Key Points
Question
How often are older adults discharged with changes to their outpatient diabetes medication regimens following hospitalization for common medical conditions?
Findings
In this cohort study of 16 178 older adults hospitalized in the Veterans Health Administration national health system, 1 in 10 patients was discharged with intensified diabetes medications. Nearly half of patients receiving intensifications had already reached outpatient blood glucose goals or had limited life expectancy.
Meaning
During hospitalization, consideration of long-term diabetes control is needed in addition to inpatient blood glucose recordings to reduce potentially nonbeneficial medication changes when older adults are discharged home.
This cohort study estimates the prevalence of diabetes medication intensification and the likelihood of benefit associated with medication intensification among older adults hospitalized in a Veterans Health Administration hospital.
Abstract
Importance
Elevated blood glucose levels are common in hospitalized older adults and may lead clinicians to intensify outpatient diabetes medications at discharge, risking potential overtreatment when patients return home.
Objective
To assess how often hospitalized older adults are discharged with intensified diabetes medications and the likelihood of benefit associated with these intensifications.
Design, Setting, and Participants
This retrospective cohort study examined patients aged 65 years and older with diabetes not previously requiring insulin. The study included patients who were hospitalized in a Veterans Health Administration hospital for common medical conditions between 2012 and 2013.
Main Outcomes and Measures
Intensification of outpatient diabetes medications, defined as receiving a new or higher-dose medication at discharge than was being taken prior to hospitalization. Mixed-effect logistic regression models were used to control for patient and hospitalization characteristics.
Results
Of 16 178 patients (mean [SD] age, 73 [8] years; 15 895 [98%] men), 8535 (53%) had a preadmission hemoglobin A1c (HbA1c) level less than 7.0%, and 1044 (6%) had an HbA1c level greater than 9.0%. Overall, 1626 patients (10%) were discharged with intensified diabetes medications including 781 (5%) with new insulins and 557 (3%) with intensified sulfonylureas. Nearly half of patients receiving intensifications (49% [791 of 1626]) were classified as being unlikely to benefit owing to limited life expectancy or already being at goal HbA1c, while 20% (329 of 1626) were classified as having potential to benefit. Both preadmission HbA1c level and inpatient blood glucose recordings were associated with discharge with intensified diabetes medications. Among patients with a preadmission HbA1c level less than 7.0%, the predicted probability of receiving an intensification was 4% (95% CI, 3%-4%) for patients without elevated inpatient blood glucose levels and 21% (95% CI, 15%-26%) for patients with severely elevated inpatient blood glucose levels.
Conclusions and Relevance
In this study, 1 in 10 older adults with diabetes hospitalized for common medical conditions was discharged with intensified diabetes medications. Nearly half of these individuals were unlikely to benefit owing to limited life expectancy or already being at their HbA1c goal.
Introduction
During hospitalization, outpatient medication regimens are frequently modified by inpatient clinicians.1,2,3 While medication changes are often related to the condition that led to hospitalization (eg, receiving antiplatelets following an acute myocardial infarction), inpatient monitoring may lead to adjustments of medication regimens prescribed for chronic diseases, such as diabetes and hypertension, that are not directly connected to the primary condition for which the patient was hospitalized. Nonessential modification of chronic disease regimens during hospitalization may risk medication confusion and adverse drug events if patients are discharged with prescriptions for those modified regimens.
Prior research indicates that intensifications of hypertension regimens are common in hospitalized older adults and are driven by inpatient measurements.3,4 Similar to blood pressure, blood glucose levels are monitored frequently in hospitalized patients with diabetes and elevated inpatient recordings may lead clinicians to discharge patients with prescriptions for intensified diabetes medications. Despite controversy over the benefit of strict inpatient glycemic control,5,6,7 the frequency of changes to outpatient diabetes regimens following hospitalization is unknown. For patients with severely uncontrolled diabetes (eg, hemoglobin A1c [HbA1c] level >9.0% [to convert to proportion of total hemoglobin, multiply by 0.01]), medication intensification at discharge may improve hyperglycemia symptoms and set them on the path toward improved long-term glycemic control. In contrast, intensifications of diabetes medication regimens for patients with previously well-controlled diabetes may contribute to unnecessary polypharmacy and pose a risk of overtreatment. Both overtreatment and medication confusion may risk hypoglycemia,8 particularly when insulins and sulfonylureas are intensified.9
Understanding the impact of hospitalization on outpatient diabetes control is particularly crucial for older adults, more than 25% of whom have diabetes. Older adults are the most frequently hospitalized age group, and the balance of risks and benefits from strict blood glucose control may vary owing to limited life expectancy and elevated risks of hypoglycemia, polypharmacy, and adverse drug events.10 Thus, we examined a national cohort of hospitalized older adults with diabetes not previously requiring insulin to assess how often outpatient diabetes medications were intensified at hospital discharge, to identify which medications were most commonly intensified, and to determine whether life expectancy or prior outpatient diabetes control were associated with intensification decisions.
Methods
We conducted a retrospective cohort study of older adults admitted to Veterans Affairs Administration (VHA) hospitals using VHA clinical and pharmacy data merged with VHA and Medicare claims data. This research was approved by the institutional review boards of the San Francisco Veterans Affairs Medical Center and University of California, San Francisco. A waiver of informed consent was obtained because administrative data were used and all data were deidentified. Data analysis was performed from October 20, 2018, to September 1, 2019. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Study Population
The study cohort consisted of all patients aged 65 years and older with a diagnosis of diabetes who were not taking insulin prior to admission, received regular VHA outpatient care, and were admitted to a VHA hospital between January 1, 2011, and December 31, 2013, for common medical conditions.
