Abstract
Femoroacetabular impingement describes a pathologic interaction between the bony femoral head/neck junction and acetabulum. Cam-type femoroacetabular impingement results from an aspherical femoral head architecture, which increases early contact along the acetabular surface during hip range of motion. Errant arthroscopic femoroplasty recently has been discussed within the literature to describe a preventable etiology of failed hip arthroscopy, most notably cam over- and under-resection. We present an arthroscopic surgical technique for achieving the perfectly spherical femoroplasty, meant to minimize complications and improve postoperative outcomes.
Femoroacetabular impingement (FAI) is an increasingly understood cause of anterior groin pain. This condition describes a pathologic interaction between the femoral head/neck junction and acetabulum due to abnormal bony morphology. Cam morphology (defined as an alpha angle of >55°)1,2 of the femoral head/neck junction, a type of FAI, results from an aspherical femoral head architecture, which increases early contact along the acetabular surface during hip flexion and rotation. Increased frictional contact between these structures can lead to injuries of the chondrolabral junction. Repetitive injury, left symptomatic and untreated, can in turn predispose patients to irreversible chondrolabral degeneration.3 Early degeneration causing symptomatic pain can lead to osteoarthritis and ultimately early total hip arthroplasty.4,5 In an effort to curtail and delay this pathologic sequence of events, recent literature has focused on early recognition and intervention of symptomatic FAI.
Varying ways to surgically manage cam-type FAI have been published previously.6 Cam-type FAI was first addressed with open surgical dislocation; however, more recently hip arthroscopy has been used as a minimally invasive method for achieving clinical improvement with decreased morbidity, equivalent or better patient-reported outcomes, and return to sport or function.7,8 Arthroscopic femoroplasty aims to sculpt the femoral head in ideally a perfectly spherical contour, thereby providing relief of mechanical symptoms previously unresponsive to conservative, nonoperative measures. Errant femoroplasty has recently been discussed within the literature to describe a preventable etiology of failed hip arthroscopy, most notably cam over- and under-resection. In fact, the most common etiology of revision hip arthroscopy is residual cam lesions due to under-resection.9,10 Over-resection, although not as common as its counterpart, has much graver consequences. Aggressive resection has been documented to cause inferior clinical outcomes,11 negatively affect hip joint biomechanics,12 predispose to femoral neck fractures,13, 14, 15 and produce a high conversion rate to total hip arthroplasty.11 We present an arthroscopic surgical technique for achieving the perfectly spherical femoroplasty, meant to minimize complications using fluoroscopic guidance to confirm accuracy of resection, and ultimately improve postoperative patient outcomes.11 Advantages, risks, and limitations for arthroscopic spherical femoroplasty are noted in Table 1.11,16
Table 1.
| Advantages | Risks | Limitations |
|---|---|---|
|
|
|
FAI, femoroacetabular impingement.
This study was performed in accordance with the ethical standards in the 1964 Declaration of Helsinki. This study was carried out in accordance with relevant regulations of the US Health Insurance Portability and Accountability Act. Details that might disclose the identity of the subjects under study have been omitted. This study was approved by the institutional research board (ID: 5276).
Step-by-Step Surgical Technique (With Video Illustration)
Video 1 explains the spherical femoroplasty technique in detail. Clockface values for the identified head/neck junction are based on the study by Ross et al.17
Part A. Patient Preparation, Positioning, and Portal Placement
General anesthesia and full muscle relaxation of the operative extremity are essential for manipulation and accurate cam resection; verify with the anesthesiologist that this is optimized before the start of the case. Place the patient in the modified supine position on a traction table (Supine Hip Positioning System, Smith & Nephew, Andover, MA) with a well-padded wide perineal post. Abut the medial thigh of the operative extremity to provide patient stability as well as a lateralizing force vector along the femoral head, which will aid in arthroscopic visualization of the central compartment.
Place the patient in the 10° to 15° Trendelenburg position. This position harnesses the gravitational force and helps decrease pressure along the perineum, therefore minimizing potential traction-related complications such as pudendal nerve neuropathy or tissue necrosis.18
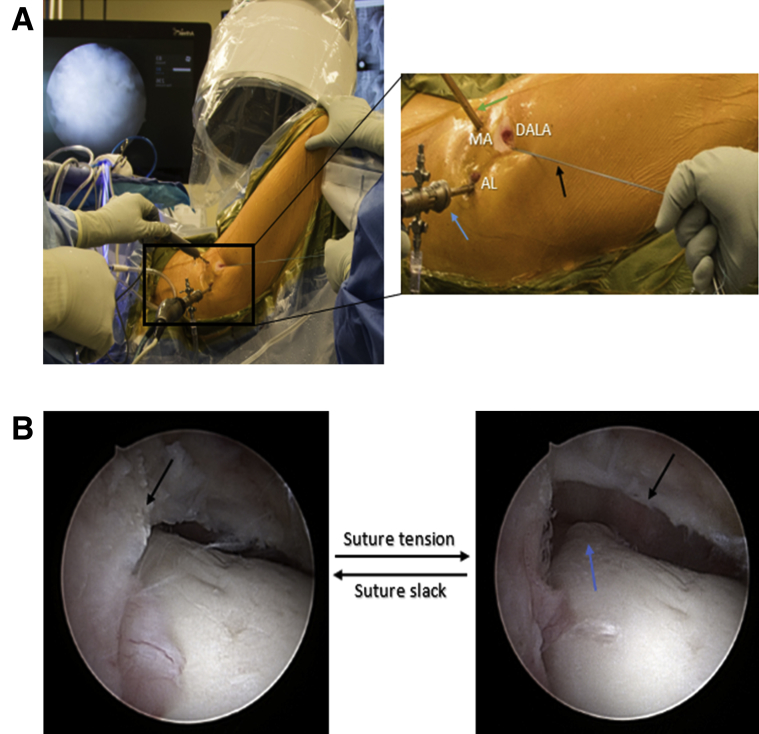
Once the patient is secured: (1) Apply manual bilateral traction simultaneously to achieve full contact between the perineum and the padded post; and (2) adduct, slightly flex, and apply slight 5° to 10° of internal rotation to the operative extremity. Using a 70° arthroscope, access the hip joint via anterolateral (AL), mid-anterior (MA), distal anterolateral accessory (DALA), as well as posterolateral portals if needed for labral reconstruction (Fig 1A).19,20
Fig 1.
