Abstract
Background
Up-to-date studies are needed on the protection provided by face masks used by dentists. We assessed the relative filtering efficacy of two currently used surgical face masks (one a molded mask, the other a tie-on mask) and a certified personal particulate respirator, all made by a single manufacturer.
Methods
The authors sprayed bicarbonate particulate against a porcelain surface (representing the patient's mouth) and collected it via a mannequin head (representing the dentist's head) placed 40 centimeters away and a tube with two airflow rates (0.5 cubic meters per hour and 9 m3/hour). They calculated the dry residue weight. They performed three separate runs for each mask and three runs with no mask at the two airflow rates with and without aerosol.
Results
With no mask (control), the authors recorded significant weight gains at both airflow rates with and without vaporization. With vaporization, the three masks were associated with different dry residue weights (P < .03 with the Kruskal-Wallis test at both flow rates), the respirator providing the lowest amount. The respirator provided an efficiency of 94 to 96 percent, compared with 90 to 92 percent and 85 to 86 percent for the molded and tie-on surgical masks, respectively.
Conclusions
These data provide independent evidence that a certified personal respirator can be more effective than high-quality surgical masks in dental settings.
Clinical Implications
Dentists should be aware that a certified particulate respirator can provide them with superior filtering protection.
Key Words: Surgical masks, infection control, particulate, respirators
Face masks greatly reduce the risk of dental care workers' inhaling aerosols from patients' airways, which can contain pathogenic microorganisms related to diseases ranging from influenza to tuberculosis, meningitis or even severe acute respiratory syndrome. Such aerosols also contain large quantities of saliva, microorganisms, blood, tooth particles and restorative materials.1, 2, 3, 4, 5, 6 High-speed, air-driven dental handpieces and ultrasonic scalers produce large amounts of aerosol and spatter,1, 2, 3, 4, 5, 6 including visible and invisible particles, the latter ranging in diameter from 50 micrometers to submicron sizes.7, 8, 9 Particulate matter in the 1- to 5-μm range is considered the most hazardous because it can reach the terminal bronchioli and nonciliated alveoli.10, 11 It has been reported that 95 percent of the particles measure less than 5 μm in diameter; 75 percent of these are contaminated by microorganisms.12 Furthermore, the particles are concentrated mainly within 2 meters of the patient, where they easily can be inhaled by dental operators.13, 14 For these reasons, use of surgical face masks in dentistry has been advocated to protect clinicians from inhaling aerosols containing organic or inorganic particulates, and also to protect the patient from possible contamination from the dental operator.
Various studies have been performed on the filtering efficacy of different general-purpose surgical face masks.10, 11, 15, 16, 17, 18, 19 In 1971, Micik and colleagues11 exposed 15 general-purpose surgical face masks to aerosols comparable to those generated during dental procedures and found that only those made of glass or synthetic fiber displayed relatively high filtering efficiency. In 1987, Pippin and colleagues18 showed that even when masks were worn correctly, the airflow during inhalation could bypass the mask material, resulting in reduced filtering efficacy and an increased health risk for dental operators. Moreover, general-purpose surgical face masks are designed mainly to capture microorganisms in exhaled breath rather than to protect operators from airborne infections. Although specifically designed personal respirators now exist, to our knowledge, no study of efficacy has yet been reported in the scientific literature.
We performed simulations to compare the levels of protective efficacy against particles and aerosols of two surgical face masks in current use among many dental operators with those of a recently developed personal device: a facial filter protection (FFP) 2 disposable particulate respirator certified in accordance with standard EN 149:2001 as set by the European Committee for Standardization.20
METHODS
We performed simulations of a dental hygiene procedure involving an artificial bicarbonate aerosol in a vacant dentist's surgery room (Figure 1 ). Aerosols were formed using the Mini-Clean device (Castellini SpA, Bologna, Italy) with air pressure set to 6 to 7 atmospheres and water flow to 1 atm. We placed the aerosol distributor at a distance of 1 centimeter from a smooth porcelain surface that simulated the patient's mouth. We used a mannequin head to simulate the dentist's face and placed it at a distance of 40 cm from the porcelain surface. The mannequin's oral cavity was covered with latex and had one entry (mouth) and one exit (throat), connected to a 250-milliliter collection flask containing 50 mL of distilled water by a polytetrafluoroethylene tube 30 cm long and 1 cm in diameter that terminated well below the surface of the water. A vacuum pump (Cattani SpA, Parma, Italy) attached to the flask provided two possible airflow rates through the tube of 0.5 cubic meters per hour and 9 m3/hour to simulate human breathing at rest and during exercise, respectively. We adjusted the airflow rates using the lock nut attached to the pump and calibrated by a flow meter. Using scanning electron microscopy, we found that the bicarbonate dust (Airflow Prophylaxis Powder, Electro Medical Systems, Nyon, Switzerland) was composed of particles of monosodium hydrogen carbonate (5–300 μm in diameter), silica particles (< 1 μm in diameter) and other (probably organic) particles of variable dimensions (10–20 μm in diameter).
Figure 1.
