Abstract
Background
Ultrasound is used in the treatment of a wide variety of musculoskeletal disorders, which include acute ankle sprains. This is an update of a Cochrane review first published in 1999, and previously updated in 2004.
Objectives
To evaluate the effects of ultrasound therapy in the treatment of acute ankle sprains.
Search methods
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (September 2010), the Cochrane Central Register of Controlled Trials (The Cochrane Library 2010, Issue 3), MEDLINE (1966 to September 2010), EMBASE (1983 to September 2010), CINAHL (1982 to 2004), and PEDro ‐ the Physiotherapy Evidence Database (accessed 01/06/09). We also searched the Cochrane Rehabilitation and Related Therapies Field database, reference lists of articles, and contacted colleagues.The WHO International Clinical Trials Registry Platform was searched for ongoing trials.
Selection criteria
Randomised or quasi‐randomised trials were included if the following conditions were met: at least one study group was treated with therapeutic ultrasound; participants had acute lateral ankle sprains; and outcome measures included general improvement, pain, swelling, functional disability, or range of motion.
Data collection and analysis
Two authors independently performed study selection, and assessed the risk of bias and extracted data. Risk ratios and risk differences together with 95% confidence intervals were calculated for dichotomous outcomes and mean differences together with 95% confidence intervals for continuous outcome measures. Limited pooling of data was undertaken where there was clinical homogeneity in terms of participants, treatments, outcomes, and follow‐up time points.
Main results
Six trials were included, involving 606 participants. Five trials included comparisons of ultrasound therapy with sham ultrasound; and three trials included single comparisons of ultrasound with three other treatments. The assessment of risk of bias was hampered by poor reporting of trial methods and results. None of the five placebo‐controlled trials (sham ultrasound) demonstrated statistically significant differences between true and sham ultrasound therapy for any outcome measure at one to four weeks of follow‐up. The pooled risk ratio for general improvement at one week was 1.04 (random‐effects model, 95% confidence interval 0.92 to 1.17) for active versus sham ultrasound. The differences between intervention groups were generally small, between zero and six per cent, for most dichotomous outcomes.
Authors' conclusions
The evidence from the five small placebo‐controlled trials included in this review does not support the use of ultrasound in the treatment of acute ankle sprains. The potential treatment effects of ultrasound appear to be generally small and of probably of limited clinical importance, especially in the context of the usually short‐term recovery period for these injuries. However, the available evidence is insufficient to rule out the possibility that there is an optimal dosage schedule for ultrasound therapy that may be of benefit.
Plain language summary
Therapeutic ultrasound for acute ankle sprains
Ultrasound, or the use of high frequency sound pulses, is used for treating acute ankle sprains. It is thought that the increase in temperature caused by ultrasound helps soft tissue healing. The review aimed to look at the evidence from studies testing the use of ultrasound in clinical practice. Six trials were included in the review. Poor reporting of trial methods made it difficult to assess the risk of bias of the included studies. The six trials involved a total of 606 participants with acute ankle sprains of relatively short duration. Five trials compared ultrasound therapy with sham ultrasound (machine turned off). Three of the six trials included single comparisons of ultrasound with three other treatments. The main results were from the review of the five placebo‐controlled trials (sham ultrasound). These found that ultrasound therapy does not seem to enhance recovery or help to reduce pain and swelling after an ankle sprain, or improve the ability to stand on the affected foot and ankle. Most ankle sprains heal quickly. While ultrasound may still improve recovery in a small way, this potential benefit is probably too small to be important.
Background
Description of the condition
Acute soft tissue injuries of the ankle, involving simple stretching, partial rupture or complete rupture of at least one ligament, are the most common sports injury. These injuries result in high costs to society as a result of work absence and health care resource use. There are uncertainties regarding the optimal treatment of acute ankle injuries, and ankle sprains may be associated with long‐term complaints of pain, functional disability and absence from work (Makuloluwe 1977; Williamson 1986). In contrast to acute ankle sprains, patients with chronic instability show symptoms of pain swelling, recurrent sprains and instability for longer than six months (Karlsson 1996). Despite their importance, there is still debate regarding the management of acute ankle sprains. Standard treatment usually comprises of rest, ice, compression and leg elevation (RICE therapy), but additional treatment is often considered to be necessary (Oakland 1993; Williamson 1986).
Description of the intervention
Ultrasound has been used in the treatment of musculoskeletal conditions for many years. Ultrasound equipment consists of a generator and transducer. The generator produces electromagnetic energy with a frequency of 0.5 to 3.5 MHz, which is converted by the transducer to mechanical energy with a similar frequency and intensity of up to 3 watts/cm² (Ebenbichler 1994). Based on these experimental findings, ultrasound has been used in physical therapy to relieve pain, reduce swelling, and improve joint immobility in a wide variety of musculoskeletal disorders including ankle sprains. Ultrasound is mainly applied by physiotherapists in outpatient clinics or in primary care physiotherapy practices.
How the intervention might work
Laboratory research has demonstrated that the application of ultrasound results in the promotion of cellular metabolic rate and increased visco‐elastic properties of collagen (Maxwell 1992). In animal studies, an exposure to 1 MHz ultrasound at 50 joules/cm² is reported to be sufficient to increase tissue temperature (Hykes 1985). This rise in temperature is assumed to be the mediating mechanism for tissue repair, the enhancement of soft tissue extensibility, promotion of muscle relaxation, augmentation of blood flow, and alleviation of inflammatory reactions of soft‐tissue (Falconer 1990; Hayes 1992; Kitchen 1990; Maxwell 1992; Van der Heijden 1991).
Why it is important to do this review
This systematic review was originally published in 1999 and updated in 2004 (Van der Windt 2002), with the latest searches being performed more than six years ago. In 2004 we concluded that the extent and quality of the available evidence for the effects of therapeutic ultrasound for acute ankle sprains was limited.The magnitude of effects compared to placebo was small and of little clinical importance. An update was needed to see if new evidence has emerged to support (or refute) the use of therapeutic ultrasound therapy for ankle sprains.
Objectives
We aimed to determine whether ultrasound therapy is more effective than reference treatments (placebo intervention, no treatment, or other types of interventions) in people with acute ankle sprains with respect to the following outcomes: general recovery, improvement of pain relief, swelling, functional disability, and range of motion.
Methods
Criteria for considering studies for this review
Types of studies
Randomised and quasi‐randomised (method of allocating participants to a treatment which is not strictly random e.g. by date of birth, hospital record number, alternation) controlled clinical studies evaluating therapeutic ultrasound for acute ankle sprains were considered. While only results from full trial reports were included, other trials reported only in abstract or incompletely were sought for reference purposes. There were no language restrictions.
Types of participants
Trials that included people with pain, swelling and/or functional disability caused by acute ankle ligament injuries were considered.
Types of interventions
Trials with at least one group treated with active ultrasound therapy were considered. Comparisons with placebo interventions were allowed as well as comparisons with no treatment or other types of interventions such as exercise therapy, immobilisation, laser therapy, or medication. Trials in which all intervention groups received ultrasound as a co‐intervention were excluded as well as studies comparing phonophoresis with ultrasound (as this does not provide a contrast to ultrasound).
Types of outcome measures
Trials using at least one of the following six types of outcome measures were considered for inclusion:
Primary outcomes
General improvement (patient perceived benefit, proportion/percentage of participants recovered, etc).
Adverse events (although highly unlikely, data on any adverse event following treatment with therapeutic ultrasound were sought).
Secondary outcomes
Improvement of pain (visual analogue scale, ordinal scale, pain questionnaire).
Swelling.
Functional disability (ability to walk, sick leave, re‐uptake of sports, multiple item questionnaire to report activity limitations).
Range of motion.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (September 2010), the Cochrane Central Register of Controlled Trials (The Cochrane Library 2010, Issue 3), MEDLINE (1966 to September 2010), EMBASE (1983 to Septmber 2010), CINAHL (1982 to July 2004), and PEDro ‐ the Physiotherapy Evidence Database (accessed 01/06/09). We also searched the Cochrane Rehabilitation and Related Therapies Field database using the search term 'ultrasound' (June 2009). In MEDLINE (OVID Web) the search strategy was combined with the Cochrane Highly Sensitive Search Strategy for identifying randomised trials (sensitivity‐maximizing version) (Lefebvre 2009) (seeAppendix 1). This search was modified for use in other databases (seeAppendix 1). The WHO International Clinical Trials Registry Platform was searched for ongoing trials. No language restrictions were applied.
Searching other resources
The reference lists of all retrieved articles were screened, and we contacted colleagues to identify additional relevant publications. No further attempts were made to collect unpublished data.
Data collection and analysis
Selection of studies
Two authors independently applied the selection criteria to the publications identified by the search strategy described above. During consensus meetings, remaining disagreements were discussed and a third author was consulted in cases of remaining disagreement.
Data extraction and management
For each publication, two authors independently extracted all necessary details using standardised forms. Details were recorded for:
eligibility criteria;
interventions;
outcome measures;
length of follow‐up;
adverse reactions;
sample size;
statistical analysis (intention‐to‐treat);
data presentation.
