Abstract
The Outerbridge-Kashiwagi (O-K) procedure has conventionally been used for the treatment of osteoarthritis of the elbow and to treat posttraumatic sequelae including posttraumatic arthritis, stiffness, contracture, and ulnar neuritis. The procedure involves exposure of the posterior elbow joint as well creating a window posteriorly through the olecranon fossa to target anterior aspects of the elbow. Several case series have shown the O-K procedure to have good functional outcomes with minimal complications. Used mostly for the surgical treatment of adult osteoarthritis, the O-K procedure has not been previously described for the treatment of a pediatric supracondylar humerus fracture malunion. This article and accompanying video will present the pearls and discuss the technique of the O-K procedure used to treat the loss of elbow flexion as a sequelae of supracondylar humerus fracture malunion.
The Outerbridge-Kashiwagi (O-K) procedure was introduced by Kashiwagi in 19781 to treat early primary osteoarthritis of the elbow and was first described in the English language literature in 1990 by Stanley and Winson.2 Osteophyte formation on the olecranon, olecranon fossa, and coronoid can result in impingement and pain. Fenestration of the olecranon fossa allows for removal of loose bodies and osteophytes of both the anterior and posterior compartments of the elbow without extensive soft tissue dissection. In 1992 Morrey3 described the ulnohumeral arthroplasty, a modification of the O-K procedure that elevates rather than splits the triceps and uses a trephine slightly larger than the olecranon fossa to open the anterior part of the joint.
The O-K procedure has been used with favorable results for primary and posttraumatic osteoarthritis as well as elbow flexion contractures in brachial plexus birth injuries.1,4, 5, 6, 7 However, there is a paucity of literature on the use and outcomes of the O-K procedure for the treatment of the sequelae of supracondylar fracture malunion. This article and accompanying video (Video 1) illustrates our technique for the O-K procedure used to treat the sequelae of loss of elbow flexion due to extension malunion of a supracondylar humerus fracture.
Surgical Technique
