Abstract
Background
Most surgical procedures involve a cut in the skin that allows the surgeon to gain access to the deeper tissues or organs. Most surgical wounds are closed fully at the end of the procedure (primary closure). The surgeon covers the closed surgical wound with either a dressing or adhesive tape. The dressing can act as a physical barrier to protect the wound until the continuity of the skin is restored (within about 48 hours) and to absorb exudate from the wound, keeping it dry and clean, and preventing bacterial contamination from the external environment. Some studies have found that the moist environment created by some dressings accelerates wound healing, although others believe that the moist environment can be a disadvantage, as excessive exudate can cause maceration (softening and deterioration) of the wound and the surrounding healthy tissue. The utility of dressing surgical wounds beyond 48 hours of surgery is, therefore, controversial.
Objectives
To evaluate the benefits and risks of removing a dressing covering a closed surgical incision site within 48 hours permanently (early dressing removal) or beyond 48 hours of surgery permanently with interim dressing changes allowed (delayed dressing removal), on surgical site infection.
Search methods
In March 2015 we searched the following electronic databases: The Cochrane Wounds Group Specialised Register; The Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library); Database of Abstracts of Reviews of Effects (DARE) (The Cochrane Library); Ovid MEDLINE; Ovid MEDLINE (In‐Process & Other Non‐Indexed Citations); Ovid EMBASE; and EBSCO CINAHL. We also searched the references of included trials to identify further potentially‐relevant trials.
Selection criteria
Two review authors independently identified studies for inclusion. We included all randomised clinical trials (RCTs) conducted with people of any age and sex, undergoing a surgical procedure, who had their wound closed and a dressing applied. We included only trials that compared early versus delayed dressing removal. We excluded trials that included people with contaminated or dirty wounds. We also excluded quasi‐randomised studies, and other study designs.
Data collection and analysis
Two review authors independently extracted data on the characteristics of the trial participants, risk of bias in the trials and outcomes for each trial. We calculated risk ratios (RR) with 95% confidence intervals (CI) for binary outcomes and mean difference (MD) with 95% CI for continuous outcomes. We used RevMan 5 software to perform these calculations.
Main results
Four trials were identified for inclusion in this review. All the trials were at high risk of bias. Three trials provided information for this review. Overall, this review included 280 people undergoing planned surgery. Participants were randomised to early dressing removal (removal of the wound dressing within the 48 hours following surgery) (n = 140) or delayed dressing removal (continued dressing of the wound beyond 48 hours) (n = 140) in the three trials. There were no statistically significant differences between the early dressing removal group and delayed dressing removal group in the proportion of people who developed superficial surgical site infection within 30 days (RR 0.64; 95% CI 0.32 to 1.28), superficial wound dehiscence within 30 days (RR 2.00; 95% CI 0.19 to 21.16) or serious adverse events within 30 days (RR 0.83; 95% CI 0.28 to 2.51). No deep wound infection or deep wound dehiscence occurred in any of the participants in the trials that reported this outcome. None of the trials reported quality of life. The hospital stay was significantly shorter (MD ‐2.00 days; 95% CI ‐2.82 to ‐1.18) and the total cost of treatment significantly less (MD EUR ‐36.00; 95% CI ‐59.81 to ‐12.19) in the early dressing removal group than in the delayed dressing removal group in the only trial that reported these outcomes.
Authors' conclusions
The early removal of dressings from clean or clean contaminated surgical wounds appears to have no detrimental effect on outcomes. However, it should be noted that the point estimate supporting this statement is based on very low quality evidence from three small randomised controlled trials, and the confidence intervals around this estimate were wide. Early dressing removal may result in a significantly shorter hospital stay, and significantly reduced costs, than covering the surgical wound with wound dressings beyond the first 48 hours after surgery, according to very low quality evidence from one small randomised controlled trial. Further randomised controlled trials of low risk of bias are necessary to investigate whether dressings are necessary after 48 hours in different types of surgery and levels of contamination and investigate whether antibiotic therapy influences the outcome
Plain language summary
Early versus delayed dressing removal for people with surgical wounds
Most surgical procedures involve a cut in the skin that allows the surgeon to gain access to the deeper tissues or organs. Most surgical wounds are closed fully at the end of the procedure.The surgeon covers the closed surgical wound with either a dressing or adhesive tape.The dressing can act as a physical barrier to protect the wound until the continuity of the skin in restored (within about 48 hours). It can also absorb exudate from the wound, keeping it dry and clean, and preventing bacterial contamination from the external environment. Some studies have found that the moist environment created by some dressings accelerates wound healing, although others believe that it is a disadvantage, as excessive exudate can cause softening and deterioration of the wound and surrounding healthy tissue.
We reviewed the medical literature up to July 2013 and identified four randomised controlled trials that investigated early (permanent removal of dressings within 48 hours of surgery) versus delayed removal of dressings (permanent removal of dressings after 48 hours of surgery with interim changes of dressing allowed) in people with surgical wounds. The levels of bias across the studies were mostly high or unclear, i.e. flaws in the conduct of these trials could have resulted in the production of incorrect results. A total of 280 people undergoing planned surgery were included in this review. One‐hundred and forty people had their dressings removed within 48 hours following surgery and 140 people had their wounds dressed beyond 48 hours. The choice of whether the dressing was removed early (within 48 hours) or retained for more 48 hours was made randomly by a method similar to the toss of a coin. No significant differences were reported between the two groups in terms of superficial surgical site infection (infection of the wound), superficial wound dehiscence (partial disruption of the wound that results in it reopening at the skin surface) or the number of people experiencing serious adverse events. There were no deep wound infections or complete wound dehiscence (complete disruption of wound healing, when the wound reopens completely) in the studies that reported these complications. However, the studies were not large enough to identify small differences in complication rates. None of the studies reported quality of life. Participants in the group that had early removal of dressings had significantly shorter hospital stays and incurred significantly lower treatment costs than those in the delayed removal of dressings group, but these results were based on very low quality evidence from one small randomised controlled trial. We recommend further randomised controlled trials are performed to investigate whether dressing of wounds beyond 48 hours after surgery is necessary, since the current evidence is based on very low quality evidence from three small randomised controlled trials.
Summary of findings
Summary of findings for the main comparison. Early dressing removal compared to delayed dressing removal for surgical wounds.
| Early dressing removal compared to delayed dressing removal for surgical wounds | ||||||
| Patient or population: people with surgical site infection Settings: secondary or tertiary care Intervention: early dressing removal Comparison: delayed dressing removal | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Delayed dressing removal | Early dressing removal | |||||
| Superficial surgical site infection Superficial surgical site infection within 30 days of surgery Follow‐up: mean 30 days | 114 per 1000 | 73 per 1000 (37 to 146) | RR 0.64 (0.32 to 1.28) | 280 (3 studies) | ⊕⊝⊝⊝ very low1,2,3 | |
| Superficial wound dehiscence Superficial wound dehiscence reported within 30 days of surgery Follow‐up: mean 30 days | 11 per 1000 | 22 per 1000 (2 to 235) | RR 2.00 (0.19 to 21.16) | 180 (2 studies) | ⊕⊝⊝⊝ very low1,2,3 | |
| Serious adverse events Patients experiencing serious adverse events within 30 days of surgery Follow‐up: mean 30 days | 154 per 1000 | 128 per 1000 (43 to 386) | RR 0.83 (0.28 to 2.51) | 78 (1 study) | ⊕⊝⊝⊝ very low1,2,3 | |
| Length of hospital stay Total length of hospital stay at maximal follow up | The mean length of hospital stay in the control group was 10.2 days | The mean length of hospital stay in the intervention group was 2.00 days shorter (2.82 to 1.18 shorter) | 102 (1 study) | ⊕⊕⊝⊝ low1 | ||
| Costs Costs at maximal follow‐up | The mean cost in the control group was EUR 139 | The mean cost in the intervention groups was EUR 36.00 lower (59.81 to 12.19 lower) | 102 (1 study) | ⊕⊕⊝⊝ low1 | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate Very low quality: we are very uncertain about the estimate | ||||||
1 High risk of bias in all domains 2 < 300 events in total in both groups 3 95% confidence interval includes both 0.75 and 1.25
Background
Description of the condition
Most surgical procedures involve a cut in the skin that allows the surgeon to gain access to the deeper tissues or organs. Most surgical wounds are closed fully at the end of the procedure.This is called primary closure (Garcia‐Gubern 2010). The various techniques for wound closure include closure using sutures, staples, adhesive tapes and tissue glue (Ahn 2011; Biancari 2010; Hasan 2009). Primary closure is essential to restore the skin barrier, which prevents infection of deeper tissues. However, it is not always possible to maintain clean conditions throughout surgery, for example, when operating on a contaminated wound (external wounds resulting from trauma) or when operating on tissues that contain contaminated material (e.g. surgery on the colon, which contains faecal material). In these situations it is sometimes best to delay closure of the wound until the wound develops good granulation tissue, and this is called secondary closure (Garcia‐Gubern 2010).
