Abstract
Studies of SARS coronavirus (SARS-CoV)—the causative agent of severe acute respiratory syndrome (SARS)—have been hampered by its high transmission rate and the pathogenicity of this virus. To permit analysis of the host range and entry mechanism of SARS-CoV, we incorporated the humanized SARS-CoV spike (S) glycoprotein into HIV particles to generate a highly infectious SARS-CoV pseudotyped virus. The infection on Vero E6—a permissive cell line to SARS-CoV—could be neutralized by sera from convalescent SARS patients, and the entry was a pH-dependent process. With these highly infectious SARS-CoV pseudotypes, several cell lines derived from various tissues were revealed as susceptible to SARS-CoV, which were highly corresponding to the expression pattern of virus’s receptor angiotensin-converting enzyme 2 (ACE2). In addition, we also demonstrated angiotensin 1 converting enzyme (ACE)—the homologue of ACE2 could not function as a receptor for SARS-CoV.
Severe acute respiratory syndrome (SARS) was a life-threatening disease caused by SARS-CoV [1], [2], [3]. It has caused more than 700 deaths recorded by the World Health Organization (WHO), and new cases have been recently reported from East and Southeast Asia. Unfortunately, studies on SARS-CoV were limited because of the highly infectious nature of this virus. Among the recently reported new cases, several patients were suspected to have been infected in SARS-CoV research laboratories. Therefore, a safe approach is needed for investigative research where a wild-type SARS-CoV has to be used.
Pseudotyped viruses with heterogenic glycoproteins incorporated into retroviral particles were proved to be a safe viral entry model, which only go through a single-cycle infection and acquired the host range of the parent viruses where the glycoproteins were derived [4], [5], [6], thus they could facilitate the research on viral entry mechanism, cell tropism, neutralization antibody analysis, and receptor identification [7], [8], [9], [10].
In this report, we expressed SARS spike protein from a synthetic codon-optimized gene, which could dramatically increase S protein expression compared with native S gene. The S protein could incorporate into HIV cores to generate pseudotyped virus with high infectivity on Vero E6 cells. The infection could be neutralized by sera from convalescent SARS patients, and the entry process was pH-dependent. With these SARS-CoV pseudotypes, we analyzed the cell tropism of SARS-CoV and its correlation with its receptor ACE2 expression [11], [12]. We found that various tissue-derived cell lines were susceptible to the pseudotype infection, and the infectivity was correlated with the ACE2 expression. We also demonstrated that ACE—the homologue of ACE2 could not function as a receptor for SARS-CoV.
Materials and methods
Synthetic S gene and plasmid constructions. The cDNA of the SARS-CoV (strain BJ01, GenBank Accession No. AY278488) was a gift from Dr. Li Ruan (China CDC, Beijing). The SARS-CoV S gene was amplified by PCR using the following primers: 5′-CGGGATCCAACGAACATGTTTATTTTCTTATTATTTC-3′ and 5′-CGGAATTCGTTTATGTGTAATGTAATTTGACACCC-3′. The fragment was cloned into pcDNA3.1 (+) vector to generate the plasmid pS. In order to create a codon optimized S gene, 60 overlapping primers were synthesized and assembled by overlapping PCR. Pyrobest DNA polymerase (Takara, Japan) was used in all PCRs. In the first forward primer, tissue plasminogen activator (Tpa) signal sequence (MDAMKRGLCCVLLLCGAVFVSA) was introduced to replace the original signal peptide of the S gene (MFIFLLFLTLTSG). The chimeric wild-type S with Tpa was named TS, the synthetic S gene with Tpa was named TSh. Sequences were determined by sequencing and cloned into a pcDNA3.1 (+) vector to generate pTS and pTSh.
Cell lines. 293T cells were used as packaging cell lines for preparing the pseudotyped virus. Huh7 was a gift from Dr. Stanley M. Lemon (The University of Texas Medical Branch, USA). Human cell lines (Bel7402, T84, Colo320, SW480, SPC-A1, A549, Glc-82, and Hep-2), a monkey cell line (Vero E6), and a mouse cell line (CHO) were obtained from Wuhan Institute of Virology (Wuhan, China). To establish the ACE or ACE2 expressing cell lines, the cDNA of human ACE (gift from Dr. Pierre Corvol) or ACE2 was transduced into NIH/3T3 or HeLa cells by retroviral vector pMX, and the expression of ACE or ACE2 was detected by FACS using anti-ACE or anti-ACE2 polyclonal antibody (R&D systems, Minneapolis).
