Abstract
We aimed to describe the potential benefit of new rapid molecular respiratory tests (MRT) in decreasing inappropriate antibiotic use among the inpatients presenting with influenza-like illness (ILI). We included patients from inpatient and outpatient departments who had ILI and performed MRT between 1 January 2015 and 31 December 2016 in a 265-bed private hospital in Istanbul. At the end of 2015, we implemented antimicrobial stewardship including systematic use of MRT. Then, we compared our observations between the year 2015 and the year 2016. We designed the study according to the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) tool. A U.S. Food and Drug Administration (FDA)-cleared multiplexed polymerase chain reaction (PCR) system (BioFire FilmArray, Idaho Technology, Salt Lake City, UT) which detects 17 viruses and three bacteria was used for diagnosis. In total, 1317 patients were included; 630 (48%) were inpatients and 569 (43%) were older than 16 years of age. At least one virus was detected in 747 (57%) patients. Rhinovirus/enterovirus, influenza virus, and adenovirus were the most commonly detected. Among hospitalized patients, in children, a significant decrease in antibiotic use (44.5% in 2015 and 28.8% in 2016, p = 0.009) was observed, but in adults, the decrease was not statistically significant (72% in 2015 and 63% in 2016, p = 0.36). The duration of antibiotic use after the detection of virus was significantly decreased in both children and adults (p < 0.001 and p = 0.007, respectively). By using MRT, inappropriate antibiotic use and, also, duration of inappropriate antibiotic use after the detection of virus was significantly decreased. It is time to increase the awareness about the viral etiology in respiratory tract infections (RTIs) and implement MRT in clinical practice.
Introduction
Respiratory tract infections (RTIs) are the most common reasons for admission to healthcare facilities and one of the leading causes of hospitalization [1, 2]. The viral pathogens in the etiology of RTIs became more detectable along with the improvement in molecular diagnostic methods in recent years. In adults, influenza virus, rhinovirus, adenovirus, respiratory syncytial virus (RSV), human coronavirus, and parainfluenza virus cause infections with considerable morbidity and mortality [1, 3], and in infants, RSV is the most common reason for RTIs among hospitalized patients [4]. The antibiotic prescription rate was reported to be more than 60% despite the high proportion of viral etiology [5–8].
Unnecessary antibiotic administration in viral infections and antimicrobial resistance prompted the implementation of antimicrobial stewardship (AMS) programs. The “Implementing an antibiotic stewardship program” guideline by the Infectious Diseases Society of America (IDSA) suggested rapid viral testing for respiratory pathogens to decrease inappropriate antibiotic use [9]. In this study, we aimed to describe the viral etiology in influenza-like illness (ILI) in children and adults and to show the benefit of new rapid molecular respiratory tests (MRT) in decreasing inappropriate antibiotic use.
Methods
Study population and design
We designed the study according to the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) tool [10]. We included consequent patients from inpatient and outpatient departments, who had moderate to severe ILI, and, therefore, needed further diagnostic evaluation between 1 January 2015 and 31 December 2016 in a 265-bed private hospital in Istanbul. Only the patients whom MRT was implemented for diagnosis were included in this study. MRT was introduced in our hospital in 2013, and the demand for MRT increased over the years. At the end of 2015, we enhanced our training on antimicrobial stewardship (AMS). The intervention consists of training physicians to increase awareness about MRT, highlighting antimicrobial resistance because of unnecessary antibiotic consumption at ad hoc meetings in each related department. Then, we compared our observations between the year 2015 and the year 2016.
This was a retrospective study performed by reviewing the patient charts. Clinical features of the patients, demographic characteristics, chronic diseases including malignant disorders, diabetes mellitus, chronic kidney and liver diseases, and detailed information about antibiotic and antiviral drugs during hospitalization were collected by the chart review. Complete blood count, C-reactive protein, and liver and kidney function tests were studied among all patients. Bacterial cultures (throat, sputum, blood, and urine) were obtained, and procalcitonin (PCT) was studied in all patients with suspicion of bacterial infection and/or in critical patients. Chest X-ray and lung computed tomography was done if lower respiratory tract infection (LRTI) was suspected.
