Abstract
One Health (OH) is an interdisciplinary approach aiming to achieve optimal health for humans, animals and their environments. Case reports and systematic reviews of success are emerging; however, discussion of barriers and enablers of cross-sectoral collaboration are rare. A four-phase mixed-method Delphi survey of Australian human and animal health practitioners and policymakers (n = 52) explored areas of consensus and disagreement over: (1) the operational definition of OH; (2) potential for cross-sectoral collaboration; and (3) key priorities for shaping the development of an OH response to significantly elevated zoonotic disease risk. Participants agreed OH is essential for effective infectious disease prevention and control, and on key priorities for outbreak responses, but disagreed over definitions and the relative priority of animal health and welfare and economic considerations. Strong support emerged among Australian experts for an OH approach. There was also recognition of the need to ensure cross-sectoral differences are addressed.
Electronic supplementary material
The online version of this article (doi:10.1007/s10393-017-1264-7) contains supplementary material, which is available to authorized users.
Keywords: Animal health, Cross-sectoral collaboration, Delphi survey, Emerging infectious diseases, Human health, One Health
Introduction
Emerging and re-emerging infectious diseases (EIDs) are an unpredictable, continuing threat to human, animal and ecological health. They are characterised by complex causes, consequences and potential solutions that critically limit the effectiveness of scientific and technocratic approaches to governance (CDC 2010; Morens and Fauci 2012). EID crises create major issues for distribution of scarce resources, access to health services and global health security. Historically, EIDs have been managed in overlapping, uncoordinated, disciplinary silos (Zinsstag et al. 2006). However, since they are largely driven by human behaviours and human structures in the context of human–animal interactions, the effectiveness of traditional sectoral approaches has been limited.
“One Health” (OH) is the preferred approach to respond to EIDs. OH is based on recognition of the interdependence of human, animal and ecological health and an assumption that cross-sectoral integration of expertise, research methodologies and public health infrastructure increases the capacity for anticipating disease risk and effective intervention (Zinsstag et al. 2011; Lee and Brumme 2013). The OH literature emphasises the benefits (Zinsstag et al. 2006; Zinsstag et al. 2012; Allen-Scott et al. 2015), but there has been little attempt to identify and assess barriers to and enablers of cross-sectoral collaboration (Hueston et al. 2013; Coker et al. 2011; Okello et al. 2015; Ezenwa et al. 2015). Possibly this is because the need for an OH response seems obvious.
Against this background, OH advocates are concerned that early collaborations have not included all relevant disciplines (Hueston et al. 2013; Zinsstag 2012), especially experts from social, ecological and environmental health sciences (Manlove et al. 2016; Binot et al. 2015). Moreover, despite almost two decades of interdisciplinary advocacy by international agencies and national governments, OH still means different things to different people (Text Box 1) (Gibbs 2014). It remains an ‘umbrella concept’ for a variety of expert perspectives and disciplinary agendas. This raises concerns about the capacity and willingness of different professional groups to collaborate (Lee and Brumme 2013; Okello et al. 2014; Chien 2013) and the extent to which various sectoral priorities can be aligned, during EID response planning (Stärk et al. 2015; Brookes et al. 2015; Häsler et al. 2012).
Text Box 1.
Current Definitions of One Health
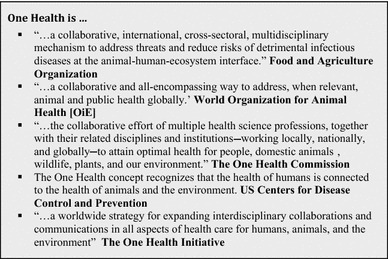
The conceptual ambiguity of OH could actually diffuse political tensions between competing sectoral agendas, allowing them to work together (Chien 2013). Nevertheless, lack of evidence about how different sectors understand OH, their roles and responsibilities and how they pursue their priorities could limit collaboration and its benefits. Because resources are limited, prioritisation and resource allocation require political decisions, based on ethical principles, about what is valued, what must be protected and what is dispensable.
In this paper, we report the results of a modified Delphi survey from a larger study, which aims to elicit the values underpinning OH and develop guidance for practitioners and policymakers. We employed mixed methods to explore areas of sectoral consensus or disagreement on: how OH should be defined; the potential for cross-sectoral collaboration in Australia; and key priorities that should shape development of an OH response to a zoonotic EID emergency, when knowledge of its nature, scale and scope is absent or fluid.