Results data were collected for the primary and secondary outcome measures (general improvement, adverse effects, improvement of pain, range of motion, swelling, and functional disability).
Assessment of risk of bias in included studies
All publications included in the review were blinded for authors, affiliation, source, and results. Subsequently, the risk of bias was independently assessed by two authors based on 10 domains, as follows.
Random sequence generation
Allocation concealment
Incomplete outcome data
Baseline similarity across intervention groups
Blinding of care provider
Control for co‐interventions
Adherence to treatment
Blinding of patients
Blinding of outcome assessment
Timing of outcome assessment
The items in this list are the same as those assessed in the Amsterdam‐Maastricht Consensus List for Quality Assessment, which was used in the previous versions of the review (Van der Windt 2002). In addition to the domains listed in The Cochrane Collaboration's 'Risk of bias' tool, four other aspects were assessed: similarity in baseline characteristics, control for co‐interventions, adherence to treatment, and timing of outcome assessment. Detailed guidelines for the assessment of each risk of bias were made available to the authors.
For each item, both authors checked whether incomplete information hampered assessment of the risk of bias. Where there was insufficient information, the item was scored as 'unclear' (?). If sufficient information was provided the item was scored as either 'yes' ('+' for low risk of bias) or 'no' ('‐' for inadequate methods, high risk of bias). Assessment would have been based on all available information for those trials with more than one report if this had occurred. Disagreements were dealt with as stated above.
Measures of treatment effect
Risk ratios and risk differences, together with 95% confidence intervals, were calculated for dichotomous outcomes; and mean differences, together with 95% confidence intervals, were calculated for continuous outcome measures. Where possible, for continuous outcome measures (e.g. visual analogue scales for pain severity), we planned to use results for differences in improvement between groups (change scores) in preference to differences between post‐treatment values. Whenever possible, general improvement and other dichotomous outcomes were calculated according to intention‐to‐treat, using the number of participants following randomisation in the denominator. If there was considerable loss to follow‐up, we also calculated these measures based on a complete case analysis (if sufficient data were presented).
Assessment of heterogeneity
We assessed heterogeneity by visual inspection of the forest plot (analysis) along with consideration of the chi² test for heterogeneity and the I² statistic.
Data synthesis
Statistical pooling of results was undertaken for subsets of studies that showed statistical homogeneity and sufficient clinical homogeneity with respect to participants, interventions, outcomes, and follow‐up time points using a random‐effects model (DerSimonian 1986; Fleiss 1993). Whenever possible, success rates and other outcomes were calculated according to the intention‐to‐treat principle. Risk ratios and risk differences together with 95% confidence intervals were calculated for dichotomous outcomes. There was no pooling of continuous outcome data. In the protocol, we stipulated that mean differences or, where different scales had been used, standardised mean differences together with 95% confidence intervals would be calculated for continuous outcome measures.
Subgroup analysis and investigation of heterogeneity
In the case of statistical heterogeneity (P < 0.10), and after consideration of the value of I² statistic, we planned to explore potential sources of heterogeneity including type of control treatment and application of co‐interventions, and the following risks of bias (lack of blinding, inadequate randomisation procedure, and high drop‐out rate). No subgroup or sensitivity analyses were performed.
Results
Description of studies
Results of the search
The search (in September 2010) yielded nine potentially relevant trials on ultrasound therapy for acute ankle sprains. Five trials were identified in MEDLINE (Makuloluwe 1977; Nyanzi 1999; Pellow 2001; Van Lelieveld 1979; Williamson 1986). Reference checking and searches in other databases resulted in the identification of four additional trials (Bradnock 1995; Middlemast 1978; Oakland 1993; Zammit 2005).
The two authors selecting trials for inclusion initially agreed on the status of six out of the nine trials on ankle sprains. After a consensus meeting, agreement was reached for the three remaining trials. As a result, six trials that met all the selection criteria were included in the review and the other three were excluded. Of the three excluded studies, Pellow 2001 used detuned (sham) ultrasound as a placebo intervention in comparison with manual therapy, Bradnock 1995 only evaluated (biomechanical) aspects of gait pattern after one treatment with ultrasound and thus did not meet our inclusion criterion regarding types of outcome measures, and Middlemast 1978 included a variety of soft‐tissue injuries but did not report separate results for ankle sprains. Finally, two studies were classified as awaiting assessment because only abstracts are available and full trial reports have not yet been found (Chen 1990;Feng 1993).
Included studies
Four trials conducted in the UK were published in English (Makuloluwe 1977; Nyanzi 1999; Oakland 1993; Williamson 1986), one conducted in Denmark was published in Danish (Van Lelieveld 1979), and the last trial conducted in Malta was published in English (Zammit 2005). These six trials involved 606 participants.
All studies involved participants with acute ankle sprains of relatively short duration. Five of the six studies compared ultrasound therapy with sham ultrasound (machine turned off) (Nyanzi 1999; Oakland 1993; Van Lelieveld 1979; Williamson 1986; Zammit 2005). Zammit 2005 also included a no treatment control group. In three studies, ultrasound therapy was compared with other treatment modalities: immobilisation by an elastic adhesive bandage (Elastoplast) (Makuloluwe 1977), Felbinac gel, a topically applied non‐steroidal anti‐inflammatory drug (Oakland 1993) and electrotherapy (Van Lelieveld 1979).
Makuloluwe 1977 compared the effectiveness of ultrasound therapy (4 to 10 treatments) with immobilisation with Elastoplast in 80 participants with mild to moderate ankle sprains. In some cases, an ice pack was applied before the first ultrasound treatment to reduce swelling. Recovery (yes/no) was assessed after one to two weeks.
Nyanzi 1999 included 58 participants with inversion injuries of the ankle (time since injury less than 100 hours). Ultrasound therapy (three sessions on three consecutive days) was compared with sham ultrasound (treatment head electronically disabled). Outcome was assessed at days one, two, three and 14. Outcome measures were: pain (10 cm visual analogue scale); swelling (ankle joint circumference); range of motion during dorsiflexion and plantar flexion (degrees); ability to bear weight (% body weight).
Oakland 1993 included 220 participants with acute injuries to the lateral ankle ligament (time since injury less than 48 hours). Ultrasound therapy (four treatments during one week) in combination with felbinac gel was compared with sham ultrasound in combination with Felbinac gel and with ultrasound therapy in combination with placebo gel. Outcome was assessed at three, five, and seven days after randomisation. Participants scored pain on movement on a 100 mm visual analogue scale. Investigators assessed swelling, pain, and general severity on a five point ordinal scale and the ability to bear weight on a four point ordinal scale. Success rates were calculated as the proportion of people showing a moderate or marked improvement.
Van Lelieveld 1979 compared ultrasound therapy (10 treatments during two weeks) with sham ultrasound and with electrotherapy. Sixty participants with acute ankle sprains (time since injury: zero to four days) were included in the study. Outcomes were assessed daily for 15 days after randomisation. Main outcome measures were: swelling (ankle joint circumference); range of motion (three point ordinal scale); pain (six point ordinal scale); and the ability to walk 20 metres without limping (yes/no).
Williamson 1986 randomised 154 participants with acute inversion injuries of the lateral ligament of the ankle joint (time since injury less than 48 hours) to treatment with either true or sham ultrasound. The length of follow‐up was three to four weeks. Outcome was assessed using a combined clinical score (0 to 15 points) consisting of five factors (each scored on a three point scale): subjective assessment of swelling; participant discomfort; degree of limp; pain on inversion; and pain on plantar flexion. Success rates were computed as the number of "cured" participants who scored either zero or one point.
Zammit 2005 randomised 34 participants with acute inversion injuries of the lateral ligament of the ankle joint (time since injury more than 24 hours and less than 96 hours) to treatment with either true, sham or no ultrasound. Outcomes were assessed at 8, 15 and 22 days after randomisation. Outcomes were assessed using a pain visual analogue scale (VAS), swelling (figure‐of eight method using a tape measure), range of motion (ROM) during dorsiflexion and plantarflexion (universal 360° goniometer), and postural stability (balance error scoring system).
All available details on study populations, interventions, drop‐out rates, outcomes, and adverse reactions are presented in the Characteristics of included studies.
Risk of bias in included studies
The results of the risk of bias assessment of the individual trials are presented in Figure 1, and summarised in Figure 2. Insufficient information was provided to assess several important risks of bias (seeFigure 1 and Figure 2 for items scored '?' or unclear). This impeded a good evaluation of the study design and mainly applied to methods used for the concealment of treatment allocation, similarity of intervention groups at baseline, and adherence to the intervention. Procedures used for the generation of a random sequence, blinding of participants, and timing of follow‐up assessment were assessed as low risk of bias in at least four out of the six publications. Three studies were considered at high risk of bias (score '‐') related to lack of blinding of the care provider (Makuloluwe 1977; Van Lelieveld 1979; Zammit 2005), patients (Makuloluwe 1977), or outcome assessment (Makuloluwe 1977; Zammit 2005). Oakland 1993 was considered at high risk of bias due to incomplete reporting of outcome data. As well as a lack of information on trial methodology, trial reports often included insufficient details on the interventions (dosage and frequency of the treatment was often unclear), and outcomes. In particular, continuous outcomes, including point estimates and measures of dispersion, were often inadequately reported and results were often presented graphically in terms of percentages without the denominators.
