Précis:
The objective of this study was to take a closer look at defense related expenses for medical malpractice cases over time. We conducted a retrospective review of medical malpractice claims reported to the Physician Insurers Association of America’s Data Sharing Project with a closing date between January 1, 1985 and December 31, 2008. On average a medical malpractice claim costs more than $27,000 to defend. Claims that go to trial are much more costly to defend than are those that are dropped, withdrawn, or dismissed. However, since the overwhelming majority of claims are dropped, withdrawn, or dismissed, the total amount spent to defend them surpasses that spent on claims that go to trial. Defense attorney expenses account for the majority of defense related expenses (74%), while expert witness expenses and other expenses split the remaining 26%. A strong association was also found between the average indemnity payment and the amount it costs to defend individual claims by specialty. Our study found that defense related expenses for medical malpractice claims are not an insignificant cost. As state and federal governments debate how to repair the malpractice system, addressing the high cost of defending claims should not be ignored.
BACKGROUND
Whenever health care reform is debated, the state of the medical professional liability (MPL) system (i.e., medical malpractice system) in the United States re-emerges as an issue of importance.1, 2 What exactly is broken with the MPL system and what the implications are is a point of contention among different stakeholder groups. Recent data demonstrate that medical liability premiums have been improving in recent years and actually held steady in 2009.3 General agreement still exists, however, that medical professional liability insurance premiums have become unaffordable for many physicians, and coverage has become less available, especially for certain medical specialties and in specific areas of the country.4–6
Multiple factors go into the determination of medical professional liability insurance premiums including return on investments, reinsurance costs, claims frequency, average amount paid out on malpractice claims, defense expenses, and administrative costs such as underwriting expense.5–7 These factors all interact with each other and, in general, evidence exists that each of these factors has played a role in the escalating cost of medical professional liability insurance.5
In order to address the medical malpractice crisis, a variety of tort reform efforts have been proposed and/or undertaken. However the majority of these reforms focus on indemnity payments related to a claim.8 These reform efforts include caps on damages, abolition of punitive damages, eliminating mandatory prejudgment interest, and modifications of the common law collateral source offset rule.9 From an insurer’s perspective, however, it is important to remember that payments related to the damages awarded are not the only factor that determines premiums; reform efforts may be missing the mark and perhaps should be focused on also controlling these other factors.
One of these factors is defense expense for malpractice claims. What is known about defense costs is limited, with many estimates being partly or entirely anecdotal.10 According to the Insurance Information Institute approximately 58% of a medical professional liability insurers total incurred losses was spent on defense costs and cost containment expenses in 2008, compared to approximately 40% in 2000.11 This percentage is even more striking when taking into account the fact that it only accounts for 13% of all insurance lines in 2008.11 What quantitative research is available about defense costs in medical malpractice cases has focused almost exclusively on claims where an indemnity payment is made.10, 12–14 This is a definite limitation of the research to date, as a large number of cases are dropped, withdrawn, or dismissed or result in a verdict for the defendant.15
The objective of this study was to take a closer look at defense related expenses for medical malpractice cases over time, focusing in on how expenses differ by adjudication status and medical specialty.
DESIGN AND METHODS
Data Source
Data for this study were obtained from the Physician Insurers Association of America’s (PIAA) Data Sharing Project. PIAA is a national insurance organization whose members are professional liability insurance companies owned and/or operated by doctors, providers and hospitals. As of 2010, the PIAA is comprised of 60 domestic insurers, 12 international insurers, and 46 affiliate members. PIAA member companies insure 325,000 medical practitioners in the U.S. and more than 400,000 in countries outside of the U.S.16 Since 1985, over half of the 60 member insurance companies of PIAA have participated in the PIAA Data Sharing Project (DSP) representing data from every state. The first goal of the PIAA DSP is to provide member companies who insure medical practitioners in the U.S. with detailed and credible information for use in risk management programs aimed at reducing the incidence of patient injury and thereby reducing physician exposure to claims.
Every six months, participating member insurance companies submit claims and loss data to the PIAA office. All data are collected in a generic format where the identity of the individual claimants, insureds, and other parties are not recorded. At the conclusion of each reporting period, PIAA produces reports based on the accumulation of this data.