Definitions
ILI was defined according to the World Health Organization (WHO) and explained as an acute respiratory infection with fever of ≥ 38 °C and cough and with onset within the last 10 days [11]. Inappropriate antibiotic use was defined as antibiotic use despite detection of virus without documented and/or suspicious bacterial infection. Antibiotic use duration was calculated as the duration of antibiotic use after the detection of virus in patients with inappropriate antibiotic use.
Diagnosis
For molecular detection and identification of respiratory viral pathogens, a U.S. Food and Drug Administration (FDA)-cleared multiplexed respiratory polymerase chain reaction (PCR) system (MRT), BioFire FilmArray (Idaho Technology, Salt Lake City, UT) which detects 17 viral respiratory pathogens (adenovirus, coronavirus HKU1, coronavirus NL63, coronavirus 229E, coronavirus OC43, hMPV, rhinovirus/enterovirus, influenza A, influenza A/H1, influenza A/H1-2009, influenza A/H3, influenza B, parainfluenza 1, parainfluenza 2, parainfluenza 3, parainfluenza 4, and RSV) and three bacteria (Bordetella pertussis, Chlamydophila pneumoniae, and Mycoplasma pneumoniae) was used according to the manufacturer’s instructions. MRT yielded results within a few hours and the results were immediately reported to the physician of the patients by laboratory staff.
Data analysis
In the statistical analysis, the t-test for continuous variables and the chi-square test for comparison of categorical variables were used. In the analysis, STATA 11 (StataCorp, College Station, TX) was used and a p-value < 0.05 was set as being significant. The Institutional Review Board of Koç University approved the study (2015.172.IRB3.087).
Results
In total, 1317 patients whom MRT was implemented were included; 630 (48%) were inpatients and 569 (43%) were older than 16 years of age. At least one virus was detected in 747 (57%) patients and 359 (48%) of them were inpatients (Fig. 1). Among the patients who have viral pathogens in etiology, 211 (28.2%) were adult, and influenza A (52 of 211) (25%), rhinovirus/enterovirus (49 of 211) (23%), and influenza B (33 of 211) (16%) were the most commonly detected viruses. Among children, rhinovirus/enterovirus (182 of 536) (34%), adenovirus (92 of 536) (17%), influenza A (66 of 536) (12%), RSV (63 of 536) (12%), and influenza B (53 of 536) (10%) were the most commonly detected viruses (Fig. 2). In 71 patients out of 747 (9.5%), multiple viral pathogens were detected.
Fig. 1.
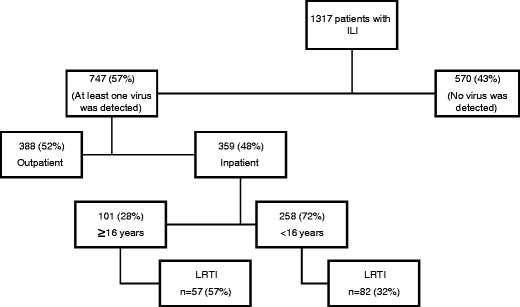
Study population. ILI: influenza-like illness; LRTI: lower respiratory tract infection
Fig. 2.
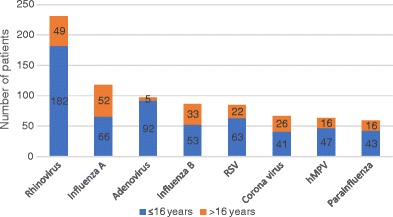
The most commonly detected viruses among all patients in whom at least one virus was detected. RSV: respiratory syncytial virus; hMPV: human metapneumovirus
The overall rate of LRTIs was 57% among inpatients. Among inpatients infected with RSV, the rate of LRTI was 91% in adults and 70% in children. Similarly, in hMPV infections, the rate of LRTI was 73% in adults and 60% in children (Table 1).
Table 1.