1.
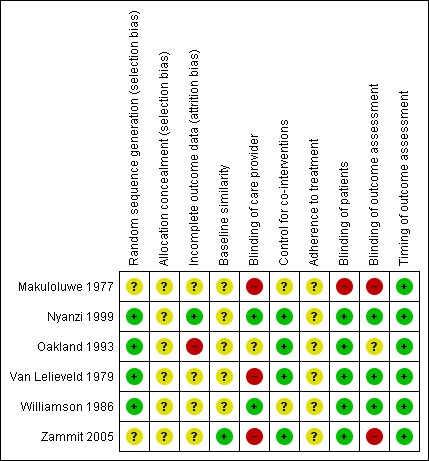
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
2.
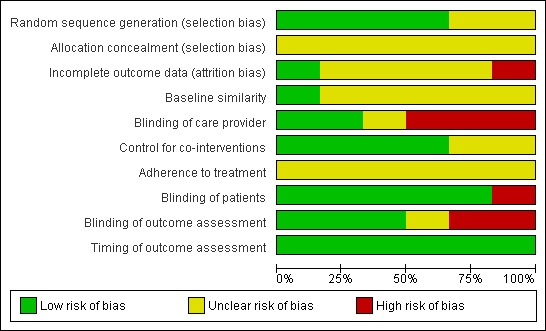
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Effects of interventions
Data were extracted on all relevant outcome measures: general improvement, pain, swelling, functional disability, range of motion and adverse reactions. The outcomes recorded in the individual trials are listed in the Outcomes sections of the Characteristics of included studies.
Two types of comparisons are presented below: comparisons between true and sham ultrasound, and comparisons between ultrasound therapy and other treatment modalities. No results are presented for the 12 participants of the 'no treatment' group of Zammit 2005.
Ultrasound therapy versus sham ultrasound
None of the five trials (Nyanzi 1999; Oakland 1993; Van Lelieveld 1979; Williamson 1986;Zammit 2005) comparing ultrasound with sham ultrasound demonstrated statistically significant differences between two treatment groups for any outcome measure. The studies varied with respect to the type of ultrasound (pulsed or continuous). Sufficient information on other treatment parameters (frequency or intensity) was only provided in Oakland 1993, Nyanzi 1999 and Zammit 2005. The four trials comparing active versus sham ultrasound treatment (Nyanzi 1999; Van Lelieveld 1979; Williamson 1986;Zammit 2005) with follow‐up periods of at least two weeks showed that the majority of participants had fully recovered at final follow‐up.
General improvement
For three studies, results of dichotomous measures of general improvement were available at seven days after randomisation. These were reported as 'moderate or marked improvement' in Oakland 1993, 'pain‐free status' in Van Lelieveld 1979, and 'cured' as indicated by a combined clinical score of zero or one point in Williamson 1986. Using an intention‐to‐treat approach, the differences in success rates ranged between 0% and 20% with the success rate in the control group ranging between 55% and 85%. The three studies were relatively homogenous in terms of study populations and follow‐up time points. Using the random‐effects model, the pooled risk ratio (RR) for general improvement was 1.04 (95% confidence interval (CI) 0.92 to 1.17; seeAnalysis 1.1). The pooled risk difference (RD) in general improvement was 3.0% (95% CI ‐6% to 12%).
1.1. Analysis.
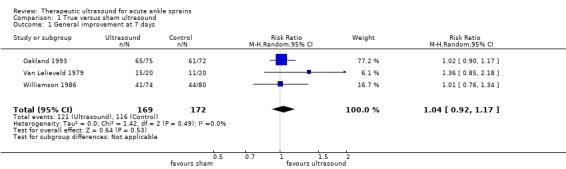
Comparison 1 True versus sham ultrasound, Outcome 1 General improvement at 7 days.
Pain
Data for continuous or ordinal outcome measures of pain were incomplete. Oakland 1993 did not demonstrate significant differences between groups in participants with a moderate or marked response of pain at seven days (seeAnalysis 1.2: 67/75 versus 57/72, RR 1.13, 95% CI 0.98 to 1.30; RD 10%, 95% CI ‐2% to 22%). Nyanzi 1999 found no significant differences between the two groups at 14 days follow‐up in pain scores on a visual analogue scale (mean difference (MD): 0.20 cm, 95% CI ‐0.57 to 0.97 cm; seeAnalysis 1.3). Zammit 2005 observed no significant differences between treatment groups in mean reduction in pain at 22 days follow‐up (VAS results: active 3.9 cm versus sham 4.0 cm) (SDs not presented).
1.2. Analysis.
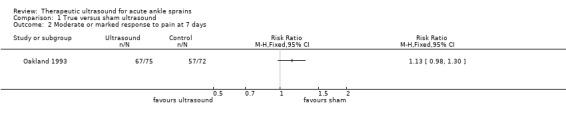
Comparison 1 True versus sham ultrasound, Outcome 2 Moderate or marked response to pain at 7 days.
1.3. Analysis.
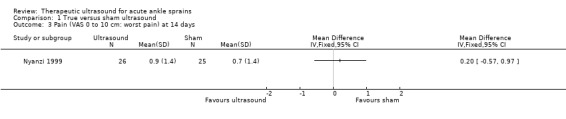
Comparison 1 True versus sham ultrasound, Outcome 3 Pain (VAS 0 to 10 cm: worst pain) at 14 days.
Swelling
Data from the three trials reporting on swelling could not be pooled. None of the trials found statistically significant differences between true and sham ultrasound. Nyanzi 1999 found minimal difference between the two groups in ankle circumference at 14 days (seeAnalysis 1.4: 51.3 cm versus 51.6 cm; mean difference ‐0.30 cm, 95% CI ‐1.59 to 0.99 cm). In Van Lelieveld 1979, more participants treated with ultrasound had less than 0.5 cm difference in ankle circumference after seven days (seeAnalysis 1.5: 13/20 versus 8/20, RR 1.63, 95% 0.87 to 3.04; RD 25%, 95% CI ‐5% to 55%). Zammit 2005 found no significant differences between the treatment groups in the mean reduction of swelling at 22 days (active 1.0 cm versus sham 1.3 cm).
1.4. Analysis.
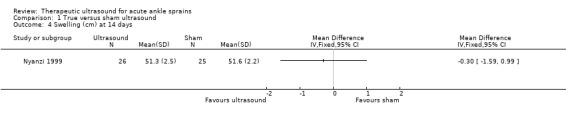
Comparison 1 True versus sham ultrasound, Outcome 4 Swelling (cm) at 14 days.
1.5. Analysis.
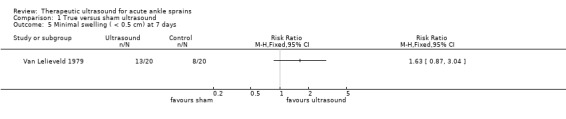
Comparison 1 True versus sham ultrasound, Outcome 5 Minimal swelling ( < 0.5 cm) at 7 days.
Functional disability
Two studies (Oakland 1993; Van Lelieveld 1979) presented dichotomous data on the ability to walk or bear weight at seven days. The differences between intervention groups were small (5% to 6%) and not statistically significant. The pooled risk ratio was 1.09 (95% CI 0.92 to 1.30; seeAnalysis 1.6). The pooled risk difference for functional disability was 6% (95% CI ‐6% to 19%). Nyanzi 1999 reported only a small difference between true and sham ultrasound for the ability to bear weight at 14 days (seeAnalysis 1.7 % body weight bourne by the affected leg: 44.7% versus 45.1%, MD ‐0.40%, 95% ‐3.21% to 2.41%). Zammit 2005 reported no significant differences between the treatment groups in postural stability, as measured by reductions at follow‐up of a median of four errors for the active group and 7.5 errors for the placebo ultrasound group.
1.6. Analysis.
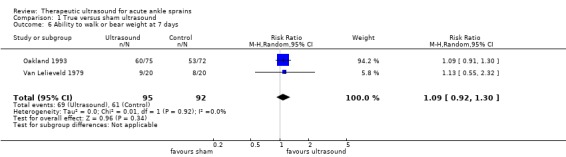
Comparison 1 True versus sham ultrasound, Outcome 6 Ability to walk or bear weight at 7 days.
1.7. Analysis.
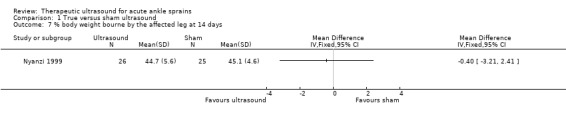
Comparison 1 True versus sham ultrasound, Outcome 7 % body weight bourne by the affected leg at 14 days.
