Abstract
Attenuated Salmonella typhimurium (S. typhimurium) was selected as a transgenic vehicle for the development of live mucosal vaccines against transmissible gastroenteritis virus (TGEV) based on the M gene. An approximate 1.0 kb DNA fragment, encoding for glycoprotein M, was amplified by RT-PCR and cloned into eukaryotic expression vector pVAX1. The recombinant plasmid pVAX-M was transformed by electroporation into attenuated S. typhimurium SL7207, and the expression and translation of the pVAX-M delivered by recombinant S. typhimurium SL7207 (pVAX-M) was detected both in vitro and in vivo. BALB/c mice were inoculated orally with SL7207 (pVAX-M) at different dosages to evaluate safety of the vaccines. The bacterium was safe to mice at a dosage of 2 × 109 CFU, almost eliminated from the spleen and liver at week 4 post-immunization and eventually cleared at week 6. Mice immunized with 1 × 109 CFU of SL7207 (pVAX-M) elicited specific anti-TGEV local mucosal and humoral responses including levels of IgA, IgG, IL-4, and IFN-γ as measured by indirect ELISA assay. Moreover, the control groups (pVAX group, PBS group) maintained at a normal level during week 4–8 post-immunization. The results indicated that attenuated S. typhimurium could be used as a delivery vector for oral immunization of TGEV M gene vaccine.
Keywords: Transmissible gastroenteritis virus, Attenuated Salmonella typhimurium, M gene
Introduction
Transmissible gastroenteritis virus (TGEV) is the etiological agent of transmissible gastroenteritis (TGE), which is a highly contagious enteric disease in piglets causing high mortality rate of up to 100 % and resulting especially in severe economic losses to the affected farms [21, 23]. The membrane (M) protein is one of the structural proteins of TGEV, while other two are the phosphorylated nucleoprotein (N) and the spike (S) protein [17]. The lipid envelope M protein is highly glycosylated and helps the viral nucleocapsid to bind to the capsule membrane [31].
The M protein of TGEV exposes the carboxy-terminal region on the external surface of the virion. The M protein-specific monoclonal antibodies were used for neutralizing TGEV and mediating TGEV-infected cellular complement-dependent lysis, which suggested that M protein has good immunogenicity and reactogenicity of TGEV [16, 22]. The M protein affects the mutation of the virus and is confined to the endoplasmic reticulum of virus assembly. It is a multifunctional protein with a crucial role in coronavirus assembly. It could interact in the membrane with the S protein and E protein. At the same time, its C-terminal domain is integrated within the viral core to drive coronavirus component [4, 7, 8]. Early study suggested that TGEV-infected piglets’ blood and gut have high levels of interferon (IFN) and confirmed that the induction of interferon related to the interaction between the M protein and the cell membrane M protein-specific monoclonal antibodies can effectively block the synthesis of α-interferon, while S and N proteins could not, which showed that the induction of interferon region located outside the M protein plays a major effector role [20]. Three structural proteins (S, N, M) were expressed with baculovirus and intraperitoneal inoculated to pigs. The results showed that these proteins induced intestinal mucosal immunity concerned with IgA antibodies to TGEV and confirmed that there was an increase in the occurrence of CD4 + CD8 + (double-positive T cells), CD2 + CD4 − CD8 + dim (natural killer), and CD2 + CD4 − CD8 + bright (cytotoxic T-cell phenotypes) accompanied by increased expression of interleukin-2 receptor [25]. Those findings indicate that M genes could be used as potential target genes for developing the genetic vaccine.
In recent years, attenuated Salmonella typhimurium (S. typhimurium) have been utilized as carriers, like other intracellular bacteria (Shigella and Listeria), for efficient delivery of either DNA vaccine or vaccine antigens for oral immunization. As a live vaccine vector, attenuated S. typhimurium has weak virulence and good invasiveness [15, 19, 33, 34]. Meanwhile, bacteria carrying the heterologous antigens orally immunized after presentation to the host immune system can induce anti-specific antigen local and systemic immune response [1, 10, 12]. In particular, attenuated S. typhimurium has been used to deliver DNA vaccines encoding immunogens of pathogenic microorganisms including HIV and PRRSV [13, 14]. Our previous studies revealed that attenuated S. typhimurium was a good carrier for TGEV S gene [33]; however, the use of S. typhimurium as a DNA vaccine vector harboring TGEV M gene has almost not been reported. In this study, to investigate the feasibility of an oral vaccine based on TGEV M gene, we constructed DNA vaccines encoding the intact TGEV glycoprotein M using the attenuated intracellular bacteria, attenuated S. typhimurium SL7207, and its safety and immunogenicity has been evaluated. Our preliminary data indicated that immunizing by orogastric intubation with the recombinant S. typhimurium could induce a specific immune response against TGEV.
Materials and methods
Cells, virus, plasmid, and bacterial strains
Swine testicle (ST) cells and human embryonic kidney (HEK-293) cells were cultured in Dulbecco’s modified Eagle medium (DMEM) with high glucose (Invitrogen) supplemented with 10 % fetal bovine serum (FBS, Invitrogen) and antibiotic–antimycotic solutions(×100; Invitrogen). The cells were maintained at 37 °C in 5 % CO2. Eukaryotic expression vector, pVAX1, was stored at −20 °C in our laboratory. The TGEV strain SC-H was isolated from Sichuan, P.R. China in 2005. The attenuated S. typhimurium aroA-strain SL7207 was kindly provided by Professor Kai Schulze of Helmholtz Centre for Infection Research, Germany.
