Abstract
The need for organ donation has become a growing concern over that last decade as the gap between organ donors and those awaiting transplant widens. According to UNOS, as of 8/2009, there were 102,962 patients on the transplant waiting list and only 6,004 donors in 2009 (UNOS.org. Accessed 4/8/2009). In 2008, an estimated 17 patients died each day awaiting transplant (OPTN.org). Though currently most organ donations come after brain death (DND or donation after neurological death), tissue donation (cornea, skin, bone, and musculoskeletal tissue), and donation after cardiac death (DCD) and are also possible. The term “extended criteria donor” refers to potential donors over 60 years of age or age 50–59 years plus 2 of the 3 following criteria: stroke as the cause of death, creatnine > 1.5 meq/dl, or a history of hypertension. Historically, extended criteria donors have had a lower organ yield per donor. In order to preserve the choice of organ donation for the family, intensive management of the potential organ donor is necessary. Since each potential donor could save seven lives or more, nihilism in the care of such patients can have far reaching ramifications. This article describes intensive care management practices that can optimize organ donation.
Keywords: Brain death, Organ donation, End of life, Hormonal therapy, Organ sparing therapy, Donation after neurological death
Case Report
A 63 year physically fit woman with a history of peripheral vascular disease, left femoral artery stenting, and ovarian cysts was admitted to the hospital for elective right superficial femoral artery stenting. She was maintained on her home dose of aspirin 325 mg daily, clopidogrel 75 mg daily, and cilostazol 100 mg twice a daily. Her preoperative coagulation studies and platelet count were normal. During the procedure she received 9,500 units of heparin and her blood pressures were maintained between 117–146/45–74 mmHg. Her activated clotting time during the procedure was measured at 135 s. Shortly after the procedure the patient complained of a headache and right sided weakness. She became progressively obtunded and a head CT revealed a 132 ml left frontal/temporal/parietal intracerebral hemorrhage with a fluid–fluid level indicative of coagulopathy and 1.14 cm of midline shift. She was administered DDAVP, protamine, and transfused platelets, with normalization of her labs. She was also hyperventilated and given osmotic therapy, but her exam rapidly deteriorated to brain death. The regional organ donor network was notified and the brain death protocol initiated. She was transferred to the ICU where her blood pressure at admission was 70/40 mm Hg. An arterial line and central venous catheter were placed. She initially received norepinephrine and volume resuscitation, but required increasing pressor doses. Hormonal therapy was then initiated with levothyroxine at 10 mcg/h, insulin infusion, and solumedrol 15 mg/kg IV bolus. Her blood pressure improved markedly to 140–180/70–80 mmHg and norepinepherine was tapered off. A transthoracic echocardiogram revealed an ejection fraction of 55%. Shortly thereafter the patient’s urine output increased to 275–500 ml/h and she was started on a vasopressin drip at 0.5 units/h. Her urine output decreased to 125–175 ml/h and her sodium levels stabilized on vasopressin. The patient underwent two neurological exams and an apnea test that were confirmatory for brain death. The family was approached for organ donation and consented. The patient underwent bronchoscopy as part of her evaluation and went on to donate both kidneys and her liver.
Comments
Identifying Potential Organ Donors
The first step in managing a potential organ donor should always be notification of the local organ donor network. Transplant and family service coordinators should be dispatched to screen the patient for donation, liaison with the family, and assist in organ sparing therapy management. Organ donor networks should be notified for all patients with impending brain death, patients with planned withdrawal of care (for potential donation after cardiac death) and after all deaths within 1 h, for potential tissue donation regardless of etiology of death or age of the patient. Some local organ donor networks have trigger cards which suggest notification if brain death testing is being discussed, with the absence of one or more cranial nerve reflexes (pupils fixed and dilated, no blink, no cough, or gag) or a Glasgow Coma Score ≤ 4. Physicians are not expected to screen patients for potential organ donation, but general contraindications to donation are listed in Table 1. Even patients who may be medical rule-outs should be reported to the local organ donor network since a screening log is maintained by most organ procurement centers.
Table 1.
