Abstract
Government and nongovernmental organizations need national and global estimates on the descriptive epidemiology of common oral conditions for policy planning and evaluation. The aim of this component of the Global Burden of Disease study was to produce estimates on prevalence, incidence, and years lived with disability for oral conditions from 1990 to 2017 by sex, age, and countries. In addition, this study reports the global socioeconomic pattern in burden of oral conditions by the standard World Bank classification of economies as well as the Global Burden of Disease Socio-demographic Index. The findings show that oral conditions remain a substantial population health challenge. Globally, there were 3.5 billion cases (95% uncertainty interval [95% UI], 3.2 to 3.7 billion) of oral conditions, of which 2.3 billion (95% UI, 2.1 to 2.5 billion) had untreated caries in permanent teeth, 796 million (95% UI, 671 to 930 million) had severe periodontitis, 532 million (95% UI, 443 to 622 million) had untreated caries in deciduous teeth, 267 million (95% UI, 235 to 300 million) had total tooth loss, and 139 million (95% UI, 133 to 146 million) had other oral conditions in 2017. Several patterns emerged when the World Bank’s classification of economies and the Socio-demographic Index were used as indicators of economic development. In general, more economically developed countries have the lowest burden of untreated dental caries and severe periodontitis and the highest burden of total tooth loss. The findings offer an opportunity for policy makers to identify successful oral health strategies and strengthen them; introduce and monitor different approaches where oral diseases are increasing; plan integration of oral health in the agenda for prevention of noncommunicable diseases; and estimate the cost of providing universal coverage for dental care.
Keywords: caries, periodontitis, edentulism, epidemiology, economic development, global health
Introduction
The Global Burden of Disease (GBD) study has demonstrated consistently that oral health represents a major neglected global population health challenge (Marcenes et al. 2013; Kassebaum et al. 2017). The GBD 2015 findings were used to advocate for integrating oral conditions with noncommunicable disease prevention and including dental services in universal health coverage (Peres et al. 2019; Watt et al. 2019). Government and nongovernmental organizations will need ongoing national and global evidence on the descriptive epidemiology of common oral conditions.
The GBD study data and analytic tools provide a chance to evaluate progress toward oral health goals across all world geographies and over time in a comparable fashion. Data from the GBD study also offer the opportunity to identify countries achieving major success toward oral health goals, thereby helping to identify successful oral health strategies to reduce the burden of oral conditions. The GBD study also indicates the countries with the greatest needs for action and the health conditions causing the highest burden (GBD 2017 DALYs and HALE Collaborators 2018).
It is also important to assess whether there is a global socioeconomic pattern in the distribution of oral conditions. For a long time, various international agencies, such as World Health Organization (WHO), World Bank, UNICEF, and United Nations Development Program, have made health inequalities a priority issue (Ruger and Kim 2006). Several high-income countries now incorporate reducing health inequalities in their health policies. However, there is no global problem definition of oral health inequalities due to a lack of comparable data. To date, there is no comprehensive study to assess inequalities among high-, middle-, and low-income countries.
The aim of this component of the GBD study was to produce estimates on the prevalence, incidence, and years lived with disability (YLDs) for untreated dental caries, severe periodontitis, and total tooth loss in 1990 and 2017 by sex, age, and countries. In addition, the study reports the global socioeconomic pattern in the burden of oral conditions by GBD Sociodemographic Index (SDI) and World Bank classification of economies. This report supersedes the GBD 2010 and 2015 reports.
Method
The GBD 2017 study gathered data on untreated dental caries, severe periodontitis, total tooth loss, and limited data on other oral disorders for 195 countries and territories. Details about the full GBD methodology can be found in the GBD capstone manuscripts (GBD 2017 DALYs and HALE Collaborators 2018; GBD 2017 Disease and Injury Incidence and Prevalence Collaborators 2018). This report outlines the methods in relation to oral conditions. The technical aspects of the modeling undertaking are detailed in the Appendix. This report adheres to the GATHER statement (Guidelines for Accurate and Transparent Health Estimates Reporting; Stevens et al. 2016).
Data Input
Data to inform models for oral conditions were from systematic reviews on the epidemiology of each oral condition (Kassebaum et al. 2014a, 2014b, 2015), which were updated for this new iteration of the project. For the GBD 2017 study, a major effort to identify unpublished survey reports was carried out in partnership with the WHO Oral Health Program. Chief dental officers and regional WHO officers were contacted and asked to provide any survey carried out in their countries/regions.
The case definitions and their associated disability were in line with earlier reports (Marcenes et al. 2013; Kassebaum et al. 2017). Briefly, case definitions were as follows:
Untreated caries: “a lesion in a pit or fissure, on a smooth tooth surface, has an unmistakable cavity, undermined enamel, or a detectably softened or floor or wall (coronal caries), or feel soft or leathery to probing (root caries).”
Severe periodontitis: “a gingival pocket depth equal or more than 6 mm, or Community Periodontal Index of Treatment Needs (CPITN) also referred as Community Periodontal Index (CPI) score of 4, or a clinical attachment loss (CAL) more than 6 mm.”
Total tooth loss: “complete loss of natural teeth.”
The last condition could be assessed either via clinical examination or self-reports. Only surveys based on random samples taken from national or regional populations—with acceptable response (>50%) and attrition (<50%) rates and reporting prevalence and/or incidence data—were included. Further methodological details, including selection criteria and data availability, can be found in the Appendix. The sources of data are listed in the Global Health Data Exchange (http://ghdx.healthdata.org).
Countries were classified by economic development according to the standard World Bank classification of economies (high-, upper-middle-, lower-middle-, and low-income countries) and the GBD SDI. The SDI is the geometric average of 3 rescaled components: average income, average educational attainment for those ≥15 y old, and number of births per woman aged 10 to 24 y. SDI scores were scaled from 0 (lowest values) to 1 (highest values). Countries were then organized into quintiles of the SDI distribution (GBD 2017 DALYs and HALE Collaborators 2018).
Data Modeling
Estimates of prevalence, incidence, and remission were generated with DisMod-MR 2.1, a Bayesian metaregression tool that ensures consistency among estimates (Flaxman et al. 2015). Further DisMod-MR 2.1 details, as applied to modeling oral conditions, are contained in the Appendix. The full time series (1990 to 2017) was recalculated to produce comparable estimates for trends.
The key population metric in the GBD study is disability-adjusted life years (DALYs), which are estimated as the sum of the years of life lost due to premature mortality and YLDs (Murray et al. 2012; GBD 2015 DALYs and HALE Collaborators 2016; GBD 2017 DALYs and HALE Collaborators 2018). Since death as a direct result of oral conditions is rare, it is assumed that they do not lead to years of life lost. All DALYs estimates for oral conditions thus reflect YLDs only. YLDs are calculated by multiplying frequency (prevalence), severity (disability weight), and duration of the condition (Salomon et al. 2012; Salomon et al. 2015). The disability for untreated symptomatic caries was defined as “a toothache, which causes some difficulty eating.” Untreated caries was classified as asymptomatic, mild, and severe. It was assumed that those with mild disability have episodic pain lasting 1 h/d. Severe disability were modeled as an “initial” stage of episodic pain and a “terminal” stage of constant pain, the length of which was determined by performing log-normal distribution of symptom duration from casualty ward studies (Kassebaum et al. 2017). The distribution of the sequelae for untreated caries was calculated via meta-analyses of the proportion of individuals with symptomatic caries and the duration of their symptoms (Appendix). The disability for severe periodontitis and total tooth loss were, respectively, “bad breath, a bad taste in the mouth, and gums that bleed a little from time to time, but this does not interfere with daily activities” and “great difficulty in eating meat, fruits, and vegetables.” All cases with severe periodontitis and total tooth loss were assumed to be symptomatic. The presence of comorbidity in each age group, sex, geography, and year was estimated through microsimulations. YLDs for each comorbid condition were then adjusted proportionally.
One DALY (YLDs = DALYs for oral conditions) reflects a year of “healthy life” lost due to diseases or injuries, whereas the sum of DALYs reflects the gap between the population’s current health status and an ideal situation where people live the standard life expectancy in full health (i.e., disease-free; GBD 2017 DALYs and HALE Collaborators 2018). The DALYs metric is commonly used to identify the top causes of burden and monitor changes over time (GBD 2017 DALYs and HALE Collaborators 2018). We report YLDs and YLD rates (per 100,000 population), prevalent and incident cases, and age-standardized prevalence and incidence (per 100). Age standardization, based on the GBD reference population (GBD 2017 Mortality Collaborators 2018), was used to account for variations in population size and age structure (GBD 2015 DALYs and HALE Collaborators 2016). Percentage change, [(estimate2017 – estimate1990) / estimate1990 ] × 100, was used to assess trends.
