Abstract
Background:
Postoperative opioid prescribing is often excessive, but the differences in opioid prescribing between teaching hospitals and non-teaching hospitals is not well understood. Given the workload of surgical training and frequent turnover of prescribers on surgical services, we hypothesized that postoperative opioid prescribing would be higher among teaching compared to non-teaching hospitals.
Study design:
We used insurance claims from a statewide quality collaborative in Michigan to identify 17,075 opioid-naïve patients who underwent 22 surgical procedures across 76 hospitals from 2012–2016. Our outcomes included 1) the amount of opioid prescribed for the initial postoperative prescription in oral morphine equivalents [OME] and 2) high risk prescribing in the 30 days after surgery (high daily dose [≥100 OME], new long-acting/extended-release opioid, overlapping prescriptions, or concurrent benzodiazepine prescription). Teaching hospital status was obtained from the 2014 American Hospital Association survey. Multilevel regression was used to adjust for patient and procedural factors and to perform reliability adjustment.
Results:
The amount of opioid prescribed per initial opioid prescription varied 4.7-fold across all hospitals from 130 OME to 616 OME. Patients discharged from teaching hospitals filled larger initial opioid prescriptions overall compared with non-teaching hospitals (251 OME vs. 232 OMEs; P=0.026). Teaching hospitals had higher risk adjusted rates of high risk prescribing compared with non-teaching hospitals (13.7% vs. 10.3%; P=0.034).
Conclusion:
In Michigan, surgical patients discharged from teaching hospitals received significantly larger postoperative opioid prescriptions and had higher rates of high risk prescribing compared to non-teaching hospitals. All hospitals, and particularly teaching institutions, should ensure adequate resources are devoted to facilitating safe postoperative opioid prescribing.
Keywords: Opioid, Opioid-Related Disorders, Pain, Postoperative/drug therapy, Surgery, Hospitals, Teaching, Education, Medical, Graduate
Introduction
The opioid epidemic in the United States is a major focus of health policy.1,2 Prescribed and non-medical use of prescription opioids plays an important role in this problem, highlighting a need for safer prescribing practices.1–3 Surgical prescribing for acute postoperative pain accounts for a considerable proportion of all prescription opioids.4 However, postoperative opioid prescribing is marked by wide variation in prescription amounts, and the majority of pills are often prescribed in excess.5–7 Overprescribing may lead to diversion of leftover pills, a common source of opioids among individuals reporting non-medical use.3
To date, specific guidelines for opioid prescribing following surgery are sparse and have not commonly been included in the rubric of surgical training. As such, surgical trainees lack standardized guidance on safe opioid prescribing. A recent study from a single teaching institution reported higher amounts of opioids prescribed among surgical residents compared to attendings.8 On the hospital level, it is unknown if opioid prescribing differs in teaching compared to non-teaching hospitals. In 2014, teaching hospitals represented 20% of hospitals yet performed 62% of surgeries in the United States, and thus may prove to be a high yield target for opioid prescribing reform.9,10 Surgical residents at teaching hospitals frequently rotate to different services, and this lack of continuity of care may adversely affect opioid prescribing compared to non-teaching hospitals with consistent providers. Understanding how postoperative opioid prescribing differs between teaching and non-teaching hospitals can help target policy and educational efforts related to opioid prescribing.
In this context, we compared opioid prescribing across hospitals within a large statewide quality collaborative to compare the amount of opioids prescribed, as well as high risk patterns of opioid prescribing, at teaching hospitals compared to non-teaching hospitals. Because surgical residents have a high workload and limited exposure to postoperative outpatient follow-up, we hypothesized that the amount of opioid prescribed per initial postoperative prescription, and incidence of high risk prescribing, would be higher at teaching than non-teaching hospitals. We also sought to identify other hospital factors associated with amount of opioids prescribed postoperatively.
Methods
Study Population
This was an analysis of commercial insurance claims from the Michigan Value Collaborative, a statewide quality collaborative whose methods of data collection have been previously described.11,12 Briefly, this dataset compiles preferred provider organization insurance claims from Blue Cross Blue Shield of Michigan which are aggregated as a statewide effort to improve value of healthcare in Michigan. We included adult patients with age 18 to 64 who underwent the following non-emergent surgical procedures between January 2012 and June 2016: open or laparoscopic appendectomy, open or laparoscopic cholecystectomy, Roux-en-Y gastric bypass, sleeve gastrectomy, open or laparoscopic non-cancer colectomy, open or thorascopic lung cancer resection, prostatectomy, colorectal cancer resection, esophagectomy, pancreatectomy, gastrectomy, coronary artery bypass graft, carotid endarterectomy, cardiac valve surgery, knee replacement, hip replacement, spine surgery, and hysterectomy. We included only cases that required an inpatient hospital stay. These procedures were chosen by the Michigan Value Collaborative in effort to improve value for these surgeries across Michigan. We chose to analyze these procedures in order to capture a broad range of procedures across multiple surgical subspecialties. We included only opioid-naïve patients to minimize variation in postoperative opioid prescribing attributable to opioid tolerance. Patients were considered opioid-naïve if they did not fill an opioid prescription within one year prior to surgery. Of note, this definition therefore does not capture patients who may obtain opioids from family, friends, or illicit sources. This study was approved by the University of Michigan Institutional Review Board.