Experiment mice
Female BALB/c mice (5 weeks old, 17–22 g) were used throughout the study, purchased from Chengdu Dossy Biological Technology Company (Chengdu, China). All animals were maintained in animal holding laboratory under controlled condition with a temperature of 25 ± 10 °C and humidity of 40 ± 10 % and given free access to food and water. The mice received humane care according to the USA’s National Institute of Health’s Guide for the Care and Use of Laboratory Animals.
Construction of TGEV M gene plasmid
Viral RNA was extracted from TGEV-infected ST cells using Beijing Tiangen total RNA extraction kit. An approximately 1.0 kb DNA fragment including the open reading frame of glycoprotein M was amplified from virus genomic RNA by RT-PCR, with the following primer pair M1: 5′-GCGGCCGCCCACAAAGTCTCTCGGACATAAG-3′ (forward) and M2: 5′-TCTAGAACTTGAACTAAACAAAATGAAG-3′ (reverse), which, respectively, introduce the Xba I and Not I restriction sites at the 5′ ends of the primers. The amplified DNA fragment of TGEV M gene was cloned into a pMD19-T vector (TaKaRa) and then sequenced. The target fragment was released from the pMD19-T plasmid by XbaI and NotI digestion and ligated into the pVAX1 vector digested by the same enzymes, and the final plasmid was named pVAX-M.
Transient expression of M protein in vitro
HEK-293 T cells were seeded into six-well tissue culture plates (Costar). Monolayers of 90 % confluent cells were transiently transfected with the plasmid pVAX-M and empty plasmid pVAX1 using Lipofectamine 2000 (Invitrogen). After 72 h post transfection, a part of the cells were collected to verify by RT-PCR. Another part of the cells were washed with phosphate-buffered saline (PBS), fixed with ice-cold methanol/acetone (1:1) at 4 °C for 30 min, and then washed with PBS again. Diluted antiserum of pig to TGEV (stored at −20 °C in the laboratory) and secondary antibodies (FITC-conjugated rabbit anti-pig IgG, Sigma) were incubated sequentially at 37 °C for 1 h. The rest of the cells were collected and cell lysis buffer was added to obtain the protein sample. The target protein was transferred to the polyvinylidene difluoride (PVDF) membrane after SDS-PAGE. The first antibody (swine TGEV- positive serum, 1:1000 dilution in TBST) and the second antibody (HRP-goat-anti-pig antibody, 1:5000 dilution in TBST) were incubated successively.
Transformation of attenuated S. typhimurium
The constructed plasmid pVAX-M or control vector pVAX1 was transformed into S. typhimurium competent cells by electroporation at 1.8 kV, 25 μF, and 200 Ω for 3 ms. The positive transformants were selected on LB agar containing 50 μg/mL kanamycin, and then detected by PCR amplification and digestion with restriction enzymes. The resulting S. typhimurium strains were named strain SL7207 (pVAX-M) and strain SL7207 (pVAX), respectively.
Stability of recombinant bacteria in vitro
Recombinant strain SL7207 (pVAX-M) was diluted 1:50 into 50 mL LB liquid medium containing kanamycin (100 μg/mL) and 50 mL LB kanamycin-free liquid medium, respectively. The bacteria culture containing plasmids in different conditions (with or without kanamycin) was taken 100 μL each to be appropriately diluted, respectively, at 3, 5, 7, 9, 12, 15, and 18 h. The dilution each of 100 μL was applied to three kanamycin-free LB plates and three LB plates containing kanamycin. After 16 h of culture colonies on the plate, colony counts were flat. According to [(the average number of colonies on the plate kanamycin LB)/(average number of colonies on the kanamycin-free LB plate)] × 100 %, calculate the resistance and the stability of the pressure in the recombinant plasmid of Salmonella non-resistant pressure under culture conditions.
RT-PCR detection for the transcription of M gene in vivo
Five-week-old mice were inoculated intragastrically with 1 × 109 CFU SL7207 (pVAX-M), and control mice were given the same dosage of SL7207 (pVAX). Three days after the immunization, Payer’s patches were removed from three mice and pooled. Cellular RNA was isolated from homogenized Payer’s patches with Beijing Tiangen total RNA extraction kit according to the manufacturer’s instructions. RT-PCR was used to amplify the full-length TGEV M gene with the primer pair as previously described.
Safety and bacterial colonization in organs
S. typhimurium strains SL7207 (pVAX-M) were cultured as described previously. The bacterial cells were collected after overnight growth by centrifugation at 5000×g for 10 min. The pellet was resuspended in PBS containing 5 % sodium bicarbonate (m/v). Three groups of 5-week-old BALB/c mice, each consisting of eighteen mice, were inoculated intragastrically using a gavage needle with SL7207 (pVAX-M) at the dosage of 5 × 108, 1 × 109, and 2 × 109 CFU [26] and boosted with the same dosage 2 weeks later. The immunized mice were monitored daily for clinical changes for 42 days. Three mice of each group were sacrificed to collect their spleens and livers every week post-immunization, and these organizations were homogenized in 2 mL PBS containing 0.1 % Triton (v/v). Bacterial counts were determined by plating 100 μL of the spleen or liver homogenates on LB agar plates containing 50 μg/mL kanamycin for overnight incubation and enumeration of colony-forming units. Bacterial colonies were picked randomly for PCR evaluation of TGEV M gene and digestion by restriction enzymes.
