Key Points
Question
Is there an association between post-2014 Medicaid expansions and rates of opioid-related emergency department visits and inpatient hospitalizations?
Findings
In this difference-in-differences study evaluating institutions in 46 states and the District of Columbia, the post-2014 Medicaid expansions were associated with a statistically significant 9.7% reduction in the rate of opioid-related inpatient hospitalizations. There did not appear to be any associations between the pre-2014 or post-2014 Medicaid expansions on the rate of opioid-related emergency department visits.
Meaning
Expanding Medicaid may be useful for reducing opioid-related hospitalizations, possibly owing to better management of opioid use disorder in outpatient settings among the newly insured population.
Abstract
Importance
The rate of opioid-related emergency department (ED) visits and inpatient hospitalizations has increased rapidly in recent years. Medicaid expansions have the potential to reduce overall opioid-related hospital events by improving access to outpatient treatment for opioid use disorder.
Objective
To examine the association between Medicaid expansions and rates of opioid-related ED visits and inpatient hospitalizations.
Design, Setting, and Participants
A difference-in-differences observational design was used to compare changes in opioid-related hospital events in US nonfederal, nonrehabilitation hospitals in states that implemented Medicaid expansions between the first quarter of 2005 and the last quarter of 2017 with changes in nonexpansion states. All-payer ED and hospital discharges from 45 states in the Healthcare Cost and Utilization Project FastStats were included.
Exposures
State implementation of Medicaid expansions between 2005 and 2017.
Main Outcomes and Measures
Rates of all opioid-related ED visits and inpatient hospitalizations, measured as the quarterly numbers of treat-and-release ED discharges and hospital discharges related to opioid abuse, dependence, and overdose, per 100 000 state population.
Results
In the 46 states and District of Columbia included in the study, 1524 observations of emergency department data and 2219 observations of opioid-related inpatient hospitalizations were analyzed. The post-2014 Medicaid expansions were associated with a 9.74% (95% CI, −18.83% to −0.65%) reduction in the rate of opioid-related inpatient hospitalizations. There appeared to be no association between the pre-2014 or post-2014 Medicaid expansions and the rate of opioid-related ED visits (post-2014 Medicaid expansions, −3.98%; 95% CI, −14.69% to 6.72%; and pre-2014 Medicaid expansions, 1.02%; 95% CI, −5.25% to 7.28%).
Conclusions and Relevance
Medicaid expansion appears to be associated with meaningful reductions in opioid-related hospital use, possibly attributable to improved care for opioid use disorder in other settings.
This observational differences-in differences study examines the rates of opioid-related emergency department visits and inpatient hospitalizations before and after state Medicaid expansions.
Introduction
The opioid epidemic has reached crisis levels in the US. Approximately 400 000 people have died from opioid overdoses over the past 20 years.1 In contrast to the recent leveling and decline in opioid prescriptions, opioid-related hospital use continues to increase rapidly. In 2005 and 2017, the national rates of opioid-related emergency department (ED) visits and inpatient hospitalizations increased 225% and 150%, respectively (eFigure 1 in the Supplement).2,3 Hospital costs represent a substantial financial burden: direct hospital costs of opioid overdoses are nearly $11 billion nationwide.4
Opioid-related hospital events (ie, visits with an opioid use disorder or overdose diagnosis) may reflect inadequate access to timely, effective treatment, such as opioid agonist treatment with buprenorphine or methadone.5,6 A major barrier to treatment is a lack of health insurance coverage. Historically, many low-income individuals with opioid use disorder were uninsured and dependent on resource-constrained safety net health care professionals. Many individuals with opioid use disorder avoid seeking treatment and subsequently require hospital care for an overdose or associated complications.7,8
One of the goals of the 2014 Affordable Care Act (ACA) Medicaid expansion was to increase access to mental health and opioid use disorder treatment. Several studies found that expanding Medicaid to the low-income population was associated with increased access to primary care and behavioral health services in general, and with increased access to outpatient treatment for opioid use disorder in particular.9,10,11,12,13,14,15 However, little is known about how Medicaid expansion affects opioid-related hospital use.
To the extent that Medicaid expansions improve access to outpatient treatment, the expansions have the potential to reduce the overall rate of opioid-related hospital events. Such reductions could generate considerable cost savings and health improvements. Conversely, newly insured patients may be more likely to use the ED if they believe that they can afford to because the visit is covered by Medicaid. Prior studies suggested that gaining Medicaid coverage can increase overall use of the ED, including for mental health conditions,16 but little is known about how Medicaid expansion affects opioid-related hospital use.
