Abstract
Background
Women frequently present with symptoms not typical of angina (NTA) making ischemic heart disease recognition, diagnosis and treatment challenging. We compared mortality in women with obstructive coronary artery disease (CAD) with NTA vs typical angina (TA).
Methods
We studied 326 Women’s Ischemia Syndrome Evaluation (WISE) participants undergoing coronary angiography for suspected myocardial ischemia with core-lab measured obstructive CAD. TA was defined as sub-sternal chest pain precipitated by physical exertion or emotional stress and relieved with rest or nitroglycerin; NTA did not meet criteria for TA. The women were followed for non-fatal events and death for a median of 5.9 and 9.6 years respectively. Multivariate cox proportional hazards regression determined relations to events.
Results
Overall, 115 (35%) of the women had TA. Baseline demographics, risk factors or additional symptom characteristics were similar between the two angina groups. Non-fatal events did not differ between groups. Women with NTA had a higher mortality compared to TA women (36% vs 26%, respectively, p = 0.047). Despite adjustment for additional major risk variables, NTA was an independent predictor of mortality compared to TA with a hazard ratio of 1.73 (95% Confidence interval: 1.04, 2.89).
Conclusions
Among women with suspected ischemia undergoing coronary angiography with obstructive CAD, NTA was more common than TA, and predicted a higher longer-term mortality. Further investigation is needed to confirm these results, and investigate potential explanations for the higher mortality observed in women with NTA women, including lower recognition or action in the setting of obstructive CAD.
Keywords: Angina, Coronary artery disease, Mortality
1. Background
Women with signs and symptoms of ischemia frequently have symptoms of non-typical angina (NTA) [1], [2], [3], [4]. Typical angina (TA), defined as substernal discomfort occurring with physical exertion or emotional stress, and relieved within 10 min by rest or nitroglycerin is frequently used to help predict the presence of obstructive coronary artery disease (CAD) [2], [5]. Although women have a similar incidence of stable angina compared to men [6], studies have shown that typical angina is less likely to be associated with obstructive CAD in women than in men [3], [7], [8], [9], [10]. Pepine et al. [4] characterized over 5000 outpatients with ischemic heart disease and chronic stable angina and found women were more likely to have atypical features of rest and mental stress angina. Further, women with ischemic heart disease are more likely than men to experience atypical symptoms in locations other than substernal including jaw, arms, shoulder, back, epigastrium as well as associated dyspnea, palpitations, fatigue and nausea [8], [11], [12], [13].
While prior work has suggested that angina symptoms are less diagnostic for obstructive CAD in women [3], [7], [8], [9], [10], [14], the predictive value of NTA for mortality in women with obstructive CAD is unknown. Previous studies have shown “nonspecific” chest pain is associated with nearly equal mortality compared to typical angina in men [15], and diabetic stable CAD not stratified by sex had similar mortality rates in asymptomatic, angina equivalents or typical angina [16]. Multiple studies however have found relatively less treatment in women presenting with unstable angina or myocardial infarctions [17], [18], [19], and relatively higher mortality [19], [20], [21], [22], [23]. We hypothesized that symptoms non typical for angina may contribute to women receiving less recognition, less appropriate treatment and increased mortality. We chose to analyze those with obstructive CAD due to existing guidelines for diagnosis and therapy in this group. As part of the Women’s Ischemia Syndrome Evaluation (WISE) we compared all-cause mortality in women with obstructive CAD with NTA versus TA.
2. Methods
2.1. Study population
The study population included 326 participants with obstructive CAD in the WISE (enrolled 1996–2001), a National Heart, Lung, and Blood Institute-Sponsored four center study [12]. In brief, participants were women over the age of 18 with signs and symptoms of ischemia who were undergoing clinically ordered coronary angiography for suspected myocardial ischemia. Major exclusion criteria include pregnancy, contraindications to provocative diagnostic testing, cardiomyopathy, New York Heart Association class IV congestive heart failure, recent myocardial infarction, significant valvular disease or congenital heart disease, as previously described [12]. In the original WISE cohort of 936 women, 364 (39%) had obstructive CAD. The current sample of 326 women includes all WISE women with obstructive CAD who could be classified as having either symptoms of typical (TA) or not typical of angina (NTA) and who had follow-up information. The study protocols were each approved by the site institutional review boards. Informed consent was obtained and all women were followed for at least one year to assess clinical events and symptom status.
