Abstract
Asians are disproportionately affected by chronic hepatitis B (HBV) infection and its fatal consequences. The Hep B Free campaign was launched to eliminate HBV in San Francisco by increasing awareness, testing, vaccination and linkage to care. The campaign conducted 306 street intercept and telephone interviews of San Francisco Asians to assess current levels of HBV knowledge, testing behaviors and effectiveness of existing campaign media materials. One-third of respondents ranked HBV as a key health issue in the Asian community, second to diabetes. General HBV awareness is high (85%); however, a majority could not name an effective prevention method. Sixty percent reported having been tested for HBV; provider recommendation was the most often cited reason for testing. Respondents reported a high level of trust in their providers to correctly assess which health issues they may be at risk for developing and test accordingly, confirming that efforts to increase HBV testing among Asians must simultaneously mobilize the public to request testing and compel providers to test high-risk patients. Regarding community awareness, more than half reported hearing more about HBV recently; younger respondents were more likely to have encountered campaign materials and recall correct HBV facts. Assessment of specific campaign materials found that while upbeat images and taglines captured attention and destigmatized HBV, messages that emphasize the pervasiveness and deadly consequence of infection were more likely to drive respondents to seek education and testing. The campaign used survey results to focus efforts on more intensive provider outreach and to create messages for a new public outreach media campaign.
Keywords: Hepatitis B, Liver cancer, Asian Americans, Health promotion, Immigrants
Background
Hepatitis B and Asians in the United States
Asians are disproportionately affected by chronic hepatitis B infection and its sequelae, which include cirrohosis, liver cancer and liver failure. Screening programs in the United States estimate that 10–15% of Asians are chronically infected with hepatitis B virus (HBV), compared to 0.5% of the general population [1–5]. Most Asians in the US are either born or have parents who were born in Asia [2, 6], where prevalence of HBV infection is as high at 8–10%. If left untreated, 25% of those with chronic HBV infections will die from liver cancer [7]. Currently in the US, Asians and Pacific Islanders have the highest incidence of liver cancer among all racial/ethnic groups (7.8 per 100,000 persons, compared to 2.6–5.7 in other groups) [8].
In order to decrease HBV-related disease, the Centers for Disease Control and Prevention (CDC) recommends routine screening of high-risk populations using serologic test for hepatitis B surface antigen (HBsAg) to identify chronically infected individuals and refer them for monitoring and treatment for liver disease [9]. CDC also recommends vaccination for all infants to prevent perinatal transmission, and for all other unvaccinated individuals at high risk for infection, such as Asians.
Assessments among North American Asian populations indicate that in general, the level of knowledge about hepatitis B is low [10]. Screening levels among Asians have also been low, ranging from 9 to 55% [11–13]. In one study conducted among Asian in the San Francisco Bay Area, two-thirds of those who were chronically infected did not know their infection status [14]. Various studies have indicated that Asians with increased knowledge about hepatitis B—specifically that Asians are at increased risk for infection and that HBV infection can cause liver cancer [11, 15]—were significantly associated with testing and taking their children to be vaccinated against hepatitis B [10, 16]. Thus, assessing gaps in knowledge about HBV is key to creating an effective education message that will lead to actionable results.
The San Francisco Hep B Free Campaign
The nine-county San Francisco Bay Area has one of the highest concentrations of Asians in the United States [17]; it also has one of the highest liver cancer rates in the country [18]. Within San Francisco County itself, one-third of its 800,000 residents are Asian, 67% of whom are foreign-born [6]. Summary of data from the San Francisco Department of Public Health Viral Hepatitis Registry indicates that 86% of hepatitis B-positive cases reported to the department from 2007 to 2008 were Asian/Pacific Islander (API), 83% of whom were Chinese, and almost half were found in individuals 35–54 years of age. Eighty-seven percent were foreign-born, with Cantonese being the primary language for 56% of cases [19].
In order to address the high prevalence of potentially unidentified and untreated hepatitis B infections in San Francisco, a citywide coalition of community groups, media organizations, healthcare and governmental organizations, spearheaded by the AsianWeek Foundation, San Francisco Department of Public Health and the Asian Liver Center, launched the San Francisco Hep B Free (SFHBF) campaign in 2007 [20–22]. SFHBF is a grassroots effort that aims to “turn San Francisco into the first hepatitis B free city in the nation” by: (1) creating public and healthcare provider awareness about the importance of testing and vaccinating Asians for hepatitis B, and referring those infected to appropriate care; (2) promoting routine hepatitis B testing and vaccination within the primary care medical community, often encouraging institutional changes to facilitate routine testing; and (3) ensuring access to treatment for chronically infected individuals.
SFHBF’s many public awareness activities have been described in detail elsewhere and include in-person educational events, public service announcements through a host of media outlets, community events such as street fairs and cultural shows, and advertisements on billboards, bus shelters and other highly visible areas [20]. In Fall 2008, SFHBF launched the “B a Hero” media campaign to convey the message that anyone can be a hero by talking to friends and family about getting tested for hepatitis B (Fig. 1). The goal of using the upbeat and positive superhero image was to destigmatize the disease within the Asian community by normalizing hepatitis B and bringing the subject into open conversation so that the importance of screening, vaccination and treatment could then be addressed. “B a Hero” posters were placed along commute corridors and other high-traffic places. While the campaign message was widely disseminated to the whole San Francisco population in English, Asians were targeted due to their high risk for infection through distributing advertisements through in-language ethnic newspapers and the use of Asian models for the media images.
Fig. 1.
San Francisco Hep B Free 2008–2009 outreach campaign—B a Hero poster
In order to determine the level of awareness about hepatitis B and evaluate the impact of the “B a Hero” media campaign in the San Francisco Asian community, three evaluation projects were launched in July 2009: (1) street interviews conducted over a 2 week period in areas of San Francisco frequented by Asians, (2) telephone survey (landlines only) of a random sample of San Francisco Asian households held both in English and Cantonese, and (3) focus groups of English- and Cantonese-speaking Asians who have not been tested to hepatitis B to provide more nuanced descriptions of prevailing attitudes regarding hepatitis B. This report summarizes results from the two survey projects, and describes how SFHBF used the findings to identify knowledge gaps in our target population in order to create a more focused follow-up media messaging built upon the awareness first raised by the “B a Hero” campaign.
Methods
Questionnaire Design
Questionnaires and sampling plan were designed jointly by SFDPH and the Henne Group, a company experienced with market research, with input from SFHBF partners. To minimize selection bias, the recruitment script focused on health issues facing the Asian community in order to avoid recruiting respondents who were already interested in or familiar with hepatitis. Domains addressed by the survey include: demographics, respondents’ priorities regarding the most important health issues facing San Francisco’s Asian community, hepatitis B knowledge, hepatitis B testing behavior and reasons for test/non-test, hepatitis B awareness, recognition of SFHBF campaign materials, and sources for health information. As an incentive for participation, those who completed interviews were entered into a drawing for one of four $50 gift cards. The questionnaire was translated from English to Chinese by SFHBF partners. Bilingual English–Cantonese interviewers were hired and trained by the Henne Group using a standard protocol to conduct both the street intercept and telephone surveys.