Uncertainty in all estimates was derived from 1,000 draws at every step of the computational process. Uncertainty comes from sampling error in data sources, the distribution of condition severity and disability weights, and model coefficients. The final estimates are calculated as the average across the 1,000 draws, with the 95% uncertainty interval (UI) computed as percentiles 25th and 975th in the distribution (GBD 2017 Disease and Injury Incidence and Prevalence Collaborators 2018).
Results
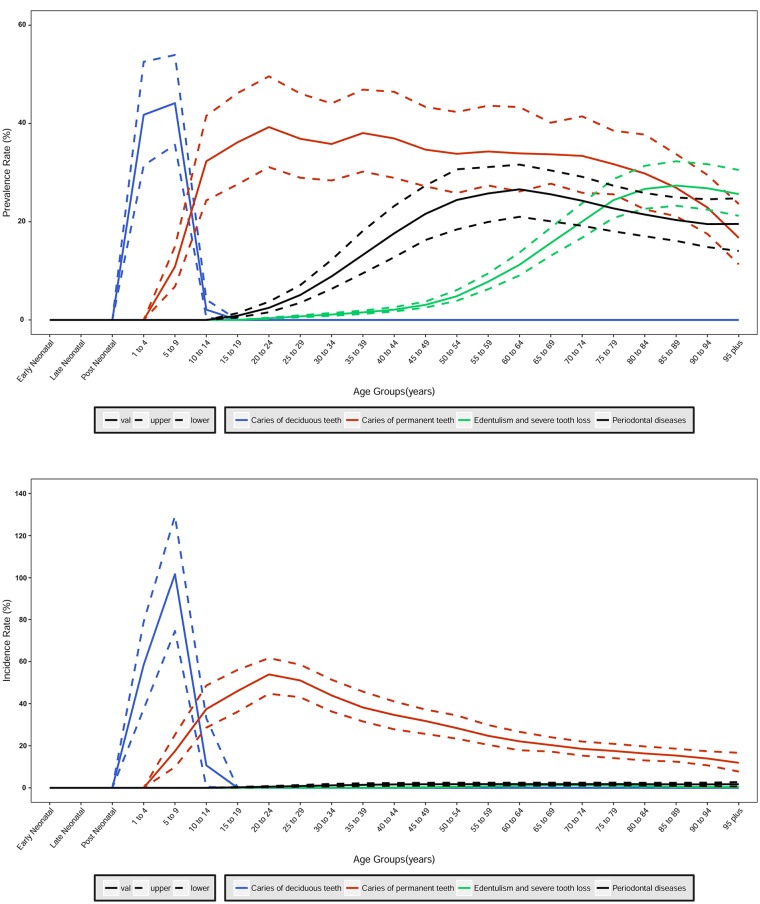
No gender differences at the global level were identified. Therefore, results are presented for both sexes together. The global patterns in prevalence and incidence of oral conditions by age in 2017 are depicted in Figure 1. Estimates for 1990 are reported in Appendix Table 11. The prevalence of untreated caries in deciduous teeth peaked at age 5 y, and that in permanent teeth was the highest at age 20 to 24 y. The prevalence of severe periodontitis peaked at age 60 to 64 y. For total tooth loss, it increased up to age 85 to 89 y and then flattened out. The geographic distribution of the burden of oral conditions is presented in Figure 2. Country-level data are presented in Appendix Tables 12 to 17.
Figure 1.
Global age pattern of prevalence and incidence of untreated caries in deciduous teeth, untreated caries in permanent teeth, severe periodontitis, and total tooth loss in 2017 for both sexes combined.
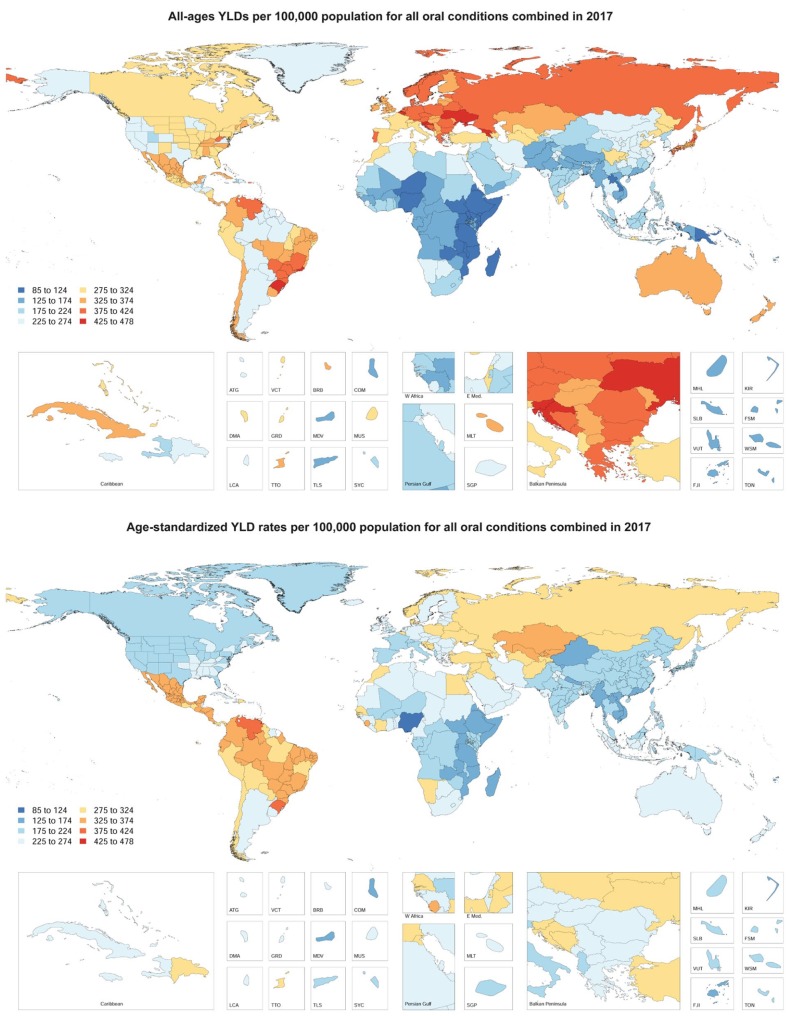
Figure 2.
World map of all-ages YLDs and age-standardized YLD rates (per 100,000 population) for all oral conditions combined in 2017 for both sexes. YLDs, years lived with disability.
Untreated Dental Caries in Deciduous Teeth
The age-standardized prevalence of caries in deciduous teeth was 7.8% (95% UI, 6.5% to 9.1%) in 2017, while the number of prevalent cases was 532 million (95% UI, 443 to 622 million; Table 1). Their corresponding percentage changes between 1990 and 2017 were –7.9% (95% UI, –9.8% to –6.6%) and 1.3% (95% UI, –0.9% to 3.0%; Table 2). The age-standardized YLD rate was 2.0 per 100,000 population (95% UI, 0.9 to 4.1) in 2017, and the number of all-ages YLDs was 0.1 million (95% UI, 0.06 to 0.3 million). Their corresponding percentage changes were –9.0% (95% UI, –11.0% to –7.3%) and 0.2% (95% UI, –2.3% to 2.2%) between 1990 and 2017.
Table 1.
Global Estimates of Burden of Oral Conditions in 2017.
| All Ages (No. of Cases) | Prevalence (Millions) | Incidence (Millions) | YLDs (Millions) |
|---|---|---|---|
| All oral conditions | 3,467 (3,272 to 3,676) | 3,600 (3,233 to 3,992) | 18.3 (10.9 to 28.3) |
| Untreated caries in deciduous teeth | 532 (443 to 622) | 1,058 (756 to 1,401) | 0.1 (0.06 to 0.3) |
| Untreated caries in permanent teeth | 2,302 (2,105 to 2,526) | 2,452 (2,234 to 2,665) | 1.6 (0.7 to 3.1) |
| Severe periodontitis | 796 (671 to 930) | 71 (62 to 81) | 5.2 (2.0 to 10.7) |
| Total tooth loss | 267 (235 to 300) | 18 (16 to 21) | 7.3 (4.9 to 10.4) |
| Other oral conditions | 139 (133 to 146) | 4.0 (2.5 to 5.9) | |
| Age Standardized | Prevalence (per 100) | Incidence (per 100) | YLD Rate (per 100,000) |
| All oral conditions | 45.0 (42.3 to 47.6) | 48.3 (43.1 to 53.9) | 228.8 (137.5 to 353.7) |
| Untreated caries in deciduous teeth | 7.8 (6.5 to 9.1) | 15.5 (11.1 to 20.5) | 2.0 (0.9 to 4.1) |
| Untreated caries in permanent teeth | 29.4 (26.8 to 32.2) | 31.6 (28.7 to 34.4) | 20.7 (8.9 to 39.2) |
| Severe periodontitis | 9.8 (8.2 to 11.4) | 0.9 (0.7 to 1.0) | 63.5 (25.0 to 130.3) |
| Total tooth loss | 3.3 (2.9 to 3.7) | 0.2 (0.2 to 0.2) | 91.7 (61.3 to 129.9) |
| Other oral conditions | 1.8 (1.7 to 1.9) | 50.9 (31.8 to 74.7) |
Number of prevalent and incident cases and YLDs, as well as age-standardized prevalence, incidence, and YLD rate, in 2017 for untreated caries, severe periodontitis, total tooth loss, other oral conditions, and all oral conditions combined, globally. Values in brackets correspond to the 95% uncertainty interval.
