Abstract
Numerous studies have assessed individual-level factors associated with intention to quit smoking. However, fewer studies have assessed how neighborhood and built environment also contribute towards individual-level behavior. We used baseline data of 340 Chinese and Vietnamese male daily smokers from August 2015 to November 2017 living in the San Francisco Bay Area, who enrolled in a lifestyle intervention trial. The outcome variable was intention to quit in 30 days. To understand the role of contextual factors participants’ residential addresses were geocoded, and neighborhood median income, ethnic composition, and tobacco retail density were computed. Individual level analysis suggested that Vietnamese American men had greater intention to quit smoking (OR = 2.90 CI = 1.59, 5.26) in comparison to Chinese Americans. However, after adding neighborhood level factors to the model, no ethnic group difference was observed. Neighborhood household median income (OR = 0.74, CI = 0.64, 0.86) and tobacco retail counts (OR = 0.79, CI = 0.67, 0.94) were negatively associated with intention to quit. Years lived in the U.S. was the only individual level factor associated with intention to quit. By comparing two Asian American groups that live in heterogeneous neighborhoods, we identify key environmental and policy drivers that are associated with quit intention. Future studies aimed at influencing individual-level behavior should take into consideration the neighborhood context and built environment characteristics.
Keywords: Tobacco use, Asian Americans, Tobacco retailers, Neighborhood characteristics, Geographic variation
1. Introduction
In the United States, smoking prevalence remains high among subpopulations of ethnic groups (Martell, 2016). Based on the National Survey on Drug Use and Health, 9% of Asian Americans (age 18 + ) are smokers in comparison to 16.6% of Whites. However, this comparison does not account for within group differences and only includes predominantly English speakers. For example, smoking prevalence is estimated between 21% and 41% for Asian American men, including Chinese and Vietnamese American men, who have limited English proficiency (California Health Interview Survey, 2019, Chan et al., 2007, Hu et al., 2010, King and Deng, 2018, Li et al., 2013, Tong et al., 2010).
Individual-level factors contributing towards disparities in tobacco use have been widely studied. Research suggests language, education, immigration status, age, socioeconomic status, and ethnic ancestry play a role in Asian Americans’ smoking (Ja and Aoki, 1993, Zhang and Wang, 2008). As tobacco use remains socially acceptable especially among men in Asian countries such as China and Vietnam where only a small percentage of smokers (2% and 8%, respectively) report intention to quit (Owusu et al., 2017), male immigrants from these countries tend to have a higher tobacco use and smoking prevalence. On the contrary, in the United States, with advanced tobacco control efforts, a majority of smokers are considering quitting smoking (Babb et al., 2017). Pooled data from the 2013–2017 California Health Interview Survey showed more than 70% of smokers in California were thinking about quitting smoking in the next 6 months, while less than 50% of Asian smokers with limited English proficiency had a similar quit intentions (California Health Interview Survey, 2019). Yet, there remain within group differences in quit intention by different subpopulations.
A study of 1374 Asian American smokers found differences in the intention to quit across Asian ethnic groups. Chinese smokers showed the least desire to quit while Vietnamese smokers showed the most desire to quit in one month (33% vs 45%) (Ma et al., 2003). Other correlates that have been found to be associated with intention to quit include age, socio-economic status, number of cigarettes smoked per day, number of years of smoking, parental smoking, family conflicts (e.g., Tsoh et al., 2011, Twigg et al., 2009). Intention to quit smoking has predicted quit attempts and smoking abstinence across studies (Vangeli et al., 2011), thus, a better understanding of the individual correlates to increase motivations of smokers and support them to quit smoking is an important focus of many cessation control programs.
While individual-level factors are important, an increasing number of studies have highlighted the role of the built environment towards contributing to health disparities (Glanz and Kegler, 2008, Northridge et al., 2003). In the context of smoking behavior, tobacco retail density and proximity to tobacco retailers are viewed as measures of built environment. Tobacco retailer density is negatively associated with neighborhood income and positively associated with ethnic minority groups (Lee et al., 2017, Loomis et al., 2013, Reid et al., 2013, Rodriguez et al., 2013, Siahpush et al., 2010, Yu et al., 2010). High density of tobacco retailers is negatively associated with quitting smoking (Cantrell et al., 2015, Kirchner et al., 2013, Paul et al., 2010). Tobacco prices also tend to be lower in low-income neighborhoods, (Dalglish et al., 2013, Henriksen et al., 2017), which could reinforce smoking behavior in certain communities. In a longitudinal study of adult smokers in Houston, residential proximity to tobacco retailers reduced the odds of abstinence (Reitzel et al., 2011). Another study examined geospatial exposure to point of sale tobacco and real-time craving using ecological momentary assessment found frequent point of contact was associated with lapsed outcome (Kirchner et al., 2017).
Neighborhood socio-economic characteristics and income inequality have also been found relevant to smoking cessation. In a smoking cessation trial with among African Americans, neighborhood unemployment was a significant predictor of smoking abstinence even after accounting for individual employment and income status (Kendzor et al., 2012). As neighborhood ethnic segregation tends to be related to income and income inequality, it would be of importance to understand whether living in a homogenous neighborhood of one’s own ethnicity promote or reinforce certain behaviors, including smoking. Yet, in a systematic review on segregation and health found only two studies that assessed the relation with smoking. Both studies found positive association between residential segregation and smoking (White and Borrell, 2011). A study based on 212 metropolitan statistical areas investigating the association between residential segregation and smoking among African-American women during pregnancy found that both a low level of segregation and, seemingly paradoxically, a high level of segregation were associated with greater odds of smoking. However, no association was found with moderate level of segregation (Bell et al., 2007). Given the limited understanding on how contextual factors drive differences in motivation to quit smoking among different ethnic groups, especially in intervention research, the purpose of this study was to assess how individual and neighborhood factors were associated with smokers’ intention to quit among two Asian American groups.