Street Intercept Surveys
Ninety hours of street intercept interviews were conducted over a 2 week period by five Cantonese–English bilingual staff, resulting in 153 successful interviews. With input from campaign staff familiar with San Francisco’s Asian community, we selected 14 interview sites frequented by Asians aged 35 years or older; we focused on this age group because a substantially higher percentage are foreign-born individuals (thus, a higher proportion are at high risk of chronic hepatitis B infection) compared to younger age groups [23]. Three of the 14 sites were at bus stops, three outside specific shops frequented by Asians, three outside community gathering places, and five at specific street intersections or along specific stretches of streets frequented by Asians. A convenience sample of potential respondents were recruited as allowed by interviewer availability. Interviewers reported a response rate of one for every six persons approached (16.7%). Respondents who did not self-identify as Asian, who were not San Francisco residents or who did not speak either English or Cantonese were excluded from the interview.
Telephone Surveys
A sample of 5,215 San Francisco landline telephone numbers associated with Asian surnames located in census tracts with high proportions of households identified as Asian was purchased through a sampling vendor. An English version of the street intercept questionnaire was programmed into a computer assisted telephone interviewing (CATI) software, excluding questions evaluating recognition of SFHBF materials because these questions required visual prompting and were not asked in the telephone surveys. Telephone interviews were conducted in the same 2 weeks as the street intercept interviews, during various times of the day and week. Respondents who did not self-identify as Asian or who did not speak either English or Cantonese were excluded from the interview. Out of 2,197 individuals called during the 2 week period, 184 persons did not meet the inclusion criteria, 380 refused or terminated the interview before completion, 1,480 were unreachable (i.e., answering machine only, or wrong or disconnected number). The interview was completed by 153 individuals, giving a response rate of 15.3%. A sample of responses were double-entered into the CATI software to verify accuracy in data entry.
Statistical Analysis
Univariate summaries were performed on all variables from the survey. Pearson’s χ2 test or Fisher’s exact test for categorical data and the Student t test for continuous data were used to detect statistically significant differences in survey responses on the following variables: age group (<35 years old, 35–64 years old, 65+ years old), years lived in the United States (US-born, less than 10 years in the US, 10+ years in the US), and mode of interview (telephone vs. street intercept). All hypothesis tests were two-tailed and p values of 0.05 or less were considered significant. Univariate and multivariate logistic regression models were used to estimate risk factors for having been tested for HBV, having asked for a HBV test, and recognition of the B a Hero logo, and perception of greater community awareness about HBV in the last year compared to years before. Covariates include sex, ethnicity, age, years spent in the US and household income. Lastly, because we had many more Chinese respondents than those from other Asian groups, sub-analyses were performed on select variables to determine whether replies from Chinese respondents were significantly different from those who were Asian but not Chinese. All analyses were performed using SAS 9.1.3 for Windows (Cary, NC).
Results
Descriptive Analysis
Demographic characteristics of interview the 306 survey respondents are presented in Table 1. The majority of the interview population were Chinese (86.3%), female (63.4%) and foreign-born (88.2%, 74% of whom were born in China). Of immigrant respondents, a majority have been in the US for more than 10 years (67.0%). Seventy-one percent of respondents chose to answer the survey in Cantonese, and 80.7% spoke Cantonese at home. When comparing the interview population by survey mode, street interview respondents were more likely to be younger (52.3% over 45 years old vs. 65.4% in telephone interviews, p = 0.005), more recent immigrants (40.7% vs. 25.6%, p = 0.001), were monolingual in or preferred speaking Cantonese (81.1% vs. 60.8% for interview language, p < 0.0001), and less likely to speak languages other than Cantonese at home (89.5% vs. 71.9%, p < 0.0001).
Table 1.
Demographics of interview population
| All (N = 306) | Street intercept interviews (N = 153) | Telephone interviews (N = 153) | p value | |
|---|---|---|---|---|
| Asian ethnicity a | ||||
| Chinese | 264 (86.3%) | 137 (89.5%) | 127 (83.0%) | 0.10 |
| Filipino | 14 (4.6%) | 3 (2.0%) | 11 (2.6%) | 0.18 |
| Japanese | 11 (3.6%) | 4 (2.6%) | 7 (4.6%) | 0.35 |
| Vietnamese | 10 (3.3%) | 5 (3.3%) | 5 (3.3%) | 1.0 |
| Taiwanese | 3 (2.0%) | 3 (2.0%) | 0 | 0.08 |
| Korean | 2 (0.7%) | 1 (0.7%) | 1 (0.7%) | 1.0 |
| Other | 5 (2.0%) | 1 (0.7%) | 4 (2.8%) | 0.17 |
| Age | ||||
| 18–24 | 30 (9.8%) | 22 (14.4%) | 8 (5.2%) | |
| 25–34 | 37 (12.1%) | 23 (15.0%) | 14 (9.2%) | |
| 35–44 | 59 (19.3%) | 28 (18.3%) | 31 (20.3%) | 0.005 |
| 45–54 | 53 (17.3%) | 24 (15.7%) | 29 (19.0%) | |
| 55–64 | 62 (20.3%) | 34 (22.2%) | 28 (18.3%) | |
| 65+ | 65 (21.2%) | 22 (14.4%) | 43 (28.1%) | |
| Sex | ||||
| Female | 194 (63.4%) | 94 (61.4%) | 100 (65.4%) | 0.47 |
| Country of birth | ||||
| United States | 36 (11.8%) | 20 (13.1%) | 16 (10.5%) | |
| China | 199 (65.0%) | 101 (66.0%) | 98 (64.1%) | 0.39 |
| Hong Kong | 34 (11.1%) | 19 (12.4%) | 15 (9.8%) | |
| Philippines | 13 (4.3%) | 3 (2.0%) | 10 (6.5%) | |
| Other | 24 (7.8%) | 10 (6.5%) | 14 (9.2%) | |
| Years in US | ||||
| 0–5 years | 50 (18.5%) | 28 (21.1%) | 22 (16.1%) | |
| 6–10 years | 39 (14.4%) | 26 (19.6%) | 13 (9.5%) | 0.001 |
| 11–20 years | 84 (31.1%) | 46 (34.6%) | 38 (27.7%) | |
| 21+ years | 97 (35.9%) | 33 (24.8%) | 64 (26.7%) | |
| Annual household income | ||||
| < $30,000 | 148 (48.4%) | 70 (45.8%) | 78 (51.0%) | |
| $30,001–$60,000 | 79 (25.8%) | 50 (32.7%) | 29 (19.0%) | |
| $60,001–$80,000 | 25 (8.2%) | 12 (7.8%) | 13 (8.5%) | 0.09 |
| $80,001–$120,000 | 13 (4.3%) | 6 (3.9%) | 7 (4.6%) | |
| > $120,000 | 11 (3.6%) | 3 (2.0%) | 8 (5.2%) | |
| Prefer not to say | 30 (9.8%) | 12 (7.8%) | 18 (11.8%) | |
| Interview language | ||||
| Cantonese | 217 (70.9%) | 124 (81.1%) | 93 (60.8%) | <0.0001 |
| English | 89 (29.1%) | 29 (19.0%) | 60 (39.2%) | |
| Languages spoken at home a | ||||
| Cantonese | 247 (80.7%) | 137 (89.5%) | 110 (71.9%) | <0.0001 |
| English | 88 (28.8%) | 36 (23.5%) | 52 (34.0%) | 0.04 |
| Mandarin | 18 (5.9%) | 6 (3.9%) | 12 (7.8%) | 0.14 |
| Tagalog | 9 (2.9%) | 1 (0.7%) | 8 (5.2%) | 0.02 |
| Toisan | 6 (2.0%) | 3 (2.0%) | 3 (2.0%) | 1.0 |
| Vietnamese | 4 (1.3%) | 1 (0.7%) | 3 (2.0%) | 0.31 |
| Korean | 1 (0.3%) | 1 (0.7%) | 0 | 0.32 |
| Other | 13 (4.3%) | 2 (1.3%) | 11 (7.2%) | 0.01 |
aDoes not add up to 100% because respondents were allowed to choose more than one answer
The interview began with an open-ended question asking respondents to identify the most important health issues facing San Francisco’s Asian community (Table 2). Almost one-third of all respondents stated hepatitis as a key issue, only second to diabetes in the overall ranking of health issues. Concerns about health insurance coverage, heart disease and cancer followed. When stratified by number of years lived in the US, the list of priorities shift slightly. Hepatitis ranks at the top of the list for those who have been here for 10 years or more, and was ranked second and third by those who have been here for fewer than 10 years and those born in the US, respectively. Significantly, hepatitis ranks in the top 3 health concerns when interviewees were not prompted with it as an answer choice.