YLDs, years lived with disability.
Table 2.
Percentage Change in Global Estimates of Burden of Oral Conditions between 1990 and 2017.
| All Ages (No. of Cases) | Age Standardized | |||||
|---|---|---|---|---|---|---|
| Prevalence | Incidence | YLDs | Prevalence | Incidence | YLD rate | |
| All oral conditions | 38.3 (36.4 to 40.3) | 31.4 (29.1 to 34.4) | 68.0 (65.2 to 70.5) | −5.5 (−6.0 to −4.9) | −0.3 (−1.1 to 0.6) | −4.0 (−5.7 to −2.4) |
| Untreated caries in deciduous teeth | 1.3 (−0.9 to 3.0) | 8.7 (6.3 to 11.2) | 0.2 (−2.3 to 2.2) | −7.9 (−9.8 to −6.6) | −2.2 (−3.9 to −0.4) | −9.0 (−11.0 to −7.3) |
| Untreated caries in permanent teeth | 35.9 (33.5 to 38.3) | 42.9 (40.1 to 45.5) | 32.0 (29.3 to 34.8) | −8.8 (−9.5 to −7.9) | 0.6 (−0.5 to 1.8) | −11.9 (−13.4 to −10.3) |
| Severe periodontitis | 90.1 (87.4 to 92.5) | 79.0 (75.5 to 82.6) | 90.2 (87.4 to 92.6) | 5.8 (4.9 to 6.6) | 4.3 (3.3 to 5.3) | 6.0 (5.2 to 6.8) |
| Total tooth loss | 75.5 (74.2 to 76.9) | 72.2 (70.1 to 74.3) | 75.5 (74.2 to 76.9) | −10.4 (−11.2 to −9.6) | −8.0 (−8.6 to −7.3) | −10.1 (−10.9 to −9.3) |
| Other oral conditions | 53.8 (52.5 to 55.2) | 53.5 (52.1 to 55.0) | 0.0 (−0.2 to 0.2) | 0.2 (−0.1 to 0.6) | ||
Percentage change in number of prevalent and incident cases and YLDs, as well as age-standardized prevalence, incidence, and YLD rate, between 1990 and 2017 for untreated caries, severe periodontitis, total tooth loss, other oral conditions, and all oral conditions combined, globally. Values in brackets correspond to the 95% uncertainty interval.
YLDs, years lived with disability.
In 2017, the lowest numbers of prevalent cases and all-ages YLDs were observed in high-income countries (41 million cases [95% UI, 32 to 49 million] and 0.02 million YLDs [95% UI, 0.01 to 0.03 million]) and the highest in lower-middle-income countries (265 million cases [95% UI, 222 to 311 million] and 0.06 million YLDs [95% UI, 0.03 to 0.13 million]). Similarly, the lowest age-standardized prevalence and YLD rate were found in high-income countries (6.1% [95% UI, 4.8% to 7.3%] and 2.3 per 100,000 population [95% UI, 1.0 to 4.6], respectively; Table 3).
Table 3.
Estimates of Burden of Oral Conditions by World Bank Income Groups.
| All Ages (No. of Cases) | Percentage Change 1990 to 2017 | Age Standardized | Percentage Change 1990 to 2017 | |||||
|---|---|---|---|---|---|---|---|---|
| Prevalence (Millions) | YLDs (Millions) | Prevalence | YLDs | Prevalence (per 100) | YLD Rate (per 100,000) | Prevalence | YLDs | |
| High-income countries | ||||||||
| All oral conditions | 534(507 to 563) | 3.8(2.4 to 5.7) | 14.0(12.4 to 15.5) | 19.9(18.6 to 21.2) | 41.2(38.7 to 43.7) | 223.0(138.4 to 337.8) | −8.2(−9.1 to −7.3) | −15.6(−17.2 to −14.4) |
| Untreated caries in deciduous teeth | 41(32 to 49) | 0.02(0.01 to 0.03) | −12.9(−16.3 to −9.6) | −13.6(−17.4 to −10.0) | 6.1(4.8 to 7.3) | 2.3(1.0 to 4.6) | −6.4(−10.1 to −3.0) | −7.1(−11.3 to −3.3) |
| Untreated caries in permanent teeth | 386(355 to 420) | 0.4(0.2 to 0.7) | 11.5(9.3 to 13.7) | 9.5(7.3 to 11.9) | 29.5(27.1 to 32.3) | 28.3(12.3 to 54.6) | −9.0(−10.2 to −7.9) | −10.4(−11.8 to −9.1) |
| Severe periodontitis | 112(93 to 132) | 0.7(0.3 to 1.5) | 23.7(20.0 to 27.8) | 23.1(19.4 to 27.0) | 6.6(5.5 to 7.8) | 42.8(16.9 to 87.9) | −14.3(−16.3 to −12.2) | −14.4(−16.3 to −12.3) |
| Total tooth loss | 74(65 to 83) | 2.0(1.4 to 2.9) | 20.3(18.9 to 21.8) | 19.9(18.5 to 21.4) | 3.6(3.1 to 4.0) | 99.0(65.8 to 141.2) | −23.7(−24.9 to −22.4) | −23.6(−24.8 to −22.2) |
| Other oral conditions | 24(23 to 25) | 0.7(0.4 to 1.0) | 24.4(23.3 to 25.5) | 23.8(22.5 to 25.1) | 1.8(1.7 to 1.8) | 50.7(31.7 to 75.2) | −0.3(−0.4 to −0.1) | −0.2(−0.8 to 0.4) |
| Upper-middle-income countries | ||||||||
| All oral conditions | 1,190(1,121 to 1,263) | 7.4(4.5 to 11.4) | 24.3(21.3 to 27.7) | 76.3(72.0 to 80.4) | 43.9(41.3 to 46.6) | 236.4(144.3 to 363.5) | −5.5(−6.4 to −4.6) | −0.6(−1.4 to 0.3) |
| Untreated caries in deciduous teeth | 150(125 to 175) | 0.04(0.02 to 0.08) | −26.6(−29.5 to −24.7) | −24.9(−27.8 to −22.8) | 8.5(7.1 to 10.0) | 2.4(1.0 to 4.7) | −6.8(−10.1 to −4.5) | −4.6(−8.1 to −2.0) |
| Untreated caries in permanent teeth | 768(702 to 839) | 0.5(0.2 to 1.1) | 20.6(16.7 to 24.7) | 20.5(17.0 to 24.5) | 27.4(24.9 to 30.1) | 19.7(8.5 to 37.4) | −9.3(−10.4 to −8.1) | −9.1(−10.1 to −7.9) |
| Severe periodontitis | 314(262 to 372) | 2.0(0.8 to 4.2) | 98.4(93.1 to 103.6) | 98.3(92.7 to 103.5) | 9.4(7.9 to 11.1) | 61.5(24.2 to 126.9) | 5.1(4.0 to 6.2) | 5.4(4.2 to 6.4) |
| Total tooth loss | 120(106 to 135) | 3.3(2.2 to 4.7) | 103.6(101.1 to 106.0) | 103.6(101.1 to 106.0) | 3.7(3.3 to 4.1) | 101.7(68.0 to 144.4) | −2.9(−3.4 to −2.4) | −2.4(−3.0 to −1.8) |
| Other oral conditions | 51(49 to 54) | 1.5(0.9 to 2.2) | 42.4(40.3 to 44.7) | 41.7(39.5 to 44.1) | 1.8(1.7 to 1.9) | 51.2(31.9 to 75.5) | 0.0(−0.1 to 0.1) | 0.2(−0.3 to 0.7) |
| Lower-middle-income countries | ||||||||
| All oral conditions | 1,434(1,347 to 1,525) | 6.1(3.5 to 9.7) | 55.4(53.1 to 58.0) | 100.0(96.6 to 103.5) | 47.0(44.3 to 49.9) | 226.4(132.2 to 356.6) | −5.7(−6.5 to −5.0) | 4.2(3.4 to 5.0) |
| Untreated caries in deciduous teeth | 265(222 to 311) | 0.06(0.03 to 0.13) | 15.0(12.7 to 17.6) | 15.6(12.7 to 18.7) | 7.9(6.6 to 9.3) | 1.9(0.8 to 3.8) | −8.3(−10.0 to −6.5) | −7.8(−10.0 to −5.7) |
| Untreated caries in permanent teeth | 943(855 to 1,035) | 0.6(0.3 to 1.1) | 55.1(52.4 to 57.9) | 55.2(52.5 to 58.0) | 30.4(27.8 to 33.4) | 18.6(8.1 to 35.0) | −10.5(−11.5 to −9.3) | −10.2(−11.2 to −8.9) |
| Severe periodontitis | 328(279 to 380) | 2.1(0.8 to 4.3) | 117.0(114.4 to 119.4) | 117.4(114.7 to 119.8) | 12.0(10.3 to 13.9) | 77.7(30.8 to 157.5) | 7.6(6.2 to 8.9) | 8.0(6.6 to 9.2) |
| Total tooth loss | 65(57 to 74) | 1.8(1.2 to 2.5) | 130.4(128.3 to 132.5) | 130.9(128.6 to 133.2) | 2.9(2.5 to 3.2) | 77.4(51.2 to 108.6) | 6.9(5.9 to 7.8) | 7.4(6.3 to 8.4) |
