Short abstract
Introduction
In 2017, 1.5 million people were diagnosed with stroke, 9 million were living with stroke and 0.4 million died because of stroke in 32 European countries. We estimate the economic burden of stroke across these countries in 2017.
Patients and methods
In a population-based cost analysis, we evaluated the cost of stroke. We estimated overall health and social care costs from expenditure on care in the primary, outpatient, emergency, inpatient and nursing/residential care settings, and pharmaceuticals. Additionally, we estimated the costs of unpaid care provided by relatives or friends of patients, lost earnings due to premature death and costs associated with individuals who temporarily or permanently left employment because of illness.
Results
In 2017 stroke cost the 32 European countries under analysis €60 billion, with health care accounting for €27 billion (45%), representing 1.7% of health expenditure. Adding the costs of social care (€5 billion), annual stroke-related care costs were equivalent to €59 per citizen, varying from €11 in Bulgaria to €140 in Finland. Productivity losses cost €12 billion, equally split between early death and lost working days. A total of €1.3 billion hours of informal care were provided to stroke survivors, costing Europe €16 billion.
Conclusion
Our study provides a snapshot of the economic consequences posed by stroke to 32 European countries in 2017. It also strengthens and updates the evidence we have gathered over the last 15 years, indicating that the costs of stroke are rising, partly due to an ageing population.
Keywords: Cost of illness, health care, informal care, productivity losses, stroke
Introduction
In 2017, stroke accounted for 438,000 deaths across Europe (EU-28, Iceland, Israel, Norway and Switzerland), representing 8% of total deaths.1,2 In addition, for many survivors, stroke exerts a negative effect on their lives by affecting many functions, hampering, therefore, the ability of survivors to perform usual activities.3,4 As a result, stroke is one of the leading causes of disability,5 and of elevated use of health- and social-care resources,6 with 8% of the €798 billion cost of brain disorders being attributable to stroke.7
In 2015, we estimated the overall cost of stroke for the European Union (EU) to be €45 billion.8 However, the 2015 study did not include the costs of institutionalisation, which may have biased the estimated costs of stroke downwards, as evidence has shown that stroke is a major predictor of subsequent institutionalisation.9
Costing studies such as these enable comparisons between the burden of different diseases and across years. In the past, using the same methodology, we estimated, in addition to the costs of stroke, the costs for overall cardiovascular disease, coronary heart disease (CHD), dementia, overall and specific cancers, and blood disorders.10–13 Comparisons of costs across disease areas can then be used to aid decision makers to prioritise scarce research funds to areas with the highest burden.14
Therefore, the study objective is to provide an estimate of the overall economic costs of stroke for all 28 countries of the EU, Iceland, Israel, Norway and Switzerland, by including direct health and social care costs, informal care costs and productivity losses.
Methods
Analysis framework and data sources
We conducted a population-based cost analysis to evaluate the costs of stroke, defined by the WHO International Classification of Diseases, 10th revision, codes I60–69. We adopted the same methodological framework for each of the 32 European countries under study, and that used in other cost-of-illness studies evaluating cardiovascular disease,10 cancer,12 blood disorders15,16 and dementia.11
We adopted a societal perspective in our analysis, including health and social care costs, informal care costs and productivity losses. We used an annual timeframe, including all costs for 2017 or from the most recent year if 2017 data were not available, irrespective of the time of disease onset. We obtained country-specific aggregate data from international and national sources, including WHO, the Organisation for Economic Co-operation and Development (OECD), the Statistical Office of the European Communities (EUROSTAT), national ministries of health and statistical institutes (Online Appendix page 15). Country-specific data on the number of incident and prevalent stroke cases were obtained from the Global Burden of Disease (GBD) study (http://ghdx.healthdata.org/gbd-results-tool).5 These data were supplemented with individual patient-level data from the Survey of Health, Ageing and Retirement in Europe (SHARE).17
SHARE is a multidisciplinary cross-national panel database of data on health, socio-economic status and social and family networks of older people. Data are collected via face-to-face, computer-aided, personal interviews, supplemented by self-completion paper and pencil questionnaires. We used data collected in Wave 2, Wave 4 and Wave 6 which included over 30,000 respondents resident in 21 European countries (Austria, Belgium, Croatia, the Czech Republic, Denmark, Estonia, France, Germany, Greece, Hungary, Ireland, Italy, Israel, Luxembourg, the Netherlands, Poland, Portugal, Slovenia, Spain, Sweden and Switzerland). Residents from Ireland and Hungary were only included in Waves 2 and 4 respectively, and the data collected in these two waves were combined with Wave 6 data on the remaining 19 countries.