(A) Right hip in a patient in the modified supine position with the hip in neutral flexion, the head toward the left and feet to the right during intraarticular joint access. The AL, MA, and DALA portals are shown. The 70° arthroscope (blue arrow) is placed in the AL portal, working instrument (green arrow) in the MA portal and a traction suture (black arrow) in the DALA portal. (B) An arthroscopic view of the right femoral head/neck junction and capsule (black arrow) Because T-capsulotomies are not routinely done, a traction suture is placed within the inferior capsule leaflet. As an assistant adds traction on a clamped suture, greater intracapsular exposure is achieved and visualization of the joint is improved, revealing the cam deformity (blue arrow). Note: this is a crucial step, as it allows for improved visualization to fully assess the peripheral compartment. (AL, anterolateral; DALA, distal anterolateral accessory; MA, mid-anterior.)
Part B. Capsulotomy
Perform an interportal capsulotomy between the AL and MA portals.
Part C. Diagnostic Arthroscopy, Central Compartment Management
Although beyond the scope of this article, the presence of other abnormalities commonly seen with FAI should be systematically identified, classified, and treated with grading schemes and treatment algorithms previously described.21,22 Other abnormalities you may encounter and address include ligamentum teres and labral tears, loose bodies, acetabular cartilage damage, and uncommon extra-articular lesions.
Part D. Spherical Femoroplasty Setup Within the Peripheral Compartment
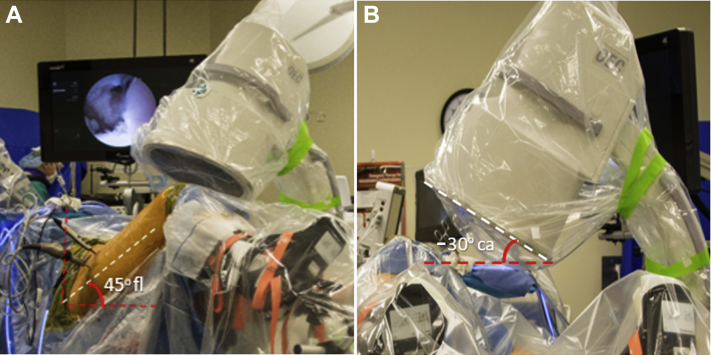
Provided a spherical femoroplasty is indicated (Table 2), position the operative hip in 45° of flexion, neutral foot rotation, and remove the perineal post (Fig 1A). Place a draped, sterile C-arm fluoroscopy on the nonoperative side of the patient at 0° tilt, –30° cantilever. Then, position the 70° arthroscope within the AL portal through a 5.0-mm cannula (Fig 1A). This improves visualization and helps to increase pump inflow in the peripheral compartment, which in turn with constant outflow helps to decrease the occurrence of postoperative heterotopic ossification.23,24
Table 2.
Indications and Contraindications of Arthroscopic Spherical Femoroplasty Technique
| Indications | Contraindications |
|---|---|
|
|
FAI, femoroacetabular impingement.
For enhanced visualization, place a nonabsorbable FiberWire traction suture (Arthrex, Naples, FL) within the inferior leaflet of the capsule exiting the DALA portal (Fig 1). A T-capsulotomy is not routinely performed, which is why the use of a traction stitch is employed (Fig 1B). Avoiding T-capsulotomy can help prevent iatrogenic instability.25, 26, 27 A stitch is used over absorbable sutures as the latter do not have the strength to support the traction.
Spherical Femoroplasty Technique: Six-Pronged Approach
Table 3 summarizes the operative extremity and C-arm positions along with the region identified on the femoral head/neck junction for cam resection.
Table 3.
Six Positions of the Hip and C-arm to Confirm Full Accuracy of Resection
| Hip Position | C-Arm Position | Anatomical Zone of Head/Neck Junction (Clockface Value∗) |
|---|---|---|
| 45° Flexion, 0° rotation | 0° tilt, cantilever –30° | Anterolateral zone (12:30-1:30) |
| 60° Flexion, 30° external rotation, 25° adduction | 0° tilt, cantilever –30° | Anteromedial zone A (1:30-2:30) |
| 60° Flexion, 60° external rotation, 25° adduction | 0° tilt, cantilever –30° | Anteromedial zone B (2:30-3:30) |
| 0° Flexion, 0° rotation (neutral rotation) | 0° tilt, cantilever –10° | Lateral zone (11:30-12:30) |
| 0° Flexion, 0° rotation (neutral rotation) | 0° tilt, cantilever 0° | Posterolateral zone (10:30-11:30) |
| 0° Flexion, 30° internal rotation +/– limb traction | 0° tilt, cantilever 0° | Further posterolateral/ posterosuperior (+limb traction) zone (9:30-10:30) |
Clockface values based on the study of Ross et al.17
Position 1. Anterolateral Zone: 12:30-1:30
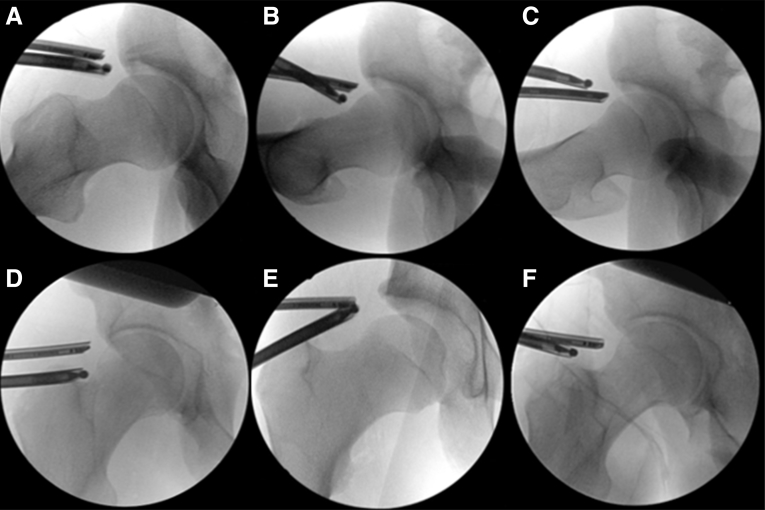
A modified Dunn lateral view (Fig 2A) of the hip is achieved with bringing the hip to 45° of flexion (Fig 3A). The C-arm remains at a 0° tilt, –30° cantilever (Fig 3B), allowing for excellent visualization of the anterolateral aspect of the femoral head/neck junction.