Indications and Imaging
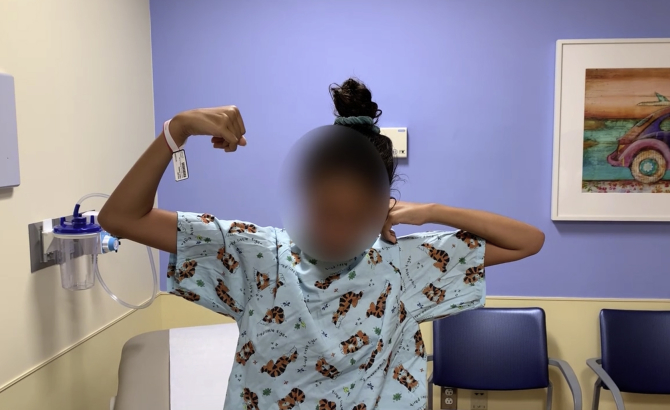
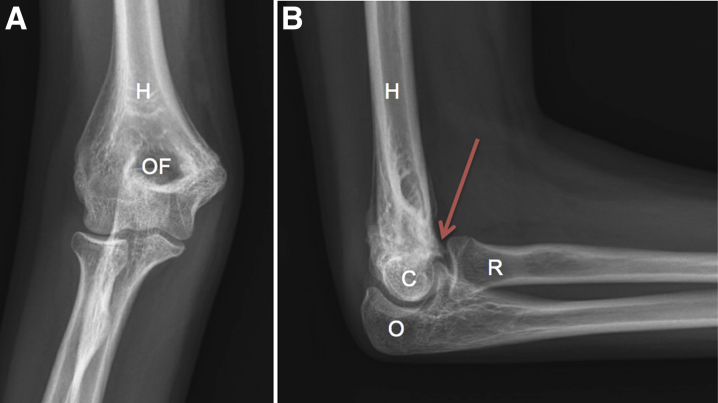
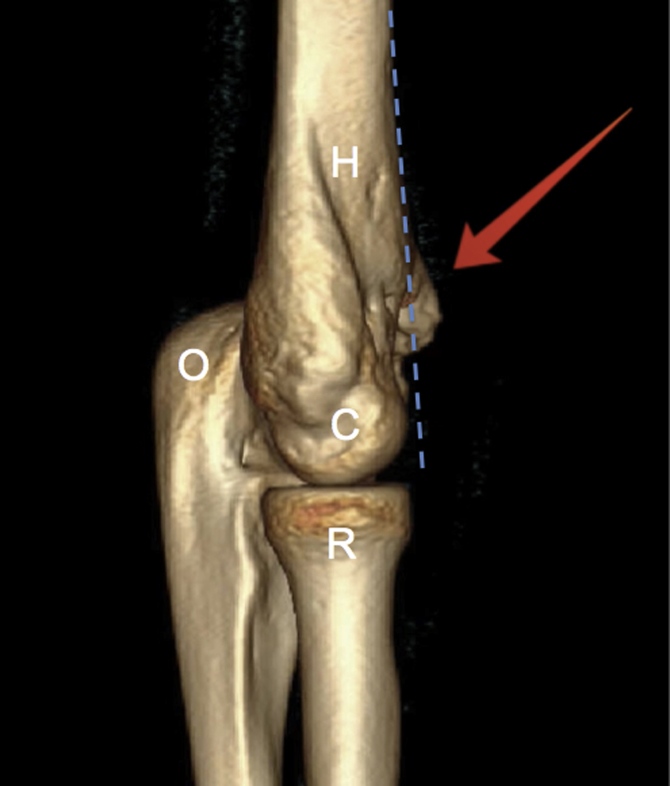
The patient was a skeletally mature 12-year-old girl who had sustained a supracondylar humerus fracture 2 years before presentation that was treated without surgery and presented with a chief complaint of decreased elbow flexion on the injured side (Fig 1). Plain radiographs reveal extension malunion of the distal humerus with some heterotopic bone anteriorly (Fig 2). Computed tomography scanning with 3-dimensional reconstruction confirms extension malunion with heterotopic bone in the coronoid fossa (Fig 3). A procedure with a quicker recovery as compared with conventional flexion osteotomy was desired, so the decision was made to proceed with an O-K procedure to restore elbow flexion.
Fig 1.
In this preoperative photo, the right elbow has decreased elbow flexion as a sequelae of a supracondylar humerus fracture extension malunion. The right hand is unable to reach the patient's face due to lack of elbow flexion.
Fig 2.
Anteroposterior (A) and lateral (B) radiographs of a right elbow showing extension malunion of the distal humerus with heterotopic bone anteriorly as depicted by the red arrow. (C, capitellum; H, humerus; O, olecranon; OF, olecranon fossa; R, radius.)
Fig 3.
Computed tomography scan with 3-dimensional reconstruction of a right elbow showing extension malunion of the distal humerus with heterotopic bone in the coronoid fossa (red arrow), which is likely limiting elbow flexion. The dashed blue line represents the anterior humeral line. (H, humerus; O, olecranon; C, capitellum; R, radius).
Patient Positioning
The patient was positioned supine, and general anesthesia was administered. A hand table was used, and a tourniquet was placed high in the right arm (Fig 4A). The extremity was cleaned, and sterile drapes were placed (Fig 4B).
Fig 4.
Patient is placed supine and the right upper extremity is placed over a hand table. (A) A tourniquet is placed high in the arm. (B) The right upper extremity is cleaned, and sterile drapes are placed. (C) The assistant helps to flex and adduct the arm over the patient's chest to facilitate exposure of the posterior distal humerus.