Medical and pharmacy claims associated with the surgical episodes were analyzed from one year prior to surgery (to evaluate preoperative opioid use) to 30 days after postoperative hospital discharge. Because the aim of this study was to evaluate the size of the initial opioid prescription rather than the incidence of postoperative prescribing, our cohort was limited to patients who filled a postoperative opioid prescription within 7 days of hospital discharge. To minimize variation in opioid use attributable to opioid tolerance, we limited our analysis to patients who were preoperatively opioid-naïve, defined as patients who did not fill an opioid prescription between 365 and 31 days prior to surgery.13,14 We excluded patients with a hospital length of stay greater than 30 days as an attempt to minimize outlier cases. Finally, to eliminate patients who had subsequent surgeries, patients were excluded if they had additional procedure codes for anesthesia within 30 days of the index procedure.13
Hospital Characteristics, Teaching Status
Hospital characteristics were identified by linking claims to the 2014 American Hospital Association Annual Survey Database (using Medicare provider identification number) and included teaching hospital status, hospital size, and for-profit status. A hospital was considered a teaching hospital if, according to the definition used by Nationwide Inpatient Sample, the hospital was a member of the Council of Teaching Hospitals or had a ratio of full-time equivalent interns and residents to beds of 0.25 or higher.15 Hospital size was categorized based on number of beds as small, medium, or large, based on the definition used by the Nationwide Inpatient Sample.16 For-profit status hospitals were identified as hospitals that were neither non-profit nor government-owned.
Patient Characteristics
Patient factors were used for risk-adjustment and included age, gender, comorbidities, and procedure type (categorized into general surgery, joint and spine surgery, oncologic surgery, cardiothoracic and vascular surgery, and gynecologic surgery). Insurance claims from the six-month preoperative period were used to identify patient comorbidities according to the methodology of the Centers for Medicare and Medicaid Services (CMS) Hierarchical Condition Categories.17,18 This established method of risk-adjustment uses ICD-9 and −10 codes to identify 79 comorbid conditions. We used stepwise selection to identify a parsimonious subset of these comorbid conditions, and comorbidities that were associated with outcome (P<0.10) were included in the final multi-level model for risk-adjustment. Although-risk adjustment involved the individual comorbid conditions, as defined by CMS, these conditions were separately categorized by organ system for descriptive analysis.
Primary Outcome: Initial Postoperative Opioid Prescription Amount
Our primary outcome was amount of the initial postoperative prescription, which was defined as the first prescription filled within seven days of discharge from the index hospital stay. Opioid prescriptions were identified from pharmaceutical claims by linking National Drug Codes to generic drug names. Prescription amount was calculated by converting opioid dosages to oral morphine equivalents (OME) using standard conversion factors19,20. For reference, prescription amount was also reported as equivalent number of 5 mg hydrocodone tablets (5 OME is equivalent to one tablet of 5 mg hydrocodone).
Secondary Outcome: High Risk Opioid Prescribing
Our secondary outcome was a binary measure indicating incidence of one or more of the following measures of high risk prescribing over the 30 days following surgery: high daily dose (≥100 OME per day), new postoperative prescription for a long-acting or extended-release opioid, overlapping opioid prescriptions, and concurrent benzodiazepine prescriptions. Overlapping and concurrent prescriptions were defined based on number of days supplied and prescription fill date. These patterns of prescribing have been previously defined in administrative claims studies and are considered high risk and potentially inappropriate prescribing practices in the acute setting.19
Analysis
The outcome of initial prescription amount was log-transformed to ensure normally distributed residuals, and multivariable hierarchical linear regression was used to estimate the association of the aforementioned hospital-and patient-level factors with outcome. This model thus had two levels (hospital and patient) which enabled adjustment for clustering of patients within hospitals. To assess variability in initial prescription amount across hospitals, this model was used to compute risk-and reliability-adjusted OME per hospital. Reliability adjustment was performed using empirical Bayes methods to reduce the random variation attributable to statistical noise resulting from hospitals with small case volume.21 For the binary outcome of high risk prescribing, multivariable hierarchical logistic regression was used to estimate the association of hospital-and patient-level factors with outcome. Significance testing used two-sided tests with significance levels of α=0.05. Analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC) and Stata version 14.2 (StataCorp LLC, College Station, TX).
Results
Study Cohort
In this cohort, 17,075 opioid-naïve patients met inclusion criteria, spanning 76 Michigan hospitals. Table 1 shows patient and hospital characteristics of this study cohort overall, and in teaching compared to non-teaching hospitals. The majority of patients were female (62.8%). Case mix included 36.3% general, 33.1% joint and spine, 4.3% oncologic, 4.2% cardiothoracic or vascular, and 22.2% gynecologic surgical procedures. In teaching hospitals compared to non-teaching hospitals, comorbidities were more common, and joint/spine, oncologic, and cardiothoracic and vascular surgical procedures were more common.