2.2. Baseline testing
All participants underwent an initial evaluation that included demographic, medical history, physical exam, psychosocial and symptom questionnaires. Blood samples including fasting blood glucose, lipids, creatinine, hemoglobin and high sensitivity C reactive protein were collected at baseline. Psychosocial questionnaires included Beck Depression and Spielberg anxiety. The complete study design and cited methodology of the WISE study have been described [12].
2.3. Angiographic assessment of obstructive CAD
As part of the WISE entry criteria, all women underwent clinically ordered angiography conducted for suspected myocardial ischemia. Coronary angiograms were analyzed by a WISE angiographic core laboratory (Rhode Island Hospital, Providence, RI, USA), masked to clinical data, as previously described [20]. The presence of obstructive CAD was defined ≥50% stenosis ≥1 major epicardial coronary artery. An angiographic CAD severity score was calculated based on stenosis severity as previously published [20].
2.4. Definition of symptoms of not typical of angina versus typical angina assessment
Symptoms were assessed at baseline. Traditional chest pain assessment, validated in large female and male populations for obstructive CAD predictions was used to classify symptoms as TA [5]. TA was defined as meeting all 3 criteria: (1) substernal discomfort, (2) precipitated by physical exertion or emotional stress, and (3) relieved within 10 min by rest or nitroglycerin and has been used to help predict the presence of obstructive coronary artery disease (CAD) [5]. NTA was defined as all other angina symptoms not meeting criteria for TA. Additionally, a subgroup of 222 women was administered a comprehensive symptom check list developed by WISE investigators after baseline testing had already been completed, to better characterize and understand symptoms not typical for angina.
2.5. Patient follow-up
During the initial follow-up phase, taking place over a median of 5.9 years (interquartile range, 2.8, 7.0), participants were contacted at 6 weeks after baseline testing and then annually. Each woman was queried about symptoms, medication use, cardiovascular events, hospitalizations or revascularization procedures since last contact. In the event of a death, a death certificate was obtained as well as descriptions by an attending physician and/or primary relative regarding the circumstances of the death. A National Death Index (NDI) search was subsequently conducted and death certificates obtained which extended the follow-up for mortality to a median of 9.6 (interquartile range 8.5, 10.5), up to a maximum of 11.5 years. A major adverse cardiac event was defined as death, non-fatal myocardial infarction, non-fatal stroke, or heart failure hospitalization. All-cause death was used, as the ultimate outcome increasingly used in studies and clinical trials, and due to the concern that death may be less commonly adjudicated as cardiovascular in women with atypical symptoms.
2.6. Statistical methods
Baseline demographics and symptom categories were compared between NTA and TA using t-tests for continuous variables and Chi-squared tests for categorical variables. Time to death among patients with TA and NTA was analyzed and plotted using Kaplan-Meier analyses. The association between survival and NTA and TA were adjusted for age and medical history indicators of hypertension, dyslipidemia, diabetes, tobacco use, and family history of CAD using a Cox Proportional Hazards regression, and reported with a hazard ratio and 95% confidence interval. A significance level of 0.05 was used for all hypothesis tests. All analyses were done using SAS version 9.3 (SAS Institute, Cary, NC).
3. Results
In this subsample of 326 WISE participants with angiographically confirmed obstructive CAD, only 115 (35%) had TA while the remainder 211 (64%) had symptoms defined as NTA. The baseline characteristics depicted in Table 1 demonstrate similar demographic, risk factor, and psychosocial profiles in the NTA and TA groups. The only exception was that women with NTA were more likely to be using ACE inhibitors (p = 0.033), a finding that is expected to occur by chance given the number of items assessed. Medication used at baseline and follow up did not differ other than the ACE inhibitor. Detailed symptom characterization demonstrated higher rates of left sided chest pain (p = 0.022) in NTA women and higher rates of chest pressure in TA women (p = 0.043) (Table 2), but was otherwise not informative beyond the traditional angina classification.
Table 1.
