Abstract
Background. Adherence to Mediterranean dietary patterns reduces the incidence of cardiovascular disease and other major chronic diseases. We aimed to assess the association between participation in kitchen-based nutrition education and Mediterranean diet intake and lifestyle medicine counseling competencies among medical trainees. Methods. The Cooking for Health Optimization with Patients (CHOP) curriculum is a hands-on cooking-based nutrition education program implemented at 32 medical programs (4125 medical trainees) across the United States. Mediterranean diet intake, nutrition attitudes, and lifestyle medicine counseling competencies were assessed via validated surveys. Multivariable-adjusted logistic regression assessed the relationship of CHOP education with Mediterranean diet intake, nutrition attitudes, and lifestyle medicine counseling competencies. Results. Individuals participating in the CHOP program were 82% more likely to follow the Mediterranean diet compared with those receiving traditional nutrition education (OR = 1.82; P < .001). CHOP participants were more likely to satisfy daily intake of fruits (OR = 1.33; P = .019) and vegetables (OR = 2.06; P < .001) and agree that nutrition counseling should be a routine component of clinical care (OR = 2.43; P < .001). Kitchen-based nutrition education versus traditional curricula is associated with a higher likelihood of total counseling competency involving 25 lifestyle medicine categories (OR = 1.67; P < .001). Conclusion. Kitchen-based nutrition education is associated with cardioprotective dietary patterns and lifestyle medicine counseling among medical trainees.
Keywords: cooking, nutrition therapy, diet, lifestyle, Mediterranean diet, cardiovascular disease, prevention
‘Society cannot effectively prevent cardiovascular and cardiometabolic disease without proper nutrition curricula infrastructure in health care education.’
Introduction
Poor-quality diet is a primary driver for morbidity and mortality in the world as well as in the United States.1-3 Dietary risk factors are implicated in nearly 1 in 5 deaths globally and are intricately linked to prevalent cardiovascular diseases and cardiometabolic conditions, including coronary heart disease, stroke, type 2 diabetes, and obesity.4-8 These diseases generate significant health burden, placing financial stress on broader health care systems.9 The lifetime risk of cardiovascular disease is nearly 50% for healthy individuals aged 30 years or older,10 and cardiovascular disease is our nation’s most expensive chronic disease, with costs expected to at least double by 2035.9,11 In the setting of these data, there is a need for substantive dietary interventions at both the patient and population-based levels to improve prevention and treatment and to help curb the cardiovascular disease epidemic.
Despite the intrinsic role of diet in both the prevention and pathophysiology of cardiovascular and cardiometabolic diseases, a disconnect exists between nutrition research, dietary education in medical training, and counseling patients about food consumption habits. According to recent reports, only one-half of primary care physicians regularly educate their patients about the dietary implications for their health.12 Likewise, only one-fifth of American medical schools have nutrition competency programs in their curricula,13 and less than one-third of medical school graduates report preparedness regarding nutrition counseling for patients.14 These findings suggest a systematic deficiency of dietary education in the continuum of medical training, one that appears to negatively affect our paradigm and approach to chronic disease prevention. Society cannot effectively prevent cardiovascular and cardiometabolic disease without proper nutrition curricula infrastructure in health care education.
Lifestyle medicine approaches, such as community-based culinary and nutrition programs, may be considered the keystone to preventing cardiovascular and cardiometabolic diseases among physicians and their patients. According to a formidable body of evidence, adherence to a Mediterranean style diet reduces total mortality as well as risk for developing cardiovascular and associated metabolic diseases.15-18 Likewise, Mediterranean diet adherence has also been shown to play a role in secondary prevention, reducing the risk of secondary cardiovascular events and slowing disease progression.19,20 The Mediterranean diet is a dietary pattern rich in fruits, vegetables, nuts, seeds, olive oil, whole grains, and legumes, supplemented with moderate amounts of fish, dairy, and poultry, with less intake of red meat.21
Previously, the Cooking for Health Optimization with Patients (CHOP) team has demonstrated that when compared with traditional medical school curricula, hands-on cooking and nutrition education for medical trainees centered on the key principles of the Mediterranean diet improves student dietary habits as well as their ability to counsel patients on nutrition.22 Now, given that more than 30 sites across the United States participate in CHOP and utilize the Health meets Food Culinary Medicine curriculum as part of their medical student or residency programs, this study has a more diverse sample and, thus, enhanced external validity compared with our previously published research. Through this larger sample, the association of kitchen-based nutrition education with clinical lifestyle medicine counseling competencies, in addition to personal dietary habits, was also assessed.
This report is an extension of CHOP, the first multicenter study on culinary medicine for medical trainees, providers, and patients and the largest nutrition education intervention study for medical trainees (ClinicalTrials.gov: NCT03443635). This study details measures of Mediterranean diet intake as well dietary counseling and attitudes among medical trainees across the United States.
Methods
Study Population
CHOP-Medical Trainees (CHOP-MT) is the CHOP substudy assessing medical trainees. From August 2012 to December 2018, nutritional surveys were completed across 32 sites, including medical schools and residency programs that offer the CHOP curriculum (Supplemental Table 1). The current sample includes 1219 medical trainees who participated in one 32-hour CHOP course (exposure) and 2906 medical trainees participating in traditional nutrition curricula (control). All 4125 medical trainees completed 1 nutrition survey during medical school training. For trainees participating in CHOP curricula, this survey was completed on completion of the kitchen-based nutrition education course. With respect to the control group, the survey was distributed and completed by a random sample of students not participating in CHOP curricula at participating institutions. Ethics approval for this research was obtained through the site-specific institutional review boards of all participating academic centers.