Table 1: Patient and Hospital Characteristics.
| Overall | Teaching hospital | Non-teaching hospital | |
|---|---|---|---|
| Patient characteristics | No. (%) or mean ± standard deviation | ||
| Total no. patients | 17,075 | 14,354 | 2,721 |
| Female | 10,720 (62.8%) | 8,857 (61.7%) | 1,863 (68.5%) |
| Age | 48.5 ± 11.5 | 48.7 ± 11.5 | 47.2 ± 11.6 |
| Type of surgery | |||
| General | 6,190 (36.3%) | 5,088 (35.5%) | 1,102 (40.5%) |
| Joint/Spine | 5,658 (33.1%) | 4,860 (33.9%) | 798 (29.3%) |
| Oncologic | 727 (4.3%) | 662 (4.6%) | 65 (2.4%) |
| Cardiothoracic/Vascular | 709 (4.2%) | 683 (4.8%) | 26 (1.0%) |
| Gynecologic | 3,791 (22.2%) | 3,061 (21.3%) | 730 (26.8%) |
| Comorbidity | |||
| Cardiovascular disease | 1,634 (9.6%) | 1,465 (10.2%) | 169 (6.2%) |
| Pulmonary | 786 (4.6%) | 673 (4.7%) | 113 (4.2%) |
| Diabetes | 2046 (12.0%) | 1,757 (12.2%) | 289 (10.6%) |
| Kidney disease | 134 (0.8%) | 119 (0.8%) | 15 (0.6%) |
| Liver disease | 90 (0.5%) | 83 (0.6%) | 7 (0.3%) |
| Other gastrointestinal | 517 (3.0%) | 443 (3.1%) | 74 (2.7%) |
| Coagulopathy | 624 (3.7%) | 570 (4.0%) | 54 (2.0%) |
| Morbid obesity | 1,594 (9.3%) | 1,384 (9.6%) | 210 (7.7%) |
| Musculoskeletal | 727 (4.3%) | 636 (4.4%) | 91 (3.3%) |
| Cancer | 1,507 (8.8%) | 1,348 (9.4%) | 159 (5.8%) |
| Psychiatric | 708 (4.2%) | 593 (4.1%) | 115 (4.2%) |
| Hospital characteristics | |||
| Total no. hospital | 76 | 51 | 25 |
| Teaching hospital | 51 (67.1%) | 51 | 0 |
| Hospital size | |||
| Small | 21 (27.6%) | 14 (27.5%) | 7 (28.0%) |
| Medium | 25 (32.9%) | 16 (31.4%) | 9 (36.0%) |
| Large | 28 (36.8%) | 21 (41.2%) | 7 (28.0%) |
| Unknown | 2 (2.6%) | 0 (0.0%) | 2 (8.0%) |
| For-profit hospital | 6 (7.9%) | 6 (11.8%) | 0 (0.0%) |
Percentages represent column percentages.
Hospital Characteristics and Prescription Size
Of the 76 hospitals in this study, 51 (67.1%) were teaching hospitals, and 6 (7.9%) were for-profit. Hospital size was distributed relatively evenly. Overall, average OME per initial opioid prescription was 321 ± 272 (64 ± 54 tablets). As shown in Figure 1, the primary outcome of initial postoperative opioid prescription amount varied 4.7-fold across hospitals in Michigan, from 130 OME (26 tablets) to 616 OME (123 tablets), after risk-and reliability-adjustment. Procedure type explained 44% of the variation in opioid prescribing practices. After the effect of surgery type was controlled for, patient characteristics explained additional 0.5%, and provider and hospital characteristics (i.e., prescriber’s specialty, teaching status, hospital size, and for profit status) explained 1% variation. Table 2 shows hospital and patient factors associated with opioid prescription amount. Teaching hospital status was associated with 8% higher prescription amount compared to non-teaching hospitals (251 OME [50 tablets] vs. 232 OMEs [46 tablets], P=0.026, Figure 2a). This is equivalent to a difference of 4 tablets of 5-mg hydrocodone on average. Neither hospital size nor for-profit status were associated with prescription amount.
Figure 1: Variation in initial opioid prescription amount across hospitals.

This figure shows variation in OME per initial postoperative prescription, across Michigan hospitals. Results are risk-and reliability-adjusted.
Table 2:
Factors associated with initial postoperative opioid prescription amount.