FACS analysis of S protein expression. S expression constructs were transfected into 293T by the calcium phosphate precipitation method. The cells were harvested 48 h after transfection and incubated with the sera for 1 h. These cells were then incubated with FITC-conjugated goat anti-human IgG (Sigma, St. Louis) for 30 min. After 3 washes, the cells were subjected to analysis using a Moflo cytometer (DAKO Cytomation, Denmark).
Western blot. Viral pellets and lysates of the transfected 293T cells were then subjected to 8% SDS–PAGE, which was followed by transfer to a nitrocellulose membrane (Amersham–Pharmacia, Germany) and incubated with sera (1:200 dilution) from rabbits immunized with the N-terminal domain (14–670) of the S protein; and an alkaline phosphatase-labeled goat anti-rabbit IgG (Santa Cruz Biotechnology, California) was used as the secondary antibody.
Pseudotyped virus infection assays. The SARS-CoV pseudotyped virus HIV/SARS was produced by a similar method which was described previously [8]. Briefly, 10 μg pNL4.3.Luc. R−E−pro− [13] and 10 μg pTSh were co-transfected into 293T cells in 10 cm dishes. Supernatants were harvested 48 h later and used in infection assays. The pseudotyped virus was purified by ultracentrifugation through a 20% sucrose cushion at 50,000g for 90 min, resuspended in 100 μl PBS, and normalized by p24 ELISA using a Vironostika HIV-1 Antigen MicroELISA Kit (Biomerieux bv, Boxtel, The Netherlands). The supernatant containing 5 ng pseudotyped virus (p24) was used to infect cells in 24-well plates (4–8 × 104 cells/well). The cells were lysed at 48 h post-infection. Twenty microliters of lysate was tested for luciferase activity by the addition of 50 μl of luciferase substrate and measured for 10 s in a Wallac Multilabel 1450 Counter (Perkin–Elmer, Singapore). For neutralization tests, diluted SARS patient’s sera were mixed with equal volumes of pseudotyped virus supernatants. After incubation at 37 °C for 30 min, 100 μl mixtures were added to Vero E6 cells in 96-well plates. The cells were lysed at 48 h post-infection and tested for luciferase activity as described above.
Cell fusion assay. COS-7 cells were transduced with S gene (TS or TSh) by retroviral vector pBabe-puro and selected in culture medium containing 5 μg/ml puromycin for one week. The puromycin resistant cells were checked for S protein expression and named TS-COS and TSh-COS, respectively. These cells were mixed with Vero E6 cells at a ratio of 1:1 and co-cultured for 8 h, and the syncytium was examined under microscope.
RT-PCR. The total RNA of target cells was isolated with a Trizol reagent (Life Technologies, Rockville, MD). The expression of ACE2 was analyzed with the following primers: forward 5′-GCACTCACGATTGTTGGGACT-3′; reverse 5′-ATTAGCCACTCGCACATCCTC-3′. The expression of mouse ACE2 was analyzed with the following primers: forward 5′-GCATTGACAATTGTTGGAACA-3′; reverse 5′-ATCACTCACTCGTACATCTTC-3′. The expression of human ACE was analyzed with the following primers: forward 5′-CGGCTCAATGGCTATGTAGATGC-3′; reverse 5′-TCCCTCAAGGCCACAGGTAAGTC-3′.
Treatment with NH 4 Cl. Huh7 cells in 24-well plates were pretreated for 1 h with serum-free DMEM containing NH4Cl at various concentrations (0–30 mM), at 37 °C. HIV/SARS, HIV/AMLV or HIV/VSV-G pseudoviruses were added onto Huh7 cells in the presence of NH4Cl at various concentrations. After 12 h incubation, the supernatant was replaced with DMEM containing 10% FBS. The luciferase activity was determined at 48 h post-infection as described above.
Results and discussion
The expression of the S protein using a codon-optimized S gene.