For countries not in SHARE, we combined data from similar countries that were in SHARE to obtain estimates for the 11 remaining countries, using the same methodology as applied in earlier studies.12–15 Therefore, for Bulgaria, Latvia, Lithuania, Romania and Slovakia, we used combined data from the Czech Republic, Estonia, Hungary, Poland and Slovenia. For Iceland, Finland and Norway, we used combined data from Denmark and Sweden. For Cyprus and Malta, we used combined data from Greece, Italy, Israel, Portugal and Spain. Finally, for the UK we used combined data from Austria, Belgium, France, Germany, Ireland, Luxembourg and the Netherlands.
All costs were expressed in 2017 prices and converted to Euros where applicable.1 To account for price differentials across countries, we employed the purchasing power parity (PPP) method.1 A brief overview of the methods used is provided below (see Online Appendix A for more detailed information).
Healthcare costs
The categories of stroke healthcare services included were primary, accident and emergency (A&E), outpatient and hospital inpatient care, as well as medications. To account for private expenditure in countries where only public expenditures were available, estimates were inflated using the proportion of total healthcare spending accounted for by private expenditure.1
Primary care consisted of visits to/from general practitioners (GPs) and practice nurses. Outpatient care consisted of specialist consultations and diagnostic investigations taking place in outpatient wards, clinics or patients’ homes. A&E care consisted of all stroke-related hospital emergency visits. We obtained information on the total number of contacts with each type of service, and then the proportion of these that were attributable to stroke using data from SHARE.17 Inpatient care costs consisted of stroke-related days in hospital, including day cases and inpatient treatments, where the primary diagnosis was stroke.1,18 Costs were calculated by applying country-specific unit costs to the total number of stroke-related contacts/hospital days.
Medication expenditure consisted of total retail and hospital sales on cardiovascular system medications (ATC code C) used for stroke. ATC-C medication expenditure was obtained predominantly from the OECD.18 For non-OECD countries, expenditure information was obtained from a number of country-specific sources (Online Appendix page 5). Only France, Germany and the Netherlands provided information on the proportion of stroke-related medicine expenditure. Hence, the average proportion across the three countries (4.64%) was applied to the total ATC-C expenditure in the remaining countries.
Social care costs
Given the availability of data across the 32 countries under study, the only social care costs included in the study were those related to nursing and residential care home institutionalisation.
For each country, we obtained data on the number of people aged 65 years or over living in a nursing or residential home care. Using individual-patient level data from SHARE, we estimated the country-specific probability of a respondent being institutionalised due to stroke. We adjusted for age, presence of dementia and/or other health conditions and country of residence (Online Appendix page 6).
Informal care costs
Informal care costs were defined as the opportunity cost of unpaid care, i.e. the working or leisure time, valued in monetary terms, that carers forgo to provide unpaid care for relatives/friends with stroke. Conservatively, we assumed that only those stroke patients severely limited in daily activities, or terminally ill, would receive informal care.
Hours of informal care for severely limited stroke patients were estimated by adding the age and sex-specific products of:
Prevalence of stroke in the population;19
Probability of a stroke patient being severely limited in daily activities;17
Probability of stroke patient receiving informal care;17 and the
Hours of informal care received.17
Hours of informal care for terminally ill stroke patients were estimated by adding the age and sex-specific products of:
Probability of receiving informal care in the year before dying from stroke;17 and the
Hours of informal care received.17
The total hours of informal care provided to stroke patients by carers of working age and employed were then valued using the average hourly wage rate.1,21 For those carers in retirement or not working, hourly minimum wages (or average wage in worst paid economic sector) were applied.1
Productivity costs due to mortality
Mortality costs were estimated as the lost earnings from premature death. These were estimated by using the age- and gender-specific number of stroke deaths to predict the working years lost at the time of death,1,20 adjusted for the age and gender-specific probability of being employed.1,22 Mortality costs were calculated using the product of the average annual earnings of male and female workers and the adjusted working years lost.1,21 As these costs would have been incurred in future years, all future lost earnings were discounted to present values using a 3.5% annual rate.
Productivity costs due to morbidity
Morbidity costs comprised costs associated with individuals taking sickness leave for a defined period of time (temporary absence), or due to individuals being declared incapacitated/disabled due to stroke (permanent absence).
