1. Case report
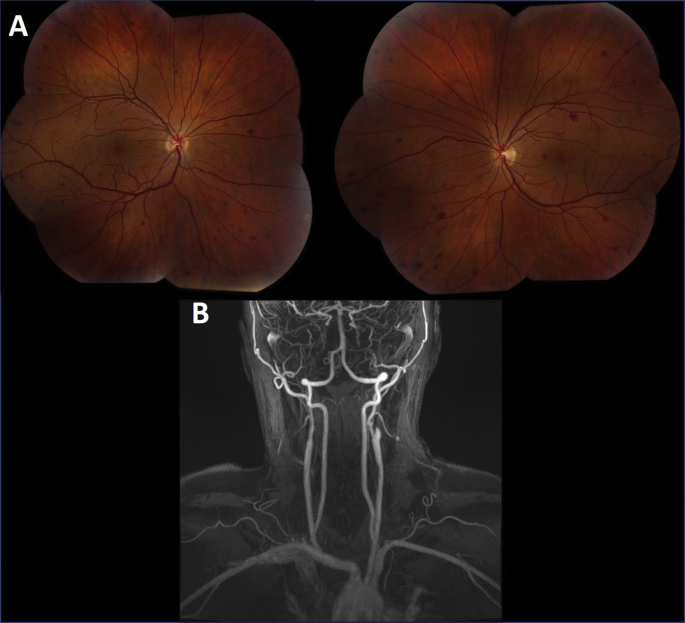
A 47-year-old man presented with intermittent episodes of simultaneous visual disturbance. He had difficulty describing his symptom except to say he had blurred vision with difficulty seeing for 10–15 min. The visual episodes would occur randomly throughout the day and sometimes several times a day. There was no precipitating factor that the patient could identify and were not posturally (e.g. laying, sitting, standing, bending) related. Other than the visual blurring he had no other associated systemic or neurological symptoms. Past medical history was notable for Moyamoya disease and a left middle cerebral artery (MCA) territory stroke requiring a left superficial temporal artery (STA) to MCA bypass. Blood pressure was 140/86 and pulse was regular at 60 beats/min. A recent electrocardiogram was normal. Visual acuity was 20/20 in each eye with normal pupillary reflexes. Slit-lamp biomicroscopy was normal in each eye with intraocular pressures of 13 mmHg right eye and 15 mmHg left eye. Dilated fundus examination showed venous dilation and mild tortuosity, with scattered large dot blot retinal hemorrhages in both eyes consistent with venous stasis retinopathy (Panel A). Magnetic resonance angiography demonstrated complete occlusion of the internal carotid arteries bilaterally (Panel B). The patient was scheduled for a right STA-MCA bypass due to the high risk of cerebral stroke and is being followed carefully for the development of retinal neovascularization, which would require either laser or anti-vascular endothelial growth factor injection therapy.
2. Discussion
Venous stasis retinopathy falls within the spectrum of ocular ischemic syndrome which includes anterior segment manifestations such as rubeosis iridis, uveitis, corneal edema, and cataract.1 Posterior segment features include retinal hemorrhages, narrowed retinal arteries, central retinal artery occlusion, neovascularization and glaucoma. Fluorescein angiography can help in the diagnosis and shows prolonged arm-to-choroid, arm-to-retina circulation time, and arterio-venous transit time.1 Venous stasis retinopathy is an early form of ocular ischemia and is categorized by some experts as nonischemic central retinal vein occlusion.2,3 The transient visual loss or amaurosis fugax is due to retinal dysfunction from poor perfusion pressure. Typically, amaurosis fugax is monocular but when binocular suggests posterior circulation or bilateral anterior circulation insufficiency.
3. Conclusion
Any patient with symptoms and findings suggestive of ocular ischemia should undergo a cardiovascular evaluation that includes imaging of the carotid artery and its branches (see Fig. 1).
Fig. 1.
A. Color fundus photograph showing right (left) and left (right) eye venous dilation and mild tortuosity, with scattered large dot blot retinal hemorrhages.
B. Magnetic resonance angiography demonstrating complete occlusion of the internal carotid arteries bilaterally. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article).
Meeting presentation
None.
Financial support
Mayo Foundation.
CRediT authorship contribution statement
Sasha A. Mansukhani: Writing - original draft, Investigation. Laurence J. Eckel: Resources, Writing - review & editing. John J. Chen: Writing - review & editing. M Tariq Bhatti: Conceptualization, Writing - original draft, Visualization, Writing - review & editing.
Declaration of competing interest
No conflicting relationship exists for any author.
Acknowledgments and disclosures
Supported by Mayo Foundation.
The following authors have no financial disclosures: SAM, LJE, JJC, MTB.
All authors attest that they meet the current ICMJE criteria for Authorship.
References
- 1.Terelak-Borys B., Skonieczna K., Grabska-Liberek I. Ocular ischemic syndrome - a systematic review. Med Sci Mon Int Med J Exp Clin Res. 2012;18:Ra138–144. doi: 10.12659/MSM.883260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dahlmann A.H., McCormack D., Harrison R.J. Bilateral hypoperfusion retinopathy. J R Soc Med. 2001;94:298–299. doi: 10.1177/014107680109400615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hayreh S.S. Classification of central retinal vein occlusion. Ophthalmology. 1983;90:458–474. doi: 10.1016/s0161-6420(83)34530-9. [DOI] [PubMed] [Google Scholar]