The spike (S) glycoprotein of the coronavirus is the major envelope protein that plays a key role in viral entry. It not only binds to the cellular receptor but also initiates membrane fusion [14], [15], [16], [17]. To develop the pseudotyped virus system for studying SARS-CoV entry, we initially transfected pTS containing the native S gene into 293T cells, but found that the expression of the S protein in transfected cells was too weak to be detected either by FACS or Western blot (Figs. 1 A and B). The poor expression from the native S gene might be due to codon bias, since the native S gene had a codon usage that differed substantially from those of human genes (Fig. 1C). We therefore synthesized a humanized S gene (TSh) in which native codons were replaced with the degenerate codons used most frequently in human genes. When the pTSh was transfected into 293T cells, the S protein could be easily detected by FACS analysis (Fig. 1A). Western blot analysis of lysates from the pTSh transfected 293T cells showed two major protein bands that reacted with anti-S sera: a 180 kDa protein corresponding to the previously described size for the mature S protein on SARS-CoV virions [18] and a 130 kDa protein consistent with the calculated molecular weight of the nonglycosylated precursors of the S protein (Fig. 1B).
Fig. 1.
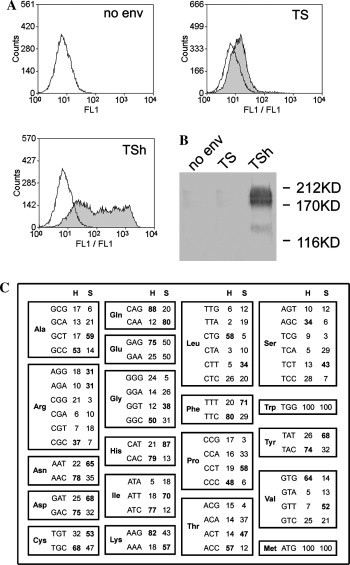
The expression of S protein from a codon-optimized S gene. (A) 293T cells were transfected with pTS, pTSh or pcDNA3.1 (+). The expression of S protein was analyzed by FACS. Transfected cells were stained with sera from SARS patients (hatched shape) or normal sera (open shape). (B) Lysates of transfected 293T cells were analyzed by Western blot using anti-S protein rabbit sera. (C) Codon usage of SARS S glycoprotein (S) and human genes (H). The percentage of each codon in degenerate codons is listed and the most prevalent codon has been shown in bold.
Infectious SARS-CoV pseudotyped virus can be assembled in vitro
We then produced the pseudotyped virus HIV/SARS by co-transfecting 293T cells with pTSh and pNL4.3.Luc.R−E−pro− [8]. As controls, pTS or pVSV-G was co-transfected with pNL4.3.Luc.R−E−pro− into 293T cells. The supernatant was collected and the virus particles were concentrated by ultra centrifugation and then normalized by p24 ELISA. These viral particles were subjected to immunoblots using rabbit polyclonal antisera raised against the S protein. The results showed that a 180 kDa band of the mature S protein was detected in virus particles generated from pTSh, indicating that the S glycoprotein expressed in 293T cells could incorporate into pseudotyped particles (Fig. 2 A). The absence of detectable S protein in virus particles generated from pTS further confirmed that the codon optimization of native S gene could improve the expression of S glycoprotein.
Fig. 2.
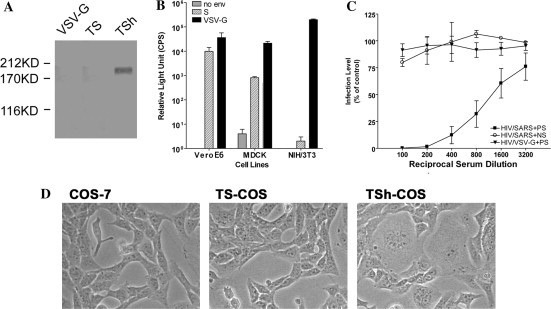
Generation of HIV/SARS pseudotyped virus. (A) The purified pseudotyped viruses were analyzed by Western blot using anti-S rabbit sera. (B) Several cell lines were infected with the HIV/SARS. The means of luciferase activity of HIV/env- (gray), HIV/TSh (striped), and HIV/VSV-G (black) are shown. (C) Neutralization assays of the HIV/SARS infection: HIV/SARS + patient’s serum (HIV/SARS + PS, black square), HIV/VSV-G + patient’s serum (HIV/VSV-G + PS, black triangle), and HIV/SARS + normal serum (HIV/SARS + NS, white circle). All the data are expressed as percentages of infectivity of control (without sera). (D) Syncytia formation occurred in co-cultured Vero E6 and TSh-COS cells. TS-COS cells and non-transduced COS-7 cells co-cultured with Vero E6 cells were used as controls.
