Abstract
Background
Our study aimed to measure the tongue volume (TV), oral cavity volume (OCV), and their ratio (TV/OCV) and correlate with upper airway using cone-beam computed tomography (CBCT).
Method
The volume of oral cavity, tongue and upper airway were obtained by the manual process of segmentation of CBCT data of 15 subjects. The mean age of the sample was 21.86 years (range 15–33 years). Segmentation of the upper airway, tongue and oral cavity was performed manually using Mimics 11.0 (Materialise, Leuven, Belgium) software at different thresholds for air and the tongue. The Hounsfield units (HU) for airway volume of the different facial region ranged from −1024 to −500. For tongue volume, Hounsfield units (HU), ranging from −200 to 200 was calculated.
Results
A significant negative correlation between TV/OCV and oropharynx (r = − 0.51; P = 0.04), TV/OCV and oral cavity airway volume (r = − 0.74; P = 0.002) was found. There was a significant and a positive correlation with TV/OCV and tongue volume (r = 0.65; P = 0.009).
Conclusion
A significant negative correlation established between TV/OCV, oropharynx and oral cavity airway volume. This finding indicates an influence tongue volume, oral cavity volume and their ratio on patency of the oropharynx.
Keywords: Tongue volume, Oral cavity volume, Cone beam computed tomography
1. Introduction
The volumetric imaging of oral cavity is technically challenging because of its complex anatomy, ill-defined boundaries and complex functionality of the soft tissues. The oral cavity comprises of two parts, the vestibule and the oral cavity proper. The oral cavity proper is a part of oral cavity which joins the oropharynx through oropharyngeal isthmus at the posterior of the oral cavity proper. Whereas, surrounding soft tissues including soft palate and tongue at the level of anterior tonsillar pillars, can open and close the isthmus. In general, the roof of the oral cavity is formed by the hard and soft portions of the palate, but the floor is made of the mylohyoid muscle diaphragm principally.1 The maxilla and mandible are the defining bony margins of the oral cavity which houses the anterior two-thirds of the tongue. Posterior one-third of the tongue is located in oropharynx which in turn is the part of the upper airway.
The nasal cavity and pharynx constitute the upper airway.2 A tortuous nasal cavity pathway, adenoids and enlarged tongue may lead to obstructive sleep apnoea(OSA).3,4 Sex, age, obesity, and anatomical factors also influence the airway. OSA patients usually have enlarged soft palate, decreased upper airway width at multiple levels, an inferiorly positioned hyoid bone and the inferior shift of the enlarged tongue.5, 6, 7, 8 An enlarged tongue inside a normal size oral cavity or normal tongue in small oral cavity might move posteriorly and partially contribute to compromising the patency of the airway.
The earlier many methods had been used for measuring tongue which included measuring the volume of water displacement,9 or by making alginate impression of tongue,10 and know the relationship with oral cavity.11 The tongue is a mobile structure, so these techniques and methodology make a poor representation of oral cavity and its structures. Two dimensional representation of three-dimensional structures lateral cephalogram has also been used for assessing the tongue and oral cavity size.12
Later, three-dimensional measurements were performed using MDCT and MRI.13,14 MDCT and MRI data have inherent limitations such as lowered tongue position in the supine position under the effect of gravity. MRIs image quality is also decreased in motion artefacts due to tongue mobility and long exposure time and is therefore not routinely acquired for orthodontic diagnosis or treatment.15 MDCT scan is a reliable and valid tool to view and measure tongue and oral cavity sizes,13 albeit, a significant drawback of being a significant radiation dose. Cone-beam computed tomography (CBCT), due to its relatively less radiation dosage and ability to obtain the scans in sitting position overcomes the major limitation of obstruction in the upper airway in the supine position due to tongue falling backwards as observed in MRI and MDCT.16 CBCT has been used to measure the volume of the tongue, and volumetric measurements are considered precise and reliable.17,18
Oral cavity volume and tongue volume could have a relationship with upper airway. In specific, we hypothesized that the tongue volume, which is the important predictor for OSA have relation to upper airway. Hence, this study aimed to investigate the relationship between tongue volumes (TV), OCV (Oral cavity volume) their ratio (TV/OCV) with upper airway using CBCT.
2. Method
This, preliminary, prospective study was performed on data of 15 (8 men, 7 female) CBCT images. Those images were collected randomly from an orthodontic clinical database irrespective of the gender of the subjects. In our 15 subjects data 3 subjects have Class II Skeletal malocclusion, 7 have Class III Skeletal malocclusion and rest 5 have skeletal Class I malocclusion. This study was approved by the Institutional Research Ethics Committee. The mean age of the sample was 21.86 years with the range of 15–33 years. Informed consent was obtained from all the subjects of our study. All CBCT images were obtained with one system i -CAT (i -CA T; Imaging Sciences International, Hatfield, PA, USA) according to a standard protocol (120 kV, 5 mA, 17 cm × 23 cm field of view, and 26 s scanning time). For CBCT scans, patient were asked to sit in an upright position, Frankfort horizontal (FH) plane parallel to the floor and keep the teeth in maximum intercuspation. The subjects were advised not to swallow, or breathe, and place the tip of the tongue on the lingual surface of the upper incisor to standardize tongue position. Data were exported in DICOM (version 1.7, Digital Imaging and Communications in Medicine) format with an isometric voxel size of 0.25–0.30 mm.