Mice immunization and sample collection
Five-week-old BALB/c mice were randomly divided into three groups with fifteen mice in each group, and immunized three times with 2-week intervals. All mice were deprived of food and water for 4 h before immunization. Mice in groups A and B were inoculated intragastrically with SL7207 (pVAX-M), and the control strain SL7207 (pVAX) with a dosage of 109 CFU per mouse. Group C mice received PBS as a negative control. Three mice from each group were sacrificed for sera and complete intestinal lavage collection at weeks 0, 2, 4, 6, and 8 after the primary immunization. Blood was obtained from the submaxillary sinus of the mice, and sera were obtained by centrifugation of the blood at 4 °C. Serum samples were stored in aliquots at −20 °C, prior to the experiments. To prepare intestinal fluid, the whole small intestine was removed from mouse and excess fat was removed, which was cut into pieces and then washed in 2 mL of PBS containing 100 μg/mL phenylmethylsulfonylfluoride (PMSF). Samples were centrifuged at 12,000×g for 20 min to remove cellular debris. The supernatant was freeze-dried using a freeze dryer and dissolved in 0.5 mL PBS containing 100 μg/mL PMSF. After centrifuged at 12,000×g for 15 min, the supernatant was collected as final intestinal lavage and stored at −20 °C prior to analysis.
Enzyme-linked immunosorbent assays
Serum IgG and intestinal IgA were determined by ELISA, and 96-well polystyrene microtitre plates (Costar) were coated overnight at 4 °C with 50 μL 5 μg/mL purified TGEV antigen, in carbonate buffer (pH 9.6), and blocked for 1 h at 37 °C with PBS containing 1 % BSA (w/v). Plates were then washed three times with PBS containing 0.02 % Tween 20 (PBST) and incubated with 100 μL of diluted mice serum or intestinal lavage samples for 1 h at 37 °C. After washed three times with PBST, HRP-conjugated goat anti-mice IgG or IgA (Sigma) diluted 1:2000 was used as the secondary antibody and incubated for 1 h at 37 °C. 3, 3′, 5, 5′-tetramethyl benzidine (TMB) was employed as the chromogenic substrate. The reaction was stopped after about 20 min of incubation in the dark by the addition of 50 μL 2 M H2SO4 at the room temperature, and the optical density was measured spectrophotometrically at 450 nm. Cytokine IL-4 and INF-γ were detected by mouse interleukin 4 (IL-4) ELISA kit (M4000B) and mouse interferon γ (INF-γ) ELISA kit (MIF00), respectively. All the steps were followed in the kits.
Statistical analysis
All data were mean ± SD from three independent experiments performed in triplicate. Results were analyzed by Student’s t test. A P value less than 0.05 was considered to be statistically significant.
Results
Construction and transient expression of pVAX-M in HEK-293 cells
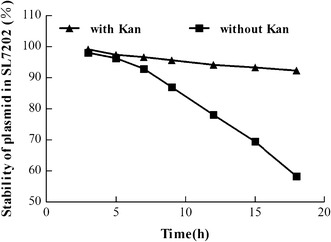
An approximately 1.0 kb DNA fragment was amplified by RT-PCR from TGEV SC-H strain, which was basically consistent with the expected length of M gene. Sequence analysis showed that the amplified TGEV SC-H strain M gene fragment was 989 bp in length containing the M gene’s open reading frame (789 bp) and encoded 262 amino acids. The result of sequence alignment showed that the predicted amino acid sequence of TGVE SC-H strain M gene fragment shared homology of 99.99 % with the sequence of TGEV Purdue strains. And the result showed that M gene fragment was successfully incorporated into pVAX1 vector by restriction analysis and PCR (Fig. 1). After transfection into HEK 293 cells, M gene detection by RT-PCR (Fig. 2) confirmed that the plasmids (pVAX-M) were eventually transfected into HEK 293 cell lines. Seventy-two hours after infection, the expression of TGEV M protein was detected via indirect immunofluorescence assay. And cyto-fluoresence was observed in HEK 293 cells transfected with pVAX-M (Fig. 3A), while not with pVAX (Fig. 3B). In the western blot assays, a specific strip of 29 kDa was observed in the expression product of pVAX-M with total TGEV-positive serum, which suggested that the eukaryotic plasmid pVAX-M could express M protein in HEK-293 cells (Fig. 4).
Fig. 1.
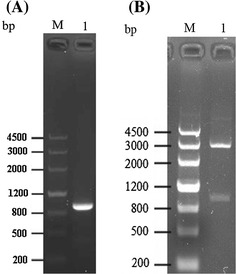
a PCR identification of pVAX-M. Lane M DNA Marker III; lane 1 M gene PCR products. b Identification by restriction analysis. Lane M DNA Marker III; lane 1 enzyme digestion products
Fig. 2.
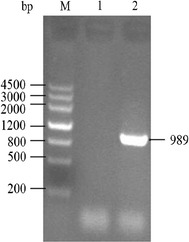
RT-PCR analysis of transcription of M gene in HEK 293 cells. Lane M DNA Marker III; lane 1 RT-PCR product of the control group of the empty plasmid pVAX; lane 2 RT-PCR products of the M gene of the recombinant plasmid pVAX-M
Fig. 3.
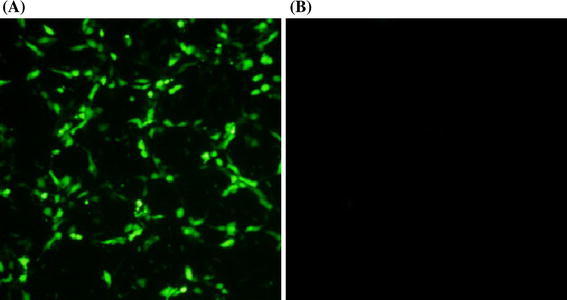
Expression of M protein in HEK 293 cells (×200). a Indirect immunofluorescence result of HEK 293 cells transfected with pVAX-M; b indirect immunofluorescence result of HEK 293 cells transfected with pVAX1
Fig. 4.
