Abstract
Background
Rare locations of hernias, as well as primary ventral hernias under certain circumstances (cirrhosis, dialysis, rectus diastasis, subsequent pregnancy), might be technically challenging. The aim was to identify situations where the treatment strategy might deviate from routine management.
Methods
The guideline group consisted of surgeons from the European and Americas Hernia Societies. The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach was used in formulating the recommendations. The Scottish Intercollegiate Guidelines Network (SIGN) critical appraisal checklists were used to evaluate the quality of full‐text papers. A systematic literature search was performed on 1 May 2018 and updated 1 February 2019. The Appraisal of Guidelines for Research and Evaluation (AGREE) instrument was followed.
Results
Literature was limited in quantity and quality. A majority of the recommendations were graded as weak, based on low quality of evidence. In patients with cirrhosis or on dialysis, a preperitoneal mesh repair is suggested. Subsequent pregnancy is a risk factor for recurrence. Repair should be postponed until after the last pregnancy. For patients with a concomitant rectus diastasis or those with a Spigelian or lumbar hernia, no recommendation could be made for treatment strategy owing to lack of evidence.
Conclusion
This is the first European and American guideline on the treatment of umbilical and epigastric hernias in patients with special conditions, including Spigelian and lumbar hernias. All recommendations were weak owing to a lack of evidence. Further studies are needed on patients with rectus diastasis, Spigelian and lumbar hernias.
This guideline addresses the treatment of umbilical and epigastric hernias in clinically challenging situations (cirrhosis, dialysis, subsequent pregnancy, rectus diastasis), as well as the treatment of Spigelian and primary lumbar hernias.
Emphasises the need for better evidence
Antecedentes
Las hernias de localización rara, así como las hernias ventrales primarias en determinadas circunstancias (cirrosis, diálisis, diástasis de recto, tras un embarazo) pueden ser complejas desde el punto de vista técnico. El objetivo fue identificar situaciones en las que la estrategia de tratamiento pudiera ser diferente del tratamiento habitual.
Métodos
Esta guía fue elaborada por cirujanos de las sociedades europeas y americana de hernia (European Hernia Society, EHS y American Hernia Society, AHS). La búsqueda sistemática de la literatura se efectuó el 1 de mayo de 2018 y se actualizó el 1 de febrero de 2019. Para evaluar la calidad de los artículos completos seleccionados se utilizó la normativa SIGN (Scottish Intercollegiate Guidelines Network). Las recomendaciones formuladas siguieron la metodología GRADE (Grading of Recommendations Assessment, Development and Evaluation) y la redacción de la guía siguió las normas AGREE (Appraisal of Guidelines for Research & Evaluation).
Resultados
La literatura es limitada en cantidad y calidad. La mayoría de las recomendaciones se calificaron como débiles en función de la baja calidad de la evidencia. En pacientes con cirrosis o en diálisis, se sugiere una reparación con malla preperitoneal. Un embarazo tras la reparación de una hernia es un factor de riesgo de recidiva. La reparación debería posponerse hasta después del último embarazo. Debido a la falta de evidencia no se pudo hacer ninguna recomendación para la reparación de hernias en pacientes con diástasis de recto concomitante o con hernias de Spigel o lumbares.
Conclusión
Esta es la primera guía europea y americana del tratamiento de hernias umbilicales y epigástricas en pacientes con patologías especiales, incluyendo las hernias de Spigel y lumbares. Todas las recomendaciones fueron débiles debido a la falta de evidencia. Se necesitan más estudios en pacientes con diástasis de recto, hernias de Spigel y lumbares.
Introduction
Procedures for umbilical and epigastric hernias are performed frequently in younger healthy individuals1. However, in clinical practice these hernias are sometimes seen in patients with special associated conditions where treatment strategy may be challenging. This could be in patients with cirrhosis, those on dialysis, women of childbearing age, or patients who have a rectus diastasis concomitant to a ventral hernia. A further clinical challenge is the diagnosis and treatment of rare primary ventral hernias, such as Spigelian and lumbar hernias.
As a part of the European (EHS) and Americas (AHS) Hernia Societies' guideline on the treatment of umbilical and epigastric hernias2, this separate guideline was developed with the aim of identifying situations where surgeons need to take special considerations into account, and where recommendations on treatment strategy might deviate from routine management.
Methods
The guideline group
The project was approved by the EHS and AHS boards in February 2017 as a part project of the guideline for treatment of primary ventral hernias. Two of the present authors were appointed to coordinate the project. The guideline was intended primarily for surgeons, but also for other physicians, general practitioners and patients. The guideline group members covered northern, southern and eastern Europe, together with Canada and the USA. The group consisted of 11 general surgeons and one plastic surgeon, all specialized in abdominal wall repair. Care was taken to include both open and laparoscopic surgeons, as well as surgeons with expertise in the creation of guidelines (both young PhD physicians and experienced researchers). Any conflict of interest (COI) for each member was analysed transparently and, when an issue existed, handled appropriately.
Timeline and meetings
A protocol including key questions (KQs) and timeline was approved at the AHS/EHS congress in Miami, Florida, USA, in March 2018, by eight group participants. The first guidelines meeting was held in Amsterdam, the Netherlands, in September 2018 with 11 participants; each team presented their systematic review of the literature for each subject, and recommendations were proposed. Subjects needing further work were identified. At the second meeting in February 2019 in Malmö, Sweden, all suggested recommendations were discussed, in some cases reformulated, and approved. A total of nine members participated and the remaining two contributed by approving the recommendations by e‐mail. All members of the group participated in person in at least two of the three meetings. The meetings were funded by the EHS and AHS. There was no involvement of industry.
Methodology
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach was used in formulating the recommendations. Scottish Intercollegiate Guidelines Network (SIGN) critical appraisal checklists were used to evaluate the quality of full‐text papers. KQs proposed by the two coordinators were revised and approved by the entire group.
The group was divided into teams (2–3 members per team) working on specific KQs. Each team decided on important outcomes of the specific questions using the PICO (patient, intervention, comparator, outcome) approach. A systematic literature review was performed for each KQ. When up‐to‐date high‐quality meta‐analyses or systematic reviews on the subject were available, the conclusions were derived from these. At the next level in quality were RCTs, and thereafter observational studies. Case series were included if they added substantial evidence information to the KQ, or if no higher level of evidence was available. Case reports and expert opinions were not included. The Appraisal of Guidelines for Research and Evaluation (AGREE) instrument was used to validate the guidelines ( Appendix SI , supporting information).
Literature search
A systematic literature search was performed by two of the present authors independently on 1 May 2018 and updated on 1 February 2019. The Cochrane Library, PubMed, Embase, CINAHL and Google Scholar were searched using Medical Subject Headings (MeSH) terms.