Temporary absence from work due to stroke was evaluated by obtaining country-specific overall annual days of sickness leave due to all conditions and then applying the proportion of sickness leave that was attributable to stroke. For permanent absence from work due to stroke-related incapacity/disability, country-specific information on the numbers of working-age individuals receiving incapacity or disability benefits and not being able to work due to all conditions was obtained, to which we applied the proportion that was attributable to stroke.
The total number of working days lost due to stroke were then multiplied by average daily earnings.1,23 However, as absent workers are likely to be replaced after some time, we used the ‘friction period’ approach, where costs are only counted during the time it takes to replace a worker, and estimated that after 90 days an employee absent from work would be replaced.24 Therefore, for all new permanent cases of disability/incapacity, or when the average spell of temporary sickness leave was more than 90 days, only the first 90 days of work absence were valued.
Statistical analysis
To explore variations in stroke-related health and social care expenditure between countries, we undertook a series of ordinary least squares (OLS) univariate regression analyses using national income, overall healthcare expenditure, stroke incidence (crude), stroke mortality (crude), case fatality (mortality over incidence) and stroke-specific Disability-Adjusted Life-Years (DALYs) as explanatory variables. Diagnostic tests were performed for omitted variables (RESET test and link test) and heteroskedasticity (Breusch–Pagan test). An explanatory variable was considered significant if its p value was lower than 0.05. All regression analyses were performed using StataMP version 15.0.
We also performed a sensitivity analysis to measure the potential effect that changes in different categories of resource use may have in terms of total costs of stroke. The aim was to identify which categories were most sensitive. Therefore, we examined the effects of a 20% increase or decrease in health and social care costs and earnings. We also assessed the effect of discounting productivity costs using rates of 0% and 5%, and of using the human capital approach, instead of the friction-period method, to estimate morbidity losses.
Results
Total stroke costs
In 2017, in the 32 European countries under study there were 9 million people living with stroke (Online Appendix Table A.7). The total economic cost of stroke was €60 billion in 2017 (Table 1). For the 28 countries in the EU, this cost was €57 billion. The four most populous countries – Germany, France, Italy and the UK – accounted for 63% (€38 billion) of all costs.
Table 1.
Costs of stroke (€million) in Europe, by country, 2017.
|
Health care costs |
Social care |
Productivity costs |
Informal care costs |
TOTAL costs |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Primary care | Outpatient care | Emergency care | Hospital care | Medications | Total healthcare | % of total healthcare expenditure | Mortality losses | Morbidity losses | Total | % GDP | |||
| Austria | 155 | 127 | 30 | 504 | 29 | 845 | 2.29% | 106 | 94 | 180 | 383 | 1608 | 0.44% |
| Belgium | 39 | 38 | 7 | 411 | 31 | 524 | 1.24% | 328 | 118 | 159 | 354 | 1484 | 0.34% |
| Bulgaria | 11 | 12 | 2 | 31 | 15 | 70 | 1.77% | 8 | 87 | 6 | 106 | 278 | 0.54% |
| Croatia | 10 | 6 | 8 | 22 | 5 | 50 | 1.50% | 2 | 31 | 26 | 101 | 211 | 0.43% |
| Cyprus | 1 | 6 | 2 | 1 | 1 | 11 | 0.90% | 2 | 5 | 6 | 13 | 37 | 0.19% |
| Czech Rep. | 25 | 64 | 3 | 280 | 18 | 390 | 3.09% | 24 | 79 | 32 | 206 | 730 | 0.38% |
