Abstract
Objective
When 2017 Hurricane Harvey struck the coastline of Texas on August 25, 2017, it resulted in 88 fatalities and more than US $125 billion in damage to infrastructure. The floods associated with the storm created a toxic mix of chemicals, sewage and other biohazards, and over 6 million cubic meters of garbage in Houston alone. The level of biohazard exposure and injuries from trauma among persons residing in affected areas was widespread and likely contributed to increases in emergency department (ED) visits in Houston and cities receiving hurricane evacuees. We investigated medical surge resulting from these evacuations in Dallas–Fort Worth (DFW) metroplex EDs.
Methods
We used data sourced from the North Texas Syndromic Surveillance Region 2/3 in ESSENCE to investigate ED visit surge following the storm in DFW hospitals because this area received evacuees from the 60 counties with disaster declarations due to the storm. We used the interrupted time series (ITS) analysis to estimate the magnitude and duration of the ED surge. ITS was applied to all ED visits in DFW and visits made by patients residing in any of the 60 counties with disaster declarations due to the storm. The DFW metropolitan statistical area included 55 hospitals. Time series analyses examined data from March 1, 2017–January 6, 2018 with focus on the storm impact period, August 14–September 15, 2017. Data from before, during, and after the storm were visualized spatially and temporally to characterize magnitude, duration, and spatial variation of medical surge attributable to Hurricane Harvey.
Results
During the study period overall, ED visits in the DFW area rose immediately by about 11% (95% CI: 9%, 13%), amounting to ~16 500 excess total visits before returning to the baseline on September 21, 2017. Visits by patients identified as residing in disaster declaration counties to DFW hospitals rose immediately by 127% (95% CI: 125%, 129%), amounting to 654 excess visits by September 29, 2017, when visits returned to the baseline. A spatial analysis revealed that evacuated patients were strongly clustered (Moran’s I = 0.35, P< 0.0001) among 5 of the counties with disaster declarations in the 11-day window during the storm surge.
Conclusions
The observed increase in ED visits in DFW due to Hurricane Harvey and ensuing evacuation was significant. Anticipating medical surge following large-scale hurricanes is critical for community preparedness planning. Coordinated planning across stakeholders is necessary to safeguard the population and for a skillful response to medical surge needs. Plans that address hurricane response, in particular, should have contingencies for support beyond the expected disaster areas.
Keywords: hurricane, medical surge, spatial analysis, interrupted time series analysis
Natural and man-made disasters in the United States increased 60% in the past 2 decades.1 Weather-related disasters, including hurricanes, are among events with the capacity for widespread immediate destruction, long-term negative outcomes due to infrastructure damage, and creation of environmental hazards.1,2 Many of these disasters cause mass casualties requiring immediate medical attention, resulting in local hospital medical surges.1 However, community hospitals in storm impact and surrounding areas may not have the resources and staff to accommodate large-scale disasters affecting thousands of persons.3
Hurricane Harvey made landfall in Texas on August 25, 2017, resulting in 88 fatalities and more than US $180 billion in damages.4 In Houston, over 125 cm of rain caused massive flooding, covering nearly one-third of the city and disturbing more than 200 000 homes.4 The flooding exposed affected areas to a toxic mix of chemicals, sewage, biohazards, and over 6 million cubic meters of garbage.5 The level of biohazard exposure and injuries from trauma among persons residing in affected areas were widespread and contributed to increases in emergency department (ED) visits in Houston and cities that received people evacuating from the hurricane impact zone.6
To explore the geographic extent of the medical surge associated with Hurricane Harvey, we assessed ED visit surges in Dallas–Fort Worth (DFW) metroplex EDs before, during, and after the storm period (August 25–September 4, 2017). Specifically, we considered evacuees from 60 Texas counties with disaster declarations who sought care outside of the storm impact zone, many in DFW, approximately 260 miles away. We examined spatial and temporal variation in ED visits to DFW hospitals attributable to the storm. We used the interrupted time series (ITS) analysis to estimate the magnitude and duration of the ED surge and global indicators of spatial autocorrelation to examine spatial clustering. Medical surge capacity is a critical component of community preparedness, with coalition building among hospitals and other health care facilities as an important concern.1 The results have implications for public health emergency preparedness and hospital preparedness policy-makers.
