Abstract
OBJECTIVE:
To compare incidence, risk factors, and etiology of women’s deaths in fertile, subfertile and ART- treated women in the years after delivery.
DESIGN:
Retrospective cohort
SETTING:
University Hospital
PATIENTS:
Women who had delivered in MA
INTERVENTIONS:
This study used data from the Society for Assisted Reproductive Technology Clinic Outcome Reporting System (SART CORS) linked to vital records, hospital stays and the Massachusetts death file. Mortality of patients delivered from 2004–2013 was evaluated through 2015. The exposure groups, determined on the basis of the last delivery, were ART-treated (linked to SART CORS), subfertile (no ART but with indicators of subfertility including birth certificate checkbox for fertility treatment, prior hospitalization for infertility (ICD9 628 or V23), and/or prior delivery with checkbox or ART), or fertile (neither ART nor subfertile). Numbers (per 100,000 women years) and causes of death were obtained from the Massachusetts death file.
MAIN OUTCOME MEASURES:
Mortality of women after delivery in each of the three fertility groups and the most common etiology of death in each.
RESULTS:
We included 483,547 women: 16,429 ART, 11,696 subfertile, and 455,422 fertile among whom there were 1,280 deaths with 21.1, 25.5, and 44.7 deaths respectively per 100,000 women years. External causes (violence, accidents, and poisonings) were the most common reasons for death in the fertile group (p< 0.05). Deaths occurred on average 46 months after delivery. When external causes of death were removed, there were 19.1, 17.0, and 25.6 deaths per 100,000 women years and leading causes of death in all groups were cancer and circulatory problems.
CONCLUSIONS:
The study presents reassuring data that death rates within 5 years of delivery in ART-treated, and subfertile women do not differ from those in fertile women.
Keywords: mortality, fertility, IVF, assisted reproduction, subfertile
Capsule:
The study presents reassuring data that rates of death within 5 years of delivery in ART-treated, and subfertile women do not differ from those in fertile women.
Introduction:
Assisted reproductive technology (ART) has enjoyed a dramatic success because of improvements in stimulation, retrieval, and laboratory services. From the most recent article on the state of ART, it was noted that from 2006–2014 (which was the latest data at the time) there were over 1.1 million IVF babies in the United States (US) and this comprised over 1.5% of all deliveries in the country (1). The numbers of live births have continued to rise from 2014–2016: 65,175 in 2014; 67,818 in 2015 (greater than 4%) and 71,296 in 2016 (greater than 5% rise from the previous year) (2). These numbers are projected to continue to grow. However, the long-term risk of ART is still in question.
Death of mothers during and following delivery is considered by leaders in obstetrics and gynecology in the United States to be on the rise (3–4). Several reviews have supported the perspective that studies need to be done to understand and counter this trend (5–7). Two previous reports have studied maternal mortality (mortality within 42 days of delivery) and mortality in the years following ART and have suggested that ART pregnancies and deliveries have reduced overall mortality compared to the fertile population (6,7). However, these studies did not adjust for confounders such as underlying infertility, health, or socio-demographic variables nor did they deal with the possible heterogeneity within the ART population itself (5). Since patients undergoing ART are screened for disease and potential complications, it is possible that the ART population was a healthier patient population. Vassard et.al. summarized their results in which lower mortality over the time period 1994–2009 in the ART group compared with a sampling from routinely delivered patients may have resulted from differences in care, in which patients treated for infertility may have changed health habits (stopped smoking, lost weight, or had psychological counseling) prior to pregnancy. For their study, they evaluated all–cause mortality to see if it was related to biological or selection mechanisms. (5) In addition, having planned a pregnancy was associated with reduced mortality risk in another study (6).
The goal of the current study was to evaluate mortality in women for the years following delivery in ART-treated and subfertile women and to compare mortality in the years following delivery in these groups to women with no identified history of subfertility or fertility treatment. Using the Massachusetts Outcome Study for Assisted Reproductive Technology (MOSART), which links clinical ART history, birth certificates, and hospital stays, our primary objective was to determine whether the ART and subfertile women were at a greater risk of mortality than fertile women in the years following delivery. The secondary objective was to determine the risk factors for mortality and etiologies for death in each fertility group.
Methods:
This was a retrospective cohort study that used Massachusetts ART data linked to state vital records and hospitalizations.
Patients:
The study included Massachusetts women ≥ 18 years of age who had an in-state live birth or fetal death delivery between July 1, 2004 and December 31, 2013. All women who delivered were part of the study with the exception of those who had acted as gestational carriers. For women with multiple deliveries during the study period, we used her last delivery to define her fertility group (ART, subfertile, fertile) even though prior hospitalizations, prior ART, and other information from prior deliveries were considered in developing the categorizations for the final delivery. We excluded women whose death records were missing date of death (n=3) and any whose date of death was recorded as prior to the last delivery (n=1).