| Estimate | 95% Confidence Interval | P-value | |
|---|---|---|---|
| Hospital characteristics | |||
| Teaching hospital | 1.08 | (1.01 1.16) | 0.026 |
| Hospital size (ref: Medium) | |||
| Small | 1.05 | (0.97 1.14) | 0.247 |
| Large | 1.07 | (0.99 1.16) | 0.085 |
| Unknown | 1.25 | (1.00 1.55) | 0.049 |
| For-profit hospital | 0.94 | (0.83 1.05) | 0.272 |
| Patient characteristics | |||
| Female | 0.96 | (0.95 0.98) | <0.001 |
| Age | 1.00 | (1.00 1.00) | 0.220 |
| Type of surgery (ref: General) | |||
| Joint/Spine | 2.53 | (2.46 2.60) | <0.001 |
| Oncologic | 1.04 | (1.00 1.08) | 0.074 |
| Cardiothoracic/Vascular | 1.34 | (1.28 1.41) | <0.001 |
| Gynecologic | 0.99 | (0.96 1.02) | 0.440 |
| Comorbidity | |||
| Rheumatoid arthritis and inflammatory connective tissue disease | 1.01 | (0.98 1.04) | 0.518 |
| Spinal cord disorders/injuries | 1.03 | (0.96 1.10) | 0.423 |
| Bone/joint/muscle infections/necrosis | 1.02 | (0.95 1.09) | 0.540 |
| Intestinal obstruction/perforation | 1.08 | (1.04 1.13) | <0.001 |
| Aspiration and specified bacterial pneumonias | 1.19 | (1.02 1.39) | 0.024 |
| Morbid obesity | 1.08 | (1.05 1.10) | <0.001 |
| Ischemic or unspecified stroke | 0.97 | (0.90 1.06) | 0.519 |
| Major depressive, bipolar, and paranoid disorders | 1.01 | (0.98 1.05) | 0.385 |
| Multiple sclerosis | 1.01 | (0.93 1.11) | 0.776 |
| Lymphoma and other cancers | 1.10 | (1.03 1.17) | 0.006 |
| Coagulation defects and other specified hematological disorders | 1.06 | (1.02 1.09) | 0.001 |
Results of the multi-level linear regression model. Outcome is log-transformed oral morphine equivalents (OME) per initial postoperative opioid prescription. Coefficient estimates are interpreted as the multiplicative change in OME per unit increase in the independent variable. Ref=reference.
Figure 2a and 2b: Initial opioid prescription amount and incidence of high risk prescribing in teaching vs. non-teaching hospitals.
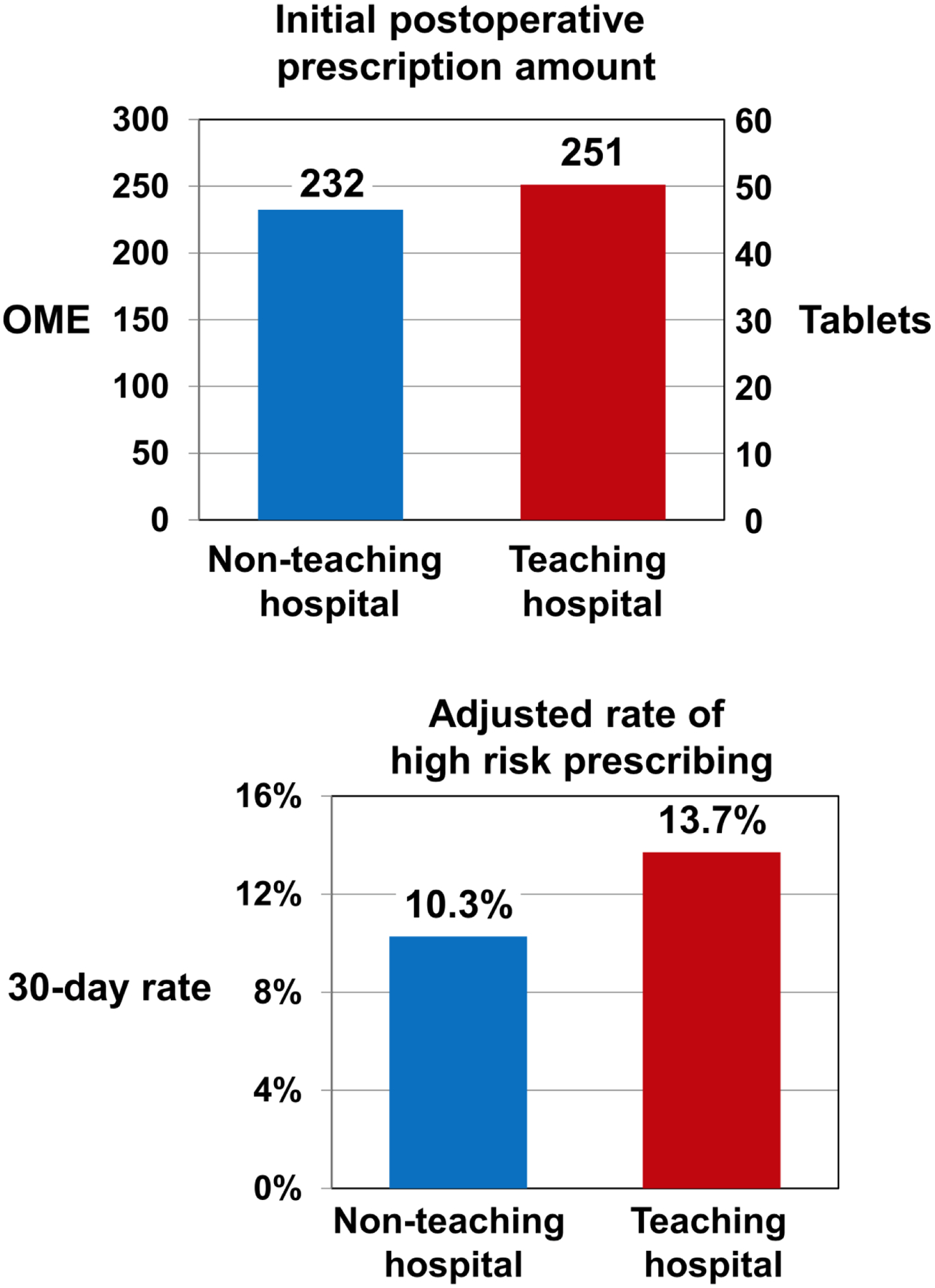
Results are risk-adjusted for patient and hospital characteristics. OME=oral morphine equivalents. Tablets indicates the equivalent amount in 5mg hydrocodone tablets.