General contraindications to organ donation
| Contraindication | Notes |
|---|---|
| Multi-system organ failure due to sepsis | |
| History of cancer | Except: skin cancer other than melanoma, certain primary brain tumors, remote prostate cancer |
| Viral infections | HIV, HTLV I, II, rabies, reactive HbsAg, measles, West Nile virus, SARS, adenovirus, enterovirus, parvovirus, active HSV, VZV, EBV, viral encephalitis/meningitis |
| Hepatitis B or C organs can be transplanted into recipients with the same virus | |
| CMV + organs can be transplanted- better success if recipient is prophylaxed | |
| Bacterial infections | Tuberculosis, gangrenous bowel, bowel perforation, intra-abdominal sepsis |
| Fungal infections | Active cryptococcus, aspergillus, Histoplasma, coccidioides, candidemia, invasive yeast infections |
| Parasitic infections | Leishmania, trypanosoma, strongyloides, malaria |
| Prion disease | CJD, vCJD, fatal familial insomnia, Gerstmann–Straussler Scheinker |
Please confer with your local organ donor organization as some contraindications are relative
HTLV Human T lymphotrophic virus, HbsAg Hepatitis B surface antigen, SARS severe acute respiratory syndrome, HSV herpes simplex virus, VZV varicella zoster virus, EBV Epstein-Barr virus, CMV cytomegalovirus, CJD Creutzfeldt–Jakob disease, vCJD variant Creutzfeldt–Jakob disease
Prior to the initiation of a protocol to declare brain death, the main goals of management are focused on the care of the neurologically injured patient. After the first brain death exam is performed, the time to declaration is typically a minimum of 6 h, since most hospitals mandate a second brain death exam. During this time, physicians are expected to keep family members informed of the clinical status of the patient and to maintain the patient in a hemodynamically stable state. In the past, once a patient has completed the protocol for the declaration of brain death, the organ procurement officer (OPO) has taken over medical care. Now in many institutions, intensivists are jointly involved in the management of these patients up until the point of procurement. Cooperative management between the intensivist and OPO may provide more consistent care.
Consent
At most centers, the approach for consent for organ or tissue donation is performed by the organ donor network team, typically after the second brain death exam. Maintaining a clear distinction between the patient care team and the organ donation team can minimize any perceived conflict of interest. However, some centers are beginning to couple the process of notification of brain death and the initial approach for donation. This means that the treating physician and family services coordinator from the organ donor network are present for both discussions. Some centers have noted an increased conversion rate of potential to actual donors with coupling, though more data are needed.
Intensive management of the brain-dead patient may be necessary while the family is being approached for consent in order to maintain viable organs for transplant. Since brain-dead patients are frequently hemodynamically unstable, failure to treat these patients will de facto eliminate the possibility of a choice to donate, and can be viewed as a paternalistic approach to patient care. In the case of a living will or a family that does not wish to pursue donation, clear documentation of this sentiment after appropriate counseling by an organ donor network representative should occur and life sustaining therapy can be withdrawn in accordance with the patient’s or family’s wishes.
Managing Hemodynamic Instability
The progression from brain death to somatic death results in the loss of 10–20% of potential donors. Hemodynamic instability following brain death can be attributed to three main causes. First, a sympathetic surge immediately preceding medullary level brain death leads to a massive release of catecholamines from postganglionic sympathetic nerve endings leading to elevated systemic vascular resistance, hypertension, left ventricular dysfunction, cardiac stunning, neurogenic pulmonary edema, and arrhythmias [1, 2]. Second, herniation following brain death leads to spinal cord infarction and loss of sympathetic tone resulting in further hypotension [3]. Third, pituitary hormonal secretion ceases and the body enters a panhypopituitary state characterized by low cortisol, T3, T4, insulin, and ADH levels [2, 4, 5]. Ensuing diabetes insipitus leads to further hypotension as the patient becomes volume depleted.
Conventional management of hypotension in brain-dead patients is inadequate and leads to persistent hemodynamic instability in 34–45% of patients [6–8]. Though many reputable publications have advocated using a combination of fluid resuscitation and standard inotropes (dopamine, dobutamine, or epinephrine) or vasopressors (norepinepherine, phenylephrine or epinephrine) as first line therapy [9, 10], I favor a more physiologically rational approach of fluid resuscitation followed by replacement of hormonal deficiency (Fig. 1). In the case of volume depletion, crystalloid resuscitation is initiated unless the patient is actively bleeding or has a hemoglobin < 7 g/dl, in which case blood product replacement can be utilized. Acceptable hemodynamic goals include a mean arterial pressure ≥ 65 mmHg, heart rate 60–100 bpm, and a urine output of 0.5–3 ml/kg/h. Patients who are hypotensive or demonstrate evidence of diabetes insipitus should be initiated on hormonal replacement therapy without delay. If DI is present (see diagnostic criteria in Table 2), I usually initiate therapy with a vasopressin infusion beginning at 0.5 u/h to a maximum of 6 u/h targeted to a urine output of 0.5–3 ml/kg/h and a serum sodium of 135–145 meq/l. DDAVP is an alternate choice (1–4 μg IV, then 1–2 μg IV every 6 h), but is less easily titrated and does not add substantial hemodynamic support. Serum sodium values should be checked every 6 h to assist with vasopressin titration. Side effects of vasopressin include hyponatremia, digital vasoconstriction, and thrombosis.
Fig. 1.
