally be kept to a minimum, since there is a negligible prostate translocation with <2-fold changes in bladder volume. Thus, a “comfortably full” bladder is a reasonable aim, given the low probability of inducing a subsequent ≥ 2-fold increase.10 Furthermore, this is supported by a recent study that investigated two preparation protocols, finding no difference in bladder volume when enforcing a strict bladder-filling protocol or when giving an instruction to maintain a comfortably full bladder.13 Of note, the authors also concluded that expectations of maintaining a strictly controlled bladder volume at a repeat sitting scan causes patient discomfort and can have a negative impact on the treatment.13
Several studies have reported that rectal distension can significantly impact prostate translocation, whilst the impact of bladder filling appears more negligible.7, 8, 9, 10 This is in accordance with our study, given that the differences in rectal volumes yielded higher levels of translocation than differences in the bladder volume.7, 8, 9, 10 In both groups the amplitudes of prostate translocation were similar to previously published studies, and with a similar pattern of displacement observed, with the most prominent direction of translocation being in the AP direction.7, 8, 9, 10 In both groups the base of the prostate was shown to have a larger amplitude of translocation than the apex, presumably due to apex being relatively fixed in position due to the surrounding pelvic floor musculature.10, 30 In the bladder group, only 10% of examinations resulted in a translocation ≥ 5 mm, with a maximum translation of 8 mm. This falls within the range of planning target volume margins (5–8 mm) when using daily cross-sectional imaging, and based on soft-tissue registration or use of implanted fiducial markers.4, 31
Previous studies have evaluated distortion in relation to radiotherapy treatment planning.32, 33, 34, 35 Our study focused on differences in bladder volume and the effect of this on whole gland distortion. We observed similar mean and maximum values of prostate distortion compared to previous studies.32, 33, 34, 35 When comparing study groups, the results show that rectal volume differences impact prostate distortion to a higher degree than bladder volume differences. Furthermore, this group difference was most pronounced in the posterior prostate. Nichol et al. previously investigated the effect of bladder and rectal fillings on prostate distortion; however, they did not prove any association concluding that this was due to their use of bowel and bladder regimens.35 In our study we were also unable to show an association with rectal volume, possibly due to the small number of examinations within the rectal sub-study group, however, a moderate positive correlation with prostate distortion was observed in the bladder group.
A strength of our study is the robust methodology used, with sub-millimetre 3D whole gland delineation, which should be considered a gold standard. Only two studies utilized three-dimensional contouring in the process of prostate translocation evaluation, even though CT was used as the imaging modality.8, 12 Despite whole gland delineation being time consuming, future Machine Learning methods might be exploited for automated prostate segmentation, reducing the operator-dependence and the outlining time in manual segmentation procedures, making this method more feasible in both research and clinical settings.36
Our study has some limitations. The study population was composed of healthy volunteers, which may not be representative of a patient population, which typically would be older, with larger prostatic volume and the potential for outflow obstruction. It should also be noted that the study design allowed for relatively extreme differences in bladder volume from full (pre-void) to almost empty (post-void); such conditions would be unusual during relatively short clinical intra-fractional periods. Thus, the relatively minimal effect shown by bladder volumes in our study offers further reassurance from a clinical standpoint. Lastly, the number of cases within the rectal group was small due to the evaluation of rectal volume effect on prostate being only a secondary aim of the study. The effect of rectum volume appears to be greater than the effect of bladder volume on prostate translocation, however further work with more controlled methodology is needed to establish the effect.
In conclusion, bladder volume has only a minimal effect on prostate translocation and effect on prostate distortion is negligible. Prostate translocation may be minimalised if a < 2-fold increase in the bladder volume is maintained for the study duration.
Acknowledgements
The authors acknowledge research support from Royal College of Radiologists UK, Cancer Research UK (Grant number C19212/A16628), Prostate Cancer UK, National Institute of Health Research Cambridge Biomedical Research Centre, Cancer Research UK and the Engineering and Physical Sciences Research Council Imaging Centre in Cambridge and Manchester and the Cambridge Experimental Cancer Medicine Centre, Addenbrooke’s Charitable Trust, the National Institute for Health Research (NIHR) Cambridge Biomedical Research, Cambridge University Hospitals NHS Foundation Trust.