Dolphin imaging software (version 11.9 premium; Dolphin Imaging and Management Solutions, Chatsworth, Calif) imported these DICOM data sets for orientation. These images were rendered into volumetric images, and sagittal, axial, coronal slices and the three-dimensional images were obtained. The Frankfort horizontal plane and trans-orbital plane horizontally and midsagittal plane vertically were aligned after obtaining the volume-rendered.19
After orientation of each of the volume rendered image data set was exported to Mimics 11.0 (Materialise, Leuven, Belgium) for the purpose of segmentation. An expert orthodontist undertook the manual process of the segmentation of the upper airway subregions, oral cavity and tongue. The boundaries limits and segmentation method used for the airway parameters (Table 1) were selected based on the works of Neelapu BC.20
Table-1.
Boundary limits of upper airway, maxillary sinus and oral cavity.
| Regions | Anterior limit | Posterior limit | Superior limit | Inferior limit | Lateral limit |
|---|---|---|---|---|---|
| Nasopharynx | Line perpendicular to FH plane passing through PNS in sagittal view | Line perpendicular to FH plane passing through C2sp | Soft tissue contour of the pharyngeal wall | Line parallel to FH plane passing through PNS in sagittal view | Soft tissue contour of the pharyngeal lateral walls |
| Oropharynx | Line perpendicular to FH plane to anterosuperior border of hyoid bone | Line perpendicular to FH plane passing through C2sp | Line parallel to FH plane passing through PNS, in sagittal view | Line parallel to FH plane passing through C3ai | Soft tissue contour of the pharyngeal lateral walls |
| Hypopharynx | Line perpendicular to FH plane passing through PNS | Line perpendicular to FH plane passing through C2sp | Line parallel to FH plane passing through C3a | Line parallel to FH plane passing through C4a | Soft tissue contour of the pharyngeal lateral walls |
| Nasoethmoid Sinus | Line perpendicular to FH passing through tip of nose | Line perpendicular to FH plane passing through PNS | Line parallel to FH plane passing through Nasion | Line parallel to FH plane passing through PNS | Plane perpendicular to FH plane passing through the lateral walls of the maxillary sinus |
| Maxillary Sinus | Plane perpendicular to the FH plane, passing through the most anterior point of maxillary sinus | Plane perpendicular to the FH plane, passing through the most posterior point of maxillary sinus | Plane parallel to the FH plane, passing through the most upper point of maxillary sinus | Plane parallel to the FH plane, passing through the most lower point of maxillary sinus | Plane perpendicular to the FH plane passing through lateral walls of maxillary sinus |
| Oral cavity | Compact bone of the alveolar arches and mandible | Line perpendicular to FH plane to anterosuperior border of hyoid bone | Line parallel to FH plane passing through PNS | Lines joining the most anterior point on the hyoid body (H) to vallecula posterior and lingual point pogonion anteriorly | Junction of upper and lower posterior teeth (Maxillary and mandibular arch |
PNS: posterior nasal spine, C2sp: second cervical superior posterior, C3ai: third cervical anterior inferior, C4ai: fourth cervical anterior inferior.
The volume of the nasopharyngeal airway, oropharyngeal airway, hypopharyngeal airway, nasoethmoid cavity (nasal cavity and ethmoid sinus), right and left maxillary sinus and oral cavity airway were calculated. Segmentation of nasal cavity per se was not possible due to ill-defined boundaries. The best option was to consider nasal cavity along with ethmoid sinus as a nasoethmoid entity. The airway volume of the different facial region ranged from −1024 to −500 Hounsfield units (HU) was calculated.
Anterior boundary of the oral cavity is indicated by the compact bone of the alveolar arches and mandible.1 Superior boundary parallel to the palatal plane, Inferior boundary as the lower end of the mandible, lateral boundaries by maxillary and mandibular arches1 and posterior boundary formed by a line perpendicular to FH plane from the anterio-superior point of hyoid bone.
