Abstract
We recently introduced the concept of the infectome as a means of studying all infectious factors which contribute to the development of autoimmune disease. It forms the infectious part of the exposome, which collates all environmental factors contributing to the development of disease and studies the sum total of burden which leads to the loss of adaptive mechanisms in the body. These studies complement genome-wide association studies, which establish the genetic predisposition to disease. The infectome is a component which spans the whole life and may begin at the earliest stages right up to the time when the first symptoms manifest, and may thus contribute to the understanding of the pathogenesis of autoimmunity at the prodromal/asymptomatic stages. We provide practical examples and research tools as to how we can investigate disease-specific infectomes, using laboratory approaches employed from projects studying the “immunome” and “microbiome”. It is envisioned that an understanding of the infectome and the environmental factors that affect it will allow for earlier patient-specific intervention by clinicians, through the possible treatment of infectious agents as well as other compounding factors, and hence slowing or preventing disease development.
Keywords: Autoimmunity, Autoimmune disease, Environment, Infection, Immunity, Microbiome
Introduction
We recently introduced the concept of the infectome as a means of studying all infections throughout life which contribute to the development/progression of disease [1], as it is now viewed that the majority of diseases develop as a result of the interaction between genetic and environmental influences [2–4]. Autoimmune diseases are especially seen to be caused by this interaction [2, 3, 5]. It is now estimated that approximately 5–20 % of North Americans are affected by at least one autoimmune disease [6, 7]. The mosaic of autoimmunity is a concept which reflects the fact that many patients with one autoimmune disease have several concomitant autoimmune diseases at any given time with heterogeneous triggers and aetiological factors [8–15].
Much attention has been given to genetic research on the path to uncovering the underlying factors of autoimmunity [16]. In addition to molecular signalling pathways [17], genome-wide association studies (GWAS) have identified numerous gene–disease associations in several autoimmune diseases [3]. The essential number of associated genes needed for the maintenance of autoaggressive responses and the development of clinically overt disease has not been properly delineated [18]. However, environmental factors, possibly occurring even in utero, must be given equal attention in the study of the nature of autoimmune disease [2, 3, 19, 20]. Epidemiological and clinical studies using toxicological, microbiological, biochemical and immunological testing are now being used to identify these diverse environmental factors, which include infectious organisms, xenobiotics, chemical compounds and heavy metals, although the list of materials may be exhaustive [2, 21–24]. Autoimmune (auto-inflammatory) syndrome induced by adjuvants (ASIA) is one example where vaccinations and heavy metals have been implicated as triggers of autoimmunity. Recent news regarding the role of prosthetic metal on metal hip replacements has also shown how immune dysfunction and damage can be caused in distant organs due to the release of metals such as chromium and nickel from such prostheses. Recent findings from the National Institute of Environmental Health Sciences workshop on autoimmunity and environment support these findings and have reported significant evidence linking particular autoimmune disease to specific environmental agents [25, 26].
The exact interaction of these exposures and their interplay with genes that confer susceptibility remains poorly defined. It should also be noted that some common mechanisms may underlie the development of all or most autoimmune diseases, with subsequent exposures differentiating one disease from the other [27].
The concept of an “exposome” is being used as a means of collating and measuring the effects of environmental factors, both internal and external. These factors may be responsible for increased susceptibility to a disease, or protection from developing the disease. The internal factors include the balance of the flora in the microbiome, the nutritional status of the individual such as vitamin D levels and balance of essential fatty acids, the state of the antioxidant pathways that protect against the deleterious effects of free radicals generated during infective episodes, as well as factors relating to immune function/balance such as the health of the endocrine axis. This review will emphasise the role of the “infectome” as the infectious component of the microbiome/exposome which contributes to the development of autoimmune disease. As the infectome could broadly describe the infectious components of the exposome responsible for the induction of non-autoimmune in addition to autoimmune diseases, we may need to differentiate the “autoinfectome” from that not related to autoimmunity. In other words, there may be particular components that are only seen in autoimmune disease, and possibly certain features common to all autoimmune diseases.
Overview of the exposome
The exposome represents all exogenous and endogenous environmental exposures which begin preconception and carry on throughout life [28–32]. The endogenous factors are unique to the exposome as compared to previous epidemiological studies [30]. The study of the exposome addresses both external triggers and endogenous factors directly or indirectly linked to the environment [31, 32]. By-products of inflammation, lipid peroxidation, as well as oxidative stress are examples of endogenous sources [30]. Several of these constituents serve as nucleophiles or electrophiles and are capable of DNA and protein modification [33], which may also occur due to bacterial infection [34–36]. It is likely that the collation of these components would be unique to a disease, much like GWAS [33]. Also akin to GWAS, quantification of exposure may be a critical piece of information.
It may be clinically useful to look at causes within an individual in terms of exposure, times of exposure, sequence of exposure, time-points of exposure events, as well as other risk factors (genetic, epigenetic and other) that induce or maintain an inflammation state and exposure to various stimuli that provoke further autoaggression. If these exposures could be examined independently, they may help identify the pieces of the jigsaw puzzle that lead to the breakdown of tolerance and the induction of pathological alterations as the result of the autoimmune attack. Components of the exposome may also serve as measurable biomarkers [33] in the blood or body fluids of affected patients or individuals prone to develop autoimmune diseases [4, 31–33]. Technologies such as liquid chromatography–tandem mass spectrometry [37], DNA adducts [38], functional measurements of antioxidant capacity and breath analysis may be utilised in such instances [29].
Two methods of exposomal measurement have been proposed: the “bottom-up” method which measures the external factors [30] and the “top-down” method which measures internal factors. Both methods may provide the whole picture of a measurable exposome when they are used in conjunction with extensive questionnaires and other established epidemiological tools [30–32]. Frequent sampling could provide evidence of significant changes of these markers over time, especially during critical phases of the disease (sub-clinical course, remission, relapses) [30]. One such study indicated that breath analysis for particular biomarkers provides critical information as to whether one has been exposed, what the dosage was, and how rapidly the body is eliminating the toxicant [29]. The plausibility of the exposome has been demonstrated by Patel et al. [39]. These investigators conducted an “environmental-wide association study” on late diabetes mellitus, where epidemiological data were systematically assessed with methodologies comparable to those used in GWAS, and found associations with 37 environmental factors, including organochlorine pesticides, nutrients/vitamins, polychlorinated biphenyls and dioxins [39]. Other studies have demonstrated similar results on an immunological cross-reactivity level [40] [41]. The complexity and breadth of these components would suggest that breaking them down into multiple components may allow for more in-depth analysis [1].
There is no need to underline how difficult it would be to trace down all these highly heterogenous triggers. Homogenous technology platforms suffer from limitations, as all human biomarker measurements are subject to inter- and intra-subject variance. The creation of a uniform platform that will incorporate and analyse the obtained data would be a milestone, even in the age of ultra-fast computing. Breaking down the heterogenous and highly diverse components could be a more logical step. Screening for the presence of individual infections is routinely used in a small scale [31]. Medium-scale multi-parametric immunoassays for antibodies of various isotypes specific to bacterial or viral antigens, urine and stool cultures and polymerase chain reaction (PCR) are also used in larger laboratories and provide a wealth of information [31]. The ultimate step would be to go a step further and introduce technological platforms that enable high-scale testing of dozens—if not hundreds—of infectious agents at one time, similar to what has been achieved for genes through GWAS. Other functional tests that are available within the realm of scientific research may be brought into clinical and epidemiological use. Examples of these include functional assays of antioxidant pathways, tests of immune sensitivity designed for environmental factors as opposed to biological antigens, DNA adducts, assessment of methylation status and assessment of cellular membrane structure to name but a few.
From exposome- to infectome-induced autoimmunity
Infectious and non-infectious agents comprise environmental triggers [5, 42–46]. Non-infectious triggers are numerous, and some examples from our literature search can be found in Table 1 [42, 47–75]. An infectious burden in autoimmunity has been documented and the triggers are numerous, including bacteria, viruses, parasites and fungi, with variations on particular organisms being found from one autoimmune disease to the next [5, 76, 77]. Geo-epidemiological, microbiological and immunological data indicate the existence of infectious burdens varying from one autoimmune disease to another. Autoantibody burdens in infected individuals have also been noted, but these individuals have not been followed-up for long and it is not know how many of those could develop autoimmune disease [78]. We define the group of disease-causing or disease-linked infections as the “infectome”. Alterations in the presence of these organisms or the body’s immune response to them would also be noted, such as in the case of treatment with antibiotics [79, 80] or exposure to xenobiotics [81–83]. Such exposures may alter the disease course or its progression by altering the flora present. In contrast to the hygiene hypothesis which supports a protective role played by infections [84–88], work on clinical biomaterial and experimental animal models of autoimmune diseases clearly demonstrates that infectious agents break immunological tolerance to self-antigens and can induce autoimmune disease [5]. Examples include acute rheumatic fever presenting several weeks after infection with Streptococcus pyogenes [89], Helicobacter pylori and autoimmune gastritis [90], as well as between Trypanosoma cruzi and Chagas’ cardiomyopathy [91], and Mycoplasma with rheumatoid arthritis [92]. These exposures likely begin as early as the transfer of maternal antibodies via the placenta or via breast milk in the gastrointestinal tract, but it is important to identify which of these exposures contributes to the development of disease. It is also important to highlight differences with the microbiome, which identified all microorganisms in a particular region, but is unable to identify those which cause (or protect from) the development and/or progression of a disease. It is also a measure which occurs at a single time point, and thus, only gives a snapshot of which organisms are present throughout a lifetime. Likewise, environmental factors may influence the development of autoimmunity by infectious agents through several routes. The co-expression of xenobiotics or metals, such as nickel, aluminium or mercury, for example, which are now ubiquitous in our environment and a constant part of the human exposome, may act as adjuvants to the immune system. If this occurs in anatomical positions, such as the oral cavity, which is key to the development of oral tolerance through various dental interventions, it may have vast ramification for the development of immunity and autoimmunity. Likewise, the effects of metals have not been fully studied on the human gut microbiome. Potential damage to the gut microflora has potentially extensive implications for the protective role of these floras against pathogen invasion as well as the interactions of the microflora with the mucosal-associated immune system. Mercury is well known for its immunomodulating effects and is frequently used in experimental models for inducing immune reactions (e.g. mercuric chloride model for vasculitis). It also is known to have immunosuppressive effects, and this in its own right may impair the immune system’s response to infections (Fig. 1).
Table 1.
Environmental agents associated with the development of autoimmune disease
| Environmental triggers | Disease | Reference |
|---|---|---|
| Allopurinol | Immune haemolytic anaemia | [65] |
| Captopril | Autoimmune thrombocytopenia | [66] |
| Chlorpromazine | Anti-phospholipid syndrome, haemolytic anaemia, SLE, AiLD | [67–73] |
| Estrogens | PBC, SLE, RA | [149–152, 310–314] |
| Halothane | AIH | [72, 315, 316] |
| Iodine | Autoimmune thyroid | [57] |
| Penicillins | AiLD, immune haemolytic anaemia | [72, 317] |
| Rifampicin | AIH, autoimmune thyroid, immune haemolytic anaemia | [318–320] |
| Tetracyclines | AIH, DM, SLE | [74, 321–330] |
| Vaccinations | PBC, AIH, SLE, RA, MS, MG, DM, polyarteritis nodosa | [270, 331–343] |
| Smoking | PBC, COPD, RA, autoimmune thyroid | [149–152, 344–349] |
| Silicone and collagen implants | SLE, Sjogren’s, SSc | [347, 350–356] |
This table provides examples of several non-infectious agents which have been associated with the development of autoimmune disease. These agents are highly varied and range from pharmacological materials to waste products and cigarette smoke. Note that this list is not extensive, but serves to give examples from a variety of sources
AIH autoimmune hepatitis, AiLD autoimmune liver disease, COPD chronic obstructive pulmonary disease, DM dermatomyositis, MG myasthenia gravis; rheumatoid arthritis, SLE systemic lupus erythematosus, SSc systemic sclerosis
Fig. 1.
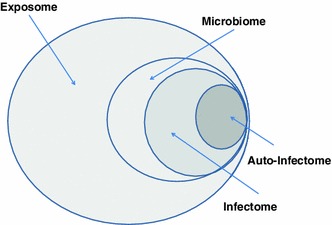
From exposome to infectome via microbiome. “Exposome” describes all environmental factors which we are exposed to in a lifetime, both exogenous and endogenous, infectious and non-infectious. Environmental exposures are basically subdivided into infectious and non-infectious agents. The concept of “infectome” that we introduce describes the part of the exposome which refers to the collection of an individual’s exposures to infectious agents participating in the pathogenesis of autoimmune disease (“auto-infectome”). The infectome can be considered a part of “microbiome”, the collection of the microbial products which the human body is exposed to at a given time
Moreover, induction of autoimmunity by viruses or bacteria is probably done by a “hit-and-run” mechanism when the causative agent has been cleared from circulation by the time of diagnosis. Tracking down each individual’s exposure to infectious agents as well as anti-microbial immune responses may be important for the establishment of a causative link between infection and autoimmunity. The infectome allows for the analysis of affected tissue not only at the time of overt infection, but also allows for the analysis of humoral and cellular immune responses to that infection, possibly some time after the causative organism has been cleared. Hence, the infectome allows for the ongoing surveillance of infection, response and possible change in clinical course. When done in several individuals over time, a particular disease “fingerprint” may be established in relation to triggering infectious agents (Fig. 2).
Fig. 2.
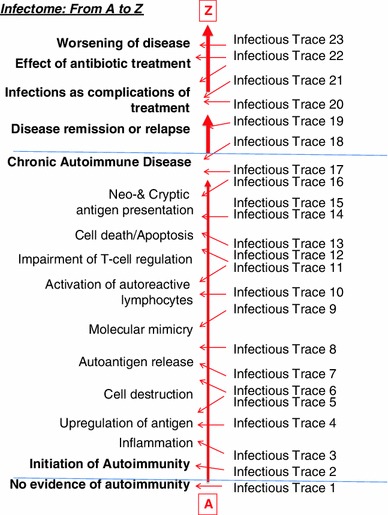
The infectome from A to Z. The study of the infectome at various time-points in both sub-clinical and clinically overt disease can provide hints regarding the mechanisms leading to the loss of immunological tolerance. Infectious agents unrelated to the development of the induction of the disease may play a role in the appearance of concomitant autoimmune manifestations/diseases or specific clinical patterns (relapses/remission)
It is envisioned that the infectome would be most helpful in autoimmune diseases with long subclinical stages and frequent remission–relapse states such as multiple sclerosis (MS), primary biliary cirrhosis (PBC), rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE) [93]. Highly specific antibodies appear years before the onset of symptoms in most of these diseases [94–96]. Reasons underlying relapse–remission in these diseases are unknown, making them ideal candidates for the investigation of the infectome.
SLE as an infectome model
Systemic lupus erythematosus is often characterised by a prodromal stage of anti-Sm and anti-Ro antibody responses with no clinical signs [97, 98]. Many first-degree relatives of SLE patients also have ANA reactivity, predominantly anti-dsDNA and anti-Ro/SSA antibody reactivity [99–101]. Published data have suggested that high ANA titre, anti-dsDNA, anti-Ro/SSA and anti-chromatin may be of prognostic relevance for the subsequent development of SLE [99]. It is unknown why some, but not all, individuals go on to develop clinical SLE, with disease flares [21]. Multiple infectious factors have been involved in the pathogenesis of SLE, ranging from EBV and cytomegalovirus (CMV) to parvovirus B19 [43, 97, 98, 100–106]. In the case of CMV, for example, one study found that all female patients with SLE are infected with CMV compared to 75 % of controls [104]. Another study reported that the pp65 antigen of CMV induces autoantibodies in SLE patients and mice prone to develop autoimmune disease [107]. It must be noted that the transient nature of these viruses may influence the detection rates within individuals. Hence, it is difficult to say whether the virus was present at a particular time frame of the disease. It is possible that SLE and/or SLE flares can develop after infection with specific agents, and the study of the infectome can serve as a model to study the role played by infections in such cases. First-degree relatives of SLE patients or other individuals at high risk to develop the disease such as those with autoantibody positivity may be screened at regular follow-ups. SLE patients would also be checked, and alterations of clinical phenotypes may be associated with exposure to particular infectious agents. Comprehensive analysis of the data initiated by the infectome may narrow-down the large list of organisms implicated in disease’s development.
Multiple sclerosis and infectome
Multiple sclerosis, a chronic autoimmune neurological syndrome, serves as another prototype autoimmune disease in which the infectome model can be assessed, as it is characterised by periods of relapse and remission [108, 109]. It is likely that several risk factors accumulated over a long period of time are responsible for the development of the disease [110–112].
The relapsing–remitting form of MS is most common and is characterised by flares that include the worsening of previous/current symptoms and the development of new ones [113]. Flares are followed by complete or partial recovery, with a variable period of duration from one patient to the next, and several patients acquire secondary progressive MS. Primary progressive MS (PPMS) is a form of MS characterised by stable progression of the disease with worsening of the symptomatology over the course of time. Two further forms of the disease are also found: the benign form characterised by minimal or mild progression of disability and full recovery of sporadic sensory episodes [113], and the Marburg variant of MS, a rapidly progressive disease, which eventually leads to death. It is currently unknown as to why these clinically distinct variants exist within one disease [113].
Pathologically, MS is characterised by inflammatory lesions with areas of demyelination in the CNS, which consist of mononuclear cell infiltrates composed of T and B lymphocytes, plasma cells, macrophages and microglia in the perivascular spaces that develop into plaques [108, 114].
Multiple sclerosis has a strong genetic background, as identical twins are 100 times more likely to develop MS if their co-twin has MS, whereas non-twin siblings are 20 times more likely [115, 116]. Previous studies have demonstrated that the strongest genetic association of MS is with HLA-DRB1*1501 [117], though GWAS studies [109] have also implicated non-HLA immunomodulatory genes, including IL7R, IL12RA, CLEC16 and CD226 [118, 119]. In support of a pivotal role for environmental influences in the development of MS is the fact that MS-related implicated genes have only demonstrated an odds ratio of less than 1.3 and that there is a 30 % concordance for MS twins [108, 109, 120, 121] (Table 2).
Table 2.