Using state-level hospital discharge data from 46 states and the District of Columbia from 2005 to 2017, we assessed the association between Medicaid expansion and rates of opioid-related ED visits and inpatient hospitalizations and explored whether there are differences across states based on their preexisting opioid use disorder treatment capacity. Previous literature has documented, for example, that state variation in the availability of Drug Addiction Treatment Act–waivered physicians qualified to prescribe buprenorphine for opioid use disorder treatment is associated with increased prescriptions of buprenorphine.17,18,19 We also looked at the association between Medicaid expansion and the share of hospital care for Medicaid enrollees vs the uninsured.
Methods
Data Sources
Our ED and hospital discharge data came from the Healthcare Cost and Utilization Project FastStats—a database query tool published by the Agency for Healthcare Research and Quality.20 The FastStats data are drawn from the Agency for Healthcare Research and Quality’s State Inpatient Databases and State Emergency Department Databases, administrative data from US nonfederal, nonrehabilitation hospitals. The State Inpatient Databases capture nearly all hospitalizations, including those that originated from the ED, and the State Emergency Department Databases capture emergency visits at hospital-affiliated EDs that did not result in hospitalization (ie, treat-and-release visits). An observation in the State Emergency Department Databases will not be double-counted in the inpatient data because ED visits reported in the State Emergency Department Databases are limited to treat-and-release visits.
The FastStats have been used to study the association between state-level policies and hospital events.21,22 We obtained state quarterly-level inpatient data from 46 participating states and the District of Columbia, as well as ED data from 34 states and the District of Columbia, between the first quarter of 2005 and the last quarter of 2017. The data include inpatient and ED discharges for the overall population and selected subpopulations. We included data from as far back as 2005 (the first available year of FastStats) to have multiple pretreatment periods to assess differences in temporal trends between expansion and nonexpansion states before implementation of the expansions. FastStats reports visits for opioid use disorder and overdose from all opioid types, not distinguishing between illicit and licit sources.
Variable Measurement
Our main outcomes were the rates of all opioid-related ED visits and inpatient hospitalizations, measured as the quarterly number of discharges related to opioid abuse, dependence, or overdose, per 100 000 state population. Opioid-related conditions were identified by International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) and International Statistical Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) diagnostic codes. The eMethods in the Supplement provides the full set of diagnostic codes associated with opioid-related conditions. We used a natural logarithm version of the outcome variables to obtain normally distributed residuals in our linear regression analysis. The estimates from the logarithmic transformation provided us with the relative percentage changes of the outcomes.
Furthermore, we studied the shares of opioid-related ED visits and inpatient hospitalizations by expected primary payers (ie, Medicaid, private insurance, Medicare, and uninsured). In supplementary analyses, we studied outcomes among patient demographic subgroups identifiable in the FastStats data, including (1) sex, (2) age categories at admission (<25, 25-44, 45-64, and ≥65 years), (3) community-level income quartiles based on the median household income of patients’ zip code of residence, and (4) patient location (large metropolitan, medium metropolitan, small metropolitan, and rural).
Our key independent variables were indicators for state implementation of Medicaid expansions for low-income adults. We included separate indicators for the expansions that occurred in or after January 2014 (post-2014 expansions), and for those before 2014 (pre-2014 expansions); although it is important to learn from both periods, the post-2014 Medicaid expansions were more comprehensive than those that occurred earlier. The post-2014 expansions included 30 state expansions (including the District of Columbia) under the ACA State Plan Amendments provision or the Section 1115 waiver.23 The pre-2014 expansions included 9 state expansions under the Health Insurance Flexibility and Accountability waiver between 2005 and 2010 plus 3 states that were early, partial adopters of the ACA expansions between 2010 and 2013.14,23,24,25 The policy indicators were assigned a value of 1 in each full year subsequent to the effective date of the expansion in a state, and a value of 0 in preexpansion years in expansion states and for all years in the nonexpansion states. eTable 1 in the Supplement provides a detailed summary of state Medicaid expansions. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for case-control studies. The study was deemed exempt from approval and informed patient consent as using aggregate state-level deidentified data by the University of Kentucky Institutional Review Board.
Statistical Analysis
To estimate the association of Medicaid expansions with opioid-related hospital events, we used a difference-in-differences design that included state and year-quarter fixed effects. The 2-way, fixed-effects approach is commonly used in multistate, multipolicy analyses.26,27 Our state and year-quarter fixed effects accounted for unobserved, underlying differences across states as well as national secular trends and common changes (eg, the ICD-9 to ICD-10 transition in October 2015) that may have correlated with fluctuations in opioid-related hospital events and with state decisions on Medicaid expansion.