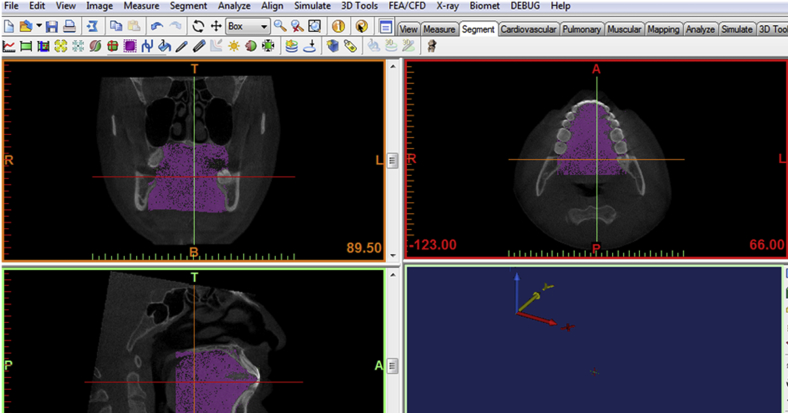
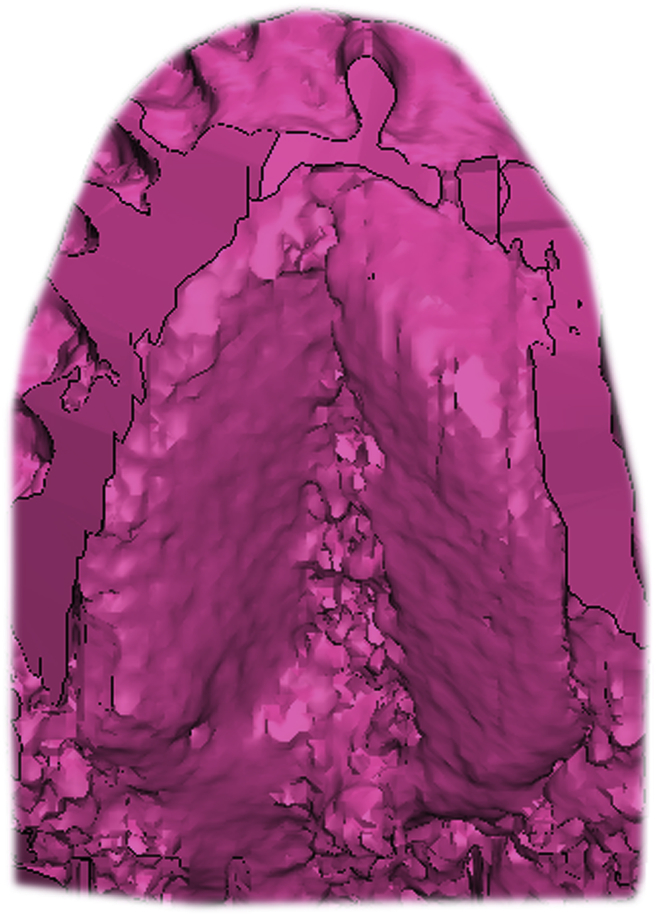
For oral cavity volume that included both oral cavity air volume and soft tissue volume, ranged from −1000 to 200 Hounsfield units (HU) was calculated (Fig. 1). For tongue volume, Hounsfield units (HU), ranging from −200 to 200 was calculated. In the sagittal plane, boundaries of tongue were limited superiorly by the dorsum of the tongue and inferiorly by lines joining the most anterior point on the hyoid body (H) to vallecula posterior and lingual point pogonion anteriorly which is the highest point on the lingual contour of the symphysis.14 Posteriorly it follows the tongue curvature in the oropharynx.18 The tongue was manually separated with Hounsfield and grey value for soft tissue scan tool. The inside of the tongue was smeared on each of the axial, coronal, and sagittal planes and the tongue volume was calculated (Fig. 2).
Fig. 1.
Image showing the calculated volume of the oral cavity.
Fig. 2.
Image showing the calculated volume of the tongue.
To reduce the measurements error, the manual segmentation of the upper airway, maxillary sinus and oral cavity was performed on 15 Subjects’ data on two separate occasions with an interval of 2 weeks using MIMICS software and average reading was taken for analysis.
3. Results
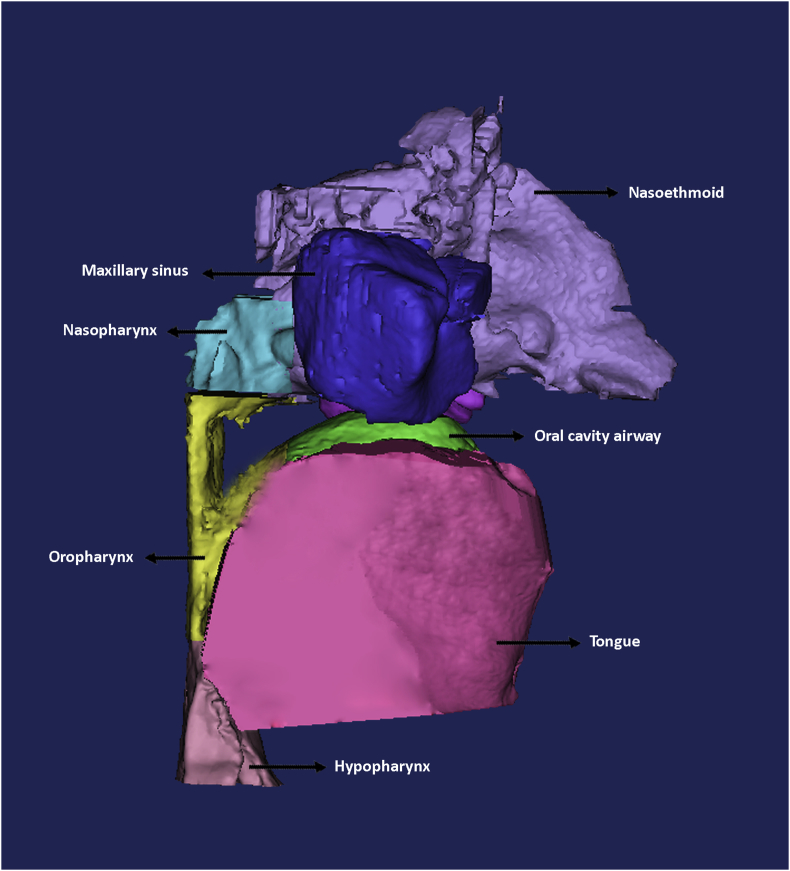
Tongue volume, oral cavity volume, TV/OCV ratio, upper airway volume and maxillary sinus volume of subjects are shown in Table-2, Fig. 3. Intraclass correlation coefficient (ICC) of the volumes segmented during 2 trails was done to know the intraobserver reliability of segmentation. Based on the 95% confident interval intraclass correlation coefficient was excellent for left maxillary sinus (0.99), right maxillary sinus (0.99), Nasoethmoid(0.97), Nasopharynx(0.96), Oropharynx(0.99), Oral cavity airway volume(0.99), and good for hypopharynx(0.81), oral cavity volume(0.78), and tongue volume(0.85). Spearman's correlation coefficient was used to know the correlation between the different variable and shown in (Table-3). A value of p < 0.05 was considered to indicate statistical significance. Our result shows that significant negative correlation found between TV/OCV and oropharynx (r = − 0.51; P = 0.04), oral cavity airway volume (r = − 0.74; P = 0.002) and significant positive correlation with TV/OCV and tongue volume (r = 0.65; P = 0.009).