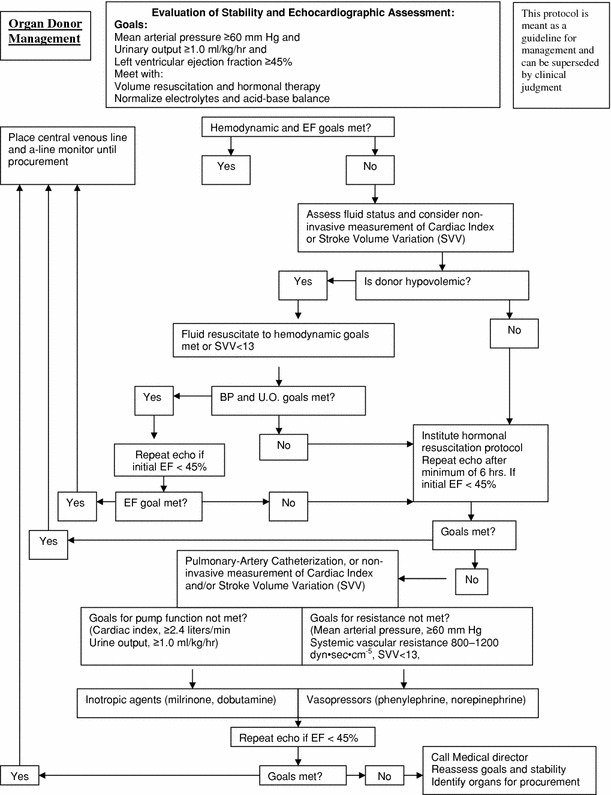
Flow diagram for organ donor management. EF ejection fraction, UO urine output, SVV stroke volume variation
Table 2.
Organ sparing hormonal therapy
| Drug | Dosage | Comments |
|---|---|---|
| Thyroxine T4 | Administer 10 U regular insulin with 1 ampule of D50 (unless glucose > 300 mg/dl) then | Inotropic effect, can be used as a pressor |
| 20 mcg T4 IV bolus (mixed 200 mcg in 500 ml NS) followed by | Causes hyperkalemia with bolus- must administer insulin and D50 prior to initiation | |
| 10 mcg/h of T4 IV maximum dose 20 mcg/h | T4 shown to be more beneficial than T3 [4, 12, 14, 18] | |
| Vasopressin | 0.5 units/h IV (25 u in 250 ml NS or D5W) | Check for DI: |
| maximum dose 6 u/h | UOP ≥ 5 cc/kg/h for ≥ 2 hours, urine specific gravity < 1.005, serum Na > 145 meq/l, OR serum osmolality > 300 mOsm/kg and urine osmolarity < 200 mOsm/kg | |
| Titration should be based on BP, UOP, Na+ levels and urine specific gravity | ||
| Insulin | 1 unit/h IV (25 u in 250 ml NS) | Adjust to maintain glucose 100–140 mg/dl |
| Methylprednisolone | 15 mg/kg IV bolus repeat daily | Improves potential for lung donation |
D50 50% dextrose solution, IV intravenous
Hormonal Replacement Therapy
Hormone replacement therapy should be instituted to address the panhypopituitary state that accompanies brain death and leads to refractory hypotension. This typically consists of administration of levothyroxine, solumedrol, insulin, and vasopressin (Table 2). Hormonal replacement therapy has been shown to decrease cardiovascular lability, ECG changes, and acid–base disturbances [11–13]. In a prospective study of 19 hemodynamically unstable brain-dead patients refractory to fluid resuscitation, traditional vasopressors, and inotropes, hormone replacement therapy with levothyroxine and solumedrol led to a significant decrease in pressor requirement such that 53% of patients were able to be weaned completely off traditional pressors [14]. Not only does hormonal therapy improve hemodynamics, but it also improves organ donation rates and graft function [6, 15]. In a retrospective study of 10, 292 brain-dead patients, those who received hormonal replacement therapy with T3, insulin, and vasopressin were found to have a 22.5% higher organ yield than those who did not receive hormonal replacement. Additionally, there was a significant increase in donation of kidney, heart, liver, lung, and pancreas [16]. In a multivariate model, both steroid and desmopressin use predicted organ yield [17]. Similarly, in a study of 4,543 heart transplant recipients, donor organs that were exposed to hormonal therapy suffered 3.8% graft loss and 5.6% graft dysfunction compared to 7.9% graft loss and 11.6% graft dysfunction in those that did not receive hormonal therapy (P = 0.01). There was a 46% reduction in the odds of recipient death in 30 days among those who received organs exposed to hormonal therapy [18]. Use of hormonal replacement therapy has steadily increased from 8.8% of all brain dead organ donors in 2000 to 20% of donors in 2004 [4]. I usually initiate the solumedrol and insulin components of hormonal replacement therapy after the first brain death exam and initiate levothyroxine and/or vasopressin if the patient is hypotensive or has diabetes insipitus. There are some, however, who advocate use of levothyroxine and vasopressin even in hemodynamically stable brain dead patients. Common side effects of levothyroxine include tachyarrhythmias and hypertension. Clinical studies that are routinely performed for the potential donor are listed in Table 3.