METHODS
Data Sources and Measurement
Data were extracted from the Texas Health Services Region 2/3 syndromic surveillance data and associated ESSENCE analytics through the North Texas Syndromic Surveillance System during the period of March 1, 2017–January 06, 2018. The data captured for the North Texas area included all 109 contributing EDs – 55 in the DFW metroplex.7 These secondary data, collected through the aforementioned syndromic surveillance system, were analyzed for this study, with special focus on ED visit data from the patients who resided in the 60 counties with Federal Emergency Management Agency (FEMA) disasters declarations due to Hurricane Harvey.7 Surveillance data were de-identified and exempted from an institutional review board review.
We analyzed visit data of patients presenting at EDs in the DFW area, which may have received evacuees due to the storm. ITS analyses, previously applied by Wilt et al. and Ekperi et al. in 2018, examined the period March 1, 2017–January 6, 2018, defining the event that “interrupted” or perturbed the time series as August 25, 2017, the day that Hurricane Harvey made landfall in Texas.8,9 There were 177 days pre-event and 135 days post-event. Spatio-temporal analyses focused especially on the period surrounding Hurricane Harvey, August 14–September 15, 2017.
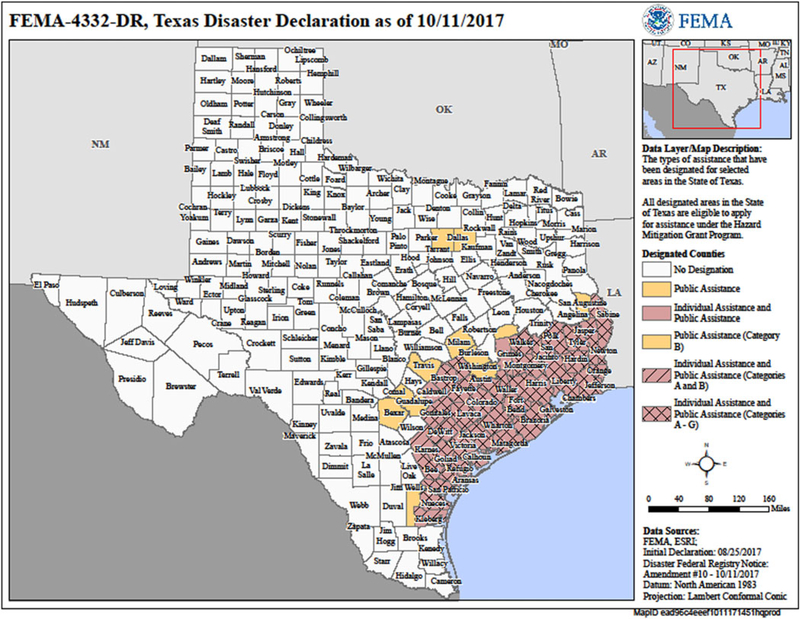
To identify Hurricane Harvey–attributable medical surge, we considered 3 types of visits with increasing specificity: all reported ED visits; evacuee visits, which were visits by patients who reported zip codes indicating residence in any of the 60 counties with disaster declarations due to Hurricane Harvey (evacuee); and Harvey chief complaints (CC) visits, visits where the chief complaint or triage notes mentioned “hurricane,” “Harvey,” “evacuee,” or “evacuate.” In the DFW area, daily counts for all ED visits and evacuee ED visits were examined. It was only possible to examine Harvey CC visit counts for dates after August 25, 2017, the day that Hurricane Harvey made landfall in Texas, because CC could not reference the event prior to that date. Figure 1 displays Texas counties with disaster declarations. Counties shaded in pink had disaster declarations.
FIGURE 1. Texas County-Level Disaster Declarations (n = 60) Due to Hurricane Harvey, 2017.
Note: Reprinted from FEMA website: https://gis.fema.gov/maps/dec_4332.pdf. Accessed January 2019.