We defined diabetes as at least 2 outpatient diagnoses or 1 hospital discharge diagnosis of diabetes in the 2 years preceding the index hospitalization.11,12 Algorithms based on administrative codes may capture patients with a history of diabetes, so we examined only patients who were taking a diabetes medication prior to hospitalization and those who were not taking a diabetes medication but who had an HbA1c level greater than 6.5% in the year preceding admission.
Discharge diagnoses were identified by primary diagnosis code grouped by Clinical Classification Software categories13 and included medical and cardiovascular conditions. Medical conditions included asthma, chronic obstructive pulmonary disease, pneumonia, sepsis, skin infection, and urinary tract infection. Cardiovascular conditions included arrhythmia, chest pain, coronary artery disease, acute coronary syndrome, conduction disorders, congestive heart failure, heart valve disorder, stroke, and transient ischemic attack. These conditions were chosen as they are among the most common reasons for hospitalization and their acute management does not typically require intensification of outpatient diabetes medications. We excluded patients with secondary discharge diagnoses of diabetic ketoacidosis or hyperglycemic hyperosmolar syndrome, which might necessitate an acute change in diabetes treatment.
To ensure accurate capture of medication use, we limited our sample to patients who received at least 80% of their outpatient care in VHA settings and thus were expected to regularly receive medications from VHA pharmacy sources, and we excluded patients admitted from or discharged to an institutional setting and those admitted to the hospital in the preceding 30 days.14 As insulin is given by injection and instructions to change insulin doses are often not accompanied by a new prescription, dosing changes cannot be accurately assessed using pharmacy databases, so we limited our study to patients not taking insulin prior to hospitalization. Detailed exclusion criteria are provided in the eFigure in the Supplement.
Identifying Medication Intensifications
Our primary outcome was whether a patient received 1 or more intensified outpatient diabetes medications at hospital discharge. We examined all major diabetes medication classes in use during our study period, which included sulfonylureas, biguanides, thiazolidinediones, α-glucosidase inhibitors, dipeptidyl peptidase-4 inhibitors, meglitinides, glucagon-like peptide agonists, and insulins.
We identified intensifications based on a previously validated algorithm comparing medications in use prior to hospital admission with medications prescribed at hospital discharge.3,15 We defined medications in use at hospital admission as the latest pharmacy fill being for a quantity sufficient to last until at least 60 days before admission. Discharge medications were defined as prescriptions filled by the outpatient VHA pharmacy between 2 days before and 2 days after discharge and prescriptions filled by the inpatient pharmacy on the day of discharge with a supply of at least 7 days.
Medication intensifications were defined to include both new medication additions and dose increases of admission medications. Medications not present on admission but prescribed at discharge were classified as additions. Admission medications for which a discharge prescription was filled for greater than 20% of the preadmission dose were classified as dose increases.
Covariates
The primary variables evaluated for association were preadmission and inpatient diabetes control. Preadmission diabetes control was measured using the most recent HbA1c laboratory value measured within 1 year prior to hospitalization and categorized as tightly controlled (HbA1c level <7.0%), controlled (HbA1c level 7.0%-8.9%), elevated (HbA1c level >9.0%), or not measured in prior year. Inpatient diabetes control was measured by inpatient blood glucose recordings and categorized as severely elevated (>3 recordings >299 mg/dL [to convert to millimoles per liter, multiply by 0.0555]), moderately elevated (>3 recordings >199 mg/dL), or not elevated.
Covariates included age, sex, ethnicity, median household income estimated from residential zip codes, counts of diabetes and overall admission medications, preadmission adherence to diabetes medications defined by composite proportion of days covered in the prior year, individual conditions of the Charlson Comorbidity Index (calculated from VHA and Medicare claims during the 24 months before hospitalization),16 and outpatient kidney function measured by estimated glomerular filtration rate.17 Hospitalization-related covariates included year of admission, training hospital status, length of stay, primary discharge diagnosis, inpatient glomerular filtration rate measured on the hospital day closest to discharge, and an indicator variable for receipt of inpatient corticosteroid medications, as corticosteroids are associated with elevated blood glucose levels.18
Statistical Analysis
We present unadjusted proportions of patients who received diabetes medication intensifications overall, by medication class, and by intensification type. We describe the proportion of patients receiving high-risk intensifications, defined as receipt of intensified insulin or sulfonylurea medications, as these medications are more strongly associated with severe hypoglycemia than other diabetes medications.
Based on prior research and national guidelines that recommend less strict HbA1c targets in older adults with limited life expectancy,10,19,20,21 we examined the proportion of patients discharged with intensifications who were likely or unlikely to benefit from stricter glycemic control based on preadmission HbA1c and estimated life expectancy. Estimated life expectancy was calculated from age and Charlson Comorbidity Index score and categorized as less than 5 years, 5 to 10 years, and greater than 10 years, as in prior studies.22,23 Patients were categorized as likely to benefit if their preadmission HbA1c level was greater than 9.0%. Patients were categorized as unlikely to benefit if their preadmission HbA1c level was less than 7.5% regardless of life expectancy or if their preadmission HbA1c level was less than 9.0% and estimated life expectancy was less than 5 years. All others were classified as indeterminate.