To test if the pseudotyped virus was infectious and displayed the same host range as SARS-CoV, we infected Vero E6, MDCK, and NIH/3T3 cells with HIV/SARS. Our data showed that Vero E6 and MDCK were susceptible to HIV/SARS infection (Fig. 2B). This is consistent with the infection pattern of the wild-type SARS-CoV [3], [19]. To determine whether the infectivity of HIV/SARS can be mediated by S protein and was SARS-CoV specific, we incubated the pseudotyped virus with sera from convalescent SARS patients before adding them onto Vero E6 cells for infection. We showed that convalescent SARS patients’ sera had a high neutralizing activity on SARS-CoV pseudotypes, while they failed to neutralize pseudotypes with VSV G glycoprotein (Fig. 2C). This result indicated that the entry process of SARS-CoV was mediated by S protein and this mechanism is similar to those of murine hepatitis virus and transmissible gastroenteritis coronavirus [16], [17].
The key role of the S protein in viral entry was further confirmed by cell fusion assay. We transduced pTS or pTSh into COS-7 cells to establish COS-TS and COS-TSh cell lines. When these cells were co-cultured with Vero E6 cells, large amounts of syncytia were observed in Vero E6 plus COS-TSh, but not in Vero E6 plus COS-7 or Vero E6 plus COS-TS (Fig. 2D). The entry mechanism of SARS-CoV pseudotyped virus in our results was similar to those recently demonstrated by Graham Simmons et al. [20], who increased the expression of S protein by utilizing a chicken β-actin promoter and generated HIV(SARS-S) pseudovirions. In our experiment, codon optimization dramatically increased the expression of S protein and led to high titer HIV/SARS production. Moreover, the luciferase reporter gene used in our experiment provided a convenient and high throughput assay.
Cell tropism of SARS-CoV and its correlation with ACE2 expression
The establishment of the pseudotyped virus HIV/SARS provided us a convenient and safe method for studying the viral tropism, which would help to reveal potential SARS-CoV target tissues besides the lung. Using this virus, we assessed the infectivity of SARS-CoV using a panel of cell lines. Among the tested cell lines, Huh7 (human liver cell line) and Vero E6 exhibited the highest susceptibility to HIV/SARS. Two other human liver cell lines (HepG2 and Bel7402), one lung cell line (Glc82), and two colon intestine cell lines (T84 and Colo320) could also be infected by HIV/SARS to various degrees. A canine kidney-derived cell line (MDCK) also exhibited susceptibility to HIV/SARS. However, HeLa, A549, H7402, L02, Hep-2, SW480, NIH/3T3, COS-7, RD, and CHO cells were not infected by HIV/SARS. As a control, all cell lines were readily infected by HIV/VSV-G (Fig. 3 A).
Fig. 3.
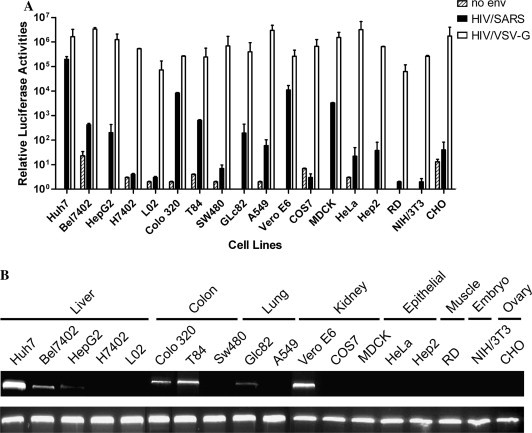
Analysis of cell tropism and its correlation with the expression pattern of ACE2. (A) Various cell lines were infected with HIV/SARS (black). Pseudotypes with no envelope protein (striped) or with VSV-G (white) were used as negative and positive controls. All infections were performed in triplicate. The error bar stands for SD. (B) Analysis of the ACE2 expression in these cells by RT-PCR. Total RNA from these cells was amplified with primers specific for ACE2 or β-actin as a control (bottom).