Table 2.
Mean value and standard deviation of different parameters.
| Parameter | Mean | Standard deviation |
|---|---|---|
| Nasopharynx | 6.93 cm3 | 4.08 cm3 |
| Oropharynx | 17.62 cm3 | 8.96 cm3 |
| Hypopharynx | 4.09 cm3 | 2.45 cm3 |
| Nasoethmoid | 24.18 cm3 | 7.19 cm3 |
| RT maxillary sinus | 13.09 cm3 | 5.94 cm3 |
| Lt maxillary sinus | 14.06 cm3 | 5.93 cm3 |
| Oral cavity airway volume | 4.88 cm3 | 4.78 cm3 |
| oral cavity volume (OCV) | 111.09 cm3 | 19.6 cm3 |
| Tongue volume (TV) | 98.32 cm3 | 23.0 cm3 |
| TV/OCV | 89.49 | 18.88 |
Fig. 3.
Image showing the calculated means volume of the upper airway, maxillary sinus, oral cavity airway volume, tongue volume.
Table 3.
Correlation coefficient of different parameters.
| Parameters | Nasopharynx |
Oropharynx |
Hypopharynx |
Nasoethmoid |
RT maxillary sinus |
Lt maxillary sinus |
Oral cavity airway volume |
TV |
OCV |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| r value | P value | r value | P value | r value | P value | r value | P value | r value | P value | r value | P value | r value | P value | r value | P value | r value | P value | |
| TV | .29 | .29 | -.75 | .79 | -.02 | .94 | .42 | .11 | .25 | .38 | .45 | .09 | -.47 | .08 | 1 | 1 | .44 | .09 |
| OCV | .81 | .000 | .51 | .05 | .28 | .32 | .88 | .001 | .71 | .003 | .77 | .001 | .36 | .19 | .44 | .09 | 1 | 1 |
| TV/OCV | -.31 | .27 | -.51 | .04* | -.30 | .27 | -.28 | .36 | -.28 | .31 | -.13 | .64 | -.74 | .002* | .65 | .009* | -.29 | .28 |
*p value < 0.05 taken as statistically significant.
4. Discussion
The volume of the airway, oral cavity, and tongue were measured using segmentation of the CBCT using MIMICS and patient specific threshold range based on density of tissues.
4.1. Tongue volume
The mean tongue volume in this study was 98.32 ± 23.0 cm3. Uysal T et al., CBCT study on 60 patients between 16 and 36 years of age calculated the mean tongue volume 28.13 ± 8.54 cm3 for females and 31.02 ± 9.75 cm3 for males with no significant difference in males and females.17 Uysal T et al. measurements are smaller compared to our study. The main reason was being the differing definition of the volume of the tongue. The tongue posterior boundary was at the level of posterior nasal spine and the lower boundary of the tongue was at the plane of the cement–enamel junction of the lower first molars and premolars. It represents the tongue in part and is not the true representation of the entire volume of the tongue. We measured the whole tongue volume which included anterior two third portion of the oral cavity and posterior one-third part in the oropharynx. Similarly, in another CBCT study, 20 adults (10 men, 10 women) with a mean age of 30.1 ± 2.3 years (range 26.5–34.7 years) the mean TV was 47.07 ± 7.08 cm3 which is much smaller than our study. It is because they defined the inferior border of tongue as the plane passing through the midpoint of the anterior margin of the lingual frenulum, parallel to the palatal plane.18 However, tongue is attached inferiorly to hyoid bone anatomically. Hence, they did not present the anatomical tongue volume.
In MDCT study, the tongue volume was found to be 87.5 ± 14.4 cm3 for normal to mild OSA subjects and 91.2 ± 13.3 cm3 for moderate to severe OSA subjects. Snoring/OSA male Subjects (n = 64) were included in this retrospective study. OSA was diagnosed when the apnea-hypopnea index (AHI) was higher than 5 (mild 5–14; moderate 15–29; severe>30).21 Volume of the tongue, posterior airway space volume, and intra-mandibular space were measured using volumetric CT images. They used only coronal section for tongue volume measurements.