Statistical Methods
Descriptive statistics of the mean, standard deviation, and range were calculated during 3 periods before (August 14–24, 2017), during (August 25–September 4, 2017), and after (September 5–15, 2017) the storm for all ED visits and evacuee ED visits. Statistical and time series analyses were conducted using SAS v9.3 (SAS Institute, Inc., Cary, NC). Spatial analyses were conducted using GeoDa 1.6.7 (Tempe, AZ) with visualization using ArcMap 10.5 (Redlands, CA).
ITS models of daily ED visit counts in DFW for all and evacuee ED visits were estimated via a maximum likelihood. These models were estimated for the period of March 1, 2017–January 6, 2018, the extended pre-event period allowing improved estimation of seasonal variation in the baseline. The ITS models were specified as linear segmented regressions with autoregressive errors to adjust for seasonal cyclical variation in ED visits.10 The resulting estimated parameters and standard errors were used to produce estimates and associated 95% confidence intervals of the event-attributable number and percentage change in visits at several time points post-event, the total, or cumulative, number of excess visits attributable to the event, including the date at which visits returned to normal or where predicted visits were not significantly different from the counterfactual trend, the predicted level in the absence of the event.11 We use the term surge to refer to the event-attributable number and percentage change in visits, which is also referred to as excess visits.
For a comparison of results obtained using ITS, the switching detection algorithm (Poisson/Regressions/EWMA*) was applied in ESSENCE12 to all and evacuee ED visit counts on August 4–September 23, 2017 to identify a statistically significant ED surge. A statistically significant medical surge was defined as the statistically significant difference between expected and observed daily visit counts. There were 50 days in each time series with 20 days pre-event (August 4, 2017–August 24, 2017) and 30 days post-event (August 25, 2017–September 23, 2017). However, ESSENCE includes a tuning period of 40 days prior to the start date of a time series to establish the baseline time series seasonal characteristics. We examined the magnitude, duration, and spatial variation of the identified statistically significant medical surge associated with Hurricane Harvey for all ED visits and for evacuee ED visits.
Data from evacuee visits to DFW hospitals during 3, 11-day periods before, during, and after the storm were analyzed for spatial autocorrelation (clustering) using global Moran’s I in GeoDa 1.6.7 (Tempe, AZ) and visualized using ArcMap 10.5 (Redlands, CA). The periods were broken up evenly (into 11-day increments) so that the change in space and volume would be more easily comparable: before the storm (August 14–24, 2017), during the storm (August 25–September 4, 2017), and after the storm (September 5–15, 2017). The maps provided visual information on where within the affected region (defined as counties with disaster declarations, n = 60) higher numbers of evacuated patients came from and which hospitals received the greatest spikes in visits. These maps characterize magnitude, duration, and geographic variation of medical surge associated with Hurricane Harvey. Evacuee visits were analyzed by CC, presenting ED, and patient characteristics.
RESULTS
As seen in Table 1, the means of all visits, evacuee visits, and Harvey CC visits rose during the event and after the event, compared with the time period before the event. The relative increase is most dramatic for evacuee visits during the event, when mean visits rose by over 260%, from 22 to 80 visits per day. All visits displayed a small relative increase during the event of 1.6%, from 7499 to 7615 visits per day, but that increase was magnified after the event to 7.4%, to 8056 per day. Harvey CC averaged 5 visits per day during and after the event, with the variability in visits declining in the after-event period. In addition to an increase in the mean number of visits, the standard deviation increased both during and after the event.
TABLE 1.
Descriptive Statistics for Daily Emergency Department Visits, Metropolitan Dallas—Fort Worth, TX, August 4, 2017–September 15, 2017
| Before Event* (August 14–24, 2017) |
During Event (August 25-September 4, 2017) |
After Event (September 5–15, 2017) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Mean | Std Dev | Minimum | Maximum | Mean | Std Dev | Minimum | Maximum | Mean | Std Dev | Minimum | Maximum |
| All Emergency Departments Visits in DFW** | 7,499 | 433 | 6,707 | 8,016 | 7,615 | 466 | 6,665 | 8,413 | 8,056 | 620 | 7,053 | 8,976 |
| Visits in DFW by persons residing in Counties with Emergency Declarations | 22 | 4 | 16 | 27 | 80 | 23 | 37 | 123 | 39 | 10 | 23 | 56 |
| Visits with chief complaint of Hurricane Harvey | 0 | 0 | 0 | 0 | 5 | 6 | 2 | 18 | 5 | 3 | 1 | 12 |
Event = August 25, 2017, the date that Hurricane Harvey made landfall in Texas.