We then analyzed the expression of ACE2 in these cells in order to establish a correlation between ACE2 expression and HIV/SARS susceptibility. Our data showed that ACE2 expressed in all susceptible cell lines except MDCK; however, the ACE2 did not express in non-permissive cells such as HeLa and NIH/3T3. The MDCK cell line was canine-derived and we were not sure whether our PCR primers were suitable because the ACE2 sequence in canines was unavailable. The expression level of ACE2 was relatively high in Vero E6 and Huh7 cells and was weaker in Bel7402, HepG2, T84, Colo320, and Glc82 (Fig. 3B). These data established a strong correlation between ACE2 expression and the cell susceptibility to the HIV/SARS.
ACE2 is highly expressed in respiratory, cardiovascular tissues, and in the gastrointestinal systems [21]. Previous studies have shown that respiratory and gastrointestinal system were major targets for SARS-CoV in vivo [1], [3], [22], [23]. The high level of ACE2 expression can explain the tropism of SARS-CoV in these two systems. Thus, the tissue-specificity of SARS-CoV infection may be determined, at least in part, by tissue-dependent expression of ACE2.
ACE cannot function as receptor for SARS-CoV
Recent studies showed that the immune system was impaired during the course of SARS, including decreases of T lymphocyte in the acute phase and the observation of virus-like particles in mononuclear macrophage [24], [25]. We analyzed the expression of ACE2 in these cells by RT-PCR but failed to detect its expression (data not shown). It was reported that ACE—the homologue of ACE2, was expressed in T lymphocyte, macrophage, and dendritic cells [26], [27], and this was confirmed by our RT-PCR results (data not shown). To test whether ACE could mediate the entry of SARS-CoV as ACE2, we transduced cDNA of human ACE into NIH/3T3 cells or HeLa cells, the ACE expressing cells could neither be infected by HIV/SARS (Fig. 4 A) nor bind to soluble S protein (Fig. 4B). Our data indicated that the ACE could not function as a receptor for SARS-CoV and the impairment of immune system in SARS patients might be due to other unknown reasons.
Fig. 4.

ACE could not function as a receptor for SARS-CoV. The cDNA of ACE or ACE2 was transduced into NIH/3T3 or HeLa cells by retroviral vector pMX. (A) The transduced cells were infected with HIV/SARS pseudovirus and the luciferase activity was assayed 2 days post-infection. Non-transduced NIH3T3 and HeLa cells were used as control. (B) The ACE or ACE2 expressing HeLa cells were incubated with soluble S protein (hatched shape) or control (open shape), anti-S sera, and fluorescence-labeled secondary antibody. The binding of S was analyzed by FACS.
SARS-CoV pseudotyped virus entry is pH-dependent
Enveloped viruses enter host cells mainly through two pathways. One is direct fusion at the plasma membrane that occurs in a neutral environment. The other is receptor-mediated endocytosis in which low pH within the endosome is required to trigger membrane fusion. Inhibitors of vacuolar acidification, such as ammonium chloride, can prevent virus entry through the latter pathway [28]. To assess through which pathway HIV/SARS used to enter the cell, we treated the Huh7 cells with ammonium chloride before infection. Pseudotyped viruses HIV/VSV-G and HIV/AMLV demonstrating pH-dependent and independent entry were used as positive and negative controls, respectively. Infectivity of HIV/SARS and HIV/VSV-G, but not HIV/AMLV, was similarly diminished by ammonium chloride (Fig. 5 ). Treatment with 30 mM ammonium chloride caused complete inhibition of infection by HIV/SARS (Fig. 5). This result was consistent with the recent report by Yang et al. [29]. The pH dependency of infection indicated that the entry of HIV/SARS into host cells was most likely mediated by endocytosis.
Fig. 5.
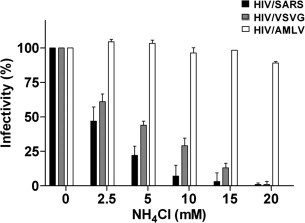
pH-dependency of HIV/SARS infectivity. Huh7 cells treated with various concentrations of NH4Cl were infected with HIV/SARS. The pH-dependent HIV/VSV-G and pH-independent HIV/AMLV pseudotyped viruses were used as positive and negative controls, respectively.