Hospital Characteristics and High-Risk Prescribing
Table 3 shows unadjusted patterns of high risk prescribing by teaching hospital status. Compared to non-teaching hospitals, teaching hospitals had significantly higher rates of high risk prescribing (13.0% vs. 10.0%, P<0.001). Specific patterns of high risk prescribing that were significantly more common in teaching hospitals compared to non-teaching hospitals included high daily dose (8.9% vs. 6.8%, P<0.001) and concurrent benzodiazepine prescriptions (3.3% vs. 2.5%, P=0.038). Table 4 shows hospital and patient factors associated with high risk prescribing. Teaching hospital status was associated with a 51% increase in odds of high risk prescribing (adjusted rates 13.7% vs. 10.3%, P=0.034, Figure 2b). Neither hospital size nor for-profit status were associated with high risk prescribing (6 out of 76 hospitals were considered for-profit).
Table 3: Patterns of high risk prescribing by teaching hospital status.
.
| Overall | Teaching hospital | Non-teaching hospital | |
|---|---|---|---|
| N (%) | |||
| Any high risk prescribing | 2,142 (12.5%) | 1,871 (13.0%)* | 271 (10.0%) |
| High daily dose (≥100 OME per day) | 1,456 (8.5%) | 1,272 (8.9%)* | 184 (6.8%) |
| New long-acting/extended release | 188 (1.1%) | 161 (1.1%) | 27 (1.0%) |
| Overlapping opioid prescriptions | 231 (1.4%) | 198 (1.4%) | 33 (1.2%) |
| Concurrent benzodiazepine prescription | 546 (3.2%) | 477 (3.3%)* | 69 (2.5%) |
Numbers represent unadjusted incidence of the four markers of high risk prescribing.
indicates P<0.05 for teaching hospital compared to non-teaching hospital. OME=oral morphine equivalents.
Table 4: Factors associated with high risk prescribing.
| Odds Ratio | 95% Confidence Interval | P-value | |
|---|---|---|---|
| Hospital characteristics | |||
| Teaching hospital | 1.51 | (1.03 2.21) | 0.034 |
| Hospital size (ref: Medium) | |||
| Small | 0.69 | (0.44 1.08) | 0.104 |
| Large | 0.96 | (0.66 1.39) | 0.829 |
| Unknown | 4.34 | (1.58 11.88) | 0.004 |
| For-profit hospital | 0.88 | (0.45 1.71) | 0.706 |
| Patient characteristics | |||
| Female | 0.97 | (0.87 1.08) | 0.588 |
| Age | 0.99 | (0.98 0.99) | <0.001 |
| Type of surgery (ref: General) | |||
| Joint/Spine | 18. 08 | (15.07 21.69) | <0.001 |
| Oncologic | 1.62 | (1.08 2.43) | 0.019 |
| Cardiothoracic/Vascular | 3.29 | (2.37 4.56) | <0.001 |
| Gynecologic | 0.97 | (0.76 1.25) | 0.828 |
| Comorbidity | |||
| Rheumatoid arthritis, inflammatory connective tissue disease | 1.25 | (1.00 1.57) | 0.053 |
| Spinal cord disorders/injuries | 1.08 | (0.71 1.65) | 0.723 |
| Bone/joint/muscle infections/necrosis | 1.13 | (0.76 1.70) | 0.546 |
| Intestinal obstruction/perforation | 2.40 | (1.58 3.63) | <0.001 |
| Aspiration and bacterial pneumonias | 2.25 | (0.92 5.51) | 0.076 |
| Morbid obesity | 1.14 | (0.96 1.35) | 0.143 |
| Ischemic or unspecified stroke | 1.34 | (0.71 2.52) | 0.364 |
| Major depressive, bipolar, paranoia disorders | 1.40 | (1.07 1.82) | 0.015 |
| Multiple sclerosis | 1.24 | (0.64 2.40) | 0.533 |
| Lymphoma and other cancers | 1.95 | (1.14 3.34) | 0.015 |
| Coagulation defects and other hematological disorders | 1.30 | (1.03 1.64) | 0.030 |
Results of the multi-level logistic regression model. Outcome is any high risk prescribing. Ref=reference.
Discussion
In this statewide analysis of commercial insurance claims, the amount of opioid prescribed per initial postoperative opioid prescription varied widely across hospitals. After risk-adjustment for differences in hospital case mix, opioid prescriptions written in teaching hospitals were significantly larger, and high-risk prescribing was significantly more common in teaching hospitals, compared to non-teaching hospitals. Other hospital factors, including size and for-profit status, were not associated with opioid prescription amount.