Infectious agents implicated in multiple sclerosis
| Strong evidence base | Weak evidence base | ||
|---|---|---|---|
| Epstein–Barr virus | [357–372] | Chlamydia pneumoniae | [373] |
| Human herpesvirus 6 | [142–146, 374, 375] | Borrelia burgdorferi | [376] |
| Varicella zoster virus | [377–379] | Mycobacterium tuberculosis | [380] |
| Human cytomegalovirus | [381] | ||
| Retroviruses | [382, 383] | ||
| Coronavirus | [384, 385] | ||
| Torque teno virus | [147] | ||
| JC virus | [386, 387] | ||
| Rubella virus | [388] | ||
| Parainfluenza virus I | [389] | ||
| Measles virus | [390, 391] | ||
| Mumps virus | [392] | ||
Several infectious agents have been implicated in the pathogenesis of multiple sclerosis (MS), but few have a strong evidence base. Interestingly, only viruses appear to be strongly linked with the disease, whereas several viruses and bacteria have weak or circumstantial associations. It may be the case that several of the infectious agents with a weak evidence base reflect the lack of investigation into these organisms. As well, it is unclear as to whether any of these infectious agents also play a role in the relapsing–remitting course of the disease. By applying the infectome model, it will likely be easier to define which of the organisms listed below (and likely more) are involved in the development and progression of MS, as well as possibly defining particular subtypes of the disease
Vitamin D appears to be a non-infectious agent that is involved in the induction of MS and other autoimmune diseases [109, 122–134]. Vitamin D appears to play a role in the modulation of pro-inflammatory pathways and T cell regulation [109]. Increased distance from the equator has been correlated with low vitamin D, and interestingly, MS rates increase as distance from the equator increases [108]. As well, populations with increased dietary vitamin D intake have lower rates of MS [109]. An Australian study found a decreased risk of a first demyelinating event in those with increased sun exposure, who also had increased levels of serum vitamin D [135]. This has also been found in other studies [136]. As well, the effect of month of birth on MS development was more apparent in familial MS groupings, suggesting an influence on prenatal vitamin D levels, as well as an interaction between genes and environment [109]. Smoking has also been associated with MS development [137]. Smoking appears to have an interaction with genetic features (so-called gene–environmental interactions) and in particular with HLA-DRB1*15 and the absence of HLA-A*02, which appears to increase the risk of developing MS [138]. Heavy metals may also play a role in some MS patients [139]. Several bacteria and viruses have been implicated in MS (Table 3) [108, 109, 120, 121, 140, 141], including EBV [108, 109, 120, 121] and human herpesvirus 6 (HHV6) have been implicated. Interestingly, the relapse–remittance pattern of HHV6 is similar to the clinical phenotype of MS [109], and HHV6 reservoirs have been demonstrated in serum, CSF [142, 143] and CNS tissues of patients with MS [144, 145]. Molecular mimicry involving myelin basic protein and HHV6 encoded U24 mimics, and T cell cross-reactivity has been documented [146]. Other implicated viruses include coronaviruses, varicella zoster virus, Torque teno virus, retroviruses and JC virus [108, 109, 120, 121]. Reactivity to several viral peptides was found, which has led to the speculation that continual exposure to a variety of viruses can lead to T cell expansion reactive against highly conserved proteins, including self-peptides [147].
Table 3.
Infectious agents implicated in primary biliary cirrhosis
| Bacteria | Escherichia coli | [170, 172, 256, 258, 393, 394] |
| Novosphingobium aromaticivorans | [172, 393] | |
| Mycobacterium gordonae | [395–397] | |
| Lactobacillus delbrueckii subsp. bulgaricus | [250, 270] | |
| Viruses | Βetaretrovirus | [263, 267, 398, 399] |
This table provides examples of infectious organisms which have been implicated in the pathogenesis of primary biliary cirrhosis (PBC). Although several organisms have been implicated, we have only included those which appear to have strong evidence base so far, based on multiple studies and case reports. Many implicated pathogens have not been studied in any great depth so far
In addition to providing answers to the aetiology of autoimmune disease, it is also envisioned that the infectome may also identify the cause of certain disease characteristics, such as variable presentation and progression, disease flares, or relapse–remittance.
Primary biliary cirrhosis and infectome
Primary biliary cirrhosis can also be used as a model disease to investigate the role of the infectome [148]. This is largely based in its relatively common (as far as autoimmune disease go) prevalence, its long preclinical phase with positivity for antimitochondrial antibodies (AMA) that are pathognomonic for the disease, its differing progression among patients, and growing evidence for an involvement of genetic, environmental and infectious pathogenetic factors [149–157]. Clinical, histopathological and experimental data support that the disease is autoimmune [94, 153, 158–178]. Infectious agents and xenobiotics mimicking the autoepitopic region of PDC-E2, the major PBC self-target, induce PBC-specific autoantibodies and bile duct destruction.
Primary biliary cirrhosis is characterised by a long preclinical phase of AMA positivity with no biochemical evidence of liver disease, which is followed by a period of biochemical abnormalities and then clinically overt disease. The disease has a long preclinical phase which may take several years. Most sera from patients with PBC have AMA at diagnosis [95, 169, 178–204], which is also predictive of eventual disease development [205]. PBC is also characterised by disease-specific anti-nuclear autoantibodies (ANA) that identify patients with worst disease [206–221]. Familial PBC has been noted and the risk of developing PBC is high amongst family members of PBC patients [222–228]. Most patients with PBC also have other extra-hepatic disease, including autoimmune rheumatic diseases, and autoimmune thyroiditis.
An interesting feature of PBC is that it does not respond to immunosuppressive treatment, which eliminates the need to consider the effects of immunosuppressive therapy on relapse/remission states, thus making PBC ideal for an infectome study.
A “bottom-up” approach has been taken in various epidemiological studies examining associated risk factors and has identified several environmental factors [149–152] [153–156, 229]. This has been associated with animal models [153, 230–234].Genetic risks involve HLA [235, 236], non-HLA [237–243] and sex-linked genes [244–246]. It is likely that some genetic factors may influence the potential penetrance of infectious agents. For example, HLA-DRB1*11 and HLA-DRB1*13 have a negative association with PBC. It is of interest that such genes confer protection to hepatotropic viruses, such as hepatitis B and C. This highlights the notion that the infectome and GWAS (and likely all exposome components) cannot be studied in isolation. Various pathogens are linked with PBC including E.coli due to a link with UTI (Table 2) [158, 176, 244, 247–270]. Microbial/self-molecular mimicry has been proposed as a bridge linking infections and autoimmunity [158, 176, 247–251, 255, 265, 266, 270–276].
Approaches to study the infectome
We have previously outlined how the infectome may be studied [1]. In brief, this would involve several steps, beginning with the determination of HLA class I and II, ideally at birth. This may allow for subgrouping individuals into high- or low-risk groups. Second, urine, oro-nasal swabs, saliva, faecal material and blood (for isolation of plasma, serum and peripheral blood mononuclear cells—PBMCs) would be collected, with once-yearly follow-ups with collection of samples. Meticulous recording of clinical data and collection of samples are needed when anti-infective treatment is applied for incidental/casual infections at the preclinical stages of the disease, as this may affect the final outcome of the underlying processes. All samples would be stored and then analysed for associated infectious agents and non-associated agents using multiplex technology (Table 4). This type of regular follow-up and sample collection with analysis would occur throughout the disease, paying close attention to the findings at times of change in clinical course, such as the development of symptoms.
Table 4.
Multiparametric systems for the diagnosis of autoimmune-related infectious agents can be based on the technology currently used for the multiparametric detection of systemic infections [290–292]
| Molecular detection | |
| Multiplex real-time PCR | Real-time PCR and higly specific melting point analysis, e.g., LightCycler SeptiFast (25 pathogens) |
| Molecular hybridisation | Commercially available platforms are already in use, e.g., simultaneous detection of multiple viral types and subtypes from nasopharygeal swabs and simultaneous detection of viral, bacterial and protozoan parasites causing gastrointestinal diseases |
| Nucleotide sequencing | Nucleotide (pyro)sequencing |
| Next-generation sequencing (highly massive pyrosequencing technology, sequencing by synthesis (SBS), sequencing by oligonucleotide ligation and detection (SOLiD) system) | |
| Mass spectrometry | Post-culture microbial identification by MALDI-TOF |
| Post-PCR microbial identification by PCR-ESI | |
| Integrated fluidic systems | |
| Immunological assays | Multiparametric ELISA, line blots/dots |
| Multiparametric IFA chips | |
| Magnetic and non-magnetic bead-multiplex immunoassays | |
| Lateral flow immunochromatographic | |
| Assays | |
| Triplex lateral flow immunoassay | |
| Optical immunosensor systems | |
| Electrochemical-based ELISA | |
It should be kept in mind that several patterns of infection may be seen in individuals with a particular disease characteristic or with a particular concomitant autoimmune disease. For example, a differing pattern of infection may be seen in patients with fast-progressing versus slow-progressing PBC. This of course applies to all autoimmune diseases.
Can we learn from the microbiome and immunome projects?
As described above, the microbiome and infectome are two distinct, yet complementary entities. The microbiome is region/organ-specific (such as the gut, oral cavity or inguinal crease), where microbial genes are found to be prevalent [277–286]. It provides a snapshot of the flora of that region in a particular state in time and often reflects what would be termed normal flora by performing metagenomic screens of bacterial populations in these regions. The microbiome is not necessarily limited to normal flora, but may also be applied to a disease-affected body site, such as the gastrointestinal tract in children with irritable bowel syndrome (IBS) [283]. Saulnier and colleagues [283] obtained 71 faecal samples from 22 children with IBS and 22 healthy children aged 7–12 years. Analysis showed an elevated percentage of γ-proteobacteria in the gut flora of children with IBS, with Haemophilus parainfluenza being a prominent component [283]. Although similar, the infectome relates only to those organisms which are disease causing and is not limited to one body site.
It may be argued that the organisms of the human microbiome do not usually induce antigen-specific systemic humoral and cellular immune responses provoking local or systemic inflammatory response, while others believe that these organisms may not be pathogenic, but create disease through dysbiosis of the gut flora and participate in the induction of autoimmunity. This is a key difference between the microbiome and the infectome as the former appreciates the direct or indirect effect of immune responses against infectious agents as pivotal for the initiation of autoaggression and immune-mediated, self-targeting pathology. For the infectome, monitoring of the microbial/host immunity is as important as the isolation of potentially harmful bacterial products, since the host/microbe immunological interaction is the likely cause of the self-destruction in the case of non-cytopathic viruses and microbes. It may also be important to measure the degree to which normal flora may play in disease, as in the case of dysbiosis where beneficial bacteria become pathogenic, as with E. coli, clostridia and Klebsiella, for example.
Although separate, the infectome and microbiome complement each other in providing a micropathological profile (or profiles) of a particular disease. As well, the microbiome is essential to define the normal flora of a particular region and then collectively the entire body. Recent microbiome studies have been able to provide an idea of what “normal” may be in the gut by performing metagenomic screens of bacterial populations in these regions [279–282, 285]. What is normal in one individual may be abnormal for another and may vary from race to race and from one geographical location to the next. Likewise, studies of the gut flora of neonates over the past few decades have shown that the percentage of prevalent bacteria is changing from one generation to the next. An understanding of the normal flora of a particular region (as established by the exposome) is essential. For example, studying the microbiome of the urinary bladder and vagina may help us understand the role of UTI in PBC [149–152, 287, 288]. Investigation of multiple body sites would likely prove to be useful [266, 289].
Who to select for screening?
Population screening is unlikely in the case of the infectome, from both a practical and financial standpoint. It is more logical to study individuals at high risk to develop autoimmune manifestations. These individuals are usually the family members or individuals with HLAs conferring susceptibility to the disease. In those individuals who are initially asymptomatic, or who are at high risk, ongoing sampling and analysis may shed light as to whether the infections that induce the diseases are different to those that participate in the progression of the disease from early to advanced stages. Infectome profiling/burdens may play a decisive role in rapidly progressive patients or in patients who have frequent relapses. Common patterns may become apparent with particular disease subsets.
Screening methods and sampling sites
The easiest samples to obtain from patients include blood, urine or saliva. Analysis may be done by several methods and some of those are already in use. IgM, IgA and IgG antibody infectious serology testing is likely to be the most common method of detecting organisms, but also the most economical and efficient. Multiplex immunoassays such as ELISA and indirect immunofluorescence for the detection of antibodies against infectious agents are relatively inexpensive and provide valid information [290–292]. Large-scale multiplex technologies include protein microarrays and peptidome libraries, which are able to detect antibody responses to several hundred antigens [293–295].
A large German study used a PCR approach to detect a variety of organisms in archived liver tissues of PBC patients [296], which has been adopted in several other studies examining the role of mycobacteria in PBC [297–299], as well as beta-retroviral material in liver and lymph node tissue from PBC patients [267, 268]. Detection of viral and bacterial genetic material in tissues by a multi-parametric approach may also prove to be promising. DNA sequencing technology, and specifically the so-called high-throughput DNA sequencers, can determine hundreds of megabases of DNA sequences per run, allowing for the analysis of a broad range of infectious agents [300–303]. Massive, parallel sequencing might be the next step of this approach for that it is the most sensitive procedure available and allows for the detection of a multitude of infectious agents at the same time [304]. Although immunohistochemical testing for several microbial agents in tissue samples can be applied [305], it is likely that tissue-based methods will be applied to the infectome, as they are time consuming, and tissue of the affected organ may not be readily available from all patients. The “top-down” approach suggested by other researchers may include the analysis of blood, faecal material, urine or saliva is more plausible and can be used for screening and reflecting [30]. Multiplex PCR is a useful tool for evaluating the presence of microorganisms from a variety of sample types. Other technologies include the use of 16S/18S rRNA gene sequencing, which allows for the mass analysis of samples [281, 283]. However, one drawback of this approach in comparison with immune profiles is the risk of missing the right time or site of sampling.
Multiple body sites may need sampling. In addition to the affected organ, general or systemic infections should be an indication for sampling and may include urine and stool samples in urinary and gastrointestinal tract infections, respectively, or blood cultures in febrile patients. Latent infections such as Lyme disease or mycoplasma may also be detected, in addition to chronic low-grade infections due to dental treatment. It is becoming more apparent that the oral cavity should be examined for infection in patients with autoimmune disease [306–308]. Alterations in the flora of the oral mucosa, which may lead to a dysbiosis in the gut microbiome, can also contribute to the pathogenesis of IBD [306]. On the other hand, the increased frequency of dental problems in IBD patients may be due to alterations in oral flora. Helenius et al. [308] indicate that patients with rheumatic conditions had various alterations in salivary flow and composition, and oral health. These findings warrant further investigation into the oral flora of patients with autoimmune conditions.
The infectome serves not only to characterise which infections lead to the development/progression of disease, but also provides clinicians an opportunity for early intervention and treatment. This could be achieved through the proper use of antibiotic or antiviral therapy, or supportive treatments to prevent damage through free radical stress, which would ideally be initiated early on in the management of these patients. It is envisioned that this intervention may allow for the slower progression of the disease or possibly the prevention of it in at-risk individuals. Guidelines for such treatment should be agreed upon in larger forums, to ensure best patient care and safety [263, 267, 268, 309].