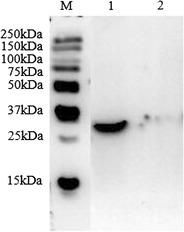
Analysis of M protein expression by Western blot. Lane M Precision Plus Protein™ WesternC™; lane 1 Western blot result of protein M; lane 2 Western blot result of pVAX1
Stability of recombinant bacteria SL7207 (pVAX-M) in vitro
The SL7207 (pVAX-M) were applied on LB solid medium containing kanamycin or free of kanamycin, and its colonies on the colony plate counts were calculated for each recombinant attenuated Salmonella at two different time points of medium carrying plasmid stability. The results showed that under conditions without antibiotics, recombinant attenuated Salmonella plasmid with recombinant bacteria proliferation rapidly lost, indicating that the recombinant plasmid in the absence of antibiotics is not stable enough; and under the conditions of antibiotics, recombinant attenuated Salmonella plasmid at 18 h after the culture is stable enough (Fig. 5).
Fig. 5.
Stability of plasmid in SL7207 when cultured in LB broth with (filled triangle) or without kanamycin (filled square)
Safety and colonization of recombinant S. typhimurium in organs
As for safety analysis, female BALB/c mice were inoculated orally with recombinant SL7207 (pVAX-M) at different dosages. No clinical aberrations were observed during the 6-week observation period except for being lassitude in the first day after gavage. The kinetics of bacteria colonization and persistence in vivo was investigated. Bacteria were isolated from liver and spleen of different dosage groups during weeks 1–5 post-inoculation, and the experiment suggested that they were eventually eliminated from liver and spleen at 6 weeks post-inoculation (Fig. 6). PCR result revealed the constant presence of M gene in recovered bacterial isolates (Fig. 7).
Fig. 6.
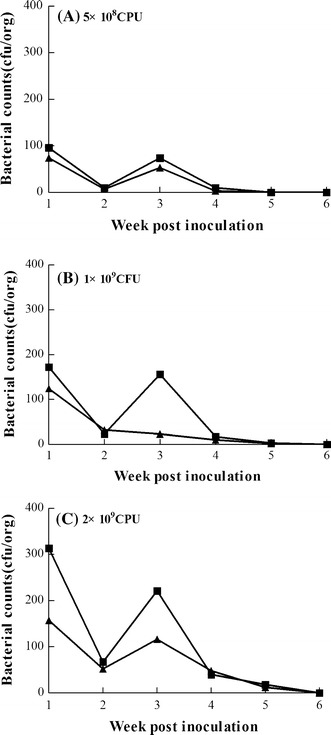
Bacterial colonization in organs. Persistence of the SL7207 (pVAX-M) in spleen (filled triangle) and liver (filled square) of mice inoculated orally with SL7207 (pVAX-M) at the dosage of 5 × 108 CFU (a), 1 × 109 CFU (b), and 2 × 109 CFU (c) and boosted with the same dosage 2 weeks later. Fresh spleens and livers were collected and homogenized in PBS for bacteria CFU determination on LB agar plates containing 50 μg/mL kanamycin every week
Fig. 7.
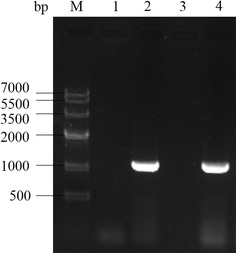
PCR identification of pVAX-M in organs. Lane M DNA Marker IV; lane 1 M gene PCR products of pVAX control group in spleen; lane 2 M gene PCR products of pVAX-M in spleen; lane 3 M gene PCR products of pVAX control group in liver; lane 4 M gene PCR products of pVAX-M in liver
Mucosal antibody responses induced by attenuated S. typhimurium harboring TGEV DNA vaccine
The ability of the recombinant S. typhimurium to induce a mucosal immune response was determined by measuring the level of IgA antibody to TGEV in intestinal lavage sample. As shown in Fig. 8, recombinant S. typhimurium induced detectable IgA antibodies to TGEV in mice as rapidly as week 2 post-vaccination. Considerably, enhanced antibody titers could be observed in group A, which received SL7207 (pVAX-M) at the dosage of 109 CFU, at week 4–6 post-immunization. The antibody level of group A was much higher than that of the SL7207 (pVAX) group (group B) (P < 0.05) and significantly greater than that of the PBS group (group C) (P < 0.01). Until the 8th week after the second immunization, the antibody level of group A was significantly higher than those of both groups B and C (P < 0.01).
Fig. 8.
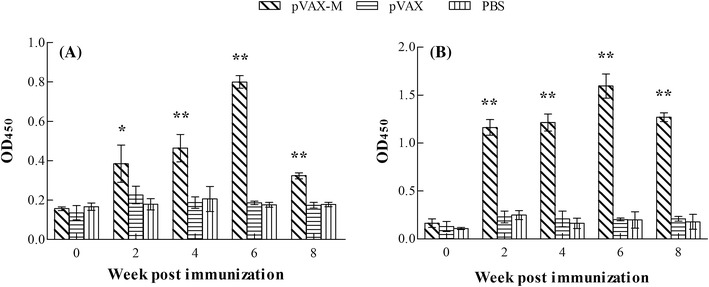
End-point dilution ELISA analysis of the anti-TGEV antibody in murine intestinal lavage or serum after immunization: a intestinal IgA and b serum IgG. Five-week-old BALB/c mice were inoculated intragastrically with SL7207 (pVAX-M) three times in 2-week intervals at a dosage of 109 CFU per mouse. Control mice received 109 CFU of SL7207 (pVAX), while PBS group mice received PBS as a negative control. Murine intestinal lavage and serum, collected at weeks 0, 2, 4, 6, and 8 post-immunization, were analyzed by end-point dilution ELISA assay using TGEV as a coating antigen. Absorbance was measured at 450 nm in an automated plate reader. Results are expressed as means of the OD 450 ± SD (n = 3). Numbers on x-axis indicate weeks post-immunization. ** stands for P < 0.01, * stands for P < 0.05
Humoral immune responses induced by attenuated S. typhimurium harboring TGEV DNA vaccine
The ability of the recombinant S. typhimurium to induce a humoral immune response was determined by measuring the level of IgG antibody to TGEV in serum sample. As shown in Fig. 8, none of the groups had any detectable antibody response at week 2 post-vaccination. Mice in group A, which received SL7207 (pVAX-M) at a dosage of 109 CFU, showed different levels of antibody response during the experiment. At week 6 post-immunization, the antibody titers generated in group A reached their peak. There were no detectable specific anti-TGEV antibodies in the SL7207 (pVAX) group (group B) and PBS group (group C) during experiment.