In this study, we generated a SARS-CoV pseudotyped virus HIV/SARS using a synthetic codon-optimized SARS-CoV S gene, and showed that the entry of HIV/SARS was mediated by the S protein and was a pH-dependent process; we also showed that the entry of HIV/SARS into host cells could be blocked by the convalescent sera from SARS patients. Most importantly, our cell tropism analysis indicated that multiple tissues besides the lung might be susceptible to SARS-CoV infection because of the specific expression of ACE2. Finally, this SARS-CoV pseudotyped virus we generated in this study can be used as an efficient and safe system for analyzing the character of SARS-CoV infection including immune responses to SARS-CoV infection, development of neutralizing antibodies, and detailed characterization of the S protein function.
Acknowledgments
We thank Dr. Tung-Tien Sun, Dr. Xiangpeng Kong, Dr. Hui Zhang, and Dr. Ryan Young for critical reading of the manuscript. We thank Dr. Pierre Corvol for providing ACE cDNA plasmid. We also acknowledge Liying Du for providing the technical support during flow cytometric analysis. This research was supported by National Nature Science Foundation of China Grant (30340027), Ministry of Science and Technology Grant (2003CB514116), National Nature Science Foundation of China for Outstanding Young Scientist Award (30125022) National Natural Science Foundation of China and German Research Association Grant (GZ237[202/10]0, and 6th Framework Program of European Commission Grant (511063) to H. Deng, and Ministry of Science and Technology Grant (G1999011904) to M. Ding.
References
- 1.Drosten C., Gunther S., Preiser W., van der Werf S., Brodt H.R., Becker S., Rabenau H., Panning M., Kolesnikova L., Fouchier R.A., Berger A., Burguiere A.M., Cinatl J., Eickmann M., Escriou N., Grywna K., Kramme S., Manuguerra J.C., Muller S., Rickerts V., Sturmer M., Vieth S., Klenk H.D., Osterhaus A.D., Schmitz H., Doerr H.W. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N. Engl. J. Med. 2003;348:1967–1976. doi: 10.1056/NEJMoa030747. [DOI] [PubMed] [Google Scholar]
- 2.Fouchier R.A., Kuiken T., Schutten M., van Amerongen G., van Doornum G.J., van den Hoogen B.G., Peiris M., Lim W., Stohr K., Osterhaus A.D. Aetiology: Koch’s postulates fulfilled for SARS virus. Nature. 2003;423:240. doi: 10.1038/423240a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ksiazek T.G., Erdman D., Goldsmith C.S., Zaki S.R., Peret T., Emery S., Tong S., Urbani C., Comer J.A., Lim W., Rollin P.E., Dowell S.F., Ling A.E., Humphrey C.D., Shieh W.J., Guarner J., Paddock C.D., Rota P., Fields B., DeRisi J., Yang J.Y., Cox N., Hughes J.M., LeDuc J.W., Bellini W.J., Anderson L.J. A novel coronavirus associated with severe acute respiratory syndrome. N. Engl. J. Med. 2003;348:1953–1966. doi: 10.1056/NEJMoa030781. [DOI] [PubMed] [Google Scholar]
- 4.Dong J., Roth M.G., Hunter E. A chimeric avian retrovirus containing the influenza virus hemagglutinin gene has an expanded host range. J. Virol. 1992;66:7374–7382. doi: 10.1128/jvi.66.12.7374-7382.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Landau N.R., Page K.A., Littman D.R. Pseudotyping with human T-cell leukemia virus type I broadens the human immunodeficiency virus host range. J. Virol. 1991;65:162–169. doi: 10.1128/jvi.65.1.162-169.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Suomalainen M., Garoff H. Incorporation of homologous and heterologous proteins into the envelope of Moloney murine leukemia virus. J. Virol. 1994;68:4879–4889. doi: 10.1128/jvi.68.8.4879-4889.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chan S.Y., Empig C.J., Welte F.J., Speck R.F., Schmaljohn A., Kreisberg J.F., Goldsmith M.A. Folate receptor-alpha is a cofactor for cellular entry by Marburg and Ebola viruses. Cell. 2001;106:117–126. doi: 10.1016/s0092-8674(01)00418-4. [DOI] [PubMed] [Google Scholar]