Baseline characteristics for NTA vs. TA.
| NTA n = 211 |
TA n = 115 |
p-value | |
|---|---|---|---|
| Age, years | 61.8 ± 11.4 | 61.7 ± 11.7 | 0.96 |
| Obese (BMI ≥ 30) | 77 (37%) | 45 (39%) | 0.76 |
| White/Non-Hispanic | 160 (76%) | 93 (81%) | 0.30 |
| Post-Menopausal | 171 (83%) | 97 (85%) | 0.63 |
| Current Smoker | 49 (23%) | 23 (20%) | 0.50 |
| Ever Smoked | 126 (60%) | 64 (56%) | 0.48 |
| Diabetes | 85 (41%) | 39 (34%) | 0.23 |
| History of Dyslipidemia | 131 (68%) | 75 (70%) | 0.65 |
| History of Hypertension | 147 (70%) | 69 (60%) | 0.07 |
| Family History of CAD | 142 (70%) | 72 (65%) | 0.39 |
| Coronary Severity Score | 27 ± 17 | 26 ± 16 | 0.54 |
| Beck Depression | 11.8 ± 8.6 | 10.8 ± 8.7 | 0.47 |
| Spielberger Anxiety | 19.4 ± 5.6 | 19.0 ± 5.7 | 0.70 |
| DASI | 16.6 ± 12.6 | 15.1 ± 11.9 | 0.30 |
| Symptom intensity (usual)* | 2.6 ± 1.1 | 2.5 ± 1.0 | 0.24 |
| Symptom intensity (at worst)* | 4.0 ± 1.2 | 4.0 ± 1.0 | >0.99 |
| Symptoms almost ≥ every day | 81 (38%) | 54 (47%) | 0.13 |
| Perceived Quality of Life | 6.9 ± 2.4 | 7.0 ± 2.0 | 0.56 |
| History of HRT | 92 (45%) | 54 (47%) | 0.70 |
| Baseline Lab Results | |||
| Total Cholesterol (mg/dL) | 196 ± 44 | 196 ± 52 | 0.97 |
| Triglycerides (mg/dL) | 178 ± 141 | 170 ± 107 | 0.62 |
| High density lipoprotein (mg/dL) | 53 ± 13 | 52 ± 10 | 0.84 |
| Low density lipoprotein (mg/dL) | 112 ± 39 | 110 ± 45 | 0.83 |
| Glucose (fasting) (mg/dL) | 135 ± 70 | 129 ± 78 | 0.48 |
| Creatinine (mg/dL) | 0.95 ± 0.60 | 0.90 ± 0.67 | 0.54 |
| Hemoglobin (g/dL) | 12.8 ± 1.4 | 13.0 ± 1.4 | 0.40 |
| High sensitivity-C reactive protein (mg/L) | 0.98 ± 1.77 | 1.38 ± 2.49 | 0.20 |
| Medications at Baseline | |||
| ACE Inhibitors | 77 (37%) | 29 (25%) | 0.033 |
| Angiotensin Receptor Blockers | 8 (4%) | 6 (5%) | 0.56 |
| Diuretic | 71 (34%) | 39 (34%) | 0.99 |
| Calcium Channel Blockers | 70 (34%) | 35 (30%) | 0.62 |
| Aspirin | 158 (75%) | 89 (77%) | 0.66 |
| Beta Blockers | 109 (52%) | 52 (45%) | 0.23 |
| Statins | 76 (36%) | 33 (29%) | 0.16 |
| Nitrates | 108 (52%) | 63 (55%) | 0.59 |
HRT = hormone replacement therapy, ACE = angiotensin converting enzyme inhibitor, BMI = body mass index, CAD = coronary artery disease, DASI = Duke Activity Status Inventory.
Symptom intensity, range 1 (lowest) – 5 (highest).
Table 2.
Subgroup Symptom Analysis for NTA vs. TA, n = 222.