Data Sources:
Data were obtained from 1) the Society for Assisted Reproductive Technology Clinic Outcome Reporting System (SART CORS), which is a national registry containing cycle-based ART data from the majority of US ART clinics and 2) the Massachusetts Pregnancy to Early Life Longitudinal (PELL) data system, which is an ongoing population-based data system that compiles information from birth certificates, fetal death records, and hospital utilization data. The study took place under a Memorandum of Understanding between SART, the Massachusetts Department of Public Health (MDPH) and the project principal investigators. Human subject’s approval was obtained from MDPH and the Committee for the Protection of Human Subjects at Dartmouth College.
The SART CORS contains demographic, ART diagnosis, ART cycle treatment, and pregnancy and delivery data from over 90% of US ART clinics. Data are entered by individual clinics throughout the country and reported to the Centers for Disease Control and Prevention (CDC) in compliance with the Fertility Clinic Success Rate and Certification Act of 1992 (Public Law 102–493). All Massachusetts clinics reported data to SART CORS during the study period. The data in the SART CORS are validated annually with some clinics having on-site visits for chart review based on an algorithm for clinic selection. During each visit, data reported by the clinic were compared with information recorded in patients’ charts. Ten out of 11 data fields selected for validation were found to have discrepancy rates of ≤5% (8).
The PELL data system links information on over 98% of Massachusetts births and fetal deaths to corresponding hospital utilization data for individual women and their children. The MDPH and the Massachusetts Center for Health Information and Analysis are the custodians of the PELL data.
Linkage of databases:
The population based MOSART database was constructed by linking the SART CORS and PELL data systems for all Massachusetts resident women delivering in Massachusetts hospitals between July 1, 2004 and December 31, 2013. The starting date was chosen based on the availability of SART CORS data (January 1, 2004 cycle starts with first deliveries occurring in July). A deterministic five phase linkage algorithm methodology was used with matching based on mother’s date of birth, her first name and last name; father/partner’s last name, baby’s date of birth, plurality, and infant gender (9). Our linkage rate for 2004–2013 data was 90.2% overall and 94.5% for deliveries in which both mother’s zip code and clinic were located in Massachusetts. Birth records from MOSART database were further linked to the Massachusetts death file using names, zip code and woman’s date of birth.
Exposure Groups:
Exposure groups were defined according to the last delivery for each woman. As we have reported previously (10), women were classified as ART-treated if the delivery was linked to an ART cycle in the SART CORS database. ART cycles in SART CORS include all of those cycles in which oocytes were obtained and cultured outside of a woman’s body. Cycles include all fresh and frozen embryo transfers using both autologous and donor oocytes with the exception of gestational carrier cycles which cannot accurately be linked to birth certificates. ART cycles do not include intrauterine insemination or other fertility enhancing treatments. They were classified as subfertile if the birth certificate for the delivery included a checked box that indicated that they had received fertility treatment but the delivery was not also linked to an ART cycle in SART CORS or if they had either a prior diagnosis of infertility (ICD9 628.9 or V23) in any hospitalization prior to the index delivery or if they had had a prior ART delivery. Women were classified as fertile if they did not fall into the ART-treated or subfertile groups.
Outcome Measures:
Deaths were ascertained through record linkage to the Massachusetts death file. Women were followed from the date of their last delivery in MOSART until death or the end of follow-up on December 31, 2015 whichever came first. Information on date of death and underlying cause of death was obtained from the Massachusetts death file. The death file compiles information from death certificates, the most accurate available source to identify deaths. Causes of death were classified according to the International Classification of Disease, ICD10 categories established by the world health organization (See Supplemental Table 1). The primary outcomes were death from all-causes and death excluding external causes (ICD10 codes: V01-Y98) at any time after last delivery until end of follow-up. External causes of mortality were defined as deaths as a result of poisonings, accidents, suicide, homicide or unintentional injuries.
Potential confounding variables:
Socio-demographic covariates were obtained from the birth/death certificates. Medical history was determined from a combination of birth certificates and hospital records (inpatient or outpatient hospital stays or emergency room visits). Data included date of last delivery, mother’s age, race/ethnicity, education, marital status, insurance at delivery, any history of chronic diabetes and hypertension, and history pre-eclampsia. Any history of chronic hypertension was defined as a woman ever having an ICD9 code 401–405 on hospital records or the checkbox for chronic hypertension on the birth certificate. Any history of chronic diabetes is defined as a woman ever having an ICD9 code 250 or 648.0 on hospital records or checkbox for chronic diabetes on the birth certificate. Pregnancy hypertension/eclampsia/pre-eclampsia is defined as a woman having an ICD9 code of 642, 642.4, 642.5, 642.6, or 642.7 on hospital records or checkbox for pre-eclampsia, eclampsia, or pregnancy hypertension on the birth certificate on her last delivery record.