DFW = Metropolitan Dallas-Fort Worth, Texas.
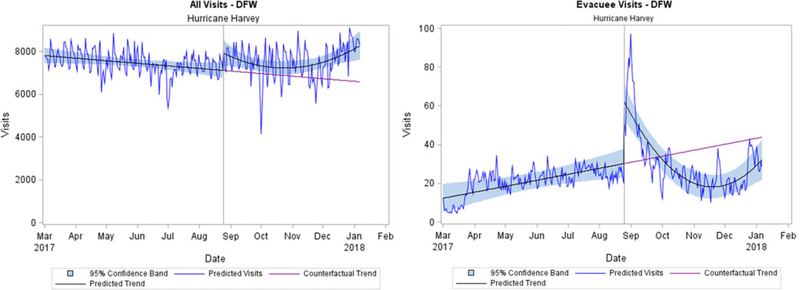
Table 2 and Figure 2 present results from the ITS analysis that estimated the magnitude and duration of the medical surge in 55 DFW metroplex EDs. The immediate effect of the event on all ED visits was an increase of 11.2% (95% CI: 8.7%, 12.7%), or 794 visits (95% CI: 587, 959), which was significant at P = 0.05. This immediate effect is represented in Figure 2 by the upward shift in the predicted trend of all visits at the Hurricane Harvey reference line. While the predicted trend does not ever cross the counterfactual trend, predicted visits fall below the counterfactual trend on September 21, 2017. At that point, 27 days after the event, estimated surge, or excess visits, attributable to Hurricane Harvey ended, amounting to 16 505 (95% CI: 14 379, 17 208) total visits, or ~611 excess visits per day. This estimated total impact was 6.7% (95% CI: 4.6%, 9.5%) more visits than would have occurred during that 27-day period if Hurricane Harvey had not made landfall in Texas.
TABLE 2.
Total and Percent Change * in Visits from Hurricane Harvey in Metropolitan Dallas—Fort Worth, TX on Daily Emergency Department Visits, March 1, 2017–January 6, 2018
| All Excess Visits |
Excess Evacuee Vists |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total Change From Baseline |
Percent Change from Baseline |
Total Change From Baseline |
Percent Change from Baseline |
|||||||||
| Time Post-Event** | Estimate | 95%CI |
Estimate | 95%CI |
Estimate | 95%CI |
Estimate | 95%CI |
||||
| Immediate Effect | 794 | 587 | 959 | 11.2 | 8.7 | 12.7 | 31.7 | 29.1 | 40.2 | 126.9 | 124.6 | 128.7 |
| Cumulative Effect at 1 week post event | 5,861 | 4,778 | 6,583 | 10.0 | 8.9 | 10.9 | 247.7 | 210.8 | 284.6 | 112.5 | 112.7 | 112.2 |
| Cumulative Effect at 2 week post event | 10,152 | 9,093 | 10,505 | 9.2 | 9.1 | 9.3 | 412.1 | 354.4 | 469.8 | 99.0 | 98.2 | 110.1 |
| Cumulative Effect at Return to Baseline*** | 16,505 | 14,379 | 17,208 | 8.0 | 6.8 | 9.3 | 653.5 | 571.5 | 742.3 | 15.0 | 29.3 | 33.1 |
Estimated using Interrupted Time Series analysis specified as segmented with autoregressive errors.
Event = August 25, 2017, the date that Hurricane Harvey made landfall in Texas.
All visits returned to baseline by 9/21/2017 and Evacuee visits returned to baseline by 9/29/2017.