We conducted multivariable mixed-effect logistic regression analyses to determine associations between diabetes medication intensification and preadmission and inpatient diabetes control. Adjusted analyses included the covariates we have noted, a random-effect term to account for clustering by hospital, and an interaction term to account for the association between preadmission and inpatient diabetes control. Missing data were imputed using iterative Markov chain Monte Carlo method and 10 imputation sets. We used postestimation margins following regression analyses to calculate predicted probabilities of intensification by preadmission and inpatient diabetes control and likelihood to benefit category.
We determined statistical significance by using 95% confidence intervals and 2-tailed tests with P < .05 as the threshold for significance. We used Stata version 14.1 (StataCorp) for all analyses.
Results
We identified 16 178 older adults (mean [SD] age, 73 [8] years; 15 895 [98%] men) with diabetes who were discharged from VHA medical centers (Table 1). Nearly 70% of patients were taking 1 or more diabetes medications prior to hospitalization, with metformin and sulfonylureas most commonly used. More than one-quarter of patients had an estimated life expectancy less than 5 years. The most common discharge diagnoses were congestive heart failure (16%), pneumonia (12%), coronary artery disease (11%), conduction disorders (10%), and chronic obstructive pulmonary disease (10%).
Table 1. Cohort Characteristicsa.
| Characteristic | Patients, No. (%) (N = 16 178) |
|---|---|
| Demographic and comorbidity | |
| Age, median (IQR), y | 73 (67-80) |
| Female | 283 (2) |
| Race/ethnicity | |
| White | 13 138 (81) |
| Black | 2336 (14) |
| Hispanic | 225 (1) |
| Other | 479 (3) |
| Income, mean (SD), $ | 26 653 (46 601) |
| Selected comorbidities | |
| Congestive heart failure | 6722 (42) |
| Kidney disease | 5061 (31) |
| Cerebrovascular accident | 4217 (26) |
| Prior myocardial infarction | 3024 (20) |
| Malignant neoplasm | 3574 (22) |
| Dementia | 519 (3) |
| Estimated life expectancy, yb | |
| >10 | 7065 (44) |
| 5-10 | 4652 (29) |
| <5 | 4461 (28) |
| Hospitalization | |
| Year of hospitalization | |
| 2011 | 6370 (39) |
| 2012 | 5101 (32) |
| 2013 | 4707 (29) |
| Training hospital | 14 551 (90) |
| Length of stay, median (IQR), d | 4 (2-6) |
| Discharge diagnosis | |
| Arrhythmia | 217 (1) |
| Asthma | 84 (1) |
| Chronic obstructive pulmonary disease | 1531 (10) |
| Chest pain | 664 (4) |
| Conduction disorders | 1617 (10) |
| Coronary artery disease | 1795 (11) |
| Acute coronary syndrome | 971 (6) |
| Congestive heart failure | 2553 (16) |
| Heart valve disorder | 312 (2) |
| Pneumonia | 1893 (12) |
| Sepsis | 285 (2) |
| Skin infection | 1377 (9) |
| Stroke | 791 (5) |
| Transient ischemic attack | 263 (2) |
| Urinary tract infection | 1429 (9) |
| Venous thromboembolism | 396 (3) |
| Estimated glomerular filtration rate, mean (SD), mL/min/1.73 m2 | |
| Preadmission | 66 (24) |
| Discharge | 68 (27) |
| Medication use | |
| No. of admission medications, median (IQR) | 9 (6-12) |
| No. of admission diabetes medications | |
| 0 | 4153 (26) |
| 1 | 8263 (51) |
| 2 | 3350 (21) |
| ≥3 | 412 (3) |
| Admission diabetes medications | |
| Sulfonylureas | 7830 (48) |
| Biguanides | 7328 (45) |
| Thiazolidinediones | 535 (3) |
| α-Glucosidase inhibitors | 265 (2) |
| Dipeptidyl peptidase-4 inhibitors | 145 (1) |
| Meglitinides | 28 (0) |
| Glucagon-like peptide agonists | 5 (0) |
| Prior diabetes medication adherence, proportion of days covered, %c | |
| <80 | 3700 (23) |
| ≥80 | 8325 (52) |
| Not taking diabetes medications at admission | 4153 (26) |
| Any receipt of inpatient corticosteroids | 1810 (11) |
Abbreviation: IQR, interquartile range.
Multiple imputation was used to account for missing data, which included inpatient estimated glomerular filtration rate (1300 patients), outpatient estimated glomerular filtration rate (1356 patients), and inpatient glucose recordings (673 patients).
Life expectancy was calculated based on number of comorbidities and age.
Adherence was calculated from electronic pharmacy dispensing data as the proportion of days covered for each admission diabetes medication in the year prior to index hospital admission. A threshold of 80% is a commonly used criterion to determine clinically significant nonadherence. To account for patients taking multiple diabetes mediations prior to hospitalization, a composite proportion of days covered was calculated as the mean of each individual diabetes medication proportion of days covered.