Methods
Participants
A heterogeneous and geographically dispersed group of experts in human and veterinary medicine, health law and wildlife ecology and representatives of agricultural industries and animal welfare/protection organisations were invited to participate in this survey. We defined ‘experts’ as individuals with knowledge and experience of EID risks and outbreaks among humans and animals (Ziglio 1996). Sampling was purposive, to ensure representation of traditional OH stakeholders. Potential participants were identified through institutional websites and researchers’ professional networks.
Delphi Processes
The rationale of Delphi surveys is that group consensus about contentious issues is more valid than individual opinions (Jones and Hunter 1995). Anonymous data are collected from individuals, collated and then represented to the group to elicit further responses (Ziglio 1996). In this study, we analysed data iteratively in parallel with data collection. Rather than force consensus, we employed a modified technique that allows participants to explain their views. Except for early discussions about OH definitions (Round [R] 2/Q1), consensus ‘cut offs’ (i.e. fixed levels of agreement) were not employed to limit the choices available to survey participants. Otherwise, participants were asked to judge and respond to the levels of consensus/disagreement that emerged from each round to provide greater insight into the operational relevance of OH. Participants who completed each round were invited to participate in the next, but were free to withdraw at any time. We used an online survey platform [Limesurvey].
In R1, we asked participants about their understanding of OH and to respond to three hypothetical scenarios, each describing a substantially elevated risk of a significant EID event in Australia. Scenarios [available in online materials] were adapted, with permission, from a similar study in Singapore (see acknowledgements). Responses were analysed qualitatively and coded thematically by two authors (CD and JJ) using framework analysis, a matrix-based method for ordering and synthesising textual data (Gale et al. 2013). During rounds 2–4, participants’ comments, key arguments and levels of consensus from previous rounds were presented as quotations, bar charts and summaries of qualitative findings, taking care to weigh different opinions and arguments equally. Individual comments were de-identified.
Additional data and comments were collected, using Likert scales and free text responses. On completion of each round, participants’ Likert scores were tabulated and free text answers analysed qualitatively, as described. The final stage of analysis during preparation of this report drew on the knowledge and professional experience of the research team.
To aid analysis, each participant was allocated to a disciplinary/sectoral category—animal or human health—based on their qualifications and current responsibilities. Consistent with previous reports that ecologists and environmental scientists are poorly represented in OH discourse (Zinsstag 2012; Binot et al. 2015), participants from these disciplines all occupied positions within the animal health sector and were allocated accordingly. This study was approved by the University of Sydney Human Research Ethics Committee.
Results
Participants
Email invitations were sent to 85 potential participants, of whom 52 (61%) from a range of relevant OH roles, disciplines and geographic regions, responded (Table 1). Invitations included an individualised link to the online survey, through which participant consent was obtained.
Table 1.
Professional/Employment Characteristics and Geographic Locations of Panel Participants
| Round 1 | Round 2 | Round 3 | Round 4 | |
|---|---|---|---|---|
| n = 52 | n = 40 | n = 34 | n = 24 | |
| Response rate | 62% | 77% | 85% | 71% |
| Employment setting | ||||
| Federal government | 7 (0.135)* | 6 (0.15) | 5 (0.147) | 4 (0.167) |
| Provincial governments | 17 (0.323) | 14 (0.35) | 11 (0.323) | 9 (0.375) |
| Regional/local health authorities | 7 (0.135) | 4 (0.1) | 4 (0.117) | 2 (0.083) |
| NGO/industry | 6 (0.115) | 5 (0.125) | 4 (0.117) | 1 (0.042) |
| University | 15 (0.288) | 11 (0.275) | 10 (0.294) | 8 (0.333) |
| Geographic area | ||||
| Federal/national | 12 (0.231) | 11 (0.275) | 8 (0.235) | 5 (0.208) |
| NSW | 13 (0.25) | 10 (0.25) | 9 (0.265) | 7 (0.292) |
| Victoria | 8 (0.154) | 5 (0.125) | 5 (0.147) | 4 (0.167) |
| Queensland | 6 (0.115) | 3 (0.075) | 3 (0.088) | 3 (0.125) |
| Western Australia | 5 (0. 096) | 4 (0.1) | 3 (0.088) | 0 |
| Northern Territory | 3 (0.057) | 3 (0.075) | 2 (0.059) | 2 (0.083) |
| South Australia | 2 (0.038) | 2 (0.05) | 2 (0.059) | 1 (0.042) |
| ACT | 2 (0.038) | 1 (0.025) | 1 (0.029) | 1 (0.042) |
| Tasmania | 1 (0.019) | 1 (0.025) | 1 (0.029) | 1 (0.042) |
| Primary role/responsibility | ||||
| Chief Medical/Veterinary Officers | 6 (0.115) | 4 (0.01) | 3 (0.088) | 2 (0.083) |
| Directors of Health/Biosecurity agencies | 11 (0.212) | 10 (0.25) | 9 (0.265) | 7 (0.292) |
| Public Health/Veterinary Officers | 9 (0.173) | 5 (0.125) | 4 (0.117) | 3 (0.125) |
| Senior Policy officer/research scientist | 12 (0.231) | 10 (0.25) | 8 (0.235) | 5 (0.208) |
| Academic clinician/researcher | 14 (0.269) | 11 (0.275) | 10 (0.294) | 7 (0.292) |
| Disciplinary/sectoral background | ||||
| Human health | 24 (0.462) | 20 (0.50) | 17 (0.5) | 11 (0.458) |
| Animal health | 28 (0.538) | 20 (0.50) | 17 (0.5) | 13 (0.542) |
* Data in brackets are proportions of total in each category.