Table 2.
Respondents’ priorities on the most important health issues facing San Francisco’s Asian community
| Health issuea | All | US-born | In US 10+ years | In US <10 years | ||||
|---|---|---|---|---|---|---|---|---|
| Rank | % | Rank | % | Rank | % | Rank | % | |
| Diabetes | 1 | 29.4 | 4 | 19.4 | 2 | 31.5 | 1 | 29.2 |
| Hepatitis | 2 | 29.1 | 3 | 22.2 | 1 | 32.0 | 2 | 25.8 |
| Health insurance too expensive/no coverage | 3 | 23.2 | 2 | 25.0 | 4 | 21.6 | 2 | 25.8 |
| Heart disease | 4 | 22.5 | 5 | 16.7 | 3 | 22.7 | 2 | 25.8 |
| Cancer | 5 | 20.9 | 1 | 27.8 | 5 | 18.8 | 3 | 22.4 |
| Smoking | 6 | 15.0 | 1 | 27.8 | 6 | 11.1 | 4 | 18.0 |
| Drug/alcohol abuse | 7 | 6.9 | 6 | 8.3 | 9 | 2.8 | 5 | 14.6 |
| Obesity | 8 | 5.6 | 7 | 5.6 | 7 | 4.4 | 6 | 7.9 |
| Language barrier | 9 | 3.6 | 8 | 2.8 | 9 | 2.8 | 7 | 5.6 |
| HIV/AIDS | 10 | 2.3 | 8 | 3.3 | 9 | 1.2 | ||
| Influenza/SARS | 10 | 2.3 | 8 | 2.8 | 9 | 2.8 | 8 | 2.3 |
| Nutrition | 11 | 2.0 | 8 | 2.8 | 11 | 1.5 | 8 | 2.3 |
| Access to doctors | 12 | 1.3 | 11 | 1.5 | 9 | 1.2 | ||
| Arthritis/body aches | 12 | 1.3 | 12 | 1.1 | 9 | 1.2 | ||
| High Cholesterol | 12 | 1.3 | 10 | 2.2 | ||||
| Depression/mental health | 12 | 1.3 | 7 | 5.6 | 8 | 2.3 | ||
| “Asians get sicker” | 13 | 0.7 | 8 | 2.8 | 13 | 0.6 | ||
| General awareness of illnesses | 13 | 0.7 | 8 | 2.8 | ||||
| Lung cancer/disease | 13 | 0.7 | 13 | 0.6 | 9 | 1.2 | ||
| Tuberculosis | 13 | 0.7 | 13 | 0.6 | 9 | 1.2 | ||
| Not sure | – | 19.6 | – | 13.9 | – | 21.0 | – | 19.1 |
Bold values indicate rankings for the hepatitis
aRespondents allowed to give multiple reasons; this was an open-ended question with no prompting from the interviewer regarding answer choices
Table 3 describes respondents’ current levels of hepatitis B knowledge. General awareness of a medical condition called hepatitis and specifically hepatitis B is high—92 and 85%, respectively. When stratified by age group, awareness of either conditions were significantly higher among younger respondents: for “hepatitis”, awareness was 94–95% those under 65 year old, and 83.1% for those 65 years old and older (p = 0.01); for “hepatitis B”, awareness was 88–90% for those under 65 years old and 70.1% for those 65 years old or older (p = 0.007). However, when probed in an open-ended manner about how hepatitis B transmission may be prevented, the most common answer was “not sure” (31.7%), with the highest percentage of “not sure” answers coming from older respondents (23–30% from those under 65, and 45% in those 65 and over, p = 0.03). Three of the top five methods given involved good hygiene and keeping clear of contaminated food (“Make sure food or water are not contaminated”, “Don’t share eating utensils”, “Wash hands/general cleanliness/good hygiene”), which are generally prevention methods for hepatitis A infection and are ineffective for hepatitis B; the remaining two involved having protected sex and not sharing intimate items, both of which are effective against hepatitis B. US-born respondents were more likely to cite having protected sex as a prevention method, and those under 35 years old were the only ones to cite “avoiding blood and bodily fluid contact” and “get tested” as prevention methods.
Table 3.
Hepatitis B knowledge among respondents
| Knowledge questions | N | % |
|---|---|---|
| Have you ever heard of a medical condition called hepatitis? | ||
| Yes | 282 | 92.2 |
| No | 22 | 7.2 |
| Not sure | 2 | 0.7 |
| Have you ever heard of a hepatitis B? | ||
| Yes | 261 | 85.3 |
| No | 33 | 10.8 |
| Not sure | 12 | 3.9 |
| To the best of your knowledge, how can someone prevent themselves from getting hepatitis B, or giving it to others?a | ||
| Not sure | 97 | 31.7 |
| Make sure food or water are not contaminated | 56 | 18.3 |
| Don’t share toothbrushes, razors or other intimate items | 52 | 17.0 |
| Don’t share eating utensils | 51 | 16.7 |
| Wash hands/general cleanliness/good hygiene | 33 | 10.8 |
| Have protected sex | 30 | 9.8 |
| Don’t touch, kiss or hug someone with hepatitis | 26 | 8.5 |
| Ask close contacts to get vaccinated | 22 | 7.2 |
| Don’t do drugs | 16 | 5.2 |
| Don’t drink alcohol | 12 | 3.9 |
| Avoid blood or bodily fluid contact | 10 | 3.3 |
| Get tested | 6 | 2.0 |
| Keep a healthy diet | 6 | 2.0 |
| Don’t smoke | 5 | 1.6 |
| Don’t eat in restaurants | 5 | 1.6 |
| Exercise, get rest | 5 | 1.6 |
| Get regular check-up | 3 | 1.0 |
| Drink Chinese herbs | 2 | 0.7 |
| Avoid riding the bus/public places | 2 | 0.7 |
aRespondents allowed to give multiple reasons; this was an open-ended question with no prompting from the interviewer regarding answer choices
Sixty percent of our respondents reported having been tested for hepatitis B, with 1 in 10 being unsure whether they had been tested in the past (Table 4). Among those who had been tested, half reported having asked their provider for a test. A third were tested in the past year, a third between 1 and 3 years ago, and the rest 4 or more years ago. When asked in an open-ended manner why they decided to get tested, the most commonly cited reason was that their doctor recommended testing (33.3%), followed by testing being part of a physical (15.3%) and a mandate from work or school (13.1%). Among those under 35 years old, 11% cited “request from family or friend” as a reason for testing, compared to only 0–2% in respondents 35 or over (p = 0.01).