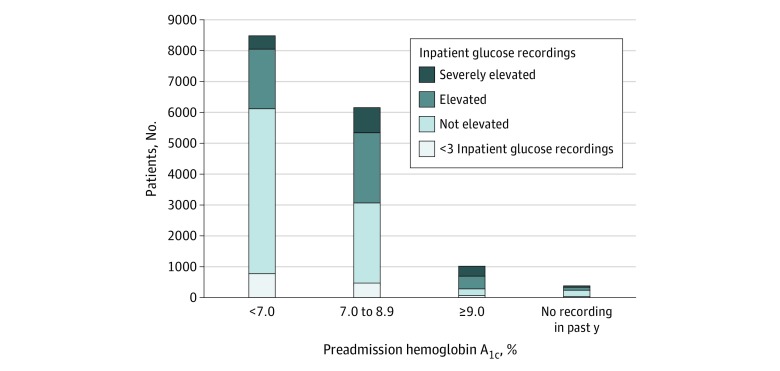
Association Between Preadmission and Inpatient Diabetes Control
Prior to hospitalization, 8535 patients (53%) had an HbA1c level less than 7.0%, 6199 (38%) had an HbA1c level between 7.0% and 8.9%, 1044 (6%) had an HbA1c level greater than 9.0%, and 400 (2%) did not have HbA1c level measured. During hospitalization, 1626 patients (10%) had severely elevated inpatient blood glucose levels (≥3 recordings >299 mg/dL) and 4724 (29%) had moderately elevated inpatient blood glucose levels (≥3 recordings >199 mg/dL). Elevated inpatient blood glucose levels were more common in patients with elevated preadmission HbA1c (P < .001 for trend); however, 37% of patients with elevated inpatient blood glucose levels had a preadmission HbA1c level less than 7.0% (Figure 1).
Figure 1. Association Between Inpatient Blood Glucose Recordings and Preadmission Outpatient Hemoglobin A1c Level.
Preadmission hemoglobin A1c was measured using most recent hemoglobin A1c laboratory value collected within 1 year preceding hospitalization. Inpatient blood glucose control was defined by the number of elevated blood glucose recordings as severely elevated (≥3 recordings of ≥300 mg/dL [to convert to millimoles per liter, multiply by 0.0555]), moderately elevated (≥3 recordings of ≥200 mg/dL without meeting criteria for severely elevated), or not elevated. Preadmission hemoglobin A1c was found to be associated with inpatient blood glucose categories (P < .001 using a χ2 test). To convert hemoglobin A1c to proportion of total hemoglobin, multiply by 0.01.
Diabetes Medication Intensifications
A total of 1626 patients (10%) were discharged with intensified diabetes medications and 1301 (8%) were discharged with intensified high-risk diabetes medications (Table 2). The most common intensifications were insulin additions, which occurred in 781 hospitalizations (5%). Intensifications of sulfonylureas occurred in 557 hospitalizations (3%); however, 94 patients with new sulfonylureas were noted to have filled a different sulfonylurea prior to admission, so these changes may reflect therapeutic substitutions. Intensifications of metformin were also common, occurring in 382 hospitalizations (2%), while intensifications of all other medication classes were infrequent.
Table 2. Diabetes Medication Intensifications.
| Intensification | Patients, No. (%) (N = 16 178) |
|---|---|
| Any intensification | 1626 (10) |
| Intensification of high-risk medicationsa | 1301 (8) |
| Insulin | |
| Any | 781 (5) |
| Long-acting insulin start | 678 (4) |
| Short-acting insulin start | 307 (2) |
| Both long and short acting insulin start | 204 (1) |
| Sulfonylureas | |
| Any | 557 (3) |
| New startb | 425 (3) |
| Dose increase | 132 (1) |
| Metformin | |
| Any | 382 (2) |
| New start | 298 (2) |
| Dose increase | 84 (1) |
| Other | |
| Anyc | 38 (0) |
| Dipeptidyl peptidase-4 inhibitors | 17 (0) |
| α-Glucosidase inhibitors | 11 (0) |
| Thiazolidinediones | 8 (0) |
| Meglitinides | 4 (0) |
| Glucagon-like peptide-1 agonists | 0 |
High-risk medications were defined as classes with increased risk of hypoglycemia and included insulins and sulfonylureas.
Ninety-four patients with new sulfonylureas were noted to have filled a different sulfonylurea prior to admission.
All other diabetes medication intensifications were new prescriptions with the exception of 3 patients receiving dose increases of α-glucosidase inhibitors.
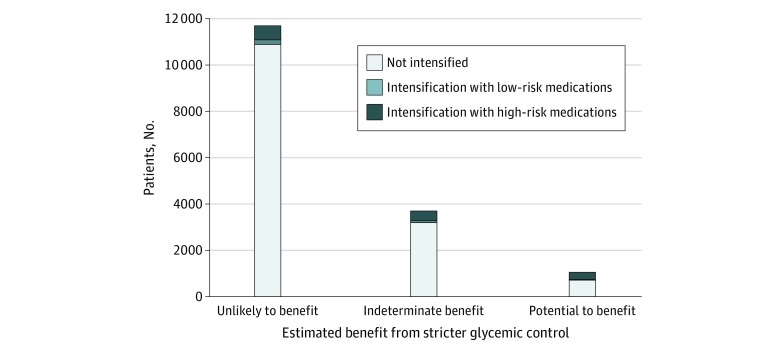
The majority of patients (77% [12 441 of 16 178]) were classified as being unlikely to benefit from more intensive diabetes control based on preadmission diabetes control and life expectancy, 6% (1044 of 16 178) were categorized as being likely to benefit, and 17% (2693 of 16 178) were categorized as having indeterminate benefit (eTable 1 in the Supplement). Figure 2 shows that 49% of patients receiving intensifications (791 of 1626) were classified as unlikely to benefit, 20% (329 of 1626) as likely to benefit, and 31% (506 of 1626) as having indeterminant benefit. Among patients receiving intensifications with high-risk medications, 45% (588 of 1301) were classified as being unlikely to benefit, 23% (305 of 1301) as likely to benefit, and 31% (408 of 1301) as having indeterminant benefit.