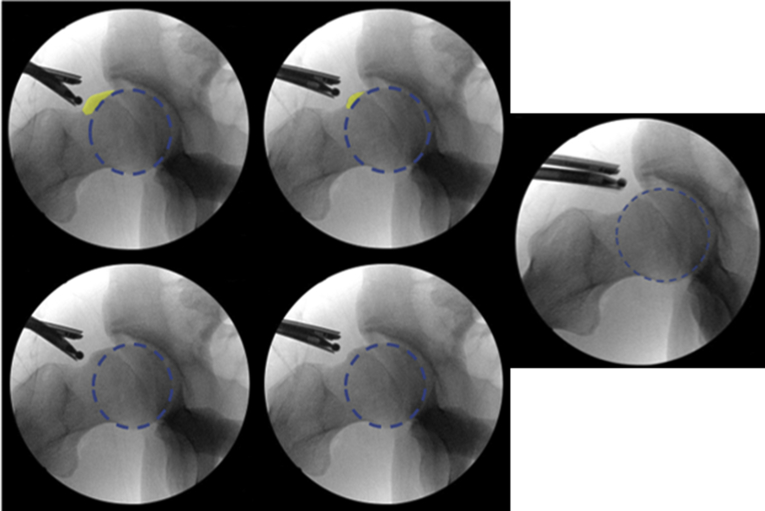
Fig 2.
Postoperative fluoroscopic views of the right hip taken at the 6 corresponding patient operative extremity and C-arm positions (Table 3), producing the 6 anatomical regions of the head/neck junction. (A) Anterolateral zone (12:30-1:30). (B) Anteromedial zone A (1:30-2:30). (C) Anteromedial zone B (2:30-3:30). (D) Lateral zone (11:30-12:30). (E) Posterolateral zone (10:30-11:30). (F) Further posterolateral/ posterosuperior (+limb traction) zone (9:30-10:30).
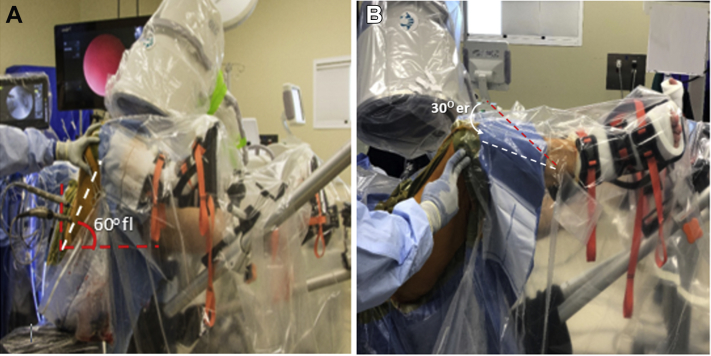
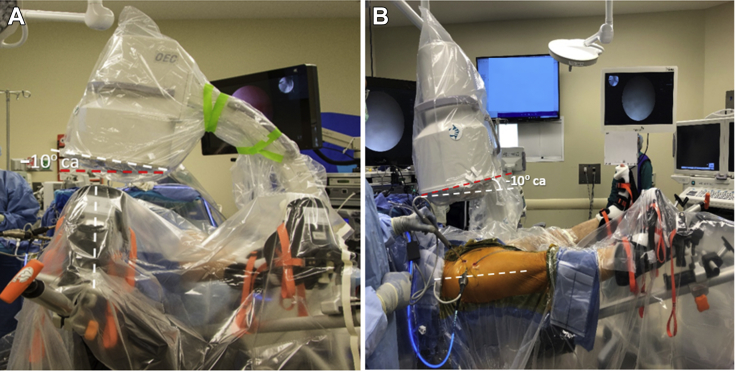
Fig 3.
Position 1. Patient operative extremity and corresponding C-arm positioning needed to isolate the anterolateral zone (12:30-1:30) of the head/neck region during the 6-pronged approach femoroplasty. The patient is in a modified supine position with the head toward the left and feet to the right. The angle of the C-arm is shown in reference to the mayo stand as horizontal. (A) operative hip is in 45° flexion; (B) C-arm is set to 0°, −30° cantilever. (ca, cantilever; fl, flexion.)
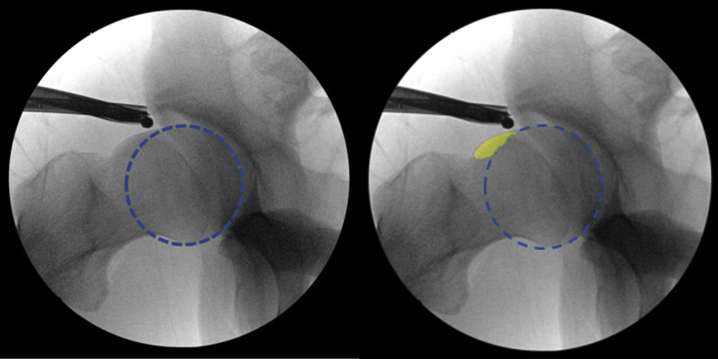
The most proximal extent of the osteoplasty is marked via electrocautery (Fig 4). Then, remove the periosteum from the marked region using a radiofrequency ablation device (Smith & Nephew) within the MA portal (Fig 5). The placement of the radiofrequency ablation device is based on the measured resection level needed to optimize alpha angle. The AL viewing portal provides excellent visualization of the femoral head/neck junction, both medially and laterally.
Fig 4.
Starting fluoroscopic Dunn view image of the anterolateral femoral head/neck junction of the right hip. Proximal extent of the cam lesion (highlighted) is identified.