| Denmark | 20 | 19 | 6 | 114 | 7 | 166 | 0.58% | 155 | 124 | 83 | 148 | 677 | 0.23% |
| Estonia | 9 | 15 | 2 | 33 | 1 | 61 | 4.34% | 3 | 14 | 24 | 35 | 137 | 0.58% |
| Finland | 19 | 161 | 29 | 421 | 10 | 640 | 3.12% | 133 | 83 | 163 | 92 | 1111 | 0.50% |
| France | 292 | 401 | 87 | 1165 | 199 | 2143 | 0.83% | 630 | 519 | 1271 | 1260 | 5823 | 0.25% |
| Germany | 1155 | 1359 | 24 | 6408 | 143 | 9089 | 2.60% | 866 | 1483 | 1191 | 4971 | 17,600 | 0.54% |
| Greece | 6 | 11 | 17 | 209 | 41 | 284 | 1.93% | 36 | 82 | 89 | 160 | 650 | 0.36% |
| Hungary | 20 | 37 | 6 | 196 | 28 | 286 | 3.42% | 13 | 87 | 12 | 168 | 567 | 0.46% |
| Ireland | 27 | 26 | 23 | 83 | 14 | 172 | 0.84% | 17 | 67 | 111 | 83 | 451 | 0.15% |
| Italy | 250 | 418 | 188 | 2160 | 115 | 3131 | 2.08% | 375 | 543 | 501 | 2355 | 6905 | 0.40% |
| Latvia | 4 | 8 | 1 | 13 | 3 | 30 | 1.90% | 3 | 36 | 16 | 59 | 144 | 0.53% |
| Lithuania | 13 | 14 | 1 | 32 | 2 | 62 | 2.39% | 5 | 47 | 29 | 59 | 203 | 0.48% |
| Luxembourg | 2 | 5 | 0 | 21 | 2 | 29 | 0.90% | 19 | 6 | 4 | 17 | 75 | 0.14% |
| Malta | 1 | 1 | 0 | 7 | 1 | 10 | 1.15% | 2 | 3 | 5 | 8 | 29 | 0.26% |
| Netherlands | 83 | 217 | 12 | 450 | 169 | 932 | 1.28% | 210 | 247 | 117 | 484 | 1991 | 0.27% |
| Poland | 45 | 261 | 9 | 253 | 67 | 636 | 2.29% | 89 | 331 | 35 | 421 | 1512 | 0.33% |
| Portugal | 37 | 60 | 44 | 91 | 24 | 257 | 1.53% | 15 | 133 | 74 | 304 | 783 | 0.40% |
| Romania | 19 | 61 | 4 | 88 | 26 | 198 | 2.33% | 33 | 234 | 17 | 333 | 815 | 0.43% |
| Slovakia | 32 | 78 | 3 | 55 | 8 | 177 | 3.07% | 11 | 54 | 22 | 83 | 347 | 0.41% |
| Slovenia | 10 | 8 | 2 | 25 | 4 | 48 | 1.41% | 9 | 15 | 12 | 45 | 129 | 0.30% |
| Spain | 427 | 336 | 178 | 569 | 175 | 1685 | 1.68% | 133 | 274 | 357 | 1109 | 3557 | 0.30% |
| Sweden | 121 | 289 | 55 | 311 | 12 | 788 | 1.55% | 231 | 122 | 122 | 193 | 1455 | 0.31% |
| Total EU-27 | 2832 | 4038 | 743 | 13,955 | 1146 | 22,715 | 1.72% | 3,459 | 4920 | 4665 | 13,549 | 49,308 | 0.36% |
| UK | 399 | 516 | 123 | 1636 | 101 | 2775 | 1.19% | 767 | 1044 | 1046 | 1838 | 7470 | 0.32% |
| Total EU-28 | 3231 | 4554 | 866 | 15,590 | 1247 | 25,489 | 1.64% | 4,226 | 5964 | 5711 | 15,387 | 56,778 | 0.36% |
| Iceland | 8 | 6 | 1 | 11 | 1 | 27 | 1.76% | 6 | 7 | 5 | 4 | 48 | 0.23% |
| Israel | 20 | 49 | 36 | 84 | 12 | 201 | 0.86% | 22 | 57 | 195 | 123 | 597 | 0.19% |
| Norway | 43 | 46 | 8 | 211 | 8 | 316 | 0.90% | 186 | 68 | 277 | 78 | 926 | 0.26% |
| Switzerland | 23 | 13 | 8 | 482 | 33 | 558 | 0.75% | 307 | 139 | 81 | 170 | 1256 | 0.21% |
| Total Europe | 3324 | 4669 | 919 | 16,378 | 1301 | 26,592 | 1.65% | 4748 | 6235 | 6269 | 15,762 | 59,605 | 0.36% |
Results of the sensitivity analysis showed that using a human capital cost approach to value morbidity losses had the biggest impact on total stroke costs (9% change). A 20% variation in healthcare resource use had the second biggest impact on total stroke costs (5% change), with the resulting total costs varying between €56 billion and €63 billion (Online Appendix Figure A.1).
Healthcare costs
The healthcare cost of stroke for the 32 healthcare systems was €27 billion (Table 1), accounting for 1.65% of total healthcare expenditure. For EU healthcare systems, the cost was €25 billion representing 1.64% of EU healthcare expenditure. Out of the €27 billion healthcare costs due to stroke, €16 billion (62%) were due to inpatient hospital care, followed by outpatient care (€4.7 billion, 18%), primary care (€3.3 billion, 13%), pharmaceuticals (€1.3 billion – 5%) and emergency care (€919 million, 3%). Unit cost and resource use are reported in Online Appendix Tables A.5, A.8 and A.9.