As expected, the panel size gradually decreased as participants withdrew (Keeney et al. 2001), but the balance between human and animal health sectors and characteristics of participants remained substantially constant (Table 1). The final round was run at the request of participants who were keen to give further feedback on the findings.
Responses to Questions on How OH Should be Defined
Seven statements describing OH were compiled from participants’ responses to questions about the nature of OH. In R2, they were asked to indicate the extent to which they agreed/disagreed with these statements [Supplementary materials]. To focus discussion, we applied a cut off of >65% agreement. The three statements that met or exceeded this threshold were presented to participants in R3, namely:
The interrelationship between human, animal and environmental health [A].
The integration of human, animal and environmental health [B].
Cross-disciplinary collaboration and communication between veterinary, medical and ecological sciences and relevant government agencies [D].
Participants were asked to indicate, with reasons for their choice, which statement best reflected their view of OH (Table 2).
Table 2.
Level of Support for Different Definitions of One Health.
| Statement | Delphi Round 3 | Delphi Round 4 | ||||
|---|---|---|---|---|---|---|
| Human health sector (n = 17) | Animal health sector (n = 17) | Round 3 Total (n = 34) |
Human health sector (n = 11) | Animal health sector (n = 13) | Round 4 Total (n = 24) |
|
| 1 [A] | 9 (0.52) | 8 (0.46) | 17 (0.50) | 5 (0.45) | 7 (0.54) | 12 (0.50) |
| 2 [B] | 4 (0.24) | 3 (0.18) | 7 (0.21) | 0 | 3 (0.23) | 3 (0.13) |
| 3 [D] | 4 (0.24) | 6 (0.36) | 10 (0.29) | 6 (0.55) | 3 (0.23) | 9 (0.37) |
Data from rounds 3 and 4.
* Data in brackets are proportions of total in each category.
Key differences (as revealed in comments) were the extent to which participants considered OH to be: a concept for understanding linkages between human, animal and environmental health (statement 1); an emerging integrative discipline (statement 2); or a political initiative to promote cross-disciplinary collaboration (statement 3). Several participants regarded none of these statements as satisfactory, citing the limited importance given to the environment in current discourse. One participant commented:
DP #26 - The problem at the moment with the way many people in the veterinary and human health fields use the term ‘One Health’ is that it focuses on human and terrestrial animal health i.e. zoonoses, and excludes the other organisms (plants, fish) and their interactions with the environment. … If we are serious about a concept of ‘One Health’ then it needs to be used to describe the interactions and interrelationships across all organisms and the environment otherwise it’s not ‘One Health’.
In R4, participants were shown a representative sample of comments and given the opportunity to change their position. Table 2 shows that support (in relative terms) drifted from statement 2 to statement 3. Participants who still preferred statement 2 in R4 were all aligned with the animal health sector. Otherwise, disciplinary background appeared not to influence how participants defined OH.
These results revealed the difficulty of arriving at a consensus definition of OH, despite considerable cross-disciplinary agreement. Substantively, the three statements are very similar; the key tension is whether OH is a means to reach an holistic understanding of EID threats or a road map for effective cross-sectoral responses. Comments from R3 and R4 (Table S1 Supplementary data) suggested that participants who preferred statement 1 were resistant to disciplinary integration or specific outcomes, whereas those who preferred statement 3 were more pragmatic and focused on cross-sectoral collaboration as the key driver of a successful OH approach.