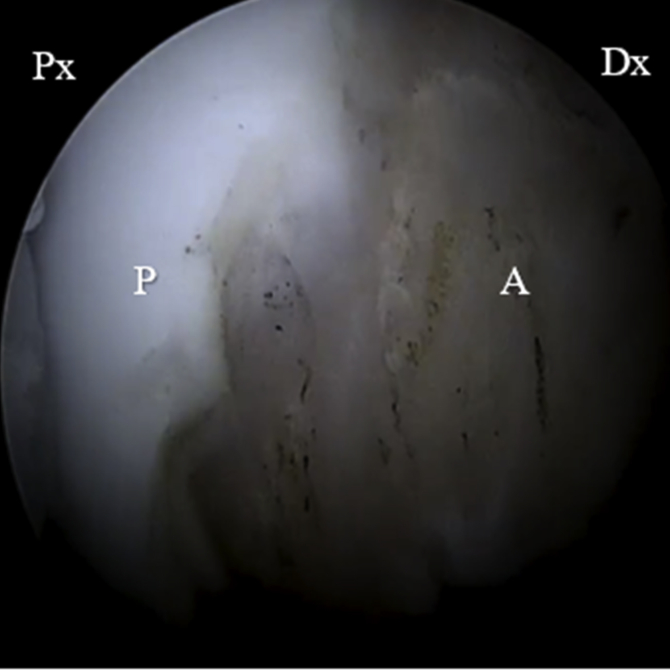
Fig 5.
View from the anterolateral portal of the right hip with a 70° arthroscope. Note the removal of the periosteum from the surface of the femoral head. (A, ablated area; Dx, distal; P, periosteum; Px, proximal.)
Use a 5.5-mm arthroscopic round burr to begin the femoral resection level, starting distally and working proximally (Fig 6). Care should be taken to remove more bone distally than proximally (Fig 7). This technique helps maintain convexity of the head/neck junction, improves the offset ratio, and prevents errant over-resection.21 The same process is followed for the next 5 positions.
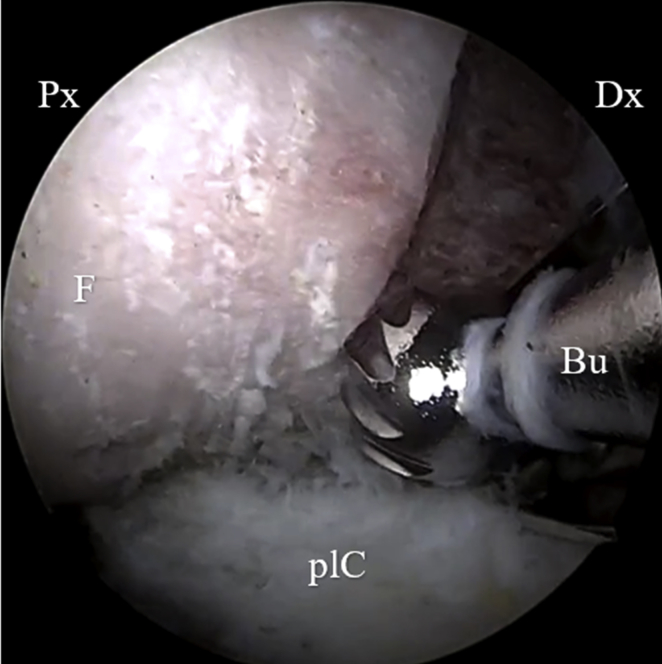
Fig 6.
View from the anterolateral portal of the right hip with a 70° arthroscope. Note marked resection level starting distal along anterolateral femoral head/neck junction, to improve offset ratio as well as resect cam lesion. (Bu, burr; F, femoral head; Dx, distal; plC, posterolateral capsule; Px, proximal.)
Fig 7.
Dunn view of the anterolateral zone (12:30-1:30) of the femoral head/neck region (position 1) of the right hip showing gradual resection of the cam lesion distally to proximally. The femoral head/neck junction has been recontoured with the cam lesion fully resected. Note: Extreme care was taken to avoid over-resection of the head/neck junction by maintaining convexity.
Position 2. Anteromedial Zone A: 1:30-2:30
Place the operative extremity into 60° of flexion, 30° of external rotation, and 25° of adduction (Fig 8A). Keep the C-arm at a 0° tilt, –30° cantilever (Fig 8B). This allows for excellent visualization of the anteromedial aspect of the femoral head/neck junction (Fig 2B).
Fig 8.
Position 2. Patient operative extremity and corresponding C-arm positioning needed to isolate the snteromedial zone A (1:30-2:30) of the head/neck region during the 6-pronged approach femoroplasty. The patient is in a modified supine position with the head toward the left and feet to the right. The angle of the C-arm is shown in reference to the mayo stand as horizontal. (A-B) Operative hip is in 60° flexion, 30° external rotation, 25° adduction. The C-arm remains at 0° tilt, −30° cantilever. cantilever. Again, C-arm tilt is added to correct for Trendelenburg. (er, external rotation; fl, flexion.)
Position 3. Anteromedial Zone B: 2:30-3:30
Place the operative extremity into 60° of flexion, 60° of external rotation, and 25° of adduction (Fig 9). Keep the C-arm at a 0° tilt, –30° cantilever. This allows for extended visualization of the anteromedial aspect of the femoral head/neck junction (Fig 2C).
Fig 9.

Position 3. Patient operative extremity and corresponding C-arm positioning needed to isolate the snteromedial zone B (2:30-3:30) of the head/neck region during the 6-pronged approach femoroplasty. The patient is in a modified supine position with the head toward the left and feet to the right. The angle of the C-arm is shown in reference to the mayo stand as horizontal. Operative hip is in 60° flexion, 60° external rotation, 25° adduction. The C-arm remains at 0° tilt, −30° cantilever. cantilever. Again, C-arm tilt is added to correct for Trendelenburg. (ca, cantilever; er, external rotation.)
Position 4. Lateral Zone: 11:30-12:30
Place the operative extremity into 0° of flexion and 0° of rotation (neutral position, Fig 10A). Place the C-arm at a 0° tilt, –10° cantilever (Fig 10B). This allows for excellent visualization of the lateral aspect of the femoral head/neck junction (Fig 2D).
