Abstract
Objective:
In a previous report on a randomized clinical trial of a 3-month program of Cognitive Remediation Therapy (CRT) augmented by work therapy (WT) compared with WT alone for older Veterans with substance use disorder (SUD), we reported significantly greater improvements at six- month follow-up on neurocognitive outcomes of working memory and executive functions for the CRT+WT condition. However, no difference was found between conditions on substance use disorder (SUD) outcomes, with both groups showing unusually high levels of abstinence. In the present study, we extended follow-up to 12 months to test whether there was an SUD outcome “sleeper effect” from CRT+WT. To better understand the effects of WT, we added a treatment-as-usual (TAU) comparison sample.
Method:
48 Veterans with SUD receiving standard outpatient VA care were randomized into CRT+WT or WT. Clinical Global Impression (CGI) ratings were performed on 43/48 participants with up-to-date medical records. TAU comparison group (n = 44) with similar demographic and illness characteristics was added to the analysis.
Results:
Treatment groups did not differ significantly at 12 months on CGI (p=.27), with 77% receiving CRT+WT showing favorable SUD outcomes compared to 62% in WT. Both groups had better CGI outcomes (p<.01) compared to the TAU comparison group (27%). Hours of WT participation WT (r = −0.49, p=0.001) and hours of CRT (r = −0.45, p=0.048) were associated with better CGI scores.
Conclusion:
While no sleeper effect was found for CRT, robust effect for WT on SUD outcomes was strongly supported.
Keywords: Cognitive Remediation, Work Therapy, Clinical Global Impression, Substance Use Disorder, Older Veterans
1. Introduction:
We previously reported (Bell et al., 2017) on neurocognitive and substance use outcomes of an RCT that compared 3-months of Cognitive Remediation Therapy with Work Therapy (CRT+WT) to Work Therapy (WT) alone in a sample of Veterans who were mostly in their early 50’s and in the early phase of outpatient Substance Use Disorder (SUD) treatment. Our rationale for using CRT, which employed cognitive training software developed by Posit Science (Brain HQ), was to address the neurocognitive deficits in SUD that may hinder rehabilitation, and our rationale for combining it with WT, paid work in accommodating placements on the VA medical center campus, was to increase the generalization of cognitive gains as we had found in our research using this approach in schizophrenia studies (e.g. Bell et al., 2007, 2008). We also thought that WT would sustain engagement in the study, which is often a problem in outpatient SUD research. We used WT as an active control for our CRT+WT, since WT had previous support for efficacy from a study of SUD outcomes in VA residential programs that involved WT (Rosenheck & Seibyl, 1997) and in programs with homeless Veterans (Kashner et al., 2002).
As expected, our initial analyses revealed high baseline rates of cognitive impairment, with 87.5% of the sample showing significant decline from premorbid IQ on at least 1 measure, and with participants averaging significant decline on 3 out of 14 measures. Adherence to the research intervention was excellent and follow-up rates were 95.7% at 3 months and 87.5% at 6 months. Mixed effects models of cognitive change over 6 months revealed significant differences favoring CRT+WT on working memory and executive function indices. However, no differences were found between conditions on substance use outcomes as WT alone was highly effective. CRT+WT had a mean of 97% days of abstinence at 3 months, 94% in the 30 days prior to 6-month follow-up, and 24/26 weeks of total abstinence. WT had only slightly worse SUD outcomes at 3 months with a mean of 87% days of abstinence, but they also had 94% days of abstinence in the 30 days prior to 6-month follow-up and averaged 24/26 weeks of total abstinence.
These outcomes compare favorably to substance use outcomes that have been reported in other outpatient studies of substance abuse. For example, a recent secondary analysis of large RCT’s of alcohol pharmacotherapy trials (Falk et al., 2019) reported that in the last 4 weeks of the trials the placebo groups (n = 588) and the medication groups (n = 563) had respectively 16% (n =94) and 22.7% (n = 128) abstinence rates and 29.3% (n = 172) and 36.8% No Heavy Drinking Day rates across the trials. A VA study that followed 298 subjects from a 21-day inpatient Alcohol Treatment Unit (Curran et al., 2000) over 12 months reported 56.1% continuous abstinence at 3 months, 38.6% at 6 months, 30.5% at 9 months and 26.2% at 12 months.