Various factors affect wound healing, such as infection or mechanical strain leading to wound dehiscence (breakdown of wound along the incision), wound infection (currently termed 'surgical site infection') or both. Three types of surgical site infections (SSIs) have been classified: they are defined as 1) superficial incisional surgical site infections that involve only the skin or subcutaneous tissue around the incision, 2) deep incisional surgical site infections that involve deep soft tissues, such as the fascia and muscles (both occurring within 30 days of procedure, or one year in the case of implants), and 3) organ/space surgical site infections that involve any part of the body (excluding the skin incision, fascia or muscle layers) that is opened or manipulated during the operative procedure (Horan 1992). The incidence of SSI varies according to the classification of surgical wounds. Surgical wounds can be classified in different ways. One accepted classification that has been adopted by the Centers for Disease Prevention and Control (CDC) is to define wounds as clean, clean‐contaminated, contaminated, and dirty or infected (Garner 1986). This classification is shown in Appendix 1. The incidence of SSI can vary between 1% and 80% depending upon the types of surgery, the hospital setting (community hospital, tertiary‐care hospital, etc), the classification of surgical wounds, and the method of skin closure (Biancari 2010; Broex 2009; Garner 1986). It is estimated that the presence of SSI can double the costs of surgery (Broex 2009). Some of the methods used to prevent SSI include administration of prophylactic antibiotics and dressing of wounds.
Description of the intervention
Surgeons cover closed surgical wounds using either a dressing or adhesive tape (steri‐strips), or both. Wound dressings are classified in a number of ways according to their function (e.g. occlusive, absorbent), type of material (e.g. hydrocolloid, collagen) and the physical form of the dressing (e.g. ointment, film, foam) (Boateng 2008). Some dressings are designed to control the environment for wound healing, for example, to donate fluid (hydrogels), maintain hydration (hydrocolloids), or to absorb wound exudates (alginates, foams) (BNF 2011). These dressings can be either transparent (e.g. vapour‐permeable films), so that the wound can be monitored without the need for frequent dressing changes, or non‐transparent. Wound dressings are customarily left in place for at least 48 hours after surgery (delayed dressing removal) irrespective of the level of contamination of wounds, or other factors such as antibiotic administration.
How the intervention might work
Dressings can act as a physical barrier to protect wounds until the continuity of the skin (epithelialisation) has been achieved ‐ this occurs within about 48 hours of surgery (Lawrence 1998) ‐ and to absorb exudate from the wound, keeping it dry and clean with the aim of avoiding bacterial contamination from the external environment (Hutchinson 1991; Mertz 1985; Ubbink 2008). Another reason for using a dressing is to prevent contamination of the surrounding area by any wound discharge (Downie 2010), although this is mainly applicable for clean‐contaminated, contaminated, and dirty or infected wounds. Some studies have found that the moist environment created by some dressings accelerates wound healing (Dyson 1988), although others believe that it is a disadvantage, as excessive exudate can cause maceration (softening and breakdown) of the wound and the surrounding healthy tissue (Cutting 2002). Ideally surgeons choose suitable dressings to ensure that the wound remains:
free of clinical infection and excessive slough;
free of toxic chemicals, particles or fibres;
at the optimum temperature for healing;
undisturbed by the need for frequent changes;
at the optimum pH value.
As wound healing progresses, it may be appropriate to use different types of dressings (BNF 2011).
Why it is important to do this review
Dressings applied to surgical wounds at the time of surgery can either be removed early, changed regularly, or retained until the removal of sutures or strips. This may cause inconvenience to the patient and increase nursing time, with an inevitable increase in associated costs (Chrintz 1989; Dosseh 2008; Merei 2004). In simulated wounds, where dressings increase the chance of localised sweating and can reduce moisture evaporation, the resulting increased dampness potentially acts as a nidus (point at which micro‐organisms enter the body) for infection (Gwosdow 1993). Thus, there are some potential disadvantages to delaying dressing removal. There has been no systematic review of early dressing removal (permanent dressing removal within 48 hours after surgery) versus delayed dressing removal (permanent dressing removal 48 hours after surgery with dressing changes allowed in the interim) for surgical wounds.
Objectives
To evaluate the benefits and risks of removing a dressing covering a closed surgical incision site within 48 hours (early dressing removal) or beyond 48 hours (delayed dressing removal) of surgery, on surgical site infection.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised clinical trials (RCTs), irrespective of their use of blinding, language of publication, publication status, date of publication, study setting or sample size. We included cluster RCTs provided that the effect estimate, after adjusting for the cluster effect, was available. We excluded quasi‐randomised studies (where the methods of allocating participants to a treatment are not strictly random, for example, based on date of birth, hospital record number, alternation) and other study designs.
Types of participants
People, of any age and sex, undergoing a surgical procedure (major, minor or day‐case procedure) who had their wound closed (primary wound closure), irrespective of the material and method used for the primary closure and the location of the wound. We excluded trials that included people with contaminated or dirty (infected) wounds unless separate information was provided for the clean and clean‐contaminated wounds.
Types of interventions
When wound dressings are used they are almost always applied immediately after surgery. We included trials comparing the permanent removal of the wound dressing within 48 hours after surgery (early group) with continued dressing of the wound beyond 48 hours with interim dressing changes allowed (delayed group). We made no differentiation in the type of dressing and whether the dressing applied at the time of surgery was retained or changed. Co‐interventions were allowed (e.g. antibiotics, wound drainage, etc.), provided that they were used equally across all groups.
Types of outcome measures
Primary outcomes
-
Surgical site infection (SSI) within 30 days of operation. We attempted to use the definition of SSI that matches the standard definition of SSI described by Horan 1992. Otherwise, we accepted the definitions used by the trial authors.
Superficial SSI.
Deep SSI.
-
Wound dehiscence within 30 days of operation. Postoperative wound dehiscence is the term given to wound disruptions that result from poor wound healing; it is caused by a variety of factors, such as type of incision, infection, anaemia, diabetes, ascorbic acid deficiency, etc. (Keill 1973). Wound dehiscence is classified as:
superficial (dehiscence involving skin and subcutaneous tissue); or
deep (burst abdomen).
Other serious adverse events within 30 days of operation, defined as any event that would increase mortality; is life‐threatening; requires inpatient hospitalisation or prolongation of existing hospitalisation; results in a persistent or significant disability or incapacity; or any important medical event that might have jeopardised the person, or requires intervention to prevent it (ICH‐GCP 1996). We recognised that the main role of dressings is to prevent wound‐related complications, but we wanted to assess the impact of dressings in the overall context of the operation.
Secondary outcomes
Quality of life at maximal follow‐up (however defined by authors).
Length of hospital stay at maximal follow‐up.
Time taken to return to work.
Costs at maximal follow‐up (however reported by authors).
Search methods for identification of studies
Electronic searches
For this first update we searched:
The Cochrane Wounds Group Specialized Register (Searched 24/03/15)
The Cochrane Central Register of Controlled Trials (CENTRAL) ‐ The Cochrane Library 2015, Issue 2
Ovid MEDLINE & Ovid MEDLINE ‐ In‐Process & Other Non‐Indexed Citations 2013 to March 23 2015
Ovid EMBASE ‐ 2013 to March 23 2015
EBSCO CINAHL ‐ 2013 to March 24 2015
The search strategies for Ovid MEDLINE, Ovid EMBASE and EBSCO CINAHL can be found in Appendix 1. We combined the Ovid MEDLINE search with the Cochrane Highly Sensitive Search Strategy for identifying randomised trials in MEDLINE: sensitivity‐ and precision‐maximising version (2008 revision) (Lefebvre 2011). We combined the EMBASE and CINAHL searches with the trial filters developed by the Scottish Intercollegiate Guidelines Network (SIGN 2013). We did not restrict studies with respect to language, date of publication or study setting.
We used the following search strategy in The Cochrane Central Register of Controlled Trials (CENTRAL):
#1 MeSH descriptor Bandages explode all trees #2 (dressing* or hydrocolloid* or alginate* or hydrogel* or "foam" or "bead" or "film" or "films" or tulle or gauze or non‐adherent or "non adherent" or silver or honey or matrix):ti,ab,kw #3 (#1 OR #2) #4 MeSH descriptor Surgical Wound Infection explode all trees #5 MeSH descriptor Surgical Wound Dehiscence explode all trees #6 surg* NEAR/5 infect*:ti,ab,kw #7 surg* NEAR/5 wound*:ti,ab,kw #8 surg* NEAR/5 site*:ti,ab,kw #9 surg* NEAR/5 incision*:ti,ab,kw #10 surg* NEAR/5 dehiscen*:ti,ab,kw #11 wound* NEAR/5 infect*:ti,ab,kw #12 wound* NEAR/5 dehiscen*: ti,ab,kw #13 (#4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12) #14 (#3 AND #13)
The search strategies used for the original version of this review are detailed in Appendix 3.
Searching other resources
We did not undertake any additional searches for this update.
Data collection and analysis
We performed the systematic review following instructions in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a).
Selection of studies
We did not apply any restrictions regarding language or publication status of trial reports. Two review authors (CT and KG) independently read the titles and abstracts of potentially‐relevant reports identified by the searches, and decided which references should be retrieved in full. We sought the full text for any reference that at least one review author considered was likely to meet the inclusion criteria. Final decisions on inclusion or exclusion of studies were based on reading the full text. We also listed the excluded studies with reasons for their exclusion (Characteristics of excluded studies).