Disclosure
No potential conflicts of interest were disclosed.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2019. CA Cancer J Clin. 2019;69:7–34. doi: 10.3322/caac.21551. [DOI] [PubMed] [Google Scholar]
- 2.Thompson I, Thrasher JB, Aus G, Burnett AL, Canby-Hagino ED, Cookson MS. Guideline for the management of clinically localized prostate cancer: 2007 update. J Urol. 2007;177:2106–31. doi: 10.1016/j.juro.2007.03.003. et al. [DOI] [PubMed] [Google Scholar]
- 3.Bekelman JE, Rumble BR, Chen RC, Pisansky TM, Finelli A, Feifer A. Clinically localized prostate cancer: ASCO clinical practice guideline endorsement of an American Urological Association/American Society for Radiation Oncology/Society of Urologic Oncology Guideline. J Clin Oncol. 2018;36:3251–8. doi: 10.1200/JCO.18.00606. et al. [DOI] [PubMed] [Google Scholar]
- 4.Maggio A, Gabriele D, Garibaldi E, Bresciani S, Delmastro E, Di Dia A. Impact of a rectal and bladder preparation protocol on prostate cancer outcome in patients treated with external beam radiotherapy. Strahlenther Onkol. 2017;193:722–32. doi: 10.1007/s00066-017-1163-4. et al. [DOI] [PubMed] [Google Scholar]
- 5.Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, van der Kwast T. EAU guidelines on prostate cancer.part 1: screening, diagnosis, and local treatment with curative intent-update 2013. Eur Urol. 2014;65:124–37. doi: 10.1016/j.eururo.2013.09.046. et al. [DOI] [PubMed] [Google Scholar]
- 6.Kupelian P, Meyer JL. Image-guided, adaptive radiotherapy of prostate cancer: toward new standards of radiotherapy practice. Front Radiat Ther Oncol. 2011;43:344–68. doi: 10.1159/000322485. [DOI] [PubMed] [Google Scholar]
- 7.Adamson J, Wu Q. Inferences about prostate intrafraction motion from pre-and posttreatment volumetric imaging. Int J Radiat Oncol Biol Phys. 2009;75:260–7. doi: 10.1016/j.ijrobp.2009.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zelefsky MJ, Crean D, Mageras GS, Lyass O, Happersett L, Ling CC. Quantification and predictors of prostate position variability in 50 patients evaluated with multiple CT scans during conformal radiotherapy. Radiother Oncol. 1999;50:225–34. doi: 10.1016/S0167-8140(99)00011-0. et al. [DOI] [PubMed] [Google Scholar]
- 9.Wang KK, Vapiwala N, Bui V, Deville C, Plastaras JP, Bar-Ad V. The impact of stool and gas volume on intrafraction prostate motion in patients undergoing radiotherapy with daily endorectal balloon. Radiother Oncol. 2014;112:89–94. doi: 10.1016/j.ijrobp.2004.07.711. et al. [DOI] [PubMed] [Google Scholar]
- 10.Villeirs GM, De Meerleer GO, Verstraete KL, De Neve WJ. Magnetic resonance assessment of prostate localization variability in intensity-modulated radiotherapy for prostate cancer. Int J Radiat Oncol Biol Phys. 2004;60:1611–21. doi: 10.1016/j.ijrobp.2004.07.711. [DOI] [PubMed] [Google Scholar]
- 11.Bayley AJ, Catton CN, Haycocks T, Kelly V, Alasti H, Bristow R. A randomized trial of supine vs. prone positioning in patients undergoing escalated dose conformal radiotherapy for prostate cancer. Radiother Oncol. 2004;70:37–44. doi: 10.1016/j.radonc.2003.08.007. et al. [DOI] [PubMed] [Google Scholar]
- 12.Melian E, Mageras GS, Fuks Z, Leibel SA, Niehaus A, Lorant H. Variation in prostate position quantitation and implications for three-dimensional conformal treatment planning. Int J Radiat Oncol Biol Phys. 1997;38:73–81. doi: 10.1016/s0360-3016(97)00221-6. et al. [DOI] [PubMed] [Google Scholar]