| Symptom | NTA (n = 143) | TA (n = 79) | p |
|---|---|---|---|
| Left side of chest | 52 (36%) | 17 (22%) | 0.022 |
| Neck or jaw | 32 (22%) | 22 (28%) | 0.36 |
| Left arm | 51 (36%) | 25 (32%) | 0.54 |
| Abdominal pain | 18 (13%) | 10 (15%) | 0.62 |
| Arm/shoulder pain | 91 (64%) | 50 (76%) | 0.11 |
| Back Pain | 66 (47%) | 22 (33%) | 0.056 |
| Chest Pain | 104 (74%) | 53 (80%) | 0.34 |
| Chest Pressure | 97 (69%) | 55 (82%) | 0.043 |
| Chest tightness | 88 (63%) | 48 (73%) | 0.18 |
| Chest heaviness, burning, tenderness | 96 (67%) | 51 (76%) | 0.70 |
| Cough | 33 (24%) | 18 (27%) | 0.56 |
| Dizziness, lightheadedness | 70 (50%) | 29 (43%) | 0.34 |
| Feel lousy | 71 (51%) | 41 (62%) | 0.12 |
| Heartburn/indigestion/stomach problem | 61 (43%) | 27 (40%) | 0.60 |
| Impending doom | 25 (18%) | 11 (17%) | 0.69 |
| Jaw pain | 38 (27%) | 14 (21%) | 0.46 |
| Fainting | 9 (6%) | 7 (11%) | 0.29 |
| Nausea/vomiting | 38 (27%) | 18 (27%) | 0.98 |
| Neck pain | 48 (34%) | 19 (29%) | 0.43 |
| Numbness/tingling in arm or hand | 67 (48%) | 35 (53%) | 0.49 |
| Palpitations | 61 (44%) | 32 (49%) | 0.54 |
| Shortness of breath | 97 (69%) | 47 (72%) | 0.61 |
| Sweating | 63 (45%) | 28 (42%) | 0.69 |
| Weakness, fatigue, faintness | 74 (52%) | 39 (58%) | 0.44 |
| Pain wakes patient at night | 65 (48%) | 30 (45%) | 0.68 |
Bold values denotes Higher rates of chest pressure in women with TA.
Over a median of 5.9 years, 18 women (5.5%) experienced a non-fatal myocardial infarction, 22 (6.7%) a non-fatal stroke, 35 (11%) were hospitalized for heart failure, and 126 experienced at least one hospitalization for recurrent chest pain. NTA women had similar rates of major cardiac events compared to TA women, although there was a trend toward double the rate of heart failure hospitalizations (Table 3).
Table 3.
All-cause Mortality and Major Adverse Cardiac Events in NTA vs TA.
| NTA n = 211 | TA n = 115 | p-value (Age Adjusted) | p-value (Full Model Adjusted) | |
|---|---|---|---|---|
| 9.6 Year (Median) Events | ||||
| All-cause Mortality | 77 (36%) | 30 (26%) | 0.047 | 0.035 |
| 6.0 Year (Median) Events | ||||
| Non-fatal Myocardial Infarction | 13 (6%) | 5 (5%) | 0.42 | 0.18 |
| Non-fatal Stroke | 15 (7%) | 7 (6%) | 0.68 | 0.79 |
| Heart Failure Hospitalization | 27 (13%) | 8 (7%) | 0.09 | 0.31 |
| Angina Hospitalization | 81 (39%) | 45 (41%) | 0.97 | 0.72 |
| Any Major Event* | 90 (43%) | 43 (38%) | 0.29 | 0.33 |
Major events include death (up to 8 years) and non-fatal myocardial infarction, stroke, or heart failure hospitalization.
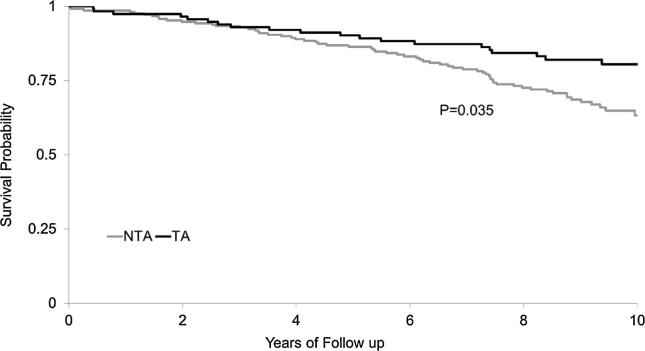
Over a median of 9.6 years, 107 (33%) women died. Those with NTA had a higher mortality rate (36% vs 26%, respectively, age-adjusted log-rank p = 0.047) (Table 3), with a hazard ratio (95% confidence interval) of 1.55 (1.005, 2.40). NTA remained a strong predictor after adjusting, in addition, for baseline tobacco use, history of diabetes, hypertension, dyslipidemia and family history of CAD (HR 1.73, 95% CI 1.04, 2.89) (Fig. 1).
Fig. 1.
Fully adjusted Kaplan-Meier plot for 10-year All-Cause Mortality in Not-Typical Angina (NTA) (n = 211) vs Typical Angina (TA) (n = 115).