Conclusion
It is now generally viewed that most diseases, including autoimmune disease, develop from an initial genetic susceptibility followed by several environmental exposures, including infections. GWAS is now characterising the genetic components to disease development, with the exposome serving to characterise all exogenous and endogenous environmental exposures. The complex nature of the exposome may require that it be broken down to several sub-components, such as the infectome, which reflects the characterisation and measurement of all infectious organisms that we are exposed to, and which contribute to the development and progression of disease. This characterisation will likely begin with at-risk individuals (such as family members), with further development as patients develop disease symptoms or the progression of the disease changes. Many of these infectious exposures may be preventable or treatable and therefore represent a modifiable set of risk factors in their own right. On the other hand, it may be possible to modulate risk factors for the progression of disease such as the compounding effect of environmental exposures and the body’s intrinsic protective pathways through supportive therapies.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
Abbreviations
- AMA
Anti-mitochondrial antibody
- ANA
Anti-nuclear antibody
- CMV
Cytomegalovirus
- CSF
Cerebrospinal fluid
- EBV
Epstein–Barr virus
- EWAS
Environmental-wide association study
- FDR
First-degree relatives
- GWAS
Genome-wide association study
- HHV6
Human herpesvirus 6
- LC–MS/MS
Liquid chromatography–tandem mass spectrometry
- MS
Multiple sclerosis
- IBS
Irritable bowel syndrome
- PBC
Primary biliary cirrhosis
- PCR
Polymerase chain reaction
- PDC
Pyruvate dehydrogenase complex
- SLE
Systemic lupus erythematosus
Dimitrios P. Bogdanos

References
- 1.Bogdanos DP, Smyk DS, Invernizzi P, Rigopoulou EI, Blank M, Pouria S, et al. Infectome: a platform to trace infectious triggers of autoimmunity. Autoimmun Rev. 2012 doi: 10.1016/j.autrev.2012.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gourley M, Miller FW. Mechanisms of disease: environmental factors in the pathogenesis of rheumatic disease. Nat Clin Pract Rheumatol. 2007;3(3):172–180. doi: 10.1038/ncprheum0435. [DOI] [PubMed] [Google Scholar]
- 3.Lettre G, Rioux JD. Autoimmune diseases: insights from genome-wide association studies. Hum Mol Genet. 2008;17(R2):R116–R121. doi: 10.1093/hmg/ddn246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rappaport SM, Smith MT. Epidemiology. Environ dis risks Sci. 2010;330(6003):460–461. doi: 10.1126/science.1192603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kivity S, Agmon-Levin N, Blank M, Shoenfeld Y. Infections and autoimmunity–friends or foes? Trends Immunol. 2009;30(8):409–414. doi: 10.1016/j.it.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 6.Jacobson DL, Gange SJ, Rose NR, Graham NM. Epidemiology and estimated population burden of selected autoimmune diseases in the United States. Clin Immunol Immunopathol. 1997;84(3):223–243. doi: 10.1006/clin.1997.4412. [DOI] [PubMed] [Google Scholar]
- 7.Moroni L, Bianchi I, Lleo A. Geoepidemiology, gender and autoimmune disease. Autoimmun Rev. 2012;11(6–7):A386–A392. doi: 10.1016/j.autrev.2011.11.012. [DOI] [PubMed] [Google Scholar]
- 8.Blank M, Gershwin ME. Autoimmunity: from the mosaic to the kaleidoscope. J Autoimmun. 2008;30(1–2):1–4. doi: 10.1016/j.jaut.2007.11.015. [DOI] [PubMed] [Google Scholar]
- 9.Brickman CM, Shoenfeld Y. The mosaic of autoimmunity. Scand J Clin Lab Invest Suppl. 2001;235:3–15. [PubMed] [Google Scholar]
- 10.Rahamim-Cohen D, Shoenfeld Y. The mosaic of autoimmunity. a classical case of inhalation of a polyclonal activating factor in a genetically and hormonally susceptible patient leading to multiple autoimmune diseases. Isr Med Assoc J. 2001;3(5):381–382. [PubMed] [Google Scholar]
- 11.Shepshelovich D, Shoenfeld Y. Prediction and prevention of autoimmune diseases: additional aspects of the mosaic of autoimmunity. Lupus. 2006;15(3):183–190. doi: 10.1191/0961203306lu2274rr. [DOI] [PubMed] [Google Scholar]
- 12.Shoenfeld Y, Blank M, Abu-Shakra M, Amital H, Barzilai O, Berkun Y, et al. The mosaic of autoimmunity: prediction, autoantibodies, and therapy in autoimmune diseases–2008. Isr Med Assoc J. 2008;10(1):13–19. [PubMed] [Google Scholar]
- 13.Shoenfeld Y, Gilburd B, Abu-Shakra M, Amital H, Barzilai O, Berkun Y, et al. The mosaic of autoimmunity: genetic factors involved in autoimmune diseases–2008. Isr Med Assoc J. 2008;10(1):3–7. [PubMed] [Google Scholar]
- 14.Asherson RA, Gunter K, Daya D, Shoenfeld Y. Multiple autoimmune diseases in a young woman: tuberculosis and splenectomy as possible triggering factors? Another example of the “mosaic” of autoimmunity. J Rheumatol. 2008;35(6):1224–1226. [PubMed] [Google Scholar]
- 15.de Carvalho JF, Pereira RM, Shoenfeld Y. The mosaic of autoimmunity: the role of environmental factors. Front Biosci (Elite Ed) 2009;1:501–509. doi: 10.2741/e46. [DOI] [PubMed] [Google Scholar]
- 16.Costenbader KH, Gay S, Alarcon-Riquelme ME, Iaccarino L, Doria A. Genes, epigenetic regulation and environmental factors: which is the most relevant in developing autoimmune diseases? Autoimmun Rev. 2012;11(8):604–609. doi: 10.1016/j.autrev.2011.10.022. [DOI] [PubMed] [Google Scholar]
- 17.Mavropoulos A, Orfanidou T, Liaskos C, Smyk DS, Billinis C, Blank M, et al. p38 mitogen-activated protein kinase (p38 MAPK)-mediated autoimmunity: lessons to learn from ANCA vasculitis and pemphigus vulgaris. Autoimmun Rev. 2012 doi: 10.1016/j.autrev.2012.10.019. [DOI] [PubMed] [Google Scholar]
- 18.Karlson EW, Deane K. Environmental and gene-environment interactions and risk of rheumatoid arthritis. Rheum Dis Clin North Am. 2012;38(2):405–426. doi: 10.1016/j.rdc.2012.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Villeda SA, Wyss-Coray T. The circulatory systemic environment as a modulator of neurogenesis and brain aging. Autoimmun Rev. 2012 doi: 10.1016/j.autrev.2012.10.014. [DOI] [PubMed] [Google Scholar]
- 20.Simon KC, van der Mei IA, Munger KL, Ponsonby A, Dickinson J, Dwyer T, et al. Combined effects of smoking, anti-EBNA antibodies, and HLA-DRB1*1501 on multiple sclerosis risk. Neurology. 2010;74(17):1365–1371. doi: 10.1212/WNL.0b013e3181dad57e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gatto M, Zen M, Ghirardello A, Bettio S, Bassi N, Iaccarino L, et al. Emerging and critical issues in the pathogenesis of lupus. Autoimmun Rev. 2012 doi: 10.1016/j.autrev.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 22.Selmi C, Leung PS, Sherr DH, Diaz M, Nyland JF, Monestier M, et al. Mechanisms of environmental influence on human autoimmunity: a national institute of environmental health sciences expert panel workshop. J Autoimmun. 2012;39(4):272–284. doi: 10.1016/j.jaut.2012.05.007. [DOI] [PubMed] [Google Scholar]
- 23.Bogdanos DP, Smith H, Ma Y, Baum H, Mieli-Vergani G, Vergani D. A study of molecular mimicry and immunological cross-reactivity between hepatitis B surface antigen and myelin mimics. Clin Dev Immunol. 2005;12(3):217–224. doi: 10.1080/17402520500285247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smyk DS, Rigopoulou EI, Muratori L, Burroughs AK, Bogdanos DP. Smoking as a risk factor for autoimmune liver disease: what we can learn from primary biliary cirrhosis. Ann Hepatol. 2012;11(1):7–14. [PubMed] [Google Scholar]
- 25.Miller FW, Alfredsson L, Costenbader KH, Kamen DL, Nelson LM, Norris JM, et al. Epidemiology of environmental exposures and human autoimmune diseases: findings from a national institute of environmental health sciences expert panel workshop. J Autoimmun. 2012;39(4):259–271. doi: 10.1016/j.jaut.2012.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Germolec D, Kono DH, Pfau JC, Pollard KM. Animal models used to examine the role of the environment in the development of autoimmune disease: findings from an NIEHS expert panel workshop. J Autoimmun. 2012;39(4):285–293. doi: 10.1016/j.jaut.2012.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Anaya JM. Common mechanisms of autoimmune diseases (the autoimmune tautology) Autoimmun Rev. 2012;11(11):781–784. doi: 10.1016/j.autrev.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 28.Arlt VM, Schwerdtle T. UKEMS/Dutch EMS-sponsored workshop on biomarkers of exposure and oxidative DNA damage & 7th GUM-32P-postlabelling workshop, University of Munster, Munster, Germany, 28-29 March 2011. Mutagenesis. 2011. doi: 10.1093/mutage/ger036. [DOI] [PubMed]
- 29.Pleil JD, Stiegel MA, Sobus JR, Liu Q, Madden MC. Observing the human exposome as reflected in breath biomarkers: heat map data interpretation for environmental and intelligence research. J Breath Res. 2011;5(3):037104. doi: 10.1088/1752-7155/5/3/037104. [DOI] [PubMed] [Google Scholar]
- 30.Rappaport SM. Implications of the exposome for exposure science. J Expo Sci Environ Epidemiol. 2011;21(1):5–9. doi: 10.1038/jes.2010.50. [DOI] [PubMed] [Google Scholar]
- 31.Wild CP. Complementing the genome with an “exposome”: the outstanding challenge of environmental exposure measurement in molecular epidemiology. Cancer Epidemiol Biomarkers Prev. 2005;14(8):1847–1850. doi: 10.1158/1055-9965.EPI-05-0456. [DOI] [PubMed] [Google Scholar]
- 32.Wild CP. Environmental exposure measurement in cancer epidemiology. Mutagenesis. 2009;24(2):117–125. doi: 10.1093/mutage/gen061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Smith MT, Zhang L, McHale CM, Skibola CF, Rappaport SM. Benzene, the exposome and future investigations of leukemia etiology. Chem Biol Inter. 2011;192(1–2):155–159. doi: 10.1016/j.cbi.2011.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Collin M, Shannon O, Bjorck L. IgG glycan hydrolysis by a bacterial enzyme as a therapy against autoimmune conditions. Proc Natl Acad Sci U S A. 2008;105(11):4265–4270. doi: 10.1073/pnas.0711271105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Allhorn M, Olin AI, Nimmerjahn F, Collin M. Human IgG/Fc gamma R interactions are modulated by streptococcal IgG glycan hydrolysis. PLoS ONE. 2008;3(1):e1413. doi: 10.1371/journal.pone.0001413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McCulloch J, Zhang YW, Dawson M, Harkiss GD, Peterhans E, Vogt HR, et al. Glycosylation of IgG during potentially arthritogenic lentiviral infections. Rheumatol Int. 1995;14(6):243–248. doi: 10.1007/BF00262090. [DOI] [PubMed] [Google Scholar]
- 37.Polacco BJ, Purvine SO, Zink EM, Lavoie SP, Lipton MS, Summers AO, et al. Discovering mercury protein modifications in whole proteomes using natural isotope distributions observed in liquid chromatography-tandem mass spectrometry. Mol Cell Proteomics. 2011 doi: 10.1074/mcp.M110.004853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McLaren Howard J. The detection of DNA adducts (risk factors for DNA damage). A method for genomic DNA, the results and some effects of nutritional intervention. J Nutr Environ Med. 2002;12:19–31. doi: 10.1080/13590840220123334. [DOI] [Google Scholar]
- 39.Patel CJ, Bhattacharya J, Butte AJ. An environment-wide association study (EWAS) on type 2 diabetes mellitus. PLoS ONE. 2010;5(5):e10746. doi: 10.1371/journal.pone.0010746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Karges W, Hammond-McKibben D, Cheung RK, Visconti M, Shibuya N, Kemp D, et al. Immunological aspects of nutritional diabetes prevention in NOD mice: a pilot study for the cow’s milk-based IDDM prevention trial. Diabetes. 1997;46(4):557–564. doi: 10.2337/diabetes.46.4.557. [DOI] [PubMed] [Google Scholar]
- 41.Guggenmos J, Schubart AS, Ogg S, Andersson M, Olsson T, Mather IH, et al. Antibody cross-reactivity between myelin oligodendrocyte glycoprotein and the milk protein butyrophilin in multiple sclerosis. J Immunol. 2004;172(1):661–668. doi: 10.4049/jimmunol.172.1.661. [DOI] [PubMed] [Google Scholar]
- 42.Molina V, Shoenfeld Y. Infection, vaccines and other environmental triggers of autoimmunity. Autoimmunity. 2005;38(3):235–245. doi: 10.1080/08916930500050277. [DOI] [PubMed] [Google Scholar]
- 43.Pordeus V, Szyper-Kravitz M, Levy RA, Vaz NM, Shoenfeld Y. Infections and autoimmunity: a panorama. Clin Rev Allergy Immunol. 2008;34(3):283–299. doi: 10.1007/s12016-007-8048-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Doria A, Sarzi-Puttini P, Shoenfeld Y. Infections, rheumatism and autoimmunity: the conflicting relationship between humans and their environment. Autoimmun Rev. 2008;8(1):1–4. doi: 10.1016/j.autrev.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 45.Tozzoli R, Barzilai O, Ram M, Villalta D, Bizzaro N, Sherer Y, et al. Infections and autoimmune thyroid diseases: parallel detection of antibodies against pathogens with proteomic technology. Autoimmun Rev. 2008;8(2):112–115. doi: 10.1016/j.autrev.2008.07.013. [DOI] [PubMed] [Google Scholar]
- 46.Corthesy B. Role of secretory IgA in infection and maintenance of homeostasis. Autoimmun Rev. 2012 doi: 10.1016/j.autrev.2012.10.012. [DOI] [PubMed] [Google Scholar]
- 47.Brown JM, Pfau JC, Pershouse MA, Holian A. Silica, apoptosis, and autoimmunity. J Immunotoxicol. 2005;1(3):177–187. doi: 10.1080/15476910490911922. [DOI] [PubMed] [Google Scholar]
- 48.Otsuki T, Hayashi H, Nishimura Y, Hyodo F, Maeda M, Kumagai N, et al. Dysregulation of autoimmunity caused by silica exposure and alteration of Fas-mediated apoptosis in T lymphocytes derived from silicosis patients. Int J Immunopathol Pharmacol. 2011;24(1 Suppl):11S–16S. [PubMed] [Google Scholar]
- 49.Cooper GS, Wither J, Bernatsky S, Claudio JO, Clarke A, Rioux JD, et al. Occupational and environmental exposures and risk of systemic lupus erythematosus: silica, sunlight, solvents. Rheumatology. 2010;49(11):2172–2180. doi: 10.1093/rheumatology/keq214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Finckh A, Cooper GS, Chibnik LB, Costenbader KH, Watts J, Pankey H, et al. Occupational silica and solvent exposures and risk of systemic lupus erythematosus in urban women. Arthritis Rheum. 2006;54(11):3648–3654. doi: 10.1002/art.22210. [DOI] [PubMed] [Google Scholar]
- 51.Parks CG, Cooper GS. Occupational exposures and risk of systemic lupus erythematosus: a review of the evidence and exposure assessment methods in population- and clinic-based studies. Lupus. 2006;15(11):728–736. doi: 10.1177/0961203306069346. [DOI] [PubMed] [Google Scholar]
- 52.Griffin JM, Gilbert KM, Lamps LW, Pumford NR. CD4(+) T-cell activation and induction of autoimmune hepatitis following trichloroethylene treatment in MRL +/+ mice. Toxicol Sci. 2000;57(2):345–352. doi: 10.1093/toxsci/57.2.345. [DOI] [PubMed] [Google Scholar]
- 53.Khan MF, Kaphalia BS, Prabhakar BS, Kanz MF, Ansari GA. Trichloroethene-induced autoimmune response in female MRL +/+ mice. Toxicol Appl Pharmacol. 1995;134(1):155–160. doi: 10.1006/taap.1995.1179. [DOI] [PubMed] [Google Scholar]
- 54.Duntas LH. Environmental factors and thyroid autoimmunity. Ann Endocrinol (Paris). 2011;72(2):108–113. doi: 10.1016/j.ando.2011.03.019. [DOI] [PubMed] [Google Scholar]
- 55.Parks CG, Walitt BT, Pettinger M, Chen JC, de Roos AJ, Hunt J, et al. Insecticide use and risk of rheumatoid arthritis and systemic lupus erythematosus in the women’s health initiative observational study. Arthritis Care Res. 2011;63(2):184–194. doi: 10.1002/acr.20335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fortes C. Lupus erythematosus. are residential insecticides exposure the missing link? Med Hypotheses. 2010;75(6):590–593. doi: 10.1016/j.mehy.2010.07.041. [DOI] [PubMed] [Google Scholar]
- 57.Burek CL, Talor MV. Environmental triggers of autoimmune thyroiditis. J Autoimmun. 2009;33(3–4):183–189. doi: 10.1016/j.jaut.2009.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gold LS, Ward MH, Dosemeci M, De Roos AJ. Systemic autoimmune disease mortality and occupational exposures. Arthritis Rheum. 2007;56(10):3189–3201. doi: 10.1002/art.22880. [DOI] [PubMed] [Google Scholar]
- 59.Sobel ES, Gianini J, Butfiloski EJ, Croker BP, Schiffenbauer J, Roberts SM. Acceleration of autoimmunity by organochlorine pesticides in (NZB x NZW)F1 mice. Environ Health Perspect. 2005;113(3):323–328. doi: 10.1289/ehp.7347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mayes MD. Epidemiologic studies of environmental agents and systemic autoimmune diseases. Environ Health Perspect. 1999;107(Suppl 5):743–748. doi: 10.1289/ehp.99107s5743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Artukovic M, Ikic M, Kustelega J, Artukovic IN, Kaliterna DM. Influence of UV radiation on immunological system and occurrence of autoimmune diseases. Coll Antropol. 2010;34(Suppl 2):175–178. [PubMed] [Google Scholar]