Explanatory Variables
CHOP Curriculum
The fundamental curriculum is an elective 32-hour nutrition and culinary course delivered through a sequence of eight 4-hour modules (one 4-hour module provided once per week over the course of 8 weeks). All 32 hours instruct students on evidence-based principles of the Mediterranean diet through both case-based team learning and hands-on cooking as well as validated approaches for patient nutrition counseling. The programming translates Mediterranean diet principals for the American kitchen, making the diet both more relevant and more accessible to students and patients. The 8 module topics include: (1) introduction to culinary medicine; (2) weight management, portion control, and breakfast; (3) dietary fats; (4) food allergy and intolerance; (5) dietary protein and vegetarian diets; (6) renal function, dietary sodium, hypertension, and flavor building; (7) dietary carbohydrates, snacks, and desserts; and (8) dietary patient interventions. Each professional health care student module involves an online 60-minute didactic program designed to introduce students to concepts of the Mediterranean diet. Students participate in an in-kitchen component involving 1.5 hours of team-based case studies and nutrition discussion along with 1.5 hours of hands-on cooking. The cooking component is intended to demonstrate the clinical and pathophysiologic concepts from the didactic phase, in a functional manner. Each module concludes with students engaging in completion and discussion of clinical case studies while consuming and sharing their prepared recipes. The CHOP curriculum is implemented as an elective course at participating institutions and is, thus, considered a passive explanatory variable that was not specifically allocated to participants.
Traditional Nutrition Education
A random sample of trainees not participating in CHOP curricula were selected as controls. These control group trainees derived from all participating institutions in the current analysis. Traditional nutrition education through medical education curricula was assumed to be homogeneous across all 32 participating partner sites. There is currently no evidence-based nutrition education standard broadly offered within schools, and most schools do not satisfy the minimum 25 nutrition hours recommended by the National Academy of Sciences.23
Outcome Variables
Mediterranean Diet Score
Mediterranean diet intake was assessed through a regularly utilized and validated questionnaire utilized by Trichopoulou et al15 in 2003 (Supplemental Table 2). This score assesses Mediterranean diet pattern intake by allocating 1 point for satisfying intake of protective foods, 1 point for restricting intake of nonprotective foods, and 0 points in the opposite of the 2 latter situations.15 This food frequency questionnaire involves a list of 9 dietary item categories central to the Mediterranean diet, including monounsaturated fats, fruit, vegetables, legumes, nuts/seeds, fish, red meat, whole grains, and alcohol. Survey respondents are given a score of 0 or +1 for each of the 9 food components using a food frequency questionnaire intended to capture dietary habits over the previous 6 months. A value of +1 was assigned in the following situations: 4 or more servings per day for vegetables, 1 or more servings per week for legumes, 3 or more servings per week for fruit, 1 or more servings per week for nuts/seeds, less than 2 and 3 servings per week of red meat for women and men, respectively, 2 or more servings per week of nonfried fish, 1 or more servings per day for whole grains, higher reported intake of unsaturated fats versus saturated fats, ½ to 1 drink or less of alcohol per day for women, and 1 to 2 drinks or less of alcohol per day for men. In all other situations, we assigned a 0 for each of the 9 food components. Scores were totaled for each participant to yield a continuous composite score. A higher score corresponds to a higher intake of Mediterranean diet components.
Nutritional Attitudes, Lifestyle Medicine Counseling Competencies, and Dietary Habits
A 25-item survey was developed to measure self-reported competencies in key lifestyle medicine–related topics, including competencies involving the Mediterranean diet, serving size, food labels, and total calories. Responses using a 3-point Likert scale24 were utilized to assess (1) attitudes regarding the role of nutrition counseling in patients’ dietary habits and (2) total competency in 25 key lifestyle medicine–related topics. Personal dietary habits were measured using a 6-point scale, which was unique and separate from the Mediterranean diet intake score. These latter scales were developed and modified from previously published nutrition and exercise scales for appropriate investigation of the novel intervention.25,26 Attitudes regarding the role of nutrition counseling in patients’ dietary habits were evaluated through the following survey statements: (1) nutrition counseling should be routine; (2) specific counseling can improve patients’ diets; and (3) physician counseling can improve patients’ diets. The specific format of these 3 surveys (nutrition attitudes, lifestyle medicine competencies, personal dietary habits) are represented in Supplemental Tables 3 and 4. The CHOP survey was developed using criterion-related validity by means of using the gold standard of the traditional Mediterranean Diet Score as a template for areas of interest to track for medical trainee behaviors for both the exposure and control groups.27 The CHOP Survey has been tested using hypothesis-testing validity for tracking validity of CHOP exposure by means of using the traditional nutrition curricula exposure group as a control.28 Surveys were completed by medical trainees in the exposure group 6 weeks after the date of their last CHOP curriculum class. Medical trainees in the control group had up to 6 weeks to complete the survey after electronically receiving the study surveys. The response rate for the CHOP surveys was 86%, such that of the 1418 students who participated in CHOP education, 1219 students filled out a survey.
Statistical Analysis
The CHOP curriculum was studied as an observational exposure variable in this cross-sectional study. Responses for nutritional attitudes, lifestyle medicine counseling competencies, and dietary habits were assessed in a binary fashion in statistical analyses; nutritional attitudes: strong agreement versus not; lifestyle medicine counseling competencies: complete proficiency versus not; dietary habits: satisfying daily intake requirement versus not. Strong agreement and complete proficiency for nutritional attitudes and lifestyle medicine counseling competencies, respectively, were defined through selection of the “mostly confident to totally confident” on the 3-point Likert-based surveys (Supplemental Table 3). The 3-point Likert scale was used to generate a response for each individual item. Satisfying daily intake was defined as follows: 3 to 5 times per/wk or more for vegetables, fruits, whole grains, and monounsaturated fats; 1 to 2 times per/wk or more for legumes and nut butters; 1 to 2 times per/wk or less for cheese or fermented dairy, nonfried fish or seafood, alcohol, and saturated fats; once per month/never for red and processed meat, baked products, and calorie-containing beverages (Supplemental Table 4).
