Abstract
Knee arthroscopy has evolved greatly from its inception in the twentieth century. Of the many arthroscopic knee surgeries, meniscectomy is the most commonly performed. Arthroscopic meniscectomy is the most common orthopaedic surgical procedure performed in the United States. We continue to develop more minimally invasive procedures, and the NanoScope has provided a new generation of possibilities. The system does not require the use of a standard incision or portal, and with the use of nanoinstruments, we can perform treatments as well as diagnostic arthroscopy without incisions. This technique provides an updated incisionless option to perform a partial medial meniscectomy.
Minimally invasive surgery results in reduced pain, swelling, complications, and a quicker recovery. Arthroscopic knee surgery has evolved greatly from its inception in the twentieth century. Arthroscopic meniscectomy is the most commonly performed orthopaedic surgical procedure in the United States. Kim et al.1 showed that the number of arthroscopic partial meniscectomies increased by 49% to approximately 500,000 between 1996 and 2,006 in the United States. The diagnosis of intraarticular pathology such as meniscal tears depends on history, physical examination, and imaging modalities including plain radiography and magnetic resonance imaging (MRI). Arthroscopy is the gold standard in diagnosis because it allows direct visualization of pathology. MRI, although incredibly valuable, is not perfect; in a recent meta-analysis Phelan et al.2 evaluated the diagnostic accuracy of MRI in knee pathology specifically anterior cruciate ligament tears and meniscal injuries. The authors found that for anterior cruciate ligament tears, the sensitivity and specificity of MRI were 87% and 93%, for medial meniscal tears 89% and 88%, respectively, and for lateral meniscal tears 78% and 95%, respectively. Although Phelan et al.2 found compelling numbers for the diagnostic accuracy using MRI, this modality can be an expensive proposition, and with rising cost of health care, it calls into question whether there is a better, more cost-effective way to evaluate joint pathology. The NanoScope needle arthroscopy system (Arthrex, Naples, FL) is both diagnostic and therapeutic in that it allows direct visualization of intraarticular pathology and for instrumentation to treat meniscal tears. Although needle arthroscopy is mainly studied as a diagnostic tool that may be used in an in-office setting, the capabilities of the NanoScope system allow it to become a substitute for regular arthroscopy in certain cases such as partial meniscectomies as demonstrated in this technique. The NanoScope eliminates the need for incisions, requiring only a spinal needle to establish access to the joint.
Surgical Technique
Fig 1, Fig 2, Fig 3, Fig 4, Fig 5, Fig 6, Fig 7, Fig 8, Fig 9 and Video 1 show the surgical technique.
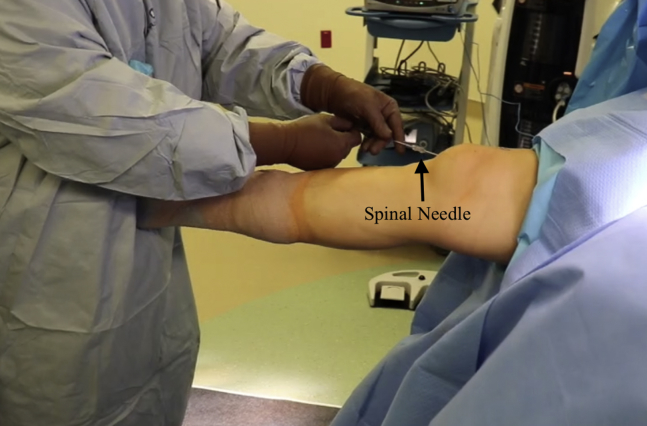
Fig 1.
Viewing the right knee from outside of the knee, the spinal needle is seen inserted into the patellofemoral joint while the knee is in full extension.
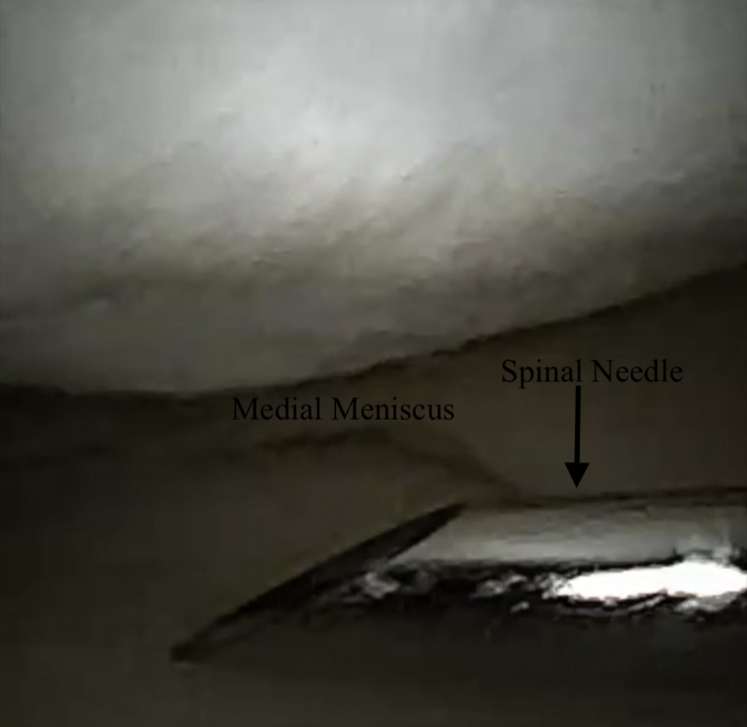
Fig 2.