2. Methods
2.1. Study sample
We used baseline data from 340 Chinese and Vietnamese male daily smokers who were enrolled in a lifestyle intervention research trial, which was designed to promote smoking cessation, healthy eating, and physical activities. Eligible criteria included: 1) age 18 and older, 2) self-identification as ethnic Chinese or Vietnamese, 3) ability to speak and read Chinese or Vietnamese, and 4) daily cigarette smoking (having smoked at least one cigarette daily in the previous 7 days). In addition, smokers were required to participate with one non-smoking adult family member who live in the same household with no use of tobacco in the past 12 months. Participants had to agree to attend 2 in-person small group sessions led by a lay health worker (LHW). Participants received $25 for completing the baseline survey that provided the data for the present study.
Four community-based organizations (CBOs), based in San Francisco and Santa Clara Counties in Northern California, partnered with the research team to recruit participants. The CBOs recruited 61 Chinese or Vietnamese women and men to serve as Lay Health Worker (LHWs) to recruit smokers and their family members to the study. LHWs must report no use of tobacco including e-cigarette in the past 12 months, and had no certification or licensure in the U.S. as a health professional. The CBOs worked with LHWs, through their social networks and/or advertisements to recruit smoker-family dyads. The study was described as a research project to examine different approaches to promote healthy eating, physical activity, and smoking cessation. At the time of recruitment, participants were informed that quitting smoking was not an expectation nor a requirement for participation. LHWs were not randomized until they had completed recruitment of or were assigned at least 2, but up to 7 eligible smoker-family dyads. After UCSF research staff confirmed smoker and family member participants’ eligibility by telephone, participants then completed a baseline survey. LHWs and their participants were randomized into either the Smoking Cessation (SC) or Healthy Living (HL) groups. After randomization, LHWs received two additional training sessions on the assigned health topic. The present study is based on the data collected at baseline, prior to randomization.
Given that the participants were recruited predominantly from two major counties in the Greater San Francisco Bay Area – San Francisco and Santa Clara – this study provides a unique opportunity to assess how the environmental and neighborhood context of a city could be associated with the within-group differences in bolstering the motivation to quit smoking.
3. Measures
3.1. Dependent variable
Our response variable was assessed by asking participants “Are you planning to quit in the next 30 days?” Similar measures to assess intention to quit smoking have been applied to Asian American smokers (Tong et al., 2018, Tsoh et al., 2015, Tsoh et al., 2011) as well as general population of the United States (Prochaska et al., 2001, Vangeli et al., 2011) and globally (Owusu et al., 2017). Participants’ intention to quit smoking within 30 days was coded dichotomously (yes vs no/don’t know).
3.2. Covariates
We examined covariates at the individual and neighborhood levels. Individual-level covariates included participants’ sociodemographics: ethnicity (Chinese vs Vietnamese), marital status (married vs others), age, education (<high school, high school, some college or beyond), self-reported household annual income (less than $20,000, $20,000 or more, or unknown), self-rated health (“excellent”/”very good”/”good” vs “fair”/“poor”) and years lived in the U.S. Years lived in the US was rescaled by 10 for meaningful interpretation. Participants’ smoking characteristics included nicotine dependence, which was assessed by time to first cigarette smoked after awakening (within 30 minutes vs >30 minutes), and intensity of daily cigarette smoking, which was dichotomized (<10 cigarettes vs 10 or more).
Neighborhood measures were obtained by geocoding participants’ residential addresses in Maptitude, a software by Caliper Corporation™. To define neighborhoods, we used buffers of 1000 feet around each participant’s home location and estimated socio-demographic characteristics and tobacco retailers within this buffer zone. Our choice of defining neighborhood based on 1000 feet was based on a combination of factors. Proximity and density-based policies for regulating tobacco retailers are usually are based on 500 or 1000 feet (San Francisco Tobacco Free Project, 2018) and hence studies examining the impact of retail density on ethnic disparities usually use one of these measures (Myers et al., 2015, Ribisl et al., 2016, Vyas et al., 2020). Other studies on proximity and density of tobacco retailers have used distances from 800 m up to ½ mile radius or even 2 km in some cases (Henriksen et al., 2008, Ribisl et al., 2016, Schleicher et al., 2016). In the context of smoking, alcohol, and health outcomes such as obesity, neighborhoods are usually based on what is perceived as a reasonable walking distance (Hobbs et al., 2019, Lovasi et al., 2008). Our approach to defining neighborhoods by using buffers around participants’ home locations differs from studies that define neighborhood based on administrative boundaries such as county, census tracts, or zip code. Assigning a participant, a census tract or zip code based on where they live becomes an issue especially when participants live at the edge of a census tract (Higgs, 2004). Another limitation of defining neighborhood based on administrative boundaries is it cannot account for cross-boundary interactions (Higgs, 2004).
To estimate socio-demographic characteristics within the neighborhoods, an overlay procedure was used within these buffers. This procedure uses areal weighting to disaggregate the data from a higher administrative unit or political boundaries and can be used to estimate demographics from multiple census tracts or administrative boundaries that fall within the same buffer (Gabriel et al., 2000, Gregorio and Samociuk, 2003, Lovasi et al., 2008). For example, if three census tracts fall within a 1000 feet buffer, then the variable is weighted based on the proportion of the census tract that falls within the buffer.
Based on this procedure, we obtained estimates of neighborhood median household income, percent of Chinese residents, percent of Vietnamese residents, and counts of tobacco retailers. We included percent of people belonging to their own ethnicity who lived in the neighborhood as a measure of ethnic concentration. Neighborhood median household income was rescaled by $10,000 and tobacco retailer counts were rescaled by 5 for the ease of interpretation.
3.3. Statistical analysis
We used generalized estimating equations to examine individual and neighborhood effects while accounting for clustering between participants from the same lay health worker group. We conducted two logistic regression models. Model 1 examined the association between intention to quit and individual factors including ethnicity, marital status, income, years lived in the U.S., intensity of cigarette smoking, and nicotine dependence. Model 2 added neighborhood measures to Model 1 to examine influences from the neighborhood factors on intention to quit. We added neighborhood median household income, tobacco retailer density, and ethnic composition of participants in the neighborhood in Model 2. A significance level of 0.05 was used for all statistical tests.