PubMed search terms were: (‘Liver Cirrhosis’[Mesh] OR ‘Ascites’[Mesh]) AND ‘Hernia, Ventral’[Majr]; ‘Peritoneal Dialysis’[Mesh] AND ‘Hernia, Ventral’[Majr]; ‘Hernia, Ventral’[Mesh] AND ‘Diastasis Recti And Weakness Of The Linea Alba’[Supplementary Concept]; rect* divarc* OR diast* AND umbilical hernia; (‘Pregnancy’[Mesh] OR ‘Reproductive Behavior’[Mesh] AND ‘Hernia, Ventral’[Majr]) AND Review[ptyp]; (Spigelian[All Fields] AND (‘hernia’[MeSH Terms] OR ‘hernia’[All Fields])); (grynfelt[All Fields] AND (‘hernia’[MeSH Terms] OR ‘hernia’[All Fields])) OR (petit's[All Fields] AND (‘hernia’[MeSH Terms] OR ‘hernia’[All Fields])).
The records were screened by title and abstract by two assessors independently for each subject. Full texts were evaluated by two assessors independently for eligibility with the use of SIGN critical appraisal checklists. Only papers rated as ‘acceptable’ or ‘high quality’ by SIGN were included, to limit the risk of bias. Any disagreement between assessors was settled by discussion either in the entire group or by a third assessor.
Results
Umbilical and epigastric hernia repair in patients with compromised liver function
Twelve KQs were formulated, and a total of 64 studies were finally included (Fig. 1).
Figure 1.
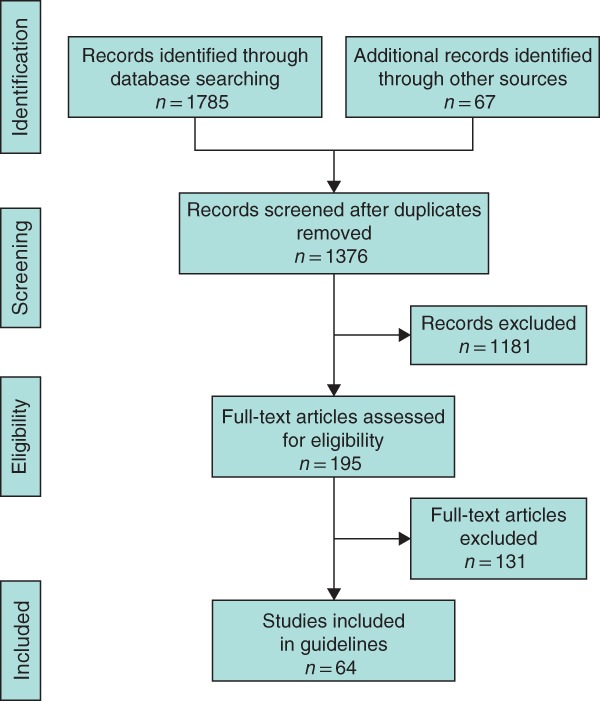
PRISMA flow diagram showing selection of articles for review
KQ 1: Should patients with compromised liver function be offered elective umbilical or epigastric hernia repair?
Statement: Acceptable evidence finds that elective umbilical hernia repair is safe in most patients with cirrhosis and/or ascites. Emergency repair is associated with a high rate of morbidity and mortality. Risk factors for poor outcome are a Model for End‐stage Liver Disease (MELD) score above 15, presence of ascites and albumin level below 3 g/dl. There is no evidence on epigastric hernia repair.
Recommendation: It is suggested to offer elective umbilical or epigastric hernia repair after optimization of liver function in patients with liver cirrhosis (MELD score below 15).
Quality of evidence:

Strength of recommendation: Weak
KQ 2: What is the preferred method of repair of an umbilical or epigastric hernia in patients with compromised liver function?
Statement: Acceptable evidence finds that open umbilical hernia repair with mesh is safe in patients with cirrhosis and/or ascites. Laparoscopic hernia repair seems safe in patients without ascites. In patients with ascites, the risk of complications increases. Sutured repair has a very high recurrence rate. There is no evidence on epigastric hernia repair.
Recommendation: It is suggested to use an open repair with onlay or preperitoneal mesh for umbilical or epigastric hernias in patients with compromised liver function.
Quality of evidence:

Strength of recommendation: Weak
Umbilical hernia is seen frequently in patients with cirrhosis and associated ascites, with a reported incidence of 20 per cent3. Perioperative morbidity and mortality may increase in patients with cirrhosis, making timing of surgery important. The 30‐day mortality rate after umbilical hernia repair in patients with cirrhosis has been reported to be around 5 per cent, compared with less than 1 per cent in the general population4, 5.
The severity of cirrhosis may be assessed using the Child–Pugh classification, including total bilirubin, serum albumin, prothrombin time or international normalized ratio (INR) level, presence of ascites and/or encephalopathy6. Elective surgery is generally accepted in patients with Child–Pugh grade A, and may be tolerated also in patients with grade B after preoperative optimization. Surgery in patients with Child–Pugh grade C is associated with a high risk of morbidity and mortality. Downstaging of Child–Pugh grades should be considered if possible6, 7.
The Model for End‐stage Liver Disease (MELD) score is a widely used scale predicting surgical morbidity and mortality (based on total bilirubin, INR and creatinine levels)8. Two large database studies9, 10 evaluated risk stratification for hernia repair in patients with ascites. The presence of non‐malignant ascites was a risk factor for increased morbidity at 30 days. Morbidity increased by approximately 3 per cent for each MELD score above 1510. This is consistent with findings by others5, demonstrating age above 65 years, MELD score above 15 and albumin level below 3 g/dl to be associated with increased morbidity after umbilical hernia repair. A nomogram has been proposed9 based on a multivariable logistic regression analysis, including MELD score, white blood cell count, platelets and albumin to predict mortality in patients with ascites undergoing umbilical hernia repair.
One high‐quality review11 from 2012 on non‐hepatic surgery in patients with cirrhosis included a separate section on abdominal wall surgery based on one RCT12, two large database studies13, 14 and two retrospective case series15, 16. A further four large database studies5, 9, 10, 17 from the American College of Surgeons' National Surgical Quality Improvement Program were identified.
Elective umbilical hernia repair with mesh in patients with cirrhosis is associated with low morbidity and mortality rates, comparable to rates in non‐cirrhotic patients5, 14. Sutured repair with non‐absorbable sutures resulted in a high recurrence rate of 15 per cent at 6 months' follow‐up5, 14. Cirrhotic patients who have an emergency umbilical hernia repair have a higher complication rate than those having planned surgery. Some 26–37 per cent of patients not planned for any surgical intervention did receive an emergency repair later5, 14. Emergency repair results in a sevenfold increased mortality rate11, 13.
Thirty‐day mortality was compared in patients with a MELD score above 9 who underwent either open or laparoscopic elective ventral hernia repair, including both primary and incisional hernias17. Overall, laparoscopic ventral hernia repair was associated with fewer wound‐related complications and a shorter length of stay. However, in a subgroup analysis of patients with ascites, laparoscopic repair was associated with systemic complications and mortality17.