Figure 2. Intensification of Diabetes Medications by Estimated Likelihood to Benefit.
High-risk intensifications included addition of insulin and/or addition or dose increase of sulfonylurea medications. Likelihood of benefit from diabetes medication intensification was estimated using preadmission hemoglobin A1c and estimated life expectancy. Patients were categorized as having potential to benefit if their preadmission hemoglobin A1c level was greater than 9.0% (to convert to proportion of total hemoglobin, multiply by 0.01). Patients were categorized as unlikely to benefit if their preadmission hemoglobin A1c level was less than 7.5% regardless of life expectancy or if their preadmission hemoglobin A1c level was less than 9.0% and their estimated life expectancy was less than 5 years. All others were classified as having indeterminate benefit (eTable 1 in the Supplement). Estimated likelihood of benefit was found to be associated with intensification category (P < .001 using a χ2 test).
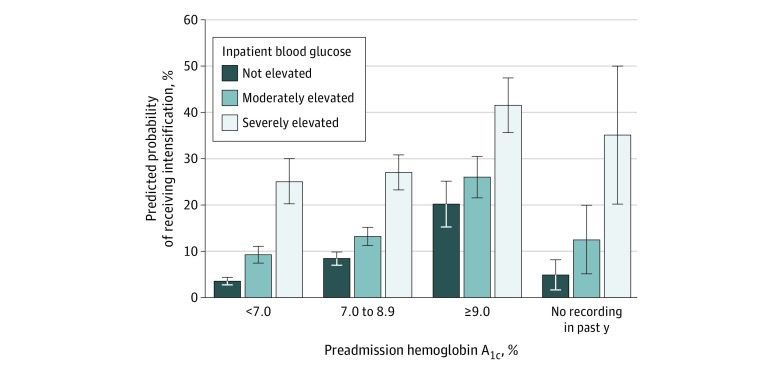
Probability of Intensification by Preadmission and Inpatient Diabetes Control
Figure 3 shows the predicted probabilities of receiving intensifications by both preadmission and inpatient diabetes control and demonstrates that each preadmission HbA1c category was associated with increasingly greater predicted probabilities of receiving intensifications based on patients’ inpatient blood glucose recordings. For example, among patients with a preadmission HbA1c level less than 7.0%, the predicted probability of being discharged with intensifications was 4% (95% CI, 3%-4%) for those without elevated inpatient blood glucose levels and 21% (95% CI, 15%-26%) for those with severely elevated inpatient blood glucose levels.
Figure 3. Predicted Probability of Receiving a Diabetes Medication Intensification at Discharge, by Inpatient and Outpatient Glucose Control.
Preadmission hemoglobin A1c was measured using the most recent laboratory value collected within 1 year preceding hospitalization. Inpatient blood glucose control was defined by the number of elevated blood glucose recordings as severely elevated (≥3 recordings of ≥300 mg/dL [to convert to millimoles per liter, multiply by 0.0555]), moderately elevated (≥3 recordings of ≥200 mg/dL without meeting criteria for severely elevated), or not elevated. Predicted probabilities were estimated following mixed-effect logistic regression accounting for age, sex, race/ethnicity, income, Charlson Comorbidity Index score, length of stay, primary discharge diagnosis, year, hospital training status, receipt of steroids during hospitalization, preadmission hemoglobin A1c, inpatient blood glucose level, an interaction term for preadmission hemoglobin A1c and inpatient blood glucose level, and random effects to account for clustering by Veterans Health Administration hospital. Error bars indicate 95% CIs. To convert hemoglobin A1c to proportion of total hemoglobin, multiply by 0.01.
Notably, both elevated preadmission HbA1c level and inpatient glucose control were associated with receipt of intensifications, with the odds of receiving intensifications increasing with increasing severity of both inpatient blood glucose level and outpatient and preadmission HbA1c level. However, 30% of patients receiving intensifications (486 of 1626) had tightly controlled HbA1c prior to hospitalization (eTable 2 in the Supplement).
Other Factors Associated With Diabetes Medication Intensifications
eTable 3 in the Supplement shows the adjusted odds ratios (ORs) for each covariate included in the model. Receiving no diabetes medications prior to hospitalization was associated with higher odds of receiving intensifications compared with taking 1 medication on admission (OR, 1.84; 95% CI, 1.58-2.15). Other hospitalization factors associated with increased odds of receiving intensifications were receipt of inpatient corticosteroids (OR, 1.24; 95% CI, 1.04-1.49) and longer length of stay (OR, 1.41; 95% CI, 1.12-1.78 for length of stay ≥14 days compared with <3 days). Hospitalization with heart failure (OR, 1.46; 95% CI, 1.15-1.84) and coronary artery disease (OR, 1.35; 95% CI, 1.06-1.73) was associated with increased odds of receiving intensifications compared with a reference condition of pneumonia. Preadmission medication adherence was not associated with receiving diabetes medication intensifications.