In CT imaging study of 40 Japanese male Subjects with OSA, the mean tongue volume was 79.00 ± 1.06 cm3.22 The age of the subjects selected were range from 25 to 77 years, with an average age of 52.61 years. However, they did not define the boundary of the tongue and used automatic or semiautomatic method for segmentation. Iida et al. used magnetic resonance imaging and reported the mean tongue volume of normal group was 138.84 cm3 ± 16.92 and for OSA group was 131.26 cm3 ± 20.0 with no significant difference between the groups.23 However, difference it varies from our study because they had involved pharyngeal muscles in tongue volume.23 Soft tissues volume from MR images in 51 Japanese males (31 Subjects with OSA and 20 healthy control subjects) were measured by Okubo et al. and they reported that the mean tongue volume was 78.1 ± 11.9 cm3 in subjects with OSA, and 77.1 ± 11.6 cm3 in control subjects. However, they also did not mention boundaries for tongue.24
Our result shows that tongue has a negative correlation with oropharynx and oral cavity airway but at statistically insignificant level. Lee et al. also observed no significant correlations between OSA severity and MRI volumetric measurements of the tongue.25 Other studies also supported our study and reported that there was no relationship between tongue volume and AHI.21,24,26 These studies suggests that there is a need for consensus to define oral cavity volume and tongue volume in three dimensional imaging techniques. CBCT appears a reasonable modality of scanning, however, consensus on recording and validity of measurements in different settings needs to be investigated.
4.2. Oral cavity volume
The mean oral cavity volume in this study was 111.09 ± 19.6 cm3. Iida et al. reported the mean oral cavity volume of the normal group is 159.78 cm3 ± 20.74 and for OSA group is 144.9 cm3 ± 12.42.23 They reported higher value as they involved oropharyngeal volume in oral cavity volume.
In our study, total oral cavity volume was found to have a significant positive correlation between nasopharynx, nasoethmoid and right and left maxillary sinus. Craniofacial morphology of individual is correlated to the size of different cavities surrounding the oral cavity. Hence oral cavity volume has a strong positive correlation with the volume of nasopharynx, nasoethmoid and right and left maxillary sinus. Our results are supported by a study in which the subjects with reduced maxillary and mandibular length and intermaxillary space, the nasopharyngeal airway was also narrower and directly related to OSA.27 Distance between the lateral walls of the nasal cavity and the nasal septum is often reduced in subjects with transverse maxillary deficiency, so that resistance of nasal airflow is increased.28 With the increase in size of oral cavity, the palatal plane dimension also increases and it increases the nasal cavity size, because of palatal plane forms the floor of nasal cavity and roof of the oral cavity. Rhinomanometry and acoustic rhinometry studies before and after the expansion revealed the increase in nasal volume and minimum cross-sectional area (MCA) of nose, but decreases the nasal resistance.29, 30, 31 The nasopharynx is anatomically located behind the posterior nasal concha, above the level of a palatal plane. Posterior expansion of the maxilla has a positive influence on the function of the nasopharyngeal cavity32 and increases the oral cavity volume and the nasopharyngeal size.
4.3. TV/OCV
Different subjects have the different physique and skeletal framework. Their tongue and oral cavity volume also changes with subject's physique and skeletal framework, so tongue and oral cavity volume ratio is taken in this study and it represents the oral configuration regardless of the physique and skeletal framework of a subject.
In our study the mean of TV/OCV ratio is 89.49 ± 18.88. A recent CBCT study also found a correlation between TV and OCC (Oral cavity capacity).18 The mean value was 91.4 ± 5.4%. This value is different from our study as they did not define the boundaries of oral cavity and used different boundaries for the tongue. A study with 20 OSA male subjects and 20 healthy male adults tongue volume/oral cavity volume ratio (TV/OCV ratio) on the basis of the shapes of the tongue and palate obtained by magnetic resonance imaging (MRI). The mean TV/OCV ratio was 90.56 ± 2.15% in the OSAS patient group and 86.98 ± 3.16% in the control group.23 However, they also involved oropharyngeal muscle and airway in tongue volume and oral cavity volume respectively.