4. Discussion
Our results demonstrate in women with suspected ischemia undergoing coronary angiography with obstructive CAD, that NTA is more common that TA, however further angina characterization did not appear to be informative. Notably, we observed a higher all-cause mortality in the NTA vs TA group at 10-year follow-up – these findings are relevant because all women underwent clinically indicated coronary angiography and access to diagnostic resources cannot be blamed. There were similar rates of major adverse cardiac events, with a trend toward increased heart failure hospitalization in NTA women. Adjustment for baseline differences, including a relatively higher ACE use among NTA, did not substantially alter the results and further suggest that access to therapeutic resources also did not contribute to the adverse outcome.
Women with NTA were more often on an ACE inhibitor suggesting they were more hypertensive, and although adjustment for these important risk variables did not alter the mortality results, there may be pathophysiological links between hypertension and symptom quality. Increased myocardial oxygen demand and diminished coronary blood flow and/or coronary flow reserve is related to hypertension [24], leading to left ventricular impedance and intramyocardial wall tension, increasing myocardial demand leading to angina [24]. Another possible link is the damage to the endothelial function caused by persistent hypertension which may cause a different constellation of symptoms and or increase risk of CV events [24]. In a study comparing presentation, treatment and outcomes of MI in men versus women, women were more often hypertensive [22]. Perhaps those with NTA and hypertension will help identify those at a higher risk for CV outcomes; further work is needed to help understand this elevated risk.
Our results are consistent with prior work demonstrating that women more often present with atypical symptoms [1], [4], [5], [8], and our hypothesis that symptoms non typical for angina may contribute to women receiving less recognition, less appropriate treatment and increased mortality. Our results demonstrating elevated mortality in women with NTA compared to TA suggests the possible explanation that atypical symptoms may contribute to the observed lower use of lifesaving treatments and have worse outcomes in women with CAD [18], [19], [21], [22], [25]. We focused on all-cause mortality due to concerns for underdiagnosis of CVD related deaths in women who present with atypical symptoms. Prior WISE work has demonstrated a majority of the deaths in this population are adjudicated to be cardiovascular deaths [26], [27]. Women with NTA had at least similar rates of major adverse cardiac events compared to TA. Therefore, women with NTA and suspected or proven obstructed CAD need careful attention and perhaps greater monitoring due to their atypical symptoms. Of note, sex-specific presentation, pathophysiological mechanisms and outcomes remain evident, and cardiovascular disease remains the leading cause of death among women [23].
NTA was more common that TA in patients undergoing clinically indicated coronary angiogram for suspected CAD, even in those who were found to have obstructive CAD [28]. Historically, predicting the likelihood of obstructive CAD has been challenging in women. Once diagnosed with obstructive CAD and stable angina the use of guideline-driven medical therapy is not optimal in women and men [25]. A proposed algorithm from these results of potential relevance to clinical care to close the adverse outcomes preferentially experienced by women would be to consider the presence of symptoms suggestive of ischemia and not the strict definition of TA used in the past when treating women with known obstructive CAD. Further investigation is needed to improve diagnostic and therapeutic strategies in women who present with NTA.
4.1. Limitations
Our study limitations include use of a relatively small, but carefully phenotyped population of women. Further, our use of clinically referred cohort which may not be representative of all women with suspected ischemia and obstructive CAD. Follow-up events were gathered per patient report with confirmation by medical records and cause of death, which could result in reporting bias. Our lack of information about CAD extent and revascularization treatment is a limitation and may have influenced prognosis. Our use of all-cause mortality could be misleading, however this is considered a strength as the ultimate outcome in studies and trials, and prior WISE work has demonstrated a majority of the deaths in this population are adjudicated to be cardiovascular deaths [26], [27]. Another important limitation includes having a low statistical power for the non-fatal events which we only followed for 6 years.
5. Conclusions
Among women with suspected ischemia undergoing coronary angiography with obstructive CAD, NTA was more common than TA, and predicted a higher longer-term mortality. Further investigation is needed to confirm these results and investigate potential explanations for the higher mortality observed in women with NTA women, including lower recognition or action in the setting of obstructive CAD.