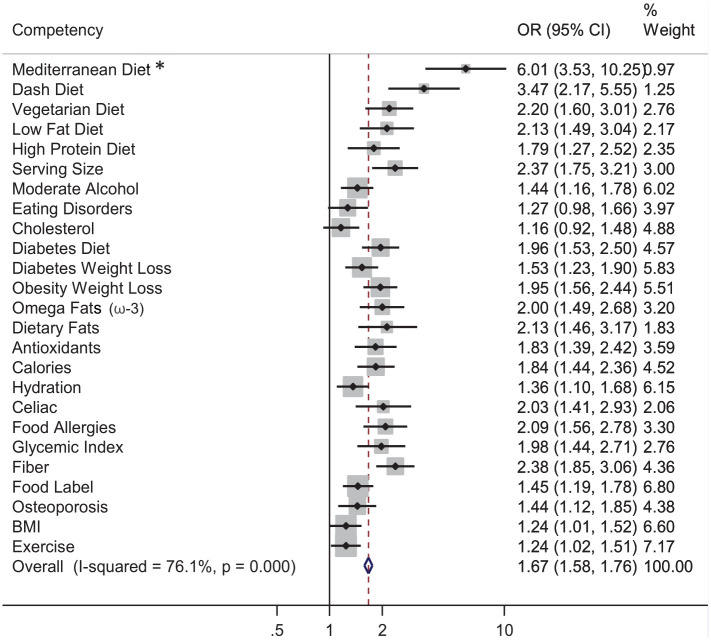
Propensity score–weighted logistic regression models were used to test the association of culinary medicine education on Mediterranean diet intake and nutritional attitudes, with traditional nutrition education serving as the reference independent variable. Propensity score methodology covets to control for unobserved heterogeneity from baseline differences as well as for self-selection.29,30 Study participants were matched based on their survey date as a means to control serial correlation as well as selection bias. Because of the dearth of validated psychometric end points for student lifestyle counseling competencies, fully adjusted odds ratios for total proficiency in each counseling category were generated. Using inverse variance–weighted meta-analysis, odds ratios and 95% CIs were subsequently pooled to produce 1 effect estimate (Figure 1). Cochran’s Q test and I2 statistic were used to test for heterogeneity of the effect estimate across a priori designated subgroup analysis by program year. Significant heterogeneity was determined using a P value threshold of .10. A more detailed version of our statistical methodology has been previously described in our previous CHOP series article involving medical trainees.22
Figure 1.
CHOP medical students (n = 4125): inverse variance–weighted meta-analysis of propensity score–adjusted multilevel mixed effects regression panel analysis of 25 competency topics in nutrition counseling.
Abbreviations: BMI, body mass index; CHOP, Cooking for Health Optimization with Patients; OR, odds ratio.
Sample size calculations were performed using previous treatment effect estimates of nutrition education on medical trainees. Power calculations demonstrated that 400 participant responses in total and 100 treatment-specific responses specifically were required to detect at least a 40% greater likelihood of Mediterranean diet intake and nutrition attitudes, with a power of 90%. Analyses were performed controlling for time-invariant unobserved traits as well as important covariates, including age, gender, race, prior nutrition education, special diet, school year, intended specialty, medical school, and likelihood of receiving CHOP classes. There was no clustering effect attributed to the CHOP curriculum exposure variable because the curriculum is provided regularly throughout the year and trainee participation is not restricted to certain groups of individuals or to certain dates of the year. Individuals with missing exposure, outcome, or covariate data were excluded from the analyses.
Results
Women represented a little more than one-half of the study sample, and individuals were on average 26 years of age. Nearly one-third of the study sample participated in the CHOP curriculum (Table 1).
Table 1.
Characteristics of 4125 Medical Trainees.
| Variable | Measure |
|---|---|
| Gender (%) | |
| Female | 51.13 |
| Male | 48.87 |
| Racea (%) | |
| White | 66.58 |
| Nonwhite | 33.42 |
| Age, years, mean (SD) | 25.98 (3.64) |
| Medical trainee training levelb (%) | |
| Preclinical | 64.36 |
| Clinical | 35.64 |
| Prior nutrition educationc (%) | 14.68 |
| Special dietary practicesd (%) | 20.54 |
| Participation in CHOP educational seriese (%) | 29.55 |
Abbreviation: CHOP, Cooking for Health Optimization with Patients.
Nonwhite defined as African American, Native American, Asian, and/or Hispanic.
Preclinical defined as medical school year levels 1 and 2.
Prior nutrition education defined as formal nutrition training in undergraduate or graduate coursework.
Special dietary practices defined by, but not limited to, gluten free, vegetarian, Weight Watchers, and/or kosher.
Reflects the percentage of survey respondents who were CHOP participants.
Culinary medicine education shared a significant positive association with all Mediterranean diet categories except wine (Table 2). Compared with students enrolled in traditional nutrition education, participants were at least twice as likely to adhere to Mediterranean diet guidelines involving monounsaturated fats (P = .009), fruit (P = .019), vegetables (P < .001), and legumes (P < .001). Similarly, CHOP program participants were 33%, 39%, 40%, and 70% more likely to adhere to Mediterranean diet guidelines regarding fruits (P = .019), whole grains (P = .001), fish (P = .002), and red meat (P < .001), respectively. Intake of olive oil had the highest magnitude point estimate among all Mediterranean diet categories (OR = 2.14; 95% CI = 1.21, 3.79).
Table 2.
Propensity Score–Adjusted Mixed-Effects Multivariable Regression of CHOP Versus Control on Overall Mediterranean Diet Intake and Individual Food Group Categories.a
| Category | OR (95% CI) | P Value |
|---|---|---|
| High/Medium vs low | 1.82 (1.45, 2.29) | <.001 |
| Olive oil | 2.14 (1.21, 3.79) | .009 |
| Fruit | 1.33 (1.05, 1.70) | .019 |
| Vegetables | 2.06 (1.61, 2.64) | <.001 |
| Legumes | 2.04 (1.49, 2.80) | <.001 |
| Fish | 1.41 (1.13, 1.75) | .002 |
| Alcohol | 1.40 (0.98, 1.98) | .064 |
| Meat | 1.71 (1.33, 2.20) | <.001 |
| Whole grains | 1.39 (1.15, 1.69) | .001 |
Abbreviations: CHOP, Cooking for Health Optimization with Patients.
Adjusted for age, gender, race, prior nutrition education, special diet, school year, intended specialty, medical school, likelihood of receiving CHOP classes, and time invariant unobserved traits.
Figure 1 demonstrates the relationship between the CHOP curricula and 25 lifestyle medicine counseling competency categories. Trainees were 6 times as likely to master total competency regarding Mediterranean diet principles compared with students who did not participate in culinary medicine education (P < .001). Likewise, students enrolled in hands-on culinary medicine education were more likely to achieve proficiency in 22 additional lifestyle medicine counseling categories, notably recommendations involving fiber (OR = 2.38; CI = 1.85, 3.06), serving size (OR = 2.37; CI = 1.75, 3.21), omega-3 fatty acids (OR = 2.00; CI = 1.49, 2.68), and a vegetarian diet (OR = 2.20; CI = 1.49, 2.68). CHOP education relationships with cholesterol and eating disorder competencies were nonsignificant. Participants were more than 2 times as likely to strongly agree with regular nutrition counseling for patients compared with students in traditional medical education curricula (Table 3).