TV/OCV ratio has a significant negative correlation with oropharynx, oral cavity airway and significant positive correlation with tongue in our study. It means for a constant oral cavity size. Increased tongue size decreased the oropharyngeal airway or for a constant tongue size, decreased oral cavity volume decreased the oropharyngeal airway. For a constant oral cavity size if tongue size increased, the oral cavity volume is less capable of accommodating the increased tongue volume. As a result, the enlarged tongue moves posteriorly, decreasing the oropharyngeal airway volume. This is supported by various pathological tongue enlargement disorders like haemangioma of tongue33 amyloidosis of tongue34 Melkersson-Rosenthal syndrome (MRS) is associated with OSA.35
For a constant tongue size, if oral cavity size was decreased, again tongue will move posteriorly. As seen in orthodontics extractions followed by large retraction of the anterior teeth could possibly lead to narrowing of the upper airway due to reduced of oral cavity size.36,37 Mandibular setback with maxillary advancement surgeries lead to less compromised post-surgical pharyngeal airways compared with mandibular setback alone in class III subjects because oral cavity size not reduce more in double jaw surgeries.38
This is supported by CT imaging study with 40 male subjects with OSA, the, the upper airway was negatively related with Tongue/Mandible ratio (P = 0.046). This study is limited to the airway, tongue, and mandible.22 In other MDCT study, it was found that standardized tongue volume, which implies mandible size means ratio of tongue and mandible, was much higher in Mod-Sev OSA group.21 However these studies were used ratio of tongue to mandible instead of ratio of tongue to oral cavity. Iida et al. concluded that OSA Subjects had a larger TV/OCV ratio than normal and this ratio is likely involved in development of OSA and can be used as a diagnostic tool. It means when ratio is increased, oropharyngeal airway should be decreased.23
Our study, unlike previous work, is not limited by oropharynx, instead we measured upper airway consisted by nasoethmoid, nasopharynx, oropharynx and hypopharynx and correlate each segment with the tongue volume, oral cavity and their ratio (Table 4). This study has used keen methodology on tongue and oral cavity segmentation and used manual slice by slice editing of defined boundaries. By using the slice edit tools oversegmented and undersegmented marking on the slices were edited. By using a Boolean tool overlapping volumes between 2 anatomic segments were edited. In this tool, overlapping volumes between 2 anatomic segments were edited during the segmentation process. However, these are time consuming but it may provide the more precise volume. We also used the image enhancement tools for better visualization of data and accurate segmentation. Tongue volume measurement is also influenced by tongue position,39,40 Hence, we instructed the subjects to position the tip of the tongue to contact the lingual surfaces of the lower incisors.39,40 Tongue attached to the hyoid bone inferiorly; hence the most anatomical inferior boundary for tongue presents more defined tongue volume which this study used. Our intraclass correlation coefficient also shows excellent to good results and supports our measurement reliability.
Table-4.
Comparison of different studies for oral cavity and tongue volume measurements.
| S. No. | Authors/Year | Aim of study | Sample Size | Modalities | Results | Limitation |
|---|---|---|---|---|---|---|
| 1 | Iida-Kondo C et al.25(2006) | To compared the tongue volume/oral cavity volume (TV/OCV) ratio | 40, 20- OSA 20- Non OSA |
MRI | Patients with OSA had a larger TV/OCV ratio than Controls. |
|
| 2 | Okubo M et al.26 (2006) | To evaluate the volume of the upper airway soft tissues. | 51, 31-OSA 20- Non OSA |
MRI | Not significantly different between the OSAHS and the control groups |
|
| 3 | Shigeta Y et al.24 (2011) | To know the influence on the upper airway of the size ratio of tongue and mandible (T/M ratio) | 40- OSA | CT | Negative correlation between airway volume and T/M ratio (P.046) |
|
| 4 | Uysal T et al.17 (2013) | To evaluate the relationship between the tongue volume and incisor irregularity. | 60-Non OSA | CBCT | Significant inverse correlation (r = − 0.429; P = 0.029) was determined between lower incisor irregularity and tongue volume in males. |
|
| 5 | Ahn SH et al.23(2015) | To identify correlations between OSA severity and tongue volume. | 64- OSA | CT | No associations between tongue volume or posterior airway space and the AHI were observed. |
|
| 6 | Ding X et al.18 (2018) | To measure tongue volume (TV) and oral cavity capacity (OCC) and to assess the relationship between them. | 20 - Non OSA | CBCT | Significant correlation between TV and OCC (r = 0.920; p < 0.01). |
|
OSA- Obstructive Sleep Apnoea.
This finding indicates an influence tongue volume, oral cavity volume and their ratio on the upper airway and TV/OCV could be used for OSA diagnosis, tongue resection in macroglossia condition. This study has limitations of small sample size, and age range of evaluated subjects also wide. We also did not measure the tongue volume, oral cavity volume according to skeletal relation and growth pattern of patient that is also affecting the upper airway size.
5. Conclusion
A significant negative correlation established between TV/OCV, oropharynx and oral cavity airway volume. This finding indicates an influence tongue volume, oral cavity volume and their ratio in effecting patency of the oropharynx. Our sample was adult non OSA subjects and further studies can be done in OSA subjects to know the ratio of TV/OCV and its effect on upper airway.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors do not have any potential conflict of interest.
Contributor Information
S.S. Rana, Email: rana.shailu0612@gmail.com.
O.P. Kharbanda, Email: opk15@hotmail.com, dr.opk15@gmail.com.