Responses to Questions on Cross-sectoral Collaboration
In R2, we asked participants to indicate on a Likert scale their (dis)agreement with the statement in Text Box 2.
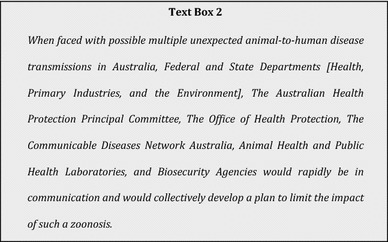
Just over two-thirds of participants agreed; the statement was most strongly endorsed by human health sector participants. Those from the animal health sector were more pessimistic or unsure about the immediate prospects for cross-sectoral collaboration (Fig. 1).
Fig. 1.
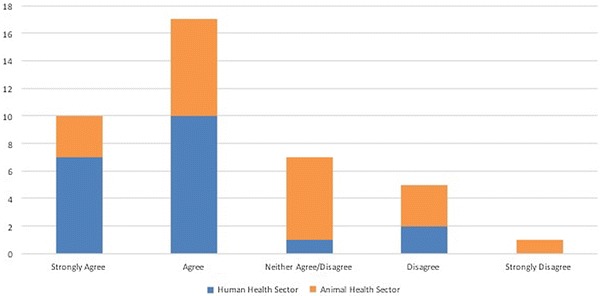
The extent to which participants from human and animal health sectors Agreed/Disagreed with the statement in Text Box 2
To explore these positions, we constructed a list of potential barriers to OH approaches, from participants’ responses to R1 scenarios. Figure 2 shows the extent to which R2 participants agreed or disagreed with each.
Fig. 2.
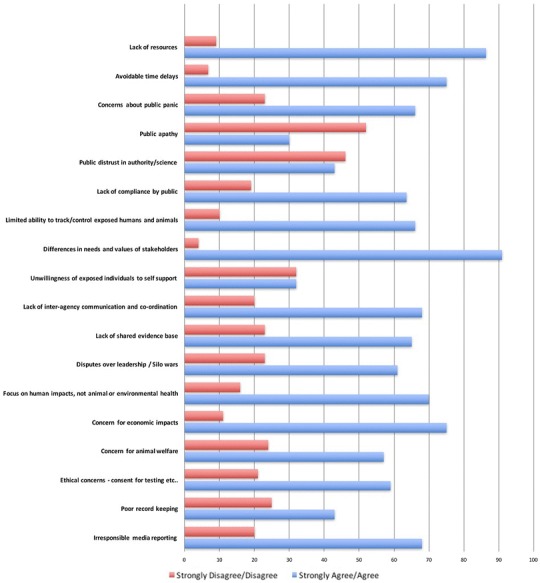
The extent to which participants Agreed/Disagreed with different barriers to a One Health approach identified in Round 1 of the survey
Although participants were generally optimistic that different sectors would work together during a significant EID outbreak, we were surprised by how strongly they believed that most barriers were likely to impede an OH response.
A comment from one participant [R3] illustrates this:
DP #46 - … there are quite a number of issues preventing an optimal response to a major zoonotic disease outbreak. It will require additional resources and plenty of planning and training (including a merging of cultures) to provide the sort of response we should expect. … This does NOT mean we should abandon the process of One Health but serves to illustrate the many difficulties to overcome.
A general theme of the comments was the need for inter-agency consultation, relationship building, planning and funding allocation, to deal with cross-sectoral differences before threats occur. Participants’ responses were analysed according to disciplinary background. Applying Fisher’s exact test (comparing agree vs. disagree and excluding the neither agree/disagree group) (Routledge 1998), the only significant (p < 0.05) difference was that participants from the animal health sector were more likely to see a focus on human, rather than animal or environmental health, as a barrier to an OH response.
By R4, only 2 of 24 participants did not agree with the original statement (Text Box 2); most believed that, despite differences or mutual cynicism, different sectors would set aside conflicting interests to mount an effective response to a significant zoonotic threat. However, many were convinced that a response could not be implemented rapidly and seamlessly, unless overall responsibility for infectious disease control and prevention in humans and animals were located within a single agency.