Social care costs
Across Europe there were approximately 43 million days spent in nursing/residential care home due to stroke in 2017. This resulted in a total cost for European social care systems of €4.7 billion (Table 1).
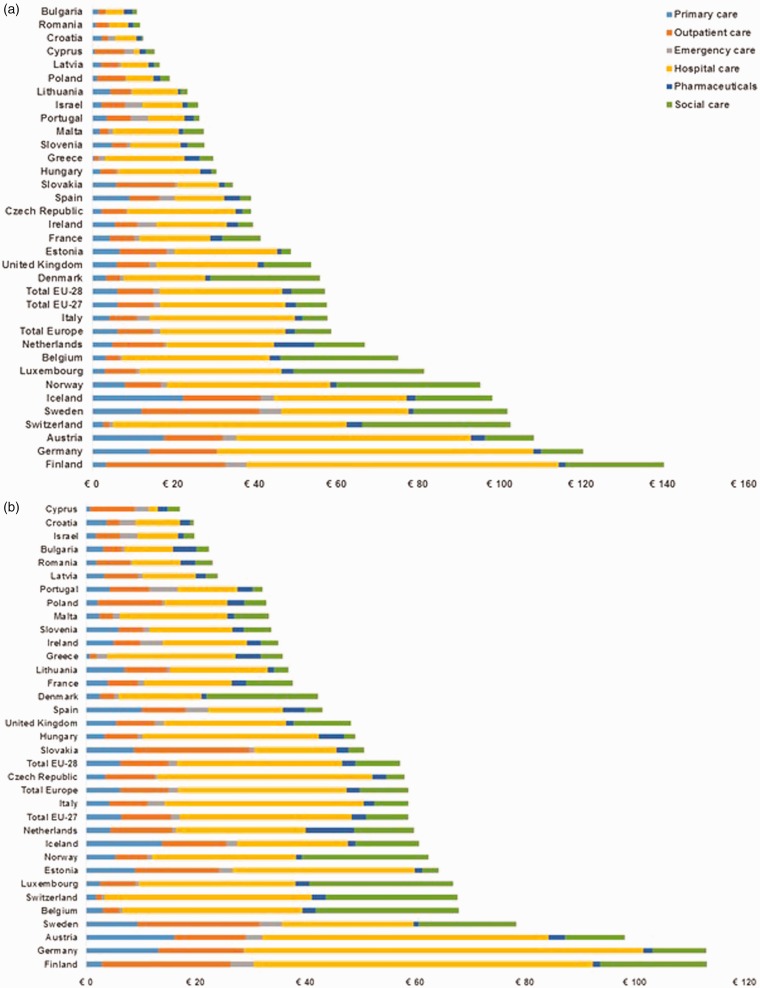
Health and social care expenditure
Overall, stroke-related direct health and social care expenditure across the 32 European countries was €31 billion, of which €27 billion was due to healthcare spending (85%). In the EU-28, this total was €30 billion (Table 1). When divided by every European citizen, the stroke-related cost of health and social care was €59 per person for all the 32 countries. Per capita levels of health and social care expenditure varied widely by countries, from €11 in Bulgaria to €140 in Finland. After adjusting for price differentials using PPI, country differences become less pronounced (Figure 1).
Figure 1.
Health and social care costs of stroke per person across Europe in 2017, by care service category. (a) Not adjusted for price differentials and (b) adjusted for price differentials.
We also evaluated the health and social care costs per prevalent stroke. When divided by all people with stroke, the stroke-related cost of health and social care was €3,483 per person with stroke in all the 32 European countries (Online Appendix Figure A2).
The OLS results showed a positive significant relationship between stroke-related health and social care costs and overall healthcare expenditure (p < 0.001), with each additional €1,000 of overall health expenditure per capita increasing stroke-related care costs by €13.5 (Online Appendix Figure A3).
Non-health and social care stroke costs
Of the nearly 9 million people in the 32 countries under study with stroke, 1.2 million were severely hampered in their activities of daily living. These 1.2 million stroke survivors received a total of 1.3 billion hours of care from friends or family (Online Appendix Figure A4). Informal care provided across Europe was valued at €16 billion in 2017 (Table 1). Stroke also accounted for 438,000 deaths in the 32 countries under study, representing 286,000 potential years of work lost, which were estimated at €6.2 billion after adjusting for employment rates and discounted to present values. Stroke-related morbidity accounted for approximately 38 million working days lost, which, when adjusted using the friction period approach, accounted for €6.3 billion.