Data extraction and management
Two review authors (CT and KG) extracted the following data independently.
Year and language of publication.
Country of conduct of the trial.
Year of conduct of the trial.
Inclusion and exclusion criteria.
Sample size.
Anatomical location of wound.
Type of operation (primary closure versus secondary closure; actual operation; clean or clean contaminated wound).
Type of wound closure.
Type of dressing (occlusive versus non‐occlusive; moist versus dry; manufacturer's name; type of material).
Co‐morbidities in participants (for example, diabetes).
Antibiotics used.
Outcome data for primary and secondary outcomes (by group).
Duration of follow‐up.
Number of withdrawals (by group).
Assessment of risk of bias (as described below).
We sought further information from trial authors when sufficient information was not available in the report. In future, if multiple reports exist for a trial, we will examine all the reports for information (on this occasion there were no multiple reports for the included trials). If there is any doubt about whether the trials share the same participants ‐ completely or partially (by identifying common authors and centres) ‐ we plan to contact the trial authors to check whether the trial report has been duplicated, and to seek clarification for any unclear or missing information. We resolved any differences in opinion through discussion amongst the review authors.
Assessment of risk of bias in included studies
We followed instructions in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b). According to empirical evidence (Kjaergard 2001; Moher 1998; Schulz 1995; Wood 2008), we assessed the risk of bias of included trials based on the following risk of bias domains:
Sequence generation
Low risk of bias: the method used was either adequate (e.g. computer‐generated random numbers, table of random numbers) or unlikely to introduce confounding.
Unclear risk of bias: there was insufficient information to assess whether the method used was likely to introduce confounding.
High risk of bias (the method used was improper and likely to introduce confounding (e.g. quasi‐randomised studies)). We excluded such studies.
Allocation concealment
Low risk of bias: the method used was unlikely to induce bias on the final observed effect (e.g. central allocation).
Unclear risk of bias: there was insufficient information to assess whether the method used was likely to induce bias on the estimate of effect.
High risk of bias: the method used was likely to induce bias on the final observed effect (e.g. open random allocation schedule).
Blinding of participants and personnel
It was impossible to blind the participants, so, we classified patient‐reported outcomes such as quality of life at high risk of bias, as this is a subjective outcome and a person's belief may influence the reporting of quality of life. However, it was possible to blind the healthcare providers. So, we considered outcomes that were not reported by participants as follows.
Low risk of bias: blinding was performed adequately, or the outcome measurement was not likely to be influenced by lack of blinding.
Unclear risk of bias: there was insufficient information to assess whether the type of blinding used was likely to induce bias on the estimate of effect.
High risk of bias: no blinding or incomplete blinding, and the outcome or outcome measurement was likely to be influenced by lack of blinding.
Blinding of outcome assessors
Low risk of bias: blinding was performed adequately, or the outcome measurement was not likely to be influenced by lack of blinding.
Unclear risk of bias: there was insufficient information to assess whether the type of blinding used was likely to induce bias on the estimate of effect.
High risk of bias: no blinding or incomplete blinding, and the outcome or the outcome measurement was likely to be influenced by lack of blinding.
Incomplete outcome data
Low risk of bias: the underlying reasons for missing data were unlikely to make treatment effects depart from plausible values, or proper methods were employed to handle missing data.
Unclear risk of bias: there was insufficient information to assess whether the missing data mechanism in combination with the method used to handle missing data was likely to induce bias on the estimate of effect.
High risk of bias: the crude estimate of effect was clearly biased due to the underlying reasons for missing data, and the methods used to handle missing data were unsatisfactory (e.g. complete case estimate).
Selective outcome reporting
Low risk of bias: the trial protocol was available and all of the trial's pre‐specified outcomes that were of interest to this review were reported; if the trial protocol was not available, all the primary outcomes in this review were reported.
Unclear risk of bias: there was insufficient information to assess whether the magnitude and direction of the observed effect was related to selective outcome reporting.
High risk of bias: not all of the trial's pre‐specified primary outcomes were reported.
We considered trials that were classified as being at low risk of bias in all the above domains as 'low bias‐risk trials'. We considered the other trials to be at unclear risk of bias (if at least one of the domains was at unclear risk of bias and none of the domains was at high risk of bias) or 'high bias‐risk trials' (if at least one of the domains was at high risk of bias).
Measures of treatment effect
For dichotomous variables, we calculated the risk ratio (RR) with 95% confidence intervals (CI). For continuous variables, we calculated the mean difference (MD) with 95% CI for outcomes that could be quantified, such as hospital stay and return to work, and planned to calculate the standardised mean difference (SMD) with 95% CI for outcomes such as quality of life where different assessment scales may have been used in different studies. We also reported the results of risk difference (RD) if they were different from those of risk ratio. This is because the risk difference takes account of trials with an absence of events in both treatment groups, while risk ratio does not include such trials in the meta‐analysis.
Unit of analysis issues
We included simple RCTs of parallel design. The unit of analysis was the individual person. We did not anticipate or identify any cluster‐RCTs. We excluded trials of other designs, such as cross‐over trials.
Dealing with missing data
We planned to perform an intention‐to‐treat analysis whenever possible (Newell 1992). We planned to impute data for binary outcomes using various scenarios such as best‐best scenario, worst‐worst scenario, best‐worst scenario, and the worst‐best scenario (Gurusamy 2009). In the best‐best scenario, participants with missing outcome data would be considered not to have developed a complication. In the worst‐worst scenario, participants with missing outcome data would be considered to have developed a complication. In the best‐worst scenario, participants with missing outcome data in the intervention group would be considered not to have developed a complication, while those in the control group would be considered to have developed a complication. In the worst‐best scenario, participants with missing outcome data would be considered to have developed a complication in the intervention group and not to have developed a complication in the control group.
For continuous outcomes, we planned to use the available‐case analysis where intention‐to‐treat analysis was not possible. We planned to impute the standard deviation from P values according to instructions in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011c), and to use the median for the meta‐analysis when the mean was not available. Where it was not possible to calculate the standard deviation from the P value or the confidence intervals, we planned to impute the standard deviation as the highest standard deviation in the other trials included under that outcome, fully recognising that this form of imputation decreases the weight of the study for calculation of mean differences and bias the effect estimate towards no effect in case of standardised mean difference (Higgins 2011d).
Assessment of heterogeneity
We explored heterogeneity by the Chi2 test with the threshold for statistical significance set at P value 0.10, and measured the quantity of heterogeneity by the I2 statistic (Higgins 2002).
Thresholds for the interpretation of the I2 statistic can be misleading. A rough guide to interpretation is as follows (Deeks 2011).
0% to 40%: might not be important.
30% to 60%: may represent moderate heterogeneity.
50% to 90%: may represent substantial heterogeneity.
75% to 100%: represents considerable heterogeneity.
Assessment of reporting biases
If we had included at least 10 trials, we planned to use visual asymmetry on a funnel plot to explore reporting bias (Egger 1997; Macaskill 2001). We had also planned to perform the linear regression approach described by Egger 1997 to determine the funnel plot asymmetry.
Data synthesis
We performed the meta‐analysis using RevMan 5 software (RevMan 2011), and followed the recommendations of The Cochrane Collaboration (Deeks 2011). We used both a random‐effects model (DerSimonian 1986), and fixed‐effect model (DeMets 1987), of meta‐analysis. We planned to report both results where we identified discrepancy between the two models from the pooled estimates and their confidence intervals, resulting in a change in conclusions. However, we did not find any such outcomes, so have reported the results of the fixed‐effect model. With regard to dichotomous outcomes, risk ratio calculations do not include trials in which no events occurred in either group in the meta‐analysis, whereas risk difference calculations do. We planned to report the risk difference (RD) if the results using this association measure were different from risk ratio in terms of statistical significance. However, risk ratio is the measure that we have used to derive conclusions, since risk ratios perform better when there are differences in the control event rate (proportion of people who develop the event in the control group(s)).
Summary of findings
We have presented the 'Table 1' for all the reported primary and secondary outcomes (Schünemann 2011).
Subgroup analysis and investigation of heterogeneity
We planned to perform the following subgroup analyses in the presence of an adequate number of trials.
Trials with low risk of bias (considered to be at low risk of bias in all the risk of bias domains) compared to trials with high or unclear risks of bias.
Based on the type of dressing (dry, moist, occlusive, absorbent) (some types of dressings may be useful while other types of dressings may not be useful).
Based on type of surgery (trunk versus extremities) (wound healing rates may be different in the trunk and extremities, particularly in people who have peripheral vascular diseases).
Based on type of wound closure (sutures versus staples versus adhesive tapes). Dressings may be useful in some types of wound closure while they may not be useful in other forms.
Based on degree of contamination (clean versus clean‐contaminated). Dressings may be useful in clean‐contaminated wounds because they absorb exudate, while they may not be useful in clean wounds.
Antibiotic treatment up to 48 hours after surgery versus antibiotic treatment for more than 48 hours after surgery (i.e. continuation of antibiotic after removal of dressing in the early group). Antibiotics may eradicate bacteria, even in wounds that become contaminated, in which they may prevent infection.