In addition to the overall policy effect of Medicaid expansions, we explored heterogeneous outcomes between states with high vs low capacity for outpatient OUD treatment. In the main analyses, treatment capacity was determined based on the per-capita number of Drug Addiction Treatment Act–waivered physicians (ie, office-based physicians who were qualified to prescribe buprenorphine for opioid use disorder treatment) in a state, and we divided states into those above and below the national average.28 Although not all prescribers with a waiver are active in prescribing buprenorphine, there is an association between the supply of waivered prescribers and the quantity of buprenorphine dispensed.29 In sensitivity analyses, we used the per capita number of outpatient specialty treatment facilities that provided opioid use disorder treatment with buprenorphine, methadone, and/or naltrexone as an alternative measure of treatment capacity.18
All models were weighted by state population30 and included time-varying control variables that adjusted for state-level health care supply, general economic conditions, and concurrent policies, including (1) per capita number of hospital beds, (2) poverty rate, (3) unemployment rate, (4) establishment and (5) comprehensive mandates of statewide prescription drug monitoring programs, (6) pain clinic laws, (7) Good Samaritan laws, (8) naloxone access laws, and (9) medical and (10) recreational marijuana laws and dispensaries. Standard errors were clustered at the state level to allow for arbitrary correlation within states but assume independence across states.31
Additional information on data sources, variable measurement, and model specification is presented in the eMethods in the Supplement. With 2-sided testing, P values <.05 were considered statistically significant. Analyses were conducted using Stata, version 16 (StataCorp).
Results
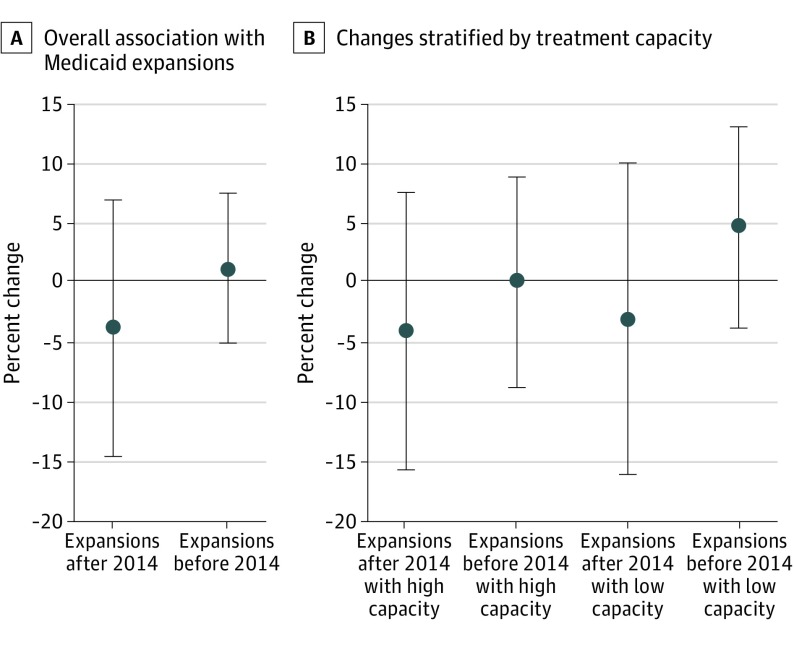
A total of 1524 observations of ED data and 2219 observations of opioid-related inpatient hospitalizations were analyzed. We did not find any statistically significant change in the rate of opioid-related ED visits associated with implementation of either the post-2014 Medicaid expansions (−3.98%; 95% CI, −14.69% to 6.72%) or pre-2014 Medicaid expansions (1.02%; 95% CI, −5.25% to 7.28%) (Table and Figure 1).
Table. Association Between Medicaid Expansion and Opioid-Related Hospital Eventsa.
| Variable | Without expansion (quarterly rate per 100 000 population) | Percentage change (95% CI) | |
|---|---|---|---|
| With post-2014 expansion | With pre-2014 expansion | ||
| Emergency department visits | 29.52 | −3.98 (−14.69 to 6.72) | 1.02 (−5.25 to 7.28) |
| Inpatient hospitalizations | 47.12 | −9.74 (−18.83 to −0.65)b | −3.91 (−9.16 to 1.33) |
Analysis of the Healthcare Cost and Utilization Project inpatient and emergency department data 2005-2017: 1524 state-quarter observations for emergency department visits, and 2219 state-quarter observations for inpatient hospitalizations. Baseline rates were calculated by setting the policy indicators for the implementation of the post-2014 expansions and the implementation of the pre-2014 expansions to 0s. The percentage changes corresponded to the estimated regression coefficients on the policy indicators for state implementation of the post-2014 expansions and the pre-2014 expansions, respectively. All regressions also controlled for covariates described in the eMethods in the Supplement.
Significant at P = .04; 95% CI clustered at the state level.