Statistical Analyses:
Women’s survival times were calculated with women-years of follow-up defined as time between date of last delivery in MOSART, and death or end of follow-up (December 31, 2015). We reported the incidence of all-cause mortality rates (Table 1) as number of deaths per 100,000 women years. The numbers can be interpreted as follows: given a mortality rate of 19.1 per 100,000 women-years in one group, incidence of mortality will occur, on average, 19.1 times in 10,000 mothers over 10 years (10,000 times 10=100,000) or in 100,000 mothers over 1 year (100,000 times 1=100,000).
Table 1:
Summary of Deaths*
| ART | Subfertile | Fertile | ||||
|---|---|---|---|---|---|---|
| N | Rate (per 100,000 Women Years) | N | Rate (per 100,000 Women Years) | N | Rate (per 100,000 Women Years) | |
| Number of Women | 16,429 | 11,696 | 455,422 | |||
| All Deaths (All-cause mortality) | 21 | (21.1) | 18 | (25.5) | 1,280 | (44.7) |
| Women Years All Deaths | 99,331 | 70,461 | 2,865,459 | |||
| All deaths (all-cause mortality) excluding external causes of mortality† | 19 | (19.1) | 12 | (17.0) | 733 | (25.6) |
| Women years (All death excluding external causes of mortality) † | 99,324 | 70,438 | 2,863,217 | |||
This table presents the number of deaths after delivery in the 3 groups: fertile (no history of infertility), subfertile (indicators of subfertility but, no ART), and ART (ART treatment) which show a significant difference between the fertile group and both the subfertile and ART groups when all causes of mortality are included. Once the external causes are removed in the lower part of the table there is no significant difference between the groups.
Excludes women who died from Injuries, external causes of mortality (includes opioids, accidents and injuries).
We used Poisson regression to examine differences in rates across fertility groups. Socio-demographic and health characteristics among fertility groups were evaluated using χ2- tests for categorical variables, with p-values ≤0.05 noted as significant (Table 2). Cox proportional hazard models were used to assess the hazard ratios of select maternal characteristics with mortality, as well as the hazard ratios for mortality among ART-treated, subfertile, and fertile women (Table 3). Crude (HR) and adjusted hazard ratios (aHR) and 95% confidence intervals (CI) are reported. We performed Cox models for a subset of the sample excluding external causes of death. The adjusted models were controlled for fertility group, maternal age, race/ethnicity, education, marital status, insurance at delivery, any history of chronic diabetes and hypertension, and pregnancy hypertension/eclampsia/pre-eclampsia in the last pregnancy. The proportional hazards assumption was assessed via plot of the cumulative martingale residuals for each of the covariates.
Table 2:
Demographic and Maternal Characteristics According to Whether or Not the Women Died*
| Demographic Characteristic | All Women | Excluding External Causes of Deaths | ||
|---|---|---|---|---|
| Women who did not die % (n) | Women who died † % (n) | Women who did not die % (n) | Women who died † % (n) | |
| N | 482,228 | 1,319 | 482,228 | 764 |
| Mother’s Age (years) at last delivery | ||||
| <25 | 18.1 | 24.4 | 18.1 | 14.4 |
| 25–29 | 23.1 | 23.3 | 23.1 | 20.0 |
| 30–34 | 31.7 | 24.4 | 31.7 | 28.1 |
| 35–39 | 21.4 | 21.2 | 21.4 | 27.9 |
| 40+ | 5.8 | 6.7 | 5.8 | 9.6 |
| Mother’s Race | ||||
| Hispanic | 15.6 | 10.5 | 15.6 | 11.6 |
| Non-Hispanic White | 64.6 | 73.4 | 64.6 | 70.0 |
| Non-Hispanic Black | 9.4 | 10.3 | 9.4 | 11.6 |
| Asian and Pacific Islander | 8.6 | 3.5 | 8.6 | 4.7 |
| American Indian, Other and Unknown | 1.9 | 2.3 | 1.9 | 2.1 |
| Mother’s Education | ||||
| ≤High School or GED | 41.7 | 67.4 | 41.7 | 60.7 |
| Some college or Associate | 15.4 | 13.2 | 15.4 | 12.5 |
| ≥Bachelor’s degree | 42.9 | 19.4 | 42.9 | 26.8 |
| Marital Status | ||||
| Married | 66.7 | 39.6 | 66.7 | 51.7 |
| Not Married | 33.3 | 60.4 | 33.3 | 48.3 |
| Insurance at delivery | ||||
| Private | 56.3 | 33.5 | 56.3 | 44.0 |
| Public | 43.7 | 66.5 | 43.7 | 56.0 |
| Parity | ||||
| 1 | 37.8 | 33.6 | 37.8 | 31.3 |
| 2+ | 62.2 | 66.4 | 62.2 | 68.7 |
| Any History of Chronic Diabetes | ||||
| No | 97.7 | 92.3 | 97.7 | 90.8 |
| Yes | 2.3 | 7.7 | 2.3 | 9.2 |
| Any History of Chronic Hypertension | ||||
| No | 95.3 | 84.0 | 95.3 | 79.2 |
| Yes | 4.7 | 16.0 | 4.7 | 20.8 |
| Pregnancy Hypertension/Eclampsia/Pre-eclampsia | ||||
| No | 95.2 | 93.1 | 95.2 | 92.0 |
| Yes | 4.8 | 6.9 | 4.8 | 8.0 |
Demographic and maternal characteristics compare each characteristic according to whether women lived or died. This is considered for all women and for the population in which external causes of death were not included. Not surprisingly, those who lived had less medical or social issues such as hypertension, hypertension in pregnancy/eclampsia/pre-eclampsia, and diabetes. Furthermore, they had higher education, more insurance, and fewer deliveries.