Discussion
We estimated the total cost of stroke across 32 European countries to be €60 billion a year in 2017, of which €27 billion (45%) were incurred by healthcare systems, representing 1.65% of these countries healthcare systems’ budgets. In addition, a further €5 billion (8%) were incurred by social care systems, representing an annual stroke care spend of €59 per capita in the Europe. However, 47% (€29 billion) of the economic burden of stroke was in non-health or social care areas, with an estimated €16 billion (27%) in informal care costs and €13 in lost productivity due to early death or absence from work.
In the USA, the cost of stroke to the healthcare system was estimated at $28 billion for the year 2014/15 (the last year for which such estimates are available).25 After adjustment,1 the stroke-related costs to the US healthcare system were €20 billion, which was smaller than the €27 billion estimated for the 32 European countries in our study. However, on a per capita basis, healthcare related spend on stroke was higher in the USA (€84) than in Europe (€59). Stroke-related healthcare costs per person living with stroke, 7 million people with stroke in the USA and 9 million in Europe,25 were similar in the USA and Europe (€3,857 vs. €3,483).
The results from our regression analyses indicate that per capita stroke-related health and social care costs were significantly associated, with increases in a nation’s wealth resulting in increased stroke-related costs. However, we found that even for countries with the same levels of national income, health and social care expenditure on stroke varied widely. For example, despite per capita gross domestic product (GDP) in Germany (€39,600) and Belgium (€38,700) being similar in 2017,1 Germany’s expenditure on stroke-specific health and social care was nearly twice that for Belgium on a per capita basis (€113 vs. €68, respectively, adjusted for price differentials). We also observed a clear and significant linear trend between increases in overall health care expenditure and stroke-related health and social care expenditure, with each additional €10,000 of overall health expenditure per capita increasing stroke-related care costs by €135.
We have estimated the costs of stroke for the EU over the last 15 years in some of our previous work. In 2003, we estimated the total care costs of stroke to be €34 billion for the 25 countries forming the EU at that time (i.e. excluding Bulgaria, Croatia and Romania).10 For these same countries, costs rose to €38 billion in 2009,26 and to a further €45 billion in 2015.8 In our current analysis, we found that for these 25 EU countries total costs of stroke were estimated at €55 billion for 2017. By using the same approach to estimate the cost of stroke over time, it is possible to reliably compare the economic burden of stroke over time. This comparative evidence is useful to decision makers and health policy planners, as it helps informing evaluations of the impact of public health interventions to, for example, decrease the prevalence of stroke risk factors. A previous analysis in 30 European countries (i.e. Iceland, Norway, Switzerland and the EU excluding Croatia) found that the costs of brain disorders was €798 billion in 2010, of which stroke accounted for €64 billion (8%).5 Given that health care and wage rates since 2010 have increased minimally,1 and considering the nature of these studies, the results between our study and that by Oleson and colleagues are relatively similar.
However, this is the first analysis we have conducted to include the costs associated with long-term institutionalisation in a nursing/residential care home due to stroke. We have also fully utilised the information contained in the SHARE database, to capture the proportion of primary, outpatient and emergency care due to stroke. In our previous analyses, this information relied on the assumption that the proportion of visits to primary, outpatient or emergency care would be the same as the proportion of hospital discharges due to stroke.
The accuracy of our study depends on the quality and availability of comparable stroke-related data across countries. Given that our study included 32 countries, for each of which eight major categories of cost were examined, requiring the identification of unit costs in each country to value each resource use type, over 200 sources were consulted and utilised to conduct our comprehensive analyses. Our study encountered deficiencies in available information on some resource use and unit costs, which required us to rely on some assumptions. In addition, some of the differences in per capita costs might have resulted, to an extent, from variation in the methodology used to derive resource use or unit costs. As previously mentioned, the vast majority of countries report no data on the number of primary, outpatient and emergency care visits due to stroke. As a result, we had to make use of SHARE. For countries not in SHARE, we had to combine data from similar countries that were in SHARE.