- 8.Deng H., Liu R., Ellmeier W., Choe S., Unutmaz D., Burkhart M., Di Marzio P., Marmon S., Sutton R.E., Hill C.M., Davis C.B., Peiper S.C., Schall T.J., Littman D.R., Landau N.R. Identification of a major co-receptor for primary isolates of HIV-1. Nature. 1996;381:661–666. doi: 10.1038/381661a0. [DOI] [PubMed] [Google Scholar]
- 9.Wool-Lewis R.J., Bates P. Characterization of Ebola virus entry by using pseudotyped viruses: identification of receptor-deficient cell lines. J. Virol. 1998;72:3155–3160. doi: 10.1128/jvi.72.4.3155-3160.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Deng H.K., Unutmaz D., KewalRamani V.N., Littman D.R. Expression cloning of new receptors used by simian and human immunodeficiency viruses. Nature. 1997;388:296–300. doi: 10.1038/40894. [DOI] [PubMed] [Google Scholar]
- 11.Wang P., Chen J., Zheng A., Nie Y., Shi X., Wang W., Wang G., Luo M., Liu H., Tan L., Song X., Wang Z., Yin X., Qu X., Wang X., Qing T., Ding M., Deng H. Expression cloning of functional receptor used by SARS coronavirus. Biochem. Biophys. Res. Commun. 2004;315:439–444. doi: 10.1016/j.bbrc.2004.01.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li W., Moore M.J., Vasilieva N., Sui J., Wong S.K., Berne M.A., Somasundaran M., Sullivan J.L., Luzuriaga K., Greenough T.C., Choe H., Farzan M. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003;426:450–454. doi: 10.1038/nature02145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Connor R.I., Chen B.K., Choe S., Landau N.R. Vpr is required for efficient replication of human immunodeficiency virus type-1 in mononuclear phagocytes. Virology. 1995;206:935–944. doi: 10.1006/viro.1995.1016. [DOI] [PubMed] [Google Scholar]
- 14.Sturman L.S., Holmes K.V. Proteolytic cleavage of peplomeric glycoprotein E2 of MHV yields two 90K subunits and activates cell fusion. Adv. Exp. Med. Biol. 1984;173:25–35. doi: 10.1007/978-1-4615-9373-7_3. [DOI] [PubMed] [Google Scholar]
- 15.Jackwood M.W., Hilt D.A., Callison S.A., Lee C.W., Plaza H., Wade E. Spike glycoprotein cleavage recognition site analysis of infectious bronchitis virus. Avian Dis. 2001;45:366–372. [PubMed] [Google Scholar]
- 16.Leparc-Goffart I., Hingley S.T., Chua M.M., Phillips J., Lavi E., Weiss S.R. Targeted recombination within the spike gene of murine coronavirus mouse hepatitis virus-A59: Q159 is a determinant of hepatotropism. J. Virol. 1998;72:9628–9636. doi: 10.1128/jvi.72.12.9628-9636.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sanchez C.M., Izeta A., Sanchez-Morgado J.M., Alonso S., Sola I., Balasch M., Plana-Duran J., Enjuanes L. Targeted recombination demonstrates that the spike gene of transmissible gastroenteritis coronavirus is a determinant of its enteric tropism and virulence. J. Virol. 1999;73:7607–7618. doi: 10.1128/jvi.73.9.7607-7618.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rota P.A., Oberste M.S., Monroe S.S., Nix W.A., Campagnoli R., Icenogle J.P., Penaranda S., Bankamp B., Maher K., Chen M.H., Tong S., Tamin A., Lowe L., Frace M., DeRisi J.L., Chen Q., Wang D., Erdman D.D., Peret T.C., Burns C., Ksiazek T.G., Rollin P.E., Sanchez A., Liffick S., Holloway B., Limor J., McCaustland K., Olsen-Rasmussen M., Fouchier R., Gunther S., Osterhaus A.D., Drosten C., Pallansch M.A., Anderson L.J., Bellini W.J. Characterization of a novel coronavirus associated with severe acute respiratory syndrome. Science. 2003;300:1394–1399. doi: 10.1126/science.1085952. [DOI] [PubMed] [Google Scholar]