Table 4.
Testing behavior among respondents
| Testing behavior and attitudes | N | % |
|---|---|---|
| Have you ever been tested for hepatitis B? | ||
| Yes | 183 | 59.8 |
| No | 87 | 28.4 |
| Not sure | 36 | 11.8 |
| Of those who report having been tested for hepatitis B | ||
| What made you decide to get tested for hepatitis B?a | ||
| My doctor told me I should | 61 | 33.3 |
| Part of regular body check | 28 | 15.3 |
| Work/school mandate | 24 | 13.1 |
| Wanted to know if I’m infected | 15 | 8.2 |
| I asked my doctor | 14 | 7.7 |
| Have family/friend with hepatitis B | 9 | 4.9 |
| Learned about it in newspaper/TV/ad | 8 | 4.4 |
| Request from family/friend | 7 | 3.8 |
| It was free | 7 | 3.8 |
| For travel | 6 | 3.3 |
| Pregnant | 3 | 1.8 |
| Not sure | 3 | 1.6 |
| Other reason | 11 | 0.6 |
| When you were tested, did you ask your doctor specifically for a hepatitis B test? | ||
| Yes | 89 | 48.6 |
| No | 75 | 41.0 |
| Not sure | 19 | 10.4 |
| How long ago were you tested? | ||
| In the past 6 months [Feb–Aug 2009] | 32 | 17.5 |
| 7 months to 1 year ago [Aug 2008–Jan 2009] | 32 | 17.5 |
| Between 1–3 years ago [August 2007–July 2008] | 61 | 33.3 |
| 4–10 years ago [August 1997–July 2007] | 34 | 18.6 |
| More than 10 years ago [Before August 1997] | 19 | 10.4 |
| Don’t remember | 5 | 2.7 |
| Where did you get tested? | ||
| At a clinic | 101 | 55.2 |
| My doctor’s office | 67 | 36.6 |
| Screening event | 5 | 2.7 |
| Street fair | 5 | 2.7 |
| Don’t remember | 5 | 2.7 |
| Of those who report not having been tested for hepatitis B | ||
| If you have not been tested, why not?a | ||
| Doctor says I don’t need to be tested | 29 | 23.6 |
| Don’t know much about it | 22 | 17.9 |
| I’m immune | 17 | 13.8 |
| Not sure | 15 | 12.2 |
| Doctor did not say that I need to be tested | 14 | 11.3 |
| I don’t have a doctor | 8 | 6.5 |
| No insurance or insurance doesn’t cover test | 7 | 5.7 |
| It’s too expensive | 6 | 4.9 |
| No time/too much of a hassle | 5 | 4.1 |
| I don’t know anyone who has hepatitis | 3 | 2.4 |
| Don’t do regular blood tests/check-ups | 3 | 2.4 |
| Don’t think I have hepatitis B/I’m healthy | 3 | 2.4 |
| Don’t want to find out | 2 | 1.6 |
| Don’t like blood draws | 1 | 0.8 |
| Need to look at medical records | 1 | 0.8 |
| Planning to go | 1 | 0.8 |
aRespondents allowed to give multiple reasons; this was an open-ended question with no prompting from the interviewer regarding answer choices
As for reasons for not having been tested, respondents commonly mentioned a lack of recommendation from their healthcare providers: for 23.6%, the respondents’ doctors told them that they did not need to be tested (when stratified by age, 39% among those 65 and over, compared to 13–18% among those under 65, p = 0.02), and for 11.3%, respondents did not explicitly receive a recommendation to test from their providers. Eighteen percent cited a lack of knowledge about the test. Cost was a big concern for younger respondents, with 17% of those under 35 giving “it’s too expensive” as a reason for not getting tested (vs. 1–3% in those 35 and over, p = 0.008).
Respondents were then asked about their impression of how often and what they had heard about hepatitis B in their community lately compared to a year ago (Table 5). Almost half of the respondents reported hearing more about hepatitis B in their community recently, with those between 35 and 64 and those under 35 years old having heard more in the past year than those over 65 years old (51% and 43% vs. 34%, p = 0.003). When probed in an open-ended manner, most of the information that respondents have heard about hepatitis in the community lately is correct, with the fact that Asians are at higher risk for infection than those in other ethnic groups being the most common fact they have heard (11.1%). Other correct facts include: “It can give you cancer”, “I should get vaccinated”, “There is a vaccine for it”, and “There are free testing clinics” (Table 5).
Table 5.