Range of motion
Van Lelieveld 1979 reported incomplete range of motion data, and Oakland 1993 reported that problems with measurement had precluded presenting results for this outcome. Nyanzi 1999 reported small but statistically non‐significant differences in range of motion (degrees) between true and sham ultrasound at 14 days follow‐up: dorsiflexion (MD ‐1.80 degrees, 95% CI ‐7.49 to 3.89 degrees) and plantar flexion (MD 4.60 degrees, 95% CI ‐1.67 to 10.87 degrees) (seeAnalysis 1.8). Zammit 2005 observed no significant differences between the treatment groups in plantar and dorsal flexion: mean increases in plantarflexion were 4.7 degrees in the ultrasound group and 4.6 degrees in the sham ultrasound group; mean increases in dorsiflexion were 10.0 degrees in the ultrasound group and 5.2 degrees in the sham ultrasound group.
1.8. Analysis.
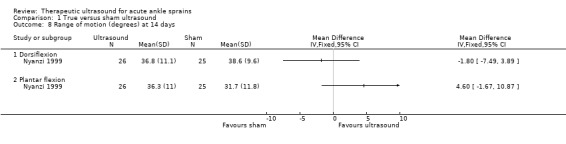
Comparison 1 True versus sham ultrasound, Outcome 8 Range of motion (degrees) at 14 days.
Adverse reactions
Adverse reactions were only reported by Oakland 1993. Eight out of 73 participants allocated to ultrasound therapy (plus placebo gel) reported 11 non‐serious adverse reactions including gastrointestinal events and skin reactions. In one person, treatment was discontinued due to skin reactions and the person withdrew from the trial.
Comparisons between ultrasound therapy and other treatment modalities
One study reported superior effects of ultrasound therapy compared with immobilisation with Elastoplast (Makuloluwe 1977). However, there were data discrepancies and the values of percentages (success) probably indicated some undeclared loss to follow‐up from the 40 participants in each group. Makuloluwe 1977 reported that 46.2% in the ultrasound group versus 26.6% in the Elastoplast group had recovered at seven days, and 86.4% versus 58.6% at 14 days. Based on rounded up data, estimated risk difference results for the two time periods are 19% after one week (95% CI ‐2% to 40%) and 27% after two weeks (95% CI 8% to 46%).
In Oakland 1993, the comparison between ultrasound therapy and Felbinac gel resulted in small and non‐significant differences between the two groups at seven days in moderate or marked improvement generally (RR 0.99, 95% CI 0.86 to 1.14; RD ‐1% 95 CI ‐13% to 11%), in pain (RR 1.06, 95% CI 0.90 to 1.23; RD 4% 95 CI ‐8% to 17%) and ability to weight bear (RR 1.04, 95% CI 0.86 to 1.26; RD 3%, 95% CI ‐11% to 17%) (seeAnalysis 2.1).
2.1. Analysis.
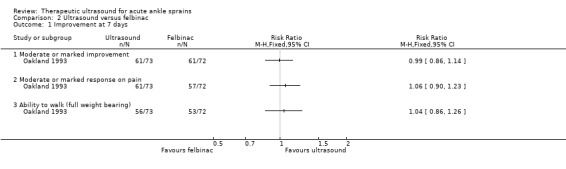
Comparison 2 Ultrasound versus felbinac, Outcome 1 Improvement at 7 days.
In Van Lelieveld 1979, while ultrasound therapy appeared less beneficial than electrotherapy at seven days, there were no statistically significant differences between the two groups in recovery (pain‐free status) (RR 0.83, 95% CI 0.62 to 1.12; RD ‐15%, 95% CI ‐38% to 8%); minimal swelling (less than 0.5 cm) (RR 0.76, 95% CI 0.53 to 1.11; RD ‐20%, 95% CI ‐46% to 6%) or ability to walk (RR 0.64, 95% CI 0.37 to 1.13; RD ‐25%, 95% CI ‐55% to 5%) (seeAnalysis 3.1).
3.1. Analysis.
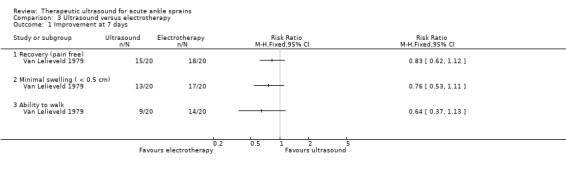
Comparison 3 Ultrasound versus electrotherapy, Outcome 1 Improvement at 7 days.
Discussion
Summary of main results
The results of this review show that there is little evidence for beneficial effects of ultrasound therapy for acute ankle sprains. Six trials met the selection criteria. Five placebo‐controlled trials could not detect statistically significant or clinically important differences between true and sham ultrasound for any outcome measure: general improvement, pain, swelling, functional disability or range of motion. The number of studies included in this review was relatively small and only one was of good methodological quality. Due to differences in the definition of outcome measures statistical pooling of results was only sensible for some comparisons and for which data from only two or three studies could be used. These pooled estimates also resulted in small and non‐significant differences between true and sham ultrasound.
One study did detect large and significant differences in favour of ultrasound therapy when compared with immobilisation using Elastoplast (Makuloluwe 1977). However, this study was considered to be of relatively poor validity and at high risk of bias from lack of blinding. Another pragmatic study comparing ultrasound with electrotherapy reported better results for electrotherapy with respect to improvements of swelling, pain, and ability to walk (Van Lelieveld 1979). None of the trials included a follow‐up period longer than one month. Ultrasound therapy is assumed to be most effective in the first phase of treatment (Roebroeck 1998) and long‐term effects may not be expected. Indeed as already stated, the four trials with follow‐up periods of two to four weeks showed that the large majority of participants had fully recovered by that time and any differences between intervention groups were negligible.
Overall completeness and applicability of evidence
Our searches identified only a small number of trials reporting on the effectiveness of therapeutic ultrasound for ankle sprains, and no ongoing trials were found in the WHO database. We excluded two potentially relevant trials that were only published as abstracts. One of these trials was carried out in professional athletes and coaches in China (Chen 1990) and this population may not be representative of the patient population treated by most physical therapists. The other trial (Feng 1993), also carried out in China, included patients with either acute wrist or ankle injuries, with data for ankle injuries not being presented separately. Although the evidence base is small we feel that the trials included in our systematic review represent patient populations encountered in (European) physiotherapy practice.
Quality of the evidence
We prefer to base conclusions regarding the effectiveness of ultrasound therapy on studies with low risk of bias. The Amsterdam‐Maastricht Consensus list is one of the many scales and checklists that have been designed to assess the quality of randomised trials (Moher 1996). We added several items from this checklist to The Cochrane Collaboration's 'Risk of bias' tool, as we considered these to be of specific importance in this area of research including control for co‐interventions and adherence to treatment. However, very few trials provided information on these aspects of design and conduct. Some sources of bias, particularly those concerning co‐interventions and prognostic similarity, were originally associated with frequent disagreement among our authors and have now been revised by providing more explicit instructions for assigning positive or negative scores.
Insufficient reporting of trial methods often hampered the assessment of risk of bias in this review. Journal style or editorial decisions may partly be the reason for the lack of information on important items. A more complete and informative trial report could reveal additional flaws in design or conduct. For example, for none of the trials in this review could we confirm adequate procedures for treatment allocation and adherence to treatment. Insufficient information frequently concerned not only aspects of trial validity but also diagnostic criteria, details concerning the study populations (athletes or sedentary people), treatment parameters including information on testing and calibration of ultrasound machines, and outcome measures. In this area of research the introduction of guidelines for the reporting of trials (CONSORT statement), does not seem to have led to much improvement in the quality of reporting, which can prevent difficulties during quality assessment and ensure adequate data presentation and analysis (Altman 1996; Moher 2001; Moher 2010).
In the six studies included in the review, outcome measures were not uniform and the definitions of general improvement, pain, swelling, and functional disability varied across studies. Some of these measures have probably been designed on the basis of face validity and may have proved useful in clinical practice. Important characteristics of the outcome measures such as reproducibility, validity, responsiveness, or applicability were not described. A thorough assessment of the quality of outcome measures used in the six studies was not feasible within the scope of this review.
Lack of blinding was most often considered to be a source of bias, especially in trials without placebo control, or in trials in which the therapist was aware he or she was providing sham ultrasound. Sham ultrasound can be a good placebo (Van der Heijden 1991), but only if the therapist is adequately blinded. Lack of blinding may therefore have resulted in inflated effect sizes in some of the trials. In two trials (Oakland 1993; Williamson 1986) there was at least 20% lost to follow‐up by the end of the study; this is relatively high in trials with a follow‐up period of only one to four weeks.