Funding
This work was supported by contracts from the National Heart, Lung and Blood Institutes nos. N01-HV-68161, N01-HV-68162, N01-HV-68163, N01-HV-68164, grants U0164829, U01 HL649141, U01 HL649241, K23HL105787, T32HL69751, R01 HL090957, 1R03AG032631 from the National Institute on Aging, GCRC grant MO1-RR00425 from the National Center for Research Resources, the National Center for Advancing Translational Sciences Grant UL1TR000124 and UL1TR000064, and grants from the Gustavus and Louis Pfeiffer Research Foundation, Danville, NJ, The Women’s Guild of Cedars-Sinai Medical Center, Los Angeles, CA, The Ladies Hospital Aid Society of Western Pennsylvania, Pittsburgh, PA, and QMED, Inc., Laurence Harbor, NJ, the Edythe L. Broad and the Constance Austin Women’s Heart Research Fellowships, Cedars-Sinai Medical Center, Los Angeles, California, the Barbra Streisand Women’s Cardiovascular Research and Education Program, Cedars-Sinai Medical Center, Los Angeles, The Society for Women’s Health Research (SWHR), Washington, D.C., The Linda Joy Pollin Women’s Heart Health Program, the Erika Glazer Women’s Heart Research Initiative, and the Adelson Family Foundation, Cedars-Sinai Medical Center, Los Angeles, California. Dr. Pepine was also supported by National Institute of Health grants HL33610, HL56921; UM1 HL087366; the Gatorade Trust through funds distributed by the University of Florida, Department of Medicine; NIH NCATS—University of Florida Clinical and Translational Science UL1TR001427; and PCORnet-OneFlorida Clinical Research Consortium CDRN-1501-26692.This work is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or National Institutes of Health.
References
- 1.Johnson B.D., Shaw L.J., Pepine C.J., Reis S.E., Kelsey S.F., Sopko G., Rogers W.J., Mankad S., Sharaf B.L., Bittner V. Persistent chest pain predicts cardiovascular events in women without obstructive coronary artery disease: results from the NIH-NHLBI-sponsored Women's Ischaemia Syndrome Evaluation (WISE) study. Eur. Heart J. 2006;27:1408–1415. doi: 10.1093/eurheartj/ehl040. [DOI] [PubMed] [Google Scholar]
- 2.Diamond G.A., Staniloff H.M., Forrester J.S., Pollock B.H., Swan H. Computer-assisted diagnosis in the noninvasive evaluation of patients with suspected coronary artery disease. J. Am. Coll. Cardiol. 1983;1:444–455. doi: 10.1016/s0735-1097(83)80072-2. [DOI] [PubMed] [Google Scholar]
- 3.Cheng V.Y., Berman D.S., Rozanski A., Dunning A.M., Achenbach S., Al-Mallah M., Budoff M.J., Cademartiri F., Callister T.Q., Chang H.-J. Performance of the traditional age, sex, and angina typicality-based approach for estimating pretest probability of angiographically significant coronary artery disease in patients undergoing coronary computed tomographic angiography results from the multinational coronary CT angiography evaluation for clinical outcomes: an international multicenter registry (CONFIRM) Circulation. 2011;124:2423–2432. doi: 10.1161/CIRCULATIONAHA.111.039255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pepine C.J., Abrams J., Marks R.G., Morris J.J., Scheidt S.S. Handberg E and investigators T. Characteristics of a contemporary population with angina pectoris. Am. J. Cardiol. 1994;74:226–231. doi: 10.1016/0002-9149(94)90361-1. [DOI] [PubMed] [Google Scholar]
- 5.Diamond G.A. A clinically relevant classification of chest discomfort. J. Am. Coll. Cardiol. 1983;1:574–575. doi: 10.1016/s0735-1097(83)80093-x. [DOI] [PubMed] [Google Scholar]
- 6.Hemingway H., McCallum A., Shipley M., Manderbacka K., Martikainen P., Keskimäki I. Incidence and prognostic implications of stable angina pectoris among women and men. JAMA. 2006;295:1404–1411. doi: 10.1001/jama.295.12.1404. [DOI] [PubMed] [Google Scholar]