Hepatitis B and San Francisco Hep B Free awareness among respondents
| Awareness questions | N | % |
|---|---|---|
| Do you feel that you have been hearing more or less about hepatitis B in your community lately, compared to a year ago? | ||
| More | 140 | 45.8 |
| Less | 48 | 15.7 |
| Not sure | 78 | 25.5 |
| Have not heard or seen anything about hepatitis B | 40 | 13.1 |
| What have you seen or heard about hepatitis B in your community?a | ||
| People in my ethnic group are at greater risk of infection than people in other ethnic groups | 42 | 15.8 |
| It’s a problem | 34 | 11.1 |
| People like me are at risk for infection | 30 | 9.8 |
| It can give you cancer | 24 | 9.0 |
| I should get vaccinated | 21 | 7.9 |
| There is a vaccine for it | 19 | 7.1 |
| There are free testing clinics | 10 | 3.8 |
| I should ask my doctor to test me for hepatitis B | 10 | 3.8 |
| People in my ethnic group are at greater risk of dying from liver cancer compared to people in other ethnic groups | 5 | 1.9 |
| Be aware of it | 3 | 1.1 |
| All Asians should get tested | 3 | 1.1 |
| Can cause liver damage | 1 | 0.3 |
| Easy to get infection | 1 | 0.3 |
| Doesn’t get much attention in the US | 1 | 0.3 |
| Can make people tired and affects the body | 1 | 0.3 |
| Prevention strategies | 1 | 0.3 |
| Get checked if you feel run down because it can take time to show symptoms | 1 | 0.3 |
| Not really serious | 1 | 0.3 |
| School offers testing | 1 | 0.3 |
| Infection stays for a long time | 1 | 0.3 |
| Yellowish color is a symptom | 1 | 0.3 |
| Weakens the blood | 1 | 0.3 |
| Where have you seen or heard information about hepatitis B?a | ||
| Asian newspaper article | 64 | 24.1 |
| TV commercial | 60 | 22.6 |
| TV news or talk show | 39 | 14.7 |
| Pamphlet, flyer or poster at clinic or doctor’s office | 39 | 14.7 |
| Not sure | 36 | 13.5 |
| Street poster | 31 | 11.7 |
| Spoke to my doctor | 22 | 8.3 |
| Radio commercial | 22 | 8.3 |
| Spoke to a friend or family member | 17 | 6.4 |
| Radio talk show | 17 | 6.4 |
| Work or school | 12 | 4.5 |
| Bus or bus shelter | 11 | 4.2 |
| Community center | 5 | 2.2 |
| Website | 4 | 1.5 |
| Street fair | 2 | 0.8 |
| Flyer mailed to home | 2 | 0.8 |
| Flyer on street | 2 | 0.8 |
| Books | 1 | 0.4 |
| Email forward from friend | 1 | 0.4 |
| Friends died from it | 1 | 0.4 |
| Newsletters | 1 | 0.4 |
| Health department | 1 | 0.4 |
| Have you seen any posters of flyers with information about hepatitis B? | ||
| Yes | 132 | 43.3 |
| No | 142 | 46.6 |
| Not Sure | 31 | 10.2 |
| Have you seen [the B a Hero poster] around town?b | ||
| Yes | 63 | 41.2 |
| No | 81 | 52.9 |
| Not Sure | 9 | 5.9 |
| What do you think the main message [of the B a Hero poster] is?b | ||
| There is free testing | 10 | |
| Confusion about hero image | 10 | |
| See doctor/get tested/go get a check-up | 8 | |
| Like Superman, be strong/fight against HBV/help others/stop spread | 5 | |
| Confused poster for movie advertisement | 4 | |
| Many Asians have hepatitis B | 3 | |
| Free blood test available for hepatitis B | 2 | |
| Don’t be afraid of hepatitis B | 1 | |
| Don’t understand the letter B | 1 | |
| Be aware of hepatitis B | 1 | |
| Infection can lead to cancer | 1 | |
| How likely do you think you would do any of the following as a result of seeing this “B a Hero” poster?b | ||
| a) Try to learn more about hepatitis B | ||
| Very/somewhat likely | 55 | 29.4 |
| Not too likely/Not likely at all | 91 | 59.4 |
| Not sure | 8 | 5.2 |
| b) Get tested for hepatitis B | ||
| Very/somewhat likely | 43 | 35.3 |
| Not too likely/Not likely at all | 90 | 58.8 |
| Not sure | 8 | 5.2 |
| c) Recommend hepatitis B testing to a friend or family | ||
| Very/somewhat likely | 39 | 25.5 |
| Not too likely/Not likely at all | 94 | 61.4 |
| Not sure | 12 | 7.8 |
| d) Get vaccinated against hepatitis B | ||
| Very/somewhat likely | 46 | 30.1 |
| Not too likely/Not likely at all | 92 | 60.2 |
| Not sure | 9 | 5.9 |
| e) Go see a doctor | ||
| Very/somewhat likely | 45 | 29.5 |
| Not too likely/Not likely at all | 99 | 63.4 |
| Not sure | 2 | 1.3 |
| f) Get medical follow-up if you test positive for hepatitis B | ||
| Very/somewhat likely | 33 | 21.6 |
| Not too likely/Not likely at all | 102 | 66.7 |
| Not sure | 11 | 7.2 |
aRespondents allowed to give multiple reasons to this open-ended question with no prompting from the interviewer regarding answer choices
bThese questions were only asked of street intercept respondents because they required visual prompting of the “Be A Hero” campaign poster
When examining where respondents had seen or heard about hepatitis B, results differed significantly based on age group: older respondents were more likely to be exposed to Asian newspaper articles (35% vs. 10–25%, p = 0.01) and TV talk shows (17–19% vs. 5%, p = 0.06), middle-aged respondents through a pamphlet or flyer in the clinic (12% vs. 2–5%, p = 0.05) and those under 35 years old through a TV commercial (24–33% vs. 6%, p = 0.001) or bus shelter advertisement (14% vs. 1–2%, p = 0.002). Forty-three percent of respondents reported seeing a flyer about hepatitis B in their community recently, with a clear trend in younger respondents being more likely to have seen a flyer than older respondents (58, 46 and 22% in <35, 35–64 and 65+ year olds, respectively, p = 0.0007). Most likely these flyers were seen at a hospital, clinic or doctor’s office (30%) and on the street (14%).
To evaluate the penetration of the 2009 “B a Hero” media campaign in this group, we asked the street intercept survey respondents about recognition of and reaction to the “B a Hero” poster (Fig. 1). Forty-one percent reported seeing the poster. When probed in a open-ended manner about what the message of the poster may be, many said “It’s about hepatitis B”, but nothing else. Ten respondents thought the “Free” of the slogan represented free testing being available, and ten expressed confusion about the hero image (e.g. “Does that mean I’m a hero if I get hepatitis B?”, “I don’t understand Superman. Why not an image of a liver?”, “Is it a movie?”, “Why use Superman? But it makes me curious to look at it.”, “[The image] should be more serious.”). Some respondents were confused about the involvement of the letter “B”. Some did correctly interpret the superhero image to mean being one to friends and family by learning more or getting tested/vaccinated for hepatitis B. While the image piqued curiosity in general, some thought the advertisement was from a company rather than a trusted source such as the health department or community hospital. When asked whether the “B a Hero” poster would prompt respondents to get tested, vaccinated, see a doctor, learn more about hepatitis B, or to recommend testing to friends or family, more than 60% indicated that they would “not likely” do so.
Lastly, to guide our planning for more effective media campaign outlets in the future, we asked respondents where they usually obtain health information for a cold, a partner’s pregnancy and a family member’s heart attack (i.e. health conditions of varying severity), aside from consulting a doctor. Overall, “word of mouth” ranked within the top three sources for all three conditions (27–34%), as followed by website/blogs for pregnancy and heart attack (24–29%). Acupuncturist and pharmacist ranked highly for a cold, as did hospital and books for pregnancy. TV, radio, newspaper/magazine, email forwards, mailing lists and social media tools did not rank within the top five health information sources for the health conditions asked about in the survey.
Because our sample consisted mainly of Cantonese-speaking Chinese respondents, we performed additional analyses to identify differences in responses between these and the rest of the respondents. Most results were similar between the groups, although Cantonese speakers were more likely to identify hepatitis as a problem in the Asian community (31% vs. 17%), more likely to have seen a flyer at a doctor’s office regarding hepatitis B (19% vs. 7%), less likely to have heard that they should be vaccinated against hepatitis B (5% vs. 21%), and less likely to hear about hepatitis from ads (8% vs. 25%) or news (3% vs. 17%) on television.