The participating member insurance companies code all data for the PIAA DSP. Coders are comprised of individuals from the member companies who have experience handling medical malpractice claims within claims and risk management departments. These individuals have various professional backgrounds including medicine, nursing, and law. Many of these coders have undergone ICD-9 coding training and certification. PIAA also provides its own training for these coders and supplies all required submission materials, guidelines, and instructions for submitting information to the PIAA DSP. Medical cause of loss information is coded utilizing the Generic ICD-9-CM codes as well as PIAA created codes. When coding data for submission to the PIAA DSP, coders reference the claims file, which includes expert testimony and applicable medical reports. Additionally coders reference the PIAA DSP reference manual as well as the ICD-9 manual.
The following files are eligible for submission to the PIAA DSP: 1) closed claims and suits and 2) suits that have been open for one year. A claim is defined as a file in which a demand for compensation has been made, while a suit is a file in which formal litigation has been instituted. Suits that have been open for one year are resubmitted at the time of closure, thus capturing any additional information available or information that may have changed since the initial reporting to the data-sharing project.
While the data contained within the PIAA DSP database represents only 25% of medical malpractice claims in the United States, this coverage is greater than any other data source available, and has allowed us to examine a much larger number of claims than in previous studies. Moreover, the PIAA DSP is the only option we are aware of for analyzing large numbers of claims that do not result in a payment; such claims are actually the majority of all claims.
Data Analysis
We worked in conjunction with PIAA to perform a query of its DSP database. Specifically, we limited our query to claims reported to the system as of January 2010 that had a closing date between January 1, 1985 and December 31, 2008. Data variables included:
allocated loss adjustment expenses (ALAE): includes any expenses paid in the process of administering or adjudicating a claim including the investigative costs required during the claim resolution process.17 Payments generally include defense costs for attorneys provided by the carrier, expert witness fees, court costs, securing of medical records, etc.
adjudication status: refers to how claims are resolved. Resolution of malpractice claims occurs by settlement, involuntary dismissal, jury verdict, alternative dispute resolution (ADR) (binding arbitration or non-binding arbitration), or contract liability agreement.17
indemnity payout: refers to settlements or awards made directly to plaintiffs as a result of claim resolution process.17 The indemnity payout amount does NOT include allocated loss adjustment expenses.
The total ALAE for each claim was a required field during database entry. ALAE was also broken out into three sub-categories: defense attorney expense, expert witness expense, and other expenses. However sub-categorization of ALAE was optional during data entry.
Unless otherwise noted all monetary amounts presented in the results section are 2008 dollar values.
RESULTS
Between January 1, 1985 and December 31, 2008, data for 240,033 closed claims were recorded in the PIAA DSP database. Twenty-nine percent (N=70,803) of these claims resulted in an indemnity payout with an average payout amount of $282,843. The total ALAE for all closed claims was $6,542,810,750 or $27,258 on average. For every dollar of indemnity paid out, an additional $0.33 was spent on ALAE. Table 1 shows these data broken out by year that the claim was reported as being closed. In general, the average ALAE has been steadily increasing from a low of $13,395 (2008 dollar value) in 1985 to $43,258 in 2008. ALAE as a percent of total payouts have also been steadily increasing from 24% in 1985 ($0.24 for every ‘indemnity dollar’ paid) to 45% in 2008 ($0.45 for every ‘indemnity dollar’ paid).
Table 1.