Table 3.
Propensity Score–Adjusted Mixed Effects Multivariable Regression of CHOP Versus Control on Overall Nutrition Attitudes.a
| Outcome | OR (95% CI) | P Value |
|---|---|---|
| Nutrition counseling should be routine | 2.43 (1.94, 3.03) | <.001 |
| Specific counseling can improve patients’ diets | 1.74 (1.45, 2.09) | <.001 |
| Physicians’ counseling can improve patient’s diets | 1.62 (1.31, 2.01) | <.001 |
Abbreviations: CHOP, Cooking for Health Optimization with Patients.
Adjusted for age, gender, race, prior nutrition education, special diet, school year, intended specialty, medical school, likelihood of receiving CHOP classes, and time-invariant unobserved traits.
Discussion
CHOP-MT is a multicenter project for culinary medicine and the largest study on nutrition education and medical trainees. Trainees exposed to an 8-week kitchen-based nutrition education course were 82% more likely to satisfy intake of fruits, vegetables, and legumes, compared with medical trainees taking part in traditional nutrition education. Similarly, hands-on culinary medicine education was associated with a one-third and more than 2-fold higher daily consumption of fruits and vegetables, respectively. These results, in combination with significant positive associations of the programming with more than 20 total competencies in lifestyle medicine counseling, suggest that teaching kitchen-based nutrition and culinary education is associated with a higher intake of Mediterranean dietary components and knowledge of cardiovascular disease prevention among medical trainees.
Our findings fit into a larger context of evidence regarding the utility of nutrition-related training among medical trainees. Our results are consistent with similar previous studies suggesting that participation in nutrition-centered courses augments trainees’ confidence in dietary counseling. For example, Conroy et al25 observed that nearly three-fourths of medical students participating in a new preventive medicine and nutrition didactic course at Harvard medical school reported improvements in personal diets following the course. This study also found that students reported significant reductions in saturated fat consumption, one important dietary modification that can lower serum low-density lipoprotein cholesterol and, thus, reduce atherosclerotic cardiovascular disease risk.25 Likewise, even exposure to online nutrition lectures among medical trainees has been noted to improve knowledge and case-based management of diet for patients.31 These data not only underline the value of incorporating nutrition education across academic medical centers, but also highlight the novelty of our current study because this study characterized the role of kitchen-based nutrition education in medical training.
As discussed earlier, the Mediterranean diet has been robustly associated with not only reduced manifestation, but also progression of cardiovascular disease in a consistent fashion.15-20,32 Three cited barriers to adopting the Mediterranean diet are limited knowledge, lack of cooking skills, and time commitment.33 CHOP-MT has previously demonstrated that culinary medicine education is associated with a higher overall consumption of Mediterranean diet foods in medical trainees, particularly mediated through modified consumption of 7 key food categories: olive oil, fruit, vegetables, legumes, fish, meat, and whole grains.22 Considering the consistency and replicability of these findings across 32 sites, structured, kitchen-based nutrition education modules may overcome prevalent (eg, limited knowledge and lack of cooking skills) as well as seeming (eg, time commitment) barriers to adopting a Mediterranean diet.
Despite the central pathophysiological as well as the preventive role of diet in cardiovascular disease, nutrition education teaching and infrastructure is lacking. According to a national survey published in Academic Medicine, medical students received a mere 19.6 hours of nutrition training throughout all 4 years of medical school.23 Likewise, more than 50% of medical students report “inadequate” knowledge of nutrition.34 Through the CHOP-MT series, culinary medicine curricula have been consistently associated with a higher proficiency and competency in lifestyle medicine counseling.22 These relationships have a high probability of benefiting future patients because previous research has shown a positive association between physician and patient preventive health behaviors.35,36 Given that kitchen-based nutrition education, through the described curriculum, has already been implemented over 30 sites across the United States, our findings may serve as a platform for broader implementation of nutrition training in medical school.
In addition to helping prevent cardiovascular disease, adherence to the Mediterranean diet may also help reduce the incidence of other major chronic diseases, including cancer, Alzheimer disease, and chronic kidney disease. In a meta-analysis that includes predominantly observational data, high adherence to a Mediterranean diet was significantly associated with a 14% lower risk of overall cancer mortality, and the most consistent protective associations were observed for colorectal and breast cancer.37 Additionally, strong inverse associations of individual Mediterranean diet components, including whole grains, nuts, fruits, vegetables, and fish, with cancer incidence and mortality have also been observed.38-41 Much of the health benefits of the Mediterranean diet may be driven by the anti-inflammatory, anti-oxidative, and endothelial-protective properties of ingested foods.37 Minimization of vascular injury via Mediterranean diet adherence may particularly help lower the risk of chronic kidney disease and Alzheimer’s dementia because vascular dysregulation has been noted to be one of the first insults in the development of both diseases.42,43 In a prospective study including more than 6 years of follow-up among a diverse cohort of 60-year old men and women, higher Mediterranean diet adherence was associated with a 17% and 12% lower risk of chronic kidney disease incidence and estimated glomerular filtration rate decline, respectively.44 Likewise, high Mediterranean diet adherence is prospectively associated with fewer structural and functional brain changes suggestive of Alzheimer’s dementia, as measured by positron emission tomography and magnetic resonance imaging, among individuals as young as 30 years of age.45,46 These results in total suggest that dietary patterns rich in fruits, vegetables, legumes, nuts, and whole grains are an important component to chronic disease prevention and may help facilitate the likelihood of healthy aging.
This study has several important strengths. The multisite design afforded a unique opportunity to assess Mediterranean diet intake, one important protective factor for both primary and secondary prevention of cardiovascular disease, in a large and diverse population. Likewise, to our knowledge, CHOP-MT is the first study to assess kitchen-based nutrition education as an exposure variable and the role it holds in medical trainee lifestyle medicine attitudes and counseling.