Meta-analysis of CRT findings with seriously mentally ill samples have suggested that the impact of CRT on functional outcomes after treatment may increase over time, a so-called “sleeper-effect” (Wykes et al., 2011; Vinogradov, 2019). The tentative explanation for the “sleeper effect” is that neurocognitive gains build the capacity for increased competency, but it takes much longer for skills to be acquired even after the ability to acquire them has increased. Extending this logic to SUD outcomes, it is possible that better neurocognitive ability increases the capacity to acquire and apply recovery skills. To test the hypothesis that the CRT+WT condition will show better substance use outcomes over time compared to WT, we used a retrospective chart review, creating a Clinical Global Impression (CGI) scale that would allow raters, blind to condition, to determine the overall SUD outcome of our participants 12 months following entry into the study (9 months after active intervention and 6 months after the last in-person follow-up).
After testing this hypothesis, we extended the same method to a carefully selected comparison sample from the same time and initial SUD treatment cohort that did not enroll in the research study and went on to receive treatment as usual (TAU) for 12 months. Although this TAU sample is post-hoc and not randomized to condition, it provides some basis for evaluating the role that WT may play in substance use recovery. We hypothesized that those receiving WT in either randomized condition, i.e. either alone or in combination with CRT (n = 43) would have better 12-month CGI scores than those in the TAU comparison group (n = 44).
2. METHOD
2.1. Participants:
Study Groups:
Veterans 18 years and older who received treatment by a substance abuse treatment clinician, mostly while enrolled in a 21-day substance abuse day program (SADP) at the Veterans Affairs Connecticut Healthcare System (VACHS), West Haven, CT, were recruited for the RCT. Recruitment began in 2011 and was completed in 2014. Eighty-seven Veterans were consented and assessed for eligibility based on the presence of SUD and detoxification within the past 30 days. Exclusion criteria included untreated psychotic disorder, current use of opioids, a legal case that might lead to incarceration, a living arrangement that would interfere with participation, and the presence of a developmental disability or medical illness that might significantly compromise cognition or prevent work activity. Of the 87 Veterans assessed, 10 did not meet the criteria, 6 declined to complete the intake, and 23 were excluded for other reasons (e.g., moving away or participating in other vocational programs that were not part of the study). The final study sample consisted of 48 participants who completed the intervention. Study participants were randomized to receive up to 20 hours of either CRT+WT or WT (see Bell et al., 2016 for complete methodological description). Of the 48 participants, 43 had sufficient information in the electronic medical records to allow a comprehensive review of their SUD course over 12 months from their date of study entry. Reasons for incomplete medical records for 4 participants included relocation, incarceration and death from an unrelated medical condition.
TAU Comparison Group:
We obtained a waiver of informed consent and HIPAA authorization to examine VACHS medical records of a historical cohort of Veterans who met the same criteria as those in the RCT, and received SADP treatment at the same time, but who did not enroll in the study, and who did not participate in WT or another VA work therapy program or receive cognitive remediation as a clinical service. Three hundred thirteen Veterans were identified as potential members of the TAU comparison group. To reduce any selection bias, individuals were randomly selected and were included if they had records spanning a 12-month period after discharge from SADP. Random selection was performed by splitting the alphabetical list of names into 7 equal parts and then randomly selecting one record from each part until 44 participants meeting these criteria were identified. All participants in RCT and the TAU comparison group had VACHS services available to them throughout the 12-month follow-up period. Services included supported housing, community reintegration programs, primary care clinics, specialized medical care and outpatient mental health and substance abuse counseling.
2.2. Measures:
The Clinical Global Impression Scale:
The CGI is a well-established approach in clinical trials recommended by National Institute of Mental Health (NIMH) to provide a brief, stand-alone assessment of the clinician’s view of the patient’s global functioning (Busner et al., 2007). A 7-point CGI scale was created to capture levels of recovery as recorded in medical records. Levels were based on broadly accepted standards of recovery including number of relapses, quality of life (including stable housing, personal finances, and personal support structure), and commitment to recovery-oriented treatments as demonstrated by reliable attendance for SUD treatment as well as medical and mental health appointments over the course of recovery. See Table 1 for CGI scoring levels.