FIGURE 2. Predicted Visits from Interrupted Time Series (ITS) Models of Daily Emergency Department Visits compared to counterfactual trend, Metropolitan Dallas–Fort Worth, TX, March 1 2017–January 6, 2018.
Note predicted visits are those predicted by the ITS model. Predicted trend is structural tred predicted by ITS model. Counterfactual trend assumes that no event occurs to interrupt the time series.
Reference line “Hurricane Harvey” is August 25, 2017, the date that Hurricane Harvey made landfall in Texas. Evacuee visits are visits by patients that reported zip codes indicating residence in any of the 60 counties with emergency declarations due to Hurricane Harvey.
95% confidence band represents the confidence interval around the predicted structural trend.
Considering only evacuee visits in 55 DFW metroplex EDs, an immediate effect of about 32 visits or 126.9% increase (95% CI: 124.6%, 128.7%) per day was observed on August 25, 2017. This effect is represented in Figure 2 by the gap between the predicted trend and the counterfactual trend at the Hurricane Harvey reference line (August 25, 2017). Note also that predicted visits continued to rise after August 25, peaking on August 31, 2017, at 66 (95% CI: 56, 96) visits or 214% (95% CI: 204%, 365%) above the baseline. The predicted trend crossed the counterfactual trend on September 29, 2017, more than 1 month after the hurricane, indicating the end of the hurricane-attributable surge in evacuee visits. At that point, evacuee visits in DFW due to Hurricane Harvey amounted to 654 (95% CI: 572, 742) or about 15% (95% CI: 29%, 33%), more than would have occurred during that 35-day period in the absence of the event.
For all ED visits, a statistically significant surge, based on the ESSENCE detection algorithm, was observed in CC categories of fever, gastrointestinal illness, rash, and respiratory illness. When considering evacuee visits only, a statistically significant surge was observed in CC categories of traffic-related injuries, fever, gastrointestinal illness, injury, neurologic complaints, rash, and respiratory illness.
Evacuee visits increased across all age groups. Although 40% of “evacuee visits” were from Harris County (Houston) residents, only about 4% of the overall surge were from counties with disaster declarations due to the storm. About 25% of evacuee visits had a CC of gastrointestinal issues with significant increases in nausea-vomiting-diarrhea (NVD), 22% respiratory, and 19% fever. Injury accounted for 14% of visits. The remaining 20% of complaints varied and were categorized as “other.” A majority of evacuees (86%) seeking treatment were discharged from the emergency room, whereas 9% of visits resulted in hospital admission. No deaths were reported among evacuee visits to the DFW hospitals during the period.
There were 259 Harvey CC visits from August 25, 2017–September 28, 2017. About 37% of these visits occurred in patients residing in counties with disaster declarations due to Hurricane Harvey, whereas 34% of visits were among DFW residents. These visits represented patients across all age groups, although 47% occurred in patients ages 18–44 years. Of the 259 visits, 37 (14%) resulted in inpatient admissions, whereas the remainder were treated in the ED and discharged. About 12% of visits were due to injuries, 7.3% for gastrointestinal complaints, 6.5% for respiratory illnesses, and 4% for fever or neurologic complaints. The remaining 69% were categorized as “other” and included requests for medication refills.