Expression levels of IL-4 and IFN-γ
IL-4 and IFN-γ standard curves were plotted according to the USA R&D system of mouse IL-4 and IFN-γ detection kit, respectively. Standard detection results of the regression equation of IL-4: y = 40.218x 2 + 11.623x + 5.638, R 2 = 0.9114, and the regression equation of the standard curve of IFN-γ: y = 253.98x 2 + 51.583x + 51.244, R 2 = 0.9433. The result was calculated by using curve equation concentration of the samples, and the contents change maps were shown in Fig. 9 IL-4 induced by recombinant SL7207 (pVAX-M) was detected on the 2nd week, which was higher than those by both SL7207 (pVAX) control group (P < 0.05) and PBS control group (P < 0.05); the maximum amount of IL-4 of the immune group was detected on the 6th week, and the content of IL-4 had significant differences (P < 0.01) in the two control groups. Figure 9 indicates that the content of IFN-γ of SL7207 (pVAX-M) was increased significantly on the 2nd week, maximized on the 6th week, and decreased on the 8th week. In the entire procedure of immunization, the immune SL7207 (pVAX-M) group performed significantly better (P < 0.01) than both SL7207 (pVAX) and PBS control groups. All the data indicate that the oral vaccine SL7207 (pVAX-M) could induce the body’s cellular immune response effectively in mice.
Fig. 9.
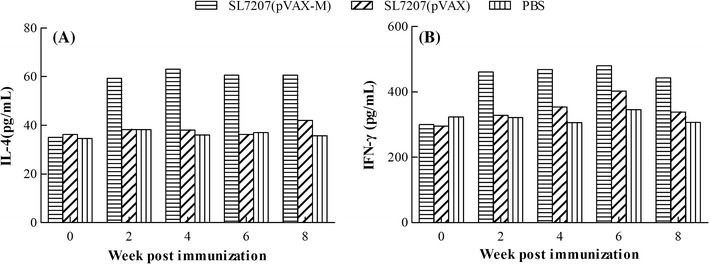
End-point dilution ELISA analysis of the a IL-4 and b IFN-γ in serum after immunization. The SL7207 (pVAX-M) group mice were inoculated as described in Fig. 8. The SL7207 (pVAX) group mice were used as control, while PBS group mice as a negative control
Discussion
TGE is an important viral disease infected through the intestinal mucosa. Secretory IgA (sIgA) induced resistance to infection by virus through the intestinal mucosa, while IgG and IgM provide little protection against these viruses. Thus, effective stimulation of the mucosal immune system to obtain mucosal immune response has important implications for the prevention and treatment of TGE. Current researches mainly focus on TGEV S and N genes, while there are only very few studies on the M gene, and we expressed TGEV M gene by the eukaryotic system for the first time. In this study, TGEV SC-H strain M with gene length of 989 bp was successfully amplified by RT-PCR including sequence of the open reading frame encoding 262 amino acids. The M gene was also detected by RT-PCR and M protein was detected by Western bolting and indirect immunofluorescence assays after eukaryotic expression plasmid (pVAX-M) transfected into HEK 293 cells, which aids a foundation for follow-up research.
New developments have focused on the production and delivery of the S protein through oral immunization. Several systems have been used to express the full-length or truncated TGEV S proteins such as Salmonella, Lactobacillus casei, and plants [11, 28, 34]. However, the expression level of antigen protein in transgenic plants is generally low and will lose its bioactivity due to the degradation of stomach acid [3, 10]. Live bacterial vectors offer many potential clinical advantages. They are stable, easy, and relatively inexpensive for mass production. They are also able to deliver multiple antigens. Oral delivery increases the safety and ease of administration. In addition, bacteria naturally possess immunostimulatory molecules such as lipopolysaccharide (LPS) that can function as an adjuvant to stimulate immune responses; furthermore, live bacterial vectors are able to induce systemic immune response, including humoral, cellular, and mucosal immunity against pathogen infection [24]. Our previous studies have shown that the expression of TGEV S gene delivered by attenuated S. typhimurium was detected in mouse peritoneal macrophages in vitro, so did the transcription of S gene in Payer’s patches in vivo. In this study, we constructed the attenuated S. typhimurium harboring TGEV M gene in the same method and detected the expression of M gene in the mouse terminal ileum. It suggested that the attenuated S. typhimurium SL7207 (pVAX-M) was practical being utilized as the oral delivery vector for TGEV DNA vaccine and the plasmids were passed to the body successfully.