Table 3.
Routine studies for the potential organ donor
| Team requesting/performing studies | Clinical studies | Timing |
|---|---|---|
| Organ donor network | Serum: HIV 1,2 antibody; HTLV 1,2 antibody; Hepatitis B surface antigen, Hepatitis B core antibody, Hepatitis B core IgM, Hepatitis C antibody, Hepatitis B/C and HIV RNA testing, CMV IgM and IgG, EBV IgM and IgG, RPR, toxoplasmosis IgG, Chagas disease antibody (for patients with travel to Texas or South America) | Once |
| Primary care team | Serum: Complete blood count, arterial blood gas, liver function tests including GGT, coagulation studies, fibrinogen, troponin/CK, chemistry panel including calcium, phospohorus and magnesium, LDH, amylase, lipase | Every 6 h |
| Primary care team | CXR, ECG, blood culture, urine culture, urinalysis, sputum culture and gram stain, HgbA1c (once), type and screen (once) | Daily and as needed |
| Primary care team | 2-D Transthoracic echocardiogram | At least once, may repeat depending on hemodynamic status |
| Organ donor network/primary care team/cardiology | Coronary catheterization | May be required for potential heart donors |
| Organ donor network/primary care team/pulmonology | Bronchoscopy | Required for potential lung donors |
HTLV Human T lymphotrophic virus, EBV Epstein-Barr virus, CMV cytomegalovirus, CXR chest X-ray, ECG electrocardiogram
Hemodynamic Monitoring
As with any ICU patient, adequate monitoring and intravascular access are crucial to donor management. Most patients have an arterial line and central venous catheter in place prior to brain death. In patients that do not have these lines, we will routinely approach the family for consent for line placement if the family is considering organ donation. We do not routinely place pulmonary artery catheters for management, but instead use non-invasive means of monitoring cardiac function and volume status using stroke volume variation and/or pulse contour analysis (Flotrak, Vigileo, Irvine, CA; PiCCO, PULSION Medical Systems AG, Munich, Germany; LiDCO Ltd, London, England). Since central venous pressure (CVP) has been shown to have a poor relationship with volume status, we do not routinely measure CVP and do not use CVP as a hemodynamic target [19].
Pulmonary Management
Certain organ specific management strategies should be mentioned. The greatest disparity between organ supply and demand exists for the lungs [20]. Lung transplantation is particularly limited due to stringent donation criteria, though there is little evidence to support a specific lung management protocol. Criteria for lung donation are listed in Table 4 [21]. These selection criteria, however, have been shown to have poor predictive power for early graft outcome [22, 23]. Procurement of donor lungs is hampered by a high incidence of gas exchange disturbance that fail to meet consensus criteria for transplant. It has been hypothesized that donor ventilator strategy may impact on allograft integrity, recipient gas exchange, and the development of peri-transplant complications including primary graft dysfunction that in part may reflect ventilatory induced lung injury (VILI) [24, 25]. Strategies to improve these impediments to successful transplant are limited by the absence of controlled trials or clearly defined models that guide donor ventilatory strategy decision making.
Table 4.
Criteria for lung donation [21]
| History |
| Age < 55 years |
| Smoking history ≤ 20 pack-years |
| No history of primary pulmonary disease |
| Absence of chest trauma |
| No active pulmonary infection |
| No sepsis |
| Laboratory values |
| PaO2 to FiO2 ratio of ≥ 300 |
| No evidence of aspiration or purulent secretions at bronchoscopy |
| Sputum or bronchoalveolar lavage with a gram stain free of bacteria, fungus or a significant number of white cells |
| Normal chest X-ray |
Ventilator Management
Typical ventilator strategies in potential organ donors have included high tidal volume and low PEEP settings. A prospective, multi-center observational study found that the average tidal volume in brain dead donors was 9.7 ml/kg of ideal body weight and the PEEP ranged from 0 to 8 cm H2O. Ninety-seven percent of patients had no adjustments to ventilator settings after brain death was declared [20]. A ventilator strategy of high tidal volumes (8–10 ml/kg) and serial recruitment maneuvers has been favored by various organ donor networks because of concerns regarding atelectasis and suboptimal oxygenation in brain dead donors. This strategy may, however, produce additional inflammation and barotrauma. Additionally, severe brain injury in the donor pool is thought to contribute to lung injury and gas exchange disturbance, in part resulting from systemic and brainstem derived inflammatory mediator release. Neurogenic pulmonary edema and an increase in lung inflammatory markers has been well described following brain death[26] and broncheo-alveolar lavage markers of inflammation such as the ratio of IL-6/IL-10 have been shown to be predictive of primary graft failure [27].