Table 1:
CGI Scoring Guidelines
| Score | Guidelines |
|---|---|
| 1 | Had no relapse during entire 12-months after entry into the study. No quality of life issues such as unstable housing, arrests or loss of social support. |
| 2 | Had no relapse in the 12 months after entry into the study. Limited quality of life issues. |
| 3 | Had relapse limited to a few days with no emergency treatment in either first 6 months of follow-up or the subsequent 6 months of follow but not in both. Actively seeking medical or mental health help for sobriety. Has quality of life issues but is seeking help. |
| 4 | Had relapse limited to a few days with no emergency treatment in either first 6 months of follow-up or the subsequent 6 months of follow but not in both. Using one or more substances. Has quality of life issues, missing medical or mental health appointments. |
| 5 | Had relapse limited to a few days with no emergency treatment in both the first 6 months of follow-up and the subsequent 6 months of follow-up. Using one or more substances. Required medical and psychological intervention, but not emergency room (ER) supports for major health or drug abuse issues. Individual has quality of life issues. |
| 6 | Had repeated relapses during the 12-month follow-up. Using one or more drugs. Required medical and psychological interventions. Required ER services related to drug use. Quality of life is in decline |
| 7 | Had repeated relapses during the 12-month follow-up. Using multiple drugs. Required ER support directly related to drug use. Quality of life is in major decline. |
2.3. Procedures:
Recruitment and Interventions
Details of recruitment and intervention procedures for the RCT can be found in the previous published article (Bell, et al., 2017). Briefly, recruitment was by clinical referral of newly relapsed patients mostly from a 21-day substance abuse day program. After informed consent, baseline assessments were obtained, and block randomization assured approximately equal distribution to the two arms of the study. No attempt was made to stratify by type of primary diagnosis, but type of SUD was similarly distributed between the two conditions.
Those assigned to CRT+WT could train up to 5 hours per week for 13 weeks using auditory and visual Posit Science software. At that time Posit Science offered two separate but complete suites of training software on CD’s, one called Brain Fitness (auditory) and the other Insight (visual). Training games began with the most elementary sensory processing tasks (i.e. auditory or visual sweeps) and progressed through a pre-set curriculum of more and more complex and demanding games. The software also recorded total time in minutes of computer training, which we converted into Hours of CRT as a variable for regression analysis.
In addition to the cognitive training, they participated in WT for up to 15 hours per week doing entry level duties at medical center job sites supervised by regular medical center staff. They also participated in group sessions for 30 minutes per week to receive support and encouragement and discuss issues in the workplace. Participants in the Work Therapy Only (WT) condition could receive up to 20 hours per week of work therapy as well as participate in the same weekly group sessions as those in CRT+WT. Participants in the WT condition did not complete any cognitive training. Participants received payment of half federal minimum wage (according to VA regulations) for their hours of productivity whether in CRT+WT or WT. Paid Hours of WT were recorded in our database as a variable for regression analysis.
Clinical Global Impression (CGI) Ratings
Medical information was extracted from the records for the 12-month follow-up period of 43 Veterans from the RCT. Four raters, blind to condition, were trained on the CGI scale and then independently rated 15 medical records. Inter-rater reliability was excellent (ICC r = .95), and the remaining medical records were then rated with occasional consensus rating when one of the raters was uncertain. Medical record information was also extracted and rated for the 44 participants who did not receive CRT or WT and who comprised the TAU group. Ratings could not be blinded for the TAU group because these charts were rated after the RCT group ratings and because research alerts regarding study participation were part of the medical record.
2.4. Statistical Methods:
Demographic variables were summarized and compared between groups using chi-square tests for categorical variables and ANOVA for continuous variables. The primary outcome was a favorable SUD outcome defined by a 12-month CGI score ≤3. This cut-off allowed for inclusion of participants with a CGI score = 3, who may have had a relapse in the early phase of recovery but who had a positive course of recovery and a sustained commitment to treatment. Logistic regression was used to evaluate the effect of condition on the odds of improvement. Demographic variables were considered in the models but did not appreciably affect estimates of treatment effects and were therefore dropped for parsimony. Continuous CGI scores were also considered as an outcome and compared among groups using t-tests and ANOVA. All tests were two-sided and used an α = 0.05 threshold for determining significance. All data were analyzed using SAS, version 9.4 (Cary, NC).
3. RESULTS
3.1. Demographic Characteristics:
Demographic characteristics for RCT groups and the TAU comparison group are presented in Table 2. Across groups, participants were, on average, slightly older than 50 years, and predominantly men with alcohol use disorder (AUD). None of the participants, including those in the TAU comparison group, were employed in the 30 days prior to SUD treatment participation, suggesting that immediate return to work was not a major part of their recovery plan. While African Americans were equally represented in each condition, Caucasians represented 29% of participants in the WT condition versus 50% and 66% in the WT+CRT condition and TAU comparison group, respectively. Otherwise, selection and randomization procedures for the TAU comparison group succeeded in matching the demographic characteristics of the RCT conditions. In particular, age, gender and rates of primary alcohol use were very similar for all groups.