Whether or not patients with cirrhosis and completely asymptomatic hernias should be offered elective hernia repair solely due to the risk of having an emergency repair is difficult to say, based on current evidence. Although retrospective database studies did suggest a high risk of emergency repair, studies of non‐operative management with long‐term follow‐up are lacking. However, it is suggested that symptomatic patients with cirrhosis and a MELD score below 15 are offered elective hernia repair. None of the studies evaluated the effect of preoperative optimization in patients with cirrhosis. It seems though reasonable to consult a hepatologist for optimization before elective surgery.
Sutured repair with non‐absorbable sutures leads to a very high recurrence rate. Laparoscopic technique increases the risk of complications in patients with ascites. It is suggested that an open mesh repair technique is used in patients with ascites.
Umbilical and epigastric hernia repair in patients on peritoneal dialysis
KQ 3: Should an umbilical or epigastric hernia be repaired before or during peritoneal dialysis?
Statement: It is unknown whether an asymptomatic umbilical or epigastric hernia repair may become symptomatic during peritoneal dialysis. The presence of a hernia may complicate peritoneal dialysis, as the hernia can enlarge over time from the instilled fluid. Repair of an umbilical or epigastric hernia before or during peritoneal dialysis is associated with low morbidity.
Recommendation: It is suggested to repair an umbilical or epigastric hernia before initiation of peritoneal dialysis. It seems safe to perform the hernia repair during peritoneal dialysis.
Quality of evidence:

Strength of recommendation: Weak
KQ 4: What is the preferred method of repair for an umbilical or epigastric hernia in patients on peritoneal dialysis?
Statement: Acceptable evidence finds that open umbilical or epigastric hernia repair without access to the peritoneal cavity is associated with low morbidity and recurrence rates. There are no data on laparoscopic umbilical or epigastric hernia repair before or during peritoneal dialysis.
Recommendation: An open umbilical or epigastric hernia repair using onlay or preperitoneal mesh placement is suggested for patients on peritoneal dialysis.
Quality of evidence:

Strength of recommendation: Weak
The frequency of umbilical hernia in patients having peritoneal dialysis is reported to be 3–15 per cent in retrospective case series18, 19. It is likely that many of these hernias were already present before peritoneal dialysis was initiated, as concluded in a prospective case series20.
One large database study21, one observational prospective study20 and some retrospective case series18, 19, 22, 23 were identified that addressed umbilical hernias in patients on peritoneal dialysis. No reviews, RCTs or studies evaluating watchful waiting or outcomes after different types of hernia repair in patients on peritoneal dialysis were available.
The presence of an abdominal wall hernia may complicate peritoneal dialysis, as the hernia is filled with fluid and may enlarge over time. It is not known whether an asymptomatic ventral hernia diagnosed before dialysis initiation will become symptomatic during dialysis. One study21 found that the hernia formation during peritoneal dialysis was associated with withdrawal of dialysis. Another study22 concluded that neither the incidence nor management of the hernia affected renal function. An umbilical hernia is suggested to be repaired before peritoneal dialysis initiation24. If an umbilical hernia develops during peritoneal dialysis, repair is associated with low morbidity18, 25.
Umbilical hernia repair was reported during ongoing peritoneal dialysis in a total of 54 patients18, 23, 25. Open repair with placement of a preperitoneal or onlay mesh without access to the peritoneal cavity was reported to be associated with low morbidity and no recurrences. However, if no mesh was implanted, the recurrence rate was 12 per cent23. Owing to raised intra‐abdominal pressure in peritoneal dialysis, mesh insertion seems advantageous. No studies evaluated the role of laparoscopic hernia repair, but it seems logical to consider the risks of port‐site hernia, fluid leakage from port sites, and intraperitoneal mesh placement.
It is suggested that an umbilical or epigastric hernia is repaired before the initiation of peritoneal dialysis. If an umbilical or epigastric hernia develops during peritoneal dialysis, it is suggested that it is repaired using an open mesh repair technique without accessing the peritoneal cavity.
Ventral hernia repair in the setting of rectus diastasis
KQ 5: What is the optimal surgical approach to an umbilical or epigastric hernia with a concomitant rectus diastasis?
Statement: There is insufficient evidence to recommend a specific type of repair for umbilical or epigastric hernias with a concomitant rectus diastasis. The presence of a rectus diastasis is a known risk factor for recurrence after sutured repair.
Recommendation: It is suggested to use a mesh repair for umbilical and epigastric hernias in patients with rectus diastasis. Simultaneous rectus diastasis repair is optional.
Quality of evidence:

Strength of recommendation: Weak
Rectus diastasis is characterized by a thinning and widening of the linea alba26. A large rectus diastasis can cause similar complaints to a large ventral hernia, but does not have the risk of incarceration or strangulation27, 28, 29. Rectus diastasis can be classified by quantitative and qualitative classification systems30, 31, 32.
The presence of a rectus diastasis and a concomitant umbilical or epigastric hernia presents a significant challenge with respect to operative management. The recurrence rate after small umbilical or epigastric hernia repair with a concomitant rectus diastasis has been reported to be higher than that in patients without a rectus diastasis33. The literature is limited. Six studies were identified: three prospective cohort27, 34, 35 and three retrospective36, 37, 38 studies.
Endoscopic repair with plication of the diastasis using a non‐absorbable loop suture followed by an onlay or preperitoneal polypropylene mesh was performed of the midline hernia and the coexisting rectus diastasis in three studies27, 34, 35. The studies of Köckerling and colleagues34 and Claus et al.35 included both incisional and primary ventral hernias, and Bellido Luque and co‐workers27 included solely primary ventral hernias. Follow‐up was 20 months, 8 months and 1 year respectively. The main complication was seroma, which occurred in up to 27% of the patients35. It was concluded that endoscopic repair is feasible, with a low number of wound impairments. One study35 reported one recurrence of the diastasis, whereas no recurrences of either the umbilical hernia or the rectus diastasis were reported by the others27, 34.
Two retrospective cohort studies36, 37 analysed open suture plication of the diastasis and concomitant ventral hernia by polydioxanone or polypropylene followed by polypropylene mesh placement. Short‐term outcomes showed eight cases of minor wound dehiscence and five of haematoma/seroma in 50 patients36, and two seromas and no wound infections in 32 patients37. Follow‐up was 2–8 years36 and mean 15 months37, with no recurrences or bulging. A retrospective cohort study38 described an open technique with self‐fixating mesh in the preperitoneal space extending superiorly including27 the umbilical hernia, with no wound complications but one hernia recurrence in 58 patients.
Data are lacking concerning the indication for surgery in the included studies. Whether it was pain from the hernia, bulging, core instability or cosmesis is unknown, which is key for examining the effect of surgery. Furthermore, patient‐related outcomes measures are generally lacking, and recurrence may not be the most important outcome.
Based on limited data, both open and endoscopic repair techniques for umbilical hernia in combination with rectus diastasis repair are feasible. The presence of a rectus diastasis seems to be a risk factor for hernia recurrence, and mesh augmentation of the hernia is therefore suggested. Simultaneous repair of the diastasis is optional and needs to be discussed with the patient. It might be helpful to consider collaboration with a plastic surgeon, especially if there is skin surplus.