Viewing the medial joint space with the 0° NanoScope while the right knee is in flexion, a spinal needle is seen inserted into the medial joint space.
Fig 3.
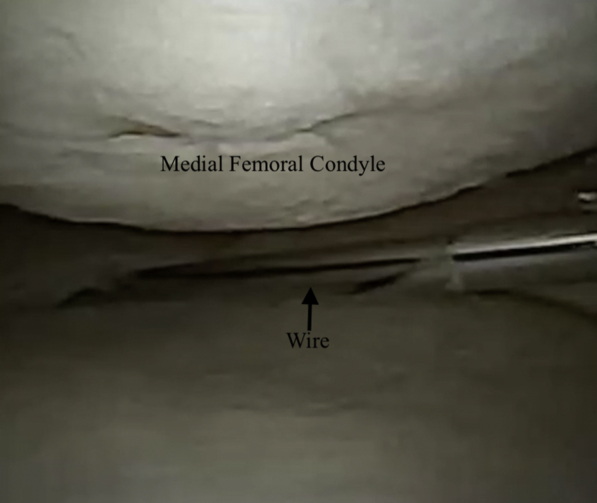
Viewing the medial joint space with the 0° NanoScope while the right knee is in flexion, a spinal needle is seen inserted into the medial joint space. A nitinol wire has been placed through the spinal needle.
Fig 4.
Viewing the right knee from outside of the joint, the NanoScope is seen placed through the lateral joint space, and the spinal needle can be seen in the medial joint space.
Fig 5.

Viewing the medial joint space with the 0° NanoScope while the right knee is in flexion, a nanobiter is seen performing the first steps of the partial medial meniscectomy.
Fig 6.
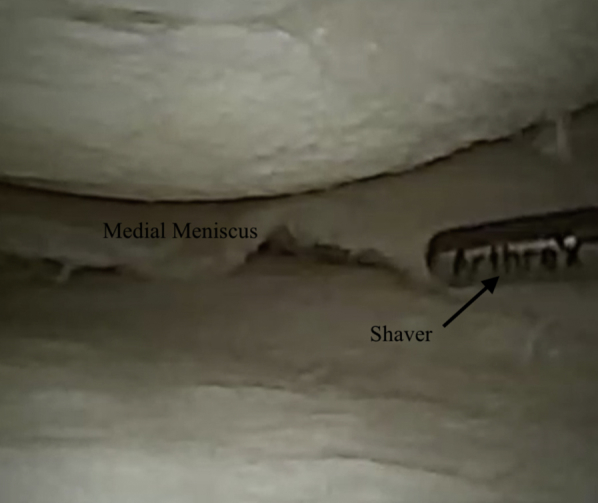
Viewing the medial joint space with the 0° NanoScope while the right knee is in flexion, a nanoshaver is seen finishing the partial medial meniscectomy.
Fig 7.
Viewing the right knee from outside the joint, the NanoScope can be seen in the lateral joint space, and nanoshaver can be seen performing the partial medial meniscectomy.
Fig 8.
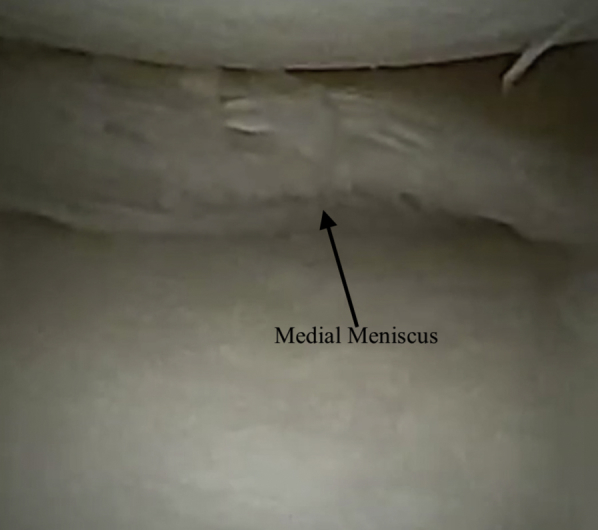
Viewing the medial joint space with the 0° NanoScope while the right knee is in flexion, the final partial medial meniscectomy has been performed.