B. Agarwal, Email: bhaskar.agg@gmail.com.
References
- 1.Unger J.M. The oral cavity and tongue: magnetic resonance imaging. Radiology. 1985;155(1):151–153. doi: 10.1148/radiology.155.1.3975395. [DOI] [PubMed] [Google Scholar]
- 2.Rana S.S., Kharbanda O.P. Letter to the editor on "Efficiency of bimaxillary advancement surgery in increasing the volume of the upper airways: a systematic review of observational studies and meta-analysis". Eur Arch Oto-Rhino-Laryngol. 2017;274(1):585. doi: 10.1007/s00405-016-4118-y. [DOI] [PubMed] [Google Scholar]
- 3.Basheer B., Hegde K.S., Bhat S.S., Umar D., Baroudi K. Influence of mouth breathing on the dentofacial growth of children: a cephalometric study. J Int Oral Health. 2014;6(6):50–55. [PMC free article] [PubMed] [Google Scholar]
- 4.Souki B.Q., Lopes P.B., Veloso N.C. Facial soft tissues of mouth-breathing children: do expectations meet reality? Int J Pediatr Otorhinolaryngol. 2014;78(7):1074–1079. doi: 10.1016/j.ijporl.2014.04.008. [DOI] [PubMed] [Google Scholar]
- 5.Sakakibara H., Tong M., Matsushita K., Hirata M., Konishi Y., Suetsugu S. Cephalometric abnormalities in non-obese and obese patients with obstructive sleep apnoea. Eur Respir J. 1999;13(2):403–410. doi: 10.1183/09031936.99.13240399. [DOI] [PubMed] [Google Scholar]
- 6.Lowe A.A., Santamaria J.D., Fleetham J.A., Price C. Facial morphology and obstructive sleep apnea. Am J Orthod DentofacialOrthop. 1986;90(6):484–491. doi: 10.1016/0889-5406(86)90108-3. [DOI] [PubMed] [Google Scholar]
- 7.Ikävalko T., Närhi M., Lakka T. Lateral facial profile may reveal the risk for sleep disordered breathing in children. Acta Odontol Scand. 2015;73(7):550–555. doi: 10.3109/00016357.2014.997795. [DOI] [PubMed] [Google Scholar]
- 8.Indriksone I., Jakobsone G. The upper airway dimensions in different sagittal craniofacial patterns: a systematic review. Stomatol. 2014;16(3):109–117. [PubMed] [Google Scholar]
- 9.Bandy H.E., Hunter W.S. Tongue volume and the mandibular dentition. Am J Orthod. 1969;56(2):134–142. doi: 10.1016/0002-9416(69)90230-9. [DOI] [PubMed] [Google Scholar]
- 10.Oliver R.G., Evans S.P. Tongue size, oral cavity size and speech. Angle Orthod. 1986;56:234–243. doi: 10.1043/0003-3219(1986)056<0234:TSOCSA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Takada K., Sakuda M., Yoshida K., Kawamura Y. Relations between tongue volume and capacity of the oral cavity proper. J Dent Res. 1980;59:2026–2031. doi: 10.1177/00220345800590120101. [DOI] [PubMed] [Google Scholar]
- 12.Sakakibara H., Tong M., Matsushita K. Cephalometric abnormalities in non-obese and obese Subjects with obstructive sleep apnea. Eur Respir J. 1999;13:403–410. doi: 10.1183/09031936.99.13240399. [DOI] [PubMed] [Google Scholar]
- 13.Roehm E.G. Computed tomographic measurements of tongue volume relative to its surrounding space. Am J Orthod. 1982;81:170–172. [Google Scholar]
- 14.Lauder R., Muhl Z.F. Estimation of tongue volume from magnetic resonance imaging. Angle Orthod. 1991;61:175–184. doi: 10.1043/0003-3219(1991)061<0175:EOTVFM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 15.Macovski A. MRI: a charmed past and an exciting future. J Magn Reson Imag. 2009;30:919–923. doi: 10.1002/jmri.21962. [DOI] [PubMed] [Google Scholar]
- 16.Kapila S., Conley R.S., Harrell W.E., Jr. The current computed tomography imaging in orthodontics. Dento maxillafacial Radiology. 2011;40:24–34. doi: 10.1259/dmfr/12615645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Uysal T., Yagci A., Ucar F.I., Veli I., Ozer T. Cone-beam computed tomography evaluation of relationship between tongue volume and lower incisor irregularity. Eur J Orthod. 2013 Oct;35(5):555–562. doi: 10.1093/ejo/cjr054. [DOI] [PubMed] [Google Scholar]
- 18.Ding X., Suzuki S., Shiga M., Ohbayashi N., Kurabayashi T., Moriyama K. Evaluation of tongue volume and oral cavity capacity using cone-beam computed tomography. Odontology. 2018 Feb 21 doi: 10.1007/s10266-017-0335-0. [Epub ahead of print] PubMed PMID: 29468332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alves M., Jr., Franzotti E.S., Baratieri C., Nunes L.K., Nojima L.I., Ruellas A.C. Evaluation of pharyngeal airway space amongst different skeletal patterns. Int J Oral Maxillofac Surg. 2012;41:814–819. doi: 10.1016/j.ijom.2012.01.015. [DOI] [PubMed] [Google Scholar]
- 20.Neelapu B.C., Kharbanda O.P., Sardana H.K. The reliability of different methods of manual volumetric segmentation of pharyngeal and sinonasalsubregions. Oral Surg Oral Med Oral Pathol Oral Radiol. 2017 Dec;124(6):577–587. doi: 10.1016/j.oooo.2017.08.020. [DOI] [PubMed] [Google Scholar]