Through SHARE we were able to obtain information stroke-related resource use information on primary, outpatient, emergency, social and informal care. However, SHARE is not a population based cohort study, in which stroke cases are ascertained through multiple overlapping methods so as to identify all stroke cases both in institutions and in the community. Rather, it is a survey, in which participants may choose not to participate or may not be deemed eligible for inclusion (e.g. major/severe stroke patients with poor cognition). In addition, diagnosis of stroke in SHARE was by self-report rather than by careful review of medical history. As a result, resource use information derived from SHARE may not be as reliable as that obtained from population-based cohort studies that carefully ascertain and follow-up people with stroke, which unfortunately have only been undertaken in a small number of countries.27
Furthermore, our sick leave and early retirement costs were only estimated during the time it takes to replace a worker with another from the pool of unemployed, i.e. the friction period. An alternative would have been to value worker absence in terms of lost earnings without any adjustment, i.e. the human capital approach. However, as there is little consensus as to which approach is best,28,29 we adjusted for the ‘friction period’ to be consistent with previous work and allow meaningful comparisons with conditions such as cancer, blood disorders and dementia.11,12,15 Nonetheless, the human capital approach was applied in sensitivity analyses, which showed that the total costs of stroke increased from €60 billion (using friction-adjusted costs) to €65 billion (using the human capital approach).
Finally, our estimates are likely to be an underestimate. Some categories of health care costs, such as, public health activities, supportive treatments, home adaptations, paid formal home care and other care provided outside the healthcare system (e.g. social worker visits, meals on wheels, and hospice care based outside hospitals) are not recorded in health care statistics. These categories of cost were not included because of data limitations and the inability to collect these data for all countries under study.
Conclusion
Our study provides a snapshot of the economic consequences posed by stroke to 32 European countries in 2017. It estimates that stroke cost these countries €60 billion a year, and together with the evidence we have gathered over the last 15 years,8,10,26 it indicates that the costs of stroke are rising over time, partly due to an ageing population, making the absolute number of people living with stroke increase throughout Europe.
Supplemental Material
Supplemental material, ESO883160 Supplemental Material for Economic burden of stroke across Europe: A population-based cost analysis by Ramon Luengo-Fernandez, Mara Violato, Paolo Candio and Jose Leal in European Stroke Journal
Acknowledgements
We are grateful to Winnie Mei for the literature review she undertook on nursing home admission after stroke. We are extremely grateful to the reviewers for their detailed comments, which have considerably strengthened this manuscript.
This paper uses data from SHARE Waves 2, 4, and 6 (DOIs: 10.6103/SHARE.w2.700, 10.6103/SHARE.w3.700, 10.6103/SHARE.w4.700, 10.6103/SHARE.w6.700, see Börsch-Supan et al. (2013) for methodological details.16
Declaration of Conflicting Interests
The author(s) declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by the Stroke Alliance For Europe (SAFE), which had no influence on the study design, data collection and presentation or the conclusions made.
Informed consent
Not applicable.
Ethical approval
Not applicable.
Guarantor
Not applicable.
Contributorship
RL-F and JL designed the study. RL-F and PC did the literature search. RL-F and MV collected data. RL-F, JL and MV analysed data. All authors interpreted data and wrote the report.
Supplemental Material
Supplemental material for this article is available online.
References
- 1.European Commission. Eurostat: your key to European Statistics, https://ec.europa.eu/eurostat/data/database (accessed 07 May 2019).
- 2.World Health Organization. Cause of death query online, http://apps.who.int/healthinfo/statistics/mortality/causeofdeath_query/ (accessed 03 September 2018).
- 3. Stroke prevention by the practitioner: epidemiology of stroke. Cerebrovasc Disord 1999; 9: 1–68. [Google Scholar]
- 4.Jenkinson C, Gibbons E, Fitzpatrick R. A structured review of patient-reported outcome measures (PROMs) for stroke: report to the Department of Health, http://phi.uhce.ox.ac.uk/pdf/PROMs_Oxford_Stroke_17092010.pdf (accessed 30 June 2019).
- 5.Global Burden of Disease Study 2013 Study Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2015; 386: 743–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Luengo-Fernandez R, Gray A, Rothwell PM. Costs of stroke using patient-level data: a critical review of the literature. Stroke 2009; 40: 23e18. [DOI] [PubMed] [Google Scholar]
- 7.Olesen J, Gustavsson A, Svensson M, et al. The economic cost of brain disorders in Europe. Eur J Neurol 2012; 19: 155–162. [DOI] [PubMed] [Google Scholar]
- 8.Wilkins E, Wilson L, Wickramasinghe K, et al. European Cardiovascular Disease Statistics 2017 edition, http://www.ehnheart.org/images/CVD-statistics-report-August-2017.pdf (2017, accessed 30 May 2019).