Clinical and laboratory findings in respiratory system infections caused by different viruses among adult and child inpatients
| Adult | Children | |||||||
|---|---|---|---|---|---|---|---|---|
| No. (%) | Mean age (years) | LRTI (%) | Fatal | No. (%) | Mean age (years) | LRTI (%) | Fatal | |
| Rhinovirus/enterovirus | 20 (20) | 62.05 (SD = 22.45) | 11 (55%) | 0 | 79 (31) | 4.6 (SD = 3.97) | 29 (37%) | 0 |
| Adenovirus | 3 (3) | 37.7 (SD = 10.6) | 2 (67%) | 0 | 57 (22) | 4.09 (SD = 1.71) | 9 (16%) | 0 |
| Influenza A | 32 (32) | 52.9 (SD = 19.9) | 17 (53%) | 1 | 32 (14) | 4.84 (SD = 3.48) | 5 (16%) | 0 |
| Influenza B | 9 (9) | 49.7 (SD = 15.7) | 2 (22%) | 0 | 16 (6) | 5.25 (SD = 3.3) | 1 (6%) | 0 |
| RSV | 11 (11) | 75.2 (SD = 12.2) | 10 (91%) | 0 | 33 (13) | 2.24 (SD = 2.48) | 23 (70%) | 0 |
| Coronavirus | 11 (11) | 69.9 (SD = 16.1) | 5 (45%) | 1 | 17 (7) | 3.35 (SD = 1.87) | 3 (18%) | 0 |
| hMPV | 11 (11) | 59.9 (SD = 15.8) | 8 (73%) | 0 | 25 (10) | 3.16 (SD = 2.54) | 15 (60%) | 0 |
| Parainfluenza | 9 (9) | 69.4 (SD = 12.8) | 6 (67%) | 0 | 17 (7) | 2.35 (SD = 2.52) | 6 (35%) | 0 |
| Total | 101 (100) | 60.4 (SD = 19.4) | 57 (57%) | 2 | 258 (100) | 3.9 (SD = 3.15) | 82 (32%) | 0 |
RSV: Respiratory syncytial virus; hMPV: human metapneumovirus; LRTI: lower respiratory tract infection
In total, among hospitalized patients, antibiotics were continued inappropriately in 45% (160/359) of all inpatients, despite detection of the virus, but there was a reduction in 2016 when compared with 2015 [51.3% (81/158) in 2015 and 39.3% (79/201) in 2016, p = 0.024] (Table 2). In children, the antibiotic continuation rate was 44.5% in 2015 and decreased to 28.8% in 2016 (p = 0.009); in adults, there was a decrease towards 2016 but this was not significant (Table 2). The mean duration of inappropriate antibiotic use after the detection of virus decreased in both adults and children in 2016 when compared with 2015. The most commonly inappropriately used antibiotics were third-generation cephalosporins, quinolones, and second-generation cephalosporins.
Table 2.
Antibiotic continuation details of inpatients with positive molecular respiratory tests (MRT)
| Children | p-Value | Adults | p-Value | |||
|---|---|---|---|---|---|---|
| Before intervention (year 2015) | After intervention (year 2016) | Before intervention (year 2015) | After intervention (year 2016) | |||
| Inappropriate antibiotic use (%) | 53/119 (44.5) | 40/139 (28.8) | 0.009 | 28/39 (72) | 39/62 (63) | 0.36 |
| Mean duration of inappropriate antibiotic use (days) | 6.5 (SD 3.1) | 4.6 (SD 2.0) | < 0.001 | 9.7 (SD 7.3) | 6.2 (SD 3.7) | 0.007 |
Discussion
In our study, rhinovirus/enterovirus, influenza, and adenovirus were the most commonly detected viruses in the etiology of ILI. In a recent study by Jain et al. [3], a population-based surveillance for community-acquired pneumonia among adults aged 18 years and older was conducted. Human rhinovirus, influenza A and B virus, and hMPV were the most commonly detected viruses in etiology. Influenza virus and rhinovirus were reported to be the most commonly detected viruses in both adults and children in Turkey [12]. Among inpatients older than 16 years of age, 57% had LRTI, and influenza A, rhinovirus, RSV, and hMPV were the most common agents. Among children, 32% had LRTI, and rhinovirus, RSV, and hMPV were the most common agents (Fig. 2; Table 1). Any effort targeted to reduce the unnecessary use of antibiotics in viral pneumonia could be useful in this era of antibiotic resistance.