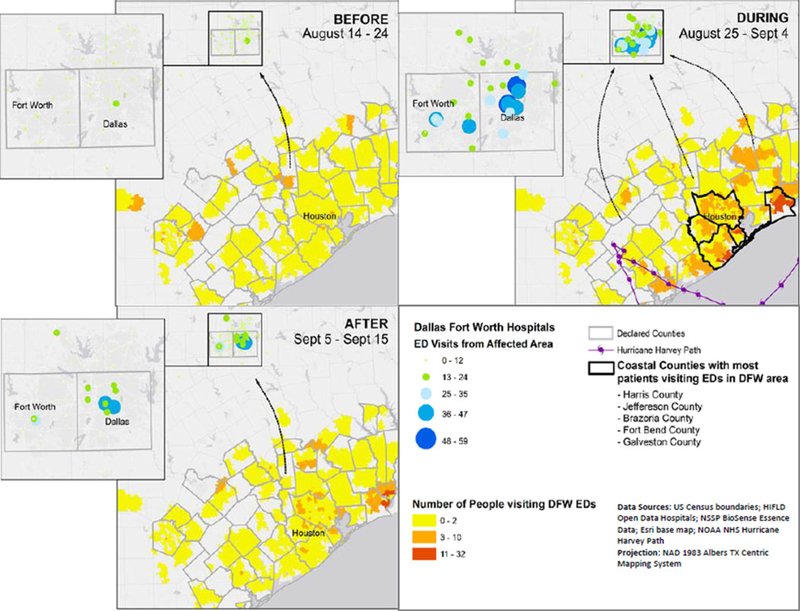
Figure 3 displays evacuee visits that presented at the ED in the DFW area. Results of the global Moran’s I analysis revealed mild to no clustering in the 11-day period before (August 14–24, 2017; Moran’s I = 0.04, P = 0.03) Hurricane Harvey hit and strong clustering in the 11-day period during (August 25–September 4, 2017; Moran’s I = 0.35, P < 0.0001) and after (September 5–15, 2017; Moran’s I = 0.29, P < 0.0001) the event. Further, Figure 3 illustrates that the highest clusters of “evacuee visits” in DFW hospitals from the August 25–September 4, 2017, period were from Harris, Galveston, Jefferson, Brazoria, and Fort Bend counties.
FIGURE 3. Spatial Analysis of Surge in Evacuees Presenting for Care at Emergency Departments in the Dallas-Fort Worth Area Before (August 14–24, 2017), During (August 25–September 4, 2017), and After (September 5–15, 2017) Hurricane Harvey.
The zip codes in declared counties are represented with a yellow-to-dark-orange scale, representing the number of emergency department visits in Dallas-Fort Worth hospitals from people with residential zip codes in emergency-declared counties. The green-to-blue graduated circles represent the number of emergency department visits in Dallas-Fort Worth hospitals from people who reside in Texas counties with disaster declarations.
Prior to the storm, there was a low number of visits in DFW among patients from the Houston area. There was a strong and significant increase in visits due to evacuees during the storm impact period. While most hospitals in the area experienced a significant surge in ED visits, at least 10 hospitals experienced a 600% increase (2 experienced > 1000% surge) in ED visits from patients seeking care in DFW from counties in the affected area. The number of evacuee patient visits in DFW decreased in the 11-day period post-storm; however, the ED visit rate was still elevated.
DISCUSSION
Although the DFW metroplex is approximately 260 miles from the major hurricane impact zone, which included Harris County (Houston) and surrounding counties, this study uncovered an ED medical surge possibly attributable to Hurricane Harvey, exceeding 16 500 visits in the 27 days following the storm. Notably, patients with zip codes from counties declaring storm emergencies accounted for only 4% of the estimated 16 500 visit total ED surge attributed to Hurricane Harvey in this study. Neither patient zip codes nor CCs were sufficiently sensitive for identifying storm-attributable ED surge and CCs were clearly the inferior method. We therefore recommend using all ED visits to estimate ED medical surge need due to hurricanes.
In addition, the spatial analysis revealed 5 counties bordering Harris County (Houston) that contributed significantly more patients than expected from those seeking care outside the storm-affected region. Thus, persons evacuating a disaster zone may seek medical care at hospitals far outside the disaster zone, in this case, 260 miles outside of the disaster zone. This study suggests that people able to evacuate may seek care in hospitals far outside disaster impact areas and outside their communities of origin. Some evacuees may also be residents from non-impacted communities who may have been in the disaster area but were able to return to their home communities for treatment due to lack of hospital access or capacity in the disaster zones. Alternatively, some patients who resided outside of the hurricane zone who would normally seek care in Houston for perceived improved medical care access may have opted to seek care in Dallas to avoid the hurricane and its aftermath. Thus, a multilayered ripple effect could result in medical surges in surrounding areas of impact zones as individuals make choices to seek optimal health care.