Table 2:
Subject Demographics by Condition
| Variable | WT (n=21) | CRT+WT (n=22) |
TAU Comparator (n=44) | PFisher |
|---|---|---|---|---|
| Male, n (%) | 20 (95%) | 20(91%) | 41 (93%) | 1 |
| Race | ||||
| Caucasian | 6 (29%) | 11(50%) | 29 (66%) | 0.014 |
| African American | 11 (52%) | 11(50%) | 13 (30%) | |
| Other | 4 (19%) | 0 (0%) | 2 (4%) | |
| Substance Use | ||||
| Alcohol | 11 (52%) | 10(45%) | 21 (48%) | 0.27 |
| Marijuana/Cannabis | 2 (10%) | 2 (9%) | 1 (2%) | |
| Cocaine | 2 (10%) | 2 (9%) | 8(18%) | |
| Opioid | 0 (0%) | 5 (23%) | 4 (9%) | |
| Polysubstance | 6 (29%) | 3 (14%) | 10 (23%) | |
| Age, mean ± SD | 53.8 ±7.9 | 52.0 ±9.0 | 50.3 ± 10.5 | 0.38 |
3.1. RCT at 12-Month Follow-up:
Distributions of CGI scores are depicted in Figure 1. With cut-off of 12-month CGI scores ≤3, 62% of participants receiving WT alone showed good SUD outcomes. As shown, augmentation with CRT increased favorable outcome rates to 77%, though did not differ significantly from WT alone (OR=2.1; 95% CI: 0.55 – 7.9; p=0.27). Total hours of work was associated with lower (better outcome) CGI scores among both groups (r = −0.49, p=0.001), while among CRT+WT participants, hours of cognitive training also suggested added benefit (r = −0.45, p=0.048). Indeed, a logistic regression revealed that for each additional hour of cognitive training performed, odds of improvement increased by a factor of 7.0% (OR=1.07; 95% CI: 0.99 – 1.15; p=0.08). Using CGI as a continuous scale, average CGI scores did not differ (p=0.65) between CRT+WT (Mean = 2.36 (1.76)) and WT alone (Mean = 2.62 (1.94)).
Figure 1.
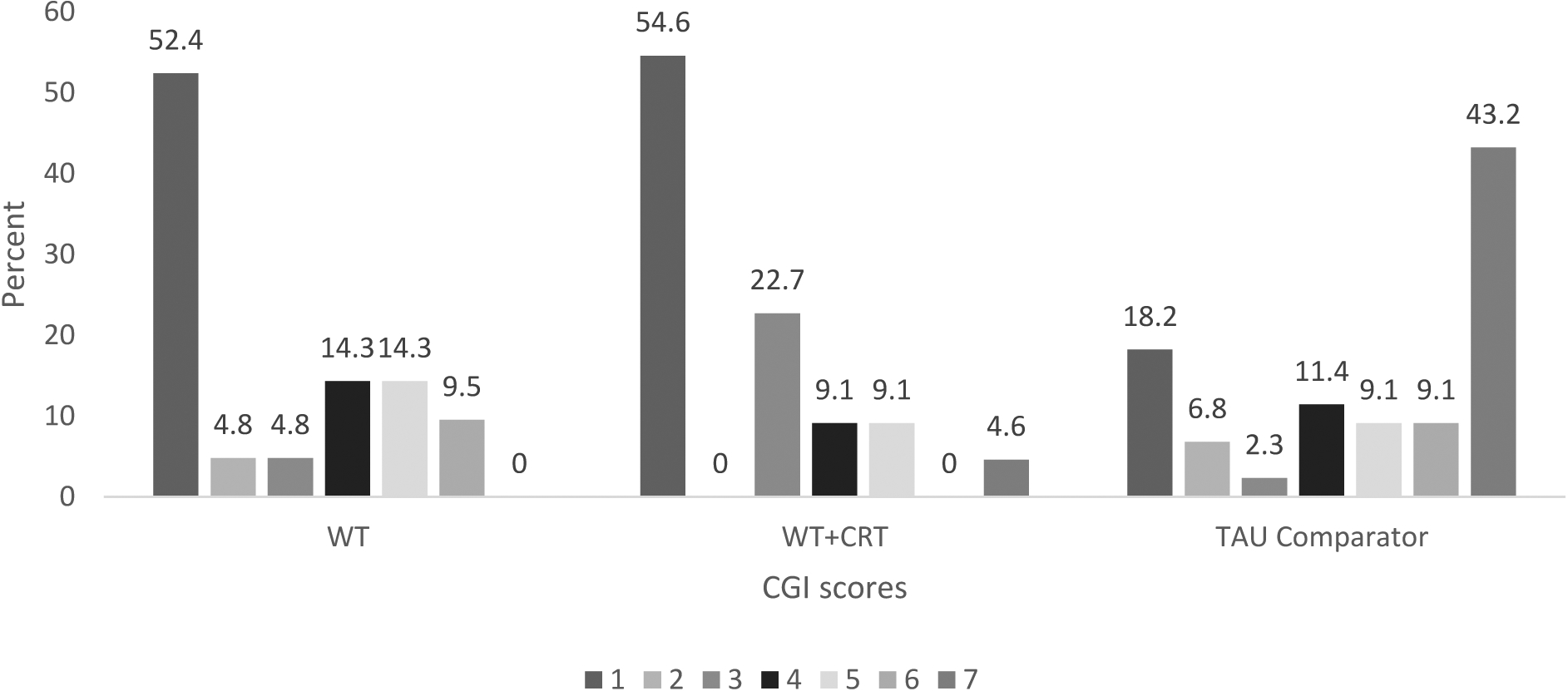
CGI score distribution for WT, CRT+WT and TAU comparison group
3.2. TAU Comparison group:
Only 27% of the TAU comparison group showed good SUD outcomes defined as 12-month CGI scores ≤3 (see Figure 2). The overall condition effect was significant (X2(2) = 15.2, p=0.0005) in a logistic regression comparing odds of improvement between WT alone and CRT+WT relative to the TAU comparison group. Specifically, both WT (OR=4.33; 95% CI: 1.43 – 13.1; p=0.009) and WT+CRT (OR=9.07; 95% CI: 2.74 – 30.0; p=0.0003) significantly increased odds of improvement compared to those in the TAU comparison group. Using CGI as a continuous variable, average CGI scores (Mean = 4.86 (2.38)) were significantly greater (worse) for the TAU comparison group relative to both experimental conditions (p<.001). Moreover, in the TAU condition, only 25% sustained sobriety (CGI ratings of 1 or 2); see Figure 1) compared with 54.6% in CRT+WT and 57.2% in WT alone.
Figure 2.
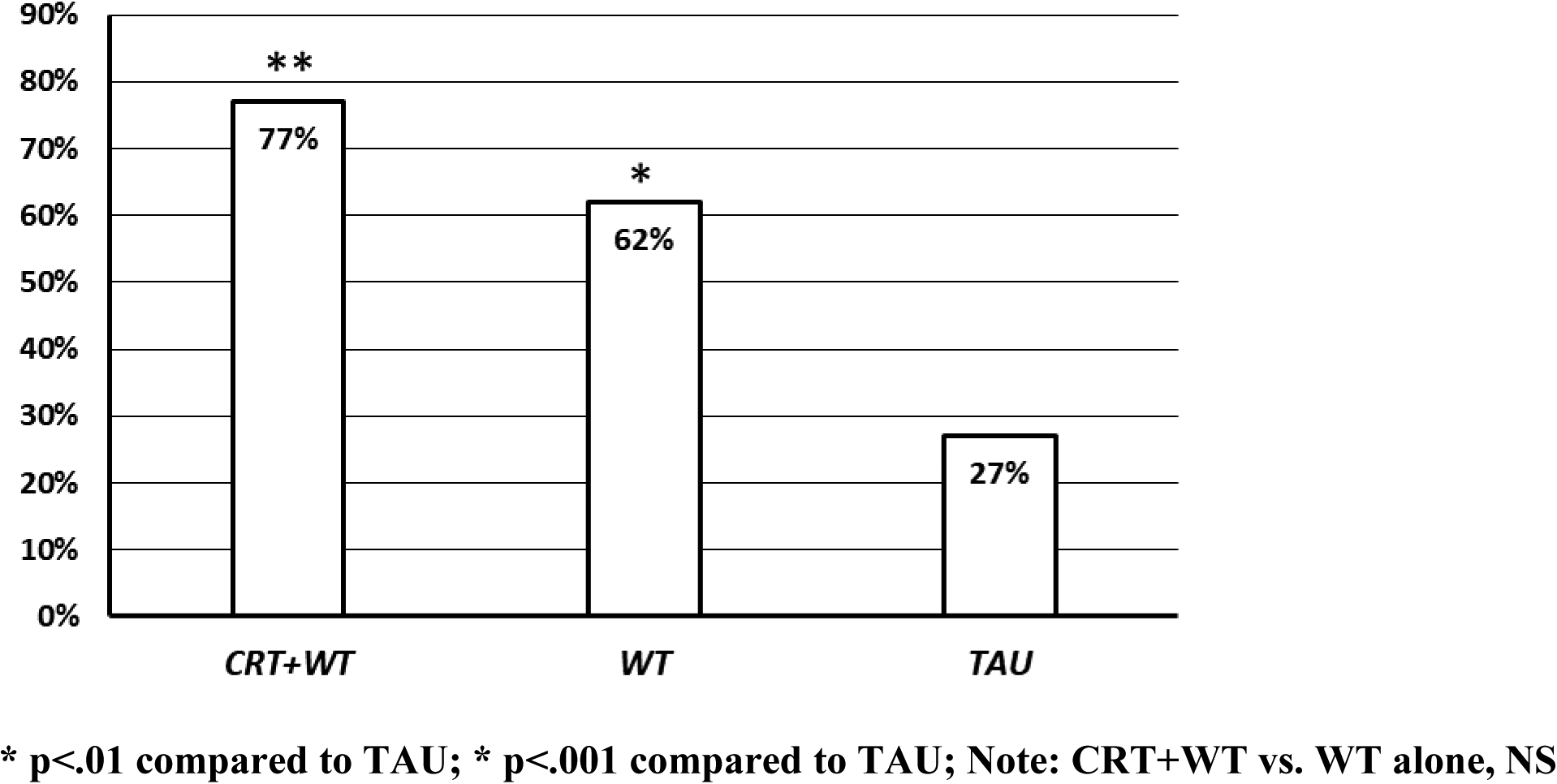
Distribution of Good Clinical Outcome (CGI ≤ 3) by Treatment Condition
4. DISCUSSION
The first aim of the study was to compare SUD outcomes in RCT participants 12 months after study entry to test the hypothesis that there may be additional SUD benefits over time (a sleeper effect) for those in the CRT+WT condition. We found that while at 12 months a higher percentage of CRT+WT participants had favorable 12-month outcomes compared to those in WT alone (77% vs. 62%), the two conditions did not differ significantly (p = .27). This trend level difference suggesting some additional benefit from CRT is supported by our finding a significant relationship between hours of cognitive remediation and CGI scores, with 7% increase in likelihood of a more favorable CGI for every hour trained.