However, there were not enough eligible studies in each subgroup to allow for this.
Sensitivity analysis
We performed sensitivity analysis by imputing data for dichotomous outcomes using various scenarios including best‐best scenario, worst‐worst scenario, best‐worst scenario and worst‐best scenario (Gurusamy 2009). We planned to perform a sensitivity analysis by excluding the trials in which the mean and the standard deviation were imputed.
Results
Description of studies
Results of the search
A total of 2513 references were identified through the searches detailed previously. We excluded 342 duplicates and 2161 irrelevant references by going through titles and abstracts, leaving eleven references for full assessment. We obtained full texts for these references. Seven references (six studies) were excluded for the reasons outlined in the Characteristics of excluded studies table. This left four trials for inclusion in this review (Ajao 1977; Dosseh 2008; Ramkumar 2006; Wipke‐Tevis 1998). No further trials were identified through searching the references of the included trials. The reference flow is shown in Figure 1.
1.
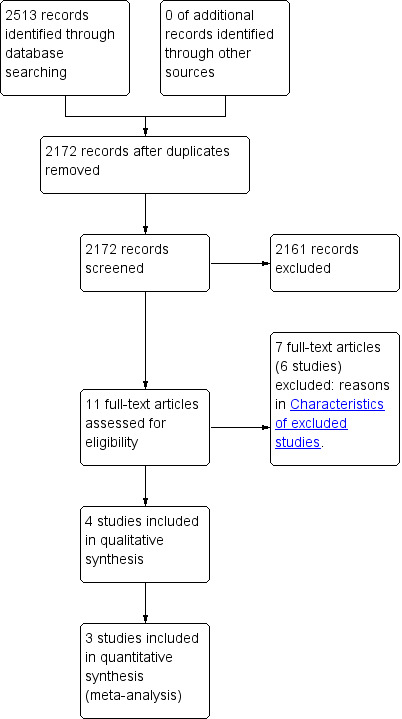
Reference Flow
Included studies
(See Characteristics of included studies table)
A total of 317 participants were included in this systematic review. Ten were lost to follow‐up. Of the remaining participants, 147 were randomised to the early dressing removal group (removal of the wound dressing within 48 hours after surgery) and the remaining 160 participants were randomised to the delayed dressing removal group (continued dressing of the wound beyond 48 hours). The trials included a variety of surgical procedures in one trial (no details about them) (Ajao 1977); various abdominal surgeries, cervical surgeries and thoracic surgeries in another (Dosseh 2008); correction of prominent ears in a third (Ramkumar 2006); and saphenous vein‐graft harvesting in patients undergoing coronary artery bypass graft surgery in the fourth (Wipke‐Tevis 1998). Routine antibiotics were not used in one trial (Ajao 1977), while in another prophylactic antibiotics were used for a period not exceeding 24 hours after surgery (Dosseh 2008). No information about antibiotic use was available from the other two trials (Ramkumar 2006; Wipke‐Tevis 1998). Early dressing removal was performed within 24 hours of surgery in Ramkumar 2006 and Wipke‐Tevis 1998; between 24 to 36 hours in Ajao 1977; and at 48 hours in Dosseh 2008. Delayed dressing removal was performed in seven to 10 days in Ajao 1977; 10 days in Ramkumar 2006; and at suture removal in Dosseh 2008 and Wipke‐Tevis 1998.
Three trials including 280 participants randomised to the early dressing removal group (140 participants) and delayed dressing removal group (140 participants) provided data for this review (Ajao 1977; Dosseh 2008; Ramkumar 2006) (Figure 1).
Excluded studies
(See Characteristics of excluded studies table for details.) Four studies were excluded for the following reasons: two studies were quasi‐randomised (Chrintz 1989; Meylan 2001); one was an RCT that compared different types of dressing against no dressing (i.e. the wound was not covered with a dressing immediately after surgery) (Law 1987); one did not compare early vs delayed dressing (Springer 2013); and one was not a randomised controlled trial (Edwards 1967). We also identified a summary report about an excluded study (Chrintz 1989) and a commentary on this review (Lisy 2014).
Risk of bias in included studies
All the trials were at high risk of bias. The proportion of trials with different classifications of risk of bias is shown in Figure 2, and the classification of domains in individual trials is shown in Figure 3.
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
3.
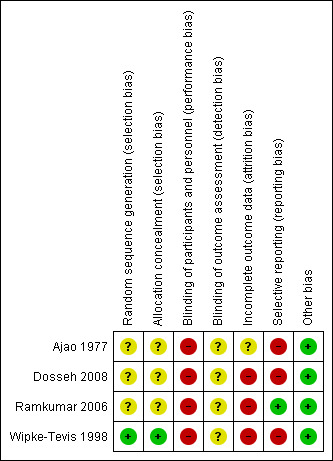
Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Allocation
One trial had a low risk of bias due to sequence generation (Wipke‐Tevis 1998), it also had a low risk of bias due to allocation concealment. The other three trials were assessed as being at unclear risk of bias.
Blinding
None of the trials had a low risk of bias due to an absence of blinding of participants, healthcare providers or outcome assessors.
Incomplete outcome data
None of the trials were at low risk of bias due to incomplete outcome data.
Selective reporting
Only one trial reported wound complications and serious adverse events, and was considered to be at low risk of bias for selective reporting (Ramkumar 2006).
Effects of interventions
See: Table 1
The results from the meta‐analysis are outlined in the Data and analyses and Table 1. Only seven outcomes were reported in the included trials.
1. Superficial surgical site infection within 30 days
Superficial surgical site infection (SSI) within 30 days of surgery was reported by Ajao 1977; Dosseh 2008 and Ramkumar 2006. Overall, 26/280 participants (9.3%) in the three trials developed SSI. There was no significant difference in the proportion of people who developed SSI between the early dressing removal group and the delayed dressing removal group (RR 0.64; 95% CI 0.32 to 1.28) (Analysis 1.1). There was no significant heterogeneity (I2 = 0%; Chi2 P value 0.88).
1.1. Analysis.
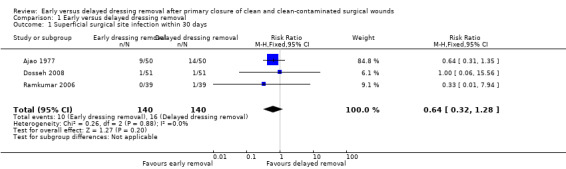
Comparison 1 Early versus delayed dressing removal, Outcome 1 Superficial surgical site infection within 30 days.
2. Deep surgical site infection within 30 days
Deep SSI was only reported by Dosseh 2008. No deep SSIs were reported in either the early or delayed dressing removal groups in this trial.
3. Superficial wound dehiscence within 30 days
Dosseh 2008 and Ramkumar 2006 presented data on superficial wound dehiscence within 30 days of surgery. Overall, 3/180 participants (1.7%) developed superficial wound dehiscence. There was no significant difference in the proportion of people who developed superficial wound dehiscence between the early and delayed dressing removal groups (RR 2.00; 95% CI 0.19 to 21.16) (Analysis 1.2). We could not assess heterogeneity, because there was no superficial wound dehiscence in either group in one trial (Dosseh 2008).
1.2. Analysis.
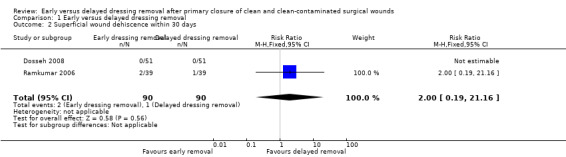
Comparison 1 Early versus delayed dressing removal, Outcome 2 Superficial wound dehiscence within 30 days.
4. Deep wound dehiscence within 30 days
Deep wound dehiscence within 30 days of surgery was reported by both Dosseh 2008 and Ramkumar 2006. No deep wound dehiscences were reported in either the early or delayed dressing removal groups in these trials.
5. Serious adverse events at 30 days
Serious adverse events at 30 days after surgery were reported by only one of the included trials (Ramkumar 2006). Overall 11/78 participants (14.1%) developed serious adverse events such as skin necrosis, wound dehiscence, haematomas, SSIs, and maceration of the wound. No significant difference was noted in the proportion of people developing serious adverse events between the early dressing removal group and the delayed dressing removal group (RR 0.83; 95% CI 0.28 to 2.51) (Analysis 1.3).
1.3. Analysis.

Comparison 1 Early versus delayed dressing removal, Outcome 3 Patients with serious adverse events at 30 days.
6. Length of hospital stay at maximal follow‐up
Length of hospital stay at maximal follow‐up was reported by Dosseh 2008. The length of hospital stay was statistically significantly shorter for participants in the early dressing removal group than those in the delayed dressing removal group (MD ‐2.00 days; 95% CI ‐2.82 to ‐1.18) (Analysis 1.4).
1.4. Analysis.
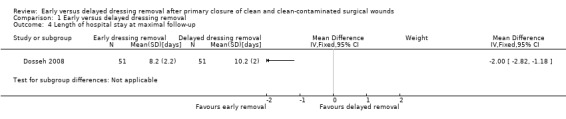
Comparison 1 Early versus delayed dressing removal, Outcome 4 Length of hospital stay at maximal follow‐up.