Figure 1. Association Between Medicaid Expansions and Opioid-Related Emergency Department Visits.
Analysis of 1524 observations from Healthcare Cost and Utilization Project emergency department data from the first quarter of 2005 to the last quarter of 2017. A and B, The percentage changes for the overall association corresponded to the estimated regression coefficients on the policy indicators for state implementation of the post-2014 expansions and the pre-2014 expansions. High vs low capacity is based on whether the state is above vs below the median in the population ratio of physicians with a waiver to prescribe buprenorphine in the postexpansion period. The percentage changes for the heterogeneous association for high- or low-capacity states corresponded to the sum of the coefficient on the expansion indicator and the coefficient on high or low treatment-capacity indicator. All regressions also control for covariates described in the eMethods in the Supplement.
We found that the post-2014 state implementation of Medicaid expansions was associated with a 9.74% (95% CI, −18.83% to −0.65%) reduction in the opioid-related inpatient hospitalization rate (Table and Figure 2), which translates to approximately 5 fewer hospital discharges per 100 000 population per quarter or, equivalently, 20 fewer discharges per 100 000 population per year. In 2005-2013, the aggregate number of opioid-related hospitalizations across all Medicaid expansion states in Healthcare Cost and Utilization Project Fast Stats was 96 728 per quarter among a total population of about 180 million in expansion states; this number implies that Medicaid expansion prevented a total of 9421 opioid-related hospitalizations per quarter. Pre-2014 expansions under the Health Insurance Flexibility and Accountability waiver and the early ACA adoption showed no association with opioid-related inpatient rate.
Figure 2. Association Between Medicaid Expansions and Opioid-Related Inpatient Hospitalizations.
Analysis of 2219 observations from Healthcare Cost and Utilization Project opioid-related inpatient hospitalization data from the first quarter of 2005 to the last quarter of 2017. A and B, The percentage changes for the overall association corresponded to the estimated regression coefficients on the policy indicators for state implementation of the post-2014 expansions and the pre-2014 expansions. High vs low capacity is based on whether the state is above vs below the median in the population ratio of physicians with a waiver to prescribe buprenorphine in the postexpansion period. The percentage changes for the heterogeneous association for high- or low-capacity states corresponded to the sum of the coefficient on the expansion indicator and the coefficient on high or low treatment-capacity indicator. All regressions also controlled for covariates described in the eMethods in the Supplement.
aP < .05.
Furthermore, the association between Medicaid expansions and opioid-related inpatient hospitalizations was more pronounced in the expansion states that had above-average rates of per capita Drug Addiction Treatment Act–waivered physicians (Figure 2; eTable 2 and eTable 3 in the Supplement). For these high-capacity states, associated reductions in opioid-related inpatient rates of 6.7% (95% CI, −12.0% to −1.3%) were noted with the pre-2014 expansions and 10.7% (95% CI, −20.7% to −0.7%) were noted with the post-2014 expansions. For states with low treatment capacity, there was no significant change in the opioid-related inpatient rate associated with pre- or post-2014 expansions. However, there is overlap in the 95% CIs of our estimates for the above- and below-average treatment capacity states, suggesting that the differences by capacity are not statistically significant from each other.
When examining the changes in opioid-related inpatient rates across different subgroups, we found that the reductions associated with Medicaid expansions were concentrated among individuals aged 25 to 64 years, individuals residing in the lowest income quartile zip codes, and those residing in large, central metropolitan areas (eTable 4 in the Supplement). These subgroups had some of the highest baseline rates of opioid hospitalizations: 66.93 hospitalizations per 100 000 population for individuals aged 25 to 44 years, 71.54 hospitalizations per 100 000 population for those residing in the lowest income quartile zip codes, and 61.65 hospitalizations per 100 000 population for those residing in large, central metropolitan areas; low-income, childless adults were the specific target of Medicaid expansion. No discernable association was found between Medicaid expansions and opioid-related ED visit rates across different subgroups (eTable 5, eTable 6, and eTable 7 in the Supplement).
In analyses in which payer share of opioid-related hospital events was the outcome variable (eTable 8 and eTable 9 in the Supplement), we found that post-2014 expansions were associated with a lower share of hospital events lacking insurance coverage, as well as with a higher share of hospital events paid for by Medicaid. Without expansion, an estimated 36.5% and 16.8% of opioid-related ED visits and inpatient hospitalizations remained uncovered by insurance, while Medicaid paid for an estimated 24.8% and 27.8% of opioid-related ED visits and inpatient admissions. For opioid-related ED visits, the post-2014 expansions were associated with a reduction in the uninsured share by 20.4 percentage points and an offsetting increase in the Medicaid share by 20.0 percentage points (eTable 8 in the Supplement). Both pre-2014 (1.85; 95% CI, 1.15-2.56 percentage points) and post-2014 (1.52; 95% CI, 0.08-2.96 percentage points) expansions were also associated with small, but statistically significant increases in the proportion of ED visits paid for by Medicare (eTable 8 in the Supplement). For opioid-related hospitalizations, the post-2014 expansions were associated with a reduction in the uninsured share by 11.1 percentage points and an increase in the Medicaid share by 10.0 percentage points (eTable 9 in the Supplement).