P values for most categories when comparing those who died with those who did not, significant at P<0.0001; except P values for parity= 0.0002 among the all women sample; among sample excluding external causes of death, P values for parity= 0.002; and pregnancy hypertension/eclampsia =0.0004
Table 3:
Hazard Ratios predicting mortality in women who delivered (2004-2013) while including and excluding external causes of mortality*
| Maternal Characteristics | All-cause mortality** | Mortality (Excluding External causes)*** | ||
|---|---|---|---|---|
| Unadjusted HR (95% CI) | Adjusted HR† (95% CI) | Unadjusted HR (95% CI) | Adjusted HR† (95% CI) | |
| Fertility Group | ||||
| Fertile | Reference | Reference | Reference | Reference |
| Subfertile | 0.58 (0.37–0.93) | 0.89 (0.56–1.42) | 0.68 (0.38–1.2) | 0.75 (0.42–1.33) |
| ART | 0.46 (0.3–0.72) | 0.75 (0.48–1.18) | 0.73 (0.46–1.16) | 0.81 (0.50–1.30) |
| Mother’s Age (years) at last delivery | ||||
| <25 | Reference | Reference | Reference | Reference |
| 25–29 | 0.75 (0.64–0.88) | 1.15 (0.98–1.35) | 1.08 (0.84–1.38) | 1.49 (1.16–1.91) |
| 30–34 | 0.56 (0.48–0.65) | 1.31 (1.11–1.55) | 1.08 (0.86–1.36) | 2.04 (1.59–2.61) |
| 35–39 | 0.66 (0.56–0.78) | 1.68 (1.4–2.01) | 1.46 (1.16–1.83) | 2.85 (2.21–3.67) |
| 40+ | 0.77 (0.61–0.98) | 1.81 (1.41–2.32) | 1.82 (1.35–2.45) | 3.23 (2.35–4.44) |
| Race/Ethnicity | ||||
| Non-Hispanic White | Reference | Reference | Reference | Reference |
| Hispanic | 0.65 (0.55–0.78) | 0.34 (0.28–0.41) | 0.76 (0.6–0.95) | 0.5 (0.39–0.63) |
| Non-Hispanic Black | 1.04 (0.87–1.25) | 0.54 (0.45–0.65) | 1.24 (0.99–1.55) | 0.71 (0.56–0.9) |
| Asian/Pacific Islanders | 0.38 (0.28–0.51) | 0.48 (0.36–0.65) | 0.54 (0.39–0.76) | 0.65 (0.46–0.91) |
| American Indians & Others | 1.00 (0.69–1.44) | 0.64 (0.45–0.93) | 0.96 (0.58–1.58) | 0.71 (0.43–1.17) |
| Education | ||||
| <HS or HS/GED | Reference | Reference | Reference | Reference |
| Some college or Associate Degree | 0.73 (0.62–0.86) | 0.87 (0.73–1.03) | 0.79 (0.63–0.98) | 0.81 (0.64–1.01) |
| Bachelor’s degree or Post-graduate | 0.31 (0.27–0.36) | 0.54 (0.45–0.64) | 0.48 (0.41–0.57) | 0.59 (0.48–0.73) |
| Marital Status | ||||
| Married | Reference | Reference | Reference | Reference |
| Not Married | 3.22 (2.88–3.6) | 2.38 (2.06–2.73) | 1.98 (1.72–2.29) | 1.84 (1.54–2.21) |
| Insurance at last delivery | ||||
| Private | Reference | Reference | Reference | Reference |
| Public | 2.85 (2.54–3.2) | 1.84 (1.58–2.14) | 1.83 (1.58–2.11) | 1.49 (1.23–1.80) |
| History of Chronic Hypertension | ||||
| No | Reference | Reference | Reference | Reference |
| Yes | 3.47 (2.99–4.02) | 2.43 (2.06–2.86) | 4.77 (4–5.69) | 3.22 (2.65–3.92) |
| Pregnancy Hypertension/Eclampsia/Preeclampsia | ||||
| No | Reference | Reference | Reference | Reference |
| Yes | 1.50 (1.21–1.86) | 1.15 (0.92–1.43) | 1.77 (1.35–2.3) | 1.2 (0.91–1.58) |
| History of Chronic Diabetes | ||||
| No | Reference | Reference | Reference | Reference |
| Yes | 3.26 (2.66–4.00) | 1.92 (1.54–2.38) | 0.58 (0.37–0.93) | 1.94 (1.49–2.54) |
Adjusted analyses of factors associated with all-cause mortality and mortality excluding external causes are shown in Table 3. The strongest parameters predicting all-cause mortality were history of mother’s age, education, marital status, and being publically insured as well as chronic hypertension, chronic diabetes. Once adjusted, fertility group (ART, subfertility) is no longer a significant predictor of all-cause mortality. Hazard ratios in bold denote significant results at P<0.05.