The manner by which these inter-related aspects of VILI (Table 5) are affected by ventilatory strategy and the impact on recipient outcome are largely untested and unknown. However, it may be prudent to consider safe ventilator practices that extrapolate from extensive data sets derived from a broader ICU population. High tidal volume ventilation exacerbates pulmonary and systemic inflammation and worsens acute lung injury/acute respiratory distress syndrome (ALI/ARDS) in living patients [20, 28, 29]. Furthermore, a regimen of high tidal volumes can actually lead to the development of ALI as demonstrated in a study of patients with traumatic brain injury, in which high tidal volumes and high respiratory rates were independent predictors of acute lung injury [30]. The cornerstone and widely adopted management recommendation for patients with ALI/ARDS is a low tidal volume targeting 6 ml/kg of ideal body weight with moderate and graded PEEP, along with a protocol designed to address plateau pressures exceeding 30 cm H2O with further limitation on cycle volume. Recent studies have shown that even patients who do not have ALI/ARDS may benefit from lung protective ventilation using low tidal volumes targeting 6 ml/kg of ideal body weight and plateau pressure targets of ≤30 cm H2O [31].
Table 5.
Causes of ventilator induced lung injury (VILI)
| Type of injury | Causative factors |
|---|---|
| Volume trauma | Excessive end-tidal volume |
| Barotrauma | Excessive transpulmonary pressure |
| Atelectrauma | closing volume at end-expiration |
| Biotrauma | Stimulation of cellular response to mechanical and other injury (such as hyperoxia) by resident and recruited cells |
Another important message that may be garnered from controlled clinical studies in ALI is that improvement in oxygenation, per se, is a poor surrogate for outcome, despite the defining role for gas exchange disturbance in acute lung injury. Improved oxygenation has not been shown to correlate with improved clinical outcomes in living patients in many studies. For example, randomized trials testing inhaled NO, prone posture, recruitment maneuvers that employ high levels of PEEP, and direct measurement of transpulmonary pressures all achieved significant gas exchange improvement, but in each case failed to show mortality benefit [32–37]. Lung recruitment strategies utilized by some organ donor networks have included trials of increased PEEP to levels of 30–40 cm H2O for several minutes followed by a return to baseline PEEP levels. Such recruitment strategies have not been shown to change mortality in large randomized trials of patients with ALI/ARDS, but do improve oxygenation [35]. A major concern with such recruitment strategies is that when PEEP is reduced to baseline, alveoli will de-recruit and recurrent recruitment episodes can lead to shearing stress. Cyclic stretch has been shown to upregulate alveolar epithelial TGF β-1 and interleukin-8 [38], which in turn may worsen pre-existing lung inflammation. Ischemia–reperfusion injury that occurs during transplant may further compound lung damage. Targeting oxygen levels as the primary criteria for lung donation may be misguided. Infact, hyperoxia induced lung injury is intimately related to an inflammatory cascade activating both cellular apoptosis and necrosis [39].
The impact of specific ventilatory mode, such as volume targeted versus pressure limited strategies, deserves additional comment. Whereas a volume cycled modality that adheres to low tidal volume strategy has the largest data set accrual, alternative modes that achieve target volume have been used in acute lung injury, but do not appear to have measurable impact on outcome. This also implies that pressure targeted modes of ventilation may be acceptable alternatives to volume cycled ventilation, as long as end-inspiratory volume targets are not exceeded. Recently, many organ donor centers have moved toward the use of pressure cycled modes such as airway pressure release ventilation (APRV), inverse ratio and bi-level ventilation to improve recruitment. These ventilator settings increase intrathoracic pressure, auto-PEEP and ambient oxygen tension, which may lead to reduced preload, cardiac arrhythmias and hyperoxic lung injury. All pressure targeted modes result in dependent variables of volume and peak flow, and utilization imposes a greater vigilance on the operator to be watchful for fluctuation and regional variability. Purported advantages of pressure targeted modes such as enhanced comfort, decreased dyssynchrony and variable and initial high flow rates that match patient effort are moot in the donor population without spontaneous inspiratory effort. A risk of enhanced barotrauma associated with pressure targeting is suggested by exaggerated inflammatory signs including neutrophil influx in lungs subjected to high flow [25, 28, 29, 38]. There have been no studies in either brain dead or living patients that have shown a superiority of APRV or bilevel over other ventilatory modes.