Key Priorities in Developing a Plan of Action
Previous studies have shown that different priorities create tensions between OH stakeholder groups (Okello et al. 2015; Chien 2013). In R2, we asked panel members to rank 19 issues for developing an action plan in response to an unexpected threat. Because our aim was to understand the key concerns and types of evidence needed to formulate a response at times of uncertainty, participants were asked to rank the issues, without contextual information, such as the nature or source of the pathogen or size of the outbreak. Rankings were determined by assigning a score equivalent to reverse rank (e.g. a score of 19 to items rated 1st); scores were multiplied by the number of participants who gave each rank, and the overall ranking was determined by adding scores for each item. Table 3 shows the final rankings, which were presented to participants in R3 for comment.
Table 3.
Key Priorities When Developing a Plan of Action Ranked from Most to Least Important.
| Overall ranking | Rating score | Rankings in 1st quartile (%) | Rankings in 2nd quartile (%) | Rankings in 3rd quartile (%) | Rankings in 4th quartile (%) | |
|---|---|---|---|---|---|---|
| Impacts on human health | 1 | 718 | 97.5 | 0.0 | 0.0 | 2.5 |
| Availability of human and health resources for plan implementation | 2 | 602 | 65.0 | 27.5 | 2.5 | 5.0 |
| Continuity of food supply and maintenance of essential services | 3 | 571 | 57.5 | 30.0 | 5.0 | 7.5 |
| Public education about the risks faced by individuals and communities | 4 | 545 | 50.0 | 30.0 | 17.5 | 2.5 |
| Economic impacts on individuals, businesses and governments | 5 | 521 | 42.5 | 37.5 | 17.5 | 2.5 |
| The financial cost of implementing the plan | 6 | 493 | 40.0 | 30.0 | 20.0 | 10.0 |
| Potential public reaction—including concerns about stigmatisation | 7 | 428 | 10.0 | 57.0 | 30.0 | 3.0 |
| Ease of tracking exposed persons | 8 | 419 | 27.5 | 27.5 | 30.0 | 12.5 |
| Welfare and health of animals | 9 | 405 | 27.5 | 27.5 | 22.5 | 12.5 |
| Emotional/psychological stress on individuals | 10 | 376 | 10.0 | 37.5 | 42.5 | 10.0 |
| The interests of other jurisdictions—[WHO, neighbouring states… etc.] | 11 | 373 | 27.5 | 35.0 | 10.0 | 27.5 |
| Confidentiality of those who are ill, being traced or involved in decision-making | 12 | 355 | 10.0 | 40.0 | 32.5 | 7.5 |
| Impacts on the environment | 13 | 313 | 12.5 | 17.5 | 37.5 | 42.5 |
| Australia’s reputation | 14 | 311 | 12.5 | 22.5 | 37.5 | 32.5 |
| The potential for research to generate valuable new knowledge | 15 | 302 | 10.0 | 25.0 | 30.0 | 35.0 |
| Impacts on the freedom of individuals | 16 | 284 | 0.0 | 25.0 | 50.0 | 25.0 |
| Impacts on tourism and travel | 17 | 215 | 0.0 | 12.5 | 45.0 | 47.5 |
| Impacts on family cohesion | 18 | 209 | 2.5 | 10.0 | 37.5 | 50.0 |
| Impacts on public transport | 19 | 158 | 0.0 | 10.0 | 32.5 | 37.5 |
Data collected in round 2 (n = 40).
The panel gave a strong endorsement to the top six items; at least 40% of participants ranked them in the top 5 and 70% in the top 10. Responses were a mix of ideal and pragmatic—burden of disease, costs of implementation and maintenance of services were key issues. In R3, participants’ comments on rankings indicated general agreement that human health, food security, resource availability and communication are appropriate primary concerns. Lower-ranked items were more evenly distributed, indicating more varied views about their importance. Several participants from both sectors expressed surprise at the relatively low rankings of social considerations, animal health and welfare and environmental health. Some were surprised at how high economic impacts and costs were ranked, commenting that it was not their role to prioritise according to economic factors. However, in subsequent rounds, it was suggested this was naïve; in the words of one participant: “Economic considerations come into everything that is done in health” (DP #33). Most agreed with the importance of proportionality such that economic factors were a consideration, but not the key consideration, in decision-making. The plurality of views caused one participant to note:
DP #5 - It depends on the particular situation: that’s why we have, and need, consultative committees with broad representation to consider each situation.
Table S2 (Supplementary data) provides a breakdown, by sector, of priorities and preferences from R3. While there was broad agreement on the top six priorities, there were some differences between sectors. Where there is a lack of evidence, animal health sector participants generally gave greater priority to economic and animal health concerns, whereas those from the human health sector were more likely to rank the effect on the emotional wellbeing and privacy of individuals and the risks of stigmatisation of those affected more highly.