Study sample for all-cause-mortality is based on (N=480,243). Missing covariates for education (n=1568), Race (N=527), and marital status (N=1457) were deleted for modeling purposes.
Study sample for mortality (excluding external causes) is based on (N= 479,693). Missing covariates for education (N=1568), Race (N=525), and marital status (N=1453) and external causes of death (N=555) were deleted for modeling purposes.
Models are simultaneously adjusted for all other maternal characteristics included in table 3.
All analyses were performed using the SAS software, version 9.3 (SAS Institute, Cary, NC).
Results:
The study sample included 483,547 women: 16,429 ART, 11,696 subfertile, and 455,422 fertile. There were 21 deaths in the ART group, 18 deaths in the subfertile group and 1,280 deaths in the fertile group. (Table 1). The incidence rate was 21.2, 25.5, and 44.7 per 100,000 women years for the ART, subfertile and fertile group, respectively.
The average follow-up time was 5.6– 6.0 years for all women after the last delivery. The average age for women who died in each group at time of death was: 46.6 ± 4.5 years for ART; 42.5 ± 6.2 years for subfertile; and 37.5 ± 7.2 years for fertile women, the fertile group being younger than the others (Supplemental Table 2).
To further evaluate the medical causes of death in the three fertility groups, deaths by external causes (N=555) were removed (Table 1). The numbers of deaths in the ART group was reduced to 19, subfertile to 12 and fertile group to 733. These decreases led to there being 19.1 deaths per 100,000 women years in the ART group;17.0 deaths per 100,000 women years in the subfertile group; and 25.6 deaths per 100,000 women years in the fertile group. There was no difference in mortality between these three groups once the external causes were removed (Table 1). Follow-up times are 2.8–4.3 years for women who died and 5.6–6.1 years for women who did not die (Supplemental Table 2). Among women who did not die the women in either the ART (42.4 ± 5.5) or the subfertile (41.2 ± 5.5) group were older than women those in the fertile group were younger (36.5 ± 6.7 years) (Supplemental Table 2).
Demographic and maternal characteristics at time of delivery among the women who died and did not die, with and without external causes of mortality are shown in Table 2. Both with and without external causes of death removed, those who died were in women <35 years of age, non-Hispanic white, less likely to be married and less likely to have had college or post graduate education. There was no difference in plurality (not shown in table, P=0.61) although those who died had increased parity. Higher mortality was seen in the public payer source group. A greater percentage of the women who died had chronic diabetes mellitus, chronic hypertension, and pre/eclampsia/eclampsia or hypertension during pregnancy compared to those who did not die (Table 2).
Table 3 presents crude HRs and aHRs for associations between selected characteristics and all-cause mortality and mortality excluding external causes of death. Adjusting for maternal characteristics, risk of all-cause mortality was higher for mothers aged 30 years and older (aged 30–34: aHR: 1.31 [95% CI: 1.11–1.55]; aged 35–39: aHR: 1.68 [95% CI: 1.40–2.01; aged ≥40: aHR: 1.81 [95% CI: 1.41–2.32]) relative to mothers younger than age 25 years. Those who were not married had higher risk of mortality compared to married women (aHR: 2.38 [95% CI: 2.06–2.73]), and those who had public insurance compared with private (aHR: 1.84 [95% CI: 0.58–2.14]). Risk of all-cause mortality was also significantly higher for mothers with history of chronic hypertension (aHR: 2.43 [95% CI: 2.06–2.86]), or history of chronic diabetes (aHR: 1.92 [95% CI: 1.54–2.38]).
The risk of all-cause mortality was significantly lower for mothers who were Hispanic aHR: 0.34 [95% CI: 0.28–0.41]), non-Hispanic blacks aHR: 0.54 [95% CI: 0.45–0.65]), Asian/Pacific Islanders aHR: 0.48 [95% CI: 0.36–0.65]), and American Indians/Other: aHR: 0.64 [95% CI: 0.45–0.93]) compared to non-Hispanic white mothers. Mothers with bachelors or more years of education had a significantly lower risk compared with those who had less than a high school education or high school education (aHR: 0.54 [95% CI: 0.45–0.64]).