Logistic Regressions
We also performed multivariate logistic regression to examine factors contributing to key outcomes of interest. Factors associated with having been tested for hepatitis B included being 65 years or older (vs. <35 years, OR: 0.36, 95% CI: 0.16–0.81), having heard more about hepatitis B in the community (vs. not having heard or not being sure, OR: 2.17; 95% CI: 1.15–4.09), and having been interviewed in English (vs. Cantonese, OR: 2.86, 95% CI: 1.27–6.46). Factors associated with having proactively asked for a hepatitis B were having been in the US for 10 years or more (OR: 5.37, 95% CI: 1.11–25.9). Lastly, those interviewed in English (OR: 2.84, 95% CI: 1.20–6.70) and those who reported having heard about hepatitis B more in their community recently (OR: 2.81, 95% CI: 1.03–7.66) were more likely recognize the “B a Hero” posters.
Discussion
Since its launch in April 2007, the San Francisco Hep B Free Campaign has focused its outreach activities to encourage the San Francisco Asian population to get tested for hepatitis B, know their infection statuses and seek treatment if they are infected. Our surveys, conducted 2 years after SFHBF began and 1 year after its first citywide media campaign, show that awareness about hepatitis B is high and that the disease is already recognized as an important health issue within the Asian community. However, our results also show that our target population still has knowledge gaps, and has a high degree of assumption that medical providers are already screening them for their infection status as a part of their routine physicals because they belong to a group at high risk for hepatitis B infection.
We used the misconceptions identified in our surveys to revise and improve the outreach messages to our target community. Similar to studies conducted in other North American cities, many of our respondents incorrectly cited clean food and water and not sharing utensils as effective prevention methods [10, 15, 24–28], with less than 10%, mostly English-speakers, correctly citing protected sex, avoiding blood contact or vaccination. Upon further probing, some respondents admitted to not knowing much about hepatitis at all beyond recognizing the term. These misconceptions may stem from a possible confusion between hepatitis A and B. Hepatitis cases interviewed by SFDPH staff for surveillance purposes have reported patients thinking that the terms A, B and C denote a progression of one disease from one phase to another, as well as inconsistency in how the local Chinese media refers to hepatitis B, with some sources using the English letter “B” and some the Chinese character equivalent for “B”.
Questions evaluating the “B a Hero” posters and messaging also indicated confusion about the use of the letter “B” and upbeat imagery for a cancer-causing disease. We used these findings to inform a new media campaign launched in Summer 2010 (Table 6), building on the awareness created by the “B a Hero” materials by highlighting the relationship between hepatitis B and liver cancer, increased risk for infection among Asians and more specific instruction on action steps to take to get tested and treated for hepatitis B infection (Fig. 2). The new “Which one deserves to die?” media materials, created by DAE Advertising, are available in English, Chinese, Korean, Vietnamese and Tagalog and have been distributed on streets, transit stations and buses throughout San Francisco (http://hepbads2010.blogspot.com), and as advertisement in a variety of ethnic newspapers. Anecdotally, partners have reported positive responses to this new material: one screening partner saw a doubling of clients within months of the new media campaign; this and other screening clinics report that clients are citing the ad as a reason for coming to the clinic; another community partner also reported that the ads have provoked many conversations about hepatitis B within the Asian community. The “Which one deserves to die?” campaign also gained national recognition by being featured on PBS NewsHour and the New York Times, and was a winner in the 2010 CLIO Healthcare Awards, which has encouraged other cities to launch similar hepatitis B awareness campaigns.
Table 6.
Application of survey findings to San Francisco Hep B Free outreach strategies
| Findings | Application |
|---|---|
| High level of recognition of the term “hepatitis B”, but lack of knowledge about correct prevention methods due to confusion with hepatitis A and belief that general good diet hygiene can prevent hepatitis B transmission. Also, current level of knowledge about hepatitis B did not compel most to seek testing | Simpler messaging to convey the basic concepts about hepatitis B disease and transmission. Aside from emphasizing that hepatitis B cannot be prevented solely through a healthy diet and exercise and that most Asians are infected via vertical transmission, we also found that: (1) the “1 in 10 are infected” message effectively conveyed how common hepatitis B infection is within the Asian community, and (2) the “which one deserves to die?” tagline effectively conveyed the potential deadly consequence of infection |
| Most respondents held a high level of trust that their primary care providers would know what diseases they are at higher risk for, to test them for these diseases as part of their routine physical and to inform them of the results |
More intensive outreach to primary care providers urging them to test and vaccinate Asians due to their high level of trust in the medical community, and to improve communication with patients regarding hepatitis test results Promoting the Hep B Free Clinician’s Honor Roll to recognize clinicians who have signed a pledge to test patients at risk for chronic hepatitis B infections in accordance with CDC guidelines. Our goal is to have 90% of primary care clinicians in San Francisco complete this pledge Producing a handout (“Ask sheet”) that people can take to providers to request testing. Its purpose is to help patients initiate conversation with their providers about testing, and to serve as an education piece and reference sheet for providers |
| While memorable, respondents were confused about the upbeat image associated with the B a Hero campaign, as well as how one can be a hero in the context of hepatitis B | Use of more appropriate imagery to convey the seriousness of hepatitis B infection, (relating it to its serious consequence of liver cancer), as well as increased risk for infection among Asian Americans. The 2010 “Which One Deserves To Die?” campaign incorporates more serious imagery about cancer as a possible consequence of hepatitis B infection in its messaging |
| Sources of health information were homogeneous among Cantonese speakers, mostly through health columns in Chinese newspapers and Chinese news talk shows, as well as pamphlets from trusted institutions. English-speakers used a wider array of sources | Two different sets of messaging and outreach methods are needed, not just separated by language needs but also considering age and level of acculturation. While Cantonese speakers may be reached largely through in-language media, English-speakers may need to be reached through a larger variety of portals, such as providing information on internet. This finding validated outreach strategies already being used by SF Hep B Free |
| Inconsistent translation of hepatitis B in Chinese media | Use of consistent terminology in all campaign outreach materials |
Fig. 2.

San Francisco Hep B Free 2010 outreach campaign posters
While the SFHBF campaign spent the first 2 years using multiple means to mobilize the public to seek testing, our findings indicate that provider recommendation was the most influential factor for those who have sought testing. Among the of respondents who were tested for hepatitis B in the last 3 years, almost half stated that they were tested because their healthcare provider recommended it or that it was assumed to be a part of the blood panel performed during their routine physical. Similarly, the primary reason for non-test was that the respondents’ healthcare provider said that they did not need to be tested. Other studies have also found provider recommendation to be the strongest influential factors for API to be tested [11, 29–31]. Respondents in general showed a high level of trust in the medical community, some explaining that they expected their providers to give them important health information, be able to correctly assess what health issues they may be at highest risk for developing, and test them for these conditions.