Several participants made the case that different situations would require different priorities; for example:
DP #22 - Outbreak of rabies, Australian Bat Lyssa Virus (ABVL) or Japanese Encephalitis (JE) would have a localised impact in which the “top six” may be less important and issues 7 - 11 assume a higher importance. It is unlikely that rabies, ABLV or JE would impact on food supply or major economic impact yet the emotional psychological stress on individuals could be really significant.
A common theme was that participants needed more information in order to make decisions about priorities. Of this one participant noted:
DP # 52 – While I agree with the sentiments expressed, it is not always possible to answer all these questions quickly enough, and actions may usually need to be undertaken before all the questions can be answered – especially how big is it and how big will it get, which may not be known until well into the outbreak.
Given that there may be little existing evidence or experience when new threats—like SARS or bovine spongiform encephalitis (BSE)—emerge, key findings of this survey include the critical role of context in EID response planning and policy decision-making. Participants hoped that sectoral differences over second-order priorities would not interfere with these key goals, rather that they be points of consultation to ensure that responses encompass different stakeholder perspectives.
Discussion
Our findings indicate high levels of support among Australian policymakers and practitioners for an OH approach to zoonotic disease control and prevention, despite several points of disagreement. One key difference was whether OH should be defined as a means to integrate disciplinary practices or as a framework to understand linkages between separate disciplines. Proponents of both positions were found in both the main sectors, suggesting that the tension between integrationists and those who want to maintain disciplinary integrity is a personal rather than sectoral preference. Focussing on differences in the definition of OH may miss the point, but the complexities of EID control and prevention probably mean that an effective response requires genuine cross-sectoral integration and re-sectoring of some institutional and professional responsibilities (Zinsstag et al. 2012). The results of this survey suggest that any such efforts are likely to meet with resistance within and across the relevant sectors.
It is notable that not all of the barriers to the effective implementation of an inter-agency plan identified by Delphi participants (Fig. 2) were addressed by key priorities for action (Table 3). This is likely to be because some of the barriers identified simply do not have a practical action that can easily be included in a plan of action. That there is substantial overlap between the two lists in this study is actually a positive sign that there are many practical and collaborative actions that can be taken in the event of an EID outbreak. Sectoral differences in participants’ responses tended to coalesce around the relative importance of each of the groups’ professional roles and responsibilities. The animal health sector, which traditionally works to maximise the value, utility and welfare of animals, emphasised economic and animal health considerations. Those working in the human health sector thought that ethical considerations and factors that affect epidemiological investigations should have higher priority. Differences in the goals and values of different sectors are not unexpected, but are likely to complicate cross-sectoral co-operation. Past experience with BSE and pandemic influenza H1N1 indicates that, in the face of scientific uncertainty and ethical ambiguity, these differences will be amplified. Consequently, sectoral interests and short-term political considerations will threaten efforts to devise effective long-term interventions (Phillips et al. 2012; Rosella et al. 2013).
There is some urgency to address disagreements revealed by this survey because calls for increased inter-sectoral co-operation, by public health practitioners and policymakers in Australia (Baum 2003; Degeling 1995), and elsewhere, are not new (Rüegg et al. 2017). Unfortunately, past experience suggests that attempts to promote a cross-sectoral approach rarely move beyond rhetoric, even when driven by the best intentions and supported by substantial resources. The problem is that arguments focus on the likely benefits of collaboration rather than what needs to be done, organisationally and politically, to achieve the desired outcomes (Degeling 1995). Established ‘sectors’ have genealogies and rationalities shaped by social, political and administrative processes; as institutions, they are inherently and structurally resistant to measures that divert resources and reorient practices away from their own sectoral priorities. Consequently, even with commitment to information-sharing, through collaborative working groups and interdepartmental committees, inter-sectoral co-operation has rarely delivered the outcomes promised. Many recognise that integrationist reforms are likely to promote more effective cross-sectoral collaboration (Coker et al. 2011; Manlove et al. 2016), and OH opinion leaders are now advocating for the establishment of a supporting OH infrastructure comprised of:
complex, polycentric organizational structures … [that] rely on multiple, strong connections and coordinated activities across sectors (Rüegg et al. 2017).