- 62.Handunnetthi L, Ramagopalan SV. UV radiation, vitamin D, and multiple sclerosis. Proc Natl Acad Sci U S A. 2010;107(33):E130; author reply E1. doi: 10.1073/pnas.1004603107. [DOI] [PMC free article] [PubMed]
- 63.Prieto S, Grau JM. The geoepidemiology of autoimmune muscle disease. Autoimmun Rev. 2010;9(5):A330–A334. doi: 10.1016/j.autrev.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 64.Kuhn A, Beissert S. Photosensitivity in lupus erythematosus. Autoimmunity. 2005;38(7):519–529. doi: 10.1080/08916930500285626. [DOI] [PubMed] [Google Scholar]
- 65.Tumgor G, Balkan C, Arikan C, Kavakli K, Aydogdu S. Immune haemolytic anaemia induced by allopurinol after liver transplantation. Acta Paediatr. 2006;95(6):762–763. doi: 10.1080/08035250500499465. [DOI] [PubMed] [Google Scholar]
- 66.Pujol M, Duran-Suarez JR, Martin Vega C, Sanchez C, Tovar JL, Valles M. Autoimmune thrombocytopenia in three patients treated with captopril. Vox Sang. 1989;57(3):218. doi: 10.1111/j.1423-0410.1989.tb00827.x. [DOI] [PubMed] [Google Scholar]
- 67.Gharavi AE, Sammaritano LR, Wen J, Miyawaki N, Morse JH, Zarrabi MH, et al. Characteristics of human immunodeficiency virus and chlorpromazine induced antiphospholipid antibodies: effect of beta 2 glycoprotein I on binding to phospholipid. J Rheumatol. 1994;21(1):94–99. [PubMed] [Google Scholar]
- 68.Canoso RT, de Oliveira RM. Chlorpromazine-induced anticardiolipin antibodies and lupus anticoagulant: absence of thrombosis. Am J Hematol. 1988;27(4):272–275. doi: 10.1002/ajh.2830270408. [DOI] [PubMed] [Google Scholar]
- 69.Stein PB, Inwood MJ. Hemolytic anemia associated with chlorpromazine therapy. Can J Psychiatry. 1980;25(8):659–661. doi: 10.1177/070674378002500810. [DOI] [PubMed] [Google Scholar]
- 70.Hadnagy C. Letter: coombs-positive haemolytic anaemia provoked by chlorpromazine. Lancet. 1976;1(7956):423. doi: 10.1016/S0140-6736(76)90251-8. [DOI] [PubMed] [Google Scholar]
- 71.Berglund S, Gottfries CG, Gottfries I, Stormby K. Chlorpromazine-induced antinuclear factors. Act Med Scand. 1970;187(1–2):67–74. doi: 10.1111/j.0954-6820.1970.tb02908.x. [DOI] [PubMed] [Google Scholar]
- 72.Liu ZX, Kaplowitz N. Immune-mediated drug-induced liver disease. Clin Liver Dis. 2002;6(3):755–774. doi: 10.1016/S1089-3261(02)00025-9. [DOI] [PubMed] [Google Scholar]
- 73.Yung RL, Richardson BC. Drug-induced lupus. Rheum Dis Clin North Am. 1994;20(1):61–86. [PubMed] [Google Scholar]
- 74.Czaja AJ. Drug-induced autoimmune-like hepatitis. Dig Dis Sci. 2011;56(4):958–976. doi: 10.1007/s10620-011-1611-4. [DOI] [PubMed] [Google Scholar]
- 75.Chighizola C, Meroni PL. The role of environmental estrogens and autoimmunity. Autoimmun Rev. 2012;11(6–7):A493–A501. doi: 10.1016/j.autrev.2011.11.027. [DOI] [PubMed] [Google Scholar]
- 76.Shapira Y, Agmon-Levin N, Renaudineau Y, Porat-Katz BS, Barzilai O, Ram M, et al. Serum markers of infections in patients with primary biliary cirrhosis: evidence of infection burden. Exp Mol Pathol. 2012;93(3):386–390. doi: 10.1016/j.yexmp.2012.09.012. [DOI] [PubMed] [Google Scholar]
- 77.Shapira Y, Agmon-Levin N, Shoenfeld Y. Defining and analyzing geoepidemiology and human autoimmunity. J Autoimmun. 2010;34(3):J168–J177. doi: 10.1016/j.jaut.2009.11.018. [DOI] [PubMed] [Google Scholar]
- 78.Berlin T, Zandman-Goddard G, Blank M, Matthias T, Pfeiffer S, Weis I, et al. Autoantibodies in nonautoimmune individuals during infections. Ann N Y Acad Sci. 2007;1108:584–593. doi: 10.1196/annals.1422.061. [DOI] [PubMed] [Google Scholar]
- 79.Saad R, Rizkallah MR, Aziz RK. Gut Pharmacomicrobiomics: the tip of an iceberg of complex interactions between drugs and gut-associated microbes. Gut Pathog. 2012;4(1):16. doi: 10.1186/1757-4749-4-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Buccigrossi V, Nicastro E, Guarino A. Functions of intestinal microflora in children. Curr Opin Gastroenterol. 2013;29(1):31–38. doi: 10.1097/MOG.0b013e32835a3500. [DOI] [PubMed] [Google Scholar]
- 81.Gielda LM, DiRita VJ. Zinc competition among the intestinal microbiota. MBio. 2012;3(4):e00171. doi: 10.1128/mBio.00171-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kivity S, Katz M, Langevitz P, Eshed I, Olchovski D, Barzilai A. Autoimmune syndrome induced by adjuvants (ASIA) in the middle east: morphea following silicone implantation. Lupus. 2012;21(2):136–139. doi: 10.1177/0961203311429551. [DOI] [PubMed] [Google Scholar]
- 83.Lidar M, Agmon-Levin N, Langevitz P, Shoenfeld Y. Silicone and scleroderma revisited. Lupus. 2012;21(2):121–127. doi: 10.1177/0961203311430703. [DOI] [PubMed] [Google Scholar]
- 84.Shoenfeld Y, Toubi E. Protective autoantibodies: role in homeostasis, clinical importance, and therapeutic potential. Arthritis Rheum. 2005;52(9):2599–2606. doi: 10.1002/art.21252. [DOI] [PubMed] [Google Scholar]
- 85.Toubi E, Shoenfeld Y. Predictive and protective autoimmunity in cardiovascular diseases: is vaccination therapy a reality? Lupus. 2005;14(9):665–669. doi: 10.1191/0961203305lu2196oa. [DOI] [PubMed] [Google Scholar]
- 86.Ram M, Anaya JM, Barzilai O, Izhaky D, Porat Katz BS, Blank M, et al. The putative protective role of hepatitis B virus (HBV) infection from autoimmune disorders. Autoimmun Rev. 2008;7(8):621–625. doi: 10.1016/j.autrev.2008.06.008. [DOI] [PubMed] [Google Scholar]
- 87.Meroni PL, Shoenfeld Y. Predictive, protective, orphan autoantibodies: the example of anti-phospholipid antibodies. Autoimmun Rev. 2008;7(8):585–587. doi: 10.1016/j.autrev.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 88.Plot L, Amital H, Barzilai O, Ram M, Nicola B, Shoenfeld Y. Infections may have a protective role in the etiopathogenesis of celiac disease. Ann N Y Acad Sci. 2009;1173:670–674. doi: 10.1111/j.1749-6632.2009.04814.x. [DOI] [PubMed] [Google Scholar]
- 89.Guilherme L, Oshiro SE, Fae KC, Cunha-Neto E, Renesto G, Goldberg AC, et al. T-cell reactivity against streptococcal antigens in the periphery mirrors reactivity of heart-infiltrating T lymphocytes in rheumatic heart disease patients. Infect Immun. 2001;69(9):5345–5351. doi: 10.1128/IAI.69.9.5345-5351.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Amedei A, Bergman MP, Appelmelk BJ, Azzurri A, Benagiano M, Tamburini C, et al. Molecular mimicry between Helicobacter pylori antigens and H + , K + –adenosine triphosphatase in human gastric autoimmunity. J Exp Med. 2003;198(8):1147–1156. doi: 10.1084/jem.20030530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Cunha-Neto E, Coelho V, Guilherme L, Fiorelli A, Stolf N, Kalil J. Autoimmunity in Chagas’ disease. identification of cardiac myosin-b13 trypanosoma cruzi protein crossreactive T cell clones in heart lesions of a chronic Chagas’ cardiomyopathy patient. J Clin Invest. 1996;98(8):1709–1712. doi: 10.1172/JCI118969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.da Rocha Sobrinho HM, Jarach R, da Silva NA, Shio MT, Jancar S, Timenetsky J. Mycoplasmal lipid-associated membrane proteins and Mycoplasma arthritidis mitogen recognition by serum antibodies from patients with rheumatoid arthritis. Rheumatol Int. 2011;31(7):951–957. doi: 10.1007/s00296-010-1612-1. [DOI] [PubMed] [Google Scholar]
- 93.Tobon GJ, Pers JO, Canas CA, Rojas-Villarraga A, Youinou P, Anaya JM. Are autoimmune diseases predictable? Autoimmun Rev. 2012;11(4):259–266. doi: 10.1016/j.autrev.2011.10.004. [DOI] [PubMed] [Google Scholar]
- 94.Jones DE. Pathogenesis of primary biliary cirrhosis. Gut. 2007;56(11):1615–1624. doi: 10.1136/gut.2007.122150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kaplan MM, Gershwin ME. Primary biliary cirrhosis. N Engl J Med. 2005;353(12):1261–1273. doi: 10.1056/NEJMra043898. [DOI] [PubMed] [Google Scholar]
- 96.Arbuckle MR, McClain MT, Rubertone MV, Scofield RH, Dennis GJ, James JA, et al. Development of autoantibodies before the clinical onset of systemic lupus erythematosus. N Engl J Med. 2003;349(16):1526–1533. doi: 10.1056/NEJMoa021933. [DOI] [PubMed] [Google Scholar]
- 97.Harley JB, Harley IT, Guthridge JM, James JA. The curiously suspicious: a role for Epstein-Barr virus in lupus. Lupus. 2006;15(11):768–777. doi: 10.1177/0961203306070009. [DOI] [PubMed] [Google Scholar]
- 98.Harley JB, James JA. Epstein-barr virus infection induces lupus autoimmunity. Bull NYU Hosp Jt Dis. 2006;64(1–2):45–50. [PubMed] [Google Scholar]
- 99.Navarra SV, Ishimori MI, Uy EA, Hamijoyo L, Sama J, James JA, et al. Studies of Filipino patients with systemic lupus erythematosus: autoantibody profile of first-degree relatives. Lupus. 2011;20(5):537–543. doi: 10.1177/0961203310385164. [DOI] [PubMed] [Google Scholar]
- 100.Zandman-Goddard G, Berkun Y, Barzilai O, Boaz M, Blank M, Ram M, et al. Exposure to Epstein-Barr virus infection is associated with mild systemic lupus erythematosus disease. Ann N Y Acad Sci. 2009;1173:658–663. doi: 10.1111/j.1749-6632.2009.04754.x. [DOI] [PubMed] [Google Scholar]
- 101.Barzilai O, Sherer Y, Ram M, Izhaky D, Anaya JM, Shoenfeld Y. Epstein-Barr virus and cytomegalovirus in autoimmune diseases: are they truly notorious? a preliminary report. Ann N Y Acad Sci. 2007;1108:567–577. doi: 10.1196/annals.1422.059. [DOI] [PubMed] [Google Scholar]
- 102.Bengtsson A, Widell A, Elmstahl S, Sturfelt G. No serological indications that systemic lupus erythematosus is linked with exposure to human parvovirus B19. Ann Rheum Dis. 2000;59(1):64–66. doi: 10.1136/ard.59.1.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Hemauer A, Beckenlehner K, Wolf H, Lang B, Modrow S. Acute parvovirus B19 infection in connection with a flare of systemic lupus erythematodes in a female patient. J Clin Virol. 1999;14(1):73–77. doi: 10.1016/S1386-6532(99)00038-4. [DOI] [PubMed] [Google Scholar]
- 104.Hrycek A, Kusmierz D, Mazurek U, Wilczok T. Human cytomegalovirus in patients with systemic lupus erythematosus. Autoimmunity. 2005;38(7):487–491. doi: 10.1080/08916930500285667. [DOI] [PubMed] [Google Scholar]
- 105.James JA, Neas BR, Moser KL, Hall T, Bruner GR, Sestak AL, et al. Systemic lupus erythematosus in adults is associated with previous Epstein-Barr virus exposure. Arthritis Rheum. 2001;44(5):1122–1126. doi: 10.1002/1529-0131(200105)44:5<1122::AID-ANR193>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 106.Seishima M, Oyama Z, Yamamura M. Two-year follow-up study after human parvovirus B19 infection. Dermatology. 2003;206(3):192–196. doi: 10.1159/000068885. [DOI] [PubMed] [Google Scholar]
- 107.Chang M, Pan MR, Chen DY, Lan JL. Human cytomegalovirus pp 65 lower matrix protein: a humoral immunogen for systemic lupus erythematosus patients and autoantibody accelerator for NZB/W F1 mice. Clin Exp Immunol. 2006;143(1):167–179. doi: 10.1111/j.1365-2249.2005.02974.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Gilden DH. Infectious causes of multiple sclerosis. Lancet Neurol. 2005;4(3):195–202. doi: 10.1016/S1474-4422(05)01017-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kakalacheva K, Lunemann JD. Environmental triggers of multiple sclerosis. FEBS Lett. 2011 doi: 10.1016/j.febslet.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 110.Hammond SR, English DR, McLeod JG. The age-range of risk of developing multiple sclerosis: evidence from a migrant population in Australia. Brain. 2000;123(Pt 5):968–974. doi: 10.1093/brain/123.5.968. [DOI] [PubMed] [Google Scholar]
- 111.Kurtzke JF, Delasnerie-Laupretre N, Wallin MT. Multiple sclerosis in North African migrants to France. Acta Neurol Scand. 1998;98(5):302–309. doi: 10.1111/j.1600-0404.1998.tb01738.x. [DOI] [PubMed] [Google Scholar]
- 112.Kurtzke JF, Hyllested K. Multiple sclerosis in the Faroe Islands: i Clinical and epidemiological features. Ann Neurol. 1979;5(1):6–21. doi: 10.1002/ana.410050104. [DOI] [PubMed] [Google Scholar]
- 113.Noseworthy JH, Lucchinetti C, Rodriguez M, Weinshenker BG. Multiple sclerosis. N Engl J Med. 2000;343(13):938–952. doi: 10.1056/NEJM200009283431307. [DOI] [PubMed] [Google Scholar]
- 114.Frohman EM, Racke MK, Raine CS. Multiple sclerosis–the plaque and its pathogenesis. N Engl J Med. 2006;354(9):942–955. doi: 10.1056/NEJMra052130. [DOI] [PubMed] [Google Scholar]
- 115.Ebers GC, Sadovnick AD, Risch NJ. A genetic basis for familial aggregation in multiple sclerosis Canadian collaborative study group. Nature. 1995;377(6545):150–151. doi: 10.1038/377150a0. [DOI] [PubMed] [Google Scholar]
- 116.Sadovnick AD, Ebers GC, Dyment DA, Risch NJ. Evidence for genetic basis of multiple sclerosis the Canadian collaborative study group. Lancet. 1996;347(9017):1728–1730. doi: 10.1016/S0140-6736(96)90807-7. [DOI] [PubMed] [Google Scholar]
- 117.Barcellos LF, Sawcer S, Ramsay PP, Baranzini SE, Thomson G, Briggs F, et al. Heterogeneity at the HLA-DRB1 locus and risk for multiple sclerosis. Hum Mol Genet. 2006;15(18):2813–2824. doi: 10.1093/hmg/ddl223. [DOI] [PubMed] [Google Scholar]
- 118.Hafler DA, Compston A, Sawcer S, Lander ES, Daly MJ, De Jager PL, et al. Risk alleles for multiple sclerosis identified by a genomewide study. N Engl J Med. 2007;357(9):851–862. doi: 10.1056/NEJMoa073493. [DOI] [PubMed] [Google Scholar]
- 119.Qu HQ, Bradfield JP, Belisle A, Grant SF, Hakonarson H, Polychronakos C. The type I diabetes association of the IL2RA locus. Genes Immun. 2009;10(Suppl 1):S42–S48. doi: 10.1038/gene.2009.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Giovannoni G, Cutter GR, Lunemann J, Martin R, Munz C, Sriram S, et al. Infectious causes of multiple sclerosis. Lancet Neurol. 2006;5(10):887–894. doi: 10.1016/S1474-4422(06)70577-4. [DOI] [PubMed] [Google Scholar]
- 121.Giovannoni G, Ebers G. Multiple sclerosis: the environment and causation. Curr Opin Neurol. 2007;20(3):261–268. doi: 10.1097/WCO.0b013e32815610c2. [DOI] [PubMed] [Google Scholar]
- 122.Arnson Y, Amital H, Shoenfeld Y. Vitamin D and autoimmunity: new aetiological and therapeutic considerations. Ann Rheum Dis. 2007;66(9):1137–1142. doi: 10.1136/ard.2007.069831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Carvalho JF, Blank M, Kiss E, Tarr T, Amital H, Shoenfeld Y. Anti-vitamin D, vitamin D in SLE: preliminary results. Ann N Y Acad Sci. 2007;1109:550–557. doi: 10.1196/annals.1398.061. [DOI] [PubMed] [Google Scholar]
- 124.Shoenfeld N, Amital H, Shoenfeld Y. The effect of melanism and vitamin D synthesis on the incidence of autoimmune disease. Nat Clin Pract Rheumatol. 2009;5(2):99–105. doi: 10.1038/ncprheum0989. [DOI] [PubMed] [Google Scholar]
- 125.Shapira Y, Agmon-Levin N, Shoenfeld Y. Mycobacterium tuberculosis, autoimmunity, and vitamin D. Clin Rev Allergy Immunol. 2010;38(2–3):169–177. doi: 10.1007/s12016-009-8150-1. [DOI] [PubMed] [Google Scholar]
- 126.Amital H, Szekanecz Z, Szucs G, Danko K, Nagy E, Csepany T, et al. Serum concentrations of 25-OH vitamin D in patients with systemic lupus erythematosus (SLE) are inversely related to disease activity: is it time to routinely supplement patients with SLE with vitamin D? Ann Rheum Dis. 2010;69(6):1155–1157. doi: 10.1136/ard.2009.120329. [DOI] [PubMed] [Google Scholar]
- 127.Toubi E, Shoenfeld Y. The role of vitamin D in regulating immune responses. Isr Med Assoc J. 2010;12(3):174–175. [PubMed] [Google Scholar]
- 128.Souberbielle JC, Body JJ, Lappe JM, Plebani M, Shoenfeld Y, Wang TJ, et al. Vitamin D and musculoskeletal health, cardiovascular disease, autoimmunity and cancer: recommendations for clinical practice. Autoimmun Rev. 2010;9(11):709–715. doi: 10.1016/j.autrev.2010.06.009. [DOI] [PubMed] [Google Scholar]
- 129.Agmon-Levin N, Blank M, Zandman-Goddard G, Orbach H, Meroni PL, Tincani A, et al. Vitamin D: an instrumental factor in the anti-phospholipid syndrome by inhibition of tissue factor expression. Ann Rheum Dis. 2011;70(1):145–150. doi: 10.1136/ard.2010.134817. [DOI] [PubMed] [Google Scholar]
- 130.Oren Y, Shapira Y, Agmon-Levin N, Kivity S, Zafrir Y, Altman A, et al. Vitamin D insufficiency in a sunny environment: a demographic and seasonal analysis. Isr Med Assoc J. 2010;12(12):751–756. [PubMed] [Google Scholar]