- 9.Luengo-Fernandez R, Paul NLM, Gray A, et al. A population-based study of disability and institutionalisation after TIA and stroke: 10-year results of the Oxford Vascular Study. Stroke 2013; 44: 2854–2861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leal J, Luengo-Fernandez R, Gray A, et al. Economic burden of cardiovascular diseases in the enlarged European Union. Eur Heart J 2006; 27: 1610–1619. [DOI] [PubMed] [Google Scholar]
- 11.Luengo-Fernandez R, Leal J, Gray A. Cost of dementia in the pre-enlargement countries of the European Union. J Alzheimer’s Dis 2011; 27: 187–196. [DOI] [PubMed] [Google Scholar]
- 12.Luengo-Fernandez R, Leal J, Gray A, et al. Economic burden of cancer across the European Union: a population-based cost analysis. Lancet Oncol 2013; 14: 1165–1174. [DOI] [PubMed] [Google Scholar]
- 13.Leal J, Luengo-Fernandez R, Sullivan R, et al. Economic burden of bladder cancer across the European Union. Eur Urol 2016; 69: 438–447. [DOI] [PubMed] [Google Scholar]
- 14.Luengo-Fernandez R, Leal J, Gray A. Research spend in the UK: comparing stroke, cancer, coronary heart disease and dementia, https://www.stroke.org.uk/sites/default/files/sa-research_spend_in_the_uk_apr2015_web.pdf (2015, accessed 30 May 2019). [DOI] [PMC free article] [PubMed]
- 15.Burns R, Leal J, Sullivan R, et al. Economic burden of malignant blood disorders across Europe: a population-based cost analysis. Lancet Haematol 2016; 3: e362–e370. [DOI] [PubMed] [Google Scholar]
- 16.Luengo-Fernandez R, Burns R, Leal J. Economic burden of non-malignant blood disorders across Europe: a population-based cost study. Lancet Haematol 2016; 3: e371–e378. [DOI] [PubMed] [Google Scholar]
- 17.Borsch-Supan A, Brandt M, Hunkler C, et al. Data resource profile: the Survey of Health, Ageing and Retirement in Europe (SHARE). Int J Epidemiol 2013; 42: 992–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.OECD OECD Health Statistics, http://www.oecd.org/els/health-systems/health-data.htm (2018, accessed 07 May 2019).
- 19.Institute of Health Metrics Global Burden of Disease, http://www.healthdata.org/gbd (accessed 14 May 2019).
- 20.Organization WH. Cause of death query online, http://apps.who.int/healthinfo/statistics/mortality/causeofdeath_query/ (accessed 03 September 2018).
- 21.Internation Labour Organization. Key indicators of the labour market, https://www.ilo.org/ilostat/faces/wcnav_defaultSelection?_afrLoop=609972699080347&_afr WindowMode=0&_afrWindowId=nhv4sik25_1#!%40%40%3F_afrWindowId%3Dnhv4sik25_1%26_afrLoop%3D609972699080347%26_afrWindowMode%3D0%26_adf.ctrl-state%3Dnhv4sik25_87 (accessed 03 September 2018).
- 22.Central Bureau of Statistics. Employed persons by industry, age, population group and sex, http://www.cbs.gov.il/publications17/lfs15_1684/pdf/t02_03.pdf (accessed 03 September 2018).
- 23.Federal Statistics Office. Private and public sectors, https://www.bfs.admin.ch/bfs/en/home/statistics/work-income/wages-income-employment-labour-costs/wage-levels-switzerland/private-public-sectors.html (accessed 02 July 2018).
- 24.Koopmanschap M, van Ineveld B. Towards a new approach for estimating indirect costs of disease. Sco Sci Med 1992; 34: 1005–1010. [DOI] [PubMed] [Google Scholar]
- 25.Benjamin EJ, Muntaner P, Alonso A, et al. Heart disease and stroke statistics – 2019 update: a report from the American Heart Association. Circulation 2019; 139: e56–e528. [DOI] [PubMed] [Google Scholar]
- 26.Nichols M, Townsend N, Scarborough P, et al. European cardiovascular disease statistics. Brussels: European Heart Network, 2012. [Google Scholar]
- 27.Feigin V, Lawes CMM, Bennett DA, et al. Stroke epidemiology: a review of population based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol 2003; 2: 43–53. [DOI] [PubMed] [Google Scholar]
- 28.Johannesson M, Karlsson G. The friction cost method: a comment. J Health Econ 1997; 16: 249–255. [DOI] [PubMed] [Google Scholar]
- 29.Drummond MF, Sculpher MJ, Torrance GW, et al. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press, 2005. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, ESO883160 Supplemental Material for Economic burden of stroke across Europe: A population-based cost analysis by Ramon Luengo-Fernandez, Mara Violato, Paolo Candio and Jose Leal in European Stroke Journal