The impact of a teaching hospital environment has been studied in the context of other surgical outcomes. Mortality is generally found to be lower in patients undergoing surgery at teaching hospitals compared to non-teaching hospitals.22–26 Surgical complications, however, are higher at teaching hospitals.23,26 Mechanisms underlying higher morbidity in teaching hospitals are unclear, but longer operative time due to resident involvement is thought to play a role.27 To date, the relationship between teaching hospitals and postoperative opioid prescribing is not well described, but trainee prescribing may be contributory. A recent study of resident prescribing practices within a single teaching hospital found that surgical residents prescribed larger total amounts of opioid compared to attending surgeons.8 The same study reported no difference in prescribing practices across resident post-graduate year. Residents may be the recipients of refill requests and thus prescribe higher amounts, despite recent evidence that amount prescribed is not correlated to incidence of refills.28,29 Our study did not investigate prescribing at the provider-level, and future work is needed to study resident prescribing practices across multiple institutions.
Education regarding safe opioid prescribing practices is inconsistent in graduate medical education, and guidelines to direct safe prescribing have been lacking.30,31 In a study of incoming surgical interns at a single academic institution, only 33% received training on opioid prescribing in medical school, and most reported feeling underprepared to prescribe opioids.32 The amount of opioids prescribed by those interns for mock surgical scenarios varied widely. Among all surgeons, opioid prescribing is variable and often excessive.5–7 In this study, even after adjusting for differences in case mix, an additional four tablets per patient on average were prescribed in teaching hospitals compared to non-teaching hospitals. This difference of four tablets on the hospital level amounts to an additional 55,000 opioid tablets potentially in excess among this sample alone. On a population level, this is a measurable and clinically relevant difference, as these excess pills have potential for diversion into the community. On the patient level, the relative increase in OME attributable to teaching hospital status will be greater in higher prescribing subgroups (such as joint and spine procedures, for example). In response, guidelines have recently been proposed for common procedures based on observed consumption data, and more work is needed to enhance and implement such guidelines.29,33,34 To effectively implement prescribing guidelines, buy-in at the hospital level should be achieved. Prescribing guidelines may be particularly important in teaching hospitals to optimize resident prescribing practices. For example, wide-ranging case mixes for trainees, who rotate through a range of surgical specialties, may impede accurate judgement of case-specific postoperative pain and analgesic requirements. Additionally, trainees have a relative lack of continuity in postoperative care. Residents often rotate off service before seeing patients in clinic postoperatively. In this manner, a resident’s opioid prescribing behavior is disconnected from the patient’s postoperative recovery. Thus, guidelines based on patient-reported pain and opioid consumption are critical to informing resident prescribing practices.
The patterns of high risk prescribing in teaching hospitals indicate that opioid prescribing curricula and guidelines should consider safe daily dosages and avoidance of overlapping prescriptions. Daily dosages greater than 100 OMEs were 31% more common in teaching hospitals than non-teaching hospitals, and this amount is considered a maximum daily dose, above which morbidity and mortality is increased.35–37 Further, concurrent prescribing of opioids and benzodiazepines should be avoided due to increased overdose risk.38 Regarding other hospital characteristics assessed in our study, we found no evidence of higher opioid prescribing in for-profit hospitals. Although interpretation of this finding should consider the limitation of low sample size (6 out of 76 hospitals were considered for-profit), this is nevertheless an encouraging result to further investigate with larger studies. With CMS linking payments to pain management satisfaction scores, there is concern that financial incentives may drive opioid prescribing. As counter-evidence to this point, recent findings demonstrated no correlation between hospital-level opioid prescribing and pain management satisfaction scores.39 As of 2018, CMS will no longer include pain management in the determination of hospital payments.40
Although the focus of this study was hospital factors, in particular teaching hospital status, our results show that patient level factors such as procedure type contribute significantly to variation in postoperative opioid prescribing. This is due in part to differences in pain and analgesic needs for different procedures, but this may also reflect differences in prescribing practices across surgical departments and an excellent candidate for intervention in need of further investigation. Our results suggest that intervention “upstream” at the hospital level is complex and should incorporate consideration for procedural factors as well. Much of the current efforts to optimize surgical opioid prescribing—such as procedure-specific guidelines, for example—are already focusing on these procedural differences. Thus, targeting hospital level factors as part of a multifaceted strategy may enable development of sustainable best practices that residents can carry forward in their future surgical careers. Previous work by Howard et al. has noted the unintentional benefits in prescribing habits across surgeries, named the “spillover effect41,” caused by evidence-based guidelines imposed on a distinct procedure. These interventions at the hospital level additionally hold promise to reduce opioid prescribing across other factors in perhaps a similar manner.
This study has several limitations. First, this was an analysis of commercial insurance claims from a single state, and thus it may not be representative of hospitals in other regions or prescribing practices for publicly insured patients. Namely, patients covered by Medicare and Medicaid are not included. However, this dataset is inclusive of a majority of the commercially insured individuals in Michigan. It is also important to note that claims data can only show prescription fills, and the actual amount consumed is unknown. Additionally, opioids procured from other sources including illicit means would not be captured in our analysis. We also cannot identify the indication for opioid prescriptions, but by limiting our analysis to opioid-naïve patients and only including fills within one week of surgery, it is likely that these prescriptions are attributable to surgical pain.