- 131.Kivity S, Agmon-Levin N, Zisappl M, Shapira Y, Nagy EV, Danko K, et al. Vitamin D and autoimmune thyroid diseases. Cell Mol Immunol. 2011;8(3):243–247. doi: 10.1038/cmi.2010.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Lerner A, Shapira Y, Agmon-Levin N, Pacht A, Ben Ami Shor D, Lopez HM, et al. The clinical significance of 25OH-Vitamin D status in celiac disease. Clin Rev Allergy Immunol. 2012;42(3):322–330. doi: 10.1007/s12016-010-8237-8. [DOI] [PubMed] [Google Scholar]
- 133.Hajas A, Sandor J, Csathy L, Csipo I, Barath S, Paragh G, et al. Vitamin D insufficiency in a large MCTD population. Autoimmun Rev. 2011;10(6):317–324. doi: 10.1016/j.autrev.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 134.Cutolo M, Pizzorni C, Sulli A. Vitamin D endocrine system involvement in autoimmune rheumatic diseases. Autoimmun Rev. 2011;11(2):84–87. doi: 10.1016/j.autrev.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 135.Lucas RM, Ponsonby AL, Dear K, Valery PC, Pender MP, Taylor BV, et al. Sun exposure and vitamin D are independent risk factors for CNS demyelination. Neurology. 2011;76(6):540–548. doi: 10.1212/WNL.0b013e31820af93d. [DOI] [PubMed] [Google Scholar]
- 136.Munger KL, Levin LI, Hollis BW, Howard NS, Ascherio A. Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis. JAMA. 2006;296(23):2832–2838. doi: 10.1001/jama.296.23.2832. [DOI] [PubMed] [Google Scholar]
- 137.Handel AE, Williamson AJ, Disanto G, Dobson R, Giovannoni G, Ramagopalan SV. Smoking and multiple sclerosis: an updated meta-analysis. PLoS ONE. 2011;6(1):e16149. doi: 10.1371/journal.pone.0016149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Hedstrom AK, Sundqvist E, Baarnhielm M, Nordin N, Hillert J, Kockum I, et al. Smoking and two human leukocyte antigen genes interact to increase the risk for multiple sclerosis. Brain. 2011;134(Pt 3):653–664. doi: 10.1093/brain/awq371. [DOI] [PubMed] [Google Scholar]
- 139.Stejskal V, Hudecek R, Stejskal J, Sterzl I. Diagnosis and treatment of metal-induced side-effects. Neuro Endocrinol Lett. 2006;27(Suppl 1):7–16. [PubMed] [Google Scholar]
- 140.Fleming JO. Helminths and multiple sclerosis: will old friends give us new treatments for MS? J Neuroimmunol. 2011;233(1–2):3–5. doi: 10.1016/j.jneuroim.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 141.Gaisford W, Cooke A. Can infections protect against autoimmunity? Curr Opin Rheumatol. 2009;21(4):391–396. doi: 10.1097/BOR.0b013e32832c2dee. [DOI] [PubMed] [Google Scholar]
- 142.Kim JS, Lee KS, Park JH, Kim MY, Shin WS. Detection of human herpesvirus 6 variant A in peripheral blood mononuclear cells from multiple sclerosis patients. Eur Neurol. 2000;43(3):170–173. doi: 10.1159/000008158. [DOI] [PubMed] [Google Scholar]
- 143.Opsahl ML, Kennedy PG. Early and late HHV-6 gene transcripts in multiple sclerosis lesions and normal appearing white matter. Brain. 2005;128(Pt 3):516–527. doi: 10.1093/brain/awh390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Albright AV, Lavi E, Black JB, Goldberg S, O’Connor MJ, Gonzalez-Scarano F. The effect of human herpesvirus-6 (HHV-6) on cultured human neural cells: oligodendrocytes and microglia. J Neurovirol. 1998;4(5):486–494. doi: 10.3109/13550289809113493. [DOI] [PubMed] [Google Scholar]
- 145.Chan PK, Ng HK, Cheng AF. Detection of human herpesviruses 6 and 7 genomic sequences in brain tumours. J Clin Path. 1999;52(8):620–623. doi: 10.1136/jcp.52.8.620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Mirandola P, Stefan A, Brambilla E, Campadelli-Fiume G, Grimaldi LM. Absence of human herpesvirus 6 and 7 from spinal fluid and serum of multiple sclerosis patients. Neurology. 1999;53(6):1367–1368. doi: 10.1212/WNL.53.6.1367-a. [DOI] [PubMed] [Google Scholar]
- 147.Sospedra M, Zhao Y, ZurHausen H, Muraro PA, Hamashin C, DeVilliers EM, et al. Recognition of conserved amino acid motifs of common viruses and its role in autoimmunity. PLoS Pathog. 2005;1(4):e41. doi: 10.1371/journal.ppat.0010041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Bogdanos DP, Gershwin ME. What is new in primary biliary cirrhosis? Dig Dis. 2012;30(Suppl 1):20–31. doi: 10.1159/000341118. [DOI] [PubMed] [Google Scholar]
- 149.Corpechot C, Chretien Y, Chazouilleres O, Poupon R. Demographic, lifestyle, medical and familial factors associated with primary biliary cirrhosis. J Hepatol. 2010;53(1):162–169. doi: 10.1016/j.jhep.2010.02.019. [DOI] [PubMed] [Google Scholar]
- 150.Gershwin ME, Selmi C, Worman HJ, Gold EB, Watnik M, Utts J, et al. Risk factors and comorbidities in primary biliary cirrhosis: a controlled interview-based study of 1032 patients. Hepatology. 2005;42(5):1194–1202. doi: 10.1002/hep.20907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Parikh-Patel A, Gold EB, Worman H, Krivy KE, Gershwin ME. Risk factors for primary biliary cirrhosis in a cohort of patients from the United States. Hepatology. 2001;33(1):16–21. doi: 10.1053/jhep.2001.21165. [DOI] [PubMed] [Google Scholar]
- 152.Prince MI, Ducker SJ, James OF. Case-control studies of risk factors for primary biliary cirrhosis in two United Kingdom populations. Gut. 2010;59(4):508–512. doi: 10.1136/gut.2009.184218. [DOI] [PubMed] [Google Scholar]
- 153.Invernizzi P, Selmi C, Gershwin ME. Update on primary biliary cirrhosis. Dig Liver Dis. 2010;42(6):401–408. doi: 10.1016/j.dld.2010.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Selmi C, Invernizzi P, Zuin M, Podda M, Gershwin ME. Genetics and geoepidemiology of primary biliary cirrhosis: following the footprints to disease etiology. Semin Liver Dis. 2005;25(3):265–280. doi: 10.1055/s-2005-916319. [DOI] [PubMed] [Google Scholar]
- 155.Selmi C, Invernizzi P, Zuin M, Podda M, Seldin MF, Gershwin ME. Genes and (auto)immunity in primary biliary cirrhosis. Genes Immun. 2005;6(7):543–556. doi: 10.1038/sj.gene.6364248. [DOI] [PubMed] [Google Scholar]
- 156.Smyk D, Cholongitas E, Kriese S, Rigopoulou EI, Bogdanos DP. Primary biliary cirrhosis: family stories. Autoimmune Dis. 2011;2011:189585. doi: 10.4061/2011/189585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Bogdanos DP, Smyk DS, Rigopoulou EI, Mytilinaiou MG, Heneghan MA, Selmi C, et al. Twin studies in autoimmune disease: genetics, gender and environment. J Autoimmun. 2012;38(2–3):J156–J169. doi: 10.1016/j.jaut.2011.11.003. [DOI] [PubMed] [Google Scholar]
- 158.Gershwin ME, Mackay IR. The causes of primary biliary cirrhosis: convenient and inconvenient truths. Hepatology. 2008;47(2):737–745. doi: 10.1002/hep.22042. [DOI] [PubMed] [Google Scholar]
- 159.Konikoff F, Pecht M, Theodor E, Shoenfeld Y. Primary biliary cirrhosis: lymphocyte subsets and function in a time frame. Hepatology. 1989;10(4):525–526. doi: 10.1002/hep.1840100427. [DOI] [PubMed] [Google Scholar]
- 160.Schlesinger M, Benbassat C, Shoenfeld Y. Complement profile in primary biliary cirrhosis. Immunol Res. 1992;11(2):98–103. doi: 10.1007/BF02918614. [DOI] [PubMed] [Google Scholar]
- 161.Shoenfeld Y. Primary biliary cirrhosis and autoimmune rheumatic diseases: prediction and prevention. Isr J Med Sci. 1992;28(2):113–116. [PubMed] [Google Scholar]
- 162.Weiss P, Shoenfeld Y. Primary biliary cirrhosis is a multisystem disorder. Ann Med Interne (Paris) 1991;142(4):283–287. [PubMed] [Google Scholar]
- 163.Weiss P, Shoenfeld Y. Primary biliary cirrhosis: increasing problem, approaching solution. Isr J Med Sci. 1992;28(10):726–728. [PubMed] [Google Scholar]
- 164.Benbassat C, Schlesinger M, Shoenfeld Y. The complement system and primary biliary cirrhosis. J Clin Lab Immunol. 1992;38(2):51–61. [PubMed] [Google Scholar]
- 165.Rotman P, Levy Y, Shoenfeld Y. Primary biliary cirrhosis–association or overlap with other autoimmune diseases. Isr J Med Sci. 1997;33(12):823–825. [PubMed] [Google Scholar]
- 166.Shapira S, Bar-Dayan Y, Gershwin ME, Shoenfeld Y. Is it possible to predict and prevent primary biliary cirrhosis? Harefuah. 1999;137(1–2):39–41. [PubMed] [Google Scholar]
- 167.Aoki CA, Roifman CM, Lian ZX, Bowlus CL, Norman GL, Shoenfeld Y, et al. IL-2 receptor alpha deficiency and features of primary biliary cirrhosis. J Autoimmun. 2006;27(1):50–53. doi: 10.1016/j.jaut.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 168.Barak V, Selmi C, Schlesinger M, Blank M, Agmon-Levin N, Kalickman I, et al. Serum inflammatory cytokines, complement components, and soluble interleukin 2 receptor in primary biliary cirrhosis. J Autoimmun. 2009;33(3–4):178–182. doi: 10.1016/j.jaut.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 169.Bogdanos DP, Baum H, Vergani D. Antimitochondrial and other autoantibodies. Clin Liver Dis. 2003;7(4):759–777. doi: 10.1016/S1089-3261(03)00104-1. [DOI] [PubMed] [Google Scholar]
- 170.Bogdanos DP, Baum H, Vergani D, Burroughs AK. The role of E. coli infection in the pathogenesis of primary biliary cirrhosis. Dis Markers. 2010;29(6):301–311. doi: 10.1155/2010/595078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Bogdanos DP, Vergani D. Origin of cross-reactive autoimmunity in primary biliary cirrhosis. Liver Int. 2006;26(6):633–635. doi: 10.1111/j.1478-3231.2006.01291.x. [DOI] [PubMed] [Google Scholar]
- 172.Bogdanos DP, Vergani D. Bacteria and primary biliary cirrhosis. Clin Rev Allergy Immunol. 2009;36(1):30–39. doi: 10.1007/s12016-008-8087-9. [DOI] [PubMed] [Google Scholar]
- 173.Gershwin ME, Mackay IR. Primary biliary cirrhosis: paradigm or paradox for autoimmunity. Gastroenterology. 1991;100(3):822–833. doi: 10.1016/0016-5085(91)80033-6. [DOI] [PubMed] [Google Scholar]
- 174.Mackay IR, Whittingham S, Fida S, Myers M, Ikuno N, Gershwin ME, et al. The peculiar autoimmunity of primary biliary cirrhosis. Immunol Rev. 2000;174:226–237. doi: 10.1034/j.1600-0528.2002.017410.x. [DOI] [PubMed] [Google Scholar]
- 175.Shimoda S, Nakamura M, Ishibashi H, Hayashida K, Niho Y. HLA DRB4 0101-restricted immunodominant T cell autoepitope of pyruvate dehydrogenase complex in primary biliary cirrhosis: evidence of molecular mimicry in human autoimmune diseases. J Exp Med. 1995;181(5):1835–1845. doi: 10.1084/jem.181.5.1835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Shimoda S, Nakamura M, Shigematsu H, Tanimoto H, Gushima T, Gershwin ME, et al. Mimicry peptides of human PDC-E2 163–176 peptide, the immunodominant T-cell epitope of primary biliary cirrhosis. Hepatology. 2000;31(6):1212–1216. doi: 10.1053/jhep.2000.8090. [DOI] [PubMed] [Google Scholar]
- 177.Shimoda S, Van de Water J, Ansari A, Nakamura M, Ishibashi H, Coppel RL, et al. Identification and precursor frequency analysis of a common T cell epitope motif in mitochondrial autoantigens in primary biliary cirrhosis. J Clin Invest. 1998;102(10):1831–1840. doi: 10.1172/JCI4213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Vergani D, Bogdanos DP. Positive markers in AMA-negative PBC. Am J Gastroenterol. 2003;98(2):241–243. doi: 10.1111/j.1572-0241.2003.07270.x. [DOI] [PubMed] [Google Scholar]
- 179.Hohenester S, Oude-Elferink RP, Beuers U. Primary biliary cirrhosis. Semin Immunopathol. 2009;31(3):283–307. doi: 10.1007/s00281-009-0164-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Neuberger J. Primary biliary cirrhosis. Lancet. 1997;350(9081):875–879. doi: 10.1016/S0140-6736(97)05419-6. [DOI] [PubMed] [Google Scholar]
- 181.Bogdanos DP, Invernizzi P, Mackay IR, Vergani D. Autoimmune liver serology: current diagnostic and clinical challenges. World J Gastroenterol. 2008;14(21):3374–3387. doi: 10.3748/wjg.14.3374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Bogdanos DP, Komorowski L. Disease-specific autoantibodies in primary biliary cirrhosis. Clin Chim Acta. 2011;412(7–8):502–512. doi: 10.1016/j.cca.2010.12.019. [DOI] [PubMed] [Google Scholar]
- 183.Dahnrich C, Pares A, Caballeria L, Rosemann A, Schlumberger W, Probst C, et al. New ELISA for detecting primary biliary cirrhosis-specific antimitochondrial antibodies. Clin Chem. 2009;55(5):978–985. doi: 10.1373/clinchem.2008.118299. [DOI] [PubMed] [Google Scholar]
- 184.Liu H, Norman GL, Shums Z, Worman HJ, Krawitt EL, Bizzaro N, et al. PBC screen: an IgG/IgA dual isotype ELISA detecting multiple mitochondrial and nuclear autoantibodies specific for primary biliary cirrhosis. J Autoimmun. 2010;35(4):436–442. doi: 10.1016/j.jaut.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 185.Ma Y, Thomas MG, Okamoto M, Bogdanos DP, Nagl S, Kerkar N, et al. Key residues of a major cytochrome P4502D6 epitope are located on the surface of the molecule. J Immunol. 2002;169(1):277–285. doi: 10.4049/jimmunol.169.1.277. [DOI] [PubMed] [Google Scholar]
- 186.Rigopoulou EI, Davies ET, Bogdanos DP, Liaskos C, Mytilinaiou M, Koukoulis GK, et al. Antimitochondrial antibodies of immunoglobulin G3 subclass are associated with a more severe disease course in primary biliary cirrhosis. Liver Int. 2007;27(9):1226–1231. doi: 10.1111/j.1478-3231.2007.01586.x. [DOI] [PubMed] [Google Scholar]
- 187.Wen L, Ma Y, Bogdanos DP, Wong FS, Demaine A, Mieli-Vergani G, et al. Pediatric autoimmune liver diseases: the molecular basis of humoral and cellular immunity. Curr Molec Med. 2001;1(3):379–389. doi: 10.2174/1566524013363672. [DOI] [PubMed] [Google Scholar]
- 188.Invernizzi P, Lleo A, Podda M. Interpreting serological tests in diagnosing autoimmune liver diseases. Semin Liver Dis. 2007;27(2):161–172. doi: 10.1055/s-2007-979469. [DOI] [PubMed] [Google Scholar]
- 189.Rigopoulou EI, Bogdanos DP, Liaskos C, Koutsoumpas A, Baum H, Vergani D, et al. Anti-mitochondrial antibody immunofluorescent titres correlate with the number and intensity of immunoblot-detected mitochondrial bands in patients with primary biliary cirrhosis. Clin Chim Acta. 2007;380(1–2):118–121. doi: 10.1016/j.cca.2007.01.023. [DOI] [PubMed] [Google Scholar]
- 190.Gilburd B, Ziporen L, Zharhary D, Blank M, Zurgil N, Scheinberg MA, et al. Antimitochondrial (pyruvate dehydrogenase) antibodies in leprosy. J Clin Immunol. 1994;14(1):14–19. doi: 10.1007/BF01541171. [DOI] [PubMed] [Google Scholar]
- 191.Konikoff F, Isenberg DA, Barrison I, Theodor E, Shoenfeld Y. Antinuclear autoantibodies in chronic liver diseases. Hepatogastroenterology. 1989;36(5):341–345. [PubMed] [Google Scholar]
- 192.Konikoff F, Isenberg DA, Kooperman O, Kennedy RC, Rauch J, Theodor E, et al. Common lupus anti-DNA antibody idiotypes in chronic liver diseases. Clin Immunol Immunopathol. 1987;43(2):265–272. doi: 10.1016/0090-1229(87)90134-6. [DOI] [PubMed] [Google Scholar]
- 193.Konikoff F, Shoenfeld Y, Isenberg DA, Barrison I, Sobe T, Theodor E, et al. Anti-Rnp antibodies in chronic liver diseases. Clin Exp Rheumatol. 1987;5(4):359–361. [PubMed] [Google Scholar]
- 194.Krause I, Hacham S, Gilburd B, Damianovitch M, Blank M, Shoenfeld Y. Absence of anti-idiotypic antibodies in IVIG preparations to autoantibodies of rare autoimmune diseases. Clin Immunol Immunopathol. 1995;77(3):229–235. doi: 10.1006/clin.1995.1148. [DOI] [PubMed] [Google Scholar]
- 195.Lorber M, Kra-Oz Z, Guilbrud B, Shoenfeld Y. Natural (antiphospholipid-PDH,-DNA) autoantibodies and their physiologic serum inhibitors. Isr J Med Sci. 1995;31(1):31–35. [PubMed] [Google Scholar]
- 196.Maran R, Dueymes M, Adler Y, Shoenfeld Y, Youinou P. Isotypic distribution of anti-pyruvate dehydrogenase antibodies in patients with primary biliary cirrhosis and their family members. J Clin Immunol. 1994;14(5):323–326. doi: 10.1007/BF01540986. [DOI] [PubMed] [Google Scholar]
- 197.Shoenfeld Y, Beresovski A, Zharhary D, Tomer Y, Swissa M, Sela E, et al. Natural autoantibodies in sera of patients with Gaucher’s disease. J Clin Immunol. 1995;15(6):363–372. doi: 10.1007/BF01541326. [DOI] [PubMed] [Google Scholar]
- 198.Zurgil N, Bakimer R, Kaplan M, Youinou P, Shoenfeld Y. Anti-pyruvate dehydrogenase autoantibodies in primary biliary cirrhosis. J Clin Immunol. 1991;11(5):239–245. doi: 10.1007/BF00918181. [DOI] [PubMed] [Google Scholar]
- 199.Zurgil N, Bakimer R, Moutsopoulos HM, Tzioufas AG, Youinou P, Isenberg DA, et al. Antimitochondrial (pyruvate dehydrogenase) autoantibodies in autoimmune rheumatic diseases. J Clin Immunol. 1992;12(3):201–209. doi: 10.1007/BF00918090. [DOI] [PubMed] [Google Scholar]
- 200.Zurgil N, Bakimer R, Slor H, Kaplan M, Moutsopoulos H, Shoenfeld Y. Pyruvate dehydrogenase as an antigen to detect antimitochondrial antibodies. Isr J Med Sci. 1990;26(12):682–685. [PubMed] [Google Scholar]