Exposure
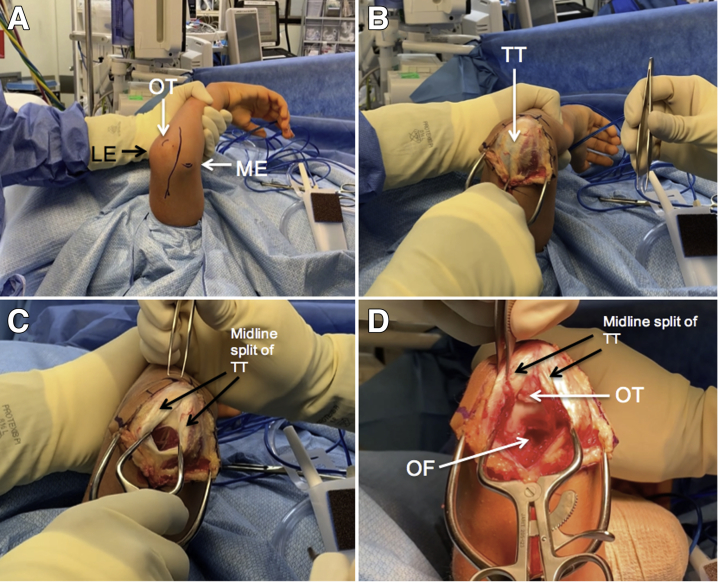
The olecranon, medial and lateral epicondyles, and the proposed incision were outlined (Fig 5A). A 5-cm incision beginning at olecranon and extending proximally was made through skin and curves medial to avoid the olecranon tip. Dissection was carried down the subcutaneous tissues, and small flaps were elevated medially and laterally to expose the triceps tendon (Fig 5B). The tendon was incised longitudinally along its midline, and the deeper soft tissue was elevated off of the distal humerus both medially and laterally to expose the olecranon fossa (Fig 5 C and D). Care was taken to avoid damage to the cartilage.
Fig 5.
Patient is positioned supine with the posterior aspect of the right elbow being shown. Bony landmarks such as the olecranon, medial and lateral epicondyles, and the proposed skin incision are outlined on the skin (A). Skin incision is made, and dissection proceeds through the subcutaneous tissues as small flaps are elevated medially and laterally to expose the triceps tendon (B). The triceps tendon is incised longitudinally along its midline (C). Deeper soft tissues are elevated from the humerus medially and laterally to expose the olecranon fossa (D). Care is taken to avoid injury to the cartilage. (LE, lateral epicondyle; ME, medial epicondyle; OF, olecranon fossa; OT, olecranon tip; TT, triceps tendon.)
Bone Excision
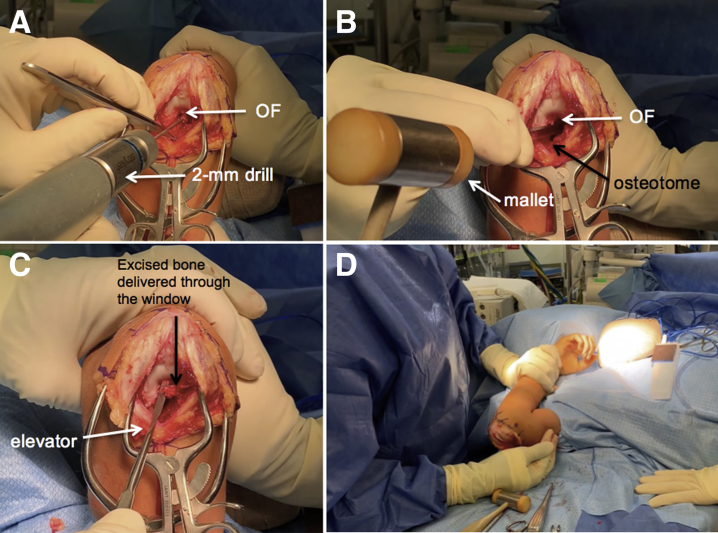
A 2-mm drill was used to create circumferential fenestrations in the olecranon fossa to guide a more-precise and -controlled osteotomy (Fig 6A). The use of burs to create a window was avoided to decrease the theoretical risk of heterotopic bone formation. Next, an osteotome and mallet was used to complete the osteotomy of the olecranon fossa (Fig 6B). A mixture of rongeurs, clamps, and curettes was used to deliver the excised bone out of the window (Fig 6C). Once adequately decompressed anteriorly, the elbow was gently manipulated in flexion to assess the increase in range of motion. The elbow now was able to flex beyond 130° of flexion, and the hand was able to reach the patient's face (Fig 6D). Before wound closure, intraoperative fluoroscopy was used to confirm adequate decompression and to ensure no iatrogenic fractures were created.
Fig 6.