Lung management strategies that have some supportive data include early referral to an organ donor network and high dose steroids (methylprednisolone 15 mg/kg IV daily), both of which appear to improve oxygenation and lung procurement rates [40, 41]. Additionally, a protocol of aggressive donor management with early bronchoscopy, chest physical therapy, strict fluid management, antibiotic therapy, and titration of the ventilator based on blood gas measurements has been shown to improve lung donation rates [42]. I favor using lung protective ventilation targeting 6 ml/kg of ideal body weight and plateau pressures < 30 cm H2O using assist control volume control mode and aggressively treating atelectasis with moderately elevated PEEP (7.5–10 cm H2O), early bronchoscopy, chest physiotherapy, periodic rotation to the lateral position, diuresis to normovolemia, directional suctioning, mucomyst nebulizers, and aggressive pulmonary toilet to minimize mucous plugging.
Cardiac Management
In regard to cardiac donation, an early transthoracic echocardiogram (TTE) should be performed to assess ejection fraction (EF). Patients who initially have an EF < 45% should be optimized with inotropic support. Since levothyroxine provides inotropy, this should be the first agent applied. Frequently, patients with stunned myocardium will recover their ejection fraction and may still be candidates for donation. Therefore, a repeat TTE should be performed after medical optimization. In patients who are potential heart donors, coronary angiography may be required prior to donation particularly in males > 55 years of age, females > 60 years, patients with a history of cocaine use, or in younger patients with several risk factors including: smoking, hypertension, diabetes, hyperlipidemia, elevated body mass index, family history of cardiac disease, history of cardiac disease, abnormal ECG, regional wall motion abnormalities on TTE or an EF ≤ 40% [10]. If an organ donor network requests cardiac catheterization this should be performed expediently, even if it means opening the cardiac catheterization lab. Prolonged medical care and a delay to harvest have been shown to lower the yield of cardiac allografts [43].
Conclusions
In summary, proactive management of the potential organ donor, including early notification of the organ donor network, hormonal replacement therapy, lung protective ventilation with aggressive pulmonary toilet, and intensive cardiac monitoring may help narrow the gap between the supply and demand for organ transplantation. More outcomes research is needed to identify optimal donor management strategies.
References
- 1.Novitzky D, Horak A, Cooper DK, Rose AG. Electrocardiographic and histopathologic changes developing during experimental brain death in the baboon. Transplant Proc. 1989;21(1 Pt 3):2567–2569. [PubMed] [Google Scholar]
- 2.Cooper DK, Novitzky D, Wicomb WN. The pathophysiological effects of brain death on potential donor organs, with particular reference to the heart. Ann R Coll Surg Engl. 1989;71(4):261–266. [PMC free article] [PubMed] [Google Scholar]
- 3.Shivalkar B, Van Loon J, Wieland W, et al. Variable effects of explosive or gradual increase of intracranial pressure on myocardial structure and function. Circulation. 1993;87(1):230–239. doi: 10.1161/01.cir.87.1.230. [DOI] [PubMed] [Google Scholar]
- 4.Novitzky D, Cooper DK, Rosendale JD, Kauffman HM. Hormonal therapy of the brain-dead organ donor: experimental and clinical studies. Transplantation. 2006;82(11):1396–1401. doi: 10.1097/01.tp.0000237195.12342.f1. [DOI] [PubMed] [Google Scholar]
- 5.Wicomb WN, Cooper DK, Lanza RP, Novitzky D, Isaacs S. The effects of brain death and 24 hours’ storage by hypothermic perfusion on donor heart function in the pig. J Thorac Cardiovasc Surg. 1986;91(6):896–909. [PubMed] [Google Scholar]
- 6.Wheeldon DR, Potter CD, Oduro A, Wallwork J, Large SR. Transforming the “unacceptable” donor: outcomes from the adoption of a standardized donor management technique. J Heart Lung Transplant. 1995;14(4):734–742. [PubMed] [Google Scholar]
- 7.Riou B, Dreux S, Roche S, et al. Circulating cardiac troponin T in potential heart transplant donors. Circulation. 1995;92(3):409–414. doi: 10.1161/01.cir.92.3.409. [DOI] [PubMed] [Google Scholar]