Stable expression of antigen gene is extremely important for oral vaccine using attenuated Salmonella, as it relates to whether it could constantly effectively stimulate the body to produce an immune response. Studies affirmed that stability of plasmid might be relevant to the plasmid copy number [6], and ovalbumin expressed by an attenuated Salmonella harboring a low-copy number plasmid could stimulate to produce specific anti-ovalbumin (CTLs reaction) when carrying a high-copy number plasmid cannot [29]. In order to enhance plasmid stability during immunization, antibiotics were injected into the mice with the period of immunity, yet the result revealed that it is not practical to get the plasmids enhanced in vivo by this method [27]. In this study, stability of recombinant attenuated Salmonella vaccine SL7207 (pVAX-M) in vivo or in vitro was detected. The results showed that the bacteria were reduced to nearly 50 % without kanamycin resistance in the stability test in vitro during the 18 h observation. In safety study, neither deaths nor side effects were found in mice post-inoculation with attenuated S. typhimurium SL7207 (pVAX-M) at different dosages (5 × l08, 1 × 109, 2 × 109 CFU). No bacteria were recovered in liver and spleen in different dosage groups after 2 weeks of boosting, indicating that attenuated S. typhimurium could be eliminated by immune system after completing the plasmid delivery. At the same time, we noticed that one week after boosting, bacteria separated from liver and spleen in different dosage groups were significantly lower at the 3rd week after first inoculation, which indicated the elimination of immune system to bacterial enhanced with the increase of inoculation frequency. And 6 weeks after the first immunization, recombinant attenuated Salmonella were finally eliminated from the body, thus indicating that the strain of the SL7207 (pVAX-M) could exist steadily. All the results above indicate that the use of attenuated S. typhimurium is an ideal choice of delivery vector for DNA vaccine orally, concerning safety for livestock. Our data showed that the attenuated S. typhimurium SL7207 (pVAX-M) has relatively good safety for bodies.
The attenuated S. typhimurium SL7207 can induce sIgA due to colonization of the specific mucosal surface and internal organs [2], which has advantages of attenuated nature and propagation restrictions in vivo [30]. In the view of TGEV pathogenesis, livestock was infected by the virus through the digestive tract and it is difficult for bodies to gain protection by IgG antibody, therefore gut-specific sIgA antibodies produced by mammalian mucosal immune protection are more significant. In our study, after orally immunizing constructed DNA vaccine containing attenuated S. typhimurium SL7207 (pVAX-M), specific serum antibodies were detected at week 2 continuing into week 8, which has appeared (very) significantly when compared with SL7207 (pVAX) group and the PBS group. The levels of both IgG and IgA antibodies had a peak level at week 6, and then gradually decreased until week 8 the last week we detected. Using mice animal models, the experiments conducted in this study showed that the level of the antibodies of IgG and IgA immunized with SL7207 (pVAX-M) was higher than in those immunized with SL7207 (pVAX-S) which is consistent with previous results in attenuated S. typhimurium harboring TGEV S gene [33].
Detection of IFN-γ and cytokine IL-4 content is often used as an important indicator reflecting mouse cellular immunologic response. In addition, IFN-γ is representative of cytokines secreted by Thl cell cytokines, while IL-4 is secreted by Th2 cells. Yang found the CD4+ response stimulation after mice were inoculated orally with the attenuated S. typhimurium containing the surface protein of leishmania (gp63), and IFN-γ and IL-2 were discovered [32]. Sestak also found significantly increased IL-2-R expression on the mononuclear cells from the mesenteric lymph nodes after their stimulation with inactivated TGEV antigens in vitro with the decrease in the CD2–CD4–CD8– phenotype [25]. In this study, IL-4 and IFN-γ content of the animal body was also significantly improved, and SL7207 (pVAX-M) was significantly higher than SL7207 (pVAX) and PBS groups.
The present study has certain limitations: a vaccine which has good immune effect on the mouse model may not produce the same immune stimulating effect in pigs. Moreover, challenge protection test for the evaluation of the effect of a new vaccine is essential, but the test cannot be conducted on the species of mice. In this study, we constructed the SL7207 (pVAX-M) M gene of TGEV, and safety and immunogenicity were preliminarily assessed using mice animal models. TGEV easily infects clinically neonatal swine in 10 days which is prone to diarrhea in stress conditions. Attenuated Salmonella test results indicated that it can be released to carry the DNA vaccine in mice, and induce humoral immunity, mucosal immunity, and cellular immune responses. In our previous study, Zhang [35] immunized 20-day-old piglets by the SL7207 (pVAX-N) oral vaccine and the serum was first collected to detect IgG and IgA at week 2 post-immunization, and the result claimed that the experiment group (pVAX-N) is improved significantly contrasting with the control group (P < 0.05). Even if the vaccine of Zhang’s induced a good immune response, however, the best time of PEDV infection had passed in these piglets. However, the mouse model itself has advantages: reducing the costs of tests, requiring smaller cultured space, and shortening the period of immune response. Balb/C mice were immunized at doses which were 5 % and 10 % formulation administered in cattle to evaluate immunogenicity of the inactivated vaccine against food-and-mouth disease virus, and specific antibodies were detected in 14, 21, 28 days post-immunization which showed an adequate immune response to the vaccine with 10 % of the immunizing dose at the 21st day psot immunization [18]. Deng found that PCV-2b could be replicated in mice and caused mice tissue damages that has its similarity in tissue damage caused in pigs, indicating that mice could be used as animal models for research of the vaccine [5]. Gravier’s studies have claimed that DNA vaccines have similar biodistribution in mouse, rabbit, and pig tissues in vivo [9]. Our further studies will focus on effective evaluation of the oral vaccine, and pregnant sows were designed to be immunized by the SL7207 (pVAX-N) oral vaccine and their piglets within 10 days of age were chosen to perform challenge assay and neutralizing assay.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (31072144) and the Special Fund for Agro-scientific Research in the Public Interest (No. 201203056).