| Other oral conditions | 54(51 to 56) | 1.5(1.0 to 2.3) | 77.5(76.3 to 78.7) | 77.6(76.0 to 79.2) | 1.8(1.7 to 1.9) | 50.7(31.7 to 74.5) | 0.2(0.0 to 0.3) | 0.5(−0.1 to 1.1) |
| Low-income countries | ||||||||
| All oral conditions | 296(276 to 318) | 0.9(0.5 to 1.4) | 100.9(99.1 to 102.7) | 115.8(113.5 to 117.9) | 47.4(44.7 to 50.3) | 194.0(114.3 to 305.6) | −1.4(−2.0 to −0.7) | 3.5(2.7 to 4.3) |
| Untreated caries in deciduous teeth | 75(61 to 88) | 0.02(0.01 to 0.03) | 81.1(76.9 to 84.6) | 82.1(76.5 to 87.6) | 7.5(6.1 to 8.8) | 1.7(0.7 to 3.5) | −3.4(−5.3 to −1.6) | −2.9(−5.7 to 0.1) |
| Untreated caries in permanent teeth | 198(179 to 219) | 0.1(0.1 to 0.2) | 104.7(102.2 to 107.1) | 105.8(102.9 to 108.4) | 33.4(30.6 to 36.3) | 19.4(8.4 to 36.3) | −3.1(−4.1 to −2.0) | −2.5(−3.8 to −1.3) |
| Severe periodontitis | 40(33 to 46) | 0.3(0.1 to 0.5) | 125.8(122.2 to 129.4) | 127.4(123.6 to 131.0) | 9.6(8.1 to 11.1) | 61.8(24.4 to 124.8) | 6.6(5.5 to 7.7) | 7.3(6.0 to 8.5) |
| Total tooth loss | 8(7 to 9) | 0.2(0.1 to 0.3) | 116.9(113.9 to 120.1) | 118.3(114.8 to 122.0) | 2.2(2.0 to 2.5) | 60.3(40.3 to 85.5) | 4.0(3.1 to 5.0) | 4.6(3.4 to 5.9) |
| Other oral conditions | 10(9 to 10) | 0.3(0.2 to 0.4) | 109.6(109.1 to 110.1) | 110.9(109.0 to 112.6) | 1.8(1.7 to 1.8) | 50.7(31.9 to 74.8) | 0.0(−0.1 to 0.0) | 0.6(−0.2 to 1.3) |
Number of prevalent cases and YLDs and age-standardized prevalence and YLD rates in 2017, as well as percentage change between 1990 and 2017, for untreated caries, severe periodontitis, total tooth loss, other oral conditions, and all oral conditions combined, by World Bank income groups. Values in brackets correspond to the 95% uncertainty interval.
YLDs, years lived with disability.
Between 1990 and 2017, the percentage change in the number of prevalent cases and all-ages YLDs decreased in high- and upper-middle-income countries and increased in low- and lower-middle-income countries. The age-standardized prevalence and YLD rate decreased in all World Bank groups of countries; however, it decreased the least in low-income countries (Table 3). A similar pattern emerged with the SDI as the measure of economic development: the number of prevalent cases and all-ages YLDs decreased in high, high-middle, and middle SDI countries and increased in low-middle and low SDI countries. Decreases in age-standardized prevalence and YLD rate were observed in all SDI quintiles of countries (Table 4).
Table 4.
Estimates of Burden of Oral Conditions by SDI Quintiles.
| All Ages (No. of Cases) | Percentage Change 1990 to 2017 | Age Standardized | Percentage Change 1990 to 2017 | |||||
|---|---|---|---|---|---|---|---|---|
| Prevalence (Millions) | YLDs (Millions) | Prevalence | YLDs | Prevalence (per 100) | YLD Rate (per 100,000) | Prevalence | YLD Rate | |
| Low SDI quintile | ||||||||
| All oral conditions | 597(558 to 640) | 1.9(1.1 to 3.1) | 81.4(79.0 to 83.8) | 112.8(109.9 to 115.7) | 48.7(45.9 to 51.7) | 201.5(115.0 to 324.1) | −2.8(−3.7 to −2.1) | 5.7(4.6 to 6.6) |
| Untreated caries in deciduous teeth | 137(113 to 161) | 0.03(0.01 to 0.06) | 49.0(45.2 to 52.6) | 49.8(44.6 to 54.9) | 7.8(6.4 to 9.2) | 1.8(0.8 to 3.6) | −5.4(−7.4 to −3.5) | −4.9(−8.0 to −1.9) |
| Untreated caries in permanent teeth | 399(360 to 440) | 0.2(0.01 to 0.04) | 85.6(83.1 to 87.8) | 86.3(83.4 to 89.0) | 33.2(30.3 to 36.2) | 19.3(8.4 to 36.1) | −6.2(−7.5 to −5.1) | −5.7(−7.2 to −4.5) |
| Severe periodontitis | 104(88 to 122) | 0.7(0.3 to 1.4) | 127.6(123.5 to 131.1) | 128.6(124.5 to 132.4) | 11.7(9.9 to 13.6) | 75.6(29.8 to 154.7) | 9.4(7.5 to 11.0) | 10.1(8.0 to 11.6) |
| Total tooth loss | 15(13 to 17) | 0.4(0.3 to 0.6) | 135.7(132.4 to 139.2) | 137.1(132.6 to 141.3) | 2.0(1.8 to 2.3) | 54.2(35.9 to 76.7) | 8.7(7.4 to 9.9) | 9.6(7.9 to 11.1) |
| Other oral conditions | 20(19 to 21) | 0.6(0.4 to 0.9) | 97.6(96.9 to 98.3) | 98.5(96.5 to 100.7) | 1.8(1.7 to 1.8) | 50.6(31.7 to 74.2) | 0.2(0.1 to 0.4) | 0.8(−0.1 to 1.7) |
| Low-middle SDI quintile | ||||||||
| All oral conditions | 733(688 to 780) | 3.2(1.9 to 5.1) | 55.3(53.0 to 57.9) | 100.7(97.3 to 104.7) | 44.4(41.8 to 47.2) | 228.3(134.7 to 358.0) | −6.0(−6.8 to −5.2) | 6.0(4.9 to 7.2) |
| Untreated caries in deciduous teeth | 141(118 to 166) | 0.03(0.01 to 0.07) | 16.9(14.8 to 19.2) | 16.8(13.5 to 20.3) | 7.3(6.1 to 8.6) | 1.7(0.7 to 3.5) | −11.5(−12.9 to −9.9) | −11.5(−13.9 to −8.9) |
| Untreated caries in permanent teeth | 467(421 to 517) | 0.3(0.1 to 0.5) | 54.8(52.0 to 58.0) | 54.6(51.7 to 58.0) | 28.1(25.5 to 30.8) | 16.7(7.3 to 31.6) | −10.4(−11.6 to −9.2) | −10.3(−11.5 to −8.9) |
| Severe periodontitis | 169(144 to 196) | 1.1(0.4 to 2.2) | 111.6(109.2 to 114.4) | 112.2(109.7 to 114.9) | 11.8(10.1 to 13.7) | 76.7(30.3 to 155.5) | 6.6(5.3 to 8.1) | 7.0(5.6 to 8.5) |
| Total tooth loss | 36(32 to 40) | 1.0(0.7 to 1.4) | 137.6(135.6 to 139.8) | 138.2(135.9 to 140.5) | 3.0(2.7 to 3.4) | 82.4(54.8 to 115.9) | 12.8(11.9 to 13.7) | 13.4(12.4 to 14.4) |
| Other oral conditions | 29(27 to 30) | 0.8(0.5 to 1.2) | 77.5(76.3 to 78.7) | 77.7(75.7 to 79.4) | 1.8(1.7 to 1.8) | 50.7(31.7 to 74.4) | 0.2(0.0 to 0.4) | 0.6(−0.2 to 1.4) |
| Middle SDI quintile | ||||||||
| All oral conditions | 981(926 to 1,040) | 5.3(3.2 to 8.3) | 35.7(32.7 to 39.1) | 95.6(90.3 to 101.4) | 46.4(43.7 to 49.1) | 237.2(141.3 to 369.0) | −3.8(−4.5 to −3.1) | 4.4(3.8 to 5.1) |
| Untreated caries in deciduous teeth | 140(118 to 164) | 0.04(0.02 to 0.08) | −14.4(−16.8 to −12.7) | −11.8(−14.6 to −9.4) | 8.7(7.3 to 10.1) | 2.4(1.0 to 4.7) | −5.0(−7.3 to −3.5) | −2.1(−5.0 to 0.4) |
| Untreated caries in permanent teeth | 644(587 to 706) | 0.4(0.2 to 0.8) | 33.3(29.4 to 37.5) | 35.7(31.7 to 40.2) | 29.4(26.8 to 32.3) | 20.3(8.8 to 38.0) | −7.6(−8.6 to −6.7) | −5.3(−6.7 to −3.8) |
| Severe periodontitis | 252(214 to 294) | 1.6(0.6 to 3.4) | 113.7(108.9 to 118.5) | 113.4(108.3 to 118.2) | 10.7(9.1 to 12.4) | 69.6(27.5 to 142.0) | 5.5(4.6 to 6.4) | 5.7(4.8 to 6.6) |