Discussion
In this national retrospective cohort study of older adults with diabetes who were hospitalized for common medical conditions, we found that intensified diabetes medications were prescribed at discharge for 1 in 10 patients, most of whom we estimated were unlikely to benefit from stricter glycemic control. Most intensifications were for insulins or sulfonylureas, classes with the highest risk of hypoglycemia,23,24 and intensifications commonly occurred in patients previously not taking diabetes medications. Elevated inpatient blood glucose recordings were associated with discharge with intensifications even in patients with previously well-controlled outpatient HbA1c values. These findings indicate that half of older adults receiving diabetes medication intensifications at hospital discharge may be at high risk of overtreatment while 20% may have potential to benefit.
In the hospital setting, many factors may cause blood glucose levels to fluctuate. Patients may experience physiologic stress hyperglycemia related to acute illness,25 be given medications that raise blood glucose levels (eg, corticosteroids or intravenous solutions containing dextrose), and have different dietary patterns than they would at home. Both acute kidney injury and inability to take pills by mouth are common in hospitalized older adults and may lead inpatient clinicians to withhold outpatient diabetes medications. For this reason, temporary inpatient sliding scale insulin protocols have become common despite risks of hypoglycemia.26 Our finding that nearly half of intensifications were for new insulin, primarily short-acting insulins, may represent high-risk carryover of inpatient regimens to the outpatient setting. While we found that most patients were unlikely to benefit from intensifications, for patients with both severe inpatient hyperglycemia and uncontrolled outpatient blood glucose levels who may benefit from intensifications, simpler guideline-based insulin regimens, starting with single dose long-acting agents, is likely to lessen hypoglycemia risks compared with more complex short-acting or multidrug insulin regimens.27
We found that one-third of patients with elevated inpatient blood glucose recordings had tightly controlled preadmission HbA1c, indicating that inpatient hyperglycemia is not a reliable marker to guide adjustments to outpatient diabetes regimens. Despite this, our findings indicate that inpatient blood glucose elevations frequently lead clinicians to intensify outpatient diabetes treatment, which may lead to unnecessarily intensive treatment. Prior evidence suggests that as many as 1 in 5 older adults receive potentially unnecessary intensive diabetes treatment, which is associated with increased risks for severe hypoglycemia.8 Evidence from the VHA and Medicare indicates that intensive treatment is common in older adults with medically complex conditions.8,28,29,30 While guidelines for long-term HbA1c targets for older adults are conflicting, there is consensus on the need to balance the benefits of intensive HbA1c control with the risks of hypoglycemia, particularly in patients with limited life expectancy.10 Our findings that nearly half of patients receiving intensifications were unlikely to benefit owing to limited life expectancy or already achieving goal HbA1c and that only 20% of patients with potential to benefit from intensifications received them indicate that likelihood for long-term benefit did not strongly influence intensification decisions made during hospitalization.
Even in patients who may benefit from stricter blood glucose control, it is unclear whether hospitalization is the right time to intensify outpatient therapy. Older adults are at an elevated risk for readmission and adverse drug events in the period after hospitalization31,32,33 and medication confusion at discharge is common and may be related to poor communication, medication reconciliation errors, delirium, or multiple changes. Few studies have examined posthospitalization changes in medications for chronic disease. One study34 of patients filling insulin following discharge observed a subsequent increased risk of death and readmissions; however, this study lacked information on patients’ inpatient or outpatient glycemic control. Another study4 examining the antihypertensive intensifications at discharge found increased risks of adverse events and readmissions. Thus, additional information is needed on the long-term outcomes of intensifying diabetes medications at discharge. In the meantime, if there is concern about persistent hyperglycemia after the patient leaves the hospital, for most patients, a safer course than intensifying medications may be to focus on communicating with outpatient providers to inform decision-making following recovery from hospitalization. For patients with severe hyperglycemia on the day of discharge, ensuring close outpatient follow-up, prioritizing restarting home medications, and, if medication intensification is warranted, choosing agents with less hypoglycemia risk may minimize potential overtreatment. For both patient groups, using hospital resources to focus on diabetes education has demonstrated long-term benefits35,36 and may be preferable to medication intensification.
Limitations
Our study has several limitations. Pharmacy records allow for identification of dose changes for oral medications but do not accurately reflect changes to insulin dosing; thus, we excluded patients taking insulin prior to hospitalization. We were unable to assess the frequency of medication discontinuations, leaving the possibility that some patients receiving intensifications may have had other diabetes medications reduced. Our study was conducted in the national VHA health system, which serves a higher proportion of men and patients with multiple chronic conditions and uses a national pharmacy benefit management system, which may limit variation in medication selection. However, as this study examined prescribing practices and the VHA is a primary training site for US graduate medical education, practices developed by trainees in the VHA may be carried on to other care settings. Our study examined only older adults; thus, our findings are not generalizable to younger populations. Since our study period, new classes of diabetes medications have been introduced, which may reduce the generalizability of our findings to current practice patterns.