4. Results
Table 1 depicts individual and neighborhood characteristics by intention to quit smoking. Among the 340 Chinese and Vietnamese male daily smoker participants aged between 21 and 83 with nearly half smoked at least 10 cigarettes per day, only 25% indicated intention to quit within 30 days. Chinese participants had lower intention to quit smoking than Vietnamese participants in the study sample, Χ2 (2, N = 340) = 24.31, p < 0.01. Participants who intended to quit smoking had lived longer in the U.S. (p < 0.01). At the neighborhood level, a wide variation was observed in ethnic composition of the participant’s neighborhood, the percentage of Chinese in the neighborhood varied from less than one percent to 83% and the Vietnamese population in the neighborhood ranged from less than 1 percent to nearly 50%. Participants who did not intend to quit lived in higher income neighborhood (t(3 3 8) = 2.11, p = 0.02). Participants who did not intend to quit lived in neighborhoods with a higher percentage of Chinese in the neighborhoods, t(3 3 8) = 3.82, p < 0.01, and in neighborhoods with a lower percentage of Vietnamese, t(3 3 8) = -3.63, p < 0.01. Tobacco retailer density was not significantly associated with intention to quit in the bivariate model.
Table 1.
Individual and neighborhood characteristics of the participants by intention to quit smoking. Participants were sampled from the San Francisco Bay Area from August 2015 to November 2017 (N = 340).
| Entire Sample (n = 340) |
Intended to quit within 30 days (n = 86) |
No Intention to quit within 30 days (n = 254) |
P values* | |
|---|---|---|---|---|
| Individual-level Characteristics | ||||
| Ethnicity | <0.01 | |||
| Chinese | 50.88% (n = 173) | 27.91% (n = 24) | 58.66% (n = 149) | |
| Vietnamese | 49.12% (n = 167) | 72.09% (n = 62) | 41.34% (n = 105) | |
| Age Mean (SD) | 54.61 (12.65) | 56.63 (12.33) | 53.92 (12.71) | 0.08 |
| Education | 0.37 | |||
| Less than high school | 44.35% (n = 149) | 47.06% (n = 40) | 43.43% (n = 109) | |
| High school | 30.65% (n = 103) | 24.71% (n = 21) | 32.67% (n = 82) | |
| Some college and beyond | 25.00% (n = 84) | 28.24% (n = 24) | 23.90% (n = 60) | |
| Missing | n = 4 | n = 1 | n = 3 | |
| Marital status | 0.05 | |||
| Married/ living with a partner | 88.24% (n = 300) | 82.56% (n = 71) | 90.16% (n = 229) | |
| Other | 11.76% (n = 40) | 17.44% (n = 15) | 9.84% (n = 25) | |
| Annual household income | 0.82 | |||
| Less than $20,000 | 40.29% (n = 137) | 38.37% (n = 33) | 40.94% (n = 104) | |
| $20,000 or more | 40.88% (n = 139) | 40.70% (n = 35) | 40.94% (n = 104) | |
| Income not reported (Unknown) | 18.82% (n = 64) | 20.93% (n = 18) | 18.11% (n = 46) | |
| Years lived in the U.S. Mean (SD) | 13.96 (11.18) | 17.83 (12.38) | 12.61 (12.61) | <0.01 |
| Missing | n = 6 | n = 0 | n = 6 | |
| Self-rated health | 0.41 | |||
| Excellent/very good/good | 47.34 (n = 160) | 51.16 (n = 44) | 46.03 (n = 116) | |
| Fair/poor | 52.66 (n = 178) | 48.84 (n = 42) | 53.97 (n = 136) | |
| Missing | n = 2 | n = 0 | n = 2 | |
| Cigarettes smoked per day | 0.35 | |||
| Less than 10 | 53.82% (n = 183) | 58.14% (n = 50) | 52.36% (n = 133) | |
| 10 or more | 46.18% (n = 157) | 41.86% (n = 36) | 47.64% (n = 121) | |
| Time to first cigarette after awakening | 0.30 | |||
| Within 30 min | 48.53% (n = 165) | 54.65% (n = 47) | 46.46% (n = 118) | |
| After 30 min | 51.47% (n = 175) | 45.35% (n = 39) | 53.54% (n = 136) | |
| Missing | n = 9 | n = 0 | n = 9 | |
| Neighborhood-level Characteristics | ||||
| Percent of Chinese in the neighbourhood Mean (SD) |
23.65 (22.55) | 15.77 (18.48) | 26.31 (23.2) | <0.01 |
| Percent of Vietnamese in the neighbourhood Mean (SD) |
10.03 (12.26) | 14.10 (13.58) | 8.65 (11.48) | <0.01 |
| Neighborhood Median Income ($) Mean (SD) |
66,975 (28,256) | 61,442 (21,925) | 68,849 (29,906) | 0.03 |
| Number of Tobacco Retailers in the Neighborhood Mean (SD) |
6.62 (10.16) | 5.52 (9.7) | 7.00 (10.30) | 0.24 |
*P-values are comparisons by quit intention groups using t-test or chi-square tests for continuous and categorical variables, respectively.
Note: Percentages were computed based on non-missing values with exception of income. The number of participants with missing values are noted for these variables: education, years lived in the U.S., self-rated health, and time to first cigarette. Other variables did not have missing data.