| Total tooth loss | 75(66 to 84) | 2.1(1.4 to 2.9) | 146.4(143.3 to 149.5) | 145.8(142.4 to 149.0) | 3.4(3.0 to 3.8) | 93.8(62.5 to 133.0) | 8.1(7.4 to 8.8) | 8.5(7.7 to 9.2) |
| Other oral conditions | 39(38 to 41) | 1.1(0.7 to 1.7) | 53.8(51.7 to 56.2) | 53.1(50.8 to 55.7) | 1.8(1.7 to 1.9) | 51.1(31.9 to 75.5) | 0.1(0.0 to 0.2) | 0.3(−0.2 to 0.8) |
| High-middle SDI quintile | ||||||||
| All oral conditions | 639(603 to 677) | 4.1(2.5 to 6.2) | 22.1(19.5 to 24.9) | 60.2(57.0 to 63.2) | 44.6(42.1 to 47.3) | 238.4(146.8 to 364.1) | −6.3(−7.2 to −5.3) | −4.7(−6.2 to −3.3) |
| Untreated caries in deciduous teeth | 75(62 to 87) | 0.02(0.01 to 0.04) | −27.0(−29.4 to −25.3) | −26.2(−29.0 to −24.3) | 8.8(7.3 to 10.2) | 2.5(1.1 to 4.9) | −5.2(−8.2 to −3.0) | −4.1(−7.5 to −1.6) |
| Untreated caries in permanent teeth | 425(389 to 464) | 0.3(0.1 to 0.6) | 18.9(15.7 to 22.4) | 16.0(12.9 to 19.6) | 28.6(26.1 to 31.3) | 20.9(9.1 to 39.9) | −10.6(−11.6 to −9.3) | −12.6(−13.8 to −11.0) |
| Severe periodontitis | 158(131 to 189) | 1.03(0.4 to 2.1) | 86.0(81.7 to 90.2) | 86.1(81.6 to 90.4) | 8.7(7.3 to 10.4) | 56.9(22.4 to 116.5) | 4.9(3.6 to 6.2) | 5.2(3.8 to 6.5) |
| Total tooth loss | 70(61 to 78) | 1.9(1.3 to 2.7) | 70.1(68.3 to 71.9) | 70.4(68.5 to 72.3) | 3.9(3.4 to 4.4) | 107.1(71.6 to 151.6) | −10.2(−10.8 to −9.7) | −9.7(−10.4 to −9.1) |
| Other oral conditions | 27(26 to 29) | 0.8(0.5 to 1.2) | 40.5(38.7 to 42.4) | 40.0(38.0 to 42.1) | 1.8(1.7 to 1.8) | 51.0(31.8 to 75.3) | −0.3(−0.4 to −0.1) | 0.0(−0.6 to 0.6) |
| High SDI quintile | ||||||||
| All oral conditions | 504(478 to 532) | 3.7(2.3 to 5.5) | 12.3(10.7 to 13.8) | 19.4(18.1 to 20.8) | 40.2(37.8 to 42.8) | 219.4(136.0 to 332.8) | −9.3(−10.3 to −8.3) | −16.2(−17.7 to −14.9) |
| Untreated caries in deciduous teeth | 37(29 to 44) | 0.01(0.01 to 0.03) | −15.0(−19.0 to −11.6) | −15.0(−19.2 to −11.3) | 6.0(4.7 to 7.2) | 2.2(1.0 to 4.5) | −7.6(−11.9 to −4.0) | −7.7(−12.2 to −3.7) |
| Untreated caries in permanent teeth | 360(331 to 391) | 0.3(0.2 to 0.7) | 8.9(6.6 to 11.2) | 7.7(5.4 to 10.0) | 28.5(26.1 to 31.3) | 27.6(12.0 to 53.6) | −10.3(−11.6 to −9.0) | −10.9(−12.2 to −9.5) |
| Severe periodontitis | 108(90 to 127) | 0.7(0.3 to 1.4) | 23.2(19.2 to 27.6) | 22.6(18.6 to 26.9) | 6.5(5.4 to 7.6) | 42.1(16.6 to 86.7) | −15.2(−17.2 to −13.1) | −15.3(−17.3 to −13.2) |
| Total tooth loss | 71(63 to 80) | 1.9(1.3 to 2.8) | 20.3(18.9 to 21.8) | 19.8(18.4 to 21.3) | 3.5(3.1 to 3.9) | 96.7(64.3 to 138.1) | −24.4(−25.5 to −23.2) | −24.3(−25.5 to −23.0) |
| Other oral conditions | 23(22 to 24) | 0.7(0.4 to 1.0) | 23.5(22.3 to 24.6) | 22.8(21.5 to 24.2) | 1.8(1.7 to 1.8) | 50.8(31.7 to 75.3) | −0.1(−0.3 to 0.0) | −0.1(−0.6 to 0.5) |
Number of prevalent cases and YLDs and age-standardized prevalence and YLD rates in 2017, as well as percentage change between 1990 and 2017, for untreated caries, severe periodontitis, total tooth loss, other oral conditions, and all oral conditions combined, by SDI quintiles. Values in brackets correspond to the 95% uncertainty interval.
SDI, Socio-demographic Index; YLDs, years lived with disability.
Untreated Caries in Permanent Teeth
The age-standardized prevalence of caries in permanent teeth was 29.4% (95% UI, 26.8% to 32.2%) in 2017, while the number of prevalent cases was 2.3 billion (95% UI, 2.1 to 2.5 billion; Table 1). Their corresponding percentage changes between 1990 and 2017 were –8.8% (95% UI, –9.5% to –7.9%) and 35.9% (95% UI, 33.5% to 38.3%; Table 2). The age-standardized YLD rate was 20.7 per 100,000 population (95% UI, 8.9 to 39.2) in 2017, while 1.6 million all-ages YLDs (95% UI, 0.7 to 3.1 million) were due to untreated caries in permanent teeth. Their corresponding percentage changes were –11.9% (95% UI, –13.4% to –10.3%) and 32.0% (95% UI, 29.3% to 34.8%) between 1990 and 2017.
In 2017, the lowest numbers of prevalent cases and all-ages YLDs were found in low- and high-income countries (198 million cases [95% UI, 179 to 219 million] and 386 million cases [95% UI, 355 to 420 million] and 0.1 million YLDs [95% UI, 0.1 to 0.2 million] and 0.4 million YLDs [95% UI, 0.2 to 0.7 million], respectively), while the highest were found in lower- and upper-middle-income countries (943 million cases [95% UI, 855 to 1,035 million] and 768 million cases [95% UI, 702 to 839 million] and 0.6 million YLDs [95% UI, 0.3 to 1.1 million] and 0.5 million YLDs [95% UI, 0.2 to 1.1 million]). The lowest age-standardized prevalence and YLD rate were found in upper-middle- and high-income countries (27.4% [95% UI, 24.9% to 30.1%] and 29.5% [95% UI, 27.1% to 32.3%] and 19.7 per 100,000 population [95% UI, 8.5 to 37.4] and 28.3 per 100,000 population [95% UI, 12.3 to 54.6]), while the highest rates were found in low- and lower-middle-income countries (33.4% [95% UI, 30.6% to 36.3%] and 30.4% [95% UI, 27.8% to 33.4%] and 19.4 per 100,000 population [95% UI, 8.4 to 36.3] and 18.6 per 100,000 population [95% UI, 8.1 to 35.0]). Between 1990 and 2017, it was found that the lower the World Bank income group, the higher the increase in the number of prevalent cases and all-ages YLDs. Although the age-standardized prevalence and YLD rate decreased in all World Bank groups of countries, it decreased the least in low-income countries (Table 3). When the SDI was used, the number of prevalent cases and all-ages YLDs was the highest in the middle SDI quintile and the lowest in the high and low SDI quintiles. The highest age-standardized prevalence and YLD rate were observed in low SDI quintiles. In addition, it was found that the higher the SDI quintile, the smaller the percentage change in number of prevalent cases and all-ages YLDs. The age-standardized prevalence and YLD rate decreased in all SDI quintiles of countries, but the smallest decrease was in the low and middle SDI quintiles (Table 4).