- 7.Sullivan A.K., Holdright D.R., Wright C.A., Sparrow J.L., Cunningham D., Fox K.M. Chest pain in women: clinical, investigative, and prognostic features. BMJ. 1994;308:883–886. doi: 10.1136/bmj.308.6933.883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnson B.D., Kelsey S.E., Merz C.N.B. Springer; 2004. Clinical risk assessment in women Coronary Disease in Women; pp. 129–141. [Google Scholar]
- 9.Shaw L.J., Merz C.N.B., Pepine C.J., Reis S.E., Bittner V., Kelsey S.F., Olson M., Johnson B.D., Mankad S., Sharaf B.L. Insights from the NHLBI-Sponsored Women’s Ischemia Syndrome Evaluation (WISE) Study: Part I: gender differences in traditional and novel risk factors, symptom evaluation, and gender-optimized diagnostic strategies. J. Am. Coll. Cardiol. 2006;47:S4–S20. doi: 10.1016/j.jacc.2005.01.072. [DOI] [PubMed] [Google Scholar]
- 10.Chaitman B.R., Bourassa M.G., Davis K., Rogers W.J., Tyras D.H., Berger R., Kennedy J., Fisher L., Judkins M., Mock M. Angiographic prevalence of high-risk coronary artery disease in patient subsets (CASS) Circulation. 1981;64:360–367. doi: 10.1161/01.cir.64.2.360. [DOI] [PubMed] [Google Scholar]
- 11.Goldberg R.J., O’Donnell C., Yarzebski J., Bigelow C., Savageau J., Gore J.M. Sex differences in symptom presentation associated with acute myocardial infarction: a population-based perspective. Am. Heart J. 1998;136:189–195. doi: 10.1053/hj.1998.v136.88874. [DOI] [PubMed] [Google Scholar]
- 12.Merz C.N.B., Kelsey S.F., Pepine C.J., Reichek N., Reis S.E., Rogers W.J., Sharaf B.L., Sopko G. The Women’s Ischemia Syndrome Evaluation (WISE) study: protocol design, methodology and feasibility report. J. Am. Coll. Cardiol. 1999;33:1453–1461. doi: 10.1016/s0735-1097(99)00082-0. [DOI] [PubMed] [Google Scholar]
- 13.Devon H.A., Rosenfeld A., Steffen A.D., Daya M. Sensitivity, specificity, and sex differences in symptoms reported on the 13-item acute coronary syndrome checklist. J Am Heart Assoc. 2014;3:e000586. doi: 10.1161/JAHA.113.000586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Villines T.C., Hulten E.A., Shaw L.J., Goyal M., Dunning A., Achenbach S., Al-Mallah M., Berman D.S., Budoff M.J., Cademartiri F. Prevalence and severity of coronary artery disease and adverse events among symptomatic patients with coronary artery calcification scores of zero undergoing coronary computed tomography angiography: results from the CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: an International Multicenter) registry. J. Am. Coll. Cardiol. 2011;58:2533–2540. doi: 10.1016/j.jacc.2011.10.851. [DOI] [PubMed] [Google Scholar]
- 15.Wilhelmsen L., Rosengren A., Hagman M., Lappas G. “Nonspecific” chest pain associated with high long-term mortality: results from the primary prevention study in Goteborg Sweden. Clin. Cardiol. 1998;21:477–482. doi: 10.1002/clc.4960210706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dagenais G.R., Lu J., Faxon D.P., Bogaty P., Adler D., Fuentes F., Escobedo J., Krishnaswami A., Slater J., Frye R.L., Group B.D.S. Prognostic impact of the presence and absence of angina on mortality and cardiovascular outcomes in patients with type 2 diabetes and stable coronary artery disease: results from the BARI 2D (Bypass Angioplasty Revascularization Investigation 2 Diabetes) trial. J. Am. Coll. Cardiol. 2013;61:702–711. doi: 10.1016/j.jacc.2012.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roger V.L., Farkouh M.E., Weston S.A., Reeder G.S., Jacobsen S.J., Zinsmeister A.R., Yawn B.P., Kopecky S.L., Gabriel S.E. Sex differences in evaluation and outcome of unstable angina. JAMA. 2000;283:646–652. doi: 10.1001/jama.283.5.646. [DOI] [PubMed] [Google Scholar]
- 18.Chandra N.C., Ziegelstein R.C., Rogers W.J., Tiefenbrunn A.J., Gore J.M., French W.J., Rubison M. Observations of the treatment of women in the United States with myocardial infarction: a report from the National Registry of Myocardial Infarction-I. Arch. Intern. Med. 1998;158:981–988. doi: 10.1001/archinte.158.9.981. [DOI] [PubMed] [Google Scholar]