Because of the high rate of inappropriate antibiotic prescription despite the availability of MRT, we decided to improve training sessions about the diagnosis and management of respiratory system infections at the end of 2015. Then, we performed an observational comparison between the practice in 2015 and 2016. There was a decrease in antibiotic use towards 2016 among all inpatients. However when analyzed separately, a significant reduction in children but not in adults was detected (Table 2). The significant reduction of antibiotic use in children but not in adults could be explained by differences in physicians’ experience in MRT. Despite the fact that there was a reduction in antibiotic use in children after the detection of virus, antibiotic prescription rates were still high. In a recent study, the impact of MRT on antibiotic use was investigated and it was seen that antibiotics were still continued in about 75% of the patients, despite the detection of virus. This finding was explained by being a new test [13]. In another study, Afzal et al. [14] reported that a positive result for MRT decreased antibiotic use duration and prescription rate but the decrease in antibiotic prescription was not statistically significant. Timbrook et al. [15] studied MRT in combination with PCT and concluded that a lower level of PCT and detection of virus by MRT were not associated with decreased use of antibiotics in RTIs, but in another study, a lower level of PCT in combination with detection of virus was found to be associated with shortened duration of antibiotic usage [16]. In a randomized controlled study, the effect of both MRT and PCT on antibiotic use was evaluated and the duration of antibiotic use was found to be decreased in cases of viral infection with lower levels of PCT [17].
One of the strongest parts of our study was having the opportunity of ordering MRT whenever needed in routine clinical practice, so we reached a large sample size. We had the opportunity of getting the results of C-reactive protein, PCT, and MRT within a few hours, so we discriminated bacterial or viral etiology quickly. One of the limitations of this study was being conducted in a single center, but our center was unique for implementing this test in clinical practice. We are unique because MRT are still expensive to perform in routine clinical practice in other hospitals.
Future studies for rapid point-of-care testing for respiratory viruses might improve clinical care by reducing unnecessary antibiotic use [18]. Future cost-effective studies for the implementation of MRT will be useful.
Conclusions
By using molecular rapid tests (MRT) in our hospital, inappropriate antibiotic use and also duration of inappropriate antibiotic use after the detection of virus was significantly decreased among inpatients. The treatment paradigm for respiratory tract infections (RTIs) is changing, but molecular viral diagnostic tests are in their infancy. It is time to increase the awareness of the viral etiology in RTIs and implement MRT in clinical practice.
Funding
No funding of any kind has been received. The data were generated as part of routine work.
Compliance with ethical standards
Conflict of interest
None to declare.
Ethical approval
Koç University IRB approved the study.
Informed consent
Not applicable.
References
- 1.Widmer K, Zhu Y, Williams JV, Griffin MR, Edwards KM, Talbot HK. Rates of hospitalizations for respiratory syncytial virus, human metapneumovirus, and influenza virus in older adults. J Infect Dis. 2012;206(1):56–62. doi: 10.1093/infdis/jis309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hirsch HH, Martino R, Ward KN, Boeckh M, Einsele H, Ljungman P. Fourth European Conference on Infections in Leukaemia (ECIL-4): guidelines for diagnosis and treatment of human respiratory syncytial virus, parainfluenza virus, metapneumovirus, rhinovirus, and coronavirus. Clin Infect Dis. 2013;56(2):258–266. doi: 10.1093/cid/cis844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jain S, Self WH, Wunderink RG, Fakhran S, Balk R, Bramley AM, Reed C, Grijalva CG, Anderson EJ, Courtney DM, Chappell JD, Qi C, Hart EM, Carroll F, Trabue C, Donnelly HK, Williams DJ, Zhu Y, Arnold SR, Ampofo K, Waterer GW, Levine M, Lindstrom S, Winchell JM, Katz JM, Erdman D, Schneider E, Hicks LA, McCullers JA, Pavia AT, Edwards KM, Finelli L, CDC EPIC Study Team Community-acquired pneumonia requiring hospitalization among U.S. adults. N Engl J Med. 2015;373(5):415–427. doi: 10.1056/NEJMoa1500245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schanzer DL, Langley JM, Tam TW. Role of influenza and other respiratory viruses in admissions of adults to Canadian hospitals. Influenza Other Respir Viruses. 2008;2(1):1–8. doi: 10.1111/j.1750-2659.2008.00035.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ebell MH, Radke T. Antibiotic use for viral acute respiratory tract infections remains common. Am J Manag Care. 2015;21(10):e567–e575. [PubMed] [Google Scholar]