Limitations of our study are also important to contemplate. Although training is part of the implementation at additional sites, the programming is taught by a variety of physicians, chefs, and dietitians, thus raising the potential for operator bias. Measures of fidelity used to reduce operator bias included standardized training of CHOP curriculum instructors, including the distribution of curriculum manuals, curriculum guides, and case studies to ensure that the CHOP curriculum exposure remained consistent, regardless of the class instructor. CHOP curriculum classes were also randomly audited by CHOP committee members to assess the standardization of all modules. Two other limitations to note are that (1) this study was unable to assess the longitudinal relationship between culinary medicine, and Mediterranean diet intake and CHOP curriculum exposure, and (2) propensity analysis may not have fully compensated for the potential situation in which individuals participating in CHOP had systematic differences in dietary patterns compared with those not participating in CHOP, regardless of the curriculum exposure. These limitations will be addressed in subsequent research by administering pre–kitchen-based and post–kitchen-based nutrition education surveys during each year of medical training among CHOP study participants, with each participant serving as his/her own control. In this way, potential selection bias will be decreased, and also observe important prospective relationships between CHOP education and dietary habits could be studied. Furthermore, the use of food frequency questionnaires after an educational exposure may bias parameter estimates in favor of the exposure or desired information. Yet this phenomenon may not be a true bias and may instead rather simply serve as a proxy of effectiveness of the educational exposure. Finally, whereas the CHOP curriculum is based on the Mediterranean diet, a dietary pattern that has consistently shown to have cardioprotective benefit, there are other dietary patterns that may be beneficial to consider with respect to cardiovascular disease prevention. Notably, adherence to the Dietary Approaches to Stop Hypertension (DASH) and vegetarian dietary patterns also reduce cardiovascular disease risk.47,48 Future studies that assess the key differences among these dietary patterns with respect to their relationship to cardiometabolic health and lifestyle medicine are undoubtedly necessary.
The current study demonstrates that kitchen-based nutrition education, when compared with traditional nutrition coursework, is associated with a higher likelihood of Mediterranean diet intake and lifestyle medicine counseling competence in medical trainees enrolled at 32 sites across the United States. Although these results are encouraging, there remain practical challenges associated with implementing culinary medicine programs more broadly, including the dearth of kitchen space at medical schools and competing educational topics in an already exhaustive medical school curriculum schedule. There are future opportunities for medical board examiners to add specific nutritional topics to board exams in an effort to incentivize incorporation of nutrition education standards across medical institutions and hospitals. In summary, our results provide a platform for nutrition education reform in American medical schools, suggesting that integrating nutrition didactics with hands-on cooking modules in a kitchen setting provides an optimized design to improve medical trainee diets as well as their clinical dietary counseling skills.
Supplemental Material
Supplemental material, Supplementary_Tables for Multisite Culinary Medicine Curriculum Is Associated With Cardioprotective Dietary Patterns and Lifestyle Medicine Competencies Among Medical Trainees by Alexander C. Razavi, Dominique J. Monlezun, Alexander Sapin, Zachary Stauber, Kara Schradle, Emily Schlag, Amber Dyer, Brennan Gagen, Isabella G. McCormack, Ofure Akhiwu, Leah Sarris, Kerri Dotson and Timothy S. Harlan in American Journal of Lifestyle Medicine
Acknowledgments
ACR, DJM, AS, ZS, KS, IGM, LS, ES, AD, BG, OA, KD, and TSH made substantial contributions to the interpretation of the data. ACR, DJM, and TSH made substantial contributions to the drafting of the manuscript. ACR and DJM made substantial contributions designing the study and analyzing the data. ACR, DJM, AS, ZS, KS, IGM, LS, ES, AD, BG, OA, KD, and TSH revised the article critically for important intellectual content and approved the final submitted version. All individuals named in the Acknowledgments section have provided consent to be named in the article.
Footnotes
Authors’ Note: Previous presentations: none. This article has not been previously published and is not under consideration at the same time or in substantially similar form in any other journal.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by several grants. Culinary Medicine programming was supported in part by the Goldring Family Foundation, The Woldenberg Family Foundation, the Humana Foundation, and the Robert Wood Johnson Foundation. Alexander C. Razavi is currently funded through a fellowship training grant supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under Grant Number F30HL147486.
Ethical Approval: Ethical approval was obtained through the local and site-specific institutional review boards for this research. Name of Institution Providing Institutional Review Board Review: The Administrators of the Tulane Educational Fund. IRB Registration No.: 00000324. FWA No.: 0000205. IRB Reference No.: 729959.
Informed Consent: Not applicable, because this article does not contain any studies with human or animal subjects.
Trial Registration: Cooking for Health Optimization with Patients (CHOP)-Family Bayesian adapted randomized controlled trial (https://clinicaltrials.gov/ct2/show/NCT03443635; unique identifier: 03443635).