Conclusions
Postoperative opioid prescribing in Michigan varies widely across hospitals, and amount prescribed is significantly higher, and prescribing patterns are more likely to be high risk, in teaching hospitals compared to non-teaching hospitals. Notably, variation in opioid prescribing is indeed multifactorial, but further work is needed to understand the degree to which this finding is related to trainee prescribing and variations between specialties. Nevertheless, promotion of safe postoperative opioid prescribing practices should include a focus on resident education, including procedure-specific guidelines to direct opioid prescribing after surgery.
Acknowledgements
Financial Support:
Supported by the National Research Service Award postdoctoral fellowship (No. 5T32 CA009672-23) (J.S.L.), the National Institute on Drug Abuse (Research Project Grant No. R01 DA042859) (C.M.B., M.J.E., and J.F.W.), the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health (No. K24-AR053120-06)(K.C.C.), the Michigan Department of Health and Human Services (C.M.B., M.J.E., and J.F.W.), and Blue Cross Blue Shield of Michigan (J.M.D).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest: C.M.B. reports a patent for Peripheral Perineural Dexmedetomidine licensed to the University of Michigan and is a consultant for Recro Pharma and Heron Therapeutics. C.M.B. has received research funding from Neuros Medical.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Michigan Department of Health and Human Services. Support for the Michigan Value Collaborative is provided by Blue Cross Blue Shield of Michigan as part of the Blue Cross Blue Shield of Michigan Value Partnerships program; however, the opinions, beliefs and viewpoints expressed by the authors do not necessarily reflect those of Blue Cross Blue Shield of Michigan or any of its employees.
References:
- 1.Guy GP Jr., Zhang K, Bohm MK, et al. Vital Signs: Changes in Opioid Prescribing in the United States, 2006–2015. MMWR Morb Mortal Wkly Rep 2017;66(26):697–704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rudd RA, Seth P, David F, Scholl L. Increases in Drug and Opioid-Involved Overdose Deaths - United States, 2010–2015. MMWR Morb Mortal Wkly Rep. 2016;65(5051):1445–1452. [DOI] [PubMed] [Google Scholar]
- 3.Han B, Compton WM, Blanco C, Crane E, Lee J, Jones CM. Prescription Opioid Use, Misuse, and Use Disorders in U.S. Adults: 2015 National Survey on Drug Use and Health. Ann Intern Med. 2017;167(5):293–301. [DOI] [PubMed] [Google Scholar]
- 4.Levy B, Paulozzi L, Mack KA, Jones CM. Trends in Opioid Analgesic-Prescribing Rates by Specialty, U.S., 2007–2012. Am J Prev Med. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hill MV, McMahon ML, Stucke RS, Barth RJ Jr. Wide Variation and Excessive Dosage of Opioid Prescriptions for Common General Surgical Procedures. Ann Surg. 2016. [DOI] [PubMed] [Google Scholar]
- 6.Bicket MC, Long JJ, Pronovost PJ, Alexander GC, Wu CL. Prescription Opioid Analgesics Commonly Unused After Surgery: A Systematic Review. JAMA Surg. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thiels CA, Anderson SS, Ubl DS, et al. Wide Variation and Overprescription of Opioids After Elective Surgery. Ann Surg. 2017. [DOI] [PubMed] [Google Scholar]
- 8.Blay E Jr., Nooromid MJ, Bilimoria KY, et al. Variation in post-discharge opioid prescriptions among members of a surgical team. Am J Surg. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Steiner CA, Karaca Z, Moore BJ, Imshaug MC, Pickens G Surgeries in hospital-based ambulatory surgery and hospital inpatient settings, 2014: statistical brief #223. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. May 2017. Available at: https://www.hcupus.ahrq.gov/reports/statbriefs/sb223-Ambulatory-Inpatient-Surgeries-2014.pdf. Accessed March 8, 2018. [Google Scholar]
- 10.Sutton JP, Washington RE, Fingar KR, Elixhauser A. Characteristics of safety-net hospitals, 2014: statistical brief #213. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. October 2016. Available at: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb213-Safety-Net-Hospitals-2014.pdf. Accessed March 8, 2018. [Google Scholar]
- 11.Herrel LA, Syrjamaki JD, Linsell SM, Miller DC, Dupree JM. Identifying Drivers of Episode Cost Variation With Radical Prostatectomy. Urology. 2016;97:105–110. [DOI] [PubMed] [Google Scholar]
- 12.Ellimoottil CE, Syrjamaki JD, Voit B, Guduguntla V, Miller DC, Dupree JM. Validation of a claims-based algorithm to characterize episodes-of-care. American Journal of Managed Care.23(11):e382–e386. [PubMed] [Google Scholar]
- 13.Brummett CM, Waljee JF, Goesling J, et al. New persistent opioid use after minor and major surgical procedures in us adults. JAMA Surgery. 2017:e170504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee JS, Hu HM, Edelman AL, et al. New Persistent Opioid Use Among Patients With Cancer After Curative-Intent Surgery. J Clin Oncol. 2017;35(36):4042–4049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project (HCUP). HCUP NIS Description of Data Elements. September 17, 2008. Available at: https://www.hcup-us.ahrq.gov/db/vars/hosp_teach/nisnote.jsp. Accessed January 15, 2018
- 16.Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project (HCUP). HCUP NIS Description of Data Elements. September 17, 2008. Available at: https://www.hcup-us.ahrq.gov/db/vars/hosp_bedsize/nisnote.jsp. Accessed January 15, 2018.