References
- 1.Cheng M, He J, Fu Y, Qiao W, Jiao Y. Antibody responses induced by mucosal DNA vaccine encoding the codon-optimized F protein of human respiratory syncytial virus (RSV) delivered with attenuated Salmonella typhimurium. Wei sheng wu xue bao = Acta Microbiol. Sin. 2011;51(7):965–971. [PubMed] [Google Scholar]
- 2.Darji A, Guzmán CA, Gerstel B, Wachholz P, Timmis KN, Wehland J, Chakraborty T, Weiss S. Oral somatic transgene vaccination using attenuated S. typhimurium. Cell. 1997;91(6):765–775. doi: 10.1016/S0092-8674(00)80465-1. [DOI] [PubMed] [Google Scholar]
- 3.Darji A, zur Lage S, Garbe AI, Chakraborty T, Weiss S. Oral delivery of DNA vaccines using attenuated Salmonella typhimurium as carrier. FEMS Immunol. Med. Microbiol. 2000;27(4):341–349. doi: 10.1111/j.1574-695X.2000.tb01448.x. [DOI] [PubMed] [Google Scholar]
- 4.de Haan CA, Smeets M, Vernooij F, Vennema H, Rottier PJ. Mapping of the coronavirus membrane protein domains involved in interaction with the spike protein. J. Virol. 1999;73(9):7441–7452. doi: 10.1128/jvi.73.9.7441-7452.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Deng ZB, Wang ND, Xu DJ, Yuan AW, Ge M, Luo W, Xue LQ, Yu XL. Viral distribution and lesions in Kunming mice experimentally infected with porcine circovirus type 2b. Vet. Res. Commun. 2011;35(3):181–192. doi: 10.1007/s11259-011-9461-2. [DOI] [PubMed] [Google Scholar]
- 6.Dunstan SJ, Simmons CP, Strugnell RA. In vitro and in vivo stability of recombinant plasmids in a vaccine strain of Salmonella enterica var. typhimurium. FEMS Immunol. Med. Microbiol. 2003;37(2–3):111–119. doi: 10.1016/S0928-8244(03)00065-8. [DOI] [PubMed] [Google Scholar]
- 7.Escors D, Ortego J, Enjuanes L. The membrane M protein of the transmissible gastroenteritis coronavirus binds to the internal core through the carboxy-terminus. Adv. Exp. Med. Biol. 2001;494:589–593. doi: 10.1007/978-1-4615-1325-4_87. [DOI] [PubMed] [Google Scholar]
- 8.Escors D, Ortego J, Laude H, Enjuanes L. The membrane M protein carboxy terminus binds to transmissible gastroenteritis coronavirus core and contributes to core stability. J. Virol. 2001;75(3):1312–1324. doi: 10.1128/JVI.75.3.1312-1324.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gravier R, Dory D, Laurentie M, Bougeard S, Cariolet R, Jestin A. In vivo tissue distribution and kinetics of a pseudorabies virus plasmid DNA vaccine after intramuscular injection in swine. Vaccine. 2007;25(39–40):6930–6938. doi: 10.1016/j.vaccine.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 10.Haneda T, Okada N, Kikuchi Y, Takagi M, Kurotaki T, Miki T, Arai S, Danbara H. Evaluation of Salmonella enterica serovar Typhimurium and Choleraesuis slyA mutant strains for use in live attenuated oral vaccines. Comp. Immunol. Microbiol. Infect. Dis. 2011;34(5):399–409. doi: 10.1016/j.cimid.2011.07.001. [DOI] [PubMed] [Google Scholar]
- 11.Ho PS, Kwang J, Lee YK. Intragastric administration of Lactobacillus casei expressing transmissible gastroenteritis coronavirus spike glycoprotein induced specific antibody production. Vaccine. 2005;23(11):1335–1342. doi: 10.1016/j.vaccine.2004.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hur J, Lee JH. Immune responses to new vaccine candidates constructed by a live attenuated Salmonella typhimurium delivery system expressing Escherichia coli F4, F5, F6, F41 and intimin adhesin antigens in a murine model. J. Vet. Med. Sci./Jpn. Soc. Vet. Sci. 2011;73(10):1265–1273. doi: 10.1292/jvms.11-0087. [DOI] [PubMed] [Google Scholar]
- 13.Jiang P, Jiang W, Li Y, Wu S, Xu J. Humoral immune response induced by oral administration of S. typhimurium containing a DNA vaccine against porcine reproductive and respiratory syndrome virus. Vet. Immunol. Immunopathol. 2004;102(3):321–328. doi: 10.1016/j.vetimm.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 14.Kotton CN, Lankowski AJ, Scott N, Sisul D, Chen LM, Raschke K, Borders G, Boaz M, Spentzou A, Galan JE, Hohmann EL. Safety and immunogenicity of attenuated Salmonella enterica serovar typhimurium delivering an HIV-1 Gag antigen via the Salmonella Type III secretion system. Vaccine. 2006;24(37–39):6216–6224. doi: 10.1016/j.vaccine.2006.05.094. [DOI] [PubMed] [Google Scholar]
- 15.Kweon CH, Kwon BJ, Lee JG, Kwon GO, Kang YB. Derivation of attenuated porcine epidemic diarrhea virus (PEDV) as vaccine candidate. Vaccine. 1999;17(20–21):2546–2553. doi: 10.1016/S0264-410X(99)00059-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Laviada MD, Videgain SP, Moreno L, Alonso F, Enjuanes L, Escribano JM. Expression of swine transmissible gastroenteritis virus envelope antigens on the surface of infected cells: epitopes externally exposed. Virus Res. 1990;16(3):247–254. doi: 10.1016/0168-1702(90)90051-C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leman AD, Straw B, Mengeling WL, Taylor DJ, editors. Diseases of Swine. 8. Ames: Iowa State University Press; 1999. [Google Scholar]