Patient is positioned supine with the posterior aspect of the right elbow exposed. A 2-mm drill is used to create fenestrations circumferentially around the olecranon fossa to order to create a precise, controlled, and safe osteotomy (A). An osteotome and mallet is used to complete the osteotomy (B). A mixture of rongeurs, elevators, and curettes is used to deliver the excised bone out of the window (C). Once adequately decompressed anteriorly, the elbow is gently manipulated in flexion to assess the increase in range of motion. The elbow now is able to flex beyond 130° of flexion and the hand is able to reach the patient's face (D). (OF, olecranon fossa.)
Closure
After wound irrigation, the wound was closed in layers. The triceps tendon was closed with absorbable suture with the elbow held in 90° of flexion to prevent over tensioning of the triceps leading to extension of the elbow. The deep dermal layer was closed with buried interrupted suture, and the skin was closed with a running absorbable subcuticular suture. A sterile soft dressing was applied to allow for immediate range of motion.
Postoperative Rehabilitation
Immediate range of motion was allowed after surgery for daily activities. Formal physical therapy for range of motion exercises was begun by 2 weeks after surgery to allow for initial wound healing.
Discussion
Supracondylar humerus fractures are the most common elbow fracture in children and most often occur between 5 and 7 years of age on the nondominant elbow.8 The most common complications of supracondylar fracture and its treatment include vascular injury, compartment syndrome, neurologic deficit, pin site infections, and cubitus varus.9 Malunion has been identified as the cause of most angular deformities, and modern surgical techniques have vastly reduced their incidence.10 However, malunion can still be frequently observed after conservative treatment or malreduction after closed reduction and percutaneous pinning. Whereas the most common type of deformity resulting from malreduction involves cubitus varus and hyperextension, isolated distal humeral extension-type malunions are still encountered, as in this case.11 Although it has been shown that remodeling of sagittal plane deformities can occur, most extension type malunions result in clinically significant limitations in elbow flexion at skeletal maturity.11 Surgical correction is therefore recommended in patients with these malunions who report functional limitations. Numerous osteotomy techniques have been described, most of which focus on realignment in the coronal and sagittal planes.12
Complications for traditional corrective osteotomies are reported in the literature to be as high as 50%.13 Reported complications include ulnar-nerve palsy, hematoma, cosmetically unacceptable scarring, measurable arm atrophy, and loss of correction.13,14 The use of the O-K procedure as an alternative to a corrective flexion osteotomy may therefore be favorable due to the low incidence of reported complications and high satisfaction.4, 5, 6, 7 It is important to keep in mind that the O-K procedure can be successful in removing heterotopic bone that is contributing to mechanical block and loss of range of motion but will not correct a deformity. Historically, the success rates for the O-K procedure for symptomatic osteoarthritis have been 74% to 88%.15 An early series of O-K procedures performed by Antuña et al.7 for this indication found that 45 patients had mean improvements in the Mayo Elbow Performance Score from 55 points before surgery to 83 points (P < .0001) at latest follow-up in addition to an increase in the mean arc of flexion-extension from 79° to 101° (P < .0001) at latest follow-up. The O-K procedure has also been shown to have favorable outcomes when performed for other indications. More recently, Brewley et al.4 reported on their series of 21 patients undergoing the O-K procedure for posttraumatic elbow sequelae and found mean improvements in the Mayo Elbow Performance Score from 52 to 84 (P < .0001) and an increase in mean arc of motion from 44° to 98° (P < .0001) at a mean of 39 months after surgery. The O-K procedure also allows for a quicker recovery time and earlier postoperative range of motion than does a formal corrective osteotomy. In conclusion, the O-K procedure may be a useful alternative in select patients for the treatment of supracondylar malunions resulting in loss of range of motion. Tables 1 and 2 depict the advantages and disadvantages, and the pearls and potential pitfalls, respectively, of the O-K procedure compared with corrective osteotomies for the treatment of supracondylar humerus fracture malunions.
Table 1.
Advantages and Disadvantages of the Outerbridge-Kashiwagi Procedure
| Advantages |
|
| Disadvantages |
|
O-K, Outerbridge-Kashiwagi.
Table 2.