Severe Periodontitis
The age-standardized prevalence of severe periodontitis was 9.8% (95% UI, 8.2% to 11.4%) in 2017, while the number of prevalent cases was 796 million (95% UI, 671 to 930 million; Table 1). Their corresponding percentage changes between 1990 and 2017 were 5.8% (95% UI, 4.9% to 6.6%) and 90.1% (95% UI, 87.4% to 92.5%; Table 2). The age-standardized YLD rate was 63.5 per 100,000 population (95% UI, 25.0 to 130.3) in 2017, while 5.2 million all-ages YLDs (95% UI, 2.0 to 10.7 million) were attributed to severe periodontitis. Their corresponding percentage changes were 6.0% (95% UI, 5.2% to 6.8%) and 90.2% (95% UI, 87.4% to 92.6%) between 1990 and 2017.
In 2017, the lowest numbers of prevalent cases and all-ages YLDs were observed in low-income countries (40 million cases [95% UI, 33 to 46 million] and 0.3 million YLDs [95% UI, 0.1 to 0.5 million]) and the highest in lower-middle-income countries (328 million cases [95% UI, 279 to 380 million] and 2.1 million YLDs [95% UI, 0.8 to 4.3 million]). The lowest age-standardized prevalence and YLD rate were found in high-income countries (6.6% [95% UI, 5.5% to 7.8%] and 42.8 per 100,000 population [95% UI, 16.9 to 87.9], respectively) and the highest in lower-middle-income countries (12% [95% UI, 10.3% to 13.9%] and 77.7 per 100,000 population [95% UI, 30.8 to 157.5]). Between 1990 and 2017, a trend was seen in the percentage change in the number of prevalent cases and all-ages YLDs, with the largest increase in low-income countries. Moreover, the age-standardized prevalence and YLD rate decreased in high-income countries while they increased in upper-middle-, lower-middle-, and low-income countries (Table 3). Similar findings were found when the SDI was used as the measure of economic development (Table 4).
Total Tooth Loss
The age-standardized prevalence of tooth loss was 3.3% (95% UI, 2.9% to 3.7%) in 2017, while the number of prevalent cases was 267 million (95% UI, 235 to 300 million; Table 1). Their corresponding percentage changes between 1990 and 2017 were –10.4% (95% UI, –11.2% to –9.6%) and 75.5% (95% UI, 74.2% to 76.9%; Table 2). The age-standardized YLD rate was 91.7 per 100,000 population (95% UI, 61.3 to 129.9) in 2017, while 7.3 million all-ages YLDs (95% UI, 4.9 to 10.4 million) were attributed to total tooth loss. Their corresponding percentage changes were –10.1% (95% UI, –10.9% to –9.3%) and 75.5% (95% UI, 74.2% to 76.9%) between 1990 and 2017.
In 2017, the lowest numbers of prevalent cases and all-ages YLDs were observed in low-income countries (8 million cases [95% UI, 7 to 9 million] and 0.2 million YLDs [95% UI, 0.1 to 0.3 million]) and the highest in upper-middle-income countries (120 million cases [95% UI, 106 to 135 million] and 3.3 million YLDs [95% UI, 2.2 to 4.7 million]). The lowest age-standardized prevalence and YLD rate were found in low-income countries (2.2% [95% UI, 2.0% to 2.5%] and 60.3 per 100,000 population [95% UI, 40.3 to 85.5], respectively) and the highest in high-income countries (3.6% [95% UI, 3.1% to 4.0%] and 99.0 per 100,000 population [95% UI, 65.8 to 141.2]) and upper-middle-income countries (3.7% [95% UI, 3.3% to 4.1%] and 101.7 per 100,000 population [95% UI, 68.0 to 144.4]). Between 1990 and 2017, the percentage change in the number of prevalent cases and all-ages YLDs was the smallest in high-income countries, while all other World Bank income groups had larger percentage change. In terms of age-standardized prevalence and YLD rate, a decrease was observed in high- and upper-middle-income countries, while an increase was observed in lower-middle- and low-income countries (Table 3). Similar findings were found when the SDI was used as the measure of economic development. The percentage changes in number of prevalent cases and all-ages YLDs were the smallest in the high and high-middle SDI quintiles of countries. While increases in the age-standardized prevalence and YLD rate were seen in the 3 bottom SDI quintiles, a decrease was observed in the top 2 SDI quintiles (Table 4).
Discussion
Oral conditions remain a significant public health challenge. Unmet demand for dental services reached approximately 3.5 billion cases in 2017, and it is likely to keep increasing because small reductions in age-standardized rates are not balancing population growth. Numbers of prevalent cases and all-ages YLDs estimates (Appendix Tables 12 to 17) are relevant to identifying countries having the highest population with unmet demand for dental services. The highest normative need for dental treatment was mainly in low- and middle-income countries with large populations. Only 1 high-income country was ranked in the top 10 for all 4 conditions. India, China, Indonesia, Brazil, and United States were in the top 10 countries with the highest normative treatment need associated with all 4 dental conditions assessed in this study. Russia was in the top 10 for all conditions except caries in deciduous teeth. Pakistan and Bangladesh were also in the top 10 but not for tooth loss. Age-standardized prevalence and YLD rate offer the potential to identify countries and systems that were successful or unsuccessful in reducing the burden of oral conditions, independent of population growth.
Policy makers should seriously consider including dental care in universal health coverage (Hosseinpoor et al. 2012; Masood et al. 2015; Mathur et al. 2015). Universal coverage for dental care based on conventional treatment modalities (fillings, crowns and bridges, root canal treatment requiring sophisticated equipment) may be very costly to address the high prevalence of oral conditions, whereas palliative measures have no benefit to reduce the impact of oral conditions on the population. Minimal intervention dentistry could help tackle such a challenge. Minimal intervention dentistry is the medical philosophy for oral disease management that focuses on intercepting disease at early stages (Innes et al. 2019). This includes the atraumatic restorative technique (Frencken 2017) and silver diamine fluoride (Fung et al. 2018; Urquhart et al. 2019). These approaches reduce the cost of dental treatment dramatically, as they do not require expensive dental equipment, thus facilitating the inclusion of dental care as part of the universal health coverage agenda.
Preventing new cases of dental diseases is crucial to reduce the burden on health services. Integrated noncommunicable diseases and oral health promotion focused on tackling unhealthy behaviors have the potential to reduce dental diseases and mortality rates attributed to cardiovascular disease, cancer, and diabetes, which are indicators for assessment of Sustainable Development Goal 3.4. This approach will be more cost-effective and will avoid duplication and/or conflicting health messages (Sheiham and Watt 2000; Watt et al. 2019). Oral diseases share risk factors, such as high sugar consumption and tobacco consumption, with these 3 noncommunicable diseases. Sugar consumption is the main cause of dental caries (Moynihan and Kelly 2014; Bernabe et al. 2016), and tobacco consumption is a major cause of periodontal diseases (Nociti et al. 2015; Leite et al. 2018).
Further data analysis assessed whether there are inequalities in the distribution of the burden of oral conditions. Hobdell et al. (2003) showed a gradient in caries experience (i.e., higher in more developed countries) and a reverse gradient in periodontitis according to the Human Development Index. More recently, El Tantawi et al. (2018) reported that economic development was positively associated with caries experience, although only among children aged 36 to 71 mo. Our GBD data showed several patterns with the World Bank’s classification of economies and the SDI as indicators of economic development. To summarize, while more economically developed countries had the lowest burden of untreated caries and severe periodontitis (measured in all-ages YLDs), they also had the greatest burden of tooth loss. The burden of dental caries in permanent teeth was highest in upper- and lower-middle-income countries. The nutrition transition has affected the global distribution of the burden of obesity (Popkin et al. 2012), diabetes (Popkin 2015), and untreated caries in permanent teeth (Moynihan and Petersen 2004), as less economically developed countries still have a traditional diet low in carbohydrates and more economically developed countries have already reduced their sugar consumption. It is interesting to note that 1) a clear gradient was observed among the youngest population (deciduous teeth) and 2) the age-standardized prevalence and YLD rate for untreated caries decreased at a higher rate in high-income countries than in low-income countries from 1990 to 2017 (Table 3). Thus, it is likely that a gradient may develop and that the gap between high-income countries and the others may increase over time. The GBD data are not comparable to previous reports from other international agencies, because they used data on caries experience while we used data on untreated oral conditions.