Similar patterns were observed in the subset of the population where we excluded external causes of death. Mothers who were older, with a history of chronic diabetes, chronic hypertension, public insurance, or unmarried had a higher risk of mortality. Mothers who were Hispanic, non-Hispanic black, or Asian had a significantly lower risk compared to non-Hispanic white, and those with a bachelors or more education had significantly lower risk of mortality compared to those with less than high school or high school education (Table 3). In the adjusted models, neither pregnancy hypertension nor fertility group was associated with death. ART-treated women compared to fertile women had an aHR of 0.48 (95%CI: 0.75, 0.48– 1.18) while or among subfertile women compared to fertile women had an aHR of 0.89 (95%CI: 0.56– 1.42) (Table 3).
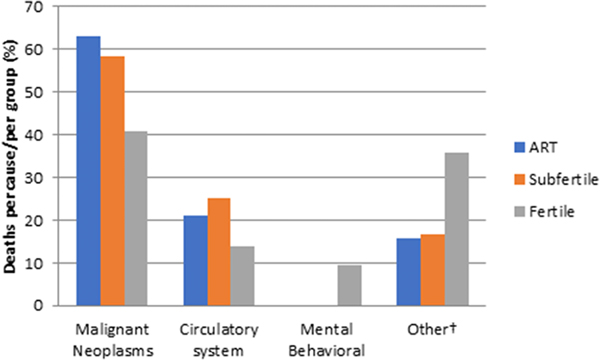
With external causes of death removed, the leading causes of mortality in each group were neoplasm and circulatory in all three groups being respectively 63% and 21% in the ART-treated women, 58% and 25% in the subfertile women and 40% and 14% in the fertile women (Figure 1: The reasons for death without external causes of mortality removed are shown in Supplemental Figure 1). It was noteworthy that when external causes of death are removed the fertile group had an increased number of deaths due to mental/behavioral issues (9%); whereas, the ART and subfertile groups had no deaths due to this etiology.
Figure 1:
Primary Causes of Death in MOSART Cohort excluding external causes of mortality, by Fertility Group (n=764).
The figure represents the relative number of etiologies of death in the ART-treated, subfertile, and fertile groups with external causes removed. Additionally, it revealed that Mental and Behavioral etiology of death was present in 9% of the fertile group and 0% in subfertile and ART groups.
† Other includes: Infectious and parasitic diseases; In situ, benign or unknown behavior neoplasm ;Diseases of the blood and blood-forming organs and disorders involving the immune mechanism Endocrine, nutritional and metabolic diseases; Diseases of nervous system ;Diseases of the respiratory system Diseases of the digestive system; Diseases of the musculoskeletal system and connective tissue; Diseases of the genitourinary system ;Pregnancy, childbirth and the puerperium; Congenital malformations; Abnormal clinical and laboratory findings, not elsewhere classified
Discussion:
In this retrospective population-based study of mortality in three fertility groups, ART-treated, subfertile, and fertile, we found that using an unadjusted model that included all deaths, there were significantly fewer deaths in the ART and subfertile than in the fertile group and that the most common cause of death for fertile women was non-medical external causes (accidents, violence and poisonings). When results were adjusted and/or when external causes of death were removed from consideration, there was no difference in deaths per 100,000 women years in the three fertility groups and the most common causes in each group were neoplasia and circulatory abnormalities.
Comparing our results to those of others demonstrated similarities and differences in outcomes for mortality but differences in study design. Our study found no differences in adjusted rates of mortality among the three fertility groups, these rates ranged from 17–19.1 deaths per 100,000 women years. These findings are in agreement with the studies of Vassard (5) who compared ART treated with untreated women and found no difference HR =0.92 (95% CI 0.79,1.07). However, Venn et. al (6) compared the ART-treated population with the general population and found that mortality was lower in the ART group (age standardized mortality ratio 0.58, 95% CI 0.48–0.69) and that the mortality rate occurring within one year of the end of ART pregnancy was 11.7 (95% CI 2.9–46.8) deaths per 100,000 women years. Braat et. al (7) also found lower rates for ART: 31 per 100,000 women as compared with general population norms of 71 per 100,000 women. Even when results were similar, there were notable differences in study design. For example, both the Venn and the Braat studies followed patients from initiation of the ART cycle while we were only able to follow patients from delivery because we relied on the birth certificates for identification of the study cohorts and were thus unable to identify pregnant patients who did not deliver. These prior investigations also had different follow-up time from our study. We had a median follow-up of 6 years while Venn (6) and Braat (7) both followed patients out to one year. Nevertheless, in all cases even with long intervals, there were only a small number of deaths.
Studies of ART have often used a fertile population as the comparison group and have ignored untreated subfertile individuals. In this study we used a subfertile comparison group in addition to the fertile comparison group. The subfertile group had numerous characteristics (e.g. age, race/ethnicity. education, insurance) that were more similar to the ART group than those of the fertile group. This, and the fact that underlying infertility, in addition to ART treatment, may contribute to mortality makes the subfertile group an important addition. Our study found that mortality rates did not differ in the ART, subfertile and fertile groups but did so only after adjustment or when external causes of death were removed. Also with regard to demographics, although we saw differences in rates of death by race further analysis of these differences are outside the scope of this paper.