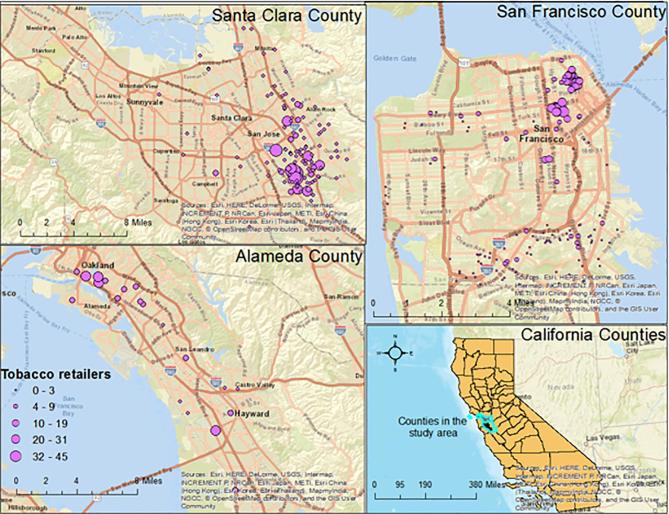
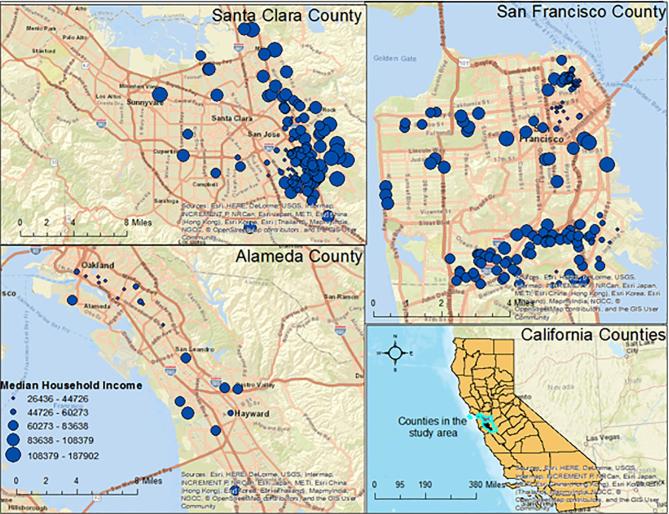
Fig. 1, Fig. 2 depict the spatial variability in tobacco retailers in the neighborhoods and the median household incomes of the participants. As shown in these figures, even though San Francisco is geographically a much smaller county in comparison to Alameda and Santa Clara, some of the participants lived in neighborhoods with fewer tobacco retailers. In contrast, even though Santa Clara and Alameda county are geographically much larger, there remain geographic pockets with a larger number of tobacco retailers in comparison to the rest of the neighborhoods where the participants lived. A similar heterogeneity could also be observed with median household income. While several participants lived in neighborhoods with high median household of over $90,000, across the three counties, some of the participants lived in neighborhood with median household income of less than $45,000.
Fig. 1.
Spatial variation in the distribution of tobacco retailers within 1000 feet buffer around a participant’s home location in the study area.
Fig. 2.
Spatial variation in the distribution of median household income within a 1000 feet buffer around a participant’s home location in the study area.
Regression results (Table 2) based on the individual-level model revealed that Vietnamese Americans had a higher intention to quit smoking within the next 30 days compared to Chinese Americans (OR 2.90, 95% CI 1.59–5.26). For every 10 additional years lived in the U.S., a participant was more ready to quit in the next 30 days (1.42, 95% CI 1.11–1.83). This association remained significant even after accounting for neighborhood factors. Interestingly, after accounting for neighborhood factors, there was no association between Vietnamese American ethnicity and intention to quit. Neighborhood median household income and tobacco retailer counts were negatively associated with the intention to quit. For every $10,000 increase in median neighborhood income, participants were less ready to quit smoking (OR 0.74, 95% CI 0.64, 0.86). And for every 5 additional tobacco retailers in the neighborhood, participants were less ready to quit (OR 0.79, 95% CI 0.67–0.94).
Table 2.
Individual and neighborhood correlates of intention to quit: Results from multivariable logistic regression models.
| Variable | Model 1 OR (CI) |
p-value | Model 2 OR (CI) |
p-value |
|---|---|---|---|---|
| Individual-level characteristics | ||||
| Ethnicity (Referent: Chinese) | ||||
| Vietnamese | 2.90 (1.59–5.26) | <0.01 | 2.04 (0.83–5.01) | 0.11 |
| Age | 1.01 (0.98–1.03) | 0.43 | 1.00 (0.98–1.03) | 0.65 |
| Education (Referent: < high school) | ||||
| High school | 0.94 (0.48–1.82) | 0.85 | 1.06 (0.53–2.13) | 0.86 |
| Some college or beyond | 0.88 (0.44–1.74) | 0.72 | 0.97 (0.46–2.03) | 0.94 |
| Marital Status (Referent: Single) | ||||
| Married/living with a partner | 0.50 (0.22–1.12) | 0.09 | 0.42 (0.17–1.02) | 0.05 |
| Annual Income (Referent: <20 K) | ||||
| 20 K or more | 0.99 (0.52–1.89) | 0.98 | 0.96 (0.49–1.88) | 0.91 |
| Unknown | 0.75 (0.35–1.61) | 0.46 | 0.68 (0.30–1.52) | 0.34 |
| Years lived in the US | 1.42 (1.11–1.83) | <0.01 | 1.44 (1.10–1.87) | <0.01 |
| Self-rated Health (Referent: Poor) | ||||
| Excellent/very good/ good | 1.21(0.71–2.08) | 0.47 | 1.12 (0.64–1.97) | 0.67 |
| Cigarettes smoked per day (Referent: 10 or more) | ||||
| <10 cigarettes per day | 1.20 (0.66–2.18) | 0.55 | 1.15 (0.61–2.15) | 0.65 |
| Time to first cigarette (Referent: within 30 min) | ||||
| More than 30 min after awakening | 0.79 (0.44–1.43) | 0.45 | 0.69 (0.37–1.28) | 0.24 |
| Neighborhood Factors | Not Included | |||
| Median household income | – | – | 0.74 (0.64–0.86) | <0.01 |
| Percent of Chinese in neighborhood | – | – | 0.98 (0.96–1.00) | 0.15 |
| Percent of Vietnamese in neighborhood | – | – | 1.00 (0.97–1.03) | 0.74 |
| Tobacco Retailer Counts | – | – | 0.79 (0.67–0.94) | <0.01 |
Note: Significant correlates attained p < 0.05 are marked in bold.