Potential biases in the review process
Our review may not be entirely free from publication bias as we included only published trial reports. Retrieving unpublished data requires a huge effort that was not within the scope of this review. Publication bias may be prevented if investigators report the results of all studies undertaken and if journal editors base their decisions to publish on aspects of quality only and not on the strength and direction of results. However, considering the fact that it is usually small studies with negative results that are less likely to be published (Dickersin 1990), we do not think that the inclusion of unpublished data would have strongly influenced the results of our review on the effectiveness of ultrasound therapy for ankle sprains. However, it must be noted that the two Chinese trials awaiting classification as they were published as abstracts only (Chen 1990; Feng 1993) reported positive results for therapeutic ultrasound. Neither trial included a placebo control and for both trials the randomisation procedure was not described at all, making it unclear if these trials used a random procedure to allocate participants to therapeutic ultrasound or the alternative treatment (infrared therapy, Chinese medicine or low dose electrotherapy). Based on the abstracts these trials appear to have a high risk of bias.
In this review we included trial reports published in any language. Unfortunately, we were unable to use the same authors for quality assessment of the studies published in English and Danish. The Danish paper (Van Lelieveld 1979) was assessed by another author, which may have resulted in a different interpretation of validity criteria. The findings of the Danish study were not systematically different from those published in English.
In our opinion it is important to consider not only the statistical significance of trial results but also the magnitude of treatment effect. Pooling of many small placebo‐controlled studies or conducting very large trials will eventually produce statistically significant results but if the size of the treatment effect is small the costs of treatment may easily outweigh the benefits. Deciding on the magnitude of a clinically important difference is difficult and certainly arbitrary as it depends on several factors including the natural history, prevalence and severity of the condition, the reference treatment, potential adverse reactions and inconvenience of therapy, treatment preferences, and costs (including costs of personnel, equipment and time spent on therapy) (Cook 1992). Although the definition of a clinically important difference depends on the condition, research in patients with musculoskeletal disorders has shown that differences between study groups may be considered to be clinically important if they exceed 20% (Goldsmith 1993). This is a considerable difference that may not be easy to achieve. Given the favourable recovery rates in ankle sprains with most patients showing a full recovery within four weeks, fairly large effect sizes may be needed to have sufficient clinical impact.
Agreements and disagreements with other studies or reviews
In 1995, Gam & Johannsen published a systematic review of 22 randomised clinical trials on the effectiveness of ultrasound therapy for musculoskeletal conditions (Gam 1995), which included two studies on ankle sprains (Van Lelieveld 1979; Williamson 1986). While they did not present separate analyses for different musculoskeletal conditions, the general conclusion of their review was that there was little evidence for the effectiveness of ultrasound therapy, from well‐designed trials.
Authors' conclusions
Implications for practice.
There are still only a few trials evaluating the effectiveness of ultrasound therapy for acute ankle sprains. The evidence from the five placebo‐controlled trials included in this review does not support the wide use of ultrasound in the treatment of acute ankle sprains. The potential treatment effects of ultrasound appear to be generally small and probably of limited clinical importance, especially in the context of the usually short‐term recovery period for these injuries. Due to the limited amount of information on treatment parameters, no conclusions can be made regarding an optimal and adequate dosage schedule for ultrasound therapy or whether such a schedule would improve on the reported effectiveness of ultrasound for ankle sprains.
Implications for research.
Although the quality of methods of most available studies on ultrasound therapy for ankle sprains may be considered to be modest, the findings of the placebo‐controlled studies consistently indicated small and non‐significant treatment effects of ultrasound therapy. Therefore, future research should preferably be directed towards the evaluation of other interventions for ankle sprains, such as exercise therapy, or to interventions for the prevention of future or recurrent ankle sprains in those who are at a relatively high risk of ankle ligament injuries (e.g. taping, external ankle support devices, or health education interventions) (Handoll 2002).
What's new
| Date | Event | Description |
|---|---|---|
| 5 May 2011 | New search has been performed | In this update, the search was updated to September 2010 and one additional trial (Zammit 2005) was included. The overall conclusions of the review remained unchanged. The recommended new format for Cochrane reviews was adopted. Risk of bias assessment replaced the original scoring system, which had included a total score for methodological quality. |
| 5 May 2011 | New citation required but conclusions have not changed | There has been a change in authorship. |
History
Protocol first published: Issue 1, 1999 Review first published: Issue 4, 1999
| Date | Event | Description |
|---|---|---|
| 12 September 2008 | Amended | Converted to new review format. |
| 15 November 2004 | New search has been performed | For the second update (Issue 1, 2005), the search was updated and no additional randomised clinical trials met the selection criteria. The conclusions of the review remained unchanged. The text was modified to conform with the Cochrane Style Guide. The title was changed from "Ultrasound therapy for acute ankle sprains" to "Therapeutic ultrasound for acute ankle sprains" to reflect current usage of 'therapeutic ultrasound' for therapy and 'diagnostic ultrasound' for diagnostics. |
| 1 November 2001 | New search has been performed | In the first substantive update (Issue 1, 2002), one additional randomised clinical trial was included (Nyanzi 1999). The conclusions of the review remained unchanged. |
Acknowledgements
The authors gratefully acknowledge the help of Wim Grooten in evaluating the study published in Danish and the help of Vicky Peng in translating the Chinese abstracts. We are grateful to Helen Handoll for her help with editing both the protocol and several versions of the review. For the later updates we are grateful to Lesley Gillespie, Lindsey Elstub, and Joanne Elliott for updating the searches, and to Janet Wale for copy‐editing as part of the Wiley copy‐editing support project. We would also like to thank the following for useful editorial comments of both the protocol and review: Prof William Gillespie, Dr Helen Handoll, A/Prof Peter Herbison, Ms Denise Jones, Prof Rajan Madhok, Prof Gordon Murray, Dr Sally Rudicel, Prof Marc Swiontkowski, and Mr Stephen Wrigley.
We acknowledge the contributions of Suzanne van den Berg and Andrea de Winter to earlier versions of this review.
Appendices
Appendix 1. Search strategies
The Cochrane Library (Wiley)
#1 MeSH descriptor Ankle Injuries, this term only #2 MeSH descriptor Sprains and Strains, this term only #3 (sprain* or strain* or injur*):ti,ab #4 (#2 OR #3) #5 ankle*:ti,ab #6 (#4 AND #5) #7 (#1 OR #6) #8 MeSH descriptor Ultrasonics, this term only #9 (ultrasound or ultrasonic*):ti,ab #10 (#8 OR #9) #11 (#7 AND #10) in Cochrane Central Register of Controlled Trials
MEDLINE (OVID Web)
1. Ankle Injuries/ 2. Ankle/ or Ankle Joint/ or Lateral Ligament, Ankle/ 3. or/1‐2 4. "Sprains and strains"/ 5. ankle$1.tw. 6. and/4‐5 7. or/3,6 8. Ultrasonics/ 9. (ultrasound or ultrasonic$1).tw. 10. or/8‐9 11. and/7,10 12. Randomized controlled trial.pt. 13. Controlled clinical trial.pt. 14. randomized.ab. 15. placebo.ab. 16. Drug therapy.fs. 17. randomly.ab. 18. trial.ab. 19. groups.ab. 20. or/12‐19 21. exp Animals/ not Humans/ 22. 20 not 21 23. and/11,22
EMBASE (OVID Web)
1. Ankle/ Or Ankle Sprain/ Or Ankle Injury/ Or Ankle Lateral Ligament/ 2. Ultrasound Therapy/ 3. (ultrasound or ultrasonic$1).tw. 4. or/2‐3 5. and/1,4 6. exp Randomized Controlled trial/ 7. exp Double Blind Procedure/ 8. exp Single Blind Procedure/ 9. exp Crossover Procedure/ 10. Controlled Study/ 11. or/6‐10 12. ((clinical or controlled or comparative or placebo or prospective$ or randomi#ed) adj3 (trial or study)).tw. 13. (random$ adj7 (allocat$ or allot$ or assign$ or basis$ or divid$ or order$)).tw. 14. ((singl$ or doubl$ or trebl$ or tripl$) adj7 (blind$ or mask$)).tw. 15. (cross?over$ or (cross adj1 over$)).tw. 16. ((allocat$ or allot$ or assign$ or divid$) adj3 (condition$ or experiment$ or intervention$ or treatment$ or therap$ or control$ or group$)).tw. 17. or/12‐16 18. or/11,17 19. limit 18 to human 20. and/5,19
CINAHL (OVID Web)
1. Ankle Injuries/ 2. Lateral Ligament, Ankle/ 3. Ankle/ or Ankle Joint/ 4. or/1‐3 5. "Sprains and Strains"/ 6. ankle$1.tw. 7. and/5‐6 8. or/4,7 9. Ultrasonic Therapy/ 10. (ultrasound or ultrasonic$1).tw. 11. or/9‐10 12. and/8,11 13. exp Clinical Trials/ 14. exp Evaluation Research/ 15. exp Comparative Studies/ 16. exp Crossover Design/ 17. clinical trial.pt. 18. or/13‐17 19. ((clinical or controlled or comparative or placebo or prospective or randomi#ed) adj3 (trial or study)).tw. 20. (random$ adj7 (allocat$ or allot$ or assign$ or basis$ or divid$ or order$)).tw. 21. ((singl$ or doubl$ or trebl$ or tripl$) adj7 (blind$ or mask$)).tw. 22. (cross?over$ or (cross adj1 over$)).tw. 23. ((allocat$ or allot$ or assign$ or divid$) adj3 (condition$ or experiment$ or intervention$ or treatment$ or therap$ or control$ or group$)).tw. 24. or/19‐23 25. or/18,24 26. and/12,25
Data and analyses
Comparison 1. True versus sham ultrasound.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 General improvement at 7 days | 3 | 341 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.92, 1.17] |
| 2 Moderate or marked response to pain at 7 days | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Pain (VAS 0 to 10 cm: worst pain) at 14 days | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Swelling (cm) at 14 days | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Minimal swelling ( < 0.5 cm) at 7 days | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6 Ability to walk or bear weight at 7 days | 2 | 187 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.92, 1.30] |
| 7 % body weight bourne by the affected leg at 14 days | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8 Range of motion (degrees) at 14 days | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.1 Dorsiflexion | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Plantar flexion | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 2. Ultrasound versus felbinac.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Improvement at 7 days | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Moderate or marked improvement | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Moderate or marked response on pain | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Ability to walk (full weight bearing) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 3. Ultrasound versus electrotherapy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Improvement at 7 days | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Recovery (pain free) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Minimal swelling ( < 0.5 cm) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Ability to walk | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Makuloluwe 1977.