Fig 9.
Viewing the right knee from outside the joint shows percutaneous needle sites but no incisions.
Patient Setup
The patient is placed in the supine position with the operative extremity in a leg holder and a tourniquet applied to the operative thigh. The nonoperative extremity is placed over a well-padded pillow in slight flexion. The operative extremity is exsanguinated, and the tourniquet is inflated.
Nanoscope Insertion
A spinal needle is inserted into anterolateral joint space while the knee is in full extension (Fig 1). A nitinol wire is inserted into the needle, and the needle is removed. A small cannula is then inserted over the wire and the wire is removed. Inflow is then placed onto the cannula, and the NanoScope is inserted for visualization of the joint (Video 1). A standard diagnostic arthroscopy is then performed in the patellofemoral joint. The NanoScope is then redirected into the medial joint space (Tables 1 and 2).
Table 1.
Pearls and Pitfalls of the incisionless Partial medial meniscectomy
| Pearls |
| The medial cannula can be removed and a 3-mm shaver inserted percutaneously for more aggressive shaving |
| The NanoScope should be redirected into compartments for each new viewing angle |
| Pitfalls |
| Care should be taken not to be overly aggressive with the small instruments |
Table 2.
Advantages and disadvantages of the incisionless Partial medial meniscectomy
| Advantages |
| Decreased loss and need for fluid |
| Less swelling and pain |
| Decreased risk for wound infection |
| Disadvantages |
| Additional cost of NanoScope |
| Difficult viewing angles |
Medial Portal
An 18-gauge spinal needle is then used to localized the medial portal location in an outside in fashion (Fig 2). A nitinol wire is inserted into the needle and the needle is removed (Figs 3 and 4). A small 2.7-mm cannula is then inserted over the wire, and the wire is removed.
Partial Medial Menisectomy
Nanoinstruments (Arthrex) are then used through this medial portal to perform the partial medial meniscectomy (Fig 5, Fig 6, Fig 7). First, the Nanobiter (Arthrex) is used to bite the posterior horn of the medial meniscus. A small Nanoshaver (Arthrex) is then used to finish the meniscectomy (Figs 8 and 9). Alternatively it may be helpful to remove the small cannula and percutaneously place a 3-mm shaver, which will allow more aggressive shaving (Table 1).
Discussion
Needle arthroscopy in the form of the NanoScope promises to be a minimally invasive method for diagnosis and treatment of intraarticular pathology. Currently, most data on needle arthroscopy compares the advantages it provides in an in-office setting for diagnostic purposes of intraarticular pathology in comparison with MRI. Gill et al. compared VisionScope needle arthroscopy to MRI and surgical diagnostic arthroscopy in 110 patients and found no statistically significant difference regarding the diagnosis of intra-articular, nonligamentous knee joint pathology.3 These results were also found in a similar study by Xerogeanes et al.4 where they showed that needle arthroscopy is more accurate than MRI and statistically equivalent to surgical arthroscopy. Deirmengian et al.5 also conducted a study where they evaluated the use of needle arthroscopy compared with MRI for the diagnosis of knee pathology. They found needle arthroscopy to be superior to MRI in both sensitivity and specificity in diagnosing meniscal tears (92.6% vs 77.8%; 100% vs 41.7%, respectively) and articular cartilage pathology. However, the incisionless partial medial meniscectomy technique focuses on treatment of pathology using a NanoScope in addition to the diagnostic purpose. This technique allows the surgeon a minimally invasive approach with the full capability of regular arthroscopy when treating partial meniscal tears. With this technique, there is no need to make an incision (Table 2). A portal is made with a 2.7-mm cannula, requiring only a spinal needle to establish access. The technique described here can also be translated into an office-based setting without the need for general anesthesia. There are limitations to the NanoScope because it has a lower image quality than most standard arthroscopes (Table 3). This could limit identification of secondary diagnoses and conditions. This procedure is also limited to smaller meniscus tears because larger tears may be difficult to manage without more flow or larger shavers (Table 2). As surgery heads more and more toward minimally invasive and cost-effective procedures, techniques such as the one we present here could lead to improved outcomes for patients.
Table 3.