Although the RCT conditions did not differ significantly on our measure of SUD recovery, both conditions appeared to have benefited from participation in WT. We found that total hours of WT was associated with better CGI scores in both groups, supporting the conclusion that engaging in WT regardless of other treatments, including CRT, is associated with better SUD outcomes. Moreover, about two thirds had a favorable SUD course (WT = 62%, CRT+WT = 77%), and more than half the participants in each condition had sustained sobriety without any relapse (CGI ratings of 1 or 2; WT = 57.2%, CRT+WT = 54.6%) which is higher than the 26.2% previously reported for those undergoing standard SUD and other VA treatment (Curran et al., 2000).
In order to have a more direct comparison sample with similar characteristics, we examined the medical records of Veterans who had completed the 21-day SADP program during the same time period as those who entered our study and met the same recruitment criteria. Our random selection of medical records from that sample appears to have produced a well-matched comparison group, similar in age, gender, and type of SUD. We found that only 25% had sustained sobriety over 12 months (CGI ratings of 1 or 2) and only 27% (Figure 1) of the participants in this TAU comparison group had a favorable SUD course (Figure 2). This low rate of sustained recovery is similar to what was reported in the Curran study of Veterans with AUD (Curran et al., 2000) and the Falk meta-analysis of drug trials for AUD (Falk et al., 2019). A recent report (Cripe & Cooper, 2019) of a quasi-experimental study of an SUD sample in residential and then outpatient treatment found 18-month follow-up sustained sobriety rates of 31% in their TAU condition (N = 50).