Contrarily, the lowest age-standardized prevalence and YLD rate associated with total tooth loss were observed in the low-income countries. This may be explained by the relationship between economic development and access to dental treatment. Higher dental attendance is often reported to be associated with keeping fewer teeth, the so-called tooth death spiral (Elderton 1990; Sheiham 2002; Qvist 2015), which may be explained by the widely adopted interventionist and invasive care. It is relevant to note that the age-standardized prevalence and YLD rate for tooth loss have decreased in high- and upper-middle-income countries, while an increase was observed in the lower-middle- and low-income countries. If this trend continues, it will reverse the current social pattern for total tooth loss.
Oral health policies based on updated high-quality descriptive epidemiology may be more effective and efficient. This article reports the change in burden of disease by country and where the largest reductions in the burden of oral conditions occurred. Further research should identify the oral health strategies adopted by those countries and advocate for their potential wider use. Furthermore, the GBD study provides robust data to independently continue monitoring progress toward improving population oral health over time and across all world areas in a comparable fashion.
This study is not without limitations. One should be cautious when interpreting the data on “other oral disorders” because they were obtained from surveys in a single country (United States). Furthermore, mouth cancers, congenital malformations (including orofacial clefts), and temporomandibular disorders were not included in this report. Second, despite a major effort in partnership with WHO to identify gray literature during this iteration of the GBD study, it was observed that data were scarce, and among those identified, most did not meet the GBD eligibility criteria for inclusion.
Conclusion
Oral conditions remain a public health challenge in 2017, and social inequalities in oral conditions exist. More economically developed countries have the lowest burden of untreated caries and periodontal disease and the highest burden of tooth loss. While the burden of all oral conditions combined decreased in more economically developed countries, it increased in less economically developed countries, suggesting that the gap between groups of countries will widen.
Author Contributions
E. Bernabe, W. Marcenes, N.J. Kassebaum, contributed to conception, design, data acquisition, analysis, and interpretation, drafted and critically revised the manuscript; C.R. Hernandez, J. Bailey, S.I. Hay, S.L. James, A.H. Mokdad, M.R. Nixon, contributed to data acquisition and analysis, critically revised the manuscript; L.G. Abreu, V. Alipour, S. Amini, J. Arabloo, Z. Arefi, A. Arora, M.A. Ayanore, T.W. Bärnighausen, A. Bijani, D.Y. Cho, D.T. Chu, C.S. Crowe, G.T. Demoz, D.G. Demsie, Z.S. Dibaji Forooshani, M. Du, M. El Tantawi, F. Fischer, M.O. Folayan, N.D. Futran, Y.C.D. Geramo, A. Haj-Mirzaian, N. Hariyani, A. Hasanzadeh, S. Hassanipour, M.K. Hole, S. Hostiuc, M.D. Ilic, R. Kalhor, M. Keramati, Y.S. Khader, S. Kisa, A. Kisa, A. Koyanagi, R. Lalloo, Q. Le Nguyen, S.D. London, N.D. Manohar, B.B. Massenburg, M.R. Mathur, H.G. Meles, T. Mestrovic, A. Mohammadian-Hafshejani, R. Mohammadpourhodki, S.D. Morrison, J. Nazari, T.H. Nguyen, C.T. Nguyen, T.O. Olagunju, K. Pakshir, M. Pathak, N. Rabiee, A. Rafiei, K. Ramezanzadeh, M.J. Rios-Blancas, E.M. Roro, S. Sabour, A.M. Samy, M. Sawhney, F. Schwendicke, F. Shaahmadi, M.A. Shaikh, C. Stein, M.R. Tovani-Palone, B.X. Tran, B. Unnikrishnan, G.T. Vu, A. Vukovic, T.S.S. Warouw, Z. Zaidi, Z.J. Zhang, contributed to data acquisition, critically revised the manuscript; L. Kemmer, contributed to data analysis, critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work.
Supplemental Material
Supplemental material, DS_10.1177_0022034520908533 for Global, Regional, and National Levels and Trends in Burden of Oral Conditions from 1990 to 2017: A Systematic Analysis for the Global Burden of Disease 2017 Study by E. Bernabe, W. Marcenes, C.R. Hernandez, J. Bailey, L.G. Abreu, V. Alipour, S. Amini, J. Arabloo, Z. Arefi, A. Arora, M.A. Ayanore, T.W. Bärnighausen, A. Bijani, D.Y. Cho, D.T. Chu, C.S. Crowe, G.T. Demoz, D.G. Demsie, Z.S. Dibaji Forooshani, M. Du, M. El Tantawi, F. Fischer, M.O. Folayan, N.D. Futran, Y.C.D. Geramo, A. Haj-Mirzaian, N. Hariyani, A. Hasanzadeh, S. Hassanipour, S.I. Hay, M.K. Hole, S. Hostiuc, M.D. Ilic, S.L. James, R. Kalhor, L. Kemmer, M. Keramati, Y.S. Khader, S. Kisa, A. Kisa, A. Koyanagi, R. Lalloo, Q. Le Nguyen, S.D. London, N.D. Manohar, B.B. Massenburg, M.R. Mathur, H.G. Meles, T. Mestrovic, A. Mohammadian-Hafshejani, R. Mohammadpourhodki, A.H. Mokdad, S.D. Morrison, J. Nazari, T.H. Nguyen, C.T. Nguyen, M.R. Nixon, T.O. Olagunju, K. Pakshir, M. Pathak, N. Rabiee, A. Rafiei, K. Ramezanzadeh, M.J. Rios-Blancas, E.M. Roro, S. Sabour, A.M. Samy, M. Sawhney, F. Schwendicke, F. Shaahmadi, M.A. Shaikh, C. Stein, M.R. Tovani-Palone, B.X. Tran, B. Unnikrishnan, G.T. Vu, A. Vukovic, T.S.S. Warouw, Z. Zaidi, Z.J. Zhang and N.J. Kassebaum in Journal of Dental Research
Footnotes
A supplemental appendix to this article is available online.
A.V. is a team member of the Program for Oral Health Improvement in Children and Youth in Serbia, program 1802, project 4015, approved by the Government of Serbia, Ministry of Health. A.M.S. acknowledges support from a fellowship from the Egyptian Fulbright Mission Program. B.U. acknowledges institutional support from Kasturba Medical College and Manipal Academy of Higher Education. T.W.B. was supported by the Alexander von Humboldt Foundation through the Alexander von Humboldt Professor Award, funded by the German Federal Ministry of Education and Research. S.L.J. reports grants from Sanofi Pasteur, outside the submitted work.