7. Total costs at maximal follow‐up
Only Dosseh 2008 reported total costs at maximal follow‐up. Costs related to the procedure and hospitalisation were significantly lower for participants in the early dressing removal group than in the delayed dressing removal group (MD (EUR) ‐36.00; 95% CI ‐59.81 to ‐12.19) (Analysis 1.5).
1.5. Analysis.

Comparison 1 Early versus delayed dressing removal, Outcome 5 Costs at maximal follow‐up.
Additional information
No differences were noted between the random‐effects model and fixed‐effect model. Therefore, only the fixed‐effect data have been reported here. There was no change in the interpretation of results when risk difference was used for binary outcomes.
Subgroup analysis
Subgroup analysis was not performed because of the low number of trials included in this review.
Sensitivity analysis
There was no change in the results when different scenarios were used in the Dosseh 2008 trial in which three people in the delayed dressing group who did not receive dressing (patients refused to have any dressing) were excluded from the analysis (Analysis 1.6; Analysis 1.7). In the two remaining trials that reported post‐randomisation drop‐outs, one trial did not report the group from which they dropped‐out (Ramkumar 2006), and the other trial did not report any of the outcomes of interest (Wipke‐Tevis 1998), so was not included in any of the sensitivity analysis. We did not impute the mean and standard deviation for any of the trials, so we did not perform any sensitivity analysis for continuous outcomes.
1.6. Analysis.
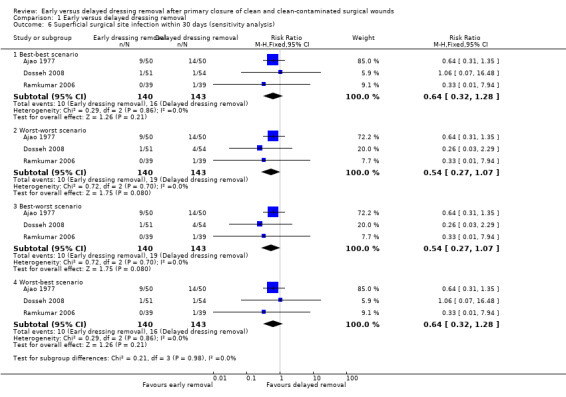
Comparison 1 Early versus delayed dressing removal, Outcome 6 Superficial surgical site infection within 30 days (sensitivity analysis).
1.7. Analysis.
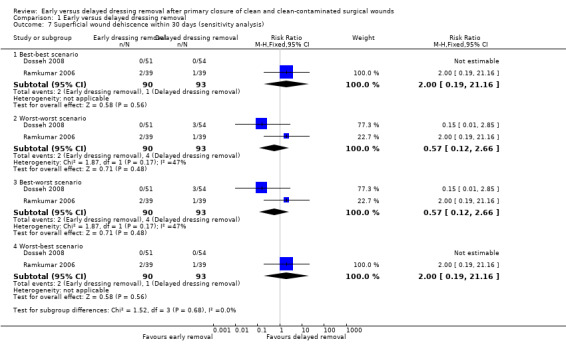
Comparison 1 Early versus delayed dressing removal, Outcome 7 Superficial wound dehiscence within 30 days (sensitivity analysis).
Reporting bias
We did not explore reporting bias because of the presence of fewer than 10 trials in the review.
Discussion
Summary of main results
This review compared the effects of early versus delayed dressing removal on a variety of outcomes, including surgical site infections (SSI), length of hospital stay and overall costs. While four trials were identified for inclusion in this review (Ajao 1977; Dosseh 2008; Ramkumar 2006; Wipke‐Tevis 1998), only three trials contributed to the meta‐analysis (Ajao 1977; Dosseh 2008; Ramkumar 2006). These trials included people undergoing assorted surgical procedures (Ajao 1977); abdominal, cervical or thoracic surgery (Dosseh 2008); unilateral or bilateral primary correction of prominent ears (Ramkumar 2006); and coronary artery bypass graft surgery with saphenous vein grafts (Wipke‐Tevis 1998). The people in the early dressing removal group removed their dressing up to 48 hours after surgery. Those in the delayed dressing removal group continued dressing the wound beyond 48 hours. It was possible to extract data for the following outcomes: both superficial and deep SSI, both superficial and deep wound dehiscence, number of people with adverse events, length of hospital stay, and total costs. None of the trials reported quality of life or time to return to work. There were no significant differences between the groups in terms of incidence of SSIs, wound dehiscence or serious adverse events. The length of hospital stay was two days shorter and the costs were EUR 36 cheaper in the early dressing removal group than the delayed dressing removal group in the only trial that reported this outcome (Dosseh 2008). This trial included direct costs, which included the intervention and the hospitalisation in Togo. Hospital stay is likely to cost more in Western countries. For example, one additional day in hospital costs approximately GBP 250 in the United Kingdom (NHS reference costs 2012).
In the absence of evidence of a difference in complications between the two groups, the shorter hospital stay and the lower costs are likely to be due to the dressing rather than a difference in complications. However one cannot rule out differences in complications, since the trials were not powered to measure these differences. Even if patients are discharged home with further instructions for dressings with the general practitioner (GP) or GP‐nurse or a nurse who visits the home, this will involve costs. If the hospital stay is likely to be longer than 48 hours for surgical reasons (rather than for dressing the wound), dressing the wound involves time for the ward staff. So, irrespective of the setting, dressing beyond 48 hours involves resources other than the cost of the dressings. If this is not balanced by a decrease in the complications, there appears to be no evidence to support dressing surgical wounds beyond 48 hours.
Overall completeness and applicability of evidence
None of the studies reported health‐related quality of life. It is important to measure the quality of life in future trials.
The findings of this review can only be applied to people with clean or clean‐contaminated surgical wounds closed by primary intention. It is not clear whether or not these findings can be applied to people with accidental injuries, or for those people undergoing delayed primary closure.
Quality of the evidence
The overall quality of the evidence is low or very low as shown in Table 1. Most of the results are based on one or two trials. However, it must be pointed out that this is the best available evidence on this topic. Evidence from observational studies may be even more unreliable, since the participants in whom wound complications are not expected to develop because of various factors including co‐morbidities, type of living environment, their ability to keep the wound clean, and the type of surgery performed, may influence the decision to remove the dressing early or late. Such selection bias can result in biased effect estimate.
Potential biases in the review process
Although we performed a thorough review of published literature and current trials, it is possible that some authors have conducted relevant trials in the pre‐registration era and have not reported the results. There are various potential sources of heterogeneity including types of dressing, surgery, and wound closure; degree of contamination; and duration of antibiotic treatment, as mentioned in the 'Subgroup analysis and investigation of heterogeneity' section. However, heterogeneity could not be explored because of the low number of trials included in this review, so the impact of these factors on the effect estimate could not be explored.
Agreements and disagreements with other studies or reviews
This is the first review on this topic. Overall, the trials concluded that wounds can be uncovered within the first 48 hours following surgery with no ill effect. It was also concluded that when dressings were removed within the first 48 hours, people spent significantly less time in hospital and the overall cost of their treatment was significantly reduced compared to people whose wounds were covered beyond the first 48 hours following surgery. While the authors of the individual trials interpreted this to mean that there was no need for dressing beyond the first 48 hours following surgery, we interpret this information with a little more caution and conclude that there is currently no evidence for dressings beyond the first 48 hours and that dressing need not be used for more than 48 hours following surgery involving clean and clean, contaminated wounds until further research shows otherwise.
Authors' conclusions
Implications for practice.
The early removal of the dressing from a clean or clean‐contaminated surgical wound appears to have no detrimental effect on the patient. However, it must be noted that the point estimate that supports this conclusion is based on very low quality evidence from three small randomised controlled trials, and that the confidence intervals around this estimate were wide. Furthermore, early dressing removal may result in a significantly shorter hospital stay and significantly reduced costs than covering the surgical wound with a wound dressing beyond the first 48 hours after surgery based on very low quality evidence from one small randomised controlled trial.
Implications for research.
Further randomised controlled trials of low risk of bias are necessary to investigate whether dressings are necessary after 48 hours in different types of surgery and levels of contamination and investigate whether antibiotic therapy influences the outcome
What's new
| Date | Event | Description |
|---|---|---|
| 25 March 2015 | New citation required but conclusions have not changed | New author added. No change to conclusions. |
| 25 March 2015 | New search has been performed | fist update, new search, no new trials identified. |
Acknowledgements
This project was funded by the National Institute for Health Research. Disclaimer of the Department of Health: 'The views and opinions expressed in the review are those of the authors and do not necessarily reflect those of the National Institute for Health Research (NIHR), National Health Services (NHS), or the Department of Health.'
We acknowledge the help and support of the Cochrane Wounds Group. The authors would also like to thank the following editors and peer referees who provided comments to improve the protocol: Susan O'Meara (editor), Evangelos Kontopantelis and Iain McCallum and to Jenny Bellorini for copy editing the protocol. The authors would also like to thank the following editors and peer referees who provided comments to improve the review: Susan O'Meara (editor), Nerys Woolacott, Evan Kontopantelis and AG Radhika and to Elizabeth Royle for copy editing the review.