- 8.Chen JM, Cullinane S, Spanier TB, et al. Vasopressin deficiency and pressor hypersensitivity in hemodynamically unstable organ donors. Circulation. 1999;100(19 Suppl):II244–II246. doi: 10.1161/01.cir.100.suppl_2.ii-244. [DOI] [PubMed] [Google Scholar]
- 9.Wood KE, Becker BN, McCartney JG, D’Alessandro AM, Coursin DB. Care of the potential organ donor. N Engl J Med. 2004;351(26):2730–2739. doi: 10.1056/NEJMra013103. [DOI] [PubMed] [Google Scholar]
- 10.Shemie SD, Ross H, Pagliarello J, et al. Organ donor management in Canada: recommendations of the forum on Medical Management to Optimize Donor Organ Potential. CMAJ. 2006;174(6):S13–S32. doi: 10.1503/cmaj.045131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Novitzky D, Cooper DK. Results of hormonal therapy in human brain-dead potential organ donors. Transplant Proc. 1988;20(5 Suppl 7):59–62. [PubMed] [Google Scholar]
- 12.Novitzky D, Cooper DK, Human PA, Reichart B, Zuhdi N. Triiodothyronine therapy for heart donor and recipient. J Heart Transplant. 1988;7(5):370–376. [PubMed] [Google Scholar]
- 13.Novitzky D, Cooper DK, Reichart B. Hemodynamic and metabolic responses to hormonal therapy in brain-dead potential organ donors. Transplantation. 1987;43(6):852–854. [PubMed] [Google Scholar]
- 14.Salim A, Vassiliu P, Velmahos GC, et al. The role of thyroid hormone administration in potential organ donors. Arch Surg. 2001;136(12):1377–1380. doi: 10.1001/archsurg.136.12.1377. [DOI] [PubMed] [Google Scholar]
- 15.Jeevanandam V. Triiodothyronine: spectrum of use in heart transplantation. Thyroid. 1997;7(1):139–145. doi: 10.1089/thy.1997.7.139. [DOI] [PubMed] [Google Scholar]
- 16.Rosendale JD, Kauffman HM, McBride MA, et al. Aggressive pharmacologic donor management results in more transplanted organs. Transplantation. 2003;75(4):482–487. doi: 10.1097/01.TP.0000045683.85282.93. [DOI] [PubMed] [Google Scholar]
- 17.Selck FW, Deb P, Grossman EB. Deceased organ donor characteristics and clinical interventions associated with organ yield. Am J Transplant. 2008;8(5):965–974. doi: 10.1111/j.1600-6143.2008.02205.x. [DOI] [PubMed] [Google Scholar]
- 18.Rosendale JD, Kauffman HM, McBride MA, et al. Hormonal resuscitation yields more transplanted hearts, with improved early function. Transplantation. 2003;75(8):1336–1341. doi: 10.1097/01.TP.0000062839.58826.6D. [DOI] [PubMed] [Google Scholar]
- 19.Marik PE, Baram M, Vahid B. Does central venous pressure predict fluid responsiveness? A systematic review of the literature and the tale of seven mares. Chest. 2008;134(1):172–178. doi: 10.1378/chest.07-2331. [DOI] [PubMed] [Google Scholar]
- 20.Mascia L, Bosma K, Pasero D, et al. Ventilatory and hemodynamic management of potential organ donors: an observational survey. Crit Care Med. 2006;34(2):321–327. doi: 10.1097/01.CCM.0000196828.87358.6E. [DOI] [PubMed] [Google Scholar]
- 21.Frost AE. Donor criteria and evaluation. Clin Chest Med. 1997;18(2):231–237. doi: 10.1016/S0272-5231(05)70374-9. [DOI] [PubMed] [Google Scholar]
- 22.Fisher AJ, Dark JH, Corris PA. Improving donor lung evaluation: a new approach to increase organ supply for lung transplantation. Thorax. 1998;53(10):818–820. doi: 10.1136/thx.53.10.818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fisher AJ, Donnelly SC, Pritchard G, Dark JH, Corris PA. Objective assessment of criteria for selection of donor lungs suitable for transplantation. Thorax. 2004;59(5):434–437. doi: 10.1136/thx.2003.007542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Geiger RC, Kaufman CD, Lam AP, Budinger GR, Dean DA. Tubulin acetylation and histone deacetylase 6 activity in the lung under cyclic load. Am J Respir Cell Mol Biol. 2009;40(1):76–82. doi: 10.1165/rcmb.2007-0307OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kotani M, Kotani T, Li Z, Silbajoris R, Piantadosi CA, Huang YC. Reduced inspiratory flow attenuates IL-8 release and MAPK activation of lung overstretch. Eur Respir J. 2004;24(2):238–246. doi: 10.1183/09031936.04.00128703. [DOI] [PubMed] [Google Scholar]
- 26.Fisher AJ, Donnelly SC, Hirani N, et al. Enhanced pulmonary inflammation in organ donors following fatal non-traumatic brain injury. Lancet. 1999;353(9162):1412–1413. doi: 10.1016/S0140-6736(99)00494-8. [DOI] [PubMed] [Google Scholar]