- 13.Braide K, Kindblom J, Lindencrona U, Månsson M, Hugosson J. The value of a bladder-filling protocol for patients with prostate cancer who receive post-operative radiation: results from a prospective clinical trial. Acta Oncol. 2019;58:463–8. doi: 10.1080/0284186X.2018.1554261. [DOI] [PubMed] [Google Scholar]
- 14.Pinkawa M, Asadpour B, Gagel B, Piroth MD, Holy R, Eble MJ. Prostate position variability and dose-volume histograms in radiotherapy for prostate cancer with full and empty bladder. Int J Radiat Oncol Biol Phys. 2006;64:856–61. doi: 10.1016/j.ijrobp.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 15.Moiseenko V, Liu M, Kristensen S, Gelowitz G, Berthelet E. Effect of bladder filling on doses to prostate and organs at risk: a treatment planning study. J Appl Clin Med Phys. 2006;8:55–68. doi: 10.1120/jacmp.v8i1.2286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zelefsky MJ, Fuks Z, Happersett L, Lee HJ, Ling CC, Burman CM. Clinical experience with intensity modulated radiationtherapy (IMRT) in prostate cancer. Radiother Oncol. 2000;55:241–9. doi: 10.1016/s0167-8140(99)00100-0. et al. [DOI] [PubMed] [Google Scholar]
- 17.Ghilezan MJ, Jaffray DA, Siewerdsen JH, Van Herk M, Shetty A, Sharpe MB. Prostate gland motion assessed with cine-magnetic resonance imaging (cine-MRI) Int J Radiat Oncol Biol Phys. 2005;62:406–17. doi: 10.1016/j.ijrobp.2003.10.017. et al. [DOI] [PubMed] [Google Scholar]
- 18.Hentschel B, Oehler W, Strauss D, Ulrich A, Malich A. Definition of the CTV prostate in CT and MRI by using CT-MRI image fusion in IMRT planning for prostate cancer. Strahlenther Onkol. 2011;187:183–90. doi: 10.1007/s00066-010-2179-1. [DOI] [PubMed] [Google Scholar]
- 19.Tanaka H, Hayashi S, Ohtakara K, Hoshi H, Iida T. Usefulness of CT-MRI fusion in radiotherapy planning for localized prostate cancer. J Radiat Res. 2011;52:782–8. doi: 10.1269/jrr.11053. [DOI] [PubMed] [Google Scholar]
- 20.Pathmanathan AU, van As NJ, Kerkmeijer LGW, Christodouleas J, Lawton CAF, Vesprini D. Magnetic resonance imaging-guided adaptive radiation therapy: A “Game Changer” for prostate treatment? Int J Radiat Oncol Biol Phys. 2018;100:361–73. doi: 10.1016/j.ijrobp.2017.10.020. et al. [DOI] [PubMed] [Google Scholar]
- 21.Yushkevich PA, Gao Y, Gerig G. ITK-SNAP: an interactive tool for semi-automatic segmentation of multi-modality biomedical images. Conf Proc IEEE Eng Med Biol Soc. 2016;2016:3342–5. doi: 10.1109/EMBC.2016.7591443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yoo TS, Ackerman MJ. Open source software for medical image processing and visualization. Commun ACM. 2005;48:55–9. doi: 10.1145/1042091.1042120. [DOI] [Google Scholar]
- 23.Avants BB, Tustison NJ, Stauffer M, Song G, Wu B, Gee JC. The insight tool kit image registration framework. Front Neuroinform. 2014;8:44. doi: 10.3389/fninf.2014.00044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tustison NJ, Cook PA, Klein A, Song G, Das SR, Duda JT. Large-scale evaluation of ANTs and FreeSurfer cortical thickness measurements. Neuro Image. 2014;99:166–79. doi: 10.1016/j.neuroimage.2014.05.044. et al. [DOI] [PubMed] [Google Scholar]