5. Discussion
Limited studies have assessed the role of spatial or contextual factors in randomized control trial or intervention studies (Ali et al., 2007, Jarvis et al., 2017, Pruitt et al., 2014). By demonstrating differences in intention to quit in two Asian American groups at baseline, this study shows how neighborhood characteristics and context of place also play a role in reinforcing individual behavior. Existing studies that have examined association between neighborhood characteristics and ethnic minorities (Loomis et al., 2013, Reid et al., 2013) have not examined factors that influence disparities in smoking and quitting within ethnic minority groups in the U.S. (Center for Disease Control and Prevention, 2019). Our study was among the first studies to examine association between spatial or neighborhood variations and intention to quit smoking among Chinese and Vietnamese American male smokers. The findings demonstrate the need to understand contextual factors that contribute to disparities within and between certain groups. One implication from these findings is that interventions that aim to address tobacco-related health disparities by changing individual behaviors should also carefully consider the potential role of neighborhood factors or community-based determinants in contributing to the disparities.
At the individual level, without consideration of the neighborhood contexts, participants’ ethnicity was associated with intention to quit. Similar results were reported from a cross-sectional study with multiple Asian groups suggesting Chinese smokers were less motivated to quit smoking than Vietnamese (Ma et al., 2003). Based on our study sample, we may be able to attribute some of these differences between Chinese and Vietnamese to the socio-demographic characteristics. For example, Vietnamese participants also had lived longer in the US when compared to the Chinese participants (15.5 vs 12.4 years, p = 0.01). Years lived in the US was a significant correlate of increased odds of intention to quit in our sample. This is consistent with some research documenting the association between acculturation and smoking cessation (Castro et al., 2009, Ma et al., 2004). Since many of the immigrants come from countries which have a high burden of tobacco use and where smoking is readily accepted in the culture, living for a longer time in the US, especially in places with stricter tobacco control policies affects social norms, and therefore may influence individual behavior (Castro et al., 2009, Ma et al., 2004). However, when neighborhood factors were accounted for, specifically neighborhood income and tobacco retailer density, ethnicity was no longer significantly associated with quit intention. These findings suggest that the difference observed between Chinese and Vietnamese participants in quit intention were due to neighborhood factors rather than individual characteristics.
At the neighborhood level, we found participants who lived in neighborhood with high tobacco retailers had a lower intention to quit in comparison to those that lived in neighborhoods that had fewer tobacco retailers. Our findings support previous findings showing associations between tobacco retailers near home environment and exposure to tobacco advertising and youth smoking (Henriksen et al., 2008, Loomis et al., 2013, Loomis et al., 2012, Schleicher et al., 2016). However, these studies have focused on younger adults and not on older, more established smokers who are trying to quit. Our findings support ongoing policy efforts aimed at reducing the density of tobacco retailers to reduce the ubiquitous availability of tobacco products, lower exposure to advertising and marketing and environmental cues that influence smoking behavior.
Interestingly, we found a negative association between neighborhood income and intention to quit. This could be due to the characteristics of our respondents as many of the participants belonged to low-income group, yet the neighborhood median household income in which they lived were much higher than their individual income. While this finding seems contradictory to the existing literature, it warrants additional investigation into the association between income inequality and intention to quit as several studies have found the role of area-level income inequality in health behavior and outcomes (Barnett et al., 2005, Blakely et al., 2002, Galea et al., 2007, Kawachi and Kennedy, 1999, Mistry et al., 2011). Unlike previous studies that have shown association between residential segregation or ethnic concentration and smoking behaviors or other health outcomes (Barnett et al., 2004, Barnett et al., 2009, Bell et al., 2007), we did not find an association between neighborhood ethnic density and intention to quit.
5.1. Limitations and strengths
This analysis is from a subset of data originally collected as part of a larger study. Furthermore, the sampling was designed to recruit smokers who were from two Asian American groups, Chinese and Vietnamese Americans in two specific California counties, San Francisco and Santa Clara. The participants could be over-sampled from some neighborhoods in comparison to others. Therefore, the sample of smokers may not be geographically representative. Another limitation of the study is the relatively small sample size in comparison to studies that are based on nationally-representative sample or population-based samples for larger regions.
Our outcome variable is the intention to quit and not actual abstinence even though research has shown strong associations between quit intention to quit attempts and abstinence prospectively (Vangeli et al., 2011). Intention to quit within a specific time period provides valuable insights on the characteristics of “hard to engage smokers” and how the intervention changed their behavior subsequently. As such understanding these differences at the baseline become even more important in the context of intervention studies. Our neighborhood measures mainly capture the environment around participants’ home locations, as we did not have information around their work locations. Hence, we could not capture the retail environment around their workplaces.
6. Conclusion
Overall, we found that both individual and neighborhood factors were associated with intention to quit smoking within 30 days among Chinese and Vietnamese male daily smokers in Northern California who were predominantly immigrants with limited English proficiency. There were ethnic differences observed in their intention to quit smoking, but the differences were explained by neighborhood factors in multivariable analyses. Lower neighborhood median household income, lower tobacco retailer counts, and longer length of residency in the U.S. were associated with having an intention to quit smoking. Findings underscore the significance of taking neighborhood factors into account in designing smoking cessation interventions when targeting subgroups of Asian American smokers where smoking prevalence remains high with a majority of the smokers had no intention to quit smoking within 30 days.