| Methods | Randomised clinical trial (no details of method). No blinding of patients, care providers and outcome assessment. | |
| Participants | Enfield, UK. 80 patients with ankle sprains. Inclusion criteria: mild or moderate ankle sprains, pain on abduction or adduction of the foot. Exclusion criteria (X‐ray): ankle fractures. | |
| Interventions | Group 1: Ultrasound therapy: 1.5 W/cm², 4 minutes, 4 to 10 sessions (n = 40). Length of treatment variable, depending on recovery. Group 2: Immobilisation by Elastoplast (n = 40). Co‐interventions: ice packs for some patients in the ultrasound group. | |
| Outcomes | Length of follow‐up: 2 weeks Success rate / recovery (yes/no) Dropouts: none reported but values of percentages indicate incomplete outcome ascertainment. Adverse reactions: not described |
|
| Notes | Authors' conclusion: ultrasound is more effective than immobilisation with Elastoplast. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described in trial report |
| Allocation concealment (selection bias) | Unclear risk | Not described in trial report |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Values of percentages (success) indicate incomplete outcome ascertainment |
| Baseline similarity | Unclear risk | No baseline characteristics per intervention group |
| Blinding of care provider | High risk | Pragmatic comparison of two different types of treatment |
| Control for co‐interventions | Unclear risk | No information in trial report |
| Adherence to treatment | Unclear risk | No information in trial report |
| Blinding of patients | High risk | Pragmatic comparison of two different types of treatment |
| Blinding of outcome assessment | High risk | Assessment by patient and physician |
| Timing of outcome assessment | Low risk | Similar timing |
Nyanzi 1999.
| Methods | Randomised clinical trial (use of computer generated randomisation scheme). Blinding of patients, care provider, and outcome assessor. | |
| Participants | Southampton, UK. 58 patients with ankle ligament sprains. Inclusion criteria: inversion injury of the joint, time since injury < 100 hours, able to follow instructions, age 14 to 65 years. Exclusion criteria: previous similar injury within 1 year, multiple injuries, diabetic, extensive varicose veins, bony injuries. 59% male, 41% female, mean age 50 years. | |
| Interventions | Group 1: pulsed ultrasound mark space ratio 1:4, 3 MHz, 0.25 W/cm², 2 minutes, 3 treatments over 3 consecutive days (n = 29). Group 2: Sham ultrasound (n = 29) Co‐interventions: elevate leg while resting, bear weight when active; Tubigrip support, paracetamol for those in need of analgesics. | |
| Outcomes | Length of follow‐up: 14 days. ‐ Pain (10 cm VAS, mean and SD) ‐ Swelling (ankle joint circumference in cm, mean and SD) ‐ ROM dorsiflexion (degrees, mean and SD) ‐ ROM plantar flexion (degrees, mean and SD) ‐ Ability to bear weight (% bodyweight, mean and SD) Dropouts: n = 7 (12%) (group 1: 3 =10%) and group 2: 4 =14%). All reported full recovery, and had no time to attend further assessments. Adverse reactions: not described. | |
| Notes | Authors' conclusion: at the dose and duration used, ultrasound is no better than placebo in the management of acute ligament injuries. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation code |
| Allocation concealment (selection bias) | Unclear risk | No information in trial report |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Seven drop outs and the data analysed included only those who completed the study. |
| Baseline similarity | Unclear risk | No complete information on prognostic factors or baseline values of outcome measures |
| Blinding of care provider | Low risk | Sham ultrasound |
| Control for co‐interventions | Low risk | Similar advice to all participants |
| Adherence to treatment | Unclear risk | No information in trial report |
| Blinding of patients | Low risk | Sham ultrasound |
| Blinding of outcome assessment | Low risk | Outcome assessment by patient or blinded observer |
| Timing of outcome assessment | Low risk | Similar timing |
Oakland 1993.
| Methods | Randomised clinical trial (use of computer generated randomisation scheme). Blinding of patients. Blinding of care providers and outcome assessment unclear. | |
| Participants | Multicentre trial, UK. 220 participants with acute ankle injuries. Inclusion criteria: injury of the lateral ankle ligament of at least mild severity, time since injury < 48 hours. Exclusion criteria: fractures, internal derangement of the joint, hypersensitivity for felbinac, abraded skin, asthma, metabolic joint diseases or rheumatic conditions, systematic connective tissue disorders, severe renal, hepatic, cardiovascular or dermatological disease, patients requiring analgesics or other NSAID, pregnant or lactating women, participants in other trials. 65% men, 35% women, mean age 28 years. | |
| Interventions | Group 1: pulsed ultrasound: 3 MHz, 0.25 to 0.5 W/cm², 2 to 3 minutes, 4 treatments over 7 days, in combination with felbinac gel: 2‐3 applications every day (n = 75). Group 2: sham ultrasound in combination with felbinac gel (n = 72). Group 3: ultrasound in combination with placebo gel (n = 73). Co‐interventions: none. | |
| Outcomes | Length of follow‐up: 1 week
‐ Pain on movement or at rest (yes/no)
‐ Moderate or marked response of pain (investigator) (yes/no)
‐ Able to bear full weight (yes/no)
‐ Moderate or marked improvement of general severity (yes/no) Dropouts: 52 (group 1: 15 = 20%, group 2: 18 = 25%, group 3: 19 = 26%) Adverse reactions (yes/no) |
|
| Notes | Authors' conclusions: there were few significant differences between the intervention groups. The effectiveness of felbinac is similar to that of ultrasound therapy. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Unclear risk | No description in trial report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss to final follow‐up: 81/220 at 7 days (37%) |
| Baseline similarity | Unclear risk | No complete information on prognostic factors or baseline values of outcome measures |
| Blinding of care provider | Unclear risk | Unable to judge from trial report |
| Control for co‐interventions | Low risk | No other interventions allowed |
| Adherence to treatment | Unclear risk | No information in trial report |
| Blinding of patients | Low risk | Sham ultrasound |
| Blinding of outcome assessment | Unclear risk | Unable to judge from trial report |
| Timing of outcome assessment | Low risk | Similar timing |
Van Lelieveld 1979.
| Methods | Randomised clinical trial (computer generated random numbers). Blinding of patients and outcome assessment. No blinding of care provider. | |
| Participants | Haslev, Denmark. All patients with acute ankle distortions referred to the X‐ray department (n = 60). Inclusion criteria: time since injury 0‐4 days, first distortion ever. 42% men, 58% women, mean age 23 to 29 years | |
| Interventions | Group 1: continuous ultrasound: 0.5 W/cm², 5 to 10 minutes, 5x/week, 2 weeks (n = 20?). Group 2: electrotherapy: diadynamic current, pulse duration 10 msec, 50/100 Hz, 4‐8 minutes (n = 20?). Group 3: sham ultrasound (n = 20?). Co‐interventions: elastic bandages, crutches, leg elevation, plantar flexion exercises. | |
| Outcomes | Length of follow‐up: 15 days.