- 18.Molin-Capeti KC, Sepulveda L, Terra F, Torres-Pioli MF, Costa-Casagrande T, Franca SC, Thomaz-Soccol V. A proposal for an alternative quality control test procedure for inactivated vaccines against food-and-mouth disease virus. Vaccine. 2013;31(9):1349–1352. doi: 10.1016/j.vaccine.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 19.Pesciaroli M, Aloisio F, Ammendola S, Pistoia C, Petrucci P, Tarantino M, Francia M, Battistoni A, Pasquali P. An attenuated Salmonella enterica serovar typhimurium strain lacking the ZnuABC transporter induces protection in a mouse intestinal model of Salmonella infection. Vaccine. 2011;29(9):1783–1790. doi: 10.1016/j.vaccine.2010.12.111. [DOI] [PubMed] [Google Scholar]
- 20.Riffault S, Grosclaude J, Vayssier M, Laude H, Charley B. Reconstituted coronavirus TGEV virosomes lose the virus ability to induce porcine interferon-alpha production. Vet. Res. 1997;28(1):77–86. [PubMed] [Google Scholar]
- 21.Risco C, Anton IM, Enjuanes L, Carrascosa JL. The transmissible gastroenteritis coronavirus contains a spherical core shell consisting of M and N proteins. J. Virol. 1996;70(7):4773–4777. doi: 10.1128/jvi.70.7.4773-4777.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Risco C, Anton IM, Sune C, Pedregosa AM, Martin-Alonso JM, Parra F, Carrascosa JL, Enjuanes L. Membrane protein molecules of transmissible gastroenteritis coronavirus also expose the carboxy-terminal region on the external surface of the virion. J. Virol. 1995;69(9):5269–5277. doi: 10.1128/jvi.69.9.5269-5277.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Saif LF, Bohl EH. Immunoglobulin classes of antibodies in milk of swine after intranasal exposure to pseudorabies virus or transmissible gastroenteritis virus. Infect. Immun. 1977;16(3):961–966. doi: 10.1128/iai.16.3.961-966.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schoen C, Stritzker J, Goebel W, Pilgrim S. Bacteria as DNA vaccine carriers for genetic immunization. Int. J. Med. Microbiol. 2004;294(5):319–335. doi: 10.1016/j.ijmm.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 25.Sestak K, Meister RK, Hayes JR, Kim L, Lewis PA, Myers G, Saif LJ. Active immunity and T-cell populations in pigs intraperitoneally inoculated with baculovirus-expressed transmissible gastroenteritis virus structural proteins. Vet. Immunol. Immunopathol. 1999;70(3–4):203–221. doi: 10.1016/S0165-2427(99)00074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stocker BA. Aromatic-dependent salmonella as anti-bacterial vaccines and as presenters of heterologous antigens or of DNA encoding them. J. Biotechnol. 2000;83(1–2):45–50. doi: 10.1016/S0168-1656(00)00297-2. [DOI] [PubMed] [Google Scholar]
- 27.Tarkka E, Muotiala A, Karvonen M, Saukkonen-Laitinen K, Sarvas M. Antibody production to a meningococcal outer membrane protein cloned into liv Salmonella typhimurium aroA vaccine strain. Microb. Pathog. 1989;6(5):327–335. doi: 10.1016/0882-4010(89)90074-0. [DOI] [PubMed] [Google Scholar]
- 28.Tuboly T, Yu W, Bailey A, Degrandis S, Du S, Erickson L, Nagy E. Immunogenicity of porcine transmissible gastroenteritis virus spike protein expressed in plants. Vaccine. 2000;18(19):2023–2028. doi: 10.1016/S0264-410X(99)00525-3. [DOI] [PubMed] [Google Scholar]
- 29.Turner SJ, Carbone FR, Strugnell RA. Salmonella typhimurium delta aroA delta aroD mutants expressing a foreign recombinant protein induce specific major histocompatibility complex class I-restricted cytotoxic T lymphocytes in mice. Infect. Immun. 1993;61(12):5374–5380. doi: 10.1128/iai.61.12.5374-5380.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weiss S. Transfer of eukaryotic expression plasmids to mammalian hosts by attenuated Salmonella spp. Int. J. Med. Microbiol. 2003;293(1):95–106. doi: 10.1078/1438-4221-00248. [DOI] [PubMed] [Google Scholar]
- 31.Wu GP, Yin YB, Wu SY. Research on porcine transmissible gastroenteritis virus (TGEV) Chin. J. Vet. Med. 2003;39(2):29–31. [Google Scholar]
- 32.Yang DM, Fairweather N, Button LL, McMaster WR, Kahl LP, Liew FY. Oral Salmonella typhimurium (AroA-) vaccine expressing a major leishmanial surface protein (gp63) preferentially induces T helper 1 cells and protective immunity against leishmaniasis. J. Immunol. 1990;145(7):2281–2285. [PubMed] [Google Scholar]
- 33.Yang H, Cao S, Huang X, Liu J, Tang Y, Wen X. Intragastric administration of attenuated Salmonella typhimurium harbouring transmissible gastroenteritis virus (TGEV) DNA vaccine induced specific antibody production. Vaccine. 2009;27(37):5035–5040. doi: 10.1016/j.vaccine.2009.06.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang H, Liu J, Cao S, Huang X, Wen X. [Construction, safety and immunogenicity analysis of attenuated Salmonella typhimurium harbouring TGEV DNA vaccine. Wei sheng wu xue bao = Acta Microbiol. Sin. 2009;49(1):72–77. [PubMed] [Google Scholar]
- 35.Zhang D, Huang X, Zhang X, Cao S, Wen X, Wen Y, Wu R, Liang E. Construction of an oral vaccine for transmissible gastroenteritis virus based on the TGEV N gene expressed in an attenuated Salmonella typhimurium vector. J. Virol. Methods. 2016;227:6–13. doi: 10.1016/j.jviromet.2015.08.011. [DOI] [PubMed] [Google Scholar]