- 19.Kudenchuk P.J., Maynard C., Martin J.S., Wirkus M., Weaver W.D., Investigators M.P. Comparison of presentation, treatment, and outcome of acute myocardial infarction in men versus women (the Myocardial Infarction Triage and Intervention Registry) Am. J. Cardiol. 1996;78:9–14. doi: 10.1016/s0002-9149(96)00218-4. [DOI] [PubMed] [Google Scholar]
- 20.Sharaf B.L., Pepine C.J., Kerensky R.A., Reis S.E., Reichek N., Rogers W.J., Sopko G., Kelsey S.F., Holubkov R., Olson M. Detailed angiographic analysis of women with suspected ischemic chest pain (pilot phase data from the NHLBI-sponsored Women’s Ischemia Syndrome Evaluation [WISE] Study Angiographic Core Laboratory) Am. J. Cardiol. 2001;87:937–941. doi: 10.1016/s0002-9149(01)01424-2. [DOI] [PubMed] [Google Scholar]
- 21.Robinson J.G., Wallace R., Limacher M., Sato A., Cochrane B., Wassertheil-Smoller S., Ockene J.K., Blanchette P.L., Ko M.G. Elderly women diagnosed with nonspecific chest pain may be at increased cardiovascular risk. J. Women's Health. 2006;15:1151–1160. doi: 10.1089/jwh.2006.15.1151. [DOI] [PubMed] [Google Scholar]
- 22.Vaccarino V., Parsons L., Every N.R., Barron H.V., Krumholz H.M. Sex-based differences in early mortality after myocardial infarction. N. Engl. J. Med. 1999;341:217–225. doi: 10.1056/NEJM199907223410401. [DOI] [PubMed] [Google Scholar]
- 23.Mehta L.S., Beckie T.M., DeVon H.A., Grines C.L., Krumholz H.M., Johnson M.N., Lindley K.J., Vaccarino V., Wang T.Y., Watson K.E., Wenger N.K., American Heart Association Cardiovascular Disease in W. Special Populations Committee of the Council on Clinical Cardiology CoE. Prevention CoC. Stroke N. Council on Quality of C. Outcomes R Acute myocardial infarction in women: a scientific statement from the American Heart Association. Circulation. 2016;133:916–947. doi: 10.1161/CIR.0000000000000351. [DOI] [PubMed] [Google Scholar]
- 24.Rosendorff C., Black H.R., Cannon C.P., Gersh B.J., Gore J., Izzo J.L., Kaplan N.M., O’Connor C.M., O’Gara P.T., Oparil S. REPRINT Treatment of hypertension in the prevention and management of ischemic heart disease a scientific statement from the American Heart Association Council for high blood pressure research and the councils on clinical cardiology and epidemiology and prevention. Hypertension. 2007;50:e28–e55. doi: 10.1161/CIRCULATIONAHA.107.183885. [DOI] [PubMed] [Google Scholar]
- 25.Dreyer R., Arstall M., Tavella R., Morgan C., Weekes A., Beltrame J. Gender differences in patients with stable angina attending primary care practices. Heart Lung Circ. 2011;20:452–459. doi: 10.1016/j.hlc.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 26.Mehta P.K., Johnson B.D., Kenkre T.S., Eteiba W., Sharaf B., Pepine C.J., Reis S.E., Rogers W.J., Kelsey S.F., Thompson D.V., Bittner V., Sopko G., Shaw L.J., Bairey Merz C.N. Sudden cardiac death in women with suspected ischemic heart disease, preserved ejection fraction, and no obstructive coronary artery disease: a report from the Women's Ischemia Syndrome Evaluation study. J. Am. Heart Assoc. 2017;6:PMC5586417. doi: 10.1161/JAHA.117.005501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kenkre T.S., Malhotra P., Johnson B.D., Handberg E.M., Thompson D.V., Marroquin O.C., Rogers W.J., Pepine C.J., Bairey Merz C.N., Kelsey S.F. Ten-year mortality in the WISE Study (Women's Ischemia Syndrome Evaluation) Circ. Cardiovasc. Qual. Outcomes. 2017;10 doi: 10.1161/CIRCOUTCOMES.116.003863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bucciarelli-Ducci C., Pennell D.J. Low diagnostic yield of elective coronary angiography. N. Engl. J. Med. 2010;363(94) author reply 94-5. [PubMed] [Google Scholar]