Primary ventral hernia repair in women of childbearing age
KQ 6: Should women of childbearing age with symptomatic umbilical or epigastric hernia be offered elective hernia repair?
Statement: Elective umbilical and epigastric hernia repair is safe in women in childbearing age. Subsequent pregnancy after hernia repair is associated with an increased risk of recurrence, which is why surgery should be postponed until after last planned pregnancy, whenever possible. A watchful waiting approach is safe when having a reducible hernia during pregnancy.
Recommendation: Elective umbilical and epigastric hernia repair should, if possible, be postponed until after pregnancy and preferably until after last pregnancy in women of childbearing age.
Quality of evidence:

Strength of recommendation: Strong (upgraded)
KQ 7: Which is the preferred repair method for women of childbearing age with a symptomatic umbilical or epigastric hernia?
Statement: For women of childbearing age becoming pregnant subsequent to an umbilical and epigastric hernia repair, the use of mesh seems to decrease the recurrence rate, but increases the risk of chronic pain significantly compared with a sutured repair.
Recommendation: If hernia repair cannot be postponed until after the last pregnancy, a sutured repair is suggested for umbilical and epigastric hernias in women of childbearing age. A mesh repair could be performed after the last pregnancy.
Quality of evidence:

Strength of recommendation: Weak
Primary ventral hernia repair is commonly performed in women of childbearing age39. Physiological changes of the abdominal wall during pregnancy may increase the risk of recurrence, which is why optimal timing of the repair is important for women of childbearing age. The current recommendations are based on four large cohort studies and two systematic reviews39, 40, 41, 42, 43.
In a large national cohort study39, the frequency of primary ventral hernia repair was assessed in 470 000 women of childbearing age. The cumulative incidence was 14 per cent over a 10‐year period. Having a subsequent pregnancy after a hernia repair resulted in a 1·6‐fold increased risk of recurrence. There was a sevenfold increased risk in parous women having a hernia repair compared with the risk in nulliparous women.
A primary ventral hernia diagnosed during pregnancy was uncommon: 0·08 per cent in a large register‐based study of more than 20 000 women44. None underwent elective or emergency repair during pregnancy. All had an uncomplicated childbirth. During postpartum follow‐up (median 4·4 years), a total of five women (0·02 per cent) had an elective primary ventral hernia repair.
The most recent systematic review39 included nine studies of both primary ventral and incisional hernias in women of childbearing age. Results for type of repair were not analysed separately, but the incidence of incisional hernia was probably low in comparison with primary ventral hernias in this age group. All included studies were retrospective except one that included more than 35 000 women. Three outcomes were reported: risk of recurrence after prepregnancy ventral hernia repair; safety of umbilical hernia repair during pregnancy; and repair in combination with caesarean section. Prepregnancy repair was associated with an increased risk of having a ventral hernia recurrence after delivery. Repair during pregnancy was recommended to be reserved for emergency cases. Routine repair at caesarean section has been reported to be safe45. Data suggest that an umbilical hernia can be left untreated at caesarean section, as postpartum repair is seldom needed.
In a national register‐based study41, 224 women were identified who had either an umbilical or an epigastric hernia repair and subsequently became pregnant. The cumulative reoperation rate for recurrence was 16 per cent after mesh repair and 11 per cent after suture repair (adjusted for BMI and hernia defect size). In contrast, in a recent questionnaire study46, 195 women of childbearing age with a history of umbilical or epigastric hernia repair who subsequently became pregnant were compared with a propensity‐matched controlled group of 246 women; the use of mesh was found to be independently associated with reduced recurrence rates. However, the use of mesh was associated with an increased risk of chronic pain (17·5 per cent) compared to that for suture repair (9·5 per cent) when having a subsequent pregnancy.
Primary ventral hernia is rare during pregnancy, and the incidence of emergency repair is extremely low. An operation, if needed, can be safely postponed until after pregnancies. A mesh repair may decrease the risk of recurrence, but increase the risk of chronic pain. As there are pros and cons of using mesh versus suture, the risks should be discussed with the patient, leading to a shared decision on repair and/or type of technique. If hernia repair cannot be postponed until after the last pregnancy, it is suggested to use a sutured repair for umbilical and epigastric hernias in women of childbearing age.
Spigelian hernia
KQ 8: What is the definition of a Spigelian hernia and how are they classified?
Statement: A Spigelian hernia is a protrusion through a defect in the aponeurosis of the transverse abdominal muscle limited by the semilunar line and the lateral edge of the rectus muscle (Fig. 2).
Recommendation: No specific classification system for Spigelian hernias exists, but it is recommended to use the existing EHS classification system for ventral hernias.
Quality of evidence:

Strength of recommendation: Strong (upgraded)
Figure 2.
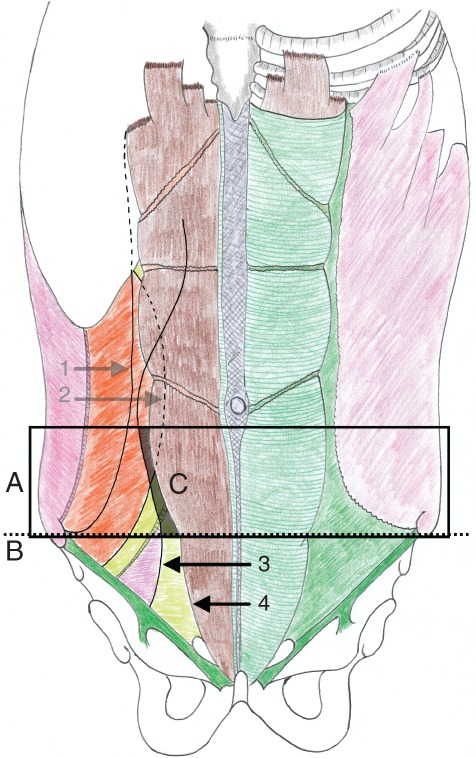
Anatomical location of Spigelian hernias A, Spigelian hernia belt: transverse 6‐cm wide zone above the interspinal plane; B, interspinal plane; C, Spigelian fascia; 1, muscular–aponeurosis transition of external oblique muscle; 2, muscular–aponeurosis transition of internal oblique muscle; 3, muscular–aponeurosis transition of transverse abdominal muscle; 4, lateral edge of rectus muscle (artist: Y. Renard).
KQ 9: Which diagnostic modalities are the most suitable for diagnosing Spigelian hernias?
Statement: Dynamic ultrasonography, CT and MRI are modalities that could be useful in combination with clinical examination for diagnosing Spigelian hernias. In unclear cases, diagnostic laparoscopy could be of value in symptomatic patients, offering a simultaneous repair in the case of a positive finding.
Recommendation: Clinical examination, ultrasonography or CT is suggested for diagnosing a Spigelian hernia.