Strengths/Limitations
ITS analysis is a robust modeling technique, the strongest quasi-experimental method for evaluating longitudinal effects of an event.13 Our use of segmented regression with autoregressive errors provides a powerful method for estimating the impact of the event while adjusting for seasonality and secular events.14 ITS statistical methods address autocorrelation and seasonality, such as the day of the week and month of the year variation, via autoregressive errors. The main threat to validity using time series methods is the potential for confounding effects due to a co-occurring or secular event. Co-occurring events might confound the effect detected, especially in overall ED visits.
In order to better evaluate longitudinal and seasonality effects, we compared our results using ITS to those obtained with the switching detection algorithm (Poisson/Regressions/EWMA) in ESSENCE, which is designed to be conservative. This detection algorithm, which uses a 40-day tuning period, does not adjust for longer ranged seasonality not observed in the tuning period and may therefore adjust too quickly to perturbing events.12 The resulting estimates of event-attributable surge magnitude and duration may therefore be biased downward. However, while ITS surge estimates reflect the difference in predicted and counterfactual visit trends, the switching detection algorithm surge estimates reflect the difference between actual and expected visits. This will typically result in a larger surge estimate. The duration of the surge estimated by the switching detection algorithm will be shorter than that estimated by ITS because the algorithm adjusts much more quickly to perturbing events.
Co-occurring events, like Labor Day weekend (August 31–September 2, 2017) in the instance of Hurricane Harvey or a co-occurring infectious disease epidemic, might confound the effect detected, especially in overall ED visits. Other than the Labor Day holiday weekend, the authors were not aware of any event that occurred in the DFW metro area at or near the time of Hurricane Harvey that could have affected the number of ED visits observed. There was no indication that the population of DFW changed significantly during the study period. We did test the effect of the Labor Day holiday weekend by including it as a segment in the segmented regression for all visits. The parameter estimate for the holiday weekend was not significant (P = 0.39), whereas the parameter estimate for the event remained sufficiently significant at P = 0.09 to affect the overall model.
We were able to place residence at the zip code level only; thus, some spatial patterns that aggregated to a larger scale may be masked (see Figure 3). Additionally, this study does not explore the underlying reasons as to why 40% of the total evacuations came from Harris County while residents from 60 counties evacuated. Understanding the demographics and exploring the social vulnerability and preparedness planning factors that led to Harris Country having the most patient visits in DFW are crucial next steps. Accounting for other emergency medical services available to evacuees would also illustrate the impact on DFW hospitals compared to the overall health care system.
Public Health Implications
Community disaster preparedness efforts should be coordinated across geographical boundaries to account for population mobility during an event. Health care coalitions within driving distance from major disasters are encouraged to coordinate preparedness plans in advance of emergencies to best prepare for the need of a potential medical surge capacity. Health care services to evacuee groups are likely to extend past the boundaries of the initial emergency event. This study highlights the utility of syndromic surveillance data and spatial and temporal methods for conducting timely analyses and detecting medical surge ED visits associated with disasters of a similar nature. Future studies may consider the impact of social, demographic, environmental, and preparedness-related factors that might contribute to medical surges occurring in areas distant from a disaster zone, but accessible to populations in surrounding areas. Going forward and applying theories of behavioral economics to medical surge analyses, as well as in other public health preparedness science research, may serve to shed light on exploration of the decision processes that people and populations use when seeking care or shelter. Behavioral economics theories emphasize that individual decisions are not always based on rational choices.15 In the context of an emergency situation, many social and psychological variables may factor into decisions regarding where to seek care, and indeed whether or not to evacuate. Our analyses call for deeper probes to understand driving forces behind disaster event-driven medical surges.
Footnotes
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Disclaimer
The findings and conclusions in this study are those of the authors and do not necessarily represent the official position of the CDC.
EWMA = exponentially weighted moving average model.
Contributor Information
William Stephens, Tarrant County Public Health, Office of Public Health Informatics, Fort Worth, Texas.
Grete E. Wilt, CDC, Division of Toxicology and Human Health Sciences, Geospatial Research, Analysis, and Services Program, Atlanta, Georgia.