There has been very little formal examination of the benefits of WT for SUD populations. However, a work-structured day has long been a staple of residential programs and therapeutic communities (e.g. Second Genesis, Phoenix House, Daytop Village). In their meta-analysis, Rosenheck & Seibyl (1997) found support for the therapeutic benefit of WT, and Kashner et al., (2002) reported on a multi-site VA RCT of the health benefits of Compensated Work Therapy (CWT) for homeless Veterans with SUD. In that study, those randomly assigned to CWT reported greater use of SUD treatment services and immediate reductions in alcohol and substance use (45%), though reductions declined over the 1-year follow-up. Authors concluded that CWT was associated with fewer problems associated with substance use including homelessness and incarceration. In an earlier study in which homeless substance abusers were randomized to TAU or a day treatment with abstinence-contingent work therapy, Milby and colleagues (1996) concluded that day treatment plus drug-free work therapy and housing components may be more effective than usual care in producing clinically significant reductions in alcohol and cocaine use, and homelessness.
From our findings and these previous reports, it appears that work therapy may be an under-utilized service with significant benefit for SUD populations pursuing recovery. Particularly in older Veterans, many of whom are no longer seeking employment because of their age, physical condition or disability status, a work therapy program which pays them a modest amount for part-time work in an accommodating setting appears to add substantially to their recovery. Remarkably, participants were exposed to WT in our study for only 3 months, yet they continued to have a better course of recovery than those in the TAU comparison group over the next 9 months. Our limited data do not provide an explanation for this effect, but we did find a relationship between greater WT participation and CGI scores, suggesting that more engagement in WT had lasting benefits.
4.1. Limitations:
We recognize that there are a number of limitations to our methods. First, since we began by comparing the RCT conditions and then subsequently added the TAU comparison group, individual raters were only blinded for the RCT samples and not the TAU comparison sample. While SUD outcome for the TAU comparison group is like that which is found in the literature, unconscious bias in CGI ratings cannot be ruled out. Second, the CGI criteria were created for this study, and clinicians and researchers might disagree about some of the defining characteristics of each level. We also do not know if our CGI should be regarded as a continuous or ordinal dimension, so statistically we treated the CGI categorically first, and then as a continuous variable. Both approaches led to similar conclusions. Third, because our CGI ratings were based on extracting data from medical records, only records which provided sufficient information could be used; thus, we could only include Veterans who maintained contact with the treatment facility. However, this likely means that the TAU comparison group was comprised of Veterans who were more compliant with treatment than those without sufficient medical record information, and therefore, more likely to have had the benefits of TAU. Finally, neurocognitive assessments were not part of the 12-month follow-up procedures, so we cannot offer any information about cognitive differences for the two randomized conditions at that timepoint, nor about the relationship between neurocognitive improvement and CGI outcomes. This is also true for work hours after WT concluded. We therefore do not know whether there would have been an association between continued neurocognitive improvement or continued work activity and CGI scores.
4.2. Strengths:
Despite these limitations, we believe that this report adds meaningfully to the small literature on the additional benefits of CRT and the therapeutic benefits of work therapy in recovery from substance use disorder. While greater CRT training time was associated with better CGI scores, the large effect of receiving WT compared with TAU alone is very striking. Moreover, it is remarkable to consider that a 3-month WT program appears to have had lasting impact at 12 months. The VA has well-established work therapy and supported employment programs, and it would be feasible to augment outpatient substance use treatments with these programs. A previous multi-site study that used CWT with homeless Veterans (Kashner et al., 2002) showed some SUD benefit, but the study was not focused primarily on Veterans with SUD and the participants faced many more psychosocial issues because of their homelessness. Importantly, their CWT involvement did not begin with engagement in SUD treatment. Outcomes may be more robust with Veterans already engaged in SUD treatment. Therefore, we believe that a larger, more rigorous VA study to test the effectiveness of work therapy augmentation early in SUD recovery seems warranted based on the very large effects found in our study and the evidence from previous studies. While work therapy may have limited appeal to younger, employed Veterans eager to return to their full-time job, there are growing numbers of older Veterans similar to those in this study who would be receptive to these services and may benefit from them. A work-structured day in an accommodating setting that supports recovery is currently available for outpatients throughout the VA. We believe our findings should encourage further research on its clinical use for Veterans in outpatient SUD treatment.
HIGHLIGHTS.
12-month follow-up of a three-month RCT of Cognitive Remediation Therapy augmented with Work Therapy (CRT+WT) or WT alone on SUD outcomes found that the conditions did not differ significantly (77% vs. 62% recovery) but were much higher than what would be expected from the literature.
Hours of CRT during the training period was associated with better SUD outcomes at 12 months.
Comparison of CRT+WT and WT alone with a post-hoc group comprised of matched participants who received Treatment as Usual (TAU) found highly significant differences with only 27% of TAU participants having favorable SUD outcomes.