Appendices
Appendix 1. Classification of surgical wounds
Clean wound
|
Clean‐contaminated wound
|
Contaminated wound
|
Dirty wound
|
Appendix 2. Search strategies for Ovid MEDLINE, Ovid EMBASE and EBSCO CINAHL
Ovid MEDLINE
1 exp Bandages/ (9807) 2 (dressing* or hydrocolloid* or alginate* or hydrogel* or foam or bead or film or films or tulle or gauze or non‐adherent or non adherent or silver or honey or matrix).tw. (240450) 3 or/1‐2 (246412) 4 exp Surgical Wound Infection/ (11510) 5 exp Surgical Wound Dehiscence/ (2940) 6 (surg* adj5 infect*).tw. (10880) 7 (surg* adj5 wound*).tw. (5622) 8 (surg* adj5 site*).tw. (7971) 9 (surg* adj5 incision*).tw. (4199) 10 (surg* adj5 dehiscen*).tw. (369) 11 (wound* adj5 infect*).tw. (12760) 12 (wound* adj5 dehiscen*).tw. (1771) 13 or/4‐12 (42204) 14 3 and 13 (2416) 15 randomized controlled trial.pt. (238104) 16 controlled clinical trial.pt. (39335) 17 randomized.ab. (193802) 18 placebo.ab. (90703) 19 clinical trials as topic.sh. (79028) 20 randomly.ab. (133232) 21 trial.ti. (71766) 22 or/15‐21 (538944) 23 (animals not (humans and animals)).sh. (1600596) 24 22 not 23 (490866) 25 14 and 24 (338)
Ovid EMBASE
1 exp "bandages and dressings"/ (19981) 2 (dressing* or hydrocolloid* or alginate* or hydrogel* or foam or bead or film or films or tulle or gauze or non‐adherent or non adherent or silver or honey or matrix).tw. (338426) 3 or/1‐2 (352047) 4 exp surgical infection/ (14084) 5 exp wound dehiscence/ (6698) 6 (surg* adj5 infect*).tw. (16176) 7 (surg* adj5 wound*).tw. (7956) 8 (surg* adj5 site*).tw. (11964) 9 (surg* adj5 incision*).tw. (6371) 10 (surg* adj5 dehiscen*).tw. (513) 11 (wound* adj5 infect*).tw. (18470) 12 (wound* adj5 dehiscen*).tw. (2527) 13 or/4‐12 (62660) 14 3 and 13 (3718) 15 Randomized controlled trials/ (22561) 16 Single‐Blind Method/ (15215) 17 Double‐Blind Method/ (84665) 18 Crossover Procedure/ (31187) 19 (random$ or factorial$ or crossover$ or cross over$ or cross‐over$ or placebo$ or assign$ or allocat$ or volunteer$).ti,ab. (918967) 20 (doubl$ adj blind$).ti,ab. (88438) 21 (singl$ adj blind$).ti,ab. (9428) 22 or/15‐21 (951325) 23 animal/ (716482) 24 human/ (8445003) 25 23 not 24 (478203) 26 22 not 25 (919579) 27 14 and 26 (506)
EBSCO CINAHL
S15 S3 and S14 S14 S4 or S5 or S6 or S7 or S8 or S9 or S10 or S11 or S12 or S13 S13 TI wound* N5 dehiscen* or AB wound* N5 dehiscen* S12 TI wound* N5 infection* or AB wound* N5 infection* S11 TI surg* N5 dehiscen* or AB surg* N5 dehiscen* S10 TI surg* N5 incision* or AB surg* N5 incision* S9 TI surg* N5 site* or AB surg* N5 site* S8 TI surg* N5 wound* or AB surg* N5 wound* S7 TI surg* N5 infection* or AB surg* N5 infection* S6 (MH "Surgical Wound") S5 (MH "Surgical Wound Dehiscence") S4 (MH "Surgical Wound Infection") S3 S1 and S2 S2 TI (dressing* or hydrocolloid* or alginat* or hydrogel or foam* or bead or gauze or tulle or film or films or gauze or non‐adherent or non adherent * or silver or honey or matrix) or AB (dressing* or hydrocolloid* or alginat* or hydrogel or foam* or bead or gauze or tulle or film or films or gauze or non‐adherent or non adherent * or silver or honey or matrix) S1 (MH "Bandages and Dressings+")
Trial registries (mRCT and ICTRP)
early AND dressing
Appendix 3. Search strategy for original review
In July 2013 we searched the following electronic databases to identify reports of relevant randomised clinical trials:
Cochrane Wounds Group Specialised Register (searched 11 July 2013);
The Cochrane Central Register of Controlled Trials (CENTRAL) (2013, Issue 6);
Database of Abstracts of Reviews of Effects (DARE) (2013, Issue 6);
Ovid MEDLINE (1948 to July Week 1 2013);
Ovid MEDLINE (In‐Process & Other Non‐Indexed Citations, 10 July 2013);
Ovid EMBASE (1980 to 2013 Week 27);
EBSCO CINAHL (1982 to 5 July 2013)
The search strategies for Ovid MEDLINE, Ovid EMBASE and EBSCO CINAHL can be found in Appendix 1. We combined the Ovid MEDLINE search with the Cochrane Highly Sensitive Search Strategy for identifying randomised trials in MEDLINE: sensitivity‐ and precision‐maximising version (2008 revision) (Lefebvre 2011). We combined the EMBASE and CINAHL searches with the trial filters developed by the Scottish Intercollegiate Guidelines Network (SIGN 2013). We did not restrict studies with respect to language, date of publication or study setting.
We searched the metaRegister of Controlled Trials (mRCT) (http://www.controlled‐trials.com/mrct/) and ICTRP (International Clinical Trials Registry Platform) portal maintained by the World Health Organization (http://apps.who.int/trialsearch/). The meta‐register includes the ISRCTN Register and NIH ClinicalTrials.gov Register among other registers. The ICTRP portal includes these trial registers along with trial registry data from a number of countries.
We searched the references of included trials to identify additional relevant trials. We contacted the suture manufacturers Johnson and Johnson, and 3M about any trials that they had conducted.
Data and analyses
Comparison 1. Early versus delayed dressing removal.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Superficial surgical site infection within 30 days | 3 | 280 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.32, 1.28] |
| 2 Superficial wound dehiscence within 30 days | 2 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.19, 21.16] |
| 3 Patients with serious adverse events at 30 days | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4 Length of hospital stay at maximal follow‐up | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5 Costs at maximal follow‐up | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6 Superficial surgical site infection within 30 days (sensitivity analysis) | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 Best‐best scenario | 3 | 283 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.32, 1.28] |
| 6.2 Worst‐worst scenario | 3 | 283 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.54 [0.27, 1.07] |
| 6.3 Best‐worst scenario | 3 | 283 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.54 [0.27, 1.07] |
| 6.4 Worst‐best scenario | 3 | 283 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.32, 1.28] |
| 7 Superficial wound dehiscence within 30 days (sensitivity analysis) | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 Best‐best scenario | 2 | 183 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.19, 21.16] |
| 7.2 Worst‐worst scenario | 2 | 183 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.12, 2.66] |
| 7.3 Best‐worst scenario | 2 | 183 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.12, 2.66] |
| 7.4 Worst‐best scenario | 2 | 183 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.19, 21.16] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ajao 1977.
| Methods | Randomised clinical trial | |
| Participants | Country: Nigeria Number randomised: 100 Post‐randomisation drop‐outs: not stated Revised sample size: 100 Average age: not stated Male: female ratio: not stated Inclusion criteria: people having various surgical procedures (all operations on the trunk) | |
| Interventions | Participants randomly assigned to 2 groups
Group 1 (n = 50): early dressing removal, wound left open 24‐36 h after suturing Group 2 (n = 50): delayed dressing removal, dressing left for 7‐10 days unless infection suspected, when the wound was inspected and dressing reapplied |
|
| Outcomes | Wound infection | |
| Notes | We attempted to contact the authors in Janaury 2013 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: this information was not available |
| Allocation concealment (selection bias) | Unclear risk | Comment: this information was not available |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: no dressing was given beyond 24‐36 h after surgery in the early dressing group while the dressing was left for 7‐10 days in the delayed dressing group making blinding of participants impossible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: this information was not available |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: this information was not available |
| Selective reporting (reporting bias) | High risk | Comment: did not report some important outcomes that would generally be assessed |
| Other bias | Low risk | Comment: no other bias was noted |
Dosseh 2008.