Author contributions
All authors approved the manuscript. Specific roles of each author are listed below:
Priyanka Vyas: Conceptualization, drafted initial version of the manuscript, data analysis, created neighborhood measures, and manuscript revisions
Janice Tsoh: Conceptualization, study supervision, data interpretation, drafted sections of manuscript, and manuscript revisions
Ginny Gildengorin: Methodology, data analysis, data interpretation
Susan Stewart: Methodology, data analysis, data interpretation
Edgar Yu: data acquisition
Alice Guan: data acquisition, data interpretation, critical revision
Amber Pham: data interpretation, critical revision
Nancy J. Burke: data interpretation, critical revision
Steven McPhee: data interpretation, critical revision
Acknowledgments
This research was supported by a grant from the National Institute on Drug Abuse (R01DA036749) awarded to Dr. Janice Tsoh. Dr. Priyanka Vyas was supported by National Institute of Cancer training grant T32CA113710. The authors also wish to express their gratitude to the project lay health workers, the study participants, and study co-investigators and team members: Dr. Angela Sun, Cindy Liang, Joyce Cheng, Joey Zhao at the Chinese Community Health Resource Center (CCHRC); Anthony Nguyen at Southeast Asian Community Center (SEACC); Anita Kearns at Vietnamese Voluntary Foundation (VIVO); Mai Pham at Immigrant Resettlement and Cultural Center (IRCC); Dr. Tung T. Nguyen, Dr. Bang Nguyen, Khanh Le, Ching Wong, Elaine Chan, Fiona Chow, Anne Chen at the University of California San Francisco; as well as advisory board members of Sức Khỏe Là Vàng!-Vietnamese Community Advisory Board, Vietnamese Reach for Health Coalition (VRHC), and Asian American Network for Cancer Awareness, Research and Training-San Francisco (SF-AANCART).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2020.101064.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Ali M., Thiem V.D., Park J.-K., Ochiai R.L., Danovaro-Holliday M.C., Kaljee L.M., Clemens J.D., Acosta C.J. Geographic analysis of vaccine uptake in a cluster-randomized controlled trial in Hue, Vietnam. Health Place. 2007;13:577–587. doi: 10.1016/j.healthplace.2006.07.004. [DOI] [PubMed] [Google Scholar]
- Babb S., Malarcher A., Schauer G., Asman K., Jamal A. Quitting smoking among adults - United States, 2000–2015. MMWR Morb. Mortal. Wkly Rep. 2017;65:1457–1464. doi: 10.15585/mmwr.mm6552a1. [DOI] [PubMed] [Google Scholar]
- Barnett R., Moon G., Kearns R. Social inequality and ethnic differences in smoking in New Zealand. Soc. Sci. Med. 2004;59:129–143. doi: 10.1016/j.socscimed.2003.10.010. [DOI] [PubMed] [Google Scholar]
- Barnett R., Pearce J., Moon G. Does social inequality matter? Changing ethnic socio-economic disparities and Maori smoking in New Zealand, 1981–1996. Soc. Sci. Med. 2005;60:1515–1526. doi: 10.1016/j.socscimed.2004.08.002. [DOI] [PubMed] [Google Scholar]
- Barnett R., Pearce J., Moon G. Community inequality and smoking cessation in New Zealand, 1981–2006. Soc. Sci. Med. 2009;68:876–884. doi: 10.1016/j.socscimed.2008.12.012. [DOI] [PubMed] [Google Scholar]
- Bell J.F., Zimmerman F.J., Mayer J.D., Almgren G.R., Huebner C.E. Associations between residential segregation and smoking during pregnancy among urban African-American women. J. Urban Health. 2007;84:372–388. doi: 10.1007/s11524-006-9152-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blakely T.A., Lochner K., Kawachi I. Metropolitan area income inequality and self-rated health–a multi-level study. Soc. Sci. Med. 2002;54:65–77. doi: 10.1016/s0277-9536(01)00007-7. [DOI] [PubMed] [Google Scholar]
- California Health Interview Survey . UCLA Center for Health Policy Research; Los Angeles, CA: 2019. CHIS Adult Survey (AskCHIS) [Online Interactive Database] [Google Scholar]
- Cantrell J., Anesetti-Rothermel A., Pearson J.L., Xiao H., Vallone D., Kirchner T.R. The impact of the tobacco retail outlet environment on adult cessation and differences by neighborhood poverty. Addiction. 2015;110:152–161. doi: 10.1111/add.12718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castro Y., Reitzel L.R., Businelle M.S., Kendzor D.E., Mazas C.A., Li Y., Cofta-Woerpel L., Wetter D.W. Acculturation differentially predicts smoking cessation among Latino men and women. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2009;18:3468–3475. doi: 10.1158/1055-9965.EPI-09-0450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention, 2019. Tobacco-Related Disparities.
- Chan N.L., Thompson B., Taylor V.M., Yasui Y., Harris J.R., Tu S.P., Acorda E., Jackson J.C. Smoking prevalence, knowledge, and attitudes among a population of Vietnamese American men. Nicotine Tob. Res. 2007;9(Suppl 3):S475–S484. doi: 10.1080/14622200701587086. [DOI] [PubMed] [Google Scholar]
- Dalglish E., McLaughlin D., Dobson A., Gartner C. Cigarette availability and price in low and high socioeconomic areas. Aust. N. Z. J. Public Health. 2013;37:371–376. doi: 10.1111/1753-6405.12086. [DOI] [PubMed] [Google Scholar]
- Gabriel R.M., Mondeaux F.P., Laws K.E., Hahn K.J., Weaver D. Reducing births of drug-affected babies: a retrospective analysis of archival data and a community wide effort. Eval. Program Plann. 2000;23:347–353. [Google Scholar]
- Galea S., Ahern J., Tracy M., Vlahov D. Neighborhood income and income distribution and the use of cigarettes, alcohol, and marijuana. Am. J. Prev. Med. 2007;32:S195–S202. doi: 10.1016/j.amepre.2007.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz K., Kegler M.C. National Cancer Institute, Division of Cancer Control & Population Science; 2008. Enviornments: Theory, Research and Measures of the Built Environment, Health Behavior Constructs: Theory, Measurement and Research Web Resources. [Google Scholar]
- Gregorio D.I., Samociuk H. Breast cancer surveillance using gridded population units, Connecticut, 1992 to 1995. Ann. Epidemiol. 2003;13:42–49. doi: 10.1016/s1047-2797(02)00258-2. [DOI] [PubMed] [Google Scholar]