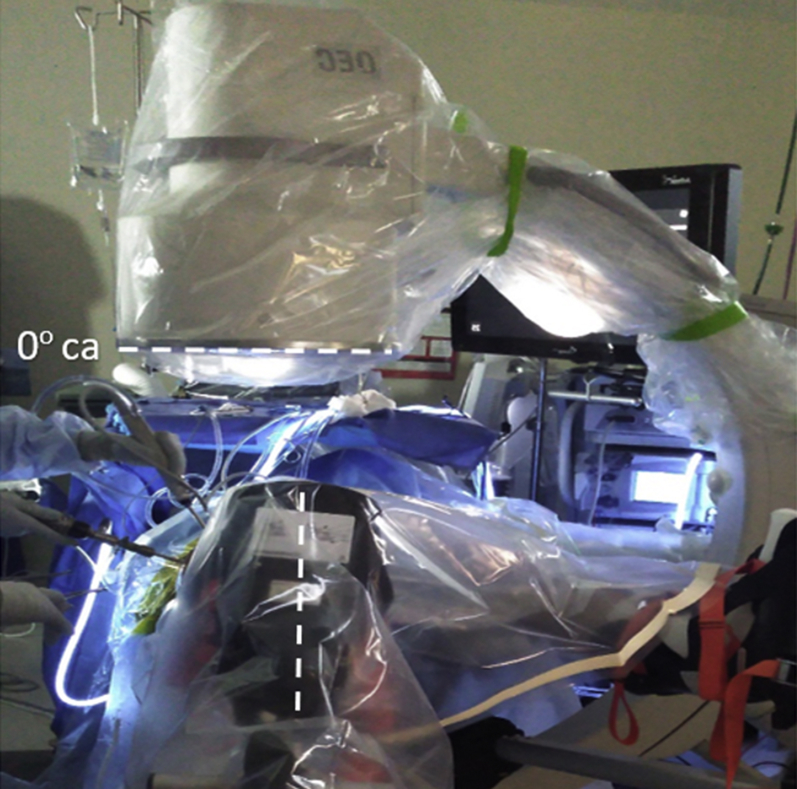
Fig 10.
Position 4. Patient operative extremity and corresponding C-arm positioning needed to isolate the lateral zone (11:30-12:30) of the head/neck region during the 6-pronged approach femoroplasty. The patient is in a modified supine position with the head toward the left and feet to the right. The angle of the C-arm is shown in reference to the mayo stand as horizontal. (A) Operative hip is in 0o flexion, 0o rotation (neutral position); (B) The C-arm is set to 0° tilt, −10° cantilever. Note: the patient is intentionally placed in Trendelenburg to minimize perineal pressure.17 Sometimes, C-arm tilt is added to correct for this (dotted lines). (ca, cantilever.)
Position 5. Posterolateral Zone: 10:30-11:30
Keep the operative extremity into 0° of flexion and 0° of rotation (neutral position, Fig 11). Place the C-arm at a 0° tilt, 0° cantilever. This allows for visualization of the posterolateral aspect of the femoral head/neck junction (Fig 2E).
Fig 11.
Position 5. Patient operative extremity and corresponding C-arm positioning needed to isolate the posterolateral zone (10:30-11:30) of the head/neck region during the 6-pronged approach femoroplasty. The patient is in a modified supine position with the head toward the left and feet to the right. The angle of the C-arm is shown in reference to the mayo stand as horizontal. Operative hip remains in 0° flexion and 0° rotation (neutral position). The C-arm is set to 0° tilt, 0° cantilever. (ca, cantilever.)
Position 6. Posterolateral Zone and Beyond: 9:30-10:30
Place the operative extremity into 0° of flexion and 30° of internal rotation (Fig 12). Keep the C-arm at a 0° tilt, 0° cantilever. Added internal rotation allows for greater posterolateral exposure. If needed, limb traction is required to address the most posterosuperior area of cam morphology (Fig 2F).
Fig 12.
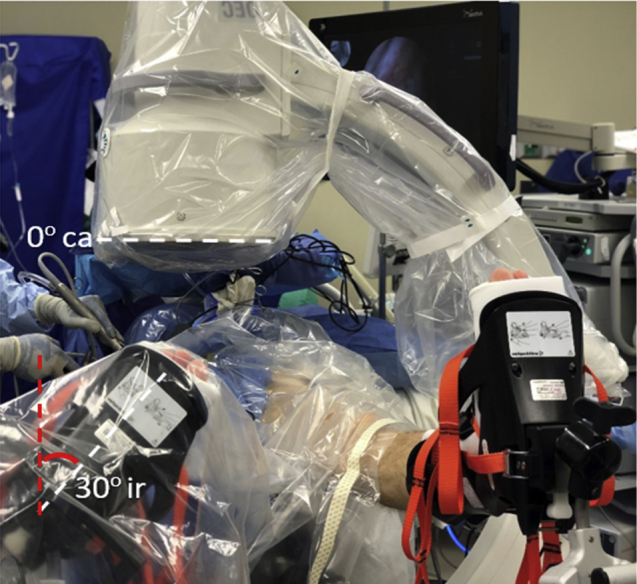
Position 6. Patient operative extremity and corresponding C-arm positioning needed to isolate further posterolaterally/posterosuperior zone (9:30-10:30) of the head/neck region during the 6-pronged approach femoroplasty. The patient is in a modified supine position with the head toward the left and feet to the right. The angle of the C-arm is shown in reference to the mayo stand as horizontal. Operative hip is in 0° flexion, 30° internal rotation to target the head/neck region further posterolaterally. Traction is added to target the posterosuperior region. The C-arm remains at 0° tilt, 0° cantilever. (ca, cantilever; ir, internal rotation.)
Inspection and Closure
To ensure full resection of the cam lesion, complete a dynamic examination of the joint and capture final fluoroscopic images of the operative extremity to show accurate resection of cam deformity, restoration of the femoral head/neck junction, and avoidance of over/under-resection. (Fig 8).
Capsular Management
If there is joint instability present as indicated by preoperative and intraoperative criteria28,29 capsular plication is performed. If no joint instability is present, capsulorrhaphy is performed. The capsule may be left open in select cases. Table 4 shows the pearls and pitfalls of the procedure.