- 201.Zurgil N, Konikoff F, Bakimer R, Slor H, Shoenfeld Y. Detection of antimitochondrial antibodies: characterization by enzyme immunoassay and immunoblotting. Autoimmunity. 1989;4(4):289–297. doi: 10.3109/08916938909014705. [DOI] [PubMed] [Google Scholar]
- 202.Tishler M, Alosachie I, Barka N, Lin HC, Gershwin ME, Peter JB, et al. Primary Sjogren’s syndrome and primary biliary cirrhosis: differences and similarities in the autoantibody profile. Clin Exp Rheumatol. 1995;13(4):497–500. [PubMed] [Google Scholar]
- 203.Bean P, Sutphin MS, Liu Y, Anton R, Reynolds TB, Shoenfeld Y, et al. Carbohydrate-deficient transferrin and false-positive results for alcohol abuse in primary biliary cirrhosis: differential diagnosis by detection of mitochondrial autoantibodies. Clin Chem. 1995;41(6 Pt 1):858–861. [PubMed] [Google Scholar]
- 204.Agmon-Levin N, Shapira Y, Selmi C, Barzilai O, Ram M, Szyper-Kravitz M, et al. A comprehensive evaluation of serum autoantibodies in primary biliary cirrhosis. J Autoimmun. 2010;34(1):55–58. doi: 10.1016/j.jaut.2009.08.009. [DOI] [PubMed] [Google Scholar]
- 205.Metcalf JV, Mitchison HC, Palmer JM, Jones DE, Bassendine MF, James OF. Natural history of early primary biliary cirrhosis. Lancet. 1996;348(9039):1399–1402. doi: 10.1016/S0140-6736(96)04410-8. [DOI] [PubMed] [Google Scholar]
- 206.Dubel L, Tanaka A, Leung PS, Van de Water J, Coppel R, Roche T, et al. Autoepitope mapping and reactivity of autoantibodies to the dihydrolipoamide dehydrogenase-binding protein (E3BP) and the glycine cleavage proteins in primary biliary cirrhosis. Hepatology. 1999;29(4):1013–1018. doi: 10.1002/hep.510290403. [DOI] [PubMed] [Google Scholar]
- 207.Leung PS, Coppel RL, Ansari A, Munoz S, Gershwin ME. Antimitochondrial antibodies in primary biliary cirrhosis. Semin Liver Dis. 1997;17(1):61–69. doi: 10.1055/s-2007-1007183. [DOI] [PubMed] [Google Scholar]
- 208.Palmer JM, Jones DE, Quinn J, McHugh A, Yeaman SJ. Characterization of the autoantibody responses to recombinant E3 binding protein (protein X) of pyruvate dehydrogenase in primary biliary cirrhosis. Hepatology. 1999;30(1):21–26. doi: 10.1002/hep.510300106. [DOI] [PubMed] [Google Scholar]
- 209.Van de Water J, Fregeau D, Davis P, Ansari A, Danner D, Leung P, et al. Autoantibodies of primary biliary cirrhosis recognize dihydrolipoamide acetyltransferase and inhibit enzyme function. J Immunol. 1988;141(7):2321–2324. [PubMed] [Google Scholar]
- 210.Bogdanos DP, Liaskos C, Pares A, Norman G, Rigopoulou EI, Caballeria L, et al. Anti-gp210 antibody mirrors disease severity in primary biliary cirrhosis. Hepatology. 2007;45(6):1583. doi: 10.1002/hep.21678. [DOI] [PubMed] [Google Scholar]
- 211.Invernizzi P, Podda M, Battezzati PM, Crosignani A, Zuin M, Hitchman E, et al. Autoantibodies against nuclear pore complexes are associated with more active and severe liver disease in primary biliary cirrhosis. J Hepatol. 2001;34(3):366–372. doi: 10.1016/S0168-8278(00)00040-4. [DOI] [PubMed] [Google Scholar]
- 212.Miyachi K, Hankins RW, Matsushima H, Kikuchi F, Inomata T, Horigome T, et al. Profile and clinical significance of anti-nuclear envelope antibodies found in patients with primary biliary cirrhosis: a multicenter study. J Autoimmun. 2003;20(3):247–254. doi: 10.1016/S0896-8411(03)00033-7. [DOI] [PubMed] [Google Scholar]
- 213.Nakamura M, Kondo H, Mori T, Komori A, Matsuyama M, Ito M, et al. Anti-gp210 and anti-centromere antibodies are different risk factors for the progression of primary biliary cirrhosis. Hepatology. 2007;45(1):118–127. doi: 10.1002/hep.21472. [DOI] [PubMed] [Google Scholar]
- 214.Rigopoulou EI, Davies ET, Pares A, Zachou K, Liaskos C, Bogdanos DP, et al. Prevalence and clinical significance of isotype specific antinuclear antibodies in primary biliary cirrhosis. Gut. 2005;54(4):528–532. doi: 10.1136/gut.2003.036558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Itoh S, Ichida T, Yoshida T, Hayakawa A, Uchida M, Tashiro-Itoh T, et al. Autoantibodies against a 210 kDa glycoprotein of the nuclear pore complex as a prognostic marker in patients with primary biliary cirrhosis. J Gastroenterol Hepatol. 1998;13(3):257–265. doi: 10.1111/j.1440-1746.1998.01553.x. [DOI] [PubMed] [Google Scholar]
- 216.Lassoued K, Guilly MN, Andre C, Paintrand M, Dhumeaux D, Danon F, et al. Autoantibodies to 200 kD polypeptide(s) of the nuclear envelope: a new serologic marker of primary biliary cirrhosis. Clin Exp Immunol. 1988;74(2):283–288. [PMC free article] [PubMed] [Google Scholar]
- 217.Muratori P, Muratori L, Ferrari R, Cassani F, Bianchi G, Lenzi M, et al. Characterization and clinical impact of antinuclear antibodies in primary biliary cirrhosis. Am J Gastroenterol. 2003;98(2):431–437. doi: 10.1111/j.1572-0241.2003.07257.x. [DOI] [PubMed] [Google Scholar]
- 218.Wesierska-Gadek J, Penner E, Battezzati PM, Selmi C, Zuin M, Hitchman E, et al. Correlation of initial autoantibody profile and clinical outcome in primary biliary cirrhosis. Hepatology. 2006;43(5):1135–1144. doi: 10.1002/hep.21172. [DOI] [PubMed] [Google Scholar]
- 219.Yang WH, Yu JH, Nakajima A, Neuberg D, Lindor K, Bloch DB. Do antinuclear antibodies in primary biliary cirrhosis patients identify increased risk for liver failure? Clin Gastroenterol Hepatol. 2004;2(12):1116–1122. doi: 10.1016/S1542-3565(04)00465-3. [DOI] [PubMed] [Google Scholar]
- 220.Duarte-Rey C, Bogdanos D, Yang CY, Roberts K, Leung PS, Anaya JM, et al. Primary biliary cirrhosis and the nuclear pore complex. Autoimmun Rev. 2012;11(12):898–902. doi: 10.1016/j.autrev.2012.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Duarte-Rey C, Bogdanos DP, Leung PS, Anaya JM, Gershwin ME. IgM predominance in autoimmune disease: genetics and gender. Autoimmun Rev. 2012;11(6–7):A404–A412. doi: 10.1016/j.autrev.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 222.Bach N, Schaffner F. Familial primary biliary cirrhosis. J Hepatol. 1994;20(6):698–701. doi: 10.1016/S0168-8278(05)80137-0. [DOI] [PubMed] [Google Scholar]
- 223.Floreani A, Naccarato R, Chiaramonte M. Prevalence of familial disease in primary biliary cirrhosis in Italy. J Hepatol. 1997;26(3):737–738. doi: 10.1016/S0168-8278(97)80444-8. [DOI] [PubMed] [Google Scholar]
- 224.Tsuji K, Watanabe Y, Van De Water J, Nakanishi T, Kajiyama G, Parikh-Patel A, et al. Familial primary biliary cirrhosis in Hiroshima. J Autoimmun. 1999;13(1):171–178. doi: 10.1006/jaut.1999.0299. [DOI] [PubMed] [Google Scholar]
- 225.Lazaridis KN, Juran BD, Boe GM, Slusser JP, de Andrade M, Homburger HA, et al. Increased prevalence of antimitochondrial antibodies in first-degree relatives of patients with primary biliary cirrhosis. Hepatology. 2007;46(3):785–792. doi: 10.1002/hep.21749. [DOI] [PubMed] [Google Scholar]
- 226.Douglas JG, Finlayson ND. Are increased individual susceptibility and environmental factors both necessary for the development of primary biliary cirrhosis? BMJ. 1979;2(6187):419–420. doi: 10.1136/bmj.2.6187.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Fagan E, Williams R, Cox S. Primary biliary cirrhosis in mother and daughter. BMJ. 1977;2(6096):1195. doi: 10.1136/bmj.2.6096.1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Tong MJ, Nies KM, Reynolds TB, Quismorio FP. Immunological studies in familial primary biliary cirrhosis. Gastroenterology. 1976;71(2):305–307. [PubMed] [Google Scholar]
- 229.Smyk DS, Rigopoulou EI, Bogdanos DP. Potential roles for infectious agents in the pathophysiology of primary biliary cirrhosis: what’s new? Curr Infect Dis Rep. 2012 doi: 10.1007/s11908-012-0304-2. [DOI] [PubMed] [Google Scholar]
- 230.Chuang YH, Ridgway WM, Ueno Y, Gershwin ME. Animal models of primary biliary cirrhosis. Clin Liver Dis. 2008;12(2):333–347. doi: 10.1016/j.cld.2008.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Hirschfield GM, Invernizzi P. Progress in the genetics of primary biliary cirrhosis. Semin Liver Dis. 2011;31(2):147–156. doi: 10.1055/s-0031-1276644. [DOI] [PubMed] [Google Scholar]
- 232.Lleo A, Invernizzi P, Mackay IR, Prince H, Zhong RQ, Gershwin ME. Etiopathogenesis of primary biliary cirrhosis. World J Gastroenterol. 2008;14(21):3328–3337. doi: 10.3748/wjg.14.3328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Selmi C, Zuin M, Gershwin ME. The unfinished business of primary biliary cirrhosis. J Hepatol. 2008;49(3):451–460. doi: 10.1016/j.jhep.2008.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Wu SJ, Yang YH, Tsuneyama K, Leung PS, Illarionov P, Gershwin ME, et al. Innate immunity and primary biliary cirrhosis: activated invariant natural killer T cells exacerbate murine autoimmune cholangitis and fibrosis. Hepatology. 2011;53(3):915–925. doi: 10.1002/hep.24113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Hirschfield GM, Gershwin ME. Primary biliary cirrhosis: one disease with many faces. Isr Med Assoc J. 2011;13(1):55–59. [PubMed] [Google Scholar]
- 236.Invernizzi P. Human leukocyte antigen in primary biliary cirrhosis: an old story now reviving. Hepatology. 2011 doi: 10.1002/hep.24414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Hemminki K, Li X, Sundquist K, Sundquist J. Shared familial aggregation of susceptibility to autoimmune diseases. Arthritis Rheum. 2009;60(9):2845–2847. doi: 10.1002/art.24749. [DOI] [PubMed] [Google Scholar]
- 238.Hirschfield GM, Liu X, Han Y, Gorlov IP, Lu Y, Xu C, et al. Variants at IRF5-TNPO3, 17q12-21 and MMEL1 are associated with primary biliary cirrhosis. Nat Genet. 2010;42(8):655–657. doi: 10.1038/ng.631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Hirschfield GM, Liu X, Xu C, Lu Y, Xie G, Gu X, et al. Primary biliary cirrhosis associated with HLA, IL12A, and IL12RB2 variants. N Engl J Med. 2009;360(24):2544–2555. doi: 10.1056/NEJMoa0810440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Liu X, Invernizzi P, Lu Y, Kosoy R, Bianchi I, Podda M, et al. Genome-wide meta-analyses identify three loci associated with primary biliary cirrhosis. Nat Genet. 2010;42(8):658–660. doi: 10.1038/ng.627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Mells GF, Floyd JA, Morley KI, Cordell HJ, Franklin CS, Shin SY, et al. Genome-wide association study identifies 12 new susceptibility loci for primary biliary cirrhosis. Nat Genet. 2011;43(4):329–332. doi: 10.1038/ng.789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Tanaka A, Invernizzi P, Ohira H, Kikuchi K, Nezu S, Kosoy R, et al. Replicated association of 17q12-21 with susceptibility of primary biliary cirrhosis in a Japanese cohort. Tissue Antigens. 2011;78(1):65–68. doi: 10.1111/j.1399-0039.2011.01684.x. [DOI] [PubMed] [Google Scholar]
- 243.Tanaka A, Ohira H, Kikuchi K, Nezu S, Shibuya A, Bianchi I, et al. Genetic association of Fc receptor-like 3 polymorphisms with susceptibility to primary biliary cirrhosis: ethnic comparative study in Japanese and Italian patients. Tissue Antigens. 2011;77(3):239–243. doi: 10.1111/j.1399-0039.2010.01600.x. [DOI] [PubMed] [Google Scholar]
- 244.Invernizzi P, Miozzo M, Battezzati PM, Bianchi I, Grati FR, Simoni G, et al. Frequency of monosomy X in women with primary biliary cirrhosis. Lancet. 2004;363(9408):533–535. doi: 10.1016/S0140-6736(04)15541-4. [DOI] [PubMed] [Google Scholar]
- 245.Invernizzi P, Pasini S, Selmi C, Gershwin ME, Podda M. Female predominance and X chromosome defects in autoimmune diseases. J Autoimmun. 2009;33(1):12–16. doi: 10.1016/j.jaut.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 246.Miozzo M, Selmi C, Gentilin B, Grati FR, Sirchia S, Oertelt S, et al. Preferential X chromosome loss but random inactivation characterize primary biliary cirrhosis. Hepatology. 2007;46(2):456–462. doi: 10.1002/hep.21696. [DOI] [PubMed] [Google Scholar]
- 247.Bogdanos DP, Baum H, Butler P, Rigopoulou EI, Davies ET, Ma Y, et al. Association between the primary biliary cirrhosis specific anti-sp100 antibodies and recurrent urinary tract infection. Dig Liver Dis. 2003;35(11):801–805. doi: 10.1016/S1590-8658(03)00466-3. [DOI] [PubMed] [Google Scholar]
- 248.Bogdanos DP, Baum H, Grasso A, Okamoto M, Butler P, Ma Y, et al. Microbial mimics are major targets of crossreactivity with human pyruvate dehydrogenase in primary biliary cirrhosis. J Hepatol. 2004;40(1):31–39. doi: 10.1016/S0168-8278(03)00501-4. [DOI] [PubMed] [Google Scholar]
- 249.Bogdanos DP, Pares A, Rodes J, Vergani D. Primary biliary cirrhosis specific antinuclear antibodies in patients from Spain. Am J Gastroenterol. 2004;99(4):763. doi: 10.1111/j.1572-0241.2004.04119.x. [DOI] [PubMed] [Google Scholar]
- 250.Bogdanos DP, Baum H, Okamoto M, Montalto P, Sharma UC, Rigopoulou EI, et al. Primary biliary cirrhosis is characterized by IgG3 antibodies cross-reactive with the major mitochondrial autoepitope and its Lactobacillus mimic. Hepatology. 2005;42(2):458–465. doi: 10.1002/hep.20788. [DOI] [PubMed] [Google Scholar]
- 251.Bogdanos DP, Baum H, Sharma UC, Grasso A, Ma Y, Burroughs AK, et al. Antibodies against homologous microbial caseinolytic proteases P characterise primary biliary cirrhosis. J Hepatol. 2002;36(1):14–21. doi: 10.1016/S0168-8278(01)00252-5. [DOI] [PubMed] [Google Scholar]
- 252.Fussey SP, Lindsay JG, Fuller C, Perham RN, Dale S, James OF, et al. Autoantibodies in primary biliary cirrhosis: analysis of reactivity against eukaryotic and prokaryotic 2-oxo acid dehydrogenase complexes. Hepatology. 1991;13(3):467–474. doi: 10.1002/hep.1840130314. [DOI] [PubMed] [Google Scholar]
- 253.Koutsoumpas A, Mytilinaiou M, Polymeros D, Dalekos GN, Bogdanos DP. Anti-Helicobacter pylori antibody responses specific for VacA do not trigger primary biliary cirrhosis-specific antimitochondrial antibodies. Eur J Gastroenterol Hepatol. 2009;21(10):1220. doi: 10.1097/MEG.0b013e32831a4807. [DOI] [PubMed] [Google Scholar]
- 254.Abdulkarim AS, Petrovic LM, Kim WR, Angulo P, Lloyd RV, Lindor KD. Primary biliary cirrhosis: an infectious disease caused by Chlamydia pneumoniae? J Hepatol. 2004;40(3):380–384. doi: 10.1016/j.jhep.2003.11.033. [DOI] [PubMed] [Google Scholar]
- 255.Burroughs AK, Butler P, Sternberg MJ, Baum H. Molecular mimicry in liver disease. Nature. 1992;358(6385):377–378. doi: 10.1038/358377a0. [DOI] [PubMed] [Google Scholar]
- 256.Burroughs AK, Rosenstein IJ, Epstein O, Hamilton-Miller JM, Brumfitt W, Sherlock S. Bacteriuria and primary biliary cirrhosis. Gut. 1984;25(2):133–137. doi: 10.1136/gut.25.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Butler P, Hamilton-Miller J, Baum H, Burroughs AK. Detection of M2 antibodies in patients with recurrent urinary tract infection using an ELISA and purified PBC specific antigens. Evidence for a molecular mimicry mechanism in the pathogenesis of primary biliary cirrhosis? Biochem Mol Biol Int. 1995;35(3):473–485. [PubMed] [Google Scholar]
- 258.Butler P, Hamilton-Miller JM, McIntyre N, Burroughs AK. Natural history of bacteriuria in women with primary biliary cirrhosis and the effect of antimicrobial therapy in symptomatic and asymptomatic groups. Gut. 1995;36(6):931–934. doi: 10.1136/gut.36.6.931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Butler P, Valle F, Hamilton-Miller JM, Brumfitt W, Baum H, Burroughs AK. M2 mitochondrial antibodies and urinary rough mutant bacteria in patients with primary biliary cirrhosis and in patients with recurrent bacteriuria. J Hepatol. 1993;17(3):408–414. doi: 10.1016/S0168-8278(05)80225-9. [DOI] [PubMed] [Google Scholar]
- 260.Donaldson PT. Genetics of liver disease: immunogenetics and disease pathogenesis. Gut. 2004;53(4):599–608. doi: 10.1136/gut.2003.031732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Floreani A, Bassendine MF, Mitchison H, Freeman R, James OF. No specific association between primary biliary cirrhosis and bacteriuria? J Hepatol. 1989;8(2):201–207. doi: 10.1016/0168-8278(89)90008-1. [DOI] [PubMed] [Google Scholar]
- 262.Leung PS, Park O, Matsumura S, Ansari AA, Coppel RL, Gershwin ME. Is there a relation between Chlamydia infection and primary biliary cirrhosis? Clin Dev Immunol. 2003;10(2–4):227–233. doi: 10.1080/10446670310001642429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Mason A, Xu L, Shen Z, Fodera B, Joplin R, Neuberger J, et al. Patients with primary biliary cirrhosis make anti-viral and anti-mitochondrial antibodies to mouse mammary tumor virus. Gastroenterology. 2004;127(6):1863–5. doi: 10.1053/j.gastro.2004.10.024. [DOI] [PubMed] [Google Scholar]