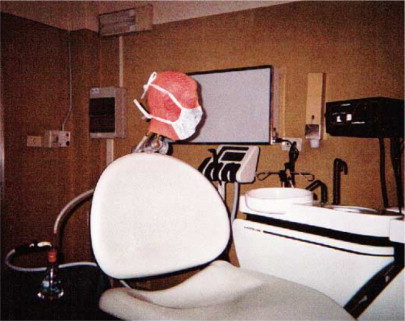
The experimental setting. Mannequin is shown with 1818 Tie-On Surgical Mask (3M ESPE SpA, Milan, Italy).
We tested two types of surgical face masks, the 1818 Tie-On Surgical Mask and the 1942 FB Fluid Resistant Molded Surgical Mask (marketed internationally as the Aseptex Fluid Resistant Molded Surgical Mask 1800) (Figure 2, Figure 3 ) and a personal respirator (1862 Health Care Particulate Respirator and Surgical Mask) certified in accordance with European Committee on Standardization standard EN 149:2001 (Figure 4 ), all made by 3M ESPE SpA (Milan, Italy). We performed four sets of experiments with each of the three masks and in the absence of any mask (control): at the two airflow rates, each with and without vaporization of bicarbonate dust (0.5 m3/hour and 9 m3/hour). We conducted all sets of experiments in triplicate, with each individual run lasting 30 minutes. The room and equipment were cleaned thoroughly between each run. In sets of experiments involving vaporization, we activated the particulate for only the first 10 minutes of the run. We carefully fitted a new mask for each separate run in the position in which it is commonly worn. At the end of each run, we extracted 25 mL of solution from the collection flask and placed it in a beaker that had been cleaned with distilled water, dried and placed in a stove at 100 C for two days, and had then been weighed with a precision (10-microgram) balance (AT 261 Δ Range AD, Mettler-Toledo, Greifensee, Switzerland) and kept in a dryer until use. After addition of the solution, we placed each beaker in a stove at a temperature of approximately 60 C until complete evaporation was achieved, and then kept it at 100 C for another day before weighing it. We calculated the amount of residual dry sediment as the difference between the baseline weight and the final weight of each beaker.
Figure 2.

1818 Tie-On Surgical Mask (3M ESPE SpA, Milan, Italy).
Figure 3.
1942 FB Fluid Resistant Molded Surgical Mask (marketed internationally as the Aseptex Fluid Resistant Molded Surgical Mask 1800) (3M ESPE SpA, Milan, Italy).
Figure 4.
1862 Health Care Particulate Respirator and Surgical Mask (3M ESPE SpA, Milan, Italy).
DATA ANALYSIS
We expressed the data for each experiment as means (± standard deviation) of the three runs. Because the distribution of the values was not normal, we used nonparametric tests. We used the Wilcoxon test (α = .05) to assess the differences between the weight gains recorded at either airflow speed with and without vaporization of bicarbonate dust under control conditions (that is, with no mask), as well as to assess the effect of each mask (in terms of gain in dry residual weight) with respect to control experiments (no mask). We used the Kruskal-Wallis test (α = .05) to compare the filtering effects of the three masks at either airflow speed with and without vaporization. We considered P values less than .05 significant.
RESULTS
Table 1 reports the mean weight gains (that is, the difference between final and baseline weights, representing the amount of residual dry sediment deposited after runs) in the presence of each mask and with no mask under the various experimental conditions (that is, at airflow rates of 0.5 m3/hour and 9 m3/hour with and without vaporization). To confirm the validity of the experimental setup, we compared the weight gains recorded with and without vaporization of bicarbonate powder in the absence of any mask (control conditions): significant differences (P < .05 with the Wilcoxon test) in weight gain were found at both airflow rates. To determine whether any measurable amount of particulate is deposited from the masks themselves during use, we compared the weight gains recorded for each mask in the absence of vaporization with the corresponding control data (no mask); the Wilcoxon test showed no significant difference between any of the masks in comparison with controls at either airflow rate. Furthermore, in the absence of vaporization, we found no difference (Kruskal-Wallis test) among the three types of masks in terms of weight gain. By contrast, we found significant differences among the three masks in the presence of vaporization of bicarbonate dust (P < .03 with the Kruskal-Wallis test at both flow rates), with the lowest amount of residual dry sediment being recorded for the 1862 respirator. Furthermore, the weight of residual dry sediment recorded with each of the three masks always was significantly lower than that found without any mask (always P < .05 using Wilcoxon test, at both flow rates). Taken together, these data indicate that all three masks provide significant filtering abilities, with the 1862 respirator performing best. For both flow rates, we calculated the efficiency of each mask in terms of the percentage weight of particulate filtered with respect to control experiments (without masks), using the following formula:
TABLE 1.