ALAE Expenses By Year
| CLOSE YEAR | # OF CLOSED CLAIMS | # OF PAID CLAIMS | % PAID TO CLOSED | AVG INDEMNITY** | AVG ALAE** | % ALAE TO INDEMNITY |
|---|---|---|---|---|---|---|
| 1985 | 8,136 | 2,649 | 33% | $174,260 | $13,395 | 24% |
| 1986 | 10,963 | 3,697 | 34% | $187,273 | $16,031 | 25% |
| 1987 | 12,470 | 3,992 | 32% | $210,869 | $17,411 | 26% |
| 1988 | 11,953 | 3,846 | 32% | $230,840 | $20,625 | 28% |
| 1989 | 10,193 | 3,325 | 33% | $228,334 | $22,737 | 31% |
| 1990 | 9,827 | 3,138 | 32% | $228,000 | $24,995 | 34% |
| 1991 | 9,128 | 3,057 | 33% | $253,192 | $23,459 | 28% |
| 1992 | 10,867 | 3,687 | 34% | $281,089 | $25,490 | 27% |
| 1993 | 12,381 | 3,798 | 31% | $277,938 | $26,021 | 31% |
| 1994 | 11,879 | 3,500 | 29% | $274,314 | $27,172 | 34% |
| 1995 | 12,339 | 3,438 | 28% | $249,611 | $24,742 | 36% |
| 1996 | 12,667 | 3,224 | 25% | $269,400 | $23,180 | 34% |
| 1997 | 11,273 | 3,027 | 27% | $300,358 | $27,761 | 34% |
| 1998 | 9,949 | 2,782 | 28% | $306,651 | $28,315 | 33% |
| 1999 | 8,687 | 2,601 | 30% | $326,397 | $30,462 | 31% |
| 2000 | 6,066 | 2,003 | 33% | $354,721 | $35,473 | 30% |
| 2001 | 7,018 | 2,244 | 32% | $359,513 | $34,272 | 30% |
| 2002 | 7,104 | 2,199 | 31% | $370,725 | $32,786 | 29% |
| 2003 | 10,048 | 2,525 | 25% | $357,614 | $31,751 | 35% |
| 2004 | 10,223 | 2,561 | 25% | $376,019 | $33,530 | 36% |
| 2005 | 11,050 | 2,661 | 24% | $346,656 | $32,673 | 39% |
| 2006 | 8,604 | 2,140 | 25% | $353,113 | $35,242 | 40% |
| 2007 | 8,918 | 2,379 | 27% | $348,424 | $39,189 | 42% |
| 2008 | 8,290 | 2,330 | 28% | $342,670 | $43,258 | 45% |
| TOTAL | 240,033 | 70,803 | 29% | $282,843 | $27,258 | 33% |
Figure 1 shows the breakdown of these claims by adjudication status. The majority of these claims were either dropped, withdrawn, or dismissed (64%) therefore resulting in no indemnity payout. Only 7% of claims actually go to trial and result in a verdict. Of that 7% of claims, only 18% result in a verdict for the plaintiff (or 1% of claims overall).
Figure 1.
Adjudication Status of Claims
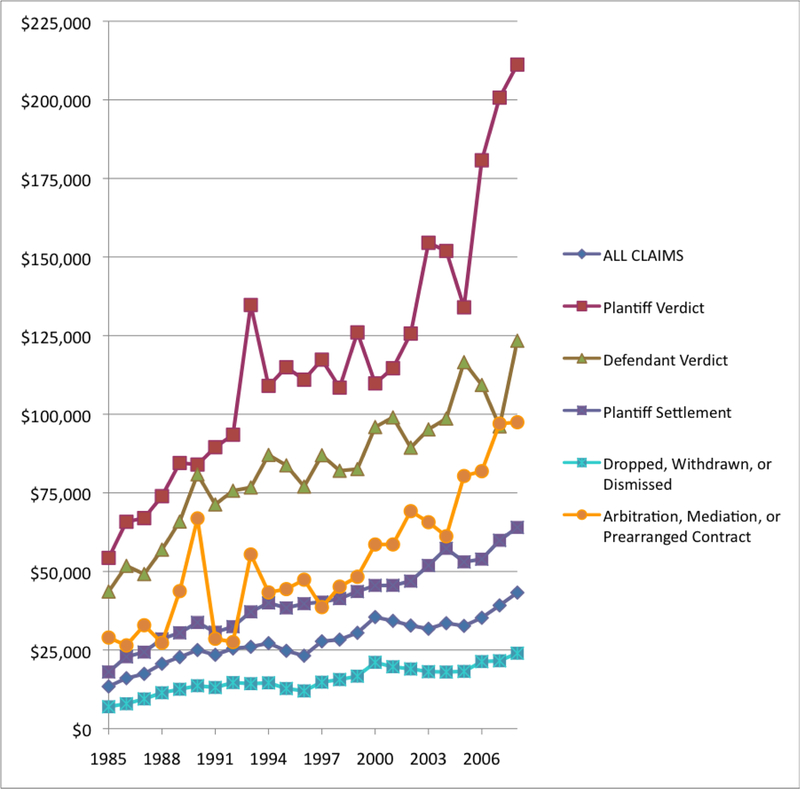
The cost to defend these claims varies greatly (See Table 2). On average the most expensive claims in terms of ALAE are those claims that result in a plaintiff settlement ($107,423) while those claims that are dropped, withdrawn, or dismissed are the least expensive ($15,056). However in terms of total money spent on ALAE those claims that are dropped, withdrawn, or dismissed are almost as expensive for insurers as those claims that result in a plaintiff settlement due to the sheer volume of claims that are dropped, withdrawn, or dismissed. Since 1985, the average amount of money spent on ALAE has been steadily increasing for all claims (See Figure 2). Except for very brief periods, the ordering of the average expenses for each type of closed claim was the same. The differences between these types of closed claims, however, has changed greatly over time.