Surveys of clinicians in the San Francisco Bay Area indicate that while almost all knew that Asians were disproportionately affected by hepatitis B infection and liver cancer, levels of hepatitis B screening and vaccination for their Asian patients remain suboptimal [32, 33]. A 1 year follow-up study of a pilot hepatitis B screening effort of Chinese Americans in the area suggest that poor clinical follow-up for screened patients may be due to ineffective communication between patients and their providers, and the lack of awareness on the part of primary care providers about appropriate follow-up actions [34]. Together with our findings, these facts suggest that efforts to increase hepatitis B screening among Asians must both mobilize the public to request testing, as well as educate providers and institute processes that would remind them to test high-risk patients. In this next phase of the campaign, SFHBF is capitalizing on our target population’s high level of trust in the medical providers by focusing on outreach to the clinician community (Table 6). In addition to continuation of educational events and distributing a screening algorithm developed earlier in the campaign, SFHBF is promoting a clinician’s honor roll to encourage clinicians to pledge to test patients at risk for hepatitis B infections, and has created a “Patient Ask Sheet” that may be distributed at public venues to help individuals proactively ask their providers for hepatitis B testing and/or vaccination (Fig. 3).
Fig. 3.
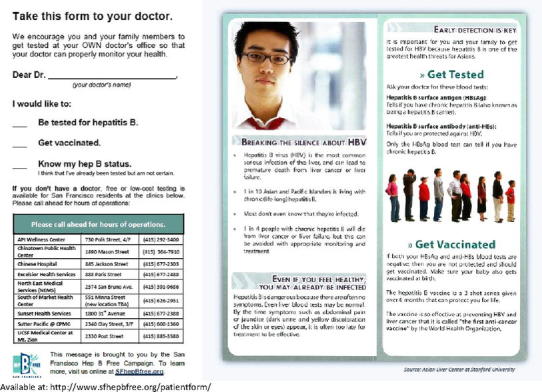
Patient “Ask Sheet”. Available at: http://www.sfhepbfree.org/patientform/
While our survey provided useful information for refining campaign strategies, it does have the following limitations. Because the campaign did not have the resources to conduct a representative-sample survey of the San Francisco Asian population, our results can only be considered an evaluation of our specific outreach program and cannot be extrapolated to all Asians living in San Francisco. Also, even though a wide array of monolingual Asians reside in San Francisco, we only had the resources to survey one monolingual group (Cantonese speakers, the largest proportion of monolingual Asians in San Francisco [6]). By recruiting for our street intercept interviews at locations frequented by Chinese residents and interviewing non-Cantonese-speaking Asians in English only, we overrepresented monolingual Cantonese speakers and may have excluded valuable feedback from non-Chinese Asians that also have high prevalence of HBV infection, such as Vietnamese, Cambodian and Korean residents. Also, while we did find a higher percentage of respondents who were familiar with hepatitis B (90%) compared to studies in similar populations in other parts of North America, (ranging from 56% to 86% [15, 26, 27, 30, 35–38]), and that almost half of our respondents reported seeing an increase in hepatitis B awareness within their community in the past year, we are unable to directly attribute these apparent increases to SFHBF due to the lack of baseline data from the period before 2007, with the most recent local data having been produced in 2000 [10].
Our evaluation project does have some strengths. It is the first recent assessment of hepatitis B knowledge, attitudes and testing behavior among Asian residents of San Francisco. Our use of many open-ended questions and lack of initial prompting about hepatitis B as the survey’s subject matter should have elicited objective feedback about how a sample of Asians in San Francisco prioritize hepatitis B in relation to other health issues in their community. We were able to use results from this project to determine where to focus upcoming campaign activities, resulting in a new and nationally-recognized media campaign with messaging that emphasizes the serious consequences of infection and a more focused strategy for clinician outreach. It is our hope that, by simultaneously driving both the Asian community to seek testing from their medical providers and the clinician community to be more vigilant in initiating testing and vaccination, SFHBF and our partner organizations can build a comprehensive and sustainable strategy to significantly decrease the burden of disease caused by hepatitis B in San Francisco.
Acknowledgments
Research support was provided by in-kind donations from San Francisco Department of Public Health and a grant from Gilead Sciences. We would like to acknowledge the Asian Liver Center for its continued leadership and support of the SF Hep B Free Campaign and evaluation efforts, the SF Hep B Free Public Awareness Evaluation Subgroup members Julia Lam, Peter Swing, Kevin Shi and Ellen Lee and the SFDPH Chronic Hepatitis Surveillance Team members Alex Leung, Karen Luk and Martina Li for feedback regarding study design, questionnaire review and translation help; Ellen T. Chang, Grace Yoo for reviewing the manuscript; and Patrick Thompson and Kevin Connors of the Henne Group for providing details on the sampling scheme.
References
- 1.Guane, R., Sui, P., Lam, K., Kim, K., Warren, V., & Liu, H. (2004). Prevalence of HBV and risk of HBV acquisition in hepatitis B screening programs in large metropolitan cities in the US. Hepatology716A.
- 2.Kim WR. Epidemiology of hepatitis B in the United States. Hepatology. 2009;49:S28–S34. doi: 10.1002/hep.22975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.CDC Screening in chronic hepatitis B among Asian/Pacific Islander populations—New York City, 2005. MMWR Morbidity and Mortality Weekly Report. 2006;55(18):505–509. [PubMed] [Google Scholar]
- 4.McQuillan G, Coleman P, Kruszon-Moran D. Prevalence of hepatitis B virus infection in the United States: The national health and nutrition examination surveys, 1976 through 1994. American Journal of Public Health. 1976;1999:14–18. doi: 10.2105/ajph.89.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chao SD, Le PV, Prapong W, Su J, So SK. High prevalence of chronic hepatitis B (HBV) infection in adult Chinese Americans living in California. Hepatology. 2004;40:717A. [Google Scholar]
- 6.2006–2008 American community survey 3 year estimates. Washington: United States Census Bureau, 2009.
- 7.World Health Organization. Hepatitis B Fact Sheet. (2008). Available at: http://www.who.int/mediacentre/factsheets/fs204/en/index.html. Accessed 10 August 2011.