- 19.Zhang Q.F., Cui J.M., Huang X.J., Lin W., Tan D.Y., Xu J.W., Yang Y.F., Zhang J.Q., Zhang X., Li H., Zheng H.Y., Chen Q.X., Yan X.G., Zheng K., Wan Z.Y., Huang J.C. Morphology and morphogenesis of severe acute respiratory syndrome (SARS)-associated virus. Sheng Wu Hua Xue Yu Sheng Wu Wu Li Xue Bao (Shanghai) 2003;35:587–591. [PubMed] [Google Scholar]
- 20.Simmons G., Reeves J.D., Rennekamp A.J., Amberg S.M., Piefer A.J., Bates P. Characterization of severe acute respiratory syndrome-associated coronavirus (SARS-CoV) spike glycoprotein-mediated viral entry. Proc. Natl. Acad. Sci. USA. 2004;101:4240–4245. doi: 10.1073/pnas.0306446101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harmer D., Gilbert M., Borman R., Clark K.L. Quantitative mRNA expression profiling of ACE2, a novel homologue of angiotensin converting enzyme. FEBS Lett. 2002;532:107–110. doi: 10.1016/s0014-5793(02)03640-2. [DOI] [PubMed] [Google Scholar]
- 22.Kuiken T., Fouchier R.A., Schutten M., Rimmelzwaan G.F., van Amerongen G., van Riel D., Laman J.D., de Jong T., van Doornum G., Lim W., Ling A.E., Chan P.K., Tam J.S., Zambon M.C., Gopal R., Drosten C., van der Werf S., Escriou N., Manuguerra J.C., Stohr K., Peiris J.S., Osterhaus A.D. Newly discovered coronavirus as the primary cause of severe acute respiratory syndrome. Lancet. 2003;362:263–270. doi: 10.1016/S0140-6736(03)13967-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leung W.K., To K.F., Chan P.K., Chan H.L., Wu A.K., Lee N., Yuen K.Y., Sung J.J. Enteric involvement of severe acute respiratory syndrome-associated coronavirus infection. Gastroenterology. 2003;125:1011–1017. doi: 10.1016/j.gastro.2003.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tang X., Yin C., Zhang F., Fu Y., Chen W., Chen Y., Wang J., Jia W., Xu A. Measurement of subgroups of peripheral blood T lymphocytes in patients with severe acute respiratory syndrome and its clinical significance. Chin. Med. J. (Engl.) 2003;116:827–830. [PubMed] [Google Scholar]
- 25.Lai R.Q., Feng X.D., Wang Z.C., Lai H.W., Tian Y., Zhang W., Yang C.H. Pathological and ultramicrostructural changes of tissues in a patient with severe acute respiratory syndrome. Zhonghua Bing Li Xue Za Zhi. 2003;32:205–208. [PubMed] [Google Scholar]
- 26.Friedland J., Setton C., Silverstein E. Induction of angiotensin converting enzyme in human monocytes in culture. Biochem. Biophys. Res. Commun. 1978;83:843–849. doi: 10.1016/0006-291x(78)91471-7. [DOI] [PubMed] [Google Scholar]
- 27.Costerousse O., Allegrini J., Lopez M., Alhenc-Gelas F. Angiotensin I-converting enzyme in human circulating mononuclear cells: genetic polymorphism of expression in T-lymphocytes. Biochem. J. 1993;290(Pt. 1):33–40. doi: 10.1042/bj2900033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sieczkarski S.B., Whittaker G.R. Dissecting virus entry via endocytosis. J. Gen. Virol. 2002;83:1535–1545. doi: 10.1099/0022-1317-83-7-1535. [DOI] [PubMed] [Google Scholar]
- 29.Yang Z.Y., Huang Y., Ganesh L., Leung K., Kong W.P., Schwartz O., Subbarao K., Nabel G.J. pH-dependent entry of severe acute respiratory syndrome coronavirus is mediated by the spike glycoprotein and enhanced by dendritic cell transfer through DC-SIGN. J. Virol. 2004;78:5642–5650. doi: 10.1128/JVI.78.11.5642-5650.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]