Discussion
We analyzed associations between Medicaid expansion and opioid-related hospital events using all-payer data on inpatient hospitalizations and ED discharges from 2005 to 2017. Our study yielded 4 main findings. First, we identified a reduction in opioid-related inpatient hospitalizations associated with the post-2014 state implementation of Medicaid expansion. Second, we found suggestive evidence of larger inpatient reductions in states with greater treatment capacity (proxied by the availability of outpatient buprenorphine prescribers) and among demographic groups most likely to benefit from Medicaid expansion (middle-aged adults and those residing in low-income zip code areas). Third, Medicaid expansion did not have any significant association with the overall rate of opioid-related ED admissions. Fourth, we found that the payers of admissions for inpatients and ED visits shifted from uninsured (ie, self-pay or charity care) to Medicaid.
Our findings suggest that expanding Medicaid may be a useful strategy for reducing opioid-related hospitalizations. This possible benefit may be due to better management of opioid use disorder in outpatient settings among newly insured individuals. Opioid use disorder is a chronic, relapsing illness that can be controlled with medications such as methadone and buprenorphine,32 but a lack of insurance may reduce access to outpatient treatment. Studies have indicated that Medicaid expansions were associated with increases in treatment admissions (18%) and buprenorphine prescriptions (70%).10,12,13,15,33
Our observed 9.7% decline in the rate of opioid-related inpatient hospitalizations following the 2014 expansions is consistent with an offsetting reduction in inpatient care, particularly among populations most likely to benefit from ACA Medicaid expansion. However, no significant reduction occurred in the pre-2014 expansions, which may be due to the relatively smaller number of people that gained coverage under these more modest eligibility expansions.
We also found some suggestive evidence that opioid-related hospitalizations decreased more in states with a greater number of outpatient health care professionals who can prescribe buprenorphine. This finding could be because there are more clinicians able to meet the demands of newly insured individuals, but access for the newly insured is not as comprehensive in states with less capacity. This association has also been suggested in a recent study that compared Medicaid expansion association with outpatient opioid use disorder treatment in lower- and higher-capacity states.13 However, we caution that the 95% CIs of our estimates for the above- and below-average treatment capacity states overlap and that further research is needed to understand the association between outpatient treatment capacity for opioid use disorder and hospitalization rates.
Our results suggest that Medicaid expansion did not have a statistically significant association with the overall rate of ED admissions. As noted, demand for ED care could either decrease if the ED is a substitute for care with outpatient clinicians or increase if newly insured patients feel more secure initiating care in the ED rather than avoiding medical clinicians altogether. Our findings cannot resolve what mechanisms may be present.
In addition, the shift in payment from self-pay and charity care to Medicaid underscores that Medicaid expansion is a financial benefit for the newly insured patients and hospitals. This shift in payment has also been observed with admissions to specialty substance use disorder care,12,34 where Medicaid expansion reduced financial burden on state and local governments. Individuals with opioid use disorder who enroll in Medicaid have very low incomes and limited access to credit. A hospital event can be financially devastating to such individuals and their families. Alternatively, medical debt among the uninsured population may be absorbed by hospital and local budgets for uncompensated care. Reducing this debt can improve the financial viability of safety net hospitals, and studies have noted that Medicaid expansion has staved off closure of these hospitals in expansion states.35
Limitations
Our study is subject to limitations. First, the Healthcare Cost and Utilization Project FastStats data are at the state level; although data are provided for some subgroups (eg, by age separately and by zip code income separately), we could not isolate the population that might be most affected by Medicaid expansion (low-income childless, nonelderly adults). Second, Medicaid expansions were not randomly assigned. Although our difference-in-differences methods control for some sources of bias, we cannot rule out the possibility that some other change occurred differentially in expansion vs nonexpansion states at the same time as the expansion, potentially biasing our difference-in-differences estimates. However, we estimated event study regressions comparing changes between expansion and nonexpansion states to assess parallel trends in the prepolicy period. eFigure 2 in the Supplement provides statistical data suggesting that the expansion and nonexpansion states mostly changed similarly in preexpansion years, which increases our confidence that the states would have continued to trend similarly were it not for the expansion.