It is possible, as suggested by Schmidt et al. (12), that, since infertility is a disease that manifests over time, there is a contribution from life–style changes involving health improvement by those who choose ART that could reduce the effect of co–morbid conditions (diabetes, hypertension) and might therefore decrease the chance of death. Denmark, Australia, and Holland where several prior studies were performed, have social and medical systems that provide comprehensive medical care (5–7, 12). This is not available to our population, despite the fact that Massachusetts has an infertility insurance mandate (13). In our study, where the main causes of death in the full (all cause) fertile group were accidental, intentional, and unintentional injuries we found that the risk for these types of deaths were driven primarily by having no private insurance, single marital status, and less education, suggesting that these causes are related to socioeconomic status and lack of adequate healthcare. A lack of care driven by lack of insurance may, as suggested by Howell et.al. (11), have resulted in differences in treatment of chronic diseases such as hypertension and chronic diabetes thereby resulting in higher mortality. Of note, however, we also found that hospital type (e.g. primary vs. secondary vs. tertiary) did not vary by fertility group suggesting that it was unlikely that the hospital care itself in the fertile group would have led to higher morbidity.
Our study of the etiologies of mortality within the three fertility groups revealed that once external causes of death were removed, there was no difference in reason for death among the three fertility groups, and the most common causes in all the groups were neoplasm and circulatory. Venn et.al. (6), also found that deaths due to neoplasm and specifically breast cancer were no more prevalent in the ART group than in their fertile group. Our fertile group, however, had a noteworthy percentage of deaths from mental health and behavioral disorders (9%); whereas, the ART and subfertile groups had none. This aspect was not studied further because it was not part of our objective, but it does suggest that an association with increase in preconception care may reduce this cause of death as it may enhance the ability to identify these problems and thus encourage treatment (14,15,16).
This study has both strengths and limitations. The strengths lie in the fact that we have been able to evaluate population mortality in a large cohort that linked ART deliveries to birth certificates and hospitalizations due to the availability of both the SART CORS and PELL databases. The dataset that was generated with the SART CORS and PELL combination (2004–2013) contained over 480,000 patients and is the largest population evaluated on this subject to date. Nevertheless, as with any retrospective study using large databases, some important data may be missing or inaccurately recorded. Limitations include that treatment exposure could only be identified from 2004 onwards due to unavailability of the SART CORS data prior to this date. Further, the fertile group could contain some subfertile women who possibly were not identified by our methods. Nevertheless, the direction of bias is such that the larger numbers in the fertile group would lessen the magnitude of the effect of this inclusion. We unfortunately, could not evaluate deaths during pregnancy because our linked data only identified patients who had delivered. One author who did study this timeframe noted there was increased morbidity and mortality (combined) in the infertility group (which did not separate ART and subfertile), but their number of mortalities (six) was very low (17). Further, small numbers of deaths in the ART and subfertile groups and MDPH regulations requiring suppression of low numbers of cases, made it impossible for us to report on some details of the causes of mortality or on maternal mortality occurring within 42 days of delivery. An additional limitation was possible immigration or out-migration of patients to or from Massachusetts during the study period. This could have resulted in a death occurring in another state and thus not being captured in our records. We also did not evaluate the time from pre-pregnancy diagnoses to first pregnancy and diagnoses out of hospital were not included in our dataset. A final limitation is that the study population was from a single US state which might not be representative of all states and countries.
In summary, our results show a crude mortality rate that is elevated in the fertile group as compared with the ART–treated or subfertile group when all causes of death were included; however, when all-cause rates were adjusted or when the external causes of death were excluded, there was no significant difference among the three fertility groups, suggesting that subfertile women, regardless of treatment with ART, are not at a higher risk of mortality than the fertile group.
Supplementary Material
Primary Causes of Death in MOSART Cohort, by Fertility Group (n=1,319).
The figure represents the relative number of etiologies of death in each of the fertile, subfertile or ART sub-groups with external causes of death included.
†Other includes: Infectious and parasitic diseases In situ, benign or unknown behavior neoplasm Diseases of the blood and blood-forming organs and disorders involving the immune mechanism Endocrine, nutritional and metabolic diseases Mental and behavioral disorders Diseases of nervous system Diseases of the respiratory system Diseases of the digestive system Diseases of the musculoskeletal system and connective tissue Diseases of the genitourinary system Pregnancy, childbirth and the puerperium Congenital malformations Abnormal clinical and laboratory findings, not elsewhere classified.
Acknowledgement:
SART wishes to thank all of its members for providing clinical information to the SART CORS database for use by patients and researchers. Without the efforts of our members, this research would not have been possible.