- 21.Ahn S.H., Kim J., Min H.J. Tongue volume influences lowest oxygen saturation but not apnea-hypopnea index in obstructive sleep apnea. PLoS One. 2015;10(8) doi: 10.1371/journal.pone.0135796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shigeta Y., Ogawa T., Ando E., Clark G.T., Enciso R. Influence of tongue/mandible volume ratio on oropharyngeal airway in Japanese male Subjects with obstructive sleep apnea. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011 Feb;111(2):239–243. doi: 10.1016/j.tripleo.2010.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Iida-Kondo C., Yoshino N., Kurabayashi T., Mataki S., Hasegawa M., Kurosaki N. Comparison of tongue volume/oral cavity volume ratio between obstructive sleep apnea syndrome Subjects and normal adults using magnetic resonance imaging. J Med Dent Sci. 2006 Jun;53(2):119–126. [PubMed] [Google Scholar]
- 24.Okubo M., Suzuki M., Horiuchi A. Morphologic analyses of mandible and upper airway soft tissue by MRI of Subjects with obstructive sleep apnea hypopnea syndrome. Sleep. 2006;29:909–915. doi: 10.1093/sleep/29.7.909. [DOI] [PubMed] [Google Scholar]
- 25.Lee R.W.W., Sutherland K., Chan A.S.L. Relationship between surface facial dimensions and upper airway structures in obstructive sleep apnea. SLEEP. 2010;33(9):1249–1254. doi: 10.1093/sleep/33.9.1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vgontzas A.N. Sleep apnea and daytime sleepiness and fatigue: relation to visceral obesity, insulin resistance, and hypercytokinemia. J Clin Endocrinol Metab. 2000;85:1151–1158. doi: 10.1210/jcem.85.3.6484. [DOI] [PubMed] [Google Scholar]
- 27.Johal A., Patel S.I., Battagel J.M. The relationship between craniofacial anatomy and obstructive sleep apnoea: a case-controlled study. J Sleep Res. 2007;16(3):319–326. doi: 10.1111/j.1365-2869.2007.00599.x. [DOI] [PubMed] [Google Scholar]
- 28.Hartgerink D.V., Vig P.S., Abbott D.W. The effect of rapid maxillary expansion on nasal airway resistance. Am J Orthod Dentofacial Orthop. 1987;92:381–389. doi: 10.1016/0889-5406(87)90258-7. [DOI] [PubMed] [Google Scholar]
- 29.Doruk C., Sökücü O., Sezer H., Canbay E.I. Evaluation of nasal airway resistance during rapid maxillary expansion using acoustic rhinometry. Eur J Orthod. 2004;26:397–401. doi: 10.1093/ejo/26.4.397. [DOI] [PubMed] [Google Scholar]
- 30.Babacan H., Sokucu O., Doruk C., Ay S. Rapid maxillary expansion and surgically assisted rapid maxillary expansion effects on nasal volume. Angle Orthod. 2006;76:66–71. doi: 10.1043/0003-3219(2006)076[0066:RMEASA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 31.Oliveira De Felippe N.L., Da Silveira A.C., Viana G., Kusnoto B., Smith B., Evans C.A. Relationship between rapid maxillary expansion and nasal cavity size and airway resistance: short- and long-term effects. Am J Orthod Dentofacial Orthop. 2008;134:370–382. doi: 10.1016/j.ajodo.2006.10.034. [DOI] [PubMed] [Google Scholar]
- 32.Cistulli P.A., Palmisano R.G., Poole M.D. Treatment of obstructive sleep apnea syndrome by rapid maxillary expansion. Sleep. 1998;21:831–835. doi: 10.1093/sleep/21.8.831. [DOI] [PubMed] [Google Scholar]
- 33.Konovalova K.I., Elfimova E.M., Butorova E.A. A clinical case of hemangioma of the face and tongue concurrent with severe obstructive sleep apnea syndrome complicated by cardiac arrhythmias and conduction disturbances] Ter Arkh. 2016;88(8):105–110. doi: 10.17116/terarkh2016888105-110. [DOI] [PubMed] [Google Scholar]
- 34.Carbone J.E., Barker D., Stauffer J.L. Sleep apnea in amyloidosis. Chest. 1985;87(3):401–403. doi: 10.1378/chest.87.3.401. [DOI] [PubMed] [Google Scholar]
- 35.Eisele H.J., Reichenberger F., Mayer K., Weissmann N., Seeger W., Schulz R. Obstructive sleep apnea in a patient with the Melkersson-Rosenthal syndrome. Sleep Breath. 2010 Sep;14(3):245–247. doi: 10.1007/s11325-009-0309-8. [DOI] [PubMed] [Google Scholar]
- 36.Hu Z., Yin X., Liao J., Zhou C., Yang Z., Zou S. The effect of teeth extraction for orthodontic treatment on the upper airway: a systematic review. Sleep Breath. 2015;19(2):441–451. doi: 10.1007/s11325-015-1122-1. [DOI] [PubMed] [Google Scholar]
- 37.Zheng Z., Liu H., Xu Q. Computational fluid dynamics simulation of the upper airway response to large incisor retraction in adult class I bimaxillary protrusion patients. Sci Rep. 2017;7:45706. doi: 10.1038/srep45706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tan S.K., Leung W.K., Tang A.T.H., Zwahlen R.A. Effects of mandibular setback with or without maxillary advancement osteotomies on pharyngeal airways: an overview of systematic reviews. PLoS One. 2017 Oct 9;12(10) doi: 10.1371/journal.pone.0185951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Peat J.H. A cephalometric study of tongue position. Am J Orthod. 1968;54:339–351. doi: 10.1016/0002-9416(68)90303-5. [DOI] [PubMed] [Google Scholar]
- 40.McKee T.L. A cephalometric radiographic study of tongue position in individuals with cleft palate deformity. Angle Orthod. 1956;26:99–109. [Google Scholar]