Third, our data did not permit us to assess whether the severity of ED and hospital admissions changed or reliably identify which ED visits might be treatable in outpatient settings. We also did not observe visits related to injection opioid use, such as endocarditis, unless these visits also had an opioid use disorder diagnosis code. Fourth, we did not have the ability to link our hospital records to other treatment settings to directly observe whether patients were engaged in opioid use disorder treatment before or after their hospital visits. Rates of linkage to outpatient treatment following overdose are low,36 and it is important to understand how Medicaid expansion may be associated with this outcome.
Conclusions
Our study underscores the importance of Medicaid expansion in altering how patients with opioid use disorder interact with the medical system. To the extent that Medicaid expansion reduces avoidable hospitalizations, the expansion may be providing individuals with more patient-centered pathways into treatment. At the policy level, this study provides evidence suggesting that Medicaid expansion may be financially beneficial to safety-net hospitals that previously had to absorb opioid-related admissions as uncompensated care and can now seek reimbursement from Medicaid.
Our findings have implications for contemporary health policy debate at state and federal levels. An increasing number of states have been adopting Medicaid expansion.37 A Senate bill was recently introduced to ensure the currently non-expansion states receive the same federal matching funding as a state that originally expanded Medicaid if they choose to participate in the expansions in the future.38 Our results provide nonexpansion states additional information to consider in expanding Medicaid.
eMethods. Variable Measurement and Model Specification
eFigure 1. Opioid-Related Hospital Events per Quarter
eFigure 2. Event Study Regression Results
eTable 1. Summary of State Implementation of Medicaid Expansions for Adult Population, 2005-2017
eTable 2. Association Between Medicaid Expansion and Opioid-Related Inpatient Hospitalizations: High vs Low Treatment Capacity States
eTable 3. Association Between Medicaid Expansion and Opioid-Related Inpatient Hospitalizations: High vs Low Treatment Capacity States
eTable 4. Association Between Medicaid Expansion and Opioid-Related Inpatient Hospitalizations
eTable 5. Association between Medicaid Expansion and Opioid-Related Emergency Department Visits: High vs Low Treatment Capacity States
eTable 6. Association Between Medicaid Expansion and Opioid-Related Emergency Department Visits: High vs Low Treatment Capacity States
eTable 7. Association Between Medicaid Expansion and Opioid-Related Emergency Department Visits
eTable 8. Association Between Medicaid Expansion and Shares of Opioid-Related Emergency Department Visits by Expected Primary Payers
eTable 9. Association Between Medicaid Expansion and Shares of Opioid-Related Inpatient Hospitalizations by Expected Primary Payers
References
- 1.Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G. Drug and opioid-involved overdose deaths—United States, 2013-2017. MMWR Morb Mortal Wkly Rep. 2018;67(5152):1419-1427. doi: 10.15585/mmwr.mm675152e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guy GP Jr, Zhang K, Bohm MK, et al. Vital signs: changes in opioid prescribing in the United States, 2006-2015. MMWR Morb Mortal Wkly Rep. 2017;66(26):697-704. doi: 10.15585/mmwr.mm6626a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Agency for Healthcare Research and Quality (AHRQ) Healthcare Cost and Utilization Project (HCUP) statistical brief #219: opioid-related inpatient stays and emergency department visits by state, 2009-2014. Updated January 2017. Accessed January 14, 2019. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb219-Opioid-Hospital-Stays-ED-Visits-by-State.pdf
- 4.Premier. Opioid overdoses costing US hospitals an estimated $11 billion annually. Published January 3, 2019. Accessed January 14, 2019. https://www.premierinc.com/newsroom/press-releases/opioid-overdoses-costing-u-s-hospitals-an-estimated-11-billion-annually
- 5.Fiellin DA, Pantalon MV, Chawarski MC, et al. Counseling plus buprenorphine-naloxone maintenance therapy for opioid dependence. N Engl J Med. 2006;355(4):365-374. doi: 10.1056/NEJMoa055255 [DOI] [PubMed] [Google Scholar]
- 6.Volkow ND, Frieden TR, Hyde PS, Cha SS. Medication-assisted therapies—tackling the opioid-overdose epidemic. N Engl J Med. 2014;370(22):2063-2066. doi: 10.1056/NEJMp1402780 [DOI] [PubMed] [Google Scholar]