- Henriksen L., Andersen-Rodgers E., Zhang X., Roeseler A., Sun D.L., Johnson T.O., Schleicher N.C. Neighborhood variation in the price of cheap tobacco products in California: results from healthy stores for a healthy community. Nicotine Tob. Res. 2017;19:1330–1337. doi: 10.1093/ntr/ntx089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henriksen L., Feighery E.C., Schleicher N.C., Cowling D.W., Kline R.S., Fortmann S.P. Is adolescent smoking related to the density and proximity of tobacco outlets and retail cigarette advertising near schools? Prev. Med. 2008;47:210–214. doi: 10.1016/j.ypmed.2008.04.008. [DOI] [PubMed] [Google Scholar]
- Higgs G. A literature review of the use of GIS-based measures of access to health care services. Health Serv. Outcomes Res. Method. 2004;5:119–139. [Google Scholar]
- Hobbs M., Griffiths C., Green M., Jordan H., Saunders J., Christensen A., McKenna J. Fast-food outlet availability and obesity: considering variation by age and methodological diversity in 22,889 Yorkshire Health Study participants. Spatial Spatio-temporal Epidemiol. 2019;28:43–53. doi: 10.1016/j.sste.2018.11.001. [DOI] [PubMed] [Google Scholar]
- J. Immigrant Minority Health. 2010;12(2):206–214. doi: 10.1007/s10903-007-9097-z. [DOI] [PubMed] [Google Scholar]
- Ja D.Y., Aoki B. Substance abuse treatment: culture and barriers in the Asian-American community. J. Psychoact. Drugs. 1993;25:61–71. doi: 10.1080/02791072.1993.10472592. [DOI] [PubMed] [Google Scholar]
- Jarvis C., Di Tanna G.L., Lewis D., Alexander N., Edmunds W.J. Spatial analysis of cluster randomised trials: a systematic review of analysis methods. Emerging Themes Epidemiol. 2017;14:12. doi: 10.1186/s12982-017-0066-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I., Kennedy B.P. Income inequality and health: pathways and mechanisms. Health Serv. Res. 1999;34:215–227. [PMC free article] [PubMed] [Google Scholar]
- Kendzor D.E., Reitzel L.R., Mazas C.A., Cofta-Woerpel L.M., Cao Y., Ji L., Costello T.J., Vidrine J.I., Businelle M.S. Individual- and area-level unemployment influence smoking cessation among African Americans participating in a randomized clinical trial. Soc. Sci. Med. 2012;74:1394–1401. doi: 10.1016/j.socscimed.2012.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King L., Deng W. New York City Department of Health and Mental Hygiene; New York City: 2018. Health Disparities among Asian New Yorkers, Epi Data Brief (100) [Google Scholar]
- Kirchner T.R., Anesetti-Rothermel A., Bennett M., Gao H., Carlos H., Scheuermann T.S., Reitzel L.R., Ahluwalia J.S. Tobacco outlet density and converted versus native non-daily cigarette use in a national US sample. Tobacco Control. 2017;26:85–91. doi: 10.1136/tobaccocontrol-2015-052487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirchner T.R., Cantrell J., Anesetti-Rothermel A., Ganz O., Vallone D.M., Abrams D.B. Geospatial exposure to point-of-sale tobacco: real-time craving and smoking-cessation outcomes. Am. J. Prev. Med. 2013;45:379–385. doi: 10.1016/j.amepre.2013.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J.G., Sun D.L., Schleicher N.M., Ribisl K.M., Luke D.A., Henriksen L. Inequalities in tobacco outlet density by race, ethnicity and socioeconomic status, 2012, USA: results from the ASPiRE Study. J. Epidemiol. Community Health. 2017 doi: 10.1136/jech-2016-208475. jech-2016-208475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li S., Kwon S.C., Weerasingh I., Rey M.J., Trinh-Shevrin C. Smoking among Asian Americans: acculturation and gender in the context of tobacco control policies in New York City. Health Promotion Practice. 2013;14:18S–28S. doi: 10.1177/1524839913485757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loomis B., Kim A., Goetz J., Juster H. Density of tobacco retailers and its association with sociodemographic characteristics of communities across New York. Public Health. 2013;127:333–338. doi: 10.1016/j.puhe.2013.01.013. [DOI] [PubMed] [Google Scholar]
- Loomis B.R., Kim A.E., Busey A.H., Farrelly M.C., Willett J.G., Juster H.R. The density of tobacco retailers and its association with attitudes toward smoking, exposure to point-of-sale tobacco advertising, cigarette purchasing, and smoking among New York youth. Prev. Med. 2012;55:468–474. doi: 10.1016/j.ypmed.2012.08.014. [DOI] [PubMed] [Google Scholar]
- Lovasi G.S., Moudon A.V., Smith N.L., Lumley T., Larson E.B., Sohn D.W., Siscovick D.S., Psaty B.M. Evaluating options for measurement of neighborhood socioeconomic context: evidence from a myocardial infarction case–control study. Health Place. 2008;14:453–467. doi: 10.1016/j.healthplace.2007.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma G.X., Tan Y., Toubbeh J., Su X. Differences in stages of change of smoking behavior among current smokers of four Asian American subgroups. Addict. Behav. 2003;28:1431–1439. doi: 10.1016/s0306-4603(03)00071-6. [DOI] [PubMed] [Google Scholar]
- Ma G.X., Tan Y., Toubbeh J.I., Su X., Shive S.E., Lan Y. Acculturation and smoking behavior in Asian-American populations. Health Educ. Res. 2004;19:615–625. doi: 10.1093/her/cyg070. [DOI] [PubMed] [Google Scholar]
- Martell B.N. Disparities in adult cigarette smoking—United States, 2002–2005 and 2010–2013. MMWR. Morbidity and Mortality Weekly Report. 2016:65. doi: 10.15585/mmwr.mm6530a1. [DOI] [PubMed] [Google Scholar]