Erica Adams Lehnert, CDC, Division of Toxicology and Human Health Sciences, Geospatial Research, Analysis, and Services Program, Atlanta, Georgia.
NoelleAngelique M. Molinari, Centers for Disease Control and Prevention (CDC), Center for Preparedness and Response, Division of State and Local Readiness, Applied Science and Evaluation Branch, Atlanta, Georgia.
Tanya Telfair LeBlanc, Centers for Disease Control and Prevention (CDC), Center for Preparedness and Response, Division of State and Local Readiness, Applied Science and Evaluation Branch, Atlanta, Georgia.
REFERENCES
- 1.Vick DJ, Wilson AB, Fisher M, Roseamelia C. Assessment of community hospital disaster preparedness in New York. J Emerg Manage. 2018; 16(4):213–227. [DOI] [PubMed] [Google Scholar]
- 2.Krause E, Reeves R. Hurricanes hit the poor the hardest. Brookings Institute. Social Mobility Memos. Monday, September 17, 2017 www.brookings.edu/blog/social-mobility-memos/2017/09/18/hurricanes-hit-the-poor-the-hardest Accessed September 19, 2019.
- 3.Shartar SE, Moore BL, Wood LM. Developing a mass casualty surge capacity protocol for emergency medical services to use for patient distribution. South Med J 2017;110(12):792–795. [DOI] [PubMed] [Google Scholar]
- 4.Pines JM. Freestanding emergency department visits and disasters: the case of Hurricane Harvey. Am J Emerg Med. 2018;36:1513–1514. [DOI] [PubMed] [Google Scholar]
- 5.Friedrich MJ. Determining health effects of hazardous materials released during Hurricane Harvey. J Am Med Assoc. 2017;318(23):2283. [DOI] [PubMed] [Google Scholar]
- 6.Liu EL, Morshedi B, Miller BL, et al. Dallas Mega Shelter Medical Operations response to Hurricane Harvey. Report from the field. Disaster Med Public Health Prep 2019;13(1):90–93. [DOI] [PubMed] [Google Scholar]
- 7.Texas Department of State Health Services. Texas Syndromic Surveillance (TxS2). 2018. https://dshs.texas.gov/txs2/ Accessed January 2019. [Google Scholar]
- 8.Wilt G, Adams E, Thomas E, et al. A space time analysis evaluating the impact of Hurricane Sandy on HIV testing rates. Int J Disaster Risk Reduct. 2018;28:839–844. [Google Scholar]
- 9.Ekperi L, Thomas E, LeBlanc TT, et al. The impact of Hurricane Sandy on HIV testing rates: an interrupted time series analysis, January 1, 2011 to December 31, 2013. PLoS Curr Disasters. 2018. doi: 10.1371/currents.dis.ea09f9573dc292951b7eb0cf9f395003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jandoc R, Burden AM, Mamdani M, et al. Interrupted time series analysis in drug utilization research is increasing: systematic review and recommendations. J Clin Epidemiol 2015;68:950–956. [DOI] [PubMed] [Google Scholar]
- 11.Molinari N, LeBlanc T, Stephens W. The impact of a case of Ebola virus disease on emergency department visits in Metropolitan Dallas-Fort Worth, TX, July 2013-July 2015: an interrupted time series analysis. PLoS Curr Outbreaks. 2018. doi: 10.1371/currents.outbreaks.e62bdea371ef5454d56f71fe217aead0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burkom HS, Elbert Y, Magruder SF, et al. Developments in the roles, features, and evaluation of alerting algorithms for disease outbreak monitoring. Johns Hopkins APL Tech Dig. 2008;27:313. [Google Scholar]
- 13.Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27:299–309. [DOI] [PubMed] [Google Scholar]
- 14.Zhang F, Wagner AK, Soumerai SB, Ross-Degnan D. Methods for estimating confidence intervals in interrupted time series analyses of health interventions. J Clin Epidemiol. 2009;62:143–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bickel WK, Moody L, Higgins ST. Some current dimensions of the behavioral economics of health-related behavior change. Prev Med. 2016; 92(2016):16–23. [DOI] [PMC free article] [PubMed] [Google Scholar]