Table 4.
Pearls and Pitfalls of Arthroscopic Femoroplasty for Cam-Type Femoroacetabular Impingement
| Pearls | Pitfalls |
|---|---|
|
|
Postoperative Rehabilitation
The patient is placed in a brace (X-Act ROM Hip Brace; Donjoy, Vista, CA) for 2 weeks. Use of crutches is encouraged for 2 weeks with weight-bearing restriction of up to 20 pounds foot-flat weight bearing. Under physiotherapist supervision, active range-of-motion exercise is initiated during the first 48 hours with continuous passive motion and/or static bicycle. Formal physical therapy protocol is begun immediately postoperatively.
Discussion
The goal of arthroscopic hip femoroplasty is to correct the anatomy of the femoral head/neck junction to restore and maintain the physiologic contact between the femoral head and native acetabular labrum, which confers inherent stability of the joint. When this contact is interrupted, the joint may become more susceptible to hip instability, labral tears, and chondrolabral delamination, thus predisposing it to developing arthritis.30,31 Therefore, it becomes essential to correct the aberrant femoral head/neck offset to prevent these future complications. To date, there is a paucity of literature describing patient outcomes solely attributed to management of cam-type FAI. This is likely because cam lesions are usually present with additional central compartment pathology, such as chondrolabral damage, and thus the effects of femoroplasty are difficult to isolate. Instead, many studies have focused on results of hip arthroscopy overall, including patient indications and complications.32,33
Previous studies have identified residual cam deformity and unaddressed FAI to be the most common etiology for revision hip arthroscopy. Philippon et al.34 published a case series that included 37 revision hip arthroscopy procedures, performed 20.5 months after index procedure. The main cause of persistent hip pain in 95% of procedures was under-resected cam lesions and unresolved FAI. It has been proposed that the increasing prevalence of under-resection is a result of surgeons erring on the side of caution in fear of over-resection, and its irreversible complications. However, it is important to note that clinical outcomes for correction of residual cam with revision arthroscopy may not be equivalent to primary treatment. Larson et al.35 published a study on a cohort of 237 cases in which 85 had residual FAI, and the authors showed that although revision hip arthroscopy improved patient outcomes, they were inferior to patients with primary FAI correction. Nonetheless, the consensus in hip arthroscopy is to be cautious rather than overzealous regarding cam resection.
Over-resection is a much more devastating complication of aggressive cam deformity decompression. One major concern is femoral neck fractures due to weakening of the tension side of bone, however, weight-bearing protocols have made this a rarity. More commonly, excessive femoral resection has led to disruption of the native labral seal, adversely affecting hip joint biomechanics.36 Mansor et al.11 reviewed a cohort of 120 patients (130 hips) and divided them into 3 groups (over-resected, under-resected, and neutral resected) who had a mean follow-up from index procedure of 39.6 months. The authors found that over-resection greater than 5% of the femoral head diameter correlated with inferior clinical outcomes (modified Harris Hip Score) compared with the under-resected population. Furthermore, over-resection predicted inferior outcomes after revision hip arthroscopy and led to greater rates of conversion to total hip arthroplasty (30% vs 0% in the under-resected population), the final endpoint of a failed arthroscopic hip procedure. Clearly, over-resection is a complication that is irreversible with severe consequences. Yet, this complication is avoidable using proper caution and excellent surgical technique.
Conclusions
The technique for achieving a perfectly spherical femoroplasty requires a steep learning curve, but, when mastered, is a powerful tool that aims to achieve precise and accurate resection at the femoral head/neck junction. The method described here is a reproducible sculpting technique of treating cam-type FAI, which minimizes complications of over- or under-resection in an effort to improve hip biomechanics. This technique will likely lead to improved clinical results in patients undergoing arthroscopic femoral osteoplasty.
Footnotes
The authors report the following potential conflict of interest or source of funding: B.G.D., or a member of his immediate family, has or may receive payments or benefits, during the study period, an amount of USD 10,000-USD 100,000 from Arthrex; an amount of USD 10,000-USD 100,000 from DJO Global; an amount of USD 10,000-USD 100,000 from Medacta International; an amount of less than USD 10,000 from Orthomerica Products; an amount of less than USD 10,000 from Pacira Pharmaceuticals; an amount of less than USD 10,000 from Medwest Associates; an amount of less than USD 10,000 from Prime Surgical; an amount of less than USD 10,000 from Trice Medical; an amount of less than USD 10,000 from Smith & Nephew; and an amount of USD 100,001–USD 1,000,000 from Stryker. A.C.L., or a member of his immediate family, has or may receive payments or benefits, during the study period, an amount of USD 10,000-USD 100,000 from Arthrex; an amount of less than USD 10,000 from Medwest Associates; an amount of USD 10,000-USD 100,000 from Smith & Nephew; an amount of less than USD 10,000 from Stryker; and an amount of less than USD 10,000 from Zimmer Biomet Holdings. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
This study was performed at the American Hip Institute, Des Plaines, Illinois, U.S.A.
Supplementary Data
Technique for achieving a perfectly spherical femoroplasty during hip arthroscopy in a patient’s right hip. The patient is placed in a supine position with Trendelenburg. Position 1 is with the hip flexed at 45° with neutral rotation applied. The modified Dunn view is achieved with a 0° tilt and –30° cantilever to the C-arm. Under fluoroscopic guidance, work is done at the inferior most head/neck junction proximally, with an effort to maintain convexity to the femoral head. Care is taken to avoid concavity, which would disrupt the labral seal. For position 2, the operative extremity is brought into 60° of flexion with 30° external rotation and 25° adduction applied. The C-arm maintains its position, providing more medial exposure to the head/neck junction. Once work is completed in position 2, 30° further external rotation is applied to the extremity, totaling 60°, again, providing even more medial exposure to the head/neck junction. Next, position 4 is achieved with the operative extremity brought into full extension and neutral rotation. The C-arm is brought to –10° cantilever. This provides posterolateral exposure to the femoral head/neck junction. Work is done in this region, again, with direct visualization fluoroscopic guidance with a goal to maintain convexity at all times. For position 5, the C-arm is brought into neutral (0°) cantilever. At certain points, traction can be applied to work on the most proximal aspect of the noted cam lesion. Lastly, in position 6, the operative extremity is brought into 30o internal rotation, which provides further posterolateral exposure. Once the perfectly spherical femoroplasty is completed, traction is removed, the hip is flexed, and a dynamic impingement test is performed by alternating the operative extremity from positions 1 and 2. Before progressing to capsular management, it is ensured that the labral seal is maintained.