- Mistry R., McCarthy W.J., de Vogli R., Crespi C.M., Wu Q., Patel M. Adolescent smoking risk increases with wider income gaps between rich and poor. Health Place. 2011;17:222–229. doi: 10.1016/j.healthplace.2010.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers A.E., Hall M.G., Isgett L.F., Ribisl K.M. A comparison of three policy approaches for tobacco retailer reduction. Prev. Med. 2015;74:67–73. doi: 10.1016/j.ypmed.2015.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Northridge M.E., Sclar E.D., Biswas P. Sorting out the connections between the built environment and health: a conceptual framework for navigating pathways and planning healthy cities. J. Urban Health: Bull. N. Y. Acad. Med. 2003;80:556–568. doi: 10.1093/jurban/jtg064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owusu D., Quinn M., Wang K.S., Aibangbee J., Mamudu H.M. Intentions to quit tobacco smoking in 14 low- and middle-income countries based on the transtheoretical model. Drug Alcohol Depend. 2017;178:425–429. doi: 10.1016/j.drugalcdep.2017.05.033. [DOI] [PubMed] [Google Scholar]
- Paul C.L., Mee K.J., Judd T.M., Walsh R.A., Tang A., Penman A., Girgis A. Anywhere, anytime: retail access to tobacco in New South Wales and its potential impact on consumption and quitting. Soc. Sci. Med. 2010;71:799–806. doi: 10.1016/j.socscimed.2010.05.011. [DOI] [PubMed] [Google Scholar]
- Prochaska J.O., Velicer W.F., Fava J.L., Rossi J.S., Tsoh J.Y. Evaluating a population-based recruitment approach and a stage-based expert system intervention for smoking cessation. Addict. Behav. 2001;26:583–602. doi: 10.1016/s0306-4603(00)00151-9. [DOI] [PubMed] [Google Scholar]
- Pruitt S.L., Leonard T., Murdoch J., Hughes A., McQueen A., Gupta S. Neighborhood effects in a behavioral randomized controlled trial. Health Place. 2014;30:293–300. doi: 10.1016/j.healthplace.2014.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid R.J., Morton C.M., Garcia-Reid P., Peterson N.A., Yu D. Examining tobacco outlet concentration in New Jersey: does income and ethnicity matter? J. Ethnicity Substance Abuse. 2013;12:197–209. doi: 10.1080/15332640.2013.798750. [DOI] [PubMed] [Google Scholar]
- Reitzel L.R., Cromley E.K., Li Y., Cao Y., Dela Mater R., Mazas C.A., Cofta-Woerpel L., Cinciripini P.M., Wetter D.W. The effect of tobacco outlet density and proximity on smoking cessation. Am. J. Public Health. 2011;101:315–320. doi: 10.2105/AJPH.2010.191676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ribisl K.M., Luke D.A., Bohannon D.L., Sorg A.A., Moreland-Russell S. Reducing disparities in tobacco retailer density by banning tobacco product sales near schools. Nicotine Tob. Res. 2016;19:239–244. doi: 10.1093/ntr/ntw185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez D., Carlos H.A., Adachi-Mejia A.M., Berke E.M., Sargent J.D. Predictors of tobacco outlet density nationwide: a geographic analysis. Tobacco Control. 2013;22:349–355. doi: 10.1136/tobaccocontrol-2011-050120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- San Francisco Tobacco Free Project, 2018. San Francisco Tobacco Density Ordinance.
- Schleicher N.C., Johnson T.O., Fortmann S.P., Henriksen L. Tobacco outlet density near home and school: associations with smoking and norms among US teens. Prev. Med. 2016;91:287–293. doi: 10.1016/j.ypmed.2016.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siahpush M., Jones P., Singh G., Timsina L., Martin J. Association of availability of tobacco products with socio-economic and racial/ethnic characteristics of neighbourhoods. Public Health. 2010;124:525–529. doi: 10.1016/j.puhe.2010.04.010. [DOI] [PubMed] [Google Scholar]
- Tong E.K., Gildengorin G., Nguyen T., Tsoh J., Modayil M., Wong C., McPhee S.J. Smoking prevalence and factors associated with smoking status among Vietnamese in California. Nicotine Tobacco Res. 2010;12:613–621. doi: 10.1093/ntr/ntq056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong E.K., Saw A., Fung L.C., Li C.S., Liu Y., Tsoh J.Y. Impact of a smoke-free-living educational intervention for smokers and household nonsmokers: a randomized trial of Chinese American pairs. Cancer. 2018;124(Suppl 7):1590–1598. doi: 10.1002/cncr.31115. [DOI] [PubMed] [Google Scholar]
- Tsoh J.Y., Burke N.J., Gildengorin G., Wong C., Le K., Nguyen A., Chan J.L., Sun A., McPhee S.J. A social network family-focused intervention to promote smoking cessation in Chinese and Vietnamese American male smokers: a feasibility study. Nicotine Tobacco Res. 2015;17:1029–1038. doi: 10.1093/ntr/ntv088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsoh J.Y., Tong E.K., Gildengorin G., Nguyen T.T., Modayil M.V., Wong C., McPhee S.J. Individual and family factors associated with intention to quit among male Vietnamese American smokers: implications for intervention development. Addict. Behav. 2011;36:294–301. doi: 10.1016/j.addbeh.2010.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twigg L., Moon G., Szatkowski L., Iggulden P. Smoking cessation in England: intentionality, anticipated ease of quitting and advice provision. Soc. Sci. Med. 2009;68:610–619. doi: 10.1016/j.socscimed.2008.11.032. [DOI] [PubMed] [Google Scholar]
- Vangeli E., Stapleton J., Smit E.S., Borland R., West R. Predictors of attempts to stop smoking and their success in adult general population samples: a systematic review. Addiction. 2011;106:2110–2121. doi: 10.1111/j.1360-0443.2011.03565.x. [DOI] [PubMed] [Google Scholar]
- Vyas P., Sturrock H., Ling P. Examining the role of a retail density ordinance in reducing concentration of tobacco retailers. Spatial Spatio-temporal Epidemiol. 2020;32:100307. doi: 10.1016/j.sste.2019.100307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White K., Borrell L.N. Racial/ethnic residential segregation: framing the context of health risk and health disparities. Health Place. 2011;17:438–448. doi: 10.1016/j.healthplace.2010.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu D., Peterson N., Sheffer M., Reid R., Schnieder J. Tobacco outlet density and demographics: analysing the relationships with a spatial regression approach. Public Health. 2010;124:412–416. doi: 10.1016/j.puhe.2010.03.024. [DOI] [PubMed] [Google Scholar]
- Zhang J., Wang Z. Factors associated with smoking in Asian American adults: a systematic review. Nicotine Tob. Res. 2008;10:791–801. doi: 10.1080/14622200802027230. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.