- 7.Stein BD, Pacula RL, Gordon AJ, et al. Where is buprenorphine dispensed to treat opioid use disorders? the role of private offices, opioid treatment programs, and substance abuse treatment facilities in urban and rural counties. Milbank Q. 2015;93(3):561-583. doi: 10.1111/1468-0009.12137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mark TL, Levit KR, Vandivort-Warren R, Buck JA, Coffey RM. Changes in US spending on mental health and substance abuse treatment, 1986–2005, and implications for policy. Health Aff (Millwood). 2011;30(2):284-292. doi: 10.1377/hlthaff.2010.0765 [DOI] [PubMed] [Google Scholar]
- 9.Andrews CM, Grogan CM, Smith BT, et al. Medicaid benefits for addiction treatment expanded after implementation of the Affordable Care Act. Health Aff (Millwood). 2018;37(8):1216-1222. doi: 10.1377/hlthaff.2018.0272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clemans-Cope L, Lynch V, Epstein M, Kenney GM Urban Institute. Medicaid coverage of effective treatment for opioid use disorder. Published May 2017. Accessed January 14, 2019. https://www.urban.org/sites/default/files/publication/90461/2001287-medicaid-coverage-of-effective-treatment-for-opiod-use-disorder-trends-in-state-buprenorphine-prescriptions-and-spending-since-2011.pdf
- 11.Golberstein E, Gonzales G. The effects of Medicaid eligibility on mental health services and out-of-pocket spending for mental health services. Health Serv Res. 2015;50(6):1734-1750. doi: 10.1111/1475-6773.12399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maclean JC, Saloner B. The effect of public insurance expansions on substance use disorder treatment: evidence from the Affordable Care Act. J Policy Anal Manage. 2019;38(2):366-393. doi: 10.1002/pam.22112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meinhofer A, Witman AE. The role of health insurance on treatment for opioid use disorders: evidence from the Affordable Care Act Medicaid expansion. J Health Econ. 2018;60:177-197. doi: 10.1016/j.jhealeco.2018.06.004 [DOI] [PubMed] [Google Scholar]
- 14.Wen H, Druss BG, Cummings JR. Effect of Medicaid expansions on health insurance coverage and access to care among low-income adults with behavioral health conditions. Health Serv Res. 2015;50(6):1787-1809. doi: 10.1111/1475-6773.12411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wen H, Hockenberry JM, Borders TF, Druss BG. Impact of Medicaid expansion on Medicaid-covered utilization of buprenorphine for opioid use disorder treatment. Med Care. 2017;55(4):336-341. doi: 10.1097/MLR.0000000000000703 [DOI] [PubMed] [Google Scholar]
- 16.Taubman SL, Allen HL, Wright BJ, Baicker K, Finkelstein AN. Medicaid increases emergency-department use: evidence from Oregon’s Health Insurance Experiment. Science. 2014;343(6168):263-268. doi: 10.1126/science.1246183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dick AW, Pacula RL, Gordon AJ, et al. Growth in buprenorphine waivers for physicians increased potential access to opioid agonist treatment, 2002-11. Health Aff (Millwood). 2015;34(6):1028-1034. doi: 10.1377/hlthaff.2014.1205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jones CM, Campopiano M, Baldwin G, McCance-Katz E. National and state treatment need and capacity for opioid agonist medication-assisted treatment. Am J Public Health. 2015;105(8):e55-e63. doi: 10.2105/AJPH.2015.302664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Knudsen HK, Lofwall MR, Havens JR, Walsh SL. States’ implementation of the Affordable Care Act and the supply of physicians waivered to prescribe buprenorphine for opioid dependence. Drug Alcohol Depend. 2015;157:36-43. doi: 10.1016/j.drugalcdep.2015.09.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Agency for Healthcare Research and Quality HCUP Fast Stats. Healthcare Cost and Utilization Project. Agency for Healthcare Research and Quality; 2018. [Google Scholar]
- 21.Nikpay S, Buchmueller T, Levy HG. Affordable Care Act Medicaid expansion reduced uninsured hospital stays in 2014. Health Aff (Millwood). 2016;35(1):106-110. doi: 10.1377/hlthaff.2015.1144 [DOI] [PubMed] [Google Scholar]
- 22.Nikpay S, Freedman S, Levy H, Buchmueller T. Effect of the Affordable Care Act Medicaid expansion on emergency department visits: evidence from state-level emergency department databases. Ann Emerg Med. 2017;70(2):215-225.e6. doi: 10.1016/j.annemergmed.2017.03.023 [DOI] [PubMed] [Google Scholar]
- 23.Atherly A, Dowd BE, Coulam RF, Guy G. The effect of HIFA waiver expansions on uninsurance rates in adult populations. Health Serv Res. 2012;47(3, pt 1):939-962. doi: 10.1111/j.1475-6773.2011.01376.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Coughlin TA, Long SK, Graves JA, Yemane A. An early look at ten state HIFA Medicaid waivers. Health Aff (Millwood). 2006;25(3):w204-w216. doi: 10.1377/hlthaff.25.w204 [DOI] [PubMed] [Google Scholar]