Against this background, there is evidence that enthusiasm for OH in Australia is genuine rather than symbolic, as governments in recent years have moved towards aggregating responsibility for agriculture and environmental health under ‘biosecurity’. Initiatives such as the Australian Antimicrobial Resistance Strategy and Hendra Virus Interagency Technical Working Group are significant attempts to achieve collaboration between human and animal health sectors. This survey showed that there is considerable agreement among human and animal health practitioners and policymakers, including about the nature and scale of barriers to effective OH collaboration and the need for further work to explore their potential impacts. This suggests that implementation of an OH strategy, based on inter-sectoral co-operation, is eminently feasible.
Strengths and Limitations
The initial response to participant invitations was moderate, which was gratifying, given that our invitation was unsolicited. Retention of participants over successive rounds was also moderate, and the balance between members of different sectors remained constant. Because participation across different sectoral roles and jurisdictions remained relatively heterogeneous throughout the survey (Table 1), we believe the risk of selection bias due to participant withdrawal is minimal. Moreover, allowing participants to express their views and comment on each other’s interpretation, via open-ended free text questions, over multiple survey rounds increased the reliability of the study and improved the validity of the results. A limitation was the lack of a clearly identifiable environmental sector, which is likely to be an artefact of how the management of infectious disease risk in Australia is currently organised.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We are indebted to our colleagues at the National University of Singapore for permission to use elements of their study design as a starting point for our Delphi survey. The work in Singapore is being conducted through the One Health, Zoonotic Diseases and Pandemic Planning Project: Creating a Bioethics Framework in Singapore; MOH/CDPHRG/0011/2014; Communicable Diseases Public Health Research Fund, Ministry of Health Singapore. Our research was funded by NHMRC Grant #1083079 Can One Health strategies be more effectively implemented through prior identification of public values?
Contributor Information
Chris Degeling, Email: chris.degeling@sydney.edu.au.
Jane Johnson, Phone: 61 2 9036 3411, Email: jane.johnson@sydney.edu.au.
References
- Allen-Scott LK, Buntain B, Hatfield JM, Meisser A, Thomas CJ. Academic institutions and one health: building capacity for transdisciplinary research approaches to address complex health issues at the animal–human–ecosystem interface. Academic Medicine. 2015;90(7):866. doi: 10.1097/ACM.0000000000000639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baum F. The new public health. Oxford: Oxford University Press; 2003. [Google Scholar]
- Binot A, Duboz R, Promburom P, et al. A framework to promote collective action within the One Health community of practice: using participatory modelling to enable interdisciplinary, cross-sectoral and multi-level integration. One Health. 2015;1:44–48. doi: 10.1016/j.onehlt.2015.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brookes V, Hernandez-Jover M, Black P, Ward M. Preparedness for emerging infectious diseases: pathways from anticipation to action. Epidemiology and infection. 2015;143(10):2043–2058. doi: 10.1017/S095026881400315X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC (2010) Operationalizing “One Health”: a policy perspective—taking stock and shaping an implementation roadmap: meeting overview. Stone Mountain, Georgia: Centers For Disease Control and Prevention
- Chien Y-J. How did international agencies perceive the avian influenza problem? The adoption and manufacture of the ‘One World, One Health’ framework. Sociology of Health & Illness. 2013;35(2):213–226. doi: 10.1111/j.1467-9566.2012.01534.x. [DOI] [PubMed] [Google Scholar]
- Coker R, Rushton J, Mounier-Jack S, et al. Towards a conceptual framework to support one-health research for policy on emerging zoonoses. The Lancet Infectious Diseases. 2011;11(4):326–331. doi: 10.1016/S1473-3099(10)70312-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degeling P. The significance of ‘sectors’ in calls for urban public health intersectroralism: an Australian perspective. Policy & Politics. 1995;23(4):289–301. doi: 10.1332/030557395782200518. [DOI] [Google Scholar]