MEAN WEIGHT GAIN IN AMOUNT OF RESIDUAL DRY SEDIMENT RECORDED AFTER 30-MINUTE RUNS.*
| EXPERIMENTAL CONDITIONS | AIR FLOW (m3/HOUR†) | WEIGHT GAIN (MILLIGRAMS) (MEAN ± SD‡ OF THREE RUNS) |
|||
|---|---|---|---|---|---|
| No Mask | 1818 Mask§ | 1942 Mask¶ | 1862 Particulate Respirator# | ||
| Without | 0.5 | 1.22 ± 0.31** | 0.77 ± 0.20 | 0.77 ± 0.45 | 0.78 ± 0.15 |
| Vaporization | 9.0 | 1.39 ± 0.17** | 1.19 ± 0.25 | 0.89 ± 0.21 | 0.64 ± 0.50 |
| With | 0.5 | 10.34 ± 4.42 | 1.59 ± 0.19††‡‡ | 0.99 ± 0.08††‡‡ | 0.60 ± 0.11††‡‡ |
| Vaporization | 9.0 | 14.90 ± 7.94 | 2.03 ± 0.26††‡‡ | 1.19 ± 0.23††‡‡ | 0.61 ± 0.21††‡‡ |
The experimental runs were conducted with two kinds of mask and one particulate respirator and without any mask (control) in the presence of each mask and with no mask (control) under various conditions (at two airflow speeds with and without vaporization of bicarbonate dust).
m3/hour: Cubic meters per hour.
SD: Standard deviation.
1818 Tie-On Surgical Mask (3M ESPE SpA, Milan, Italy).
1942 FB Fluid Resistant Molded Surgical Mask (marketed internationally as the Aseptex Fluid Resistant Molded Surgical Mask 1800) (3M ESPE SpA, Milan, Italy).
1862 Health Care Particulate Respirator and Surgical Mask (3M ESPE SpA, Milan, Italy).
Wilcoxon test, P <. 05 versus vaporization at equivalent air flow rate.
Kruskal-Wallis test, P <. 03 for all three masks.
Wilcoxon test, P <. 05 versus control (no mask).
| Efficiency = [1 − (weight gain with mask /weight gain without mask)] × 100 |
As can be seen in Table 2 , at the airflow rates we analyzed, the 1862 respirator provided 94 to 96 percent efficiency, compared with 90 to 92 percent and 85 to 86 percent for the 1942 and 1818 masks, respectively.
TABLE 2.
FILTERING EFFICIENCIES OF THE THREE SURGICAL MASKS.
| MASK TYPE | PERCENTAGES OF PARTICLES REMOVED (FILTERING EFFICIENCY) AT THE TWO AIRFLOW RATES STUDIED |
|
|---|---|---|
| Airflow Rate | ||
| 0.5 m3/hour* | 9 m3/hour | |
| 1818 Mask† | 85 | 86 |
| 1942 Mask‡ | 90 | 92 |
| 1862 Respirators§ | 94 | 96 |
m3/hour: Cubic meters per hour.
1818 Tie-On Surgical Mask (3M ESPE SpA, Milan, Italy).
1942 FB Fluid Resistant Molded Surgical Mask (marketed internationally as the Aseptex Fluid Resistant Molded Surgical Mask 1800) (3M ESPE SpA, Milan, Italy).
1862 Health Care Particulate Respirator and Surgical Mask (3M ESPE SpA, Milan, Italy).
DISCUSSION
A series of studies all performed between the 1970s and early 1990s examined—from the dentist's point of view—the filtering abilities of surgical face masks.10, 11, 15, 16, 17, 18, 19 However, more up-to-date studies are required to assess the relative filtering efficacy of available face masks used by dentists and dental team members, including disposable particulate respirators. (To our knowledge, ours is the first study to assess the filtering efficacy of a certified respirator specifically designed to protect the operator.) The relevance of such studies is highlighted by current concerns regarding severe acute respiratory syndrome. In the present simulation study, we compared a personal particulate respirator (certified in accordance with European Committee on Standardization standard EN 149:2001) with two conventional surgical masks commonly used by dentists. Our results indicate that the respirator is indeed more effective in filtering particulate of the dimensions commonly encountered in routine dental practice.
To simulate conditions commonly encountered in dental practice, we used vaporized bicarbonate particulate ranging in size from less than 1 μm to 300 μm. In other respects, the filtering simulation method we used (airflow system, collection procedures and so forth) was broadly based on that reported by Pippin and colleagues.18 We chose two different airflow rates of 0.5 m3/hour and 9 m3/hour to mimic human breathing at rest and at maximum exertion.
Having confirmed from the experiments (all performed in triplicate) that the setup was capable of distinguishing different levels of particulate uptake under the various experimental and control conditions (with and without vaporization, masks, and so forth), we found a significant difference in the filtering abilities of the three masks, with the respirator performing better than either of the conventional surgical masks. Under our experimental conditions, the personal device provided 94 to 96 percent filtering efficiency (slightly higher than the 92 percent efficiency level advertised by the manufacturer, probably owing to different testing procedures and conditions). By comparison, the levels of efficiency of the surgical masks were 90 to 92 percent and 85 to 86 percent, broadly in line with the manufacturer's claims.
It is difficult to explain these differences in terms of effective protective benefits for the operator; however, we can conclude that the respirator we studied does indeed filter the type of particulate commonly encountered in dental practice more effectively than either of the two commonly used conventional surgical masks tested. Furthermore, the two surgical masks also showed different levels of efