Abstract
As the Ebola outbreak in West Africa wanes, it is time for the international scientific community to reflect on how to improve the detection of and coordinated response to future epidemics. Our interdisciplinary team identified key lessons learned from the Ebola outbreak that can be clustered into three areas: environmental conditions related to early warning systems, host characteristics related to public health, and agent issues that can be addressed through the laboratory sciences. In particular, we need to increase zoonotic surveillance activities, implement more effective ecological health interventions, expand prediction modeling, support medical and public health systems in order to improve local and international responses to epidemics, improve risk communication, better understand the role of social media in outbreak awareness and response, produce better diagnostic tools, create better therapeutic medications, and design better vaccines. This list highlights research priorities and policy actions the global community can take now to be better prepared for future emerging infectious disease outbreaks that threaten global public health and security.
Keywords: Ebola infection, emerging infectious diseases, epidemics, surveillance, one health, public health
Introduction
As the Ebola outbreak in West Africa that claimed more than 11,000 lives wanes (Zinszer et al. 2015), it is time for the international scientific community to reflect on the lessons learned from this epidemic and time to begin preparing for the next multi-country outbreak of an emerging infectious disease. What has the Ebola outbreak taught us about how we can detect and contain future events of other emerging infectious diseases more quickly? What have we learned about the gaps in public health and clinical systems that need to be resolved before the next epidemic? What laboratory tools can we use during future events to more rapidly develop and deploy diagnostic, therapeutic, and preventive technologies?
Infectious disease epidemiologists use an “agent–host–environment triad” to describe the factors that contribute to infection emergence and spread. The environmental factors include the natural environment and the built environment. The host factors include the range of social and behavioral characteristics and policies that facilitate or limit infection transmission and containment activities. The agent factors are those that relate to the particular virus, bacterium, fungus, protozoan, or helminth causing the outbreak. Using this framework, our interdisciplinary team identified key lessons learned from the Ebola outbreak that can be clustered into three areas: environmental conditions related to early warning systems, host characteristics related to public health, and agent issues that can be addressed through the laboratory sciences. The list below highlights actions the global community can take now to be better prepared for future emerging infectious disease events that threaten global public health and security.
Environmental Conditions Related to Early Warning Systems
We Need to Increase Proactive Zoonotic and Animal Surveillance Activities
More than 60% of the emerging infectious disease events that affected humans over the past several decades have been zoonotic in origin (Jones et al. 2008). The introduction and establishment of these zoonoses (that is, diseases usually affecting animals and not humans) in human populations is the result of a combination of changing human demography, health behaviors, agricultural practices, and other environmental interactions, all of which can expose humans to a large pool of novel pathogens (Morse et al. 2012). Ebola transmission, for example, may be linked to bushmeat consumption and exposure to bat guano (Bausch and Schwarz 2014). Rather than responding to dangerous infections only after they have moved into the human population, a better plan is to promote collaborative efforts to prevent infectious diseases from jumping from animal to human populations in the first place (Gortazar et al. 2014). Proactive support of surveillance, reporting, and trade regulation is better for health than a reactive approach (Hyatt et al. 2015).
The movement of animal pathogens across borders remains a significant risk to domestic animal health, wildlife conservation, and public health. Both well-known (but often neglected) zoonotic diseases and novel pathogens that are poorly characterized may cross national borders with ease (Munro and Savel 2015; Welburn et al. 2015). Incomplete data about diverse disease-causing agents, the geographies of these pathogens, and the impact of temperature and precipitation on disease epidemiology all leave animal and human populations vulnerable to emerging infections. Any comprehensive emerging infectious disease preparedness program must include zoonotic infection surveillance, and wildlife surveillance must become a higher global public health priority. The best defense against widespread infectious disease outbreaks in wildlife, domestic animals, and humans is active surveillance by international, transdisciplinary teams coupled with new strategies for creating buffers that restrict contact between pathogens and possible hosts.
One example of this type of early warning system is the United States Agency for International Development (USAID) Emerging Pandemic Threats program, which has supported the testing of thousands of wild animals living in geographic “hotspots” where novel pathogens that could become a threat to human health are likely to be identified (Dixon et al. 2014). These and other coalitions of government agencies, universities, non-governmental organizations, and other partners and stakeholders are seeking to generate new structures for global wildlife health management. But, despite multinational efforts at “virus hunting,” these research networks were unable to forecast the emergence of middle east respiratory syndrome (MERS) in 2012 or the 2014–2015 Ebola outbreak in West Africa. Although no previous human pandemic originating as a zoonosis has been predicted prior to making the jump to humans, new mathematical modeling programs, molecular diagnostic tools, advanced meta-genomic and communications technologies, and developments in proactive public health surveillance are available for deployment in improved early warning systems (Morse et al. 2012).
Necessary components of an improved system for early detection and response to emerging zoonoses include collaborative transdisciplinary efforts to assess local risks, develop and implement new technologies for screening new and existing pathogens, manage large amounts of shared information, create improved infectious disease models, and communicate quickly and effectively. Engagement with local human populations is also critical. Global zoonotic surveillance activities will only be successful when they are created and sustained with the support of local communities and stakeholders. Active involvement of local communities builds trust, improves participation in zoonotic monitoring activities, and fosters creative solutions to improving shortcomings in existing surveillance efforts.
Much more must be done to monitor diseases in wildlife globally, particularly in biodiversity hotspots. At present, there is no one international governmental agency that conducts comprehensive ecological surveillance and monitoring of diseases in animals, or that regulates trade in wild animals and their products (Hyatt et al. 2015). The Ebola outbreak has highlighted the critical need for a coordinated response to global surveillance for zoonotic diseases. Transdisciplinary approaches involving many parties, including human and animal health professionals, ecologists, economists, social scientists, modelers, and others, would help provide comprehensive, coordinated, and cohesive strategies for addressing this immense threat (Goodwin et al. 2012). Global zoonotic surveillance has become a necessity, not an optional policy goal.
We Need to Implement More Effective Ecological Health Interventions
The Ebola “outbreak narrative” propagated by many news media outlets presented the West African outbreak as a spontaneous event in which bushmeat consumption by low-income rural residents caused a zoonotic spillover and created an alarming threat to human health worldwide (Huff and Winnebah 2015). The reality is that human–ecological interactions are not merely about local behaviors but also about regional patterns of deforestation and land use, politics and economic development, and climate change (Huff and Winnebah 2015). Human movement into West African forests and the reduction of ecotones (that is, buffers between settlements and protected forests) created a forest–agricultural mosaic that increased contact between bats and humans (Despommier et al. 2006). This increased environmental exposure facilitated the Ebola virus making the leap from wildlife to humans (Alexander et al. 2015), likely as a result of exposure to insectivorous free-tailed bats, Mops condylurus (Saéz et al. 2015). Thereafter, residents of Ebola-affected areas received often confusing or contradictory messages about bushmeat consumption, burial practices, travel bans, traditional herbal medicines, and other issues related to ecological health (Alexander et al. 2015). Decades of political instability and conflict had eroded the regional infrastructure for water, sanitation, transportation, health services, and communication needed to enact recommendations for Ebola control. The economic implications of work shutdowns and disruptions in tourism and trade were disincentives to restrict movement of people, animals, and animal products. A lack of pre-positioned personal protective equipment (PPE), essential medications, and other biomedical supplies across much of the region put caregivers at unnecessarily high risk of contracting Ebola. Meanwhile, healthcare facilities and communities struggled with how best to decontaminate buildings and objects that had been touched by Ebola patients, disinfect medical equipment, and safely discard medical waste (Decker et al. 2014).
Although its epidemiology is not yet fully understood, Ebola virus in wild primates has contributed to a marked reduction in the populations of chimpanzees (Pan troglodytes) and gorillas (Gorilla gorilla) in Central Africa (Ryan and Walsh 2011). These outbreaks are likely the result of contact between these animals and an as-yet unidentified reservoir host, most likely a bat. Several human outbreaks of Ebola in the Central African region were traced back to the handling and consumption of primate bushmeat. And Ebola is far from the only infectious disease instigated or exacerbated by the condition of the natural and built environment.
More broadly, nearly one-quarter of the global burden of disease has been attributed to environmental risk factors, and that rate is even greater for infectious diseases (Prüss-Üstün and Corvalán 2007). Poor air quality contributes to tuberculosis and other respiratory infections, poor drinking water and sanitation cause nearly all cases of infectious diarrhea, and poor environmental management (including inappropriate pest control strategies and deforestation) increases the risk of malaria and other vectorborne infections. Low-income communities often lack the information and means to implement environmental changes that reduce the risk of outbreaks. A variety of occupational exposures put healthcare workers and others at risk of acquiring infections while on the job (Prüss-Üstün and Corvalán 2007). And many countries do not screen imported wildlife for the pathogens that they might harbor. Neglecting these ecological aspects of infection prevention and control puts individuals and communities at risk.
Environmental public health interventions—improved access to clean water for drinking and hygiene, animal and vector control, occupational health and safety measures, and promotion of larger buffers between human settlements and protected forests, among others—are an essential component of outbreak prevention (Patz et al. 2004; Wilcox and Ellis 2006). Environmental hygiene at healthcare facilities, schools, farms, transportation hubs, markets, and other places where people gather all need to be considered as well as larger-scale environmental control measures. The various outbreaks in 2014—Ebola, chikungunya, polio, dengue fever, cholera, and others, including the spread of highly pathogenic avian influenza (HPAI) types H5 and H7 in birds—demonstrate the results of inadequate environmental management for animal and public health in diverse world regions. International collaborations can identify and disseminate best practices for each of these situations. Governments and their partners must then implement health policies and programs with a One Health approach to prevent and respond promptly to emerging epidemics without compromising other ecosystem services and economic functions upon which global well-being depends.
Few official national or multinational programs are documenting wildlife diseases, and the partnerships seeking to undertake this important work are under-resourced. Wildlife surveillance in the places most likely to spark animal-to-human transmission of dangerous pathogens must be funded and implemented by international teams with the necessary expertise. Human health and domestic animal health surveillance systems must be linked with systems that monitor wildlife health. Investments in these types of programs will allow national governments and other organizations to develop and deploy countermeasures to minimize the risks wildlife-related epidemics pose to trade and economics as well as to biodiversity and public health (Karesh et al. 2012). Established groups such as the World Organization for Animal Health (OIE) will need to provide leadership on One Health initiatives addressing the interface between humans, domestic animals, and wildlife (Hyatt et al. 2015).
We Need to Expand Prediction Modeling
The 2014 outbreak of Ebola was the first to occur in West Africa, but post-outbreak zoonotic niche models revealed that the risk of Ebola transmission in West Africa was similar to that found in central Africa, where all previous Ebola outbreaks had happened (Pigott et al. 2014). This information suggests that the region’s susceptibility to Ebola may have been predictable before the first cases were diagnosed.
Outbreaks usually occur as the result of a complex and integrated set of biological, social, and environmental factors. Predictive modeling strategies vary considerably regarding which of these components are included in the models and which methodological approaches are used. Spatial statistical techniques can identify relationships between disease incidence, environmental and social conditions, and geographic location, then use those characteristics to predict disease risk in new locations with similar features and to simulate the risk of a large outbreak based on demographic, climatic, and other factors. Simulation modeling approaches, such as agent-based models, can emulate potential disease transmission within a region based on models of actions and interactions between animals and humans or between infected and uninfected individuals. Mathematical modeling of infection transmission can also provide frameworks for quantifying how quickly epidemics and epizootics will grow and for evaluating the possible impact of prevention and control interventions.
Because infectious disease outbreaks are usually explicitly spatiotemporal phenomena, modeling efforts largely focus on where and when an outbreak is likely to occur. Geographic information systems (GIS) offer a framework that is well suited for this task, providing the ability to incorporate, integrate, and analyze disparate geographic and non-geographic information about diseases. GIS methods can be quite accurate in their risk predictions. For example, a model of the risk of Rift Valley fever (RVF), a disease of livestock that can also affect humans, in eastern Africa successfully identified an elevated likelihood of new cases several weeks before the first ones were diagnosed (Anyamba et al. 2009). A diversity of online databases such as the EMPRES-i Global Animal Disease Information System, and the World Animal Health Information Database (WAHID) contain up-to-date animal case information, and human case information is available from HealthMap and other programs (Stevens and Pfeiffer 2015).
The ever-increasing amount and quality of available human, animal, and ecological data has improved the ability to explore relationships between human behaviors, environmental exposures, and infectious diseases. Emerging data sources such as volunteered and ambient geographic information (VGI and AGI) and novel monitoring platforms (such as unmanned aerial vehicles) will soon provide enhanced sensing capabilities.
The ability to predict when and where a disease outbreak is likely to occur and the probable severity of such an event creates valuable opportunities for the improvement of both pre- and post-outbreak intervention strategies and initiatives (Brookes et al. 2015). Communities and regions with limited emergency management resources that are predicted to have high risk of an outbreak can be offered tailored and timely assistance in building capacity for risk mitigation, preparedness, response, and recovery. The RVF example above demonstrates that predictive modeling of disease outbreaks is currently achievable, while the 2014 Ebola outbreak demonstrates the necessity of expanding and improving risk modeling efforts.
Public Health
We Need to Better Support Medical and Public Health Systems and Improve Local and International Responses to Epidemics
Local and international responses to the Ebola outbreak revealed profound limitations in preparedness for emerging infectious disease events. In West Africa, misinformation about Ebola transmission, prevention, and treatment caused confusion in the early months of the outbreak (Wilkinson and Leach 2015). The international response was poorly coordinated, and the World Health Organization (WHO) did not release an Ebola response plan until 5 months after the outbreak had crossed its first international border (Gostin 2014). The national governments of affected countries, foreign medical teams (such as those of Médecins Sans Frontières and other non-governmental organizations), WHO offices, the Global Outbreak Alert and Response Network (GOARN, an independent body coordinated by WHO), the U.S. Centers for Disease Control and Prevention (CDC), and others contributed to epidemiological and clinical efforts, but there was no strong central leadership (Burkle 2015). In the United States, frequent updates to CDC guidelines and reactionary state-implemented plans for quarantining travelers seemed to fuel fear rather than provide assurance that science was guiding policy development (Gonsalves and Staley 2014).
The policy and implementation challenges encountered during the Ebola outbreak will require evaluation by international experts in public health, international relations, law, human rights, and political science who can propose better options for coordinating responses to outbreaks and for clarifying the roles and responsibilities of the groups likely to participate in future containment efforts. One already-identified concern is that less than 20% of the member states of the United Nations have achieved the standards spelled out by the International Health Regulations (IHR) treaty, which mandates that member states develop the surveillance systems, laboratory capabilities, and health system capacity to contain epidemics (Burkle 2015). Little funding has been made available to promote rapid IHR improvements. Increasing financial support for the implementation of IHR globally is necessary for protecting the most vulnerable world citizens (Rothstein 2015) and safeguarding global health and security (Gostin 2014; Kimball and Heymann 2014).
In addition to supporting public health development, it is also necessary to strengthen clinical preparedness and response. Healthcare workers (HCWs) in Ebola-affected West African countries were one hundred times more likely to contract Ebola than their neighbors who were not HCWs (Kilmarx et al. 2014). In the United States, two nurses caring for an Ebola patient contracted the virus (Chevalier et al. 2014). In all affected countries, hospitals and public health authorities struggled with how to implement appropriate mechanisms for diagnosing, transporting, and caring for Ebola patients and identifying, monitoring, and communicating with at-risk travelers and possible contacts of Ebola patients. Many facilities also struggled with identifying and implementing appropriate procedures for disposing of contaminated medical waste and household items (Lowe et al. 2015). The Ebola outbreak highlighted the urgent need for all HCWs, including those involved in trash removal, patient transportation, and burials, to have access to the necessary PPE and to have comprehensive training about and constant supervision of safe practices for donning and doffing PPE (Nielsen et al. 2015). In low-income countries, few hospitals have adequate stocks of PPE and other medical supplies for routine use, and it can be difficult or impossible to garner the necessary supplies during an outbreak. PPE donations, volunteer medical workers, and other forms of international humanitarian assistance during crises like the Ebola outbreak are essential not only for containing epidemics before they become widespread but also for addressing issues of global and social justice (Rid and Emanuel 2014). Coordination of these efforts is essential for ensuring that timely assistance gets to the places with greatest need.
But improved responses to acute emergencies will not stave off the next outbreak. The ability to prevent rather than merely respond to infectious disease outbreaks requires long-term investment in the sustainable development of the healthcare infrastructure in currently under-resourced areas. Both clinical and public health capacities, such as routine surveillance and outbreak investigation, need to be expanded. The world needs to have an improved international detection, reporting, and response system in place before the next outbreak of an emergent infection like SARS, Ebola, or highly pathogenic strains of influenza. Additionally, improved mechanisms for local and national dissemination of critical information about emerging infectious disease threats must be put in place in every country so that public health officials, veterinary officials, and clinical staff can quickly prepare to safely diagnose, isolate, and care for possible cases while protecting HCWs from occupational risks.
We Need to Improve Risk Communication
The need for improved communication about the risk from Ebola and appropriate responses to the outbreak was apparent in every country where Ebola patients were diagnosed and treated. During the 2014 outbreak in West Africa, many were concerned about infection prevention behaviors not being adopted quickly enough as families continued to choose home care for sick relatives and funerals continued to attract crowds, turning some traditional burial ceremonies into super-spreader events (Pandey et al. 2014). In the United States, by contrast, some feared that they were likely to contract and die from Ebola even before the first Ebola patient had set foot on American soil. Similar observations about mismatches between actual threats to health and perceptions about risks have been made about a range of health issues, including measles vaccination, an issue that became a hot topic in early 2015 in the United States when a multi-state outbreak occurred as the hype about Ebola began dissipating (Clemmons et al. 2015).
One of the core principles of risk communication is that the hazards that kill are not necessarily those that upset or frighten, and the hazards that cause fear or anxiety may have that effect because of social and policy concerns rather than morbidity and mortality rates. Skilled communicators have the opportunity to clarify misperceptions and to promote healthier attitudes and behaviors. While influential public figures can cause mass alarm when they disseminate upsetting messages—for example, by proclaiming that measles vaccines are dangerous even though scientists have declared them safe—these voices do not have to become the dominant ones (Kahan 2013). Messages explaining that vaccination rates remain high—that is, that vaccination remains the normative health behavior for the population—help promote adherence to expert recommendations by emphasizing that vaccination is the popular choice (Kahan 2013).
Best practices for risk communication during infectious disease outbreaks are being developed (Schiavo et al. 2014). During a recent Ebola outbreak in Uganda, village health teams selected by community members conducted home searches and contact tracing while also providing preventive health education (Mbonye et al. 2014). Because team members were elected from the communities they serve, they were accepted and trusted, and this resulted in greater adherence to recommended practices such as safe burials and limited interpersonal interactions (Mbonye et al. 2014). In Liberia, a task force led by local chiefs helped design and implement a village-to-village social mobilization program to address Ebola-related concerns, collect daily health surveillance data, and provide timely health education (Hagan et al. 2015).
At the global level, disaster simulations provide public information officers and health communication experts with the tools they need to perform excellently in stressful situations (Vanderford 2015), and drills with international teams may also enhance capacity for interagency cooperation during health emergencies (Gostin 2014). Additional research will elucidate evidence-based best practices for earning trust, creating awareness, deepening understanding, gaining agreement, and motivating enactment of best practices for managing uncertain physical hazards. Understanding cultural values and traditions is an essential component of infectious disease risk communication. Anthropologists, sociologists, psychologists, and other social scientists may play an important role in identifying cultural considerations to incorporate into communication strategies. Improving risk communication throughout the span of an outbreak, from the initial cases through the after-event reporting, is essential for promoting good health behaviors and preventing harmful ones.
We Need to Better Understand the Role of Social Media in Outbreak Awareness and Response
The formal press played a key role in communicating information and, sometimes, fear about the Ebola outbreak (Spencer 2015), but social media—Twitter, WhatsApp, and other programs—may have been even more influential in guiding how individuals reacted to the emerging situation. This was true in West Africa, where more than half of the population has a mobile phone subscription (O’Donovan and Bersin 2015), as well as in Europe and North America. In Nigeria, where an imported case of Ebola led to more than a dozen infected HCWs, tweeting and retweeting of misinformation was common, but the government also used Twitter to correct falsehoods (Oyeyemi et al. 2014). Ebola went more dramatically “viral” when the pathogen arrived in the United States and a fearful public looked to Internet and social media sites to find and disseminate disease-related information. Google searches for the keyword Ebola first spiked on August 8, 2014, when WHO declared Ebola to be a public health emergency, and then soared in mid-October after the first patient was diagnosed in Texas (Househ 2015). The Google Trends score remained elevated as a patient in New York City was diagnosed, treated, and discharged from the hospital, and then returned to a low level of interest by early 2015. Similarly, #ebola became a globally trending hashtag on Twitter. Our Geosocial Gauge prototype (Croitoru et al. 2013) logged more than 200,000 tweets daily during the first half of October, with that number spiking to more than 500,000 tweets—nearly 350 tweets per minute—on October 9, the day after an Ebola patient in Texas died from the infection. By January 2015, the number of Ebola tweets logged through this system was down to about 8000 daily.
These illustrations, from two countries that differ substantially in their levels of technological infrastructure but share the will of the general public to participate in information dissemination, demonstrate how social media and mHealth (mobile health) applications can be an important part of tracking outbreaks, providing health education, and receiving and disseminating other critical information (O’Donovan and Bersin 2015). When the information disseminated through social media is not curated and may therefore be incorrect (Oyeyemi et al. 2014), it may contribute to public confusion. However, early studies have highlighted the potential usefulness of Twitter-mining and other analyses for improving public health education (Odlum and Yoon 2015). In sum, big data sets raise both new challenges and new opportunities for health informatics. New applications that mine and analyze social media (Fig. 1) are needed to reveal novel ways to trace the spatiotemporal and social footprints of outbreaks and provide a more timely response to social and healthcare needs (Croitoru et al. 2013). For example, social media analysis can help identify which locations require assistance with basic human needs such as food and water and to alert residents about healthcare facilities that have suspended admissions.
Fig. 1.
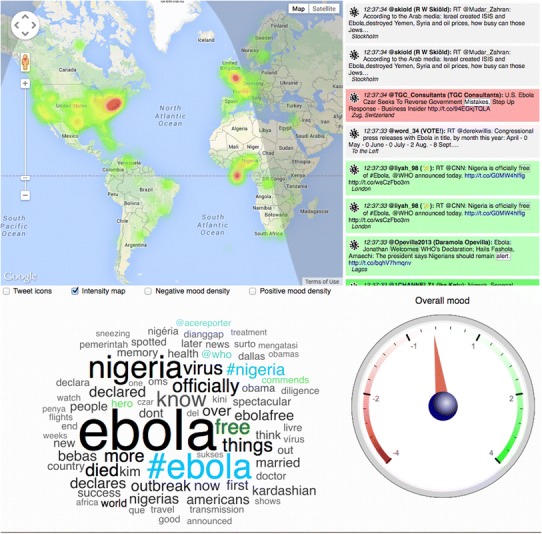
A snapshot of streaming Twitter content discussing Ebola on October 20, 2014. The map on the top left shows the hotspots of discussion. The window of the top right shows streaming tweets, classified into ones with a positive outlook (green), negative (red), or neutral (no color). The word cloud (bottom left) captures the key discussion points, while the gauge (bottom right) captures the overall mood of the crowd [A grayscale version of this image can be provided for the print version of the paper] (Color figure online).
However, a current lack of understanding of the mechanisms that drive social media participation and engagement hinders the ability to fully harness the power of cyberspace during health crises and other emergencies. Traditional models of the social amplification of risk fail to capture the complex mechanisms through which the disease-related narrative is shaped in cyberspace (Kasperson et al. 1988). Studying the geosocial nature of participation patterns to gain a better understanding of how a narrative is formed and propagated may also allow for evaluation of the effectiveness of top-down communication from governmental health agencies to the general public as well as the influence of bottom-up processes on public perception (Winerman 2009). Future public health campaigns have to make better use of these modern communication tools for improving preparedness and response.
Laboratory Sciences
We Need to Produce Better Diagnostic Tools
Laboratory tests that rapidly and reliably diagnose infections, ideally even in the early asymptomatic stages, often play a key role in outbreak containment strategies (Stamm 2015). For maximum effectiveness, medical and veterinary diagnostic tests must be sensitive and specific, they must provide rapid results, they must be affordable, and they must use technology that is user-friendly and accessible in diverse settings (Stothard and Adams 2014). Early diagnosis allows infected individuals to be isolated before they infect community members, provides HCWs with critical information about how to protect themselves and care for patients, and may improve clinical outcomes by enabling treatment to begin early in the course of infection. Biomarker-based analyses that can be carried out at the point-of-care or in a central laboratory may also be useful for the early detection of infection in contacts of infected people and for the screening of community volunteers to establish geographic areas where an infection with an environmental reservoir might be present (Reed et al. 2014).
Current Ebola diagnostics are based either on the detection of the virus (through RT-PCR or antigen testing) in body fluids or on the measurement of antibody response (Martin et al. 2015). None of the currently approved methods accurately detect the virus during the incubation period or at the beginning of the symptomatic phase (Martin et al. 2015). New techniques for the rapid creation of easy-to-use, safe, and accurate diagnostic tools are necessary for improving the early containment of emerging threats to global public health. Given the limited laboratory capabilities in many world regions, and the related lack of reliable access to electricity, clean water, and reagents, the ideal tests will also be affordable and able to be used at the point of care.
Traditional laboratory testing has been used mostly for the identification of pathogens. In recent years, new approaches such as transcriptional profiling have extended diagnostic capabilities (Ginsburg and Woods 2012). Laboratory studies exploring the interactions between the immune system and pathogens can now lead to the identification of genomic and proteomic markers predictive of individual susceptibility to and likely prognoses for specific infectious diseases (Burgner et al. 2006). The development of novel platforms capable of identifying specific signatures at both the genomic and proteomic levels may help researchers understand the immune pathogenesis of emerging infections and may lead to the identification of humans with higher risk for developing a disease.
Due to the high priority on a quick roll-out of new tests, pre-symptomatic assays should not concentrate on achieving absolute viral specificity, but rather on the recognition of a general viral intrusion, which may be achieved by comparison of the activation level of host defenses to the patient-specific baseline. Several pressing research areas have been identified. We need to develop multiplex biomarker platforms that can be used in triage as tools for differential diagnosis as well as for identifying individuals with co-infections (Yen et al. 2015). We need new molecular assays for rapid subtyping of filoviruses like Ebola as well as coronaviruses, retroviruses, and other pathogens. We need to create tools for identifying biomarkers associated with clinical outcomes and patient responses to therapy, which might allow for personalized medical care. We need tools that will help to identify individuals who might be especially susceptible to infection, and who might benefit most from preventive interventions. Once these new types of diagnostics are developed, additional work can be done to improve the sensitivity, specificity, and cost effectiveness of the tests. But the first priority is ramping up the ability to quickly develop tools during public health crises.
We Need to Create Better Therapeutic Medications
As soon as the 2014 Ebola outbreak hit the airwaves, calls went out for novel therapeutics to treat the infection. Drugs like ZMapp, TKM-Ebola, and Favipiravir were moved quickly into early-stage trials, but by early 2015 there was still no strong evidence that any of these drugs were highly effective against human Ebola virus disease (Choi et al. 2015).
When outbreaks occur, the first step of a rapid therapeutic response strategy should be to identify existing, already-approved therapeutic agents that might increase survival. The standard doses and durations of drug administration for diseases in which the drug has proven to be effective may be quite different from the regimen that is most effective for other infectious agents. The urgent demand for new and repurposed therapeutics during an outbreak situation does not remove the need to protect patients from the risk of additional harm due to inappropriate use of medications (Enserink 2014).
It is also important to speed up the process of developing new medications. Traditional therapeutics target bacteria, viruses, and parasites, but a better option for future outbreaks may be the development of host-based therapeutics that target human cells or components in a manner that affords broad-spectrum protection to the host (Princhard and Kern 2012; Prussia et al. 2011; Zhou et al. 2015). The lack of market value for specific antivirals for infections that do not affect a large proportion of the world population means that incentives to pharmaceutical companies may be required in order to encourage corporations to divert existing resources into an accelerated production program when an outbreak with high likelihood for expansion has been detected. Host-based therapeutics that have demonstrated broad-spectrum in vivo efficacy in animal models should be candidates for prioritization. Decisions about when to allow use of a candidate drug based on compassionate use prior to extensive field testing will require a critical evaluation of drug-associated risk versus the risk of mortality from the disease.
Setting up high-quality clinical trials with suitable cohorts of participants is expensive and demanding even in optimal circumstances. Trials are even more challenging to conduct during ongoing outbreaks. During emergencies, there may be a temptation to bypass the usual ethical and regulatory requirements for drug testing, or to make decisions about the effectiveness of a medication before having a sample size large enough for robust statistical conclusions. A focused research question may help minimize both the required number of participants and the duration of time needed to make a valid assessment of the benefits and risks of a candidate drug. Other limitations can be overcome when governmental and intergovernmental agencies provide leadership on leveraging existing research capacities in the communities from which participants can be drawn, making advanced laboratory capabilities available to collaborating researchers, facilitating data sharing across study sites, and providing guidance on how to maintain compliance with ethical guidelines for human subjects research. These compulsory ethical practices include an emphasis on informed consent of all participants, the protection of vulnerable populations, the implementation of safety monitoring procedures, the management and reporting of adverse events, and the protection of patient privacy and confidentiality. The ethics of using a control group must be carefully considered based on the characteristics of the pathogen causing the outbreak and the preliminary results about outcomes for both the intervention and control populations.
We Need to Design Better Vaccines
To be effective during an outbreak, a vaccine must either be efficacious as post-exposure prophylaxis or must be able to stimulate the production of protective or neutralizing antibodies within a very short time window, usually no more than a few days. When this type of vaccine is not available, a more useful prophylactic strategy is the use of passive immunization approaches (such as the administration of therapeutic monoclonal antibodies) that are specific to the pathogen causing the outbreak and have few negative side effects (Clementi et al. 2012; Sautto et al. 2013). Immunomolecule-based interventions should only be implemented after the consideration of the possible risks, including antigen-dependent enhancement of the infectious disease and immunological interference with innate immunity (Wang et al. 2014). In contrast, vaccines can be very effective for protecting healthcare personnel being deployed to affected areas and for safeguarding as-yet unaffected communities within a region hit by an outbreak of a virulent infectious disease.
Several Ebola vaccines were in development prior to the emergence of Ebola in West Africa, and they are being quickly pushed into field trials (Choi et al. 2015). To be deemed successful, these vaccines will need to produce a strong primary response to the antigen, even if a sustained response may not be maintained. The preliminary results of a ring vaccination trial that immunized individuals known to be primary or secondary contacts of Ebola patients suggest that it is likely that an effective Ebola vaccine will soon be available (Henao-Restrepo et al. 2015). The “ring” strategy employed in this trial is a creative new approach to the ethical and efficient conduct of efficacy and product safety research during an ongoing outbreak, but there is a need for further clarification of the ethics and legality of various approaches to the testing of candidate vaccines during emergency situations (Cohen and Kupferschmidt 2014).
Prior knowledge of host responses in multiple cell types that may respond to vaccine candidates (such as dendritic cell, B-cell, and T-cell responses) and to additives such as adjuvants can greatly support emergency efforts to maximize efficacy of vaccine formulations in producing such strong primary responses in vaccines. Similar strategies may also apply to the use of vaccination to prevent infection in animal populations, as has been observed for foot-and-mouth (hoof-and-mouth) disease and containment efforts for other highly contagious animal pathogens (Paton et al. 2005).
If combinatorial vaccines that protect against two or more infectious diseases or combinatorial interventions that provide both a preventive and therapeutic intervention in one are used (Kamal et al. 2011), or if multiple doses of vaccine are expected to be necessary, then additional safety studies will be required to determine tolerance to additives (such as preservatives) and to repeated doses of the antigen. Definitive assays that can predict unfavorable outcomes in individuals may be an important part of a safety strategy. Vigilant monitoring for adverse events associated with primary and booster doses will be required for any new vaccine. Similar considerations apply to the development and testing of animal vaccines (Delwart 2012).
Conclusion
These lessons learned from the Ebola outbreak point to critical research needs: enhanced wildlife and biosurveillance methods, expanded environmental and ecological assessments and intervention studies, improved modeling capabilities, more evaluations of health systems and public health needs and policies, better risk communication and social media strategies, and the application of cutting-edge laboratory science to the rapid development, ethical testing, manufacturing, and distribution of new diagnostic, therapeutic, and preventive tools. They also point to urgent needs that can be addressed through policy prioritization: support for early warning systems, health systems development, and translational medicine. We cannot wait until the next crisis to implement these changes. We must act now to ensure that we are better prepared for the next international health emergency.
A multi-pronged, transdisciplinary strategy that integrates the biomedical sciences (including cellular and molecular biology), public health, and the ecological sciences is required to address emerging infectious diseases from the individual and local to the global levels (Ezenwa et al. 2015). The recent Ebola outbreak challenges the notion that human health is an isolated concern removed from the bounds of ecology and species interactions. Human health, animal health, and ecosystem health are moving closer together, and at some point it will be inconceivable that there was ever a clear division (Zinsstag et al. 2012). Policymakers, health managers, and ecologists need a data-driven decision support system that allows practitioners to use adaptive management approaches to address dynamic disease situations. At the heart of any solution-oriented agenda is the need for better problem definition, and this list of action items provides a starting point for identifying priority actions for emerging infectious disease preparedness and response.
References
- Alexander KA, Sanderson CE, Marathe M, Lewis BL, Rivers CM, Shaman J, et al. What factors might have led to the emergence of Ebola in West Africa? PLoS Neglected Tropical Diseases. 2015;9:e0003652. doi: 10.1371/journal.pntd.0003652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anyamba A, Chretien JP, Small J, Tucker CJ, Formenty PB, Richardson JH, et al. Prediction of a Rift Valley fever outbreak. Proceedings of the National Academy of Sciences of the United States of America. 2009;106:955–959. doi: 10.1073/pnas.0806490106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bausch DG, Schwarz L. Outbreak of Ebola virus disease in Guinea: where ecology meets economy. PLoS Neglected Tropical Diseases. 2014;8:e3056. doi: 10.1371/journal.pntd.0003056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brookes VJ, Hernández-Jover M, Black PF, Ward MP. Preparedness for emerging infectious diseases: pathways from anticipation to action. Epidemiology & Infection. 2015;143:2043–2058. doi: 10.1017/S095026881400315X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgner D, Jamieson SE, Blackwell JM. Genetic susceptibility to infectious diseases: big is beautiful, but will bigger be even better? Lancet Infectious Diseases. 2006;6:653–663. doi: 10.1016/S1473-3099(06)70601-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burkle FM. Global health security demands a strong International Health Regulations treaty and leadership from a highly resourced World Health Organization. Disaster Medicine and Public Health Preparedness. 2015;9:568–580. doi: 10.1017/dmp.2015.26. [DOI] [PubMed] [Google Scholar]
- Chevalier MS, Chung W, Smith J, Weil LM, Hughes SM, Joyner SN, et al. Ebola virus disease cluster in the United States: Dallas County, Texas, 2014. MMWR Morbidity and Mortality Weekly Report. 2014;63:1087–1088. [PMC free article] [PubMed] [Google Scholar]
- Choi WY, Hong KJ, Hong JE, Lee WJ. Progress of vaccine and drug development for Ebola preparedness. Clinical and Experimental Vaccine Research. 2015;4:11–16. doi: 10.7774/cevr.2015.4.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clementi N, Criscuolo E, Casterlli M, Clementi M. Broad-range neutralizing anti-influenza A human monoclonal antibodies: new perspectives in therapy and prophylaxis. New Microbiologica. 2012;35:399–406. [PubMed] [Google Scholar]
- Clemmons NS, Gastanaduy PA, Fiebelkorn AP, Redd SB, Wallace GS. Measles—United States, January 4–April 2, 2015. MMWR Morbidity and Mortality Weekly Report. 2015;64:373–376. [PMC free article] [PubMed] [Google Scholar]
- Cohen J, Kupferschmidt K. Ebola vaccine trials raise ethical issues. Science. 2014;346:289–290. doi: 10.1126/science.346.6207.289. [DOI] [PubMed] [Google Scholar]
- Croitoru A, Crooks A, Radzikowski J, Stefanidis A. Geospatial gauge: a system prototype for knowledge discovery from social media. International Journal of Geographical Information Science. 2013;27:2483–2508. doi: 10.1080/13658816.2013.825724. [DOI] [Google Scholar]
- Decker BK, Sevransky JE, Barrett K, Davey RT, Chertow DS. Preparing for critical care services to patients with Ebola. Annals of Internal Medicine. 2014;161:831–832. doi: 10.7326/M14-2141. [DOI] [PubMed] [Google Scholar]
- Delwart E. Animal virus discovery: improving animal health, understanding zoonoses, and opportunities for vaccine development. Current Opinion in Virology. 2012;2:344–352. doi: 10.1016/j.coviro.2012.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Despommier D, Ellis BR, Wilcox BA. The role of ecotones in emerging infectious diseases. EcoHealth. 2006;3:281–289. doi: 10.1007/s10393-006-0063-3. [DOI] [Google Scholar]
- Dixon MA, Dar OA, Heymann DL. Emerging infectious diseases: opportunities at the human-animal-environment interface. Veterinary Record. 2014;174:546–551. doi: 10.1136/vr.g3263. [DOI] [PubMed] [Google Scholar]
- Enserink M. Infectious diseases: debate erupts on “repurposed” drugs for Ebola. Science. 2014;345:718–719. doi: 10.1126/science.345.6198.718. [DOI] [PubMed] [Google Scholar]
- Ezenwa VO, Prieur-Richard AH, Roche B, Bailly X, Becquart P, García-Peña GE, et al. Interdisciplinarity and infectious diseases: an Ebola case study. PLoS Pathogens. 2015;11:e1004992. doi: 10.1371/journal.ppat.1004992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsburg GS, Woods CW. The host response to infection: advancing a novel diagnostic paradigm. Critical Care. 2012;16:168. doi: 10.1186/cc11685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonsalves G, Staley P. Panic, paranoia, and public health: the AIDS epidemic’s lessons for Ebola. New England Journal of Medicine. 2014;371:2348–2349. doi: 10.1056/NEJMp1413425. [DOI] [PubMed] [Google Scholar]
- Goodwin R, Schley D, Lai KM, Ceddia GM, Barnett J, Cook N. Interdisciplinary approaches to zoonotic disease. Infectious Disease Reports. 2012;4:e37. doi: 10.4081/idr.2012.e37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gortazar C, Reperant LA, Kuiken T, de la Fuente J, Boadella M, Martínez-Lopez B, et al. Crossing the interspecies barrier: opening the door to zoonotic pathogens. PLoS Pathogens. 2014;10:e1004129. doi: 10.1371/journal.ppat.1004129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gostin LO. Ebola: towards an International Health Systems Fund. Lancet. 2014;384:e49–e51. doi: 10.1016/S0140-6736(14)61345-3. [DOI] [PubMed] [Google Scholar]
- Hagan JE, Smith W, Pillai SK, Yeoman K, Gupta S, Neatherlin J, et al. Implementation of Ebola case-finding using a village chieftaincy taskforce in a remote outbreak—Liberia, 2014. MMWR Morbidity and Mortality Weekly Report. 2015;64:183–185. [PMC free article] [PubMed] [Google Scholar]
- Henao-Restrepo AM, Longini IM, Egger M, Dean NE, Edmunds WJ, Camacho A, et al. Efficacy and effectiveness of an rVSV-vectored vaccine expressing Ebola surface glycoprotein: interim results from the Guinea ring vaccination cluster-randomized trial. Lancet. 2015;386:857–866. doi: 10.1016/S0140-6736(15)61117-5. [DOI] [PubMed] [Google Scholar]
- Househ M. Communicating Ebola through social media and electronic news media outlets: a cross-sectional study. Health Informatics Journal. 2015 doi: 10.1177/1460458214568037. [DOI] [PubMed] [Google Scholar]
- Huff AR, Winnebah T (2015) Ebola, politics and ecology: beyond the “Outbreak Narrative.” Institute of Development Studies (IDS) Practice Paper in Brief 20
- Hyatt A, Aguirre AA, Jeggo M, Woods R. Effective coordination and management of emerging infectious diseases in wildlife. EcoHealth. 2015;12:408–411. doi: 10.1007/s10393-015-1045-0. [DOI] [PubMed] [Google Scholar]
- Jones KE, Patel NG, Levy MA, Storeygard A, Balk D, Gittleman JL, Daszak P. Global trends in emerging infectious diseases. Nature. 2008;451:990–993. doi: 10.1038/nature06536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahan DM. A risky science communication environment for vaccination. Science. 2013;42:53–54. doi: 10.1126/science.1245724. [DOI] [PubMed] [Google Scholar]
- Kamal SM, Rashid AK, Bakar MA, Ahad MA. Anthrax: an update. Asian Pacific Journal of Tropical Biomedicine. 2011;1:496–501. doi: 10.1016/S2221-1691(11)60109-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karesh WB, Dobson A, Lloyd-Smith JO, Lubroth J, Dixon MA, Bennett M, et al. Ecology of zoonoses: natural and unnatural histories. Lancet. 2012;380:1936–1945. doi: 10.1016/S0140-6736(12)61678-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasperson RE, Renn O, Slovic P, Brown HS, Emel J, Goble R, et al. The social amplification of risk: a conceptual framework. Risk Analysis. 1988;8:177–187. doi: 10.1111/j.1539-6924.1988.tb01168.x. [DOI] [Google Scholar]
- Kilmarx PH, Clarke KR, Dietz PM, Hamel MJ, Husain F, McFadden JD, et al. Ebola virus disease in health care workers: Sierra Leone, 2014. MMWR Morbidity and Mortality Weekly Report. 2014;63:1168–1171. [PMC free article] [PubMed] [Google Scholar]
- Kimball AM, Heymann D. Ebola, International Health Regulations, and global safety. Lancet. 2014;384:2023. doi: 10.1016/S0140-6736(14)62330-8. [DOI] [PubMed] [Google Scholar]
- Lowe JJ, Gibbs SG, Schwedhelm S, Nguyen J, Smith PW. Nebraska Biocontainment Unit perspective on disposal of Ebola medical waste. American Journal of Infection Control. 2015;42:1256–1257. doi: 10.1016/j.ajic.2014.10.006. [DOI] [PubMed] [Google Scholar]
- Martin P, Laupland KB, Frost EH, Valiquette L. Laboratory diagnosis of Ebola virus disease. Intensive Care Medicine. 2015;41:895–898. doi: 10.1007/s00134-015-3671-y. [DOI] [PubMed] [Google Scholar]
- Mbonye AK, Wamala JF, Nanyunja M, Opio A, Makumbi I, Aceng JR. Ebola viral hemorrhagic disease outbreak in West Africa: lessons from Uganda. African Health Sciences. 2014;14:495–501. doi: 10.4314/ahs.v14i3.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morse SS, Mazet JAK, Woolhouse M, Parrish CR, Carroll D, Karesh WB, et al. Prediction and prevention of the next pandemic zoonosis. Lancet. 2012;380:1956–1965. doi: 10.1016/S0140-6736(12)61684-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munro CL, Savel RH. Viral outbreaks in an age of global citizenship. American Journal of Critical Care. 2015;24:4–6. doi: 10.4037/ajcc2015809. [DOI] [PubMed] [Google Scholar]
- Nielsen CF, Kidd S, Sillah ARM, Davis E, Mermin J, Kilmarx PH. Improving burial practices and cemetery management during an Ebola virus disease epidemic—Sierra Leone, 2014. MMWR Morbidity and Mortality Weekly Report. 2015;64:20–27. [PMC free article] [PubMed] [Google Scholar]
- O’Donovan J, Bersin A. Controlling Ebola through mHealth strategies. Lancet Global Health. 2015;3:e22. doi: 10.1016/S2214-109X(14)70357-2. [DOI] [PubMed] [Google Scholar]
- Odlum M, Yoon S. What can we learn about the Ebola outbreak from tweets? American Journal of Infection Control. 2015;43:563–571. doi: 10.1016/j.ajic.2015.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oyeyemi SO, Gabarron E, Wynn R. Ebola, Twitter, and misinformation: a dangerous combination? BMJ. 2014;349:g6178. doi: 10.1136/bmj.g6178. [DOI] [PubMed] [Google Scholar]
- Paton DJ, Valarcher JF, Bergmann I, Matlho OG, Zakharov VM, Palma EL, Thomson GR. Selection of foot and mouth disease vaccine strains: a review. Revue Scientifique et Technique. 2005;24:981–993. doi: 10.20506/rst.24.3.1632. [DOI] [PubMed] [Google Scholar]
- Pandey A, Atkins KE, Medlock J, Wenzel N, Townsend JP, Childs JE, et al. Strategies for containing Ebola in West Africa. Science. 2014;346:991–995. doi: 10.1126/science.1260612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patz JA, Daszak P, Tabor GM, Aguirre AA, Pearl MC, Epstein J, et al. Unhealthy landscapes: policy recommendations pertaining to land use change and disease emergence. Environmental Health Perspectives. 2004;112:1092–1098. doi: 10.1289/ehp.6877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pigott DM, Golding N, Mylne A, Huang Z, Henry AJ, Weiss DJ, et al. Mapping the zoonotic niche of Ebola virus disease in Africa. Life. 2014;3:e04395. doi: 10.7554/eLife.04395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Princhard MN, Kern ER. Orthopoxvirus targets for the development of new antiviral agents. Antiviral Research. 2012;94:111–125. doi: 10.1016/j.antiviral.2012.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prussia A, Thepchatri P, Snyder JP, Plemper RK. Systematic approaches towards the development of host-directed antiviral therapeutics. International Journal of Molecular Sciences. 2011;12:4027–4052. doi: 10.3390/ijms12064027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prüss-Üstün A, Corvalán C. How much disease burden can be prevented by environmental interventions? Epidemiology. 2007;18:167–178. doi: 10.1097/01.ede.0000239647.26389.80. [DOI] [PubMed] [Google Scholar]
- Reed PE, Mulangu S, Cameron KN, Ondzie AU, Joly D, Bermejo M, et al. A new approach for monitoring ebolavirus in wild great apes. PLoS Neglected Tropical Diseases. 2014;8:e3143. doi: 10.1371/journal.pntd.0003143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rid A, Emanuel EJ. Why should high-income countries help combat Ebola? JAMA. 2014;312:1297–1298. doi: 10.1001/jama.2014.12869. [DOI] [PubMed] [Google Scholar]
- Rothstein MA. The moral challenge of Ebola. American Journal of Public Health. 2015;105:6–8. doi: 10.2105/AJPH.2014.302413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan SJ, Walsh PD. Consequences of non-intervention for infectious disease in African great apes. PLoS One. 2011;6:29030. doi: 10.1371/journal.pone.0029030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saéz AM, Weiss S, Nowak K, Lapeyre V, Zimmermann F, Düx A, et al. Investigating the zoonotic origin of the West African Ebola epidemic. EMBO Molecular Medicine. 2015;7:17–23. doi: 10.15252/emmm.201404792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sautto G, Mancini N, Gorini G, Clementi M, Burioni R. Possible future monoclonal antibody (mAb)-based therapy against arbovirus infections. BioMed Research International. 2013;2013:848491. doi: 10.1155/2013/838491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiavo R, May Leung M, Brown M. Communicating risk and promoting disease mitigation measures in epidemics and emerging disease settings. Pathogens and Global Health. 2014;108:76–94. doi: 10.1179/2047773214Y.0000000127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer C. Having and fighting Ebola: public health lessons from a clinician turned patient. New England Journal of Medicine. 2015;372:1089–1091. doi: 10.1056/NEJMp1501355. [DOI] [PubMed] [Google Scholar]
- Stamm LV. Ebola virus disease: rapid diagnosis and timely case reporting are critical to the early response for outbreak control. American Journal of Tropical Medicine and Hygiene. 2015;93:438–440. doi: 10.4269/ajtmh.15-0229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens KB, Pfeiffer DU. Sources of spatial animal and human health data: casting the net wide to deal more effectively with increasingly complex disease problems. Spatial and Spatio-temporal Epidemiology. 2015;13:15–29. doi: 10.1016/j.sste.2015.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stothard JR, Adams E. A preface on advances in diagnostics for infectious and parasitic diseases: detecting parasites of medical and veterinary importance. Parasitology. 2014;141:1781–1788. doi: 10.1017/S0031182014001309. [DOI] [PubMed] [Google Scholar]
- Vanderford ML. Emergency risk communication: reflections on a year of accelerating global engagement. Spectra: The Magazine of the National Communication Association. 2015;51:8–12. [Google Scholar]
- Wang SF, Tseng SP, Yen CH, Yang JY, Tsao CH, Shen CW, et al. Antibody-dependent SARS coronavirus infection is mediated by antibodies against spike proteins. Biochemical and Biophysical Research Communications. 2014;451:208–214. doi: 10.1016/j.bbrc.2014.07.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welburn SC, Beange I, Ducrotory MJ, Okello AL. The neglected zoonoses: the case for integrated control and advocacy. Clinical Microbiology and Infection. 2015;21:433–443. doi: 10.1016/j.cmi.2015.04.011. [DOI] [PubMed] [Google Scholar]
- Wilcox BA, Ellis B. Forests and emerging infectious diseases of humans. Unasylva. 2006;57:11–18. [Google Scholar]
- Wilkinson A, Leach M. Briefing: Ebola myths, realities, and structural violence. African Affairs. 2015;114:136–148. doi: 10.1093/afraf/adu080. [DOI] [Google Scholar]
- Winerman L. Social networking: crisis communication. Nature. 2009;457:376–378. doi: 10.1038/457376a. [DOI] [PubMed] [Google Scholar]
- Yen CW, de Puig H, Tam JO, Gómez-Márquez J, Bosch I, Hamad-Schifferli K, Gehrke L. Multicolored silver nanoparticles for multiplexed disease diagnostics: distinguishing dengue, yellow fever, and Ebola viruses. Lab on a Chip. 2015;15:1638–1641. doi: 10.1039/C5LC00055F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Y, Vendantham P, Lu K, Agudelo J, Carrion R, Nunneley JW, et al. Protease inhibitors targeting coronavirus and filovirus entry. Antiviral Research. 2015;116:76–84. doi: 10.1016/j.antiviral.2015.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinsstag J, Mackenzie JS, Jeggo M, Heymann DL, Patz JA, Daszak P. Mainstreaming one health. EcoHealth. 2012;9:107–110. doi: 10.1007/s10393-012-0772-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinszer K, Morrison K, Anema A, Majumder MS, Brownstein JS. The velocity of Ebola spread in parts of West Africa. Lancet Infectious Diseases. 2015;15:1005–1007. doi: 10.1016/S1473-3099(15)00234-0. [DOI] [PubMed] [Google Scholar]