Table 2.
ALAE Expenses by Adjudication Status
| Average ALAE | |
|---|---|
| Plaintiff Verdict | $107,423 |
| Defendant Verdict | $81,590 |
| Plaintiff Settlement | $38,867 |
| Dropped, Withdrawn, or Dismissed | $15,056 |
| Arbitration, Mediation, or Prearranged Contract | $62,290 |
Figure 2.
Average ALAE by Adjudication Status and Year
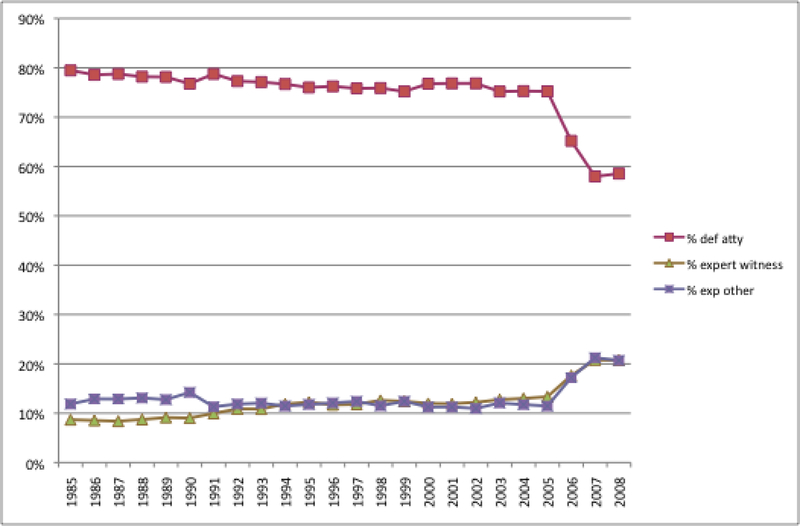
Within the PIAA DSP database, ALAE can be further sub-categorized into defense attorney expense, expert witness expense, and other expense. In general, 74% of total ALAE are allocated to defense attorney expenses while expert witness expenses and other expenses each account for 13% of total ALAE. However, since 2005 a notable shift in ALAE allocation can be seen with more money being spent on both expert witnesses and other expenses (See Figure 3). Further analysis of this data category was not possible with the data set utilized for this study.
Figure 3.