- 27.Kaneda H, Waddell TK, de Perrot M, et al. Pre-implantation multiple cytokine mRNA expression analysis of donor lung grafts predicts survival after lung transplantation in humans. Am J Transplant. 2006;6(3):544–551. doi: 10.1111/j.1600-6143.2005.01204.x. [DOI] [PubMed] [Google Scholar]
- 28.Ranieri VM, Suter PM, Tortorella C, et al. Effect of mechanical ventilation on inflammatory mediators in patients with acute respiratory distress syndrome: a randomized controlled trial. JAMA. 1999;282(1):54–61. doi: 10.1001/jama.282.1.54. [DOI] [PubMed] [Google Scholar]
- 29.Tremblay L, Valenza F, Ribeiro SP, Li J, Slutsky AS. Injurious ventilatory strategies increase cytokines and c-fos m-RNA expression in an isolated rat lung model. J Clin Invest. 1997;99(5):944–952. doi: 10.1172/JCI119259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mascia L, Zavala E, Bosma K, et al. High tidal volume is associated with the development of acute lung injury after severe brain injury: an international observational study. Crit Care Med. 2007;35(8):1815–1820. doi: 10.1097/01.CCM.0000275269.77467.DF. [DOI] [PubMed] [Google Scholar]
- 31.Schultz MJ, Haitsma JJ, Slutsky AS, Gajic O. What tidal volumes should be used in patients without acute lung injury? Anesthesiology. 2007;106(6):1226–1231. doi: 10.1097/01.anes.0000267607.25011.e8. [DOI] [PubMed] [Google Scholar]
- 32.Brower RG, Lanken PN, MacIntyre N, et al. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. 2004;351(4):327–336. doi: 10.1056/NEJMoa032193. [DOI] [PubMed] [Google Scholar]
- 33.Brower RG, Morris A, MacIntyre N, et al. Effects of recruitment maneuvers in patients with acute lung injury and acute respiratory distress syndrome ventilated with high positive end-expiratory pressure. Crit Care Med. 2003;31(11):2592–2597. doi: 10.1097/01.CCM.0000090001.91640.45. [DOI] [PubMed] [Google Scholar]
- 34.Guerin C, Gaillard S, Lemasson S, et al. Effects of systematic prone positioning in hypoxemic acute respiratory failure: a randomized controlled trial. JAMA. 2004;292(19):2379–2387. doi: 10.1001/jama.292.19.2379. [DOI] [PubMed] [Google Scholar]
- 35.Meade MO, Cook DJ, Guyatt GH, et al. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2008;299(6):637–645. doi: 10.1001/jama.299.6.637. [DOI] [PubMed] [Google Scholar]
- 36.Taylor RW, Zimmerman JL, Dellinger RP, et al. Low-dose inhaled nitric oxide in patients with acute lung injury: a randomized controlled trial. JAMA. 2004;291(13):1603–1609. doi: 10.1001/jama.291.13.1603. [DOI] [PubMed] [Google Scholar]
- 37.Wheeler AP, Bernard GR, Thompson BT, et al. Pulmonary-artery versus central venous catheter to guide treatment of acute lung injury. N Engl J Med. 2006;354(21):2213–2224. doi: 10.1056/NEJMoa061895. [DOI] [PubMed] [Google Scholar]
- 38.Yamamoto H, Teramoto H, Uetani K, Igawa K, Shimizu E. Cyclic stretch upregulates interleukin-8 and transforming growth factor-beta1 production through a protein kinase C-dependent pathway in alveolar epithelial cells. Respirology. 2002;7(2):103–109. doi: 10.1046/j.1440-1843.2002.00377.x. [DOI] [PubMed] [Google Scholar]
- 39.Bhandari V. Molecular mechanisms of hyperoxia-induced acute lung injury. Front Biosci. 2008;13:6653–6661. doi: 10.2741/3179. [DOI] [PubMed] [Google Scholar]
- 40.Follette DM, Rudich SM, Babcock WD. Improved oxygenation and increased lung donor recovery with high-dose steroid administration after brain death. J Heart Lung Transplant. 1998;17(4):423–429. [PubMed] [Google Scholar]
- 41.McElhinney DB, Khan JH, Babcock WD, Hall TS. Thoracic organ donor characteristics associated with successful lung procurement. Clin Transplant. 2001;15(1):68–71. doi: 10.1034/j.1399-0012.2001.150112.x. [DOI] [PubMed] [Google Scholar]
- 42.Gabbay E, Williams TJ, Griffiths AP, et al. Maximizing the utilization of donor organs offered for lung transplantation. Am J Respir Crit Care Med. 1999;160(1):265–271. doi: 10.1164/ajrccm.160.1.9811017. [DOI] [PubMed] [Google Scholar]
- 43.Cantin B, Kwok BW, Chan MC, et al. The impact of brain death on survival after heart transplantation: time is of the essence. Transplantation. 2003;76(9):1275–1279. doi: 10.1097/01.TP.0000093445.50624.5A. [DOI] [PubMed] [Google Scholar]