Pearls and Potential Pitfalls of the Outerbridge-Kashiwagi Procedure
| Pearls |
|
| Potential Pitfalls |
|
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video shows the technique for an Outerbridge-Kashiwagi (O-K) procedure for the treatment of an extension malunion of a pediatric supracondylar fracture resulting in anterior heterotopic bone formation and subsequent block to elbow flexion. Patient is positioned supine and general anesthesia is administered. A hand table is used and a tourniquet is placed high in the right arm. After standard prep and draping, bony landmarks such as the olecranon tip, medial and lateral epicondyles of the humerus, and the proposed skin incision are outlined. A 5-cm incision beginning at olecranon and extending proximally is made through skin and curves medial to avoid the olecranon tip. Dissection is carried down the subcutaneous tissues and small flaps are elevated medially and laterally to expose the triceps tendon. The tendon is incised longitudinally along its midline and the deeper soft tissue is elevated off of the distal humerus both medially and laterally to expose the olecranon fossa. Care is taken to avoid damage to the cartilage. Next, a 2-mm drill is used to create circumferential fenestrations in the olecranon fossa to guide a more precise and controlled osteotomy. The use of burs to create a window is avoided to decrease the theoretical risk of heterotopic bone formation. An osteotome and mallet is used to complete the osteotomy of the olecranon fossa. A mixture of rongeurs, clamps, and curettes is used to deliver the excised bone out of the window. Once adequately decompressed anteriorly, the elbow is gently manipulated in flexion to assess the increase in range of motion. After decompression, the elbow is able to flex beyond 130° and the hand is able to reach the patient's face. Before wound closure, intraoperative fluoroscopy is used to confirm adequate decompression and to ensure no iatrogenic fractures were created. After wound irrigation, the wound is closed in layers. The triceps tendon is closed absorbable suture with the elbow held in 90° of flexion to prevent over tensioning of the triceps leading to extension of the elbow. The deep dermal layer is closed with buried interrupted suture and the skin is closed with a running absorbable subcuticular suture. A sterile soft dressing is applied to allow for immediate range of motion.
References
- 1.Kashiwagi D. Intraarticular changes of the osteoarthritic elbow, especially about the fossa olecrani. J Jpn Orthop Assoc. 1978;52:1367–1382. [Google Scholar]
- 2.Stanley D., Winson I.G. A surgical approach to the elbow. J Bone Joint Surg Br. 1990;72:728–729. doi: 10.1302/0301-620X.72B4.2380238. [DOI] [PubMed] [Google Scholar]
- 3.Morrey B.F. Primary degenerative arthritis of the elbow. Treatment by ulnohumeral arthroplasty. J Bone Joint Surg Br. 1992;74:409–413. doi: 10.1302/0301-620X.74B3.1587890. [DOI] [PubMed] [Google Scholar]
- 4.Brewley E., Gorman R., Christmas K., Simon P., Chapel R., Mighell M. Use of a modified Outerbridge-Kashiwagi procedure for the treatment of posttraumatic elbow sequelae. J Shoulder Elbow Surg. 2019;28:1387–1394. doi: 10.1016/j.jse.2019.02.002. [DOI] [PubMed] [Google Scholar]
- 5.Forster M.C., Clark D.I., Lunn P.G. Elbow osteoarthritis: Prognostic indicators in ulnohumeral debridement—the outerbridge-kashiwagi procedure. J Shoulder Elbow Surg. 2001;10:557–560. doi: 10.1067/mse.2001.118416. [DOI] [PubMed] [Google Scholar]
- 6.Price A.E., Chim H., Valencia H., Grossman J.A.I. Result of modified Outerbridge-Kashiwagi procedure for elbow flexion contractures in brachial plexus birth injury. J Hand Surg. 2019;44:242–247. doi: 10.1177/1753193418797924. [DOI] [PubMed] [Google Scholar]
- 7.Antuña S.A., Morrey B.F., Adams R.A., O'Driscoll S.W. Ulnohumeral arthroplasty for primary degenerative arthritis of the elbow: Long-term outcome and complications. J Bone Joint Surg Am. 2002;84:2168–2173. doi: 10.2106/00004623-200212000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Omid R., Choi P.D., Skaggs D.L. Supracondylar humeral fractures in children. J Bone Joint Surg Am. 2008;90:1121–1132. doi: 10.2106/JBJS.G.01354. [DOI] [PubMed] [Google Scholar]