Total ALAE Composition by Year
ALAE by Medical Specialty
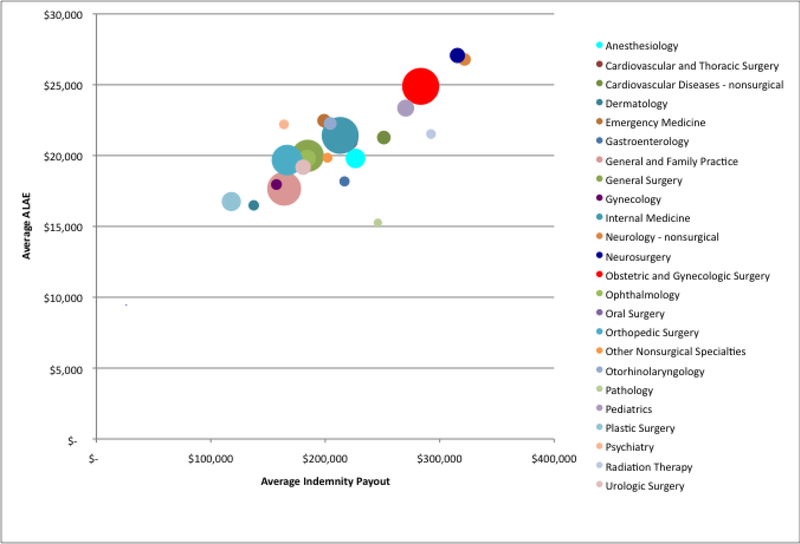
Figure 4 shows average ALAE by average indemnity payment by specialty. The size of each bubble reflects the relative number of claims for that particular specialty. This graph illustrates the large variations by specialty in terms of claims filed, costs to defend, and indemnity payouts. For example, General Practice and Family Medicine physicians had a large number of claims filed during the timeframe for this study (N=27,597) however compared to the other specialties the average indemnity payment ($164,094) and the average ALAE ($17,659) were on the lower end of the spectrum. Neurosurgery on the other hand had a relatively small number of claims by comparison (N=5,623), but the average indemnity payment ($315,487) and average ALAE ($27,068) were among the highest of the specialties included in this study. Average indemnity payments and average ALAE were strongly correlated with each other, r = 0.84, p < 0.01; while no significant correlation was seen between average ALAE and number of closed claims (r = 0.22, p = 0.28).
Figure 4.
Average ALAE vs. Average Indemnity Payout by Specialty
Table 3 shows this data in a slightly different way; looking specifically at total ALAE as a percent of indemnity payouts by specialty. Once again this percentage varies greatly by specialty. Pathology has the lowest percentage at 22%; or ALAE accounted for $0.22 for every dollar of indemnity paid out for this specialty. This is compared to oral surgery, which has the highest percent (112%). Obstetrics and Gynecologic Surgery, which has the highest number of claims reported during this time period, had total ALAE that equaled 25% of its total indemnity payouts.
Table 3.
Total ALAE as a Percent of Total Indemnity Payments By Specialty
| SPECIALTY | CLOSED CLAIMS | % ALAE to Indemnity |
|---|---|---|
| Anesthesiology | 9,239 | 27% |
| Cardiovascular and Thoracic Surgery | 7,291 | 41% |
| Cardiovascular Diseases - nonsurgical | 4,538 | 46% |
| Dermatology | 2,703 | 42% |
| Emergency Medicine | 4,357 | 43% |
| Gastroenterology | 2,516 | 46% |
| General and Family Practice | 27,597 | 34% |
| General Surgery | 25,012 | 32% |
| Gynecology | 2,842 | 38% |
| Internal Medicine | 32,688 | 40% |
| Neurology - nonsurgical | 3,832 | 39% |
| Neurosurgery | 5,623 | 30% |
| Obstetric and Gynecologic Surgery | 32,706 | 25% |
| Ophthalmology | 6,958 | 37% |
| Oral Surgery | 65 | 112% |
| Orthopedic Surgery | 22,562 | 40% |
| Other Nonsurgical Specialties | 2,398 | 42% |
| Otorhinolaryngology | 3,996 | 34% |
| Pathology | 1,686 | 22% |
| Pediatrics | 7,002 | 31% |
| Plastic Surgery | 8,921 | 54% |
| Psychiatry | 2,348 | 67% |
| Radiation Therapy | 2,327 | 26% |
| Radiology | 13,613 | 30% |
| Resident/Intern | 133 | 61% |
| Urologic Surgery | 5,797 | 36% |
DISCUSSION
Defense related expenses for medical malpractice claims are not insignificant. On average each claim will cost more than $27,000 to reach closure. Put a different way, for every ‘indemnity dollar’ paid out, an additional $0.33 is spent on defense expenses. The amount spent on defending claims has been increasing over time from a low of $13,395 (2008 dollar value) in 1985 to a high of $43,258 in 2008. This same general increase is seen regardless of adjudication status. As one might expect, however, those claims that go to trial are much more costly to defend than are those that are dropped, withdrawn or dismissed – almost 7 times more expensive. It is important to remember though that since the overwhelming majority of claims ultimately fall into this latter category, the total amount spent to defend claims that are dropped, withdrawn, or dismissed, far surpasses the total amount spent on claims that go to trial. An honest assessment must acknowledge the significant costs involved in addressing these claims; especially in defending the 64% of filed claims that were ultimate dropped, withdrawn, or dismissed. Further analysis regarding ALAE related to these dropped, withdrawn, or dismissed claims is certainly warranted, however limitations of the data set utilized for this study did not allow for it at this time.