- 264.McNally RJ, Ducker S, James OF. Are transient environmental agents involved in the cause of primary biliary cirrhosis? Evidence from space-time clustering analysis. Hepatology. 2009;50(4):1169–1174. doi: 10.1002/hep.23139. [DOI] [PubMed] [Google Scholar]
- 265.Selmi C, Balkwill DL, Invernizzi P, Ansari AA, Coppel RL, Podda M, et al. Patients with primary biliary cirrhosis react against a ubiquitous xenobiotic-metabolizing bacterium. Hepatology. 2003;38(5):1250–1257. doi: 10.1053/jhep.2003.50446. [DOI] [PubMed] [Google Scholar]
- 266.Smyk D, Mytilinaiou MG, Rigopoulou EI, Bogdanos DP. PBC triggers in water reservoirs, coal mining areas and waste disposal sites: from Newcastle to New York. Dis Markers. 2010;29(6):337–344. doi: 10.1155/2010/546926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Xu L, Sakalian M, Shen Z, Loss G, Neuberger J, Mason A. Cloning the human betaretrovirus proviral genome from patients with primary biliary cirrhosis. Hepatology. 2004;39(1):151–156. doi: 10.1002/hep.20024. [DOI] [PubMed] [Google Scholar]
- 268.Xu L, Shen Z, Guo L, Fodera B, Keogh A, Joplin R, et al. Does a betaretrovirus infection trigger primary biliary cirrhosis? Proc Natl Acad Sci U S A. 2003;100(14):8454–8459. doi: 10.1073/pnas.1433063100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Selmi C, De Santis M, Cavaciocchi F, Gershwin ME. Infectious agents and xenobiotics in the etiology of primary biliary cirrhosis. Dis Markers. 2010;29(6):287–299. doi: 10.1155/2010/752314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Bogdanos D, Pusl T, Rust C, Vergani D, Beuers U. Primary biliary cirrhosis following Lactobacillus vaccination for recurrent vaginitis. J Hepatol. 2008;49(3):466–473. doi: 10.1016/j.jhep.2008.05.022. [DOI] [PubMed] [Google Scholar]
- 271.Oldstone MB. Molecular mimicry and autoimmune disease. Cell. 1987;50(6):819–820. doi: 10.1016/0092-8674(87)90507-1. [DOI] [PubMed] [Google Scholar]
- 272.Bogdanos DP, Choudhuri K, Vergani D. Molecular mimicry and autoimmune liver disease: virtuous intentions, malign consequences. Liver. 2001;21(4):225–232. doi: 10.1034/j.1600-0676.2001.021004225.x. [DOI] [PubMed] [Google Scholar]
- 273.Vergani D, Bogdanos DP, Baum H. Unusual suspects in primary biliary cirrhosis. Hepatology. 2004;39(1):38–41. doi: 10.1002/hep.20028. [DOI] [PubMed] [Google Scholar]
- 274.Rigopoulou EI, Smyk DS, Matthews CE, Billinis C, Burroughs AK, Lenzi M, et al. Epstein-barr virus as a trigger of autoimmune liver diseases. Adv Virol. 2012;2012:987471. doi: 10.1155/2012/987471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Vergani D, Choudhuri K, Bogdanos DP, Mieli-Vergani G. Pathogenesis of autoimmune hepatitis. Clin Liver Dis. 2002;6(3):727–737. doi: 10.1016/S1089-3261(02)00018-1. [DOI] [PubMed] [Google Scholar]
- 276.Vergani D, Longhi MS, Bogdanos DP, Ma Y, Mieli-Vergani G. Autoimmune hepatitis. Semin Immunopathol. 2009;31(3):421–435. doi: 10.1007/s00281-009-0170-7. [DOI] [PubMed] [Google Scholar]
- 277.Ahn J, Yang L, Paster BJ, Ganly I, Morris L, Pei Z, et al. Oral microbiome profiles: 16S rRNA pyrosequencing and microarray assay comparison. PLoS ONE. 2011;6(7):e22788. doi: 10.1371/journal.pone.0022788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Arumugam M, Raes J, Pelletier E, Le Paslier D, Yamada T, Mende DR, et al. Enterotypes of the human gut microbiome. Nature. 2011;473(7346):174–180. doi: 10.1038/nature09944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Gill SR, Pop M, Deboy RT, Eckburg PB, Turnbaugh PJ, Samuel BS, et al. Metagenomic analysis of the human distal gut microbiome. Science. 2006;312(5778):1355–1359. doi: 10.1126/science.1124234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Kurokawa K, Itoh T, Kuwahara T, Oshima K, Toh H, Toyoda A, et al. Comparative metagenomics revealed commonly enriched gene sets in human gut microbiomes. DNA Res. 2007;14(4):169–181. doi: 10.1093/dnares/dsm018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Marchesi JR. Human distal gut microbiome. Environ Microbiol. 2011 doi: 10.1111/j.1462-2920.2011.02574.x. [DOI] [PubMed] [Google Scholar]
- 282.Qin J, Li R, Raes J, Arumugam M, Burgdorf KS, Manichanh C, et al. A human gut microbial gene catalogue established by metagenomic sequencing. Nature. 2010;464(7285):59–65. doi: 10.1038/nature08821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Saulnier DM, Riehle K, Mistretta TA, Diaz MA, Mandal D, Raza S, et al. Gastrointestinal microbiome signatures of pediatric patients with irritable bowel syndrome. Gastroenterology. 2011 doi: 10.1053/j.gastro.2011.06.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Siezen RJ, Kleerebezem M. The human gut microbiome: are we our enterotypes? Microbiol Biotechnol. 2011;4(5):550–553. doi: 10.1111/j.1751-7915.2011.00290.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Turnbaugh PJ, Hamady M, Yatsunenko T, Cantarel BL, Duncan A, Ley RE, et al. A core gut microbiome in obese and lean twins. Nature. 2009;457(7228):480–484. doi: 10.1038/nature07540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Nasidze I, Li J, Schroeder R, Creasey JL, Li M, Stoneking M. High diversity of the saliva microbiome in batwa pygmies. PLoS ONE. 2011;6(8):e23352. doi: 10.1371/journal.pone.0023352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Smyk DS, Bogdanos DP, Kriese S, Billinis C, Burroughs AK, Rigopoulou EI. Urinary tract infection as a risk factor for autoimmune liver disease: from bench to bedside. Clin Res Hepatol Gastroenterol. 2011 doi: 10.1016/j.clinre.2011.07.013. [DOI] [PubMed] [Google Scholar]
- 288.Varyani FK, West J, Card TR. An increased risk of urinary tract infection precedes development of primary biliary cirrhosis. BMC Gastroenterol. 2011;11:95. doi: 10.1186/1471-230X-11-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Smyk D, Rigopoulou EI, Baum H, Burroughs AK, Vergani D, Bogdanos DP. Autoimmunity and environment: am I at risk? Clin Rev Allergy Immunol. 2011 doi: 10.1007/s12016-011-8259-x. [DOI] [PubMed] [Google Scholar]
- 290.Gordon J, Michel G. Discerning trends in multiplex immunoassay technology with potential for resource-limited settings. Clin Chem. 2012;58(4):690–698. doi: 10.1373/clinchem.2011.176503. [DOI] [PubMed] [Google Scholar]
- 291.Bissonnette L, Bergeron MG. Next revolution in the molecular theranostics of infectious diseases: microfabricated systems for personalized medicine. Expert Rev Mol Diagn. 2006;6(3):433–450. doi: 10.1586/14737159.6.3.433. [DOI] [PubMed] [Google Scholar]
- 292.Bissonnette L, Bergeron MG. Multiparametric technologies for the diagnosis of syndromic infections. Clinical Microbiology Newsletter. 2012;34(20):159–168. doi: 10.1016/j.clinmicnews.2012.09.003. [DOI] [Google Scholar]
- 293.Natesan M, Ulrich RG. Protein microarrays and biomarkers of infectious disease. Int J Mol Sci. 2010;11(12):5165–5183. doi: 10.3390/ijms11125165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Quintana FJ, Hagedorn PH, Elizur G, Merbl Y, Domany E, Cohen IR. Functional immunomics: microarray analysis of IgG autoantibody repertoires predicts the future response of mice to induced diabetes. Proc Natl Acad Sci U S A. 2004;101(Suppl 2):14615–14621. doi: 10.1073/pnas.0404848101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Larman HB, Zhao Z, Laserson U, Li MZ, Ciccia A, Gakidis MA, et al. Autoantigen discovery with a synthetic human peptidome. Nat Biotechnol. 2011;29(6):535–541. doi: 10.1038/nbt.1856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Drebber U, Kasper HU, Ratering J, Wedemeyer I, Schirmacher P, Dienes HP, et al. Hepatic granulomas: histological and molecular pathological approach to differential diagnosis–a study of 442 cases. Liver Int. 2008;28(6):828–834. doi: 10.1111/j.1478-3231.2008.01695.x. [DOI] [PubMed] [Google Scholar]
- 297.O’Donohue J, Fidler H, Garcia-Barcelo M, Nouri-Aria K, Williams R, McFadden J. Mycobacterial DNA not detected in liver sections from patients with primary biliary cirrhosis. J Hepatol. 1998;28(3):433–438. doi: 10.1016/S0168-8278(98)80317-6. [DOI] [PubMed] [Google Scholar]
- 298.Tanaka A, Prindiville TP, Gish R, Solnick JV, Coppel RL, Keeffe EB, et al. Are infectious agents involved in primary biliary cirrhosis? A PCR approach. J Hepatol. 1999;31(4):664–671. doi: 10.1016/S0168-8278(99)80346-8. [DOI] [PubMed] [Google Scholar]
- 299.Vilagut L, Pares A, Rodes J, Vila J, Vinas O, Gines A, et al. Mycobacteria–related to the aetiopathogenesis of primary biliary cirrhosis? J Hepatol. 1996;24(1):125. doi: 10.1016/S0168-8278(96)80198-X. [DOI] [PubMed] [Google Scholar]
- 300.Chen EC, Miller SA, DeRisi JL, Chiu CY. Using a pan-viral microarray assay (Virochip) to screen clinical samples for viral pathogens. J Vis Exp. 2011;(50):e2536. doi:10.3791/2536. [DOI] [PMC free article] [PubMed]
- 301.Kistler A, Avila PC, Rouskin S, Wang D, Ward T, Yagi S, et al. Pan-viral screening of respiratory tract infections in adults with and without asthma reveals unexpected human coronavirus and human rhinovirus diversity. J Infect Dis. 2007;196(6):817–825. doi: 10.1086/520816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Nakamura S, Nakaya T, Iida T. Metagenomic analysis of bacterial infections by means of high-throughput DNA sequencing. Exp Biol Med. 2011;236(8):968–971. doi: 10.1258/ebm.2011.010378. [DOI] [PubMed] [Google Scholar]
- 303.Tang P, Chiu C. Metagenomics for the discovery of novel human viruses. Future Microbiol. 2010;5(2):177–189. doi: 10.2217/fmb.09.120. [DOI] [PubMed] [Google Scholar]
- 304.Moore RA, Warren RL, Freeman JD, Gustavsen JA, Chenard C, Friedman JM, et al. The sensitivity of massively parallel sequencing for detecting candidate infectious agents associated with human tissue. PLoS ONE. 2011;6(5):e19838. doi: 10.1371/journal.pone.0019838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Broome U, Scheynius A, Hultcrantz R. Induced expression of heat-shock protein on biliary epithelium in patients with primary sclerosing cholangitis and primary biliary cirrhosis. Hepatology. 1993;18(2):298–303. doi: 10.1002/hep.1840180212. [DOI] [PubMed] [Google Scholar]
- 306.Singhal S, Dian D, Keshavarzian A, Fogg L, Fields JZ, Farhadi A. The role of oral hygiene in inflammatory bowel disease. Dig Dis Sci. 2011;56(1):170–175. doi: 10.1007/s10620-010-1263-9. [DOI] [PubMed] [Google Scholar]
- 307.Ochoa-Reparaz J, Mielcarz DW, Ditrio LE, Burroughs AR, Foureau DM, Haque-Begum S, et al. Role of gut commensal microflora in the development of experimental autoimmune encephalomyelitis. J Immunol. 2009;183(10):6041–6050. doi: 10.4049/jimmunol.0900747. [DOI] [PubMed] [Google Scholar]
- 308.Helenius LM, Meurman JH, Helenius I, Kari K, Hietanen J, Suuronen R, et al. Oral and salivary parameters in patients with rheumatic diseases. Acta Odontol Scand. 2005;63(5):284–293. doi: 10.1080/00016350510020043. [DOI] [PubMed] [Google Scholar]
- 309.Mason AL, Xu L, Guo L, Munoz S, Jaspan JB, Bryer-Ash M, et al. Detection of retroviral antibodies in primary biliary cirrhosis and other idiopathic biliary disorders. Lancet. 1998;351(9116):1620–1624. doi: 10.1016/S0140-6736(97)10290-2. [DOI] [PubMed] [Google Scholar]
- 310.Alvaro D, Alpini G, Onori P, Franchitto A, Glaser SS, Le Sage G, et al. Alfa and beta estrogen receptors and the biliary tree. Mol Cell Endocrinol. 2002;193(1–2):105–108. doi: 10.1016/S0303-7207(02)00103-X. [DOI] [PubMed] [Google Scholar]
- 311.Cunningham M, Gilkeson G. Estrogen receptors in immunity and autoimmunity. Clin Rev Allergy Immunol. 2011;40(1):66–73. doi: 10.1007/s12016-010-8203-5. [DOI] [PubMed] [Google Scholar]
- 312.Duvic M, Steinberg AD, Klassen LW. Effect of the anti-estrogen, Nafoxidine, on NZB/W autoimmune disease. Arthritis Rheum. 1978;21(4):414–417. doi: 10.1002/art.1780210403. [DOI] [PubMed] [Google Scholar]
- 313.Holmdahl R. Estrogen exaggerates lupus but suppresses T-cell-dependent autoimmune disease. J Autoimmun. 1989;2(5):651–656. doi: 10.1016/S0896-8411(89)80004-6. [DOI] [PubMed] [Google Scholar]
- 314.Walker SE. Estrogen and autoimmune disease. Clin Rev Allergy Immunol. 2011;40(1):60–65. doi: 10.1007/s12016-010-8199-x. [DOI] [PubMed] [Google Scholar]
- 315.Mizutani T, Shinoda M, Tanaka Y, Kuno T, Hattori A, Usui T, et al. Autoantibodies against CYP2D6 and other drug-metabolizing enzymes in autoimmune hepatitis type 2. Drug Metab Rev. 2005;37(1):235–252. doi: 10.1081/dmr-200028798. [DOI] [PubMed] [Google Scholar]
- 316.Obermayer-Straub P, Strassburg CP, Manns MP. Autoimmune hepatitis. J Hepatol. 2000;32(1 Suppl):181–197. doi: 10.1016/S0168-8278(00)80425-0. [DOI] [PubMed] [Google Scholar]
- 317.Garratty G. Drug-induced immune hemolytic anemia. Hematology Am Soc Hematol Educ Program. 2009:73-9. doi: 10.1182/asheducation-2009.1.73. [DOI] [PubMed]
- 318.Khokhar O, Gange C, Clement S, Lewis J. Autoimmune hepatitis and thyroiditis associated with rifampin and pyrazinamide prophylaxis: an unusual reaction. Dig Dis Sci. 2005;50(1):207–211. doi: 10.1007/s10620-005-1302-0. [DOI] [PubMed] [Google Scholar]
- 319.Takasu N, Takara M, Komiya I. Rifampin-induced hypothyroidism in patients with Hashimoto’s thyroiditis. N Engl J Med. 2005;352(5):518–519. doi: 10.1056/NEJM200502033520524. [DOI] [PubMed] [Google Scholar]
- 320.Ahrens N, Genth R, Salama A. Belated diagnosis in three patients with rifampicin-induced immune haemolytic anaemia. Br J Haematol. 2002;117(2):441–443. doi: 10.1046/j.1365-2141.2002.03416.x. [DOI] [PubMed] [Google Scholar]
- 321.Heurgue-Berlot A, Bernard-Chabert B, Diebold MD, Thiefin G. Drug-induced autoimmune-like hepatitis: a case of chronic course after drug withdrawal. Dig Dis Sci. 2011;56(8):2504-5; author reply 5. doi:10.1007/s10620-011-1786-8. [DOI] [PubMed]
- 322.Bjornsson E, Talwalkar J, Treeprasertsuk S, Kamath PS, Takahashi N, Sanderson S, et al. Drug-induced autoimmune hepatitis: clinical characteristics and prognosis. Hepatology. 2010;51(6):2040–2048. doi: 10.1002/hep.23588. [DOI] [PubMed] [Google Scholar]
- 323.Geddes MR, Sinnreich M, Chalk C. Minocycline-induced dermatomyositis. Muscle Nerve. 2010;41(4):547–549. doi: 10.1002/mus.21487. [DOI] [PubMed] [Google Scholar]
- 324.Angulo JM, Sigal LH, Espinoza LR. Minocycline induced lupus and autoimmune hepatitis. J Rheumatol. 1999;26(6):1420–1421. [PubMed] [Google Scholar]
- 325.Bachmeyer C, Cadranel JF. Minocycline-induced lupus and autoimmune hepatitis: family autoimmune disorders as possible risk factors. Dermatology. 2002;205(2):185–186. doi: 10.1159/000063890. [DOI] [PubMed] [Google Scholar]
- 326.Bhat G, Jordan J, Jr, Sokalski S, Bajaj V, Marshall R, Berkelhammer C. Minocycline-induced hepatitis with autoimmune features and neutropenia. J Clin Gastroenterol. 1998;27(1):74–75. doi: 10.1097/00004836-199807000-00016. [DOI] [PubMed] [Google Scholar]
- 327.Chamberlain MC, Schwarzenberg SJ, Akin EU, Kurth MH. Minocycline-induced autoimmune hepatitis with subsequent cirrhosis. J Pediatr Gastroenterol Nutr. 2006;42(2):232–235. doi: 10.1097/01.mpg.0000184923.47507.ae. [DOI] [PubMed] [Google Scholar]
- 328.Colmegna I, Perandones CE, Chaves JG. Minocycline induced lupus and autoimmune hepatitis. J Rheumatol. 2000;27(6):1567–1568. [PubMed] [Google Scholar]
- 329.Gough A, Chapman S, Wagstaff K, Emery P, Elias E. Minocycline induced autoimmune hepatitis and systemic lupus erythematosus-like syndrome. BMJ. 1996;312(7024):169–172. doi: 10.1136/bmj.312.7024.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Healy J, Alexander B, Eapen C, Roberts-Thomson IC. Minocycline-induced autoimmune hepatitis. Int Med J. 2009;39(7):487–488. doi: 10.1111/j.1445-5994.2009.01971.x. [DOI] [PubMed] [Google Scholar]
- 331.Della Corte C, Carlucci A, Francalanci P, Alisi A, Nobili V. Autoimmune hepatitis type 2 following anti-papillomavirus vaccination in a 11-year-old girl. Vaccine. 2011;29(29-30):4654–4656. doi: 10.1016/j.vaccine.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 332.Karali Z, Basaranoglu ST, Karali Y, Oral B, Kilic SS. Autoimmunity and hepatitis A vaccine in children. J Investig Allergol Clin Immunol. 2011;21(5):389–393. [PubMed] [Google Scholar]
- 333.Stubgen JP. Neuromuscular disorders associated with Hepatitis B vaccination. J Neurol Sci. 2010;292(1–2):1–4. doi: 10.1016/j.jns.2010.02.016. [DOI] [PubMed] [Google Scholar]