Conclusions
This study found that 1 in 10 hospitalized older adults with diabetes was discharged with intensifications to their outpatient diabetes medication regimens, and most intensifications were initiations of new insulins and sulfonylureas. Nearly half of older adults receiving intensifications had limited life expectancy or had already achieved an outpatient HbA1c level less than 7.5%; thus, they were unlikely to benefit from this additional pharmacotherapy that appears to be prescribed largely in response to elevated inpatient blood glucose levels. Conversely, among patients with potential to benefit from stricter glycemic control, only 20% received intensifications, although even in this population, the clinical outcomes of intensifications made during recovery from acute illness are unknown. Improving diabetes care for hospitalized older adults will require efforts to move beyond treating elevated inpatient numbers and toward patient-centered decision-making that considers long-term benefits and the risks of potentially unnecessary medication intensifications.
eFigure. Cohort Construction Flowchart
eTable 1. Likelihood of Cohort Patients to Benefit From Stricter Glycemic Control
eTable 2. Rates of Diabetes Medication Intensification in Older Adults Following Hospitalization, by Inpatient and Outpatient Blood Glucose Control
eTable 3. Predictors of Diabetes Medication Intensification in Older Adults Following Hospitalization
References
- 1.Unroe KT, Pfeiffenberger T, Riegelhaupt S, Jastrzembski J, Lokhnygina Y, Colón-Emeric C. Inpatient medication reconciliation at admission and discharge: a retrospective cohort study of age and other risk factors for medication discrepancies. Am J Geriatr Pharmacother. 2010;8(2):-. doi: 10.1016/j.amjopharm.2010.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harris CM, Sridharan A, Landis R, Howell E, Wright S. What happens to the medication regimens of older adults during and after an acute hospitalization? J Patient Saf. 2013;9(3):150-153. doi: 10.1097/PTS.0b013e318286f87d [DOI] [PubMed] [Google Scholar]
- 3.Anderson TS, Wray CM, Jing B, et al. Intensification of older adults’ outpatient blood pressure treatment at hospital discharge: national retrospective cohort study. BMJ. 2018;362:k3503. doi: 10.1136/bmj.k3503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anderson TS, Jing B, Auerbach A, et al. Clinical outcomes after intensifying antihypertensive medication regimens among older adults at hospital discharge. JAMA Intern Med. 2019. Epub ahead of print. doi: 10.1001/jamainternmed.2019.3007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee YY, Lin YM, Leu WJ, et al. Sliding-scale insulin used for blood glucose control: a meta-analysis of randomized controlled trials. Metabolism. 2015;64(9):1183-1192. doi: 10.1016/j.metabol.2015.05.011 [DOI] [PubMed] [Google Scholar]
- 6.Christensen MB, Gotfredsen A, Nørgaard K. Efficacy of basal-bolus insulin regimens in the inpatient management of non-critically ill patients with type 2 diabetes: a systematic review and meta-analysis. Diabetes Metab Res Rev. 2017;33(5). doi: 10.1002/dmrr.2885 [DOI] [PubMed] [Google Scholar]
- 7.Colunga-Lozano LE, Gonzalez Torres FJ, Delgado-Figueroa N, et al. Sliding scale insulin for non-critically ill hospitalised adults with diabetes mellitus. Cochrane Database Syst Rev. 2018;11:CD011296. doi: 10.1002/14651858.CD011296.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McCoy RG, Lipska KJ, Yao X, Ross JS, Montori VM, Shah ND. Intensive treatment and severe hypoglycemia among adults with type 2 diabetes. JAMA Intern Med. 2016;176(7):969-978. doi: 10.1001/jamainternmed.2016.2275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Karter AJ, Warton EM, Lipska KJ, et al. Development and validation of a tool to identify patients with type 2 diabetes at high risk of hypoglycemia-related emergency department or hospital use. JAMA Intern Med. 2017;177(10):1461-1470. doi: 10.1001/jamainternmed.2017.3844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lipska KJ, Krumholz H, Soones T, Lee SJ. Polypharmacy in the aging patient: a review of glycemic control in older adults with type 2 diabetes. JAMA. 2016;315(10):1034-1045. doi: 10.1001/jama.2016.0299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kerr EA, Lucatorto MA, Holleman R, Hogan MM, Klamerus ML, Hofer TP; VA Diabetes Quality Enhancement Research Initiative (QUERI) Workgroup on Clinical Action Measures . Monitoring performance for blood pressure management among patients with diabetes mellitus: too much of a good thing? Arch Intern Med. 2012;172(12):938-945. doi: 10.1001/archinternmed.2012.2253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hebert PL, Geiss LS, Tierney EF, Engelgau MM, Yawn BP, McBean AM. Identifying persons with diabetes using Medicare claims data. Am J Med Qual. 1999;14(6):270-277. doi: 10.1177/106286069901400607 [DOI] [PubMed] [Google Scholar]
- 13.Healthcare Cost and Utilization Project. Clinical Classification Software (CCS) for ICD-9-CM. Published 2017. Accessed August 13, 2019. https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp
- 14.Anderson TS, Xu E, Whitaker E, Steinman MA. A systematic review of methods for determining cross-sectional active medications using pharmacy databases. Pharmacoepidemiol Drug Saf. 2019;28(4):403-421. doi: 10.1002/pds.4706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anderson TS, Jing B, Wray CM, et al. Comparison of pharmacy database methods for determining prevalent chronic medication use. Med Care. 2019;57(10):836-842. doi: 10.1097/MLR.0000000000001188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613-619. doi: 10.1016/0895-4356(92)90133-8 [DOI] [PubMed] [Google Scholar]