In general, the majority of ALAE is used to pay defense attorney expenses (74%) while expert witness expenses and other expenses equally split the remaining 26%. However since 2005 a noticeable shift in expense allocation is seen in the data with more money being spent on expert witnesses and other expenses (42% in 2008). While we can make no definitive statements on the reason for this, several possible explanations for this shift away from defense attorney expenses including technology advancements employed during jury trials, utilization of mock trials and jury consultants, application of post judgment interest, increased court reporter costs, higher hourly rates for experts, and a greater use of experts per claim. It is also possible that laws passed by individual states in this time period may have influenced costs.
When looking at the data by medical specialty, a strong association exists between the average indemnity payment and the amount it costs to defend individual specialty claims. The prevalence of claims in a specialty, however, is not correlated with the cost to defend a claim, as those specialties with the most claims appear throughout the expense spectrum. The differences are not insignificant, though, as defending claims for neurosurgery or emergency medicine can be nearly twice as expensive as those resulting from general or family practice.
When those in the public eye discuss malpractice reform, the conversation seems to focus on the need to place caps on damage awards, the high number of frivolous claims that are “clogging” up the system, or the impact that defensive medicine practices by physicians are having on health care costs. From a physician’s perspective, however, the major issue is the cost of medical malpractice liability premiums. And from an insurer’s perspective, payout amounts and number of claims filed are not the only factor that determines premiums; the expenses incurred to defend a claim also play a major role in premium determination. Our data demonstrate that the cost of defending a claim has been steadily increasing over time regardless of adjudication status. Even the claims that are ultimately dropped, withdrawn, or dismissed result in defense expenses – $15,000 on average.
It is true that the most popular tort reforms may indirectly impact defense expenses by reducing the number of claims that are brought. However a recent study looking at the impact of popular tort reforms on defense expenses found that defense expenses were actually higher in those states where noneconomic damage caps, punitive damage limits, and attorney fee limits had been implemented (Ambrose and Carroll 2007). Therefore, it is not unreasonable for state and federal governments to consider other types of reforms that may impact defense expenses more directly. For example, some have advocated for adoption of a “loser pays” system to have a more direct impact on defense expenses. However, these types of reforms can make it more difficult for people with limited means who have cases with merit proceed. A “no fault” system that would compensate patients who experience an adverse result, whether or not the doctor, hospital or nurse was at fault, has also been proposed. Implementing reforms that aim for a pre-evaluation of the merits of a case, with the goal of identifying those cases that should be dropped or dismissed earlier, might also help to curb defense expenses. Additional reforms to consider include strict expert witness requirements (to ensure the competency and quality of MPL testimony), and “early offers” to expedite the closure of MPL claims.
The reasons for rising defense costs are not entirely clear and over the past several years a notable shift can been seen in the allocation of defense expense costs, with more money being spent on both expert witnesses and other expenses. Although it is currently unclear how best to address the issue of defense expenses, the issue should not be ignored, and should at least be a focus for interventions that aim to address the high cost the malpractice system.
Acknowledgements:
All data comes from the Physician Insurers Association of America (PIAA) Data Sharing Project, Rockville, MD 20850 but was analyzed independently by study authors. The authors especially thank Kwon Miller Data Analyst, for her assistance. This project was supported by grant number R03HS017572 from the Agency for Healthcare Research and Quality. The views expressed in this article are those of the authors and do not necessarily represent those of Indiana University or the Agency for Healthcare Research and Quality.
Contributor Information
Aaron E. Carroll, Associate Director for Research, an Associate Professor of Pediatrics in the Children’s Health Services Research Program at the Indiana University School of Medicine, and the Director of the Center for Health Policy and Professionalism Research. He completed a residency in Pediatrics at the University of Washington in Seattle and also completed a health services research fellowship in the Robert Wood Johnson Clinical Scholars Program. During that time he received his masters degree in Health Services..
Parul Divya Parikh, director of loss prevention and research with the Physician Insurers Association of America (PIAA). She received her masters in Public Health from John Hopkins Bloomberg School of Public Health.
Jennifer L. Buddenbaum, Associate Researcher in the Children’s Health Services Research Program at the Indiana University School of Medicine, and the Center Coordinator of the Center for Health Policy and Professionalism Research. She completed her masters degree in Health Administration at the University of Missouri-Columbia as well as a masters degree in Industrial-Organizational Psychology at Indiana University-Purdue University Indianapolis..
REFERENCES
- 1.Stolberg S, Pear R. Obama Open to Reining in Medical Suits. The New York Times June 15, 2009. [Google Scholar]
- 2.Herszenhorn DM, Pear R. Obama Offers to Use Some G.O.P. Health Proposals. New York Times March 3, 2010. [Google Scholar]
- 3.Annual Rate Survey Issue. Medical Liability Monitor 2009;34:1–39. [Google Scholar]
- 4.Sorrel AL. Liability premiums stay stable but insurers warn this might not last. American Medical News 2009;52. [Google Scholar]
- 5.Mello MM. Understanding medical malpractice insurance: A primer: The Robert Wood Johnson Foundation; 2006. [PubMed] [Google Scholar]
- 6.Hillman R Medical Malpractice Insurance: Multiple Factors Have Contributed to Increased Premium Rates. Report to Congressional Requesters; Washington, DC: GAO; 2003. June. [Google Scholar]
- 7.Karls CC. Introduction to MPL Insurance - Ratemaking and Reserves In: Introduction to MPLI Workshop; 2009; Las Vegas, NV: Physician Insurers Association of America; 2009. [Google Scholar]
- 8.Nathanson MJ. It’s the Economy (and Combined Ratio) Stupid: Examining the Medical Malpractice Litigation “Crisis” Myth and the Factors Critical to Reform. Penn State Law Review 2004;108.4:1077–112. [Google Scholar]
- 9.Sloan FA, Shadle JH. Is there empirical evidence for “Defensive Medicine”? A reassessment. Journal of Health Economics 2009;28:481–91. [DOI] [PubMed] [Google Scholar]
- 10.Black B, Hyman DA, Silver C, Sage WM. Defense Costs and Insurer Reserves in Medical Malpractice and OTher Personal Injury Cases: Evidence from Texas, 1988–2004. American Law and Economics Review 2008;10:185–245. [Google Scholar]
- 11.Insurance Information Institute. The Insurance Fact Book 2010. New York, NY: The Institute; 2010. [Google Scholar]
- 12.Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med 2006;354:2024–33. [DOI] [PubMed] [Google Scholar]
- 13.Cohen TH, Huges KA. Medical Malpractice Insurance Claims in Seven States. Washington DC: Bureau of Justice Statistics; 2007. [Google Scholar]
- 14.Vidmar N, Lee P, MacKillop K, McCarthy K, McGwin G. Seeking the “Invisible” Profile of Medical Malpractice Litigation: Insights from Florida. DePaul Law Review 2005;54:315–56. [Google Scholar]
- 15.The Case For Medical Liability Reform. (Accessed March 17, 2010, at http://www.ama-assn.org/ama/pub/advocacy/current-topics-advocacy/practice-management/medical-liability-reform.shtml.)
- 16.Physician Insurers Association of America. (Accessed March 17, 2010, at www.piaa.us.)
- 17.Physician Insurers Association of America. Medical Professional Liability Insurance: A Practitioner’s Primer. Rockville, MD: The Association; 2001. [Google Scholar]