Quality of evidence:

Strength of recommendation: Weak
KQ 10: Which is the preferred method of repair for Spigelian hernias?
Statement: Open and laparoscopic repair have been described. Data are limited on the preferred method. If there is no palpable lump, laparoscopic repair may be advantageous.
Recommendation: It is suggested to repair a Spigelian hernia with the use of mesh. An open or laparoscopic approach may be used, based on the surgeon's expertise.
Quality of evidence:

Strength of recommendation: Weak
The Spigelian hernia got its name from the Flemish anatomist/surgeon, Adriaan van den Spieghel. He was the first to describe the semilunar line in 164547. The first description of a Spigelian hernia was in 1764 by the Czech anatomist, Josef Thaddäus Klinkosch (1735–1778)48. The Latin terms hernia spigeli and hernia lineae semilunari are also used. Literature is sparse, including only a limited number of patients. Three reviews, one RCT and one prospective case series were identified49, 50, 51, 52, 53.
A Spigelian hernia is the protrusion of preperitoneal fat, peritoneal sac or organ(s) through a congenital or acquired defect in the Spigelian aponeurosis (the aponeurosis of the transverse abdominal muscle limited by the linea semilunaris laterally and by the lateral edge of the rectus muscle medially). These hernias are commonly located in the ‘Spigelian hernia belt’, a 6‐cm wide zone above the interspinal plane (Fig. 2). The hernias can be either interstitial between the lateral muscles in the abdominal wall or subcutaneous. Sometimes only preperitoneal fat is protruding, without a peritoneal sac54. No specific classification system exists, but the EHS classification system for ventral hernia includes Spigelian hernias55.
Spigelian hernias are difficult to diagnose unless causing symptoms56. The incidence of Spigelian hernia is unknown, but seems to be higher in the fourth to seventh decade of life, including more women than men, and more left‐sided than right‐sided52, 56. It has been reported52, 56 that 17–25 per cent of Spigelian hernias are operated on as emergency cases, sometimes with incarceration of small bowel. The risk of incarceration is increased in patients with a high BMI, age above 50 years and in women57. Occult hernia orifices are sometimes found at laparoscopy for any indication and reported in 2 per cent of adults58.
One study59 evaluated the diagnostic accuracy of clinical examination, CT and ultrasonography compared with the operative findings in 54 patients. CT showed a sensitivity of 100 per cent and a positive predictive value (PPV) of 100 per cent, and ultrasonography a sensitivity of 90 per cent and a PPV of 100 per cent compared with operative findings, whereas clinical examination alone had a sensitivity of 100 per cent and a PPV of 36 per cent59.
One RCT53 compared 11 laparoscopic with 11 open repairs performed as a total extraperitoneal (TEP) repair or an intraperitoneal onlay mesh (IPOM). Patients repaired by the open approach had significantly more wound complications and a longer hospital stay. However, the number of included patients was too small to draw any valid conclusions. In a prospective case series50 from the same group, including 16 patients undergoing either TEP or IPOM repair, there were no differences in postoperative morbidity and no recurrences at 48 months' follow‐up.
In summary, for classification of Spigelian hernias it is recommended to use the EHS classification, and for diagnosis it is suggested to use clinical examination, ultrasonography or CT. For repair of a Spigelian hernia, a laparoscopic approach may decrease wound complications, and may be advantageous for both diagnostic and curable intervention if there is no palpable lump. Owing to limited data, no recommendation on a specific surgical method can be made. Either an open or laparoscopic approach may be used, based on the surgeon's expertise.
Lumbar hernias
KQ 11: What is the definition of a primary lumbar hernia, and how are these hernias classified?
Statement: A primary lumbar hernia is a defect in the lumbar region, which is bounded by the 12th rib above, the iliac crest below, the free border of the external oblique muscles anteriorly, and the vertebral column posteriorly. Primary lumbar hernias may be subclassified anatomically as superior (Grynfeltt–Lesshaft) or inferior (Petit) (Fig. 3).
Recommendation: No specific classification system for lumbar hernias exists, but it is suggested to use the existing EHS classification system for ventral hernias.
Quality of evidence:

Strength of recommendation: Weak
Figure 3.
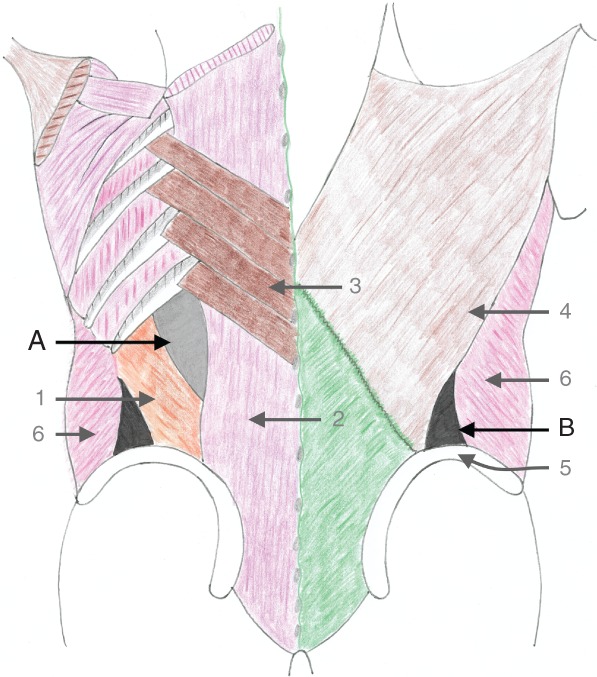
Anatomical location of primary lumbar hernias A, Grynfeltt–Lesshaft triangle (superior lumbar triangle); B, Petit's triangle (inferior lumbar triangle); 1, internal oblique muscle; 2, quadratus lumborum and erector spinae muscles; 3, serratus posterior inferior muscle; 4, latissimus dorsi muscle; 5, iliac crest; 6, external oblique muscle (artist: Y. Renard).
KQ 12: What is the preferred repair method for primary lumbar hernias?
Statement: Open and laparoscopic repair have been described for lumbar hernias. No data on the preferred method exists.
Recommendation: As lumbar hernias are rare, it is suggested to consider referring the patient to a specialized hernia centre.
Quality of evidence:

Strength of recommendation: Weak
Hernias located in the lumbar region may be acquired after trauma or retroperitoneal surgery as incisional hernias60, 61. Primary or spontaneous lumbar hernias are rare, and are the only ones addressed in this guideline.
The literature search revealed two reviews61, 62 of acceptable quality and two papers60, 63 describing atypical ventral hernias. Further, a number of anatomical and radiological studies were identified23, 64, 65, 66. There were no RCTs, cohort studies or case series evaluating surgical technique and/or outcomes after primary lumbar hernia repair.