At baseline, and daily until maximum of 15 days:
‐ % patients with swelling < 0.5 cm at 7 days
‐ % patients able to walk at 7 days
‐ % patients pain free at 7 days ‐ swelling (joint circumference in cm), means, no SD ‐ range of motion (1 = 20°, 2 = 40°, 3 = > 40° restriction), means, no SD ‐ pain (6‐point scale), means, no SD Dropouts: 3 (2 did not complete treatment; 1 incorrect diagnosis), distribution was not reported Adverse reactions: not described |
|
| Notes | Authors' conclusions: ultrasound therapy has no significant effect on the course of recovery. The assumption in the analyses of allocation of 20 patients to each group seems to be supported in the graphical representations. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random plan devised before the trial |
| Allocation concealment (selection bias) | Unclear risk | No description in trial report |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Acceptable drop‐out rate but the distribution was not reported. |
| Baseline similarity | Unclear risk | No complete information on prognostic factors or baseline values of outcome measures |
| Blinding of care provider | High risk | Physician not blinded |
| Control for co‐interventions | Low risk | Similar advice to all participants |
| Adherence to treatment | Unclear risk | No information in trial report |
| Blinding of patients | Low risk | Sham ultrasound |
| Blinding of outcome assessment | Low risk | Outcome assessment by blinded observers |
| Timing of outcome assessment | Low risk | Similar timing |
Williamson 1986.
| Methods | Randomised clinical trial (use of random numbers). Blinding of care provider, patients and outcome assessment. | |
| Participants | Manchester, UK. All patients with ankle sprains attending the emergency department (n = 154). Inclusion criteria: time since injury < 48 hours, objective injury lateral ankle ligament; age 12 to 65 years. Exclusion criteria (X‐ray): fractures, complete rupture with > 6 mm opening of the ankle mortice laterally or > 6 mm anterior displacement of the talus. | |
| Interventions | Length of treatment: until recovery (clinical score 0 or 1 point) Group 1: ultrasound on alternate days (74). (Treatment parameters not described.) Group 2: sham ultrasound (80). Co‐interventions: ice packs, exercises, Tubigrip support, crutches if needed. | |
| Outcomes | Length of follow‐up: 4 weeks Follow‐up at baseline, at 1 week and 4 weeks: General improvement (scoring system based on clinical score, swelling, patient's discomfort, limp, pain on inversion, and pain on plantar flexion), results presented as percentages in graphs Dropouts: n = 44 (29%) (23 = 31% in the ultrasound group and 21 = 26% in the sham group) after three weeks. Adverse reactions: not described. | |
| Notes | Authors' conclusions: ultrasound treatment does not hasten recovery after lateral ankle sprains. Data extrapolated from graphs. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers |
| Allocation concealment (selection bias) | Unclear risk | No description in trial report |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No numbers presented with outcome data |
| Baseline similarity | Unclear risk | No baseline information on prognostic factors |
| Blinding of care provider | Low risk | Sham ultrasound |
| Control for co‐interventions | Unclear risk | No information in trial report |
| Adherence to treatment | Unclear risk | No information in trial report |
| Blinding of patients | Low risk | Sham ultrasound |
| Blinding of outcome assessment | Low risk | Assessment by blinded observers |
| Timing of outcome assessment | Low risk | Similar timing |
Zammit 2005.
| Methods | Randomised clinical trial (method?). Blinding patients and no blinding of treatment provider and outcome assessor. | |
| Participants | Pietà, Malta All patients with ankle sprains attending the emergency department who met the inclusion and exclusion criteria (n = 34). 14 males,15 females, 5 lost to follow‐up, mean age 32 years,17 grade I injury and 12 grade II injury Inclusion criteria: grade 1 & 2 inversion injuries of the ankle joint, duration since injury: between 24 and 96 hours, age between 20 and 50 years, first distortion ever Exclusion criteria: fractures, complete ruptures (grade III), previous similar injury, multiple injuries, participants in other trials, low back pain with sciatic symptoms, signs of degeneration in lumbar spine, hips and knees, neurological impairment, diabetes, tumours or tissue in precancerous states, infected areas, uncontrollable haemophilia, severely ischaemic tissues, recent venous thrombosis, areas of atherosclerosis, areas that have received radiotherapy in the last 6 months, metal bone‐fixing pins subcutaneously placed, plastics used in replacement surgery, anaesthetic areas |
|
| Interventions | Group 1: active ultrasound on alternate days for 2 weeks, ice packs, tubigrip and exercises (n = 12)
Group 2: sham ultrasound on alternate days for 2 weeks, ice packs, tubigrip and exercises (n = 10)
Group 3: ice packs, tubigrip and exercises (n = 12) Active ultrasound: Treatment sessions were on alternate days for 2 weeks (six sessions); treatment intensity of 0.25 W cm² at a mark space ratio of 1:4 at 3 MHz was used for the first 3 treatments with duration of 10 min. A treatment intensity of 0.50 W cm² at a mark space ratio of 1:2 at 3 MHz was used for the last 3 treatments with duration of 6 min. |
|
| Outcomes | Length of follow‐up: 22 days At baseline and after 8, 15 and 22 days: ‐ Pain on activity (VAS) scores ‐ Swelling (figure‐of eight method using a tape measure) ‐ Range of motion during dorsiflexion and plantar flexion (universal 360° goniometer) ‐ Postural stability (balance error scoring system) Dropouts: 5 (3 after eight days and 2 after 15 days) (group 1: 2 =17%, group 2: 0, group 3: 3 = 25%) Adverse reactions: not described. |
|
| Notes | Authors' conclusions: ultrasound treatment does not increase the effectiveness of management of acute lateral ankle ligament sprains. The authors did not provide sufficient data to perform a meta‐analysis (no measures of dispersion, such as SD, provided). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description in trial report |
| Allocation concealment (selection bias) | Unclear risk | No description in trial report |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The analysis of drop‐outs was not described |
| Baseline similarity | Low risk | Data presented and groups are comparable |
| Blinding of care provider | High risk | No blinding of therapist |
| Control for co‐interventions | Low risk | Similar advice to all participants |
| Adherence to treatment | Unclear risk | No information in trial report |
| Blinding of patients | Low risk | Sham ultrasound |
| Blinding of outcome assessment | High risk | Trial described as single‐blind (patient blinded) |
| Timing of outcome assessment | Low risk | Similar timing |
ROM: range of motion SD: standard deviation VAS: visual analogue scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bradnock 1995 | Comparison of continuous ultrasound (45 kHz, 0.95 W), high frequency pulsed ultrasound (3 MHz, 2 W), and sham ultrasound in 47 patients with acute ankle sprains (1 treatment only). Reason for exclusion: Outcome measures are related to gait pattern: stride length, swing phase, cadence ratio, walking speed. These outcome measures were not considered to be relevant for this review (aimed at pain, swelling, functional disability, general improvement). |
| Middlemast 1978 | Comparison of pulsed ultrasound (1.5 MHz, 0.5 to 1 W/cm²), and thermotherapy (wax baths, infra‐red, or short‐wave diathermy) in 71 patients with soft tissue injuries. Study population consisted of patients with a variety of soft tissue injuries. Results for ankle sprains (n = 20, 28%) were not presented separately. |
| Pellow 2001 | Comparison of manual therapy (ankle mortice separation adjustment), and 5 minutes of detuned ultrasound (8 sessions in 4 weeks) in 30 patients. Study population consists of subacute and chronic grade I or II ankle inversion sprains and not of acute ankle sprains. |
Characteristics of studies awaiting assessment [ordered by study ID]
Chen 1990.
| Methods | Randomisation and follow‐up period are unclear |
| Participants | Professional athletes and coaches people with acute ankle injuries (grade I and II) (n = 103), age range from 12 to 48 years |
| Interventions | 1. ultrasound & infrared therapy (n = 40) 2. ultrasound only (n = 35) 3. infrared & Chinese medicine (n = 28) |
| Outcomes | 1. 10/40 cured (no pain); 24/40 better; 6 no change/ worse 2. 3/35 cured; 20/35 better; 12 no change/ worse 3. 1/28 cured; 19/28 better; 8/28 no change/ worse |
| Notes | This study is not included because it is only reported as an abstract. A full trial report has not been identified. Abstract was assessed with help from a Chinese native speaker. |
Feng 1993.
| Methods | Randomisation and follow‐up period are unclear |
| Participants | The population included people with acute ankle (n = 306) or wrist (n = 154) injuries, age ranged from 18 to 46 years |
| Interventions | 1. ultrasound & medium frequency electrotherapy (n = 230) 2. low frequency electrotherapy (n = 230) |
| Outcomes | Results are presented for overall improvement, based on reduction of pain, swelling, and extravasion: good, moderate, slight, or no improvement 1. 119/230 good; 28/230 moderate; 11/230 slight, 1/230 no improvement 2. 86/230 good; 57/230 moderate; 75/230 slight; 12/230 no improvement |
| Notes | Study is not included yet because it is only reported as an abstract. A full trial report has not been identified. There is no separate presentation of results for the 306 participants with ankle injuries. Abstract was assessed with help from a Chinese native speaker. |
Differences between protocol and review
Several changes have been made since the protocol and in comparison with previous versions of this review. The outcome measures have been categorized into primary and secondary outcome measures; the former quality assessment tool was replaced with The Cochrane Collaboration's 'Risk of bias' tool and the use of total quality scores has been abandoned.