- Ezenwa VO, Prieur-Richard A-H, Roche B, et al. Interdisciplinarity and infectious diseases: an Ebola case study. PLoS Pathog. 2015;11(8):e1004992. doi: 10.1371/journal.ppat.1004992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Medical Research Methodology. 2013;13:117. doi: 10.1186/1471-2288-13-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbs EPJ. The evolution of One Health: a decade of progress and challenges for the future. Veterinary Record. 2014;174(4):85–91. doi: 10.1136/vr.g143. [DOI] [PubMed] [Google Scholar]
- Häsler B, Gilbert W, Jones BA, Pfeiffer DU, Rushton J, Otte MJ. The economic value of One Health in relation to the mitigation of zoonotic disease risks. In: Mackenzie JS, Jeggo M, Daszak P, Richt JA, editors. One Health: The Human-Animal-Environment Interfaces in Emerging Infectious Diseases. Berlin: Springer; 2012. pp. 127–151. [Google Scholar]
- Hueston W, Appert J, Denny T, King L, Umber J, Valeri L. Assessing global adoption of one health approaches. EcoHealth. 2013;10(3):228–233. doi: 10.1007/s10393-013-0851-5. [DOI] [PubMed] [Google Scholar]
- Jones J, Hunter D. Consensus methods for medical and health services research. BMJ: British Medical Journal. 1995;311(7001):376. doi: 10.1136/bmj.311.7001.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keeney S, Hasson F, McKenna HP. A critical review of the Delphi technique as a research methodology for nursing. International Journal of Nursing Studies. 2001;38(2):195–200. doi: 10.1016/S0020-7489(00)00044-4. [DOI] [PubMed] [Google Scholar]
- Lee K, Brumme ZL. Operationalizing the One Health approach: the global governance challenges. Health Policy and Planning. 2013;28(7):778–785. doi: 10.1093/heapol/czs127. [DOI] [PubMed] [Google Scholar]
- Manlove KR, Walker JG, Craft ME, et al. “One health” or three? publication silos among the one health disciplines. PLoS Biol. 2016;14(4):e1002448. doi: 10.1371/journal.pbio.1002448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morens DM, Fauci AS (2012) Emerging infectious diseases in 2012: 20 years after the Institute of Medicine Report. mBio. doi:10.1128/mBio.00494-12 [DOI] [PMC free article] [PubMed]
- Okello AL, Bardosh K, Smith J, Welburn SC. One Health: Past successes and future challenges in three African contexts. PLoS Negl Trop Dis. 2014;8(5):e2884. doi: 10.1371/journal.pntd.0002884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okello A, Welburn S, Smith J. Crossing institutional boundaries: mapping the policy process for improved control of endemic and neglected zoonoses in sub-Saharan Africa. Health policy and planning. 2015;30(6):804–812. doi: 10.1093/heapol/czu059. [DOI] [PubMed] [Google Scholar]
- Phillips N, Bridgeman J, Ferguson-Smith M. The BSE inquiry. London: http://www.bseinquiry.gov.uk accessed on 12 February 2012: Stationery Office, 2000.
- Rosella LC, Wilson K, Crowcroft NS, et al. Pandemic H1N1 in Canada and the use of evidence in developing public health policies—a policy analysis. Social Science & Medicine. 2013;83:1–9. doi: 10.1016/j.socscimed.2013.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Routledge R. Fisher’s Exact Test. Encyclopedia of Biostatistics. New York: Wiley; 1998. pp. 1519–1523. [Google Scholar]
- Rüegg SR, McMahon BJ, Häsler B, Esposito R, et al. (2017) A blueprint to evaluate one health. Frontiers of Public Health. doi:10.3389/fpubh.2017.00020 [DOI] [PMC free article] [PubMed]
- Stärk KDC, Arroyo Kuribreña M, Dauphin G, et al. One Health surveillance—more than a buzz word? Preventive Veterinary Medicine. 2015;120(1):124–130. doi: 10.1016/j.prevetmed.2015.01.019. [DOI] [PubMed] [Google Scholar]
- Ziglio E. The Delphi method and its contribution to decision-making. In: Adler M, Ziglio E, editors. Gazing into the Oracle: The Delphi Method and its Application to Social Policy and Public Health. London: Jessica Kingsley Publishers; 1996. pp. 3–33. [Google Scholar]
- Zinsstag J. Convergence of ecohealth and one health. EcoHealth. 2012;9(4):371. doi: 10.1007/s10393-013-0812-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinsstag J, Schelling E, Wyss K, Mahamat B. Potential of cooperation between human and animal health to strengthen health systems. The Lancet. 2006;366(9503):2142–2145. doi: 10.1016/S0140-6736(05)67731-8. [DOI] [PubMed] [Google Scholar]
- Zinsstag J, Schelling E, Waltner-Toews D, Tanner M. From, “one medicine” to “one health” and systemic approaches to health and well-being. Preventive Veterinary Medicine. 2011;101(3–4):148–156. doi: 10.1016/j.prevetmed.2010.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinsstag J, Mackenzie J, Jeggo M, Heymann D, Patz J, Daszak P. Mainstreaming one health. EcoHealth. 2012;9(2):107–110. doi: 10.1007/s10393-012-0772-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