- 25.Gill AB, Czarniecki M, Gallagher F.A., Barrett T. A method for mapping and quantifying whole organ diffusion-weighted image distortion in MR imaging of the prostate. Sci Rep. 2017;7:12727. doi: 10.1038/s41598-017-13097-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Snoj Ž, Rundo L, Gill AB, Tristan Barrett T. Quantifying the effect of biopsy lateral decubitus patient positioning compared to supine prostate MRI scanning on prostate translocation and distortion. Can Urol Assoc J. 2020. In press. [DOI] [PMC free article] [PubMed]
- 27.Caglic I, Hansen NL, Slough RA, Patterson AJ, Barrett T. Evaluating the effect of rectal distension on prostate multiparametric MRI image quality. Eur J Radiol. 2017;90:174–80. doi: 10.1016/j.ejrad.2017.02.029. [DOI] [PubMed] [Google Scholar]
- 28.Lovelock DM, Messineo AP, Cox BW, Kollmeier MA, Zelefsky MJ. Continuous monitoring and intrafraction target position correction during treatment improves target coverage for patients undergoing SBRT prostate therapy. Int J Radiat Oncol Biol Phys. 2015;91:588–94. doi: 10.1016/j.ijrobp.2014.10.049. [DOI] [PubMed] [Google Scholar]
- 29.Xiangyu Ma, Huagang Yan, Ravinder Nath, Zhe Chen, Haiyun Li, Wu Liu. Adaptive imaging versus periodic surveillance for intrafraction motion management during prostate cancer radiotherapy. Technol Cancer Res Treat. 2019;18:1533033819844489. doi: 10.1177/1533033819844489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wu J, Haycocks T, Alasti H, Ottewell G, Middlemiss N, Abdolell M. Positioning errors and prostate motion during conformal prostate radiotherapy using on-line isocentre set-up verification and implanted prostate markers. Radiother Oncol. 2001;61:127–33. doi: 10.1016/s0167-8140(01)00452-2. et al. [DOI] [PubMed] [Google Scholar]
- 31.Yartsev S, Bauman G. Target margins in radiotherapy of prostate cancer. Br J Radiol. 2016;89:20160312. doi: 10.1259/bjr.20160312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van der Wielen GJ, Mutanga TF, Incrocci L, Kirkels WJ, Vasquez Osorio EM, Hoogeman MS. Deformation of prostate and seminal vesicles relative to intraprostatic fiducial markers. Int J Radiat Oncol Biol Phys. 2008;72:1604–111. doi: 10.1016/j.ijrobp.2008.07.023. et al. [DOI] [PubMed] [Google Scholar]
- 33.Deurloo KE, Steenbakkers RJ, Zijp LJ, de Bois JA, Nowak PJ, Rasch CR. Quantification of shape variation of prostate and seminal vesicles during external beam radiotherapy. Int J Radiat Oncol Biol Phys. 2005;61:228–38. doi: 10.1016/j.ijrobp.2004.09.023. et al. [DOI] [PubMed] [Google Scholar]
- 34.Nakazawa T, Tateoka K, Saito Y, Abe T, Yano M, Yaegashi Y. Analysis of prostate deformation during a course of radiation therapy for prostate cancer. PLoS One. 2015;10:e0131822. doi: 10.1371/journal.pone.0131822. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nichol AM, Brock KK, Lockwood GA, Moseley DJ, Rosewall T, Warde PR. A magnetic resonance imaging study of prostate deformation relative to implanted gold fiducial markers. Int J Radiat Oncol Biol Phys. 2007;67:48–56. doi: 10.1016/j.ijrobp.2006.08.021. et al. [DOI] [PubMed] [Google Scholar]
- 36.Rundo L, Militello C, Russo G, Garufi A, Vitabile S, Gilardi MC. Automated prostate gland segmentation based on an unsupervised fuzzy C-means clustering technique using multispectral T1w and T2w MR imaging. Information. 2017;8:49. doi: 10.3390/info8020049. et al. [DOI] [Google Scholar]