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
ORCID iDs: E. Bernabe  https://orcid.org/0000-0002-1858-3713
https://orcid.org/0000-0002-1858-3713
D.T. Chu  https://orcid.org/0000-0002-4596-2022
https://orcid.org/0000-0002-4596-2022
G.T. Demoz  https://orcid.org/0000-0002-2534-821X
https://orcid.org/0000-0002-2534-821X
M. El Tantawi  https://orcid.org/0000-0003-4989-6584
https://orcid.org/0000-0003-4989-6584
M.O. Folayan  https://orcid.org/0000-0002-9008-7730
https://orcid.org/0000-0002-9008-7730
A. Kisa  https://orcid.org/0000-0001-7825-3436
https://orcid.org/0000-0001-7825-3436
R. Lalloo  https://orcid.org/0000-0001-5822-1269
https://orcid.org/0000-0001-5822-1269
H.G. Meles  https://orcid.org/0000-0001-5773-4011
https://orcid.org/0000-0001-5773-4011
R. Mohammadpourhodki  https://orcid.org/0000-0001-5677-0133
https://orcid.org/0000-0001-5677-0133
N. Rabiee  https://orcid.org/0000-0002-6945-8541
https://orcid.org/0000-0002-6945-8541
C. Stein  https://orcid.org/0000-0003-4777-1630
https://orcid.org/0000-0003-4777-1630
B. Unnikrishnan  https://orcid.org/0000-0003-0892-8551
https://orcid.org/0000-0003-0892-8551
References
- Bernabe E, Vehkalahti MM, Sheiham A, Lundqvist A, Suominen AL. 2016. The shape of the dose-response relationship between sugars and caries in adults. J Dent Res. 95(2):167–172. [DOI] [PubMed] [Google Scholar]
- Elderton RJ. 1990. Clinical studies concerning re-restoration of teeth. Adv Dent Res. 4:4–9. [DOI] [PubMed] [Google Scholar]
- El Tantawi M, Folayan MO, Mehaina M, Vukovic A, Castillo JL, Gaffar BO, Arheiam A, Al-Batayneh OB, Kemoli AM, Schroth RJ, et al. 2018. Prevalence and data availability of early childhood caries in 193 United Nations countries, 2007–2017. Am J Public Health. 108(8):1066–1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flaxman AD, Vos T, Murray CJL, Kiyono P. 2015. An integrative metaregression framework for descriptive epidemiology. Seattle (WA): University of Washington Press. [Google Scholar]
- Frencken JE. 2017. Atraumatic restorative treatment and minimal intervention dentistry. Br Dent J. 223(3):183–189. [DOI] [PubMed] [Google Scholar]
- Fung MHT, Duangthip D, Wong MCM, Lo ECM, Chu CH. 2018. Randomized clinical trial of 12% and 38% silver diamine fluoride treatment. J Dent Res. 97(2):171–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD 2015 DALYs and HALE Collaborators. 2016. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 388(10053):1603–1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD 2017 DALYs and HALE Collaborators. 2018. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 392(10159):1859–1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. 2018. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 392(10159):1789–1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD 2017 Mortality Collaborators. 2018. Global, regional, and national age-sex-specific mortality and life expectancy, 1950-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 392(10159):1684–1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobdell MH, Oliveira ER, Bautista R, Myburgh NG, Lalloo R, Narendran S, Johnson NW. 2003. Oral diseases and socio-economic status (SES). Br Dent J. 194(2):91–96. [DOI] [PubMed] [Google Scholar]
- Hosseinpoor AR, Itani L, Petersen PE. 2012. Socio-economic inequality in oral healthcare coverage: results from the World Health Survey. J Dent Res. 91(3):275–281. [DOI] [PubMed] [Google Scholar]
- Innes NPT, Chu CH, Fontana M, Lo ECM, Thomson WM, Uribe S, Heiland M, Jepsen S, Schwendicke F. 2019. A century of change towards prevention and minimal intervention in cariology. J Dent Res. 98(6):611–617. [DOI] [PubMed] [Google Scholar]
- Kassebaum NJ, Bernabe E, Dahiya M, Bhandari B, Murray CJ, Marcenes W. 2014. a. Global burden of severe periodontitis in 1990–2010: a systematic review and meta-regression. J Dent Res. 93(11):1045–1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassebaum NJ, Bernabe E, Dahiya M, Bhandari B, Murray CJ, Marcenes W. 2014. b. Global burden of severe tooth loss: a systematic review and meta-analysis. J Dent Res. 93(7):20S–28S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassebaum NJ, Bernabe E, Dahiya M, Bhandari B, Murray CJ, Marcenes W. 2015. Global burden of untreated caries: a systematic review and metaregression. J Dent Res. 94(5):650–658. [DOI] [PubMed] [Google Scholar]
- Kassebaum NJ, Smith AGC, Bernabé E, Fleming TD, Reynolds AE, Vos T, Murray CJL, Marcenes W; GBD 2015 Oral Health Collaborators. 2017. Global, regional, and national prevalence, incidence, and disability-adjusted life years for oral conditions for 195 countries, 1990–2015: a systematic analysis for the global burden of diseases, injuries, and risk factors. J Dent Res. 96(4):380–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leite FRM, Nascimento GG, Scheutz F, Lopez R. 2018. Effect of smoking on periodontitis: a systematic review and meta-regression. Am J Prev Med. 54(6):831–841. [DOI] [PubMed] [Google Scholar]
- Marcenes W, Kassebaum NJ, Bernabe E, Flaxman A, Naghavi M, Lopez A, Murray CJ. 2013. Global burden of oral conditions in 1990–2010: a systematic analysis. J Dent Res. 92(7):592–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masood M, Sheiham A, Bernabe E. 2015. Household expenditure for dental care in low and middle income countries. PLoS One. 10(4):e0123075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathur MR, Williams DM, Reddy KS, Watt RG. 2015. Universal health coverage: a unique policy opportunity for oral health. J Dent Res. 94(3):3S–5S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moynihan P, Petersen PE. 2004. Diet, nutrition and the prevention of dental diseases. Public Health Nutr. 7(1A):201–226. [DOI] [PubMed] [Google Scholar]
- Moynihan PJ, Kelly SA. 2014. Effect on caries of restricting sugars intake: systematic review to inform WHO guidelines. J Dent Res. 93(1):8–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray CJL, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, et al. 2012. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 380(9859):2197–2223. [DOI] [PubMed] [Google Scholar]
- Nociti FH, Jr, Casati MZ, Duarte PM. 2015. Current perspective of the impact of smoking on the progression and treatment of periodontitis. Periodontol 2000. 67(1):187–210. [DOI] [PubMed] [Google Scholar]
- Peres MA, Macpherson LMD, Weyant RJ, Daly B, Venturelli R, Mathur MR, Listl S, Celeste RK, Guarnizo-Herreno CC, Kearns C, et al. 2019. Oral diseases: a global public health challenge. Lancet. 394(10194):249–260. [DOI] [PubMed] [Google Scholar]
- Popkin BM. 2015. Nutrition transition and the global diabetes epidemic. Curr Diab Rep. 15(9):64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popkin BM, Adair LS, Ng SW. 2012. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 70(1):3–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qvist V. 2015. Longevity of restorations: the “death spiral.” In: Fejerskov O, Nyvad B, Kidd E, editors. Dental caries: the disease and its clinical management. London (UK): Wiley-Blackwell; p. 443–456. [Google Scholar]
- Ruger JP, Kim HJ. 2006. Global health inequalities: an international comparison. J Epidemiol Community Health. 60(11):928–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salomon JA, Haagsma JA, Davis A, de Noordhout CM, Polinder S, Havelaar AH, Cassini A, Devleesschauwer B, Kretzschmar M, Speybroeck N, et al. 2015. Disability weights for the Global Burden of Disease 2013 study. Lancet Glob Health. 3(11):e712–e723. [DOI] [PubMed] [Google Scholar]
- Salomon JA, Vos T, Hogan DR, Gagnon M, Naghavi M, Mokdad A, Begum N, Shah R, Karyana M, Kosen S, et al. 2012. Common values in assessing health outcomes from disease and injury: disability weights measurement study for the Global Burden of Disease Study 2010. Lancet. 380(9859):2129–2143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheiham A. 2002. Minimal intervention in dental care. Med Princ Pract. 11 Suppl 1:2–6. [DOI] [PubMed] [Google Scholar]
- Sheiham A, Watt RG. 2000. The common risk factor approach: a rational basis for promoting oral health. Community Dent Oral Epidemiol. 28(6):399–406. [DOI] [PubMed] [Google Scholar]
- Stevens GA, Alkema L, Black RE, Boerma JT, Collins GS, Ezzati M, Grove JT, Hogan DR, Hogan MC, Horton R, et al. ; The GATHER Working Group. 2016. Guidelines for Accurate and Transparent Health Estimates Reporting: the GATHER statement. Lancet. 388(10062):e19–e23. [DOI] [PubMed] [Google Scholar]
- Urquhart O, Tampi MP, Pilcher L, Slayton RL, Araujo MWB, Fontana M, Guzman-Armstrong S, Nascimento MM, Novy BB, Tinanoff N, et al. 2019. Nonrestorative treatments for caries: systematic review and network meta-analysis. J Dent Res. 98(1):14–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt RG, Daly B, Allison P, Macpherson LMD, Venturelli R, Listl S, Weyant RJ, Mathur MR, Guarnizo-Herreno CC, Celeste RK, et al. 2019. Ending the neglect of global oral health: time for radical action. Lancet. 394(10194):261–272. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, DS_10.1177_0022034520908533 for Global, Regional, and National Levels and Trends in Burden of Oral Conditions from 1990 to 2017: A Systematic Analysis for the Global Burden of Disease 2017 Study by E. Bernabe, W. Marcenes, C.R. Hernandez, J. Bailey, L.G. Abreu, V. Alipour, S. Amini, J. Arabloo, Z. Arefi, A. Arora, M.A. Ayanore, T.W. Bärnighausen, A. Bijani, D.Y. Cho, D.T. Chu, C.S. Crowe, G.T. Demoz, D.G. Demsie, Z.S. Dibaji Forooshani, M. Du, M. El Tantawi, F. Fischer, M.O. Folayan, N.D. Futran, Y.C.D. Geramo, A. Haj-Mirzaian, N. Hariyani, A. Hasanzadeh, S. Hassanipour, S.I. Hay, M.K. Hole, S. Hostiuc, M.D. Ilic, S.L. James, R. Kalhor, L. Kemmer, M. Keramati, Y.S. Khader, S. Kisa, A. Kisa, A. Koyanagi, R. Lalloo, Q. Le Nguyen, S.D. London, N.D. Manohar, B.B. Massenburg, M.R. Mathur, H.G. Meles, T. Mestrovic, A. Mohammadian-Hafshejani, R. Mohammadpourhodki, A.H. Mokdad, S.D. Morrison, J. Nazari, T.H. Nguyen, C.T. Nguyen, M.R. Nixon, T.O. Olagunju, K. Pakshir, M. Pathak, N. Rabiee, A. Rafiei, K. Ramezanzadeh, M.J. Rios-Blancas, E.M. Roro, S. Sabour, A.M. Samy, M. Sawhney, F. Schwendicke, F. Shaahmadi, M.A. Shaikh, C. Stein, M.R. Tovani-Palone, B.X. Tran, B. Unnikrishnan, G.T. Vu, A. Vukovic, T.S.S. Warouw, Z. Zaidi, Z.J. Zhang and N.J. Kassebaum in Journal of Dental Research