A lumbar hernia is defined as a hernia located in the lumbar region60, 63, 65. The lumbar region is bounded by the 12th rib above, the iliac crest below, the free border of the external oblique muscles anteriorly, and the vertebral column and the erector spinae muscles posteriorly. Primary lumbar hernias may be subclassified anatomically as superior (Grynfeltt–Lesshaft) or inferior (Petit) lumbar hernias61 (Fig. 3). The superior lumbar triangle is the area for penetration of the 12th intercostal nerve pedicle, and is the most common location for primary lumbar hernias65.
CT or MRI is recommended to confirm the diagnosis, assess the anatomical location and plan a suitable repair60, 61, 62, 63. It is unknown whether a watchful waiting strategy is safe, and which patients will benefit from repair.
Repairing a lumbar hernia may be a surgical challenge because of the proximity to bony structures, which may limit proper dissection and mesh overlap61. A lumbar hernia may be repaired by an open approach with preperitoneal mesh placement or by a laparoscopic approach with preperitoneal or intraperitoneal mesh placement60, 61, 62. As lumbar hernias are rare, it may be considered to refer patients to a specialized hernia centre.
Comment
This guideline addresses a small, but clinically challenging, population of patients. Overall, the amount of evidence is limited in both quantity and quality, which is why the majority of recommendations were weak. The guideline for treatment of umbilical and epigastric hernias from the EHS and AHS suggests using open repair with a preperitoneal flat mesh for the vast majority of patients2. In patients with compromised liver function or on dialysis, the same repair method is suggested in the present guideline. For patients with a concomitant rectus diastasis, the optimal repair method for umbilical and epigastric hernia is unknown, but a mesh is suggested owing to the increased risk of recurrence. For women of childbearing age, subsequent pregnancy increases the recurrence rate, and for this reason repair should be postponed until after the last pregnancy. There are insufficient data to suggest a particular repair method for Spigelian and primary lumbar hernias.
Perspectives
Umbilical or epigastric hernia repair in patients with a concomitant rectus diastasis is an unexplored area from a scientific perspective. Both RCTs and database studies are warranted to evaluate the optimal treatment strategy. The treatment of umbilical and epigastric hernias in women of childbearing age has been examined widely by a group from Denmark. However, it remains unclear whether repair should be performed with or without mesh in women planning a subsequent pregnancy. Spigelian and primary lumbar hernias are rare, and the available evidence is consequently sparse. Prospective database studies are needed to clarify the optimal treatment strategies.
To evaluate the best repair method for rare hernias, large database studies might be the best option to collect wider experience of both indications for operation and operative techniques to be used. The information on both preoperative important patient and hernia conditions, as well as technical details at surgery, needs to be addressed thoroughly in the registers in order to have a fair chance of comparing the techniques used. These details would preferably be addressed internationally and coordinated for use in registers globally. A minimum core outcome data set should be identified.
An update of the guideline is planned for 2023. Significant results from new research are not likely to be presented before this that would change the present recommendations.
Supporting information
Appendix S1 Validation of the EHS and AHS guidelines using the AGREE instrument
Acknowledgements
The two guideline coordinators were N.A.H. and M.P.S.
N.A.H. has an indirect COI as a member of the Danish Hernia Database steering committee and has attended an industry‐sponsored meeting. A.M. is a member of the EHS board and has received speaker's fees from Intuitive and Bard (direct COI). R.K. has been at sponsored meetings (indirect COI). F.B. has received speaker's fees from Medtronic and Acelity (direct COI). J.F. has received speaker's fees from Bard, Gore and Allergan (direct COI). W.H. has received speaker's fees from Bard, Gore and Intuitive, and is a member of advisory boards for Mesh Suture and Deep Blue Medical (direct COI). D.K. has received speaker's fees from Gore, Bard and Cook (direct COI). R.L. has a direct COI in terms of speaker's fees from Medtronic and training courses from Bard (fee), and an indirect COI from being a member of the EHS board, participation in sponsored meetings, and being part of Hernientage and HerniaMed. Y.R. has received research funding from Medtronic, Bard and Hartmann (direct COI). M.A.G.U. has received speaker's fees from Gore, Medtronic and Dynamesh. M.P.S. is a member of the EHS board and participated in sponsored meetings (indirect COI).
Disclosure The authors declare no other conflicts of interest.
Funding information
Guideline meetings funded by the European Hernia Society and Americas Hernia Society
References
- 1. Helgstrand F, Jorgensen LN, Rosenberg J, Kehlet H, Bisgaard T. Nationwide prospective study on readmission after umbilical or epigastric hernia repair. Hernia 2013; 17: 487–492. [DOI] [PubMed] [Google Scholar]
- 2. Henriksen NA, Montgomery A, Kaufmann R, Berrevoet F, East B, Fischer J et al Guidelines for treatment of umbilical and epigastric hernias from the European Hernia Society and Americas Hernia Society. BJS 2020; 10.1002/bjs.11489 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 3. Coelho JC, Claus CM, Campos AC, Costa MA, Blum C. Umbilical hernia in patients with liver cirrhosis: a surgical challenge. World J Gastrointest Surg 2016; 8: 476–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hansen JB, Thulstrup AM, Vilstup H, Sorensen HT. Danish nationwide cohort study of postoperative death in patients with liver cirrhosis undergoing hernia repair. Br J Surg 2002; 89: 805–806. [DOI] [PubMed] [Google Scholar]
- 5. Cho SW, Bhayani N, Newell P, Cassera MA, Hammill CW, Wolf RF w Umbilical hernia repair in patients with signs of portal hypertension: surgical outcome and predictors of mortality. Arch Surg 2012; 147: 864–869. [DOI] [PubMed] [Google Scholar]