Contributions of authors
The update of this review was initiated by MPJ van den Bekerom and DAWM van der Windt. DAWM van der Windt conceived, designed and co‐ordinated the review, developed the search strategy and carried out the searches, screened search results and obtained papers, screened retrieved papers against inclusion criteria, carried out quality assessment and data abstraction, entered data into RevMan, carried out statistical analyses, and wrote previous versions of the review. MPJ van den Bekerom performed these tasks for the update of this review. GJMG van der Heijden conceived and designed the review, developed the search strategy, contributed to the appraisal of quality and data abstraction, commented on statistical analyses and on drafts of the review. G ter Riet contributed to the appraisal of quality and data abstraction, and commented on statistical analyses and on drafts of the protocol. LM Bouter conceived and supervised the review, and commented on drafts of the review. MPJ van den Bekerom performed the update of the review with help from DAWM van der Windt and G ter Riet.
Sources of support
Internal sources
VU University Medical Center, Amsterdam, Netherlands.
External sources
Fund for Investigative Medicine, Health Insurance Council, Netherlands.
Declarations of interest
None known.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Makuloluwe 1977 {published data only}
- Makuloluwe RT, Mouzas GL. Ultrasound in the treatment of sprained ankles. Practitioner 1977;218(1306):586‐8. [MEDLINE: ] [PubMed] [Google Scholar]
Nyanzi 1999 {published data only}
- Nyanzi CS, Langridge J, Heyworth JRC, Mani R. Randomized controlled study of ultrasound therapy in the management of acute ligament sprains of the ankle joint. Clinical Rehabilitation 1999;13(1):16‐22. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Oakland 1993 {published data only}
- Oakland C, Rapier C. A comparison of the efficacy of the topical NSAID felbinac and ultrasound in the treatment of acute ankle injuries. British Journal of Clinical Research 1993;4:89‐96. [EMBASE: 1994103542] [Google Scholar]
Van Lelieveld 1979 {published data only}
- Lelieveld DW. The value of ultrasonic and electric stimulation in the treatment of sprained ankles. Report of a controlled investigation [Vaerdien af ultralyd og el‐stimulation ved behandling af distorsioner. En kontrolleret undersogelse]. Ugeskrift for Laeger 1979;141:1077‐80. [MEDLINE: ] [PubMed] [Google Scholar]
Williamson 1986 {published data only}
- Williamson JB, George TK, Simpson DC, Hannah B, Bradbury E. Ultrasound in the treatment of ankle sprains. Injury 1986;17(3):176‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Zammit 2005 {published data only}
- Zammit E, Herrington L. Ultrasound therapy in the management of acute lateral ligament sprains of the ankle joint. Physical Therapy in Sport 2005;6(3):116‐21. [EMBASE: 2005372108] [Google Scholar]
References to studies excluded from this review
Bradnock 1995 {published data only}
- Bradnock B, Law HT. Assessment of different ultrasonic devices in the treatment of acute ankle sprains using gaitway, gait analysis [abstract]. Journal of Bone and Joint Surgery ‐ British Volume 1994;76(Suppl 2 & 3):142. [Google Scholar]
- Bradnock B, Law HT, Roscoe K. A quantitative comparative assessment of the immediate response to high frequency ultrasound and low frequency ultrasound ('longwave therapy') in the treatment of acute ankle sprains. Physiotherapy 1996;82(2):78‐84. [EMBASE: 1996060737] [Google Scholar]
Middlemast 1978 {published data only}
- Middlemast S, Chatterjee DS. Comparison of ultrasound and thermotherapy for soft‐tissue injuries. Physiotherapy 1978;64(11):331‐2. [MEDLINE: ] [PubMed] [Google Scholar]
Pellow 2001 {published data only}
- Pellow JE, Brantingham JW. The efficacy of adjusting the ankle in the treatment of subacute and chronic grade I and grade II ankle inversion sprains. Journal of Manipulative & Physiological Therapeutics 2001;24(1):17‐24. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Chen 1990 {published data only}
- Chen SF. [Ultrasound therapy for sprained ankle]. Chinese Journal of Physical Therapy 1990;13(3):182. [Google Scholar]
Feng 1993 {published data only}
- Feng WX, Quan DH. [Ultrasound and medium frequency current therapy for acute sprained ankle]. Chinese Journal of Physical Therapy 1993;16(1):1952. [Google Scholar]
Additional references
Altman 1996
- Altman DG. Better reporting of randomised controlled trials: the CONSORT statement. BMJ 1996;313(7057):570‐1. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cook 1992
- Cook DJ, Guyatt GH, Laupacis A, Sackett DL. Rules of evidence and clinical recommendations on the use of antithrombotic agents. Chest 1992;102(4 Suppl):305S‐11S. [MEDLINE: ] [PubMed] [Google Scholar]
DerSimonian 1986
- DerSimonian R, Laird N. Meta‐analysis in clinical trials. Controlled Clinical Trials 1986;7(3):177‐88. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Dickersin 1990
- Dickersin K. The existence of publication bias and risk factors for its occurrence. JAMA 1990;263(10):1385‐9. [MEDLINE: ] [PubMed] [Google Scholar]
Ebenbichler 1994
- Ebenbichler G, Resch KL. Critical evaluation of ultrasound therapy [Kritische Uberprufung des therapeutischen Ultraschalls]. Wiener Medizinische Wochenschrift 1994;144(3):51‐3. [PubMed] [Google Scholar]
Falconer 1990
- Falconer J, Hayes KW, Chang RW. Therapeutic ultrasound in the treatment of musculoskeletal conditions. Arthritis Care & Research 1990;3(2):85‐91. [MEDLINE: ] [PubMed] [Google Scholar]
Fleiss 1993
- Fleiss JL. The statistical basis of meta‐analysis. Statistical Methods in Medical Research 1993;2(2):121‐45. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Gam 1995
- Gam AN, Johannsen F. Ultrasound therapy in musculoskeletal disorders: a meta‐analysis. Pain 1995;63(1):85‐91. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Goldsmith 1993
- Goldsmith CH, Boers M, Bombardier C, Tugwell P. Criteria for clinically important changes in outcomes: development, scoring and evaluation of rheumatoid arthritis patient and trial profiles. OMERACT Committee. Journal of Rheumatology 1993;20(3):561‐5. [MEDLINE: ] [PubMed] [Google Scholar]
Handoll 2002
- Handoll HHG, Rowe BH, Quinn KM, Bie R. Interventions for preventing ankle ligament injuries. Cochrane Database of Systematic Reviews 2002, Issue 1. [DOI: 10.1002/14651858.CD001250] [DOI] [PubMed] [Google Scholar]
Hayes 1992
- Hayes KW. The use of ultrasound therapy to decrease pain and improve mobility. Critical Reviews in Physical & Rehabilitation Medicine 1992;3:271‐87. [Google Scholar]
Hykes 1985
- Hykes DL, Hendrick WR, Starchman DE. Biological effects. Ultrasound Physics and Instrumentation. New York: Churchill Livingstone, 1985:133‐47. [Google Scholar]
Karlsson 1996
- Karlsson J, Eriksson BI, Sward L. Early functional treatment for acute ligament injuries of the ankle joint. Scandinavian Journal of Medicine & Science in Sports 1996;6(6):341‐5. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kitchen 1990
- Kitchen SS, Partridge CJ. A review of therapeutic ultrasound. Physiotherapy 1990;76(10):593‐600. [EMBASE: 1992082601] [Google Scholar]
Lefebvre 2009
- Lefebvre C, Manheimer E, Glanville J. Chapter 6.4.11: Search filters. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions. Version 5.0.2 (updated September 2009). The Cochrane Collaboration, 2009. Available from www.cochrane‐handbook.org.
Maxwell 1992
- Maxwell L. Therapeutic ultrasound: Its effects on the cellular and molecular mechanisms of inflammation and repair. Physiotherapy 1992;78(6):421‐6. [EMBASE: 1992195059] [Google Scholar]
Moher 1996
- Moher D, Jadad AR, Tugwell P. Assessing the quality of randomized controlled trials. Current issues and future directions. International Journal of Technology Assessment in Health Care 1996;12(2):195‐208. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Moher 2001
- Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel‐group randomised trials. Lancet 2001;357(9263):1191‐4. [MEDLINE: ] [PubMed] [Google Scholar]
Moher 2010
- Moher D, Hopewell S, Schulz KF, Montori V, Gotzsche PC, Devereaux PJ, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c869. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Roebroeck 1998
- Roebroeck ME, Dekker J, Oostendorp RA. The use of therapeutic ultrasound by physical therapists in Dutch primary health care. Physical Therapy 1998;78(5):470‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Van der Heijden 1991
- Heijden GJMG, Bouter LM, Beckerman H, Bie RA, Oostendorp RAB. De effectiviteit van ultrageluid bij aandoeningen van het bewegingsapparaat: een op methodologische criteria gebaseerde geblindeerde review van gerandomiseerd patiëntgebonden onderzoek. Nederlands Tijdschrift voor Fysiotherapie 1991;101(7/8):169‐77. [Google Scholar]
References to other published versions of this review
Van der Windt 2002
- Windt DAWM, Heijden GJMG, Berg SGM, Ter Riet G, Winter AF, Bouter LM. Ultrasound therapy for acute ankle sprains. Cochrane Database of Systematic Reviews 2002, Issue 1. [DOI] [PubMed] [Google Scholar]