Risk and limitations of incisionless partial medial meniscectomy
| Risks |
| Quality of image is slightly lower, which may lead to missed secondary diagnosis |
| Larger meniscus tears may be more difficult to manage with smaller instruments |
| Instruments are smaller and more fragile |
Footnotes
The authors report the following potential conflicts of interest or sources of funding: C.L. receives personal fees from Arthrex. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The patient is placed in the supine position with the operative extremity (right leg) in a leg holder and a tourniquet applied to the operative thigh. The nonoperative extremity is placed over a well-padded pillow in slight flexion. The operative extremity is exsanguinated, and the tourniquet is inflated. You can see a spinal needle is inserted into anterolateral joint space while the knee is in full extension. A nitinol wire is inserted into the needle, and the needle is removed. A small, 2.7-mm cannula is then inserted over the wire, and the wire is removed. Inflow is then placed onto the cannula, and the NanoScope (Arthrex, Naples, FL) is inserted for visualization of the joint. A standard diagnostic arthroscopy is then performed in the patellofemoral joint. The nanoscope is then redirected into the medial joint space. An 18-gauge spinal needle is then used to localized the medial portal location in an outside in fashion. Next, you will see a nitinol wire is inserted into the needle, and the needle is removed. A small 2.7-mm cannula is then inserted over the wire, and the wire is removed. Nanoinstruments are then used through this medial portal to perform the partial medial meniscectomy. First, the Nanobiter (Arthrex) is used to bite the posterior horn of the medial meniscus. A small nanoshaver (Arthrex) is then used to finish the meniscectomy. Alternatively it may be helpful to remove the small cannula and percutaneously place a 3-mm shaver, which will allow more-aggressive shaving. Final images show the partial medial meniscectomy, as well as no incisions on the knee.
References
- 1.Kim S., Bosque J., Meehan J.P., Jamali A., Marder R. Increase in outpatient knee arthroscopy in the United States: A comparison of national surveys of ambulatory surgery, 1996 and 2006. J Bone Joint Surg AM. 2011;93:994–1000. doi: 10.2106/JBJS.I.01618. [DOI] [PubMed] [Google Scholar]
- 2.Phelan N., Rowland P., Galvin R., O'Byrne J.M. A systematic review and meta-analysis of the diagnostic accuracy of MRI for suspected ACL and meniscal tears of the knee. Knee Surg Sports Traumatol Arthrosc. 2016;24:1525–1539. doi: 10.1007/s00167-015-3861-8. [DOI] [PubMed] [Google Scholar]
- 3.Gill T.J., Safran M., Mandelbaum B., Huber B., Gambardella R., Xerogeanes J. A prospective, blinded, multicenter clinical trial to compare the efficacy, accuracy, and safety of in-office diagnostic arthroscopy with magnetic resonance imaging and surgical diagnostic arthroscopy. Arthroscopy. 2018;34:2429–2435. doi: 10.1016/j.arthro.2018.03.010. [DOI] [PubMed] [Google Scholar]
- 4.Xerogeanes J.W., Safran M.R., Huber B., Mandelbaum B.R., Robertson W., Gambardella R.A. A prospective multi-center clinical trial to compare efficiency, accuracy and safety of the VisionScope imaging system compared to MRI and diagnostic arthroscopy. Orthop J Sports Med. 2014;2(Suppl2):2325967114. [Google Scholar]
- 5.Deirmengian C.A., Dines J.S., Vernace J.V., Schwartz M.S., Creighton R.A., Gladstone J.N. Use of a small-bore needle arthroscope to diagnose intra-articular knee pathology: Comparison with magnetic resonance imaging. Am J Orthop. 2018;47 doi: 10.12788/ajo.2018.0007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is placed in the supine position with the operative extremity (right leg) in a leg holder and a tourniquet applied to the operative thigh. The nonoperative extremity is placed over a well-padded pillow in slight flexion. The operative extremity is exsanguinated, and the tourniquet is inflated. You can see a spinal needle is inserted into anterolateral joint space while the knee is in full extension. A nitinol wire is inserted into the needle, and the needle is removed. A small, 2.7-mm cannula is then inserted over the wire, and the wire is removed. Inflow is then placed onto the cannula, and the NanoScope (Arthrex, Naples, FL) is inserted for visualization of the joint. A standard diagnostic arthroscopy is then performed in the patellofemoral joint. The nanoscope is then redirected into the medial joint space. An 18-gauge spinal needle is then used to localized the medial portal location in an outside in fashion. Next, you will see a nitinol wire is inserted into the needle, and the needle is removed. A small 2.7-mm cannula is then inserted over the wire, and the wire is removed. Nanoinstruments are then used through this medial portal to perform the partial medial meniscectomy. First, the Nanobiter (Arthrex) is used to bite the posterior horn of the medial meniscus. A small nanoshaver (Arthrex) is then used to finish the meniscectomy. Alternatively it may be helpful to remove the small cannula and percutaneously place a 3-mm shaver, which will allow more-aggressive shaving. Final images show the partial medial meniscectomy, as well as no incisions on the knee.