- 25.Sommers BD, Kenney GM, Epstein AM. New evidence on the Affordable Care Act: coverage impacts of early Medicaid expansions. Health Aff (Millwood). 2014;33(1):78-87. doi: 10.1377/hlthaff.2013.1087 [DOI] [PubMed] [Google Scholar]
- 26.Wooldridge JM. Econometric Analysis of Cross Section and Panel Data. MIT Press; October 2010:300-315. [Google Scholar]
- 27.Wing C, Simon K, Bello-Gomez RA. Designing difference in difference studies: best practices for public health policy research. Annu Rev Public Health. 2018;39:453-469. doi: 10.1146/annurev-publhealth-040617-013507 [DOI] [PubMed] [Google Scholar]
- 28.Breen CT, Fiellin DA. Buprenorphine supply, access, and quality: where we have come and the path forward. J Law Med Ethics. 2018;46(2):272-278. doi: 10.1177/1073110518782934 [DOI] [PubMed] [Google Scholar]
- 29.Lin LK, Simon K, Hollingsworth A, Saloner B. Association between the number of certified buprenorphine prescribers and the quantity of buprenorphine prescriptions: evidence from 2015 to 2017. J Gen Intern Med. 2019;34(11):2313-2315. doi: 10.1007/s11606-019-05165-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Solon G, Haider SJ, Wooldridge JM. What are we weighting for? J Hum Resour. 2015;50(2):301-316. doi: 10.3368/jhr.50.2.301 [DOI] [Google Scholar]
- 31.Bertrand M, Duflo E, Mullainathan S. How much should we trust differences-in-differences estimates? Q J Econ. 2004;119(1):249-275. doi: 10.1162/003355304772839588 [DOI] [Google Scholar]
- 32.Center for Medicaid and CHIP Services (CMCS) Informational bulletin: medication-assisted treatment for substance use disorders. Published July 11, 2014. Accessed January 14, 2019. https://www.medicaid.gov/Federal-Policy-Guidance/Downloads/CIB-07-11-2014.pdf
- 33.Saloner B, Levin J, Chang HY, Jones C, Alexander GC. Changes in buprenorphine-naloxone and opioid pain reliever prescriptions after the Affordable Care Act Medicaid expansion. JAMA Netw Open. 2018;1(4):e181588. doi: 10.1001/jamanetworkopen.2018.1588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Olfson M, Wall M, Barry CL, Mauro C, Mojtabai R. Impact of Medicaid expansion on coverage and treatment of low-income adults with substance use disorders. Health Aff (Millwood). 2018;37(8):1208-1215. doi: 10.1377/hlthaff.2018.0124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lindrooth RC, Perraillon MC, Hardy RY, Tung GJ. Understanding the relationship between Medicaid expansions and hospital closures. Health Aff (Millwood). 2018;37(1):111-120. doi: 10.1377/hlthaff.2017.0976 [DOI] [PubMed] [Google Scholar]
- 36.Larochelle MR, Bernson D, Land T, et al. Medication for opioid use disorder after nonfatal opioid overdose and association with mortality: a cohort study. Ann Intern Med. 2018;169(3):137-145. doi: 10.7326/M17-3107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kaiser Family Foundation Status of state action on the Medicaid expansion decision. Updated January 10, 2020. Accessed January 14, 2019. https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act
- 38.Warner MR. Same Act of 2019. US Senate. Published 2019. Accessed January 14, 2019. https://www.scribd.com/document/400655579/Same-Act-of-2019
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Variable Measurement and Model Specification
eFigure 1. Opioid-Related Hospital Events per Quarter
eFigure 2. Event Study Regression Results
eTable 1. Summary of State Implementation of Medicaid Expansions for Adult Population, 2005-2017
eTable 2. Association Between Medicaid Expansion and Opioid-Related Inpatient Hospitalizations: High vs Low Treatment Capacity States
eTable 3. Association Between Medicaid Expansion and Opioid-Related Inpatient Hospitalizations: High vs Low Treatment Capacity States
eTable 4. Association Between Medicaid Expansion and Opioid-Related Inpatient Hospitalizations
eTable 5. Association between Medicaid Expansion and Opioid-Related Emergency Department Visits: High vs Low Treatment Capacity States
eTable 6. Association Between Medicaid Expansion and Opioid-Related Emergency Department Visits: High vs Low Treatment Capacity States
eTable 7. Association Between Medicaid Expansion and Opioid-Related Emergency Department Visits
eTable 8. Association Between Medicaid Expansion and Shares of Opioid-Related Emergency Department Visits by Expected Primary Payers
eTable 9. Association Between Medicaid Expansion and Shares of Opioid-Related Inpatient Hospitalizations by Expected Primary Payers