Supported by: NIH Grant R01HD067270
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Toner J, Coddington C, Doody K, Van Voorhis B, Seifer D, Ball D et al. Society for Assisted Reproductive Technology and assisted reproductive technology in the United States: a 2016 update. Fert. Steril. 2016;106:541–6. [DOI] [PubMed] [Google Scholar]
- 2.Society for Assisted Reproductive Technology. National Annual Summary Report at : https://www.sartcorsonline.com/rptcsr.
- 3.MacDorman MF, Declercq E, Cabral H, Morton C. Recent Increases in the U.S. Maternal Mortality Rate: Disentangling Trends From Measurement Issues. Obstet Gynecol 2016; 128 (3):447–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wetzel LM. Maternal Mortality Statistics. Contem Obstet Gynecol January2018:24–27. [Google Scholar]
- 5.Vassard D, Schmidt L, Pinborg A, Petersen G, Forman L, Hageman I, Glazer C, Kamper-Jorgensen M. Mortality in Women tested with assisted reproductive technology treatment- addressing the healthy patient effect. Am J Epid. 2018;187(9):1889–1895. [DOI] [PubMed] [Google Scholar]
- 6.Venn A, Hemminki E, Watson L, Bruinsma F, Healy D. Mortality in a Cohort of IVF patients. Human Repro. 2001. (16):2691–2696. [DOI] [PubMed] [Google Scholar]
- 7.Braat D, Schutte J, Bernardus R, Mooij T, Van Leeuwen F. Maternal death related to IVF in the Netherlands 1984 – 2008. Human Repro 2010 (25):1782–1786. [DOI] [PubMed] [Google Scholar]
- 8.Center for Disease Control and Prevention, American Society for Reproductive Medicine, and Society for Assisted Reproductive Technology. 2012 Assisted Reproductive Technology Success Rates: National Summary and Fertility Clinic Reports. Washington, DC: US Dept. of Health and Human Services, 2014 [Google Scholar]
- 9.Kotelchuck M, Hoang L, Stern JE, Diop H, Belano FF C, Declercq E. The MOSART Database: Linking the Sart CORS Clinical Database to the Population – Based Massachusetts PELL Reproductive Public Health Data System, Matern Child Health J. 1B (a): 2167–78, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Declercq ER, Belanoff C, Diop H, Gopal D, Hornstein M, Kotelchuck M et al. Identifying Women with Indicators of Subfertility in a Statewide Population Database: Operationalizing the missing Link in Assisted Reproducitve Technology Research. Fertil. Steril.2014;101:463–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Howell E, Egorova N, Balbierz A, Zeitlin J, and Herbert P. Black-White Differences in Service Maternal Morbidity and Site of Care. Am J Obstet Gynecol. 2016;214(1):122e1–122e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schmidt L. Infertility and Assisted Reproduction in Denmark. Epidemiology and Psychosocial Consequences. Dan. Med. Bull. 2006;53 (4):390–417. [PubMed] [Google Scholar]
- 13.Dupree J, Dickey R, Lipschultz L. Inquity between Male and Female Coverage in State Infertility Laws. Fertl Stertil. 2016; 105 (6): 1519–1522. [DOI] [PubMed] [Google Scholar]
- 14.Wilkinson H Saving Mother’s Lives. Reviewing Maternal Deaths to make motherhood safer 2006–2008. BJOG, 2011;118:1402–3. [DOI] [PubMed] [Google Scholar]
- 15.Kurinczuk J, Draper E, Field D, Bevan C, Brocklehurst P, Gray R et al. Experiences with Maternal and Perinatal Death Reviews in UK- The MBRRACE-UK Programe.BJOG 2014;121:41–4 [DOI] [PubMed] [Google Scholar]
- 16.Crawford N, Hoff H, Mersereau J. Infertile Women who screen Positive for Depression are less Likely to initiate Fertility Treatments. Hum. Reprod. 2017;32(3):582–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dayan N, Joseph K, Fell D, Laskin C, Basso O, Park A, et al. Infertility Treatment and Risk of Severe Maternal Morbidity: a Propensity Score-Matched Cohort Study. CMAJ 2019. February 4;191:E118–27. Doi: 10.1503/cmaj.181124 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Primary Causes of Death in MOSART Cohort, by Fertility Group (n=1,319).
The figure represents the relative number of etiologies of death in each of the fertile, subfertile or ART sub-groups with external causes of death included.
†Other includes: Infectious and parasitic diseases In situ, benign or unknown behavior neoplasm Diseases of the blood and blood-forming organs and disorders involving the immune mechanism Endocrine, nutritional and metabolic diseases Mental and behavioral disorders Diseases of nervous system Diseases of the respiratory system Diseases of the digestive system Diseases of the musculoskeletal system and connective tissue Diseases of the genitourinary system Pregnancy, childbirth and the puerperium Congenital malformations Abnormal clinical and laboratory findings, not elsewhere classified.