- 8.CDC Hepatocellular carcinoma—United States, 2001–2006. MMWR Morbidity and Mortality Weekly Report. 2010;59:517–520. [PubMed] [Google Scholar]
- 9.Weinbaum CM, Williams I, Mast EE, Wang SA, Finelli L, Wasley A, et al. Recommendations for identification and public health management of persons with chronic hepatitis B virus infection. MMWR Morbidity and Mortality Weekly Report. 2008;57:1–20. [PubMed] [Google Scholar]
- 10.Wu CA, Lin SY, So SK, Chang ET. Hepatitis B and liver cancer knowledge and preventive practices among Asian Americans in San Francisco Bay Area, California. Asian Pacific Journal of Cancer Prevention. 2007;8:127–134. [PubMed] [Google Scholar]
- 11.Coronado G, Taylor VM, Tu S-P, et al. Correlates of hepatitis B testing among Chinese Americans. Journal of Community Health. 2007;32:379–390. doi: 10.1007/s10900-007-9060-x. [DOI] [PubMed] [Google Scholar]
- 12.Tu S-P, Li L, Tsai JH-C, et al. A cross-border comparison of hepatitis B testing among Chinese residing in Canada and the United States. Asian Pacific Journal of Cancer Prevention. 2009;10:483–490. [PMC free article] [PubMed] [Google Scholar]
- 13.Ma GX, Fang CY, Shive SE, Toubbeh JI, Tan Y, Sui P. Risk perceptions and barriers to hepatitis B screening and vaccination among Vietnamese immigrants. Journal of Immigrant and Minority Health. 2007;9:213–220. doi: 10.1007/s10903-006-9028-4. [DOI] [PubMed] [Google Scholar]
- 14.Lin SY, Chang ET, So SK. Why we should routinely screen Asian American adults for hepatitis B: A cross-sectional study of Asians in California. Hepatology. 2007;46:1034–1040. doi: 10.1002/hep.21784. [DOI] [PubMed] [Google Scholar]
- 15.Ma GX, Shive SE, Toubbeh JI, Tan Y, Wu D. Knowledge, attitudes and behaviors of Chinese hepatitis B screening and vaccination. American Journal of Health Behavior. 2008;32:178–187. doi: 10.5993/AJHB.32.2.7. [DOI] [PubMed] [Google Scholar]
- 16.Pulido MJ, Alvarado EA, Berger W, Nelson A, Todoroff C. Vaccinating Asian Pacific Islander children against hepatitis B: Ethnic-Specific influences and barriers. Asian American and Pacific Islander Journal of Health. 2001;9:211–220. [PubMed] [Google Scholar]
- 17.Organization of Chinese Americans and Asian American Studies Program, University of Maryland. (2008). A portrait of Chinese Americans: A national demographic and social profile of Chinese Americans, pp. 46–47. College Park: University of Maryland.
- 18.Chang ET, Keagan THM, Gomez SL, et al. The burden of liver cancer in Asians and Pacific Islanders in the greater San Francisco Bay Area, 1990 through 2004. Cancer. 2007;109:2100–2108. doi: 10.1002/cncr.22642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chronic Viral Hepatitis Registry Project, Communicable Disease Control & Prevention Section. (2009). Chronic hepatitis B surveillance report 2007–2008, San Francisco [Internet]. San Francisco, CA: San Francisco Department of Public Health. Available from: http://www.sfcdcp.org/publications.html.
- 20.Bailey, M. B., Shiau, R., Zola, J., Fernyak, S. E., So, S. K., & Chang, E. T. (2010). San Francisco Hep B Free: A grassroots community coalition to prevent hepatitis B and liver cancer. Journal of Community Health [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 21.Sheu LC, Toy BC, Kwahk E, Yu A, Adler J, Lai CJ. A model for interprofessional health disparities education: Student-led curriculum on chronic hepatitis B infection. Journal of General Internal Medicine. 2010;25(Suppl 2):S140–S145. doi: 10.1007/s11606-009-1234-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gish RG, Cooper SL. Hepatitis B in the greater San Francisco Bay Area: An integrated programme to respond to a diverse local epidemic. Journal of Viral Hepatitis. 2010;18:e40–e51. doi: 10.1111/j.1365-2893.2010.01382.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.UCLA Center for Health Policy Research, California Department of Health Services, Public Health Institute. (2009). California 801 Health Interview Survey (CHIS) 2007. www.chis.ucla.edu.
- 24.Taylor VM, Tu S-P, Woodall E, et al. Hepatitis B knowledge and practices among Chinese immigrants to the United States. Asian Pacific Journal of Cancer Prevention. 2006;7:313–317. [PubMed] [Google Scholar]
- 25.Taylor VM, Choe JH, Yasui Y, Li L, Burke N, Jackson JC. Hepatitis B awareness, testing and knowledge among Vietnamese American men and women. Journal of Community Health. 2005;30:477–490. doi: 10.1007/s10900-005-7282-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Taylor VM, Jackson JC, Pineda M, Pham P, Fischer M, Yasui Y. Hepatitis B knowledge among Vietnamese immigrants: implications for prevention of hepatocellular carcinoma. Journal of Cancer Education. 2000;15:51–55. doi: 10.1080/08858190009528654. [DOI] [PubMed] [Google Scholar]
- 27.Thompson MJ, Taylor VM, Jackson JC, et al. Hepatitis B knowledge and practices among Chinese American women in seattle, Washington. Journal of Cancer Education. 2002;17:222–226. doi: 10.1080/08858190209528842. [DOI] [PubMed] [Google Scholar]
- 28.Taylor VM, Coronado G, Acorda E, et al. Development of an ESL curriculum to educate chinese immigrants about hepatitis B. Journal of Community Health. 2008;33:217–224. doi: 10.1007/s10900-008-9084-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hislop G, Teh C-Z, Low A, et al. Hepatitis B knowledge, testing and vaccination levels in Chinese immigrants to British Columbia, Canada. Canadian Journal of Public Health. 2007;98:125–129. doi: 10.1007/BF03404323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Taylor VM, Yasui Y, Burke N, et al. Hepatitis B testing among Vietnamese American men. Cancer Detection and Prevention. 2004;28:170–177. doi: 10.1016/j.cdp.2004.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nguyen T, McPhee SJ, Stewart SL, et al. Factors associated with hepatitis B testing among Vietnamese Americans. Journal of General Internal Medicine. 2010;25:694–700. doi: 10.1007/s11606-010-1285-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lai CJ, Nguyen T, Hwang J, Stewart SL, Kwan A, McPhee SJ. Provider knowledge and practice regarding hepatitis B screening in Chinese-speaking patients. Journal of Cancer Education. 2007;22:37–41. doi: 10.1007/BF03174373. [DOI] [PubMed] [Google Scholar]
- 33.Khalili, M., Guy, J., Yu, A. et al. (2010). Hepatitis B and hepatocellular carcinoma screening among Asian Americans: Survey of safety net healthcare providers. Digestive Diseases and Sciences [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 34.Chao SD, Chang ET, Le PV, Prapong W, Kiernan M, So SK. The Jade Ribbon campaign: A model program for community outreach and education to prevent liver cancer in Asian Americans. Journal of Immigrant and Minority Health. 2009;11:281–290. doi: 10.1007/s10903-007-9094-2. [DOI] [PubMed] [Google Scholar]
- 35.Taylor VM, Yasui Y, Burke N. Hepatitis B knowledge and testing among Vietnamese-American women. Ethnicity and Disease. 2005;2005:761–767. [PubMed] [Google Scholar]
- 36.Cheung J, Lee TK, Teh C-Z, Wang CY, Kwan PW, Yoshida EM. Cross-sectional study of hepatitis B awareness among Chinese and Southeast Asian Canadians in the Vancouver-Richmond community. Canadian Journal of Gastroenterology. 2005;19:245–249. doi: 10.1155/2005/583406. [DOI] [PubMed] [Google Scholar]
- 37.Taylor VM, Jackson JC, Chan N. Hepatitis B knowledge and practices among Cambodian American women in Seattle, Washington. Journal of Community Health. 2002;27:151–163. doi: 10.1023/A:1015229405765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nguyen T, Taylor VM, Chen MS, Bastani R, Maxwell AE, McPhee SJ. Hepatitis B awareness, knowledge and screening among Asian Americans. Journal of Cancer Education. 2007;22:266–272. doi: 10.1007/BF03174128. [DOI] [PubMed] [Google Scholar]