ORCID iDs: Alexander C. Razavi 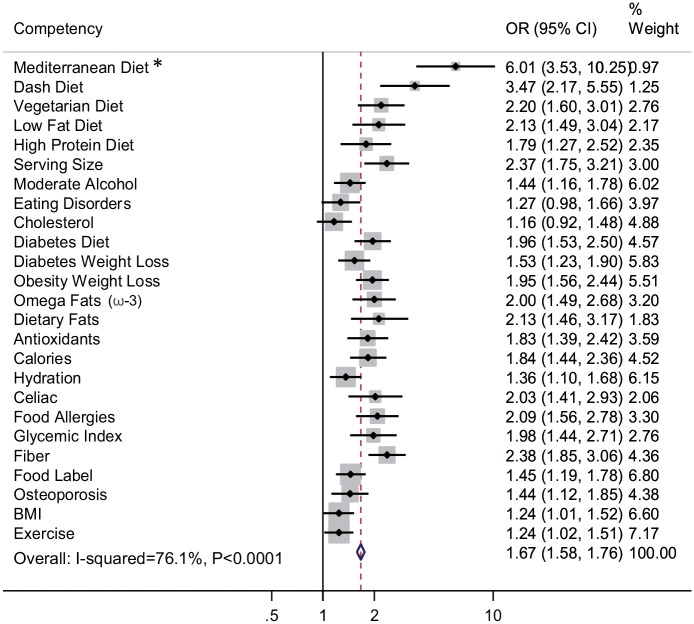 https://orcid.org/0000-0002-3213-0876
https://orcid.org/0000-0002-3213-0876
Dominique J. Monlezun 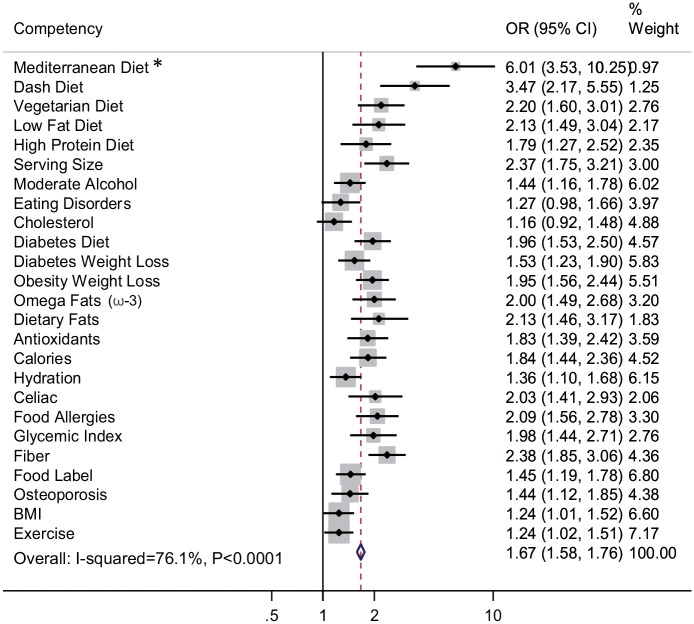 https://orcid.org/0000-0001-7671-1886
https://orcid.org/0000-0001-7671-1886
Zachary Stauber 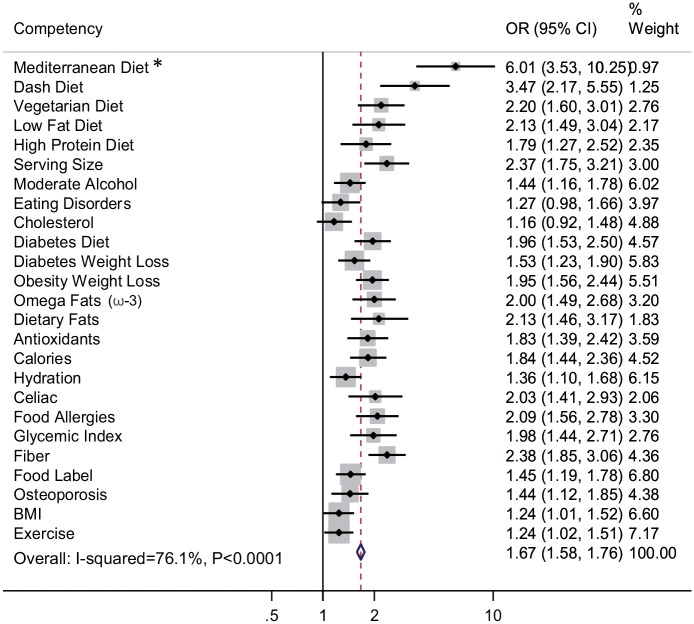 https://orcid.org/0000-0002-6628-120X
https://orcid.org/0000-0002-6628-120X
Supplemental Material: Supplemental material for this article is available online.
Contributor Information
Alexander C. Razavi, Goldring Center for Culinary Medicine, Tulane University School of Medicine, New Orleans, USA; Tulane University School of Public Health and Tropical Medicine, New Orleans, USA.
Dominique J. Monlezun, Goldring Center for Culinary Medicine, Tulane University School of Medicine, New Orleans, USA; Tulane University School of Public Health and Tropical Medicine, New Orleans, USA.
Alexander Sapin, Goldring Center for Culinary Medicine, Tulane University School of Medicine, New Orleans, USA; Tulane University School of Public Health and Tropical Medicine, New Orleans, USA.
Zachary Stauber, Goldring Center for Culinary Medicine, Tulane University School of Medicine, New Orleans, USA.
Kara Schradle, Goldring Center for Culinary Medicine, Tulane University School of Medicine, New Orleans, USA.
Emily Schlag, Goldring Center for Culinary Medicine, Tulane University School of Medicine, New Orleans, USA.
Amber Dyer, Goldring Center for Culinary Medicine, Tulane University School of Medicine, New Orleans, USA.
Brennan Gagen, Goldring Center for Culinary Medicine, Tulane University School of Medicine, New Orleans, USA.
Isabella G. McCormack, Goldring Center for Culinary Medicine, Tulane University School of Medicine, New Orleans, USA.
Ofure Akhiwu, Goldring Center for Culinary Medicine, Tulane University School of Medicine, New Orleans, USA.
Alexandria Ross, Philadelphia College of Osteopathic Medicine, Philadelphia, USA.
John Wesley McWhorter, University of Texas School of Public Health, Houston, USA.
Lisa Hamilton, Ohio State University College of Medicine, Columbus, USA.
Leah Sarris, Goldring Center for Culinary Medicine, Tulane University School of Medicine, New Orleans, USA.
Kerri Dotson, Goldring Center for Culinary Medicine, Tulane University School of Medicine, New Orleans, USA.
Timothy S. Harlan, Goldring Center for Culinary Medicine, Tulane University School of Medicine, New Orleans, USA.