- 6. Millwala F, Nguyen GC, Thuluvath PJ. Outcomes of patients with cirrhosis undergoing non‐hepatic surgery: risk assessment and management. World J Gastroenterol 2007; 13: 4056–4063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McKay A, Dixon E, Bathe O, Sutherland F. Umbilical hernia repair in the presence of cirrhosis and ascites: results of a survey and review of the literature. Hernia 2009; 13: 461–468. [DOI] [PubMed] [Google Scholar]
- 8. Northup PG, Wanamaker RC, Lee VD, Adams RB, Berg CL. Model for End‐Stage Liver Disease (MELD) predicts nontransplant surgical mortality in patients with cirrhosis. Ann Surg 2005; 242: 244–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Saleh F, Okrainec A, Cleary SP, Jackson TD. Management of umbilical hernias in patients with ascites: development of a nomogram to predict mortality. Am J Surg 2015; 209: 302–307. [DOI] [PubMed] [Google Scholar]
- 10. Ecker BL, Bartlett EK, Hoffman RL, Karakousis GC, Roses RE, Morris JB et al Hernia repair in the presence of ascites. J Surg Res 2014; 190: 471–477. [DOI] [PubMed] [Google Scholar]
- 11. de Goede B, Klitsie PJ, Lange JF, Metselaar HJ, Kazemier G. Morbidity and mortality related to non‐hepatic surgery in patients with liver cirrhosis: a systematic review. Best Pract Res Clin Gastroenterol 2012; 26: 47–59. [DOI] [PubMed] [Google Scholar]
- 12. Ammar SA. Management of complicated umbilical hernias in cirrhotic patients using permanent mesh: randomized clinical trial. Hernia 2010; 14: 35–38. [DOI] [PubMed] [Google Scholar]
- 13. Carbonell AM, Wolfe LG, DeMaria EJ. Poor outcomes in cirrhosis‐associated hernia repair: a nationwide cohort study of 32 033 patients. Hernia 2005; 9: 353–357. [DOI] [PubMed] [Google Scholar]
- 14. Gray SH, Vick CC, Graham LA, Finan KR, Neumayer LA, Hawn MT. Umbilical herniorrhapy in cirrhosis: improved outcomes with elective repair. J Gastrointest Surg 2008; 12: 675–681. [DOI] [PubMed] [Google Scholar]
- 15. Marsman HA, Heisterkamp J, Halm JA, Tilanus HW, Metselaar HJ, Kazemier G. Management in patients with liver cirrhosis and an umbilical hernia. Surgery 2007; 142: 372–375. [DOI] [PubMed] [Google Scholar]
- 16. Eker HH, van Ramshorst GH, de Goede B, Tilanus HW, Metselaar HJ, de Man RA et al A prospective study on elective umbilical hernia repair in patients with liver cirrhosis and ascites. Surgery 2011; 150: 542–546. [DOI] [PubMed] [Google Scholar]
- 17. Juo YY, Skancke M, Holzmacher J, Amdur RL, Lin PP, Vaziri K. Laparoscopic versus open ventral hernia repair in patients with chronic liver disease. Surg Endosc 2017; 31: 769–777. [DOI] [PubMed] [Google Scholar]
- 18. Banshodani M, Kawanishi H, Moriishi M, Shintaku S, Ago R, Hashimoto S et al Umbilical hernia in peritoneal dialysis patients: surgical treatment and risk factors. Ther Apher Dial 2015; 19: 606–610. [DOI] [PubMed] [Google Scholar]
- 19. Del Peso G, Bajo MA, Costero O, Hevia C, Gil F, Diaz C et al Risk factors for abdominal wall complications in peritoneal dialysis patients. Perit Dial Int 2003; 23: 249–254. [PubMed] [Google Scholar]
- 20. Celdran A, Bazire P, Garcia‐Urena MA, Marijuan JL. H‐hernioplasty: a tension‐free repair for umbilical hernia. Br J Surg 1995; 82: 371–372. [DOI] [PubMed] [Google Scholar]
- 21. Yang SF, Liu CJ, Yang WC, Chang CF, Yang CY, Li SY et al The risk factors and the impact of hernia development on technique survival in peritoneal dialysis patients: a population‐based cohort study. Perit Dial Int 2015; 35: 351–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Balda S, Power A, Papalois V, Brown E. Impact of hernias on peritoneal dialysis technique survival and residual renal function. Perit Dial Int 2013; 33: 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Martinez‐Mier G, Garcia‐Almazan E, Reyes‐Devesa HE, Garcia‐Garcia V, Cano‐Gutierrez S, Mora YFR et al Abdominal wall hernias in end‐stage renal disease patients on peritoneal dialysis. Perit Dial Int 2008; 28: 391–396. [PubMed] [Google Scholar]
- 24. Ros S, Bajo A, del Peso G, Garcia de Miguel A, Santacruz S, Fernandez E et al Cystatin C as marker of residual renal function in patients on peritoneal dialysis: relation with parameters of peritoneal function. J Nephrol 2007; 20: 468–473. [PubMed] [Google Scholar]
- 25. Garcia‐Urena MA, Rodriguez CR, Vega Ruiz V, Carnero Hernandez FJ, Fernandez‐Ruiz E, Vazquez Gallego JM et al Prevalence and management of hernias in peritoneal dialysis patients. Perit Dial Int 2006; 26: 198–202. [PubMed] [Google Scholar]
- 26. Brauman D. Diastasis recti: clinical anatomy. Plast Reconstr Surg 2008; 122: 1564–1569. [DOI] [PubMed] [Google Scholar]
- 27. Bellido Luque J, Bellido Luque A, Valdivia J, Suarez Grau JM, Gomez Menchero J, Garcia Moreno J et al Totally endoscopic surgery on diastasis recti associated with midline hernias. The advantages of a minimally invasive approach. Prospective cohort study. Hernia 2015; 19: 493–501. [DOI] [PubMed] [Google Scholar]
- 28. Gunnarsson U, Stark B, Dahlstrand U, Strigard K. Correlation between abdominal rectus diastasis width and abdominal muscle strength. Dig Surg 2015; 32: 112–116. [DOI] [PubMed] [Google Scholar]
- 29. Emanuelsson P, Gunnarsson U, Dahlstrand U, Strigard K, Stark B. Operative correction of abdominal rectus diastasis (ARD) reduces pain and improves abdominal wall muscle strength: a randomized, prospective trial comparing retromuscular mesh repair to double‐row, self‐retaining sutures. Surgery 2016; 160: 1367–1375. [DOI] [PubMed] [Google Scholar]
- 30. Nahas FX. An aesthetic classification of the abdomen based on the myoaponeurotic layer. Plast Reconstr Surg 2001; 108: 1787–1795. [DOI] [PubMed] [Google Scholar]
- 31. Beer GM, Schuster A, Seifert B, Manestar M, Mihic‐Probst D, Weber SA. The normal width of the linea alba in nulliparous women. Clin Anat 2009; 22: 706–711. [DOI] [PubMed] [Google Scholar]
- 32. Reinpold W, Kockerling F, Bittner R, Conze J, Fortelny R, Koch A et al Classification of rectus diastasis – a proposal by the German Hernia Society (DHG) and the International Endohernia Society (IEHS). Front Surg 2019; 6: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kohler G, Luketina RR, Emmanuel K. Sutured repair of primary small umbilical and epigastric hernias: concomitant rectus diastasis is a significant risk factor for recurrence. World J Surg 2015; 39: 121–126. [DOI] [PubMed] [Google Scholar]