Hours of WT during training was also associated with better SUD outcomes.
Although CRT may have some effect on SUD outcomes over time, WT appears to have a large and sustained effect on SUD outcomes.
Funding Sources:
This research is funded by VA Rehabilitation Research and Development Service Grant to Morris Bell, Ph.D.; a National Institute of Drug Abuse grant to Morris Bell, Ph.D. and by a VA Rehabilitation Research and Development Service Senior Research Career Scientist Award to Morris Bell, Ph.D.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Morris D. Bell, Department of Psychiatry, Yale University/ VA Connecticut Healthcare System
Bharath Muppala, Department of Psychiatry, Yale University.
Andrea J. Weinstein, Department of Psychiatry, Yale University
David Ciosek, VA Connecticut Healthcare System.
Brian Pittman, Department of Psychiatry, Yale University.
Ismene Petrakis, Department of Psychiatry, Yale University/ VA Connecticut Healthcare System.
Joanna M. Fiszdon, Department of Psychiatry, Yale University/ VA Connecticut Healthcare System
References:
- Bell MD, Laws HB, & Petrakis IB (2017). A randomized controlled trial of cognitive remediation and work therapy in the early phase of substance use disorder recovery for older Veterans: Neurocognitive and substance use outcomes. Psychiatric Rehabilitation Journal, 40(1), 94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell MD, Vissicchio NA, & Weinstein AJ (2016). Visual and verbal learning deficits in Veterans with alcohol and substance use disorders. Drug and Alcohol Dependence, 159, 61–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell MD, Zito W, Greig T, & Wexler BE (2008). Neurocognitive enhancement therapy with vocational services: work outcomes at two-year follow-up. Schizophrenia Research, 105(1–3), 18–29. [DOI] [PubMed] [Google Scholar]
- Bell M, Fiszdon J, Greig T, Wexler B, & Bryson G (2007). Neurocognitive enhancement therapy with work therapy in schizophrenia: 6-month follow-up of neuropsychological performance. Journal of Rehabilitation Research & Development, 44(5). [DOI] [PubMed] [Google Scholar]
- Busner J, & Targum SD (2007). The clinical global impressions scale: applying a research tool in clinical practice. Psychiatry (Edgmont), 4(7), 28. [PMC free article] [PubMed] [Google Scholar]
- Curran GM, Flynn HA, Kirchner J, Booth BM (2000). Depression after alcohol treatment as a risk factor for relapse among male veterans. Journal of Substance Abuse Treatment, 19(3), 259–265. [DOI] [PubMed] [Google Scholar]
- Cripe CT, & Cooper RL (2019). Neurocognitive improvements and increased sobriety rates using a neuroengineered-cognitive remediation/brain-computer interface training method. Presented at Cognitive Remediation in Psychiatry, Columbia University, New York, New York. [Google Scholar]
- Falk DE, O’Malley SS, Witkiewitz K, Anton RF, Litten RZ, Slater M, … & Meulien D (2019). Evaluation of drinking risk levels as outcomes in alcohol pharmacotherapy trials: a secondary analysis of 3 randomized clinical trials. JAMA Psychiatry, 2019;76(4):374–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashner TM, Rosenheck R, Campinell AB, Suris A, Crandall R, Garfield NJ, … & Wicker A (2002). Impact of work therapy on health status among homeless, substance-dependent veterans: A randomized controlled trial. Archives of General Psychiatry, 59(10), 938–944. [DOI] [PubMed] [Google Scholar]
- Milby JB, Schumacher JE, Raczynski JM, Caldwell E, Engle M, Michael M, & Carr J (1996). Sufficient conditions for effective treatment of substance abusing homeless persons. Drug and Alcohol Dependence, 43(1–2), 39–47. [DOI] [PubMed] [Google Scholar]
- Rosenheck R, & Seibyl CL (1997). Effectiveness of treatment elements in a residential–work therapy program for veterans with severe substance abuse. Psychiatric Services, 48(7), 928–935. [DOI] [PubMed] [Google Scholar]
- Vinogradov S (2019). Has the time come for cognitive remediation…again?, American Journal of Psychiatry, 176 (4). 262–264. [DOI] [PubMed] [Google Scholar]
- Wykes T, Huddy V, Cellard C, McGurk SR, & Czobor P (2011). A meta-analysis of cognitive remediation for schizophrenia: methodology and effect sizes. American Journal of Psychiatry, 168(5), 472–485. [DOI] [PubMed] [Google Scholar]