References
- 1.Mannava S., Geeslin A.G., Frangiamore S.J. Comprehensive clinical evaluation of femoroacetabular impingement: Part 2, plain radiography. Arthrosc Tech. 2017;6:e2003–e2009. doi: 10.1016/j.eats.2017.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de SA D., Urquhart N., Philippon M., Ye J.-E., Simunovic N., Ayeni O.R. Alpha angle correction in femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2014;22:812–821. doi: 10.1007/s00167-013-2678-6. [DOI] [PubMed] [Google Scholar]
- 3.Ito K., Minka M.A., Leunig M., Werlen S., Ganz R., Femoroacetabular impingement and the cam-effect An MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83:171–176. doi: 10.1302/0301-620x.83b2.11092. [DOI] [PubMed] [Google Scholar]
- 4.Kuhns B.D., Weber A.E., Levy D.M., Wuerz T.H. The natural history of femoroacetabular impingement. Front Surg. 2015;2:58. doi: 10.3389/fsurg.2015.00058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ganz R., Parvizi J., Beck M., Leunig M., Nötzli H., Siebenrock K.A. Femoroacetabular impingement: A cause for osteoarthritis of the hip. Clin Orthop. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 6.Botser I.B., Jackson T.J., Smith T.W., Leonard J.P., Stake C.E., Domb B.G. Open surgical dislocation versus arthroscopic treatment of femoroacetabular impingement. Am J Orthop (Belle Mead NJ) 2014;43:209–214. [PubMed] [Google Scholar]
- 7.Aoki S.K., Beckmann J.T., Wylie J.D. Arthroscopic femoral osteochondroplasty for cam-type femoroacetabular impingement: The trough technique. Arthrosc Tech. 2016;5:e743–e749. doi: 10.1016/j.eats.2016.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Domb B.G., Dunne K.F., Martin T.J. Patient reported outcomes for patients who returned to sport compared with those who did not after hip arthroscopy: Minimum 2-year follow-up. J Hip Preserv Surg. 2016;3:124–131. doi: 10.1093/jhps/hnv078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cvetanovich G.L., Harris J.D., Erickson B.J., Bach B.R., Bush-Joseph C.A., Nho S.J. Revision hip arthroscopy: A systematic review of diagnoses, operative findings, and outcomes. Arthroscopy. 2015;31:1382–1390. doi: 10.1016/j.arthro.2014.12.027. [DOI] [PubMed] [Google Scholar]
- 10.Gwathmey F.W., Jones K.S., Thomas Byrd J.W. Revision hip arthroscopy: Findings and outcomes. J Hip Preserv Surg. 2017;4:318–323. doi: 10.1093/jhps/hnx014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mansor Y., Perets I., Close M.R., Mu B.H., Domb B.G. In search of the spherical femoroplasty: Cam overresection leads to inferior functional scores before and after revision hip arthroscopic surgery. Am J Sports Med. 2018;46:2061–2071. doi: 10.1177/0363546518779064. [DOI] [PubMed] [Google Scholar]
- 12.Wijdicks C.A., Balldin B.C., Jansson K.S., Stull J.D., LaPrade R.F., Philippon M.J. Cam lesion femoral osteoplasty: In vitro biomechanical evaluation of iatrogenic femoral cortical notching and risk of neck fracture. Arthroscopy. 2013;29:1608–1614. doi: 10.1016/j.arthro.2013.06.021. [DOI] [PubMed] [Google Scholar]
- 13.Horner N.S., Khanduja V., MacDonald A.E., Naendrup J.-H., Simunovic N., Ayeni O.R. Femoral neck fractures as a complication of hip arthroscopy: A systematic review. J Hip Preserv Surg. 2017;4:9–17. doi: 10.1093/jhps/hnw048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ilizaliturri V.M. Complications of arthroscopic femoroacetabular impingement treatment: A review. Clin Orthop. 2009;467:760–768. doi: 10.1007/s11999-008-0618-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Merz M.K., Christoforetti J.J., Domb B.G. Femoral neck fracture after arthroscopic femoroplasty of the hip. Orthopedics. 2015;38:e696–700. doi: 10.3928/01477447-20150804-57. [DOI] [PubMed] [Google Scholar]
- 16.Byrd J.W.T., Jones K.S. Arthroscopic femoroplasty in the management of cam-type femoroacetabular impingement. Clin Orthop. 2009;467:739–746. doi: 10.1007/s11999-008-0659-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ross J.R., Bedi A., Stone R.M. Intraoperative fluoroscopic imaging to treat cam deformities: Correlation with 3-dimensional computed tomography. Am J Sports Med. 2014;42:1370–1376. doi: 10.1177/0363546514529515. [DOI] [PubMed] [Google Scholar]
- 18.Lall A.C., Saadat A.A., Battaglia M.R., Maldonado D.R., Perets I., Domb B.G. Perineal pressure during hip arthroscopy is reduced by use of Trendelenburg: A prospective study with randomized order of positioning. Clin Orthop. 2019;477:1851–1857. doi: 10.1097/CORR.0000000000000804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Domb B., Hanypsiak B., Botser I. Labral penetration rate in a consecutive series of 300 hip arthroscopies. Am J Sports Med. 2012;40:864–869. doi: 10.1177/0363546512437152. [DOI] [PubMed] [Google Scholar]
- 20.Maldonado D.R., LaReau J.M., Lall A.C., Battaglia M.R., Mohr M.R., Domb B.G. Concomitant arthroscopy with labral reconstruction and periacetabular osteotomy for hip dysplasia. Arthrosc Tech. 2018;7:e1141–e1147. doi: 10.1016/j.eats.2018.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jackson T.J., Stake C.E., Trenga A.P., Morgan J., Domb B.G. Arthroscopic technique for treatment of femoroacetabular impingement. Arthrosc Tech. 2013;2:e55–e59. doi: 10.1016/j.eats.2012.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Suarez-Ahedo C., Gui C., Rabe S.M., Chandrasekaran S., Lodhia P., Domb B.G. Acetabular chondral lesions in hip arthroscopy: Relationships Between grade, topography, and demographics. Am J Sports Med. 2017 doi: 10.1177/0363546517708192. 363546517708192. [DOI] [PubMed] [Google Scholar]