- 17.Levey AS, Coresh J, Greene T, et al. ; Chronic Kidney Disease Epidemiology Collaboration . Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006;145(4):247-254. doi: 10.7326/0003-4819-145-4-200608150-00004 [DOI] [PubMed] [Google Scholar]
- 18.Tamez-Pérez HE, Quintanilla-Flores DL, Rodríguez-Gutiérrez R, González-González JG, Tamez-Peña AL. Steroid hyperglycemia: prevalence, early detection and therapeutic recommendations: a narrative review. World J Diabetes. 2015;6(8):1073-1081. doi: 10.4239/wjd.v6.i8.1073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Inzucchi SE, Bergenstal RM, Buse JB, et al. ; American Diabetes Association (ADA); European Association for the Study of Diabetes (EASD) . Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2012;35(6):1364-1379. doi: 10.2337/dc12-0413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kirkman MS, Briscoe VJ, Clark N, et al. ; Consensus Development Conference on Diabetes and Older Adults . Diabetes in older adults: a consensus report. J Am Geriatr Soc. 2012;60(12):2342-2356. doi: 10.1111/jgs.12035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Management of Diabetes Mellitus Guideline Update Working Group VA/DoD clinical practice guideline for the management of diabetes mellitus, 2010. Version 4.0. Veterans Health Administration and Department of Defense. Updated April 2017. Accessed August 17, 2019. https://www.healthquality.va.gov/guidelines/CD/diabetes/
- 22.Walter LC, Bertenthal D, Lindquist K, Konety BR. PSA screening among elderly men with limited life expectancies. JAMA. 2006;296(19):2336-2342. doi: 10.1001/jama.296.19.2336 [DOI] [PubMed] [Google Scholar]
- 23.Roumie CL, Greevy RA, Grijalva CG, et al. Association between intensification of metformin treatment with insulin vs sulfonylureas and cardiovascular events and all-cause mortality among patients with diabetes. JAMA. 2014;311(22):2288-2296. doi: 10.1001/jama.2014.4312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shorr RI, Ray WA, Daugherty JR, Griffin MR. Incidence and risk factors for serious hypoglycemia in older persons using insulin or sulfonylureas. Arch Intern Med. 1997;157(15):1681-1686. doi: 10.1001/archinte.1997.00440360095010 [DOI] [PubMed] [Google Scholar]
- 25.Capes SE, Hunt D, Malmberg K, Gerstein HC. Stress hyperglycaemia and increased risk of death after myocardial infarction in patients with and without diabetes: a systematic overview. Lancet. 2000;355(9206):773-778. doi: 10.1016/S0140-6736(99)08415-9 [DOI] [PubMed] [Google Scholar]
- 26.Garg R, Hurwitz S, Turchin A, Trivedi A. Hypoglycemia, with or without insulin therapy, is associated with increased mortality among hospitalized patients. Diabetes Care. 2013;36(5):1107-1110. doi: 10.2337/dc12-1296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Munshi MN, Slyne C, Segal AR, Saul N, Lyons C, Weinger K. Simplification of insulin regimen in older adults and risk of hypoglycemia. JAMA Intern Med. 2016;176(7):1023-1025. doi: 10.1001/jamainternmed.2016.2288 [DOI] [PubMed] [Google Scholar]
- 28.Sussman JB, Kerr EA, Saini SD, et al. Rates of deintensification of blood pressure and glycemic medication treatment based on levels of control and life expectancy in older patients with diabetes mellitus. JAMA Intern Med. 2015;175(12):1942-1949. doi: 10.1001/jamainternmed.2015.5110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tseng CL, Soroka O, Maney M, Aron DC, Pogach LM. Assessing potential glycemic overtreatment in persons at hypoglycemic risk. JAMA Intern Med. 2014;174(2):259-268. doi: 10.1001/jamainternmed.2013.12963 [DOI] [PubMed] [Google Scholar]
- 30.Thorpe CT, Gellad WF, Good CB, et al. Tight glycemic control and use of hypoglycemic medications in older veterans with type 2 diabetes and comorbid dementia. Diabetes Care. 2015;38(4):588-595. doi: 10.2337/dc14-0599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Leape LL, Brennan TA, Laird N, et al. The nature of adverse events in hospitalized patients: results of the Harvard Medical Practice Study II. N Engl J Med. 1991;324(6):377-384. doi: 10.1056/NEJM199102073240605 [DOI] [PubMed] [Google Scholar]
- 32.Thomas EJ, Brennan TA. Incidence and types of preventable adverse events in elderly patients: population based review of medical records. BMJ. 2000;320(7237):741-744. doi: 10.1136/bmj.320.7237.741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Krumholz HM. Post-hospital syndrome—an acquired, transient condition of generalized risk. N Engl J Med. 2013;368(2):100-102. doi: 10.1056/NEJMp1212324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lysy Z, Fung K, Giannakeas V, Fischer HD, Bell CM, Lipscombe LL. The association between insulin initiation and adverse outcomes after hospital discharge in older adults: a population-based cohort study. J Gen Intern Med. 2019;34(4):575-582. doi: 10.1007/s11606-019-04849-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wexler DJ, Beauharnais CC, Regan S, Nathan DM, Cagliero E, Larkin ME. Impact of inpatient diabetes management, education, and improved discharge transition on glycemic control 12 months after discharge. Diabetes Res Clin Pract. 2012;98(2):249-256. doi: 10.1016/j.diabres.2012.09.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Healy SJ, Black D, Harris C, Lorenz A, Dungan KM. Inpatient diabetes education is associated with less frequent hospital readmission among patients with poor glycemic control. Diabetes Care. 2013;36(10):2960-2967. doi: 10.2337/dc13-0108 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure. Cohort Construction Flowchart
eTable 1. Likelihood of Cohort Patients to Benefit From Stricter Glycemic Control
eTable 2. Rates of Diabetes Medication Intensification in Older Adults Following Hospitalization, by Inpatient and Outpatient Blood Glucose Control
eTable 3. Predictors of Diabetes Medication Intensification in Older Adults Following Hospitalization