References
- 1. US Burden of Disease Collaborators; Mokdad AH, Ballestros K, et al. The state of US health, 1990-2016: burden of diseases, injuries, and risk factors among US states. JAMA. 2018;319:1444-1472. doi: 10.1001/jama.2018.0158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224-2260. doi: 10.1016/S0140-6736(12)61766-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mozaffarian D. Dietary and policy priorities for cardiovascular disease, diabetes, and obesity: a comprehensive review. Circulation. 2016;133:187-225. doi: 10.1161/CIRCULATIONAHA.115.018585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wolk A, Manson JAE, Stampfer MJ, et al. Long-term intake of dietary fiber and decreased risk of coronary heart disease among women. JAMA. 1999;281:1998-2004. doi: 10.1001/jama.281.21.1998 [DOI] [PubMed] [Google Scholar]
- 5. Vanharanta M, Voutilainen S, Lakka TA, van der Lee M, Adlercreutz H, Salonen JT. Risk of acute coronary events according to serum concentrations of enterolactone: a prospective population-based case-control study. Lancet. 1999;354:2112-2115. doi: 10.1016/S0140-6736(99)05031-X [DOI] [PubMed] [Google Scholar]
- 6. Gan Y, Tong X, Li L, et al. Consumption of fruit and vegetable and risk of coronary heart disease: a meta-analysis of prospective cohort studies. Int J Cardiol. 2015;183:129-137. doi: 10.1016/j.ijcard.2015.01.077 [DOI] [PubMed] [Google Scholar]
- 7. Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937-952. doi: 10.1016/S0140-6736(04)17018-9 [DOI] [PubMed] [Google Scholar]
- 8. Rimm EB, Ascherio A, Giovannucci E, Spiegelman D, Stampfer MJ, Willett WC. Vegetable, fruit, and cereal fiber intake and risk of coronary heart disease among men. JAMA. 1996;275:447-451. doi: 10.1001/jama.275.6.447 [DOI] [PubMed] [Google Scholar]
- 9. American Heart Association. Cardiovascular Disease: A Costly Burden for America, Projections Through 2035. Dallas, TX: American Heart Association; 2017. [Google Scholar]
- 10. Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet. 2014;383:1899-1911. doi: 10.1016/S0140-6736(14)60685-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ovbiagele B, Goldstein LB, Higashida RT, et al. American Heart Association Advocacy Coordinating Committee and Stroke Council. Forecasting the future of stroke in the United States: a policy statement from the American Heart Association and American Stroke Association. Stroke. 2013;44:2361-2375. doi: 10.1161/STR.0b013e31829734f2 [DOI] [PubMed] [Google Scholar]
- 12. Smith AW, Borowski LA, Liu B, et al. US primary care physicians’ diet-, physical activity-, and weight-related care of adult patients. Am J Prev Med. 2011;41:33-42. doi: 10.1016/j.amepre.2011.03.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Eisenberg DM, Burgess JD. Nutrition education in an era of global obesity and diabetes: thinking outside the box. Acad Med. 2015;90:854-860. doi: 10.1097/ACM.0000000000000682 [DOI] [PubMed] [Google Scholar]
- 14. Frantz DJ, McClave SA, Hurt RT, Miller K, Martindale RG. Cross-sectional study of US interns’ perceptions of clinical nutrition education. JPEN J Parenter Enteral Nutr. 2016;40:529-535. doi: 10.1177/0148607115571016 [DOI] [PubMed] [Google Scholar]
- 15. Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003;348:2599-2608. doi: 10.1056/NEJMoa025039 [DOI] [PubMed] [Google Scholar]
- 16. Sofi F, Cesari F, Abbate R, Gensini GF, Casini A. Adherence to Mediterranean diet and health status: meta-analysis. BMJ. 2008;337:a1344. doi: 10.1136/bmj.a1344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Koloverou E, Esposito K, Giugliano D, Panagiotakos D. The effect of Mediterranean diet on the development of type 2 diabetes mellitus: a meta-analysis of 10 prospective studies and 136,846 participants. Metabolism. 2014;63:903-911. doi: 10.1016/j.metabol.2014.04.010 [DOI] [PubMed] [Google Scholar]
- 18. Estruch R, Ros E, Salas-Salvadó J, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368:1279-1290. doi: 10.1056/NEJMoa1200303 [DOI] [PubMed] [Google Scholar]
- 19. de Lorgeril M, Salen P. Mediterranean diet in secondary prevention of CHD. Public Health Nutr. 2011;14(12A):2333-2337. doi: 10.1017/S136898001100259X [DOI] [PubMed] [Google Scholar]
- 20. Panagiotakos DB, Pitsavos C, Polychronopoulos E, Chrysohoou C, Zampelas A, Trichopoulou A. Can a Mediterranean diet moderate the development and clinical progression of coronary heart disease? A systematic review. Med Sci Monit. 2004;10:RA193-RA198. [PubMed] [Google Scholar]
- 21. Widmer RJ, Flammer AJ, Lerman LO, Lerman A. The Mediterranean diet, its components, and cardiovascular disease. Am J Med. 2015;128:229-238. doi: 10.1016/j.amjmed.2014.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Monlezun DJ, Dart L, Vanbeber A, et al. Machine learning-augmented propensity score-adjusted multilevel mixed effects panel analysis of hands-on cooking and nutrition education versus traditional curriculum for medical students as preventive cardiology: multisite cohort study of 3,248 trainees over 5 years. Biomed Res Int. 2018;2018:5051289. doi: 10.1155/2018/5051289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Adams KM, Kohlmeier M, Zeisel SH. Nutrition education in US medical schools: latest update of a national survey. Acad Med. 2010;85:1537-1542. doi: 10.1097/ACM.0b013e3181eab71b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Meyers LS, Gamst G, Guarino AJ. Applied Multivariate Research: Design and Interpretation. 3rd ed. Thousand Oaks, CA: Sage; 2016. https://books.google.com/books?hl=en&lr=&id=ZN5mDQAAQBAJ&oi=fnd&pg=PP1&dq=Applied+Multivariate+Research:+Design+and+Interpretation.+&ots=_RzuYUdSGJ&sig=2z1ESkjhAKgoy72umfSY36JdXL4. Accessed July 31, 2019. [Google Scholar]
- 25. Conroy MB, Delichatsios HK, Hafler JP, Rigotti NA. Impact of a preventive medicine and nutrition curriculum for medical students. Am J Prev Med. 2004;27:77-80. doi: 10.1016/j.amepre.2004.03.009 [DOI] [PubMed] [Google Scholar]
- 26. Schlair S, Hanley K, Gillespie C, et al. How medical students’ behaviors and attitudes affect the impact of a brief curriculum on nutrition counseling. J Nutr Educ Behav. 2012;44:653-657. doi: 10.1016/j.jneb.2011.08.006 [DOI] [PubMed] [Google Scholar]