| Methods | Randomised clinical trial | |
| Participants | Country: Togo Number randomised: 105 Post‐randomisation drop‐outs: 3 (2.9%) Revised sample size: 102 Average age: 36 years Male: female ratio: 67 (65.7%): 35 (34.3%) Inclusion criteria: 1. People undergoing abdominal surgery, neck surgery and thoracic surgery and having clean or clean‐contaminated wounds 2. American Society of Anesthesiologists (ASA) 1 or 2 (low anaesthetic risk) 3. Could be randomised to early or delayed dressing removal 4. Participants (or their parents) should be able to understand the protocol Exclusion criteria: 1. People who did not have internal surgery (i.e. those who had surgery for skin lesions) 2. People who deviated from the protocol | |
| Interventions | Participants randomly assigned to 2 groups
Group 1 (n = 51): early dressing removal, wound left open 48 h after surgery Group 2 (n = 51): delayed dressing removal, dressing changed every 48 h until suture removal |
|
| Outcomes | Wound infection, wound dehiscence, hospital stay, and costs | |
| Notes | We attempted to contact the authors in January 2013 Reason for post‐randomisation drop‐outs: participants in dressing group who opted for no dressing |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: this information was not available |
| Allocation concealment (selection bias) | Unclear risk | Comment: this information was not available |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: no dressing was given beyond 48 h after surgery in the early dressing group while the dressing was left until suture removal in the delayed dressing group making blinding of participants impossible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: this information was not available |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: there were post‐randomisation drop‐outs. The direction of effect was altered by imputing the data under different scenarios for superficial wound dehiscence (Analysis 1.7) |
| Selective reporting (reporting bias) | High risk | Comment: did not report some important outcomes that would generally be assessed |
| Other bias | Low risk | Comment: no other bias was noted |
Ramkumar 2006.
| Methods | Randomised clinical trial | |
| Participants | Country: United Kingdom Number randomised: 80 Post‐randomisation drop‐outs: 2 (2.5%) Revised sample size: 78 Average age: 10 years Male: female ratio: 40 (51.3%): 38 (48.7%) Inclusion criteria: children < 16 years of age undergoing a unilateral or bilateral primary correction of prominent ears Exclusion criteria: children requiring secondary revision or with any other type of congenital ear deformity | |
| Interventions | Participants randomly assigned to 2 groups Group 1 (n = 39): early dressing removal, head bandage was removed the next day Group 2 (n = 39): delayed dressing removal, head bandage was removed after 10 days Both groups received Tubigrip bandage at night‐time for 4‐6 weeks | |
| Outcomes | Wound infection and other complications | |
| Notes | We attempted to contact the authors in January 2013 Reasons for post‐randomisation drop‐outs: unable to collect information (group not stated) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: this information was not available |
| Allocation concealment (selection bias) | Unclear risk | Comment: this information was not available |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: no dressing was given beyond 24 h after surgery in the early dressing group while the dressing was left for 10 days in the delayed dressing group making blinding of participants impossible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: this information was not available |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: there were post‐randomisation drop‐outs, and the groups to which they had been randomised could be seen |
| Selective reporting (reporting bias) | Low risk | Comment: all important outcomes were reported |
| Other bias | Low risk | Comment: no other bias was noted |
Wipke‐Tevis 1998.
| Methods | Randomised clinical trial | |
| Participants | Country: USA Number randomised: 32 Post‐randomisation drop‐outs: 5 (15.6%) Revised sample size: 27 Average age: 62 years Male: female ratio: 22 (81.5%): 5 (18.5%) Inclusion criteria: people undergoing coronary artery bypass graft surgery with saphenous vein grafts Exclusion criteria: people receiving immunosuppressant medications, or undergoing intra‐aortic balloon pump therapy | |
| Interventions | Participants randomly assigned to 2 groups Group 1 (n = 7): early dressing removal, wound left open 24 h after surgery. Dry sterile dressing was used, if there was any section of the wound that continued to drain, until the discharge stopped Group 2 (n = 20): delayed dressing removal, dressing remained in place until removal of sutures. Two types of dressings were used (this again was random, so this was a 3‐armed trial of early dressing removal versus delayed dressing removal with 2 different dressings). One of the delayed dressing groups received daily dressings with sterile gauze. The remaining participants in the delayed dressing group received Tegaderm dressing (frequency of change not stated) | |
| Outcomes | None of the outcomes of interest for this review were reported | |
| Notes | We attempted to contact the authors in January 2013. Authors replied with information regarding risk of bias assessment Reason for post‐randomisation drop‐outs: incomplete data (group not stated) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A table of random numbers out of the back of a statistics book was utilized" (author replies) |
| Allocation concealment (selection bias) | Low risk | Quote: "Each potential subject was given an ID number and a sequence was placed in an opaque envelope" (author replies) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: no dressing was given beyond 24 h after surgery in the early dressing group while the dressing was left until suture removal in the delayed dressing group making blinding of participants impossible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: this information was not available |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: there were post‐randomisation drop‐outs, and the groups to which they had been randomised could be seen |
| Selective reporting (reporting bias) | High risk | Comment: did not report some important outcomes that would generally be assessed |
| Other bias | Low risk | Comment: no other bias was noted |
Abbreviations
< = less than h = hour(s)
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Chrintz 1989 | Quasi‐randomised study |
| Edwards 1967 | Not a randomised trial |
| Law 1987 | Comparison of different dressings and no dressings |
| Lisy 2014 | Commentary on the current Cochrane review |
| Meylan 2001 | Quasi‐randomised study |
| Springer 2013 | Study not comparing early versus delayed dressing removal |
Contributions of authors
Protocol
Rajarajan Ramamoorthy developed the protocol, completed the first draft of the protocol, performed part of the writing or editing, made an intellectual contribution, and approved the final version prior to submission.¬ Brian Davidson conceived the review question, secured funding, made an intellectual contribution, advised on the protocol, and approved the final version prior to submission.¬ Kurinchi Gurusamy conceived the review question, developed the protocol, co‐ordinated protocol development, secured funding, performed part of the writing or editing of the protocol, made an intellectual contribution, advised on the protocol, and approved the final version prior to submission.
Review
Clare Toon developed the review, completed the first draft, performed part of the writing or editing of the review, made an intellectual contribution and approved the final version prior to submission. Rajarajan Ramamoorthy made an intellectual contribution and approved the final version prior to submission.¬ Brian Davidson conceived the review question, secured funding, made an intellectual contribution, advised on the review and approved the final version prior to submission.¬ Kurinchi Gurusamy developed the review, co‐ordinated review development, secured funding, performed part of the writing or editing of the review, made an intellectual contribution, advised on the review, approved the final version prior to submission, and is guarantor of the review.
Update
Kurinchi Gurusamy screened the search results, assessed full text articles, edited and approved the final updated review version prior to submission, and is guarantor of the review. Charnelle Lusuku screened the search results, retrieved articles for assessment and edited the updated review.
Contributions of editorial base
Nicky Cullum: edited the protocol; advised on methodology, interpretation and protocol content. Approved the final protocol prior to submission. Joan Webster, Editor: approved the final review prior to submission. Sally Bell‐Syer: co‐ordinated the editorial process. Advised on methodology, interpretation and content. Edited the protocol,review and updated review. Ruth Foxlee: designed the search strategy and edited the search methods section. Rachel Richardson: edited the review.
Sources of support
Internal sources
No sources of support supplied
External sources
-
National Institute for Health Research (NIHR ‐ UK Government organisation for health research), UK.
NIHR provides financial support for K Gurusamy for completing the review
NIHR / Department of Health (England), (Cochrane Wounds Group), UK.