- 34. Köckerling F, Botsinis MD, Rohde C, Reinpold W, Schug‐Pass C. Endoscopic‐assisted linea alba reconstruction: new technique for treatment of symptomatic umbilical, trocar, and/or epigastric hernias with concomitant rectus abdominis diastasis. Eur Surg 2017; 49: 71–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Claus CMP, Malcher F, Cavazzola LT, Furtado M, Morrell A, Azevedo M et al Subcutaneous onlay laparoscopic approach (SCOLA) for ventral hernia and rectus abdominis diastasis repair: technical description and initial results. Arq Bras Cir Dig 2018; 31: e1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kulhanek J, Mestak O. Treatment of umbilical hernia and recti muscles diastasis without a periumbilical incision. Hernia 2013; 17: 527–530. [DOI] [PubMed] [Google Scholar]
- 37. Cheesborough JE, Dumanian GA. Simultaneous prosthetic mesh abdominal wall reconstruction with abdominoplasty for ventral hernia and severe rectus diastasis repairs. Plast Reconstr Surg 2015; 135: 268–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Privett BJ, Ghusn M. Proposed technique for open repair of a small umbilical hernia and rectus divarication with self‐gripping mesh. Hernia 2016; 20: 527–530. [DOI] [PubMed] [Google Scholar]
- 39. Oma E, Jensen KK, Bisgaard T, Jorgensen LN. Association of primary ventral hernia and pregnancy. Ann Surg 2018; 10.1097/SLA.0000000000003170 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 40. Oma E, Jensen KK, Jorgensen LN. Increased risk of ventral hernia recurrence after pregnancy: a nationwide register‐based study. Am J Surg 2017; 214: 474–478. [DOI] [PubMed] [Google Scholar]
- 41. Oma E, Jensen KK, Jorgensen LN. Recurrent umbilical or epigastric hernia during and after pregnancy: a nationwide cohort study. Surgery 2016; 159: 1677–1683. [DOI] [PubMed] [Google Scholar]
- 42. Jensen KK, Henriksen NA, Jorgensen LN. Abdominal wall hernia and pregnancy: a systematic review. Hernia 2015; 19: 689–696. [DOI] [PubMed] [Google Scholar]
- 43. Oma E, Henriksen NA, Jensen KK. Ventral hernia and pregnancy: a systematic review. Am J Surg 2019; 217: 163–168. [DOI] [PubMed] [Google Scholar]
- 44. Oma E, Bay‐Nielsen M, Jensen KK, Jorgensen LN, Pinborg A, Bisgaard T. Primary ventral or groin hernia in pregnancy: a cohort study of 20 714 women. Hernia 2017; 21: 335–339. [DOI] [PubMed] [Google Scholar]
- 45. Ozdogan M, Yildiz F, Gurer A, Orhun S, Kulacoglu H, Aydin R. Changes in collagen and elastic fiber contents of the skin, rectus sheath, transversalis fascia and peritoneum in primary inguinal hernia patients. Bratisl Lek Listy 2006; 107: 235–238. [PubMed] [Google Scholar]
- 46. Oma E, Bisgaard T, Jorgensen LN, Jensen KK. Nationwide propensity‐score matched study of mesh versus suture repair of primary ventral hernias in women with a subsequent pregnancy. World J Surg 2019; 43: 1497–1504. [DOI] [PubMed] [Google Scholar]
- 47. van den Spieghel A. Opera Quae Extant, Omnia. Johannes Blaeu: Amsterdam, 1645. [Google Scholar]
- 48. Klinkosch J. Divisionem hernitum novamque hernia ventralis proponit. Dissertatium Medicorum 1764; 184. [Google Scholar]
- 49. Mittal T, Kumar V, Khullar R, Sharma A, Soni V, Baijal M et al Diagnosis and management of Spigelian hernia: a review of literature and our experience. J Minim Access Surg 2008; 4: 95–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Moreno‐Egea A, Campillo‐Soto A, Morales‐Cuenca G. Which should be the gold standard laparoscopic technique for handling Spigelian hernias? Surg Endosc 2015; 29: 856–862. [DOI] [PubMed] [Google Scholar]
- 51. Barnes TG, McWhinnie DL. Laparoscopic Spigelian hernia repair: a systematic review. Surg Laparosc Endosc Percutan Tech 2016; 26: 265–270. [DOI] [PubMed] [Google Scholar]
- 52. Webber V, Low C, Skipworth RJE, Kumar S, de Beaux AC, Tulloh B. Contemporary thoughts on the management of Spigelian hernia. Hernia 2017; 21: 355–361. [DOI] [PubMed] [Google Scholar]
- 53. Moreno‐Egea A, Carrasco L, Girela E, Martin JG, Aguayo JL, Canteras M. Open vs laparoscopic repair of spigelian hernia: a prospective randomized trial. Arch Surg 2002; 137: 1266–1268. [DOI] [PubMed] [Google Scholar]
- 54. Skandalakis PN, Zoras O, Skandalakis JE, Mirilas P. Spigelian hernia: surgical anatomy, embryology and technique of repair. Am Surg 2006; 72: 42–48. [PubMed] [Google Scholar]
- 55. Muysoms FE, Miserez M, Berrevoet F, Campanelli G, Champault GG, Chelala E et al Classification of primary and incisional abdominal wall hernias. Hernia 2009; 13: 407–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Malazgirt Z, Topgul K, Sokmen S, Ersin S, Turkcapar AG, Gok H et al Spigelian hernias: a prospective analysis of baseline parameters and surgical outcome of 34 consecutive patients. Hernia 2006; 10: 326–330. [DOI] [PubMed] [Google Scholar]
- 57. Lau B, Kim H, Haigh PI, Tejirian T. Obesity increases the odds of acquiring and incarcerating noninguinal abdominal wall hernias. Am Surg 2012; 78: 1118–1121. [PubMed] [Google Scholar]
- 58. Paajanen H, Ojala S, Virkkunen A. Incidence of occult inguinal and Spigelian hernias during laparoscopy of other reasons. Surgery 2006; 140: 9–12. [DOI] [PubMed] [Google Scholar]
- 59. Light D, Chattopadhyay D, Bawa S. Radiological and clinical examination in the diagnosis of Spigelian hernias. Ann R Coll Surg Engl 2013; 95: 98–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Hope WW, Hooks WB III . Atypical hernias: suprapubic, subxiphoid and flank. Surg Clin North Am 2013; 93: 1135–1162. [DOI] [PubMed] [Google Scholar]
- 61. Suarez S, Hernandez JD. Laparoscopic repair of a lumbar hernia: report of a case and extensive review of the literature. Surg Endosc 2013; 27: 3421–3429. [DOI] [PubMed] [Google Scholar]
- 62. Moreno‐Egea A, Baena EG, Calle MC, Martinez JA, Albasini JL. Controversies in the current management of lumbar hernias. Arch Surg 2007; 142: 82–88. [DOI] [PubMed] [Google Scholar]
- 63. Salameh JR. Primary and unusual abdominal wall hernias. Surg Clin North Am 2008; 88: 45–60. [DOI] [PubMed] [Google Scholar]
- 64. Guillem P, Czarnecki E, Duval G, Bounoua F, Fontaine C. Lumbar hernia: anatomical route assessed by computed tomography. Surg Radiol Anat 2002; 24: 53–56. [DOI] [PubMed] [Google Scholar]
- 65. Macchi V, Porzionato A, Morra A, Picardi EEE, Stecco C, Loukas M et al The triangles of Grynfeltt and Petit and the lumbar tunnel: an anatomo‐radiologic study. Hernia 2017; 21: 369–376. [DOI] [PubMed] [Google Scholar]
- 66. Loukas M, Tubbs RS, Shoja M. Lumbar hernia, anatomical basis and clinical aspects. Surg Radiol Anat 2008; 30: 609–610. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 Validation of the EHS and AHS guidelines using the AGREE instrument