- 334.Cacoub P, Terrier B. Hepatitis B-related autoimmune manifestations. Rheum Dis Clin North Am. 2009;35(1):125–137. doi: 10.1016/j.rdc.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 335.Aron-Maor A, Shoenfeld Y. Vaccination and systemic lupus erythematosus: the bidirectional dilemmas. Lupus. 2001;10(3):237–240. doi: 10.1191/096120301673085478. [DOI] [PubMed] [Google Scholar]
- 336.Borchers AT, Keen CL, Shoenfeld Y, Silva J, Jr, Gershwin ME. Vaccines, viruses, and voodoo. J Investig Allergol Clin Immunol. 2002;12(3):155–168. [PubMed] [Google Scholar]
- 337.Chen RT, Pless R, Destefano F. Epidemiology of autoimmune reactions induced by vaccination. J Autoimmun. 2001;16(3):309–318. doi: 10.1006/jaut.2000.0491. [DOI] [PubMed] [Google Scholar]
- 338.Cohen AD, Shoenfeld Y. Vaccine-induced autoimmunity. J Autoimmun. 1996;9(6):699–703. doi: 10.1006/jaut.1996.0091. [DOI] [PubMed] [Google Scholar]
- 339.Nadler JP. Multiple sclerosis and hepatitis B vaccination. Clin Infect Dis. 1993;17(5):928–929. doi: 10.1093/clinids/17.5.928-b. [DOI] [PubMed] [Google Scholar]
- 340.Ravel G, Christ M, Horand F, Descotes J. Autoimmunity, environmental exposure and vaccination: is there a link? Toxicology. 2004;196(3):211–216. doi: 10.1016/j.tox.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 341.Shoenfeld Y, Aharon-Maor A, Sherer Y. Vaccination as an additional player in the mosaic of autoimmunity. Clin Exp Rheumatol. 2000;18(2):181–184. [PubMed] [Google Scholar]
- 342.Shoenfeld Y, Aron-Maor A. Vaccination and autoimmunity-’vaccinosis’: a dangerous liaison? J Autoimmun. 2000;14(1):1–10. doi: 10.1006/jaut.1999.0346. [DOI] [PubMed] [Google Scholar]
- 343.Shoenfeld Y, Aron-Maor A, Tanai A, Ehrenfeld M. Bcg and autoimmunity: another two-edged sword. J Autoimmun. 2001;16(3):235–240. doi: 10.1006/jaut.2000.0494. [DOI] [PubMed] [Google Scholar]
- 344.Costenbader KH, Gay S, Riquelme ME, Iaccarino L, Doria A. Genes, epigenetic regulation and environmental factors: which is the most relevant in developing autoimmune diseases? Autoimmun Rev. 2011 doi: 10.1016/j.autrev.2011.10.022. [DOI] [PubMed] [Google Scholar]
- 345.Arnson Y, Shoenfeld Y, Amital H. Effects of tobacco smoke on immunity, inflammation and autoimmunity. J Autoimmun. 2010;34(3):J258–J265. doi: 10.1016/j.jaut.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 346.Brusselle GG, Joos GF, Bracke KR. New insights into the immunology of chronic obstructive pulmonary disease. Lancet. 2011;378(9795):1015–1026. doi: 10.1016/S0140-6736(11)60988-4. [DOI] [PubMed] [Google Scholar]
- 347.Simard JF, Costenbader KH. What can epidemiology tell us about systemic lupus erythematosus? Int J Clin Pract. 2007;61(7):1170–1180. doi: 10.1111/j.1742-1241.2007.01434.x. [DOI] [PubMed] [Google Scholar]
- 348.Costenbader KH, Karlson EW. Cigarette smoking and autoimmune disease: what can we learn from epidemiology? Lupus. 2006;15(11):737–745. doi: 10.1177/0961203306069344. [DOI] [PubMed] [Google Scholar]
- 349.Rubin RL, Hermanson TM, Bedrick EJ, McDonald JD, Burchiel SW, Reed MD, et al. Effect of cigarette smoke on autoimmunity in murine and human systemic lupus erythematosus. Toxicol Sci. 2005;87(1):86–96. doi: 10.1093/toxsci/kfi217. [DOI] [PubMed] [Google Scholar]
- 350.Asherson RA, Shoenfeld Y, Jacobs P, Bosman C. An unusually complicated case of primary Sjogren’s syndrome: development of transient “lupus-type” autoantibodies following silicone implant rejection. J Rheumatol. 2004;31(1):196–197. [PubMed] [Google Scholar]
- 351.Bar-Meir E, Eherenfeld M, Shoenfeld Y. Silicone gel breast implants and connective tissue disease–a comprehensive review. Autoimmunity. 2003;36(4):193–197. doi: 10.1080/08916931000148818. [DOI] [PubMed] [Google Scholar]
- 352.Bar-Meir E, Teuber SS, Lin HC, Alosacie I, Goddard G, Terybery J, et al. Multiple autoantibodies in patients with silicone breast implants. J Autoimmun. 1995;8(2):267–277. doi: 10.1006/jaut.1995.0020. [DOI] [PubMed] [Google Scholar]
- 353.Vasey FB, Zarabadi SA, Seleznick M, Ricca L. Where there’s smoke there’s fire: the silicone breast implant controversy continues to flicker: a new disease that needs to be defined. J Rheumatol. 2003;30(10):2092–2094. [PubMed] [Google Scholar]
- 354.Vermeulen RC, Scholte HR. Rupture of silicone gel breast implants and symptoms of pain and fatigue. J Rheumatol. 2003;30(10):2263–2267. [PubMed] [Google Scholar]
- 355.Zandman-Goddard G, Blank M, Ehrenfeld M, Gilburd B, Peter J, Shoenfeld Y. A comparison of autoantibody production in asymptomatic and symptomatic women with silicone breast implants. J Rheumatol. 1999;26(1):73–77. [PubMed] [Google Scholar]
- 356.Hajdu SD, Agmon-Levin N, Shoenfeld Y. Silicone and autoimmunity. Eur J Clin Invest. 2011;41(2):203–211. doi: 10.1111/j.1365-2362.2010.02389.x. [DOI] [PubMed] [Google Scholar]
- 357.Alotaibi S, Kennedy J, Tellier R, Stephens D, Banwell B. Epstein-Barr virus in pediatric multiple sclerosis. JAMA. 2004;291(15):1875–1879. doi: 10.1001/jama.291.15.1875. [DOI] [PubMed] [Google Scholar]
- 358.DeLorenze GN, Munger KL, Lennette ET, Orentreich N, Vogelman JH, Ascherio A. Epstein-Barr virus and multiple sclerosis: evidence of association from a prospective study with long-term follow-up. Arch Neurol. 2006;63(6):839–844. doi: 10.1001/archneur.63.6.noc50328. [DOI] [PubMed] [Google Scholar]
- 359.Goodin DS. The causal cascade to multiple sclerosis: a model for MS pathogenesis. PLoS ONE. 2009;4(2):e4565. doi: 10.1371/journal.pone.0004565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Levin LI, Munger KL, O’Reilly EJ, Falk KI, Ascherio A. Primary infection with the Epstein-Barr virus and risk of multiple sclerosis. Ann Neurol. 2010;67(6):824–830. doi: 10.1002/ana.21978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.Levin LI, Munger KL, Rubertone MV, Peck CA, Lennette ET, Spiegelman D, et al. Temporal relationship between elevation of epstein-barr virus antibody titers and initial onset of neurological symptoms in multiple sclerosis. JAMA. 2005;293(20):2496–2500. doi: 10.1001/jama.293.20.2496. [DOI] [PubMed] [Google Scholar]
- 362.Lindberg C, Andersen O, Vahlne A, Dalton M, Runmarker B. Epidemiological investigation of the association between infectious mononucleosis and multiple sclerosis. Neuroepidemiology. 1991;10(2):62–65. doi: 10.1159/000110248. [DOI] [PubMed] [Google Scholar]
- 363.Lunemann JD, Edwards N, Muraro PA, Hayashi S, Cohen JI, Munz C, et al. Increased frequency and broadened specificity of latent EBV nuclear antigen-1-specific T cells in multiple sclerosis. Brain. 2006;129(Pt 6):1493–1506. doi: 10.1093/brain/awl067. [DOI] [PubMed] [Google Scholar]
- 364.Lunemann JD, Huppke P, Roberts S, Bruck W, Gartner J, Munz C. Broadened and elevated humoral immune response to EBNA1 in pediatric multiple sclerosis. Neurology. 2008;71(13):1033–1035. doi: 10.1212/01.wnl.0000326576.91097.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 365.Lunemann JD, Jelcic I, Roberts S, Lutterotti A, Tackenberg B, Martin R, et al. EBNA1-specific T cells from patients with multiple sclerosis cross react with myelin antigens and co-produce IFN-gamma and IL-2. J Exp Med. 2008;205(8):1763–1773. doi: 10.1084/jem.20072397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366.Operskalski EA, Visscher BR, Malmgren RM, Detels R. A case-control study of multiple sclerosis. Neurology. 1989;39(6):825–829. doi: 10.1212/WNL.39.6.825. [DOI] [PubMed] [Google Scholar]
- 367.Peferoen LA, Lamers F, Lodder LN, Gerritsen WH, Huitinga I, Melief J, et al. Epstein Barr virus is not a characteristic feature in the central nervous system in established multiple sclerosis. Brain. 2010;133(Pt 5):e137. doi: 10.1093/brain/awp296. [DOI] [PubMed] [Google Scholar]
- 368.Sargsyan SA, Shearer AJ, Ritchie AM, Burgoon MP, Anderson S, Hemmer B, et al. Absence of Epstein-Barr virus in the brain and CSF of patients with multiple sclerosis. Neurology. 2010;74(14):1127–1135. doi: 10.1212/WNL.0b013e3181d865a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Serafini B, Rosicarelli B, Franciotta D, Magliozzi R, Reynolds R, Cinque P, et al. Dysregulated Epstein-Barr virus infection in the multiple sclerosis brain. J Exp Med. 2007;204(12):2899–2912. doi: 10.1084/jem.20071030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370.Thorley-Lawson DA. Epstein-Barr virus: exploiting the immune system. Nat Rev Immunol. 2001;1(1):75–82. doi: 10.1038/35095584. [DOI] [PubMed] [Google Scholar]
- 371.Warner HB, Carp RI. Multiple sclerosis and Epstein-Barr virus. Lancet. 1981;2(8258):1290. doi: 10.1016/S0140-6736(81)91527-0. [DOI] [PubMed] [Google Scholar]
- 372.Willis SN, Stadelmann C, Rodig SJ, Caron T, Gattenloehner S, Mallozzi SS, et al. Epstein-Barr virus infection is not a characteristic feature of multiple sclerosis brain. Brain. 2009;132(Pt 12):3318–3328. doi: 10.1093/brain/awp200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Sriram S, Stratton CW, Yao S, Tharp A, Ding L, Bannan JD, et al. Chlamydia pneumoniae infection of the central nervous system in multiple sclerosis. Ann Neurol. 1999;46(1):6–14. doi: 10.1002/1531-8249(199907)46:1<6::AID-ANA4>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 374.Challoner PB, Smith KT, Parker JD, MacLeod DL, Coulter SN, Rose TM, et al. Plaque-associated expression of human herpesvirus 6 in multiple sclerosis. Proc Natl Acad Sci U S A. 1995;92(16):7440–7444. doi: 10.1073/pnas.92.16.7440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 375.Dockrell DH, Smith TF, Paya CV. Human herpesvirus 6. Mayo Clin Proc. 1999;74(2):163–170. doi: 10.4065/74.2.163. [DOI] [PubMed] [Google Scholar]
- 376.Chmielewska-Badora J, Cisak E, Dutkiewicz J. Lyme borreliosis and multiple sclerosis: any connection? A seroepidemic study. Ann Agric Environ Med. 2000;7(2):141–143. [PubMed] [Google Scholar]
- 377.Mancuso R, Delbue S, Borghi E, Pagani E, Calvo MG, Caputo D, et al. Increased prevalence of varicella zoster virus DNA in cerebrospinal fluid from patients with multiple sclerosis. J Med Virol. 2007;79(2):192–199. doi: 10.1002/jmv.20777. [DOI] [PubMed] [Google Scholar]
- 378.Ordonez G, Pineda B, Garcia-Navarrete R, Sotelo J. Brief presence of varicella-zoster vral DNA in mononuclear cells during relapses of multiple sclerosis. Arch Neurol. 2004;61(4):529–532. doi: 10.1001/archneur.61.4.529. [DOI] [PubMed] [Google Scholar]
- 379.Sotelo J, Martinez-Palomo A, Ordonez G, Pineda B. Varicella-zoster virus in cerebrospinal fluid at relapses of multiple sclerosis. Ann Neurol. 2008;63(3):303–311. doi: 10.1002/ana.21316. [DOI] [PubMed] [Google Scholar]
- 380.Birnbaum G, Kotilinek L, Albrecht L. Spinal fluid lymphocytes from a subgroup of multiple sclerosis patients respond to mycobacterial antigens. Ann Neurol. 1993;34(1):18–24. doi: 10.1002/ana.410340106. [DOI] [PubMed] [Google Scholar]
- 381.Wroblewska Z, Gilden D, Devlin M, Huang ES, Rorke LB, Hamada T, et al. Cytomegalovirus isolation from a chimpanzee with acute demyelinating disease after inoculation of multiple sclerosis brain cells. Infect Immun. 1979;25(3):1008–1015. doi: 10.1128/iai.25.3.1008-1015.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 382.Perron H, Garson JA, Bedin F, Beseme F, Paranhos-Baccala G, Komurian-Pradel F, et al. Molecular identification of a novel retrovirus repeatedly isolated from patients with multiple sclerosis. the collaborative research group on multiple sclerosis. Proc Natl Acad Sci U S A. 1997;94(14):7583–7588. doi: 10.1073/pnas.94.14.7583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383.Rasmussen HB, Geny C, Deforges L, Perron H, Tourtelotte W, Heltberg A, et al. Expression of endogenous retroviruses in blood mononuclear cells and brain tissue from multiple sclerosis patients. Acta Neurol Scand Supplementum. 1997;169:38–44. doi: 10.1111/j.1600-0404.1997.tb08148.x. [DOI] [PubMed] [Google Scholar]
- 384.Murray RS, Brown B, Brian D, Cabirac GF. Detection of coronavirus RNA and antigen in multiple sclerosis brain. Ann Neurol. 1992;31(5):525–533. doi: 10.1002/ana.410310511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 385.Stewart JN, Mounir S, Talbot PJ. Human coronavirus gene expression in the brains of multiple sclerosis patients. Virology. 1992;191(1):502–505. doi: 10.1016/0042-6822(92)90220-J. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 386.Ferrante P, Omodeo-Zorini E, Caldarelli-Stefano R, Mediati M, Fainardi E, Granieri E, et al. Detection of JC virus DNA in cerebrospinal fluid from multiple sclerosis patients. Mult Scler. 1998;4(2):49–54. doi: 10.1177/135245859800400202. [DOI] [PubMed] [Google Scholar]
- 387.Stoner GL, Agostini HT, Ryschkewitsch CF, Baumhefner RW, Tourtellotte WW. Characterization of JC virus DNA amplified from urine of chronic progressive multiple sclerosis patients. Mult Scler. 1996;1(4):193–199. [PubMed] [Google Scholar]
- 388.Forghani B, Cremer NE, Johnson KP, Ginsberg AH, Likosky WH. Viral antibodies in cerebrospinal fluid of multiple sclerosis and control patients: comparison between radioimmunoassay and conventional techniques. J Clin Microbiol. 1978;7(1):63–69. doi: 10.1128/jcm.7.1.63-69.1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 389.ter Meulen V, Koprowski H, Iwasaki Y, Kackell YM, Muller D. Fusion of cultured multiple-sclerosis brain cells with indicator cells: presence of nucleocapsids and virions and isolation of parainfluenza-type virus. Lancet. 1972;2(7766):1–5. doi: 10.1016/S0140-6736(72)91273-1. [DOI] [PubMed] [Google Scholar]
- 390.Haase AT, Ventura P, Gibbs CJ, Jr, Tourtellotte WW. Measles virus nucleotide sequences: detection by hybridization in situ. Science. 1981;212(4495):672–675. doi: 10.1126/science.7221554. [DOI] [PubMed] [Google Scholar]
- 391.Jacobson S, Flerlage ML, McFarland HF. Impaired measles virus-specific cytotoxic T cell responses in multiple sclerosis. J Exp Med. 1985;162(3):839–850. doi: 10.1084/jem.162.3.839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 392.Alpérovitch A, Berr C, Cambon-Thomsen A, Puel J, Dugoujon JM, Ruidavets JB, et al. Viral antibody titers, immunogenetic markers, and their interrelations in multiple sclerosis patients and controls. Hum Immunol. 1991;31(2):94–99. doi: 10.1016/0198-8859(91)90011-W. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Ortega-Hernandez OD, Levin NA, Altman A, Shoenfeld Y. Infectious agents in the pathogenesis of primary biliary cirrhosis. Dis Markers. 2010;29(6):277–286. doi: 10.1155/2010/923928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 394.Shigematsu H, Shimoda S, Nakamura M, Matsushita S, Nishimura Y, Sakamoto N, et al. Fine specificity of T cells reactive to human PDC-E2 163–176 peptide, the immunodominant autoantigen in primary biliary cirrhosis: implications for molecular mimicry and cross-recognition among mitochondrial autoantigens. Hepatology. 2000;32(5):901–909. doi: 10.1053/jhep.2000.18714. [DOI] [PubMed] [Google Scholar]
- 395.Bogdanos DP, Pares A, Baum H, Caballeria L, Rigopoulou EI, Ma Y, et al. Disease-specific cross-reactivity between mimicking peptides of heat shock protein of Mycobacterium gordonae and dominant epitope of E2 subunit of pyruvate dehydrogenase is common in Spanish but not British patients with primary biliary cirrhosis. J Autoimmun. 2004;22(4):353–362. doi: 10.1016/j.jaut.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 396.Vilagut L, Pares A, Vinas O, Vila J, Jimenez de Anta MT, Rodes J. Antibodies to mycobacterial 65-kD heat shock protein cross-react with the main mitochondrial antigens in patients with primary biliary cirrhosis. Eur J Clin Invest. 1997;27(8):667–672. doi: 10.1046/j.1365-2362.1997.1690724.x. [DOI] [PubMed] [Google Scholar]
- 397.Vilagut L, Vila J, Vinas O, Pares A, Gines A, Jimenez de Anta MT, et al. Cross-reactivity of anti-Mycobacterium gordonae antibodies with the major mitochondrial autoantigens in primary biliary cirrhosis. J Hepatol. 1994;21(4):673–677. doi: 10.1016/S0168-8278(94)80117-7. [DOI] [PubMed] [Google Scholar]
- 398.Xu L, Shen Z, Guo L, Fodera B, Keogh A, Joplin R, et al. Does a betaretrovirus infection trigger primary biliary cirrhosis? Proc Natl Acad Sci U S A. 2003;100(14):8454–8459. doi: 10.1073/pnas.1433063100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 399.Zhang G, Chen M, Graham D, Subsin B, McDougall C, Gilady S, et al. Mouse mammary tumor virus in anti-mitochondrial antibody producing mouse models. J Hepatol. 2011;55(4):876–884. doi: 10.1016/j.jhep.2011.01.037. [DOI] [PubMed] [Google Scholar]