- 27. Bolarinwa O. Principles and methods of validity and reliability testing of questionnaires used in social and health science researches. Niger Postgrad Med J. 2015;22:195-201. doi: 10.4103/1117-1936.173959 [DOI] [PubMed] [Google Scholar]
- 28. Zaragoza-Martí A, Cabañero-Martínez MJ, Hurtado-Sánchez JA, Laguna-Pérez A, Ferrer-Cascales R. Evaluation of Mediterranean diet adherence scores: a systematic review. BMJ Open. 2018;8:e019033. doi: 10.1136/bmjopen-2017-019033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kurth T, Walker AM, Glynn RJ, et al. Results of multivariable logistic regression, propensity matching, propensity adjustment, and propensity-based weighting under conditions of nonuniform effect. Am J Epidemiol. 2006;163:262-270. doi: 10.1093/aje/kwj047 [DOI] [PubMed] [Google Scholar]
- 30. Wyss R, Ellis AR, Brookhart MA, et al. The role of prediction modeling in propensity score estimation: an evaluation of logistic regression, bCART, and the covariate-balancing propensity score. Am J Epidemiol. 2014;180:645-655. doi: 10.1093/aje/kwu181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lewis KO, Frank GR, Nagel R, et al. Pediatric trainees’ engagement in the online nutrition curriculum: preliminary results. BMC Med Educ. 2014;14:190. doi: 10.1186/1472-6920-14-190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Knoops KTB, de Groot LCPGM, Kromhout D, et al. Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: the HALE project. JAMA. 2004;292:1433-1439. doi: 10.1001/jama.292.12.1433 [DOI] [PubMed] [Google Scholar]
- 33. Moore SE, McEvoy CT, Prior L, et al. Barriers to adopting a Mediterranean diet in Northern European adults at high risk of developing cardiovascular disease. J Hum Nutr Diet. 2018;31:451-462. doi: 10.1111/jhn.12523 [DOI] [PubMed] [Google Scholar]
- 34. Van Horn L. The Nutrition Academic Award: brief history, overview, and legacy. Am J Clin Nutr. 2006;83:936S-940S. doi: 10.1093/ajcn/83.4.936S [DOI] [PubMed] [Google Scholar]
- 35. Frank E, Dresner Y, Shani M, Vinker S. The association between physicians’ and patients’ preventive health practices. CMAJ. 2013;185:649-653. doi: 10.1503/cmaj.121028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Oberg EB, Frank E. Physicians’ health practices strongly influence patient health practices. J R Coll Physicians Edinb. 2009;39:290-291. doi: 10.4997/JRCPE.2009.422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Schwingshackl L, Schwedhelm C, Galbete C, Hoffmann G. Adherence to Mediterranean diet and risk of cancer: an updated systematic review and meta-analysis. Nutrients. 2017;9:E1063. doi: 10.3390/nu9101063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Aune D, Keum N, Giovannucci E, et al. Whole grain consumption and risk of cardiovascular disease, cancer, and all cause and cause specific mortality: systematic review and dose-response meta-analysis of prospective studies. BMJ. 2016;353:i2716. doi: 10.1136/bmj.i2716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Caygill CPJ, Hill MJ. Fish, n-3 fatty acids and human colorectal and breast cancer mortality. Eur J Cancer Prev. 1995;4:329-332. doi: 10.1097/00008469-199508000-00008 [DOI] [PubMed] [Google Scholar]
- 40. Aune D, Keum NN, Giovannucci E, et al. Nut consumption and risk of cardiovascular disease, total cancer, all-cause and cause-specific mortality: a systematic review and dose-response meta-analysis of prospective studies. BMC Med. 2016;14:207. doi: 10.1186/s12916-016-0730-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Aune D, Giovannucci E, Boffetta P, et al. Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality—a systematic review and dose-response meta-analysis of prospective studies. Int J Epidemiol. 2017;46:1029-1056. doi: 10.1093/ije/dyw319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Jafar TH, Stark PC, Schmid CH, et al. Progression of chronic kidney disease: the role of blood pressure control, proteinuria, and angiotensin-converting enzyme inhibition. A patient-level meta-analysis. Ann Intern Med. 2003;139:244-252. doi: 10.7326/0003-4819-139-4-200308190-00006 [DOI] [PubMed] [Google Scholar]
- 43. Iturria-Medina Y, Sotero RC, Toussaint PJ, Mateos-Pérez JM, Evans AC. Alzheimer’s Disease Neuroimaging Initiative. Early role of vascular dysregulation on late-onset alzheimer’s disease based on multifactorial data-driven analysis. Nat Commun. 2016;7:11934. doi: 10.1038/ncomms11934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Khatri M, Moon YP, Scarmeas N, et al. The association between a Mediterranean-style diet and kidney function in the Northern Manhattan Study cohort. Clin J Am Soc Nephrol. 2014;9:1868-1875. doi: 10.2215/CJN.01080114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Berti V, Walters M, Sterling J, et al. Mediterranean diet and 3-year Alzheimer brain biomarker changes in middle-aged adults. Neurology. 2018;90:e1789-e1798. doi: 10.1212/WNL.0000000000005527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Mosconi L, Walters M, Sterling J, et al. Lifestyle and vascular risk effects on MRI-based biomarkers of Alzheimer’s disease: a cross-sectional study of middle-aged adults from the broader New York City area. BMJ Open. 2018;8:e019362. doi: 10.1136/bmjopen-2017-019362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Sacks FM, Svetkey LP, Vollmer WM, et al. DASH-Sodium Collaborative Research Group. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344:3-10. doi: 10.1056/NEJM200101043440101 [DOI] [PubMed] [Google Scholar]
- 48. Satija A, Hu FB. Plant-based diets and cardiovascular health. Trends Cardiovasc Med. 2018;28:437-441. doi: 10.1016/j.tcm.2018.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplementary_Tables for Multisite Culinary Medicine Curriculum Is Associated With Cardioprotective Dietary Patterns and Lifestyle Medicine Competencies Among Medical Trainees by Alexander C. Razavi, Dominique J. Monlezun, Alexander Sapin, Zachary Stauber, Kara Schradle, Emily Schlag, Amber Dyer, Brennan Gagen, Isabella G. McCormack, Ofure Akhiwu, Leah Sarris, Kerri Dotson and Timothy S. Harlan in American Journal of Lifestyle Medicine