- 6.Mainous AG, 3rd, Saxena S, Hueston WJ, Everett CJ, Majeed A. Ambulatory antibiotic prescribing for acute bronchitis and cough and hospital admissions for respiratory infections: time trends analysis. J R Soc Med. 2006;99(7):358–362. doi: 10.1177/014107680609900719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grijalva CG, Nuorti JP, Griffin MR. Antibiotic prescription rates for acute respiratory tract infections in US ambulatory settings. JAMA. 2009;302(7):758–766. doi: 10.1001/jama.2009.1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fleming-Dutra KE, Hersh AL, Shapiro DJ, Bartoces M, Enns EA, File TM, Jr, Finkelstein JA, Gerber JS, Hyun DY, Linder JA, Lynfield R, Margolis DJ, May LS, Merenstein D, Metlay JP, Newland JG, Piccirillo JF, Roberts RM, Sanchez GV, Suda KJ, Thomas A, Woo TM, Zetts RM, Hicks LA. Prevalence of inappropriate antibiotic prescriptions among US ambulatory care visits, 2010–2011. JAMA. 2016;315(17):1864–1873. doi: 10.1001/jama.2016.4151. [DOI] [PubMed] [Google Scholar]
- 9.Barlam TF, Cosgrove SE, Abbo LM, MacDougall C, Schuetz AN, Septimus EJ, Srinivasan A, Dellit TH, Falck-Ytter YT, Fishman NO, Hamilton CW, Jenkins TC, Lipsett PA, Malani PN, May LS, Moran GJ, Neuhauser MM, Newland JG, Ohl CA, Samore MH, Seo SK, Trivedi KK. Implementing an antibiotic stewardship program: guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis. 2016;62(10):e51–e77. doi: 10.1093/cid/ciw118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization (WHO) (2014) WHO surveillance case definitions for ILI and SARI. Case definitions for influenza surveillance. Available online at: http://www.who.int/influenza/surveillance_monitoring/ili_sari_surveillance_case_definition/en
- 12.Goktas S, Sirin MC. Prevalence and seasonal distribution of respiratory viruses during the 2014–2015 season in Istanbul. Jundishapur J Microbiol. 2016;9(9):e39132. doi: 10.5812/jjm.39132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yee C, Suarthana E, Dendukuri N, Nicolau I, Semret M, Frenette C. Evaluating the impact of the multiplex respiratory virus panel polymerase chain reaction test on the clinical management of suspected respiratory viral infections in adult patients in a hospital setting. Am J Infect Control. 2016;44(11):1396–1398. doi: 10.1016/j.ajic.2016.04.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Afzal Z, Minard CG, Stager CE, Yu VL, Musher DM. Clinical diagnosis, viral PCR, and antibiotic utilization in community-acquired pneumonia. Am J Ther. 2016;23(3):e766–e772. doi: 10.1097/MJT.0000000000000018. [DOI] [PubMed] [Google Scholar]
- 15.Timbrook T, Maxam M, Bosso J. Antibiotic discontinuation rates associated with positive respiratory viral panel and low procalcitonin results in proven or suspected respiratory infections. Infect Dis Ther. 2015;4(3):297–306. doi: 10.1007/s40121-015-0087-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gelfer G, Leggett J, Myers J, Wang L, Gilbert DN. The clinical impact of the detection of potential etiologic pathogens of community-acquired pneumonia. Diagn Microbiol Infect Dis. 2015;83(4):400–406. doi: 10.1016/j.diagmicrobio.2015.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Branche AR, Walsh EE, Vargas R, Hulbert B, Formica MA, Baran A, Peterson DR, Falsey AR. Serum procalcitonin measurement and viral testing to guide antibiotic use for respiratory infections in hospitalized adults: a randomized controlled trial. J Infect Dis. 2015;212(11):1692–1700. doi: 10.1093/infdis/jiv252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brendish NJ, Malachira AK, Armstrong L, Houghton R, Aitken S, Nyimbili E, Ewings S, Lillie PJ, Clark TW. Routine molecular point-of-care testing for respiratory viruses in adults presenting to hospital with acute respiratory illness (ResPOC): a pragmatic, open-label, randomised controlled trial. Lancet Respir Med. 2017;5(5):401–411. doi: 10.1016/S2213-2600(17)30120-0. [DOI] [PMC free article] [PubMed] [Google Scholar]