- 17.Pope GC, Kautter J, Ellis RP, et al. Risk adjustment of Medicare capitation payments using the CMS-HCC model. Health Care Financ Rev. 2004;25(4):119–141. [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Medicare and Medicaid Services. Risk Adjustment. January 3, 2017. Available at: https://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/Risk-Adjustors.html. Accessed October 18, 2017
- 19.Logan J, Liu Y, Paulozzi L, Zhang K, Jones C. Opioid prescribing in emergency departments: the prevalence of potentially inappropriate prescribing and misuse. Med Care. 2013;51(8):646–653. [DOI] [PubMed] [Google Scholar]
- 20.Sullivan MD, Edlund MJ, Fan MY, Devries A, Brennan Braden J, Martin BC. Trends in use of opioids for non-cancer pain conditions 2000–2005 in commercial and Medicaid insurance plans: the TROUP study. Pain. 2008;138(2):440–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dimick JB, Ghaferi AA, Osborne NH, Ko CY, Hall BL. Reliability adjustment for reporting hospital outcomes with surgery. Ann Surg. 2012;255(4):703–707. [DOI] [PubMed] [Google Scholar]
- 22.Burke LG, Frakt AB, Khullar D, Orav EJ, Jha AK. Association Between Teaching Status and Mortality in US Hospitals. JAMA. 2017;317(20):2105–2113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pradarelli JC, Scally CP, Nathan H, Thumma JR, Dimick JB. Hospital Teaching Status and Medicare Expenditures for Complex Surgery. Ann Surg. 2017;265(3):502–513. [DOI] [PubMed] [Google Scholar]
- 24.Dimick JB, Cowan JA Jr, Colletti LM, Upchurch GR Jr Hospital teaching status and outcomes of complex surgical procedures in the United States. Arch Surg. 2004;139(2):137–141. [DOI] [PubMed] [Google Scholar]
- 25.Sheetz KH, Dimick JB, Ghaferi AA. Impact of Hospital Characteristics on Failure to Rescue Following Major Surgery. Ann Surg. 2016;263(4):692–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Holena DN, Hadler R, Wirtalla C, Carr B, Morris JB, Kelz RR. Teaching status: the impact on emergency and elective surgical care in the US. Ann Surg. 2011;253(5):1017–1023. [DOI] [PubMed] [Google Scholar]
- 27.Krell RW, Birkmeyer NJ, Reames BN, Carlin AM, Birkmeyer JD, Finks JF. Effects of resident involvement on complication rates after laparoscopic gastric bypass. J Am Coll Surg. 2014;218(2):253–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sekhri S, Arora NS, Cottrell H, et al. Probability of Opioid Prescription Refilling After Surgery: Does Initial Prescription Dose Matter? Ann Surg. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Howard R, Waljee J, Brummett C, Englesbe M, Lee J. Reduction in Opioid Prescribing Through Evidence-Based Prescribing Guidelines. JAMA Surg. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mezei L, Murinson BB. Pain education in North American medical schools. J Pain. 2011;12(12):1199–1208. [DOI] [PubMed] [Google Scholar]
- 31.Khidir H, Weiner SG. A Call for Better Opioid Prescribing Training and Education. West J Emerg Med. 2016;17(6):686–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nooromid MJ, Mansukhani NA, Deschner BW, et al. Surgical interns: Preparedness for opioid prescribing before and after a training intervention. Am J Surg. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hill MV, Stucke RS, McMahon ML, Beeman JL, Barth RJ, Jr. An Educational Intervention Decreases Opioid Prescribing After General Surgical Operations. Ann Surg. 2018;267(3):468–472. [DOI] [PubMed] [Google Scholar]
- 34.Opioid Prescribing Recommendations for Surgery. March 12, 2018. Available at: https://opioidprescribing.info/. Accessed March 28, 2018. [Google Scholar]
- 35.Bohnert AS, Valenstein M, Bair MJ, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305(13):1315–1321. [DOI] [PubMed] [Google Scholar]
- 36.Bohnert AS, Logan JE, Ganoczy D, Dowell D. A Detailed Exploration Into the Association of Prescribed Opioid Dosage and Overdose Deaths Among Patients With Chronic Pain. Med Care. 2016;54(5):435–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dunn KM, Saunders KW, Rutter CM, et al. Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med. 2010;152(2):85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sun EC, Dixit A, Humphreys K, Darnall BD, Baker LC, Mackey S. Association between concurrent use of prescription opioids and benzodiazepines and overdose: retrospective analysis. BMJ. 2017;356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee JS, Hu HM, Brummett CM, et al. Postoperative Opioid Prescribing and the Pain Scores on Hospital Consumer Assessment of Healthcare Providers and Systems Survey. JAMA. 2017;317(19):2013–2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Centers for Medicare & Medicaid Services (CMS), HHS. Medicare program. Fed Regist. 2016;81(219):79562–79892. [PubMed] [Google Scholar]
- 41.Howard R, Alameddine M, Klueh M, et al. Spillover Effect of Evidence-Based Postoperative Opioid Prescribing. J Am Coll Surg. 2018;227(3):374–381. [DOI] [PMC free article] [PubMed] [Google Scholar]