Declarations of interest
Clare D Toon: none known Charnelle Lusuku: none known Rajarajan Ramamoorthy: none known Brian R Davidson: none known Kurinchi Selvan Gurusamy: none known
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Ajao 1977 {published data only}
- Ajao OG. Surgical wound infection: a comparison between dressed and undressed wounds. Journal of Tropical Medicine and Hygiene 1977;80(9):192‐6. [PubMed] [Google Scholar]
Dosseh 2008 {published data only}
- Dosseh Ekoue D, Doleaglenou A, Fortey YK, Ayite AE. Randomized trial comparing dressing to no dressing of surgical wounds in a tropical setting [Pansement versus absence de pansement au dela de 48 heures en milieu tropical: essai randomise]. Journal de Chirurgie 2008;145(2):143‐6. [PubMed] [Google Scholar]
Ramkumar 2006 {published data only}
- Ramkumar S, Narayanan V, Laing JHE. Twenty‐four hours or 10 days? A prospective randomised controlled trial in children comparing head bandages following pinnaplasty. Journal of Plastic, Reconstructive and Aesthetic Surgery 2006;59(9):969‐74. [DOI] [PubMed] [Google Scholar]
Wipke‐Tevis 1998 {published data only}
- Wipke‐Tevis DD, Stotts NA. Effect of dressings on saphenous vein harvest incision pain, distress and cosmetic result. Progress in Cardiovascular Nursing 1998;13(3):3‐13. [PubMed] [Google Scholar]
References to studies excluded from this review
Chrintz 1989 {published data only}
- Chrintz H, Vibits H, Cordtz TO, Harreby JS, Waaddegaard P, Larsen SO. Need for surgical wound dressing. British Journal of Surgery 1989; Vol. 76, issue 2:204‐5. [DOI] [PubMed]
- Chrintz H, Vibits H, Harreby JS, Cordtz TO, Waaddegaard P, Larsen SO. Discontinuing postoperative wound dressings. Ugeskrift for Laeger 1989;151(41):2667‐8. [PubMed] [Google Scholar]
Edwards 1967 {published data only}
- Edwards RH, Killen DA. Comparison of two methods of management of clean surgical wounds. "Open" vs "closed" postoperative wound care. JAMA 1967;201(1):137‐8. [DOI] [PubMed] [Google Scholar]
Law 1987 {published data only}
- Law NW, Ellis H. Exposure of the wound‐‐a safe economy in the NHS. Postgraduate Medical Journal 1987;63(735):27‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lisy 2014 {published data only}
- Lisy K. Early vs. Delayed Removal of Dressings Covering Surgical Wounds. American Journal of Nursing 2014;23(6):326‐30. [DOI] [PubMed] [Google Scholar]
Meylan 2001 {published data only}
- Meylan G, Tschantz P. Surgical wounds with or without dressing. Prospective comparative study. Annales de Chirurgie 2001;126(5):459‐62. [DOI] [PubMed] [Google Scholar]
Springer 2013 {published data only}
- Springer BD, Beaver WB, Griffin WL. The role of surgical dressings in total knee arthroplasty: A randomized clinical trial. Clinical Orthopedic Related Research 2013;24(4):452‐3. [Google Scholar]
Additional references
Ahn 2011
- Ahn HB, Shin DM, Roh MS, Jeung WJ, Park WC, Rho SH. A comparison of 2‐octyl cyanoacrylate adhesives versus conventional suture materials for eyelid wound closure in rabbits. Korean Journal of Ophthalmology 2011;25(2):121‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Biancari 2010
- Biancari F, Tiozzo V. Staples versus sutures for closing leg wounds after vein graft harvesting for coronary artery bypass surgery. Cochrane Database of Systematic Reviews 2010, Issue 5. [DOI: 10.1002/14651858.CD008057.pub2] [DOI] [PubMed] [Google Scholar]
BNF 2011
- British Medical Association and the Royal Pharmaceutical Society of Great Britain. British National Formulary. 1st Edition. BMJ Publishing Group, 2011. [Google Scholar]
Boateng 2008
- Boateng JS, Matthews KH, Stevens HN, Eccleston GM. Wound healing dressings and drug delivery systems: a review. Journal of Pharmaceutical Sciences 2008;97(8):2892‐923. [DOI] [PubMed] [Google Scholar]
Broex 2009
- Broex EC, Asselt AD, Bruggeman CA, Tiel FH. Surgical site infections: how high are the costs?. Journal of Hospital Infection 2009;72(3):193‐201. [DOI] [PubMed] [Google Scholar]
Cutting 2002
- Cutting KF, White RJ. Maceration of the skin and wound bed. 1: Its nature and causes. Journal of Wound Care 2002;11(7):275‐8. [DOI] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG (editors), on behalf of the Cochrane Statistical Methods Group and the Cochrane Bias Methods Group. Chapter 9: Analysing data and undertaking meta‐analyses. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
DeMets 1987
- DeMets DL. Methods for combining randomized clinical trials: strengths and limitations. Statistics in Medicine 1987;6(3):341‐50. [DOI] [PubMed] [Google Scholar]
DerSimonian 1986
- DerSimonian R, Laird N. Meta‐analysis in clinical trials. Controlled Clinical Trials 1986;7(3):177‐88. [DOI] [PubMed] [Google Scholar]
Downie 2010
- Downie F, Egdell S, Bielby A, Searle R. Barrier dressings in surgical site infection prevention strategies. British Journal of Nursing 2010;19(20):S42‐6. [DOI] [PubMed] [Google Scholar]
Dyson 1988
- Dyson M, Young S, Pendle CL, Webster DF, Lang SM. Comparison of the effects of moist and dry conditions on dermal repair. Journal of Investigative Dermatology 1988;91(5):434‐9. [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey SG, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315(7109):629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Garcia‐Gubern 2010
- Garcia‐Gubern CF, Colon‐Rolon L, Bond MC. Essential concepts of wound management. Emergency Medicine Clinics of North America 2010;28(4):951‐67. [DOI] [PubMed] [Google Scholar]
Garner 1986
- Garner JS. CDC guideline for prevention of surgical wound infections, 1985. Infection Control 1986;7(3):193‐200. [DOI] [PubMed] [Google Scholar]
Gurusamy 2009
- Gurusamy KS, Gluud C, Nikolova D, Davidson BR. Assessment of risk of bias in randomized clinical trials in surgery. British Journal of Surgery 2009;96(4):342‐9. [DOI] [PubMed] [Google Scholar]
Gwosdow 1993
- Gwosdow AR, Cunningham JJ, Lydon M, Rascati R, Berglund LG. Evaporative water losses through a temporary wound dressing under simulated wound conditions. Journal of Burn Care and Rehabilitation 1993;14(4):450‐4. [DOI] [PubMed] [Google Scholar]
Hasan 2009
- Hasan Z, Gangopadhyay AN, Gupta DK, Srivastava P, Sharma SP. Sutureless skin closure with isoamyl 2‐cyanoacrylate in pediatric day‐care surgery. Pediatric Surgery International 2009;25(12):1123‐5. [DOI] [PubMed] [Google Scholar]
Higgins 2002
- Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta‐analysis. Statistics in Medicine 2002;21(11):1539‐58. [DOI] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Higgins 2011b
- Higgins JPT, Altman DG, Sterne JAC (editors) on behalf of the Cochrane Statistical Methods Group and the Cochrane Bias Methods Group. Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Higgins 2011c
- Higgins JPT, Deeks JJ (editors). Chapter 7: Selecting studies and collecting data. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Higgins 2011d
- Higgins JPT, Deeks JJ, Altman DG (editors) on behalf of the Cochrane Statistical Methods Group and the Cochrane Bias Methods Group. Chapter 16: Special topics in statistics. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Horan 1992
- Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infection Control and Hospital Epidemiology 1992;13(10):606‐8. [PubMed] [Google Scholar]
Hutchinson 1991
- Hutchinson JJ, Lawrence JC. Wound infection under occlusive dressings. Journal of Hospital Infection 1991;17(2):83‐94. [DOI] [PubMed] [Google Scholar]
ICH‐GCP 1996
- International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use. Code of Federal Regulation & ICH Guidelines. Media: Parexel Barnett, 1996. [Google Scholar]
Keill 1973
- Keill RH, Keitzer WF, Nichols WK, Henzel J, DeWeese MS. Abdominal wound dehiscence. Archives of Surgery 1973;106(4):573‐7. [DOI] [PubMed] [Google Scholar]
Kjaergard 2001
- Kjaergard LL, Villumsen J, Gluud C. Reported methodologic quality and discrepancies between large and small randomized trials in meta‐analyses. Annals of Internal Medicine 2001;135(11):982‐9. [DOI] [PubMed] [Google Scholar]
Lawrence 1998
- Lawrence WT. Physiology of the acute wound. Clinics in Plastic Surgery 1998;25(3):321‐40. [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J (editors) on behalf of the Cochrane Information Retrieval Methods Group. Chapter 6: Searching for studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Macaskill 2001
- Macaskill P, Walter SD, Irwig L. A comparison of methods to detect publication bias in meta‐analysis. Statistics in Medicine 2001;20(4):641‐54. [DOI] [PubMed] [Google Scholar]
Merei 2004
- Merei JM. Pediatric clean surgical wounds: is dressing necessary?. Journal of Pediatric Surgery 2004;39(12):1871‐3. [DOI] [PubMed] [Google Scholar]
Mertz 1985
- Mertz PM, Marshall DA, Eaglstein WH. Occlusive wound dressings to prevent bacterial invasion and wound infection. Journal of the American Academy of Dermatology 1985;12(4):662‐8. [DOI] [PubMed] [Google Scholar]
Moher 1998
- Moher D, Pham B, Jones A, Cook DJ, Jadad AR, Moher M, et al. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta‐analyses?. Lancet 1998;352(9128):609‐13. [DOI] [PubMed] [Google Scholar]
Newell 1992
- Newell DJ. Intention‐to‐treat analysis: implications for quantitative and qualitative research. International Journal of Epidemiology 1992;21(5):837‐41. [DOI] [PubMed] [Google Scholar]
NHS reference costs 2012
- Department of Health, United Kingdom. Financial year 2011 to 2012 reference costs published. http://www.dh.gov.uk/health/2012/11/2011‐12‐reference‐costs/ 2012 (accessed on 13 March 2013).
RevMan 2011 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.1. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2011.
Schulz 1995
- Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273(5):408‐12. [DOI] [PubMed] [Google Scholar]
Schünemann 2011
- Schünemann HJ, Oxman AD, Higgins JPT, Vist GE, Glasziou P, Guyatt GH (editors) on behalf of the Cochrane Applicability and Recommendations Methods Group and the Cochrane Statistical Methods Group. Chapter 11: Presenting results and ‘Summary of findings’ tables. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
SIGN 2013
- Scottish Intercollegiate Guidelines Network. Search filters. http://www.sign.ac.uk/methodology/filters.html (accessed May 24 2013).
Ubbink 2008
- Ubbink DT, Vermeulen H, Goossens A, Kelner RB, Schreuder SM, Lubbers MJ. Occlusive vs gauze dressings for local wound care in surgical patients: a randomized clinical trial. Archives of Surgery 2008;143(10):950‐5. [DOI] [PubMed] [Google Scholar]
Wood 2008
- Wood L, Egger M, Gluud LL, Schulz KF, Jüni P, Altman GD, et al. Empirical evidence of bias in treatment effect estimates in controlled trials with different interventions and outcomes: meta‐epidemiological study. BMJ 2008;336:601‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]