- 9.Pirone A.M., Graham H.K., Krajbich J.I. Management of displaced extension-type supracondylar fractures of the humerus in children. J Bone Joint Surg Am. 1988;70:641–650. [PubMed] [Google Scholar]
- 10.Tellisi N., Abusetta G., Day M., Hamid A., Ashammakhi N., Wahab K.H. Management of gartland's type III supracondylar fractures of the humerus in children: The role audit and practice guidelines. Injury. 2004;35:1167–1171. doi: 10.1016/j.injury.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 11.Simanovsky N., Lamdan R., Mosheiff R., Simanovsky N. Underreduced supracondylar fracture of the humerus in children: Clinical significance at skeletal maturity. J Pediatr Orthop. 2007;27:733–738. doi: 10.1097/BPO.0b013e3181558a63. [DOI] [PubMed] [Google Scholar]
- 12.Bauer A.S., Pham B., Lattanza L.L. Surgical correction of cubitus varus. J Hand Surg Am. 2016;41:447–452. doi: 10.1016/j.jhsa.2015.12.019. [DOI] [PubMed] [Google Scholar]
- 13.Ippolito E., Moneta M.R., D'Arrigo C. Post-traumatic cubitus varus. Long-term follow-up of corrective supracondylar humeral osteotomy in children. J Bone Joint Surg Am. 1990;72:757–765. [PubMed] [Google Scholar]
- 14.Oppenheim W.L., Clader T.J., Smith C., Bayer M. Supracondylar humeral osteotomy for traumatic childhood cubitus varus deformity. Clin Orthop Relat Res. 1984;188:34–39. [PubMed] [Google Scholar]
- 15.Sochacki K.R., Jack R.A., 2nd, Hirase T. Arthroscopic debridement for primary degenerative osteoarthritis of the elbow leads to significant improvement in range of motion and clinical outcomes: A systematic review. Arthroscopy. 2017;33:2255–2262. doi: 10.1016/j.arthro.2017.08.247. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video shows the technique for an Outerbridge-Kashiwagi (O-K) procedure for the treatment of an extension malunion of a pediatric supracondylar fracture resulting in anterior heterotopic bone formation and subsequent block to elbow flexion. Patient is positioned supine and general anesthesia is administered. A hand table is used and a tourniquet is placed high in the right arm. After standard prep and draping, bony landmarks such as the olecranon tip, medial and lateral epicondyles of the humerus, and the proposed skin incision are outlined. A 5-cm incision beginning at olecranon and extending proximally is made through skin and curves medial to avoid the olecranon tip. Dissection is carried down the subcutaneous tissues and small flaps are elevated medially and laterally to expose the triceps tendon. The tendon is incised longitudinally along its midline and the deeper soft tissue is elevated off of the distal humerus both medially and laterally to expose the olecranon fossa. Care is taken to avoid damage to the cartilage. Next, a 2-mm drill is used to create circumferential fenestrations in the olecranon fossa to guide a more precise and controlled osteotomy. The use of burs to create a window is avoided to decrease the theoretical risk of heterotopic bone formation. An osteotome and mallet is used to complete the osteotomy of the olecranon fossa. A mixture of rongeurs, clamps, and curettes is used to deliver the excised bone out of the window. Once adequately decompressed anteriorly, the elbow is gently manipulated in flexion to assess the increase in range of motion. After decompression, the elbow is able to flex beyond 130° and the hand is able to reach the patient's face. Before wound closure, intraoperative fluoroscopy is used to confirm adequate decompression and to ensure no iatrogenic fractures were created. After wound irrigation, the wound is closed in layers. The triceps tendon is closed absorbable suture with the elbow held in 90° of flexion to prevent over tensioning of the triceps leading to extension of the elbow. The deep dermal layer is closed with buried interrupted suture and the skin is closed with a running absorbable subcuticular suture. A sterile soft dressing is applied to allow for immediate range of motion.