- 23.Gao G.-Y., Zhang X., Dai L.-H. Heterotopic ossification after arthroscopy for hip impingement syndrome. Chin Med J (Engl) 2019;132:827–833. doi: 10.1097/CM9.0000000000000153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Redmond J.M., Keegan M.A., Gupta A., Worsham J.R., Hammarstedt J.E., Domb B.G. Outcomes of heterotopic ossification excision following revision hip arthroscopy. J Hip Preserv Surg. 2017;4:164–169. doi: 10.1093/jhps/hnx010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Camp C.L., Reardon P.J., Levy B.A., Krych A.J. Creating and closing the T-capsulotomy for improved visualization during arthroscopic treatment of femoroacetabular impingement. Arthrosc Tech. 2015;4:e731–e735. doi: 10.1016/j.eats.2015.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Forster-Horvath C., Domb B.G., Ashberg L., Herzog R.F. A method for capsular management and avoidance of iatrogenic instability: Minimally invasive capsulotomy in hip arthroscopy. Arthrosc Tech. 2017;6:e397–e400. doi: 10.1016/j.eats.2016.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Levy D.M., Grzybowski J., Salata M.J., Mather R.C., Aoki S.K., Nho S.J. Capsular Plication for treatment of iatrogenic hip instability. Arthrosc Tech. 2015;4:e625–e630. doi: 10.1016/j.eats.2015.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chandrasekaran S., Vemula S.P., Martin T.J., Suarez-Ahedo C., Lodhia P., Domb B.G. Arthroscopic technique of capsular plication for the treatment of hip instability. Arthrosc Tech. 2015;4:e163–e167. doi: 10.1016/j.eats.2015.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maldonado D.R., Perets I., Mu B.H. Arthroscopic capsular plication in patients with labral tears and borderline dysplasia of the hip: Analysis of risk factors for failure. Am J Sports Med. 2018;46:3446–3453. doi: 10.1177/0363546518808033. [DOI] [PubMed] [Google Scholar]
- 30.Canham C.D., Yen Y.-M., Giordano B.D. Does femoroacetabular impingement cause hip instability? A systematic review. Arthroscopy. 2016;32:203–208. doi: 10.1016/j.arthro.2015.07.021. [DOI] [PubMed] [Google Scholar]
- 31.Agricola R., Waarsing J.H., Arden N.K. Cam impingement of the hip—a risk factor for hip osteoarthritis. Nat Rev Rheumatol. 2013;9:630. doi: 10.1038/nrrheum.2013.114. [DOI] [PubMed] [Google Scholar]
- 32.Rhon D.I., Greenlee T.A., Sissel C.D., Reiman M.P. The two-year incidence of hip osteoarthritis after arthroscopic hip surgery for femoroacetabular impingement syndrome. BMC Musculoskelet Disord. 2019;20:266. doi: 10.1186/s12891-019-2646-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Litrenta J., Mu B.H.B., Ortiz-Declet V.M. Hip arthroscopy successfully treats femoroacetabular impingement in adolescent athletes. J Pediatr Orthop. 2020;40:e156–e160. doi: 10.1097/BPO.0000000000001411. [DOI] [PubMed] [Google Scholar]
- 34.Philippon M.J., Schenker M.L., Briggs K.K., Kuppersmith D.A., Maxwell R.B., Stubbs A.J. Revision hip arthroscopy. Am J Sports Med. 2007;35:1918–1921. doi: 10.1177/0363546507305097. [DOI] [PubMed] [Google Scholar]
- 35.Larson C.M., Giveans M.R., Samuelson K.M., Stone R.M., Bedi A. Arthroscopic hip revision surgery for residual femoroacetabular impingement (FAI) surgical outcomes compared with a matched cohort after primary arthroscopic FAI correction. Am J Sports Med. 2014;42:1785–1790. doi: 10.1177/0363546514534181. [DOI] [PubMed] [Google Scholar]
- 36.Dwyer M.K., Jones H.L., Field R.E., McCarthy J.C., Noble P.C. Femoroacetabular impingement negates the acetabular labral seal during pivoting maneuvers but not gait. Clin Orthop. 2015;473:602–607. doi: 10.1007/s11999-014-3760-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Technique for achieving a perfectly spherical femoroplasty during hip arthroscopy in a patient’s right hip. The patient is placed in a supine position with Trendelenburg. Position 1 is with the hip flexed at 45° with neutral rotation applied. The modified Dunn view is achieved with a 0° tilt and –30° cantilever to the C-arm. Under fluoroscopic guidance, work is done at the inferior most head/neck junction proximally, with an effort to maintain convexity to the femoral head. Care is taken to avoid concavity, which would disrupt the labral seal. For position 2, the operative extremity is brought into 60° of flexion with 30° external rotation and 25° adduction applied. The C-arm maintains its position, providing more medial exposure to the head/neck junction. Once work is completed in position 2, 30° further external rotation is applied to the extremity, totaling 60°, again, providing even more medial exposure to the head/neck junction. Next, position 4 is achieved with the operative extremity brought into full extension and neutral rotation. The C-arm is brought to –10° cantilever. This provides posterolateral exposure to the femoral head/neck junction. Work is done in this region, again, with direct visualization fluoroscopic guidance with a goal to maintain convexity at all times. For position 5, the C-arm is brought into neutral (0°) cantilever. At certain points, traction can be applied to work on the most proximal aspect of the noted cam lesion. Lastly, in position 6, the operative extremity is brought into 30o internal rotation, which provides further posterolateral exposure. Once the perfectly spherical femoroplasty is completed, traction is removed, the hip is flexed, and a dynamic impingement test is performed by alternating the operative extremity from positions 1 and 2. Before progressing to capsular management, it is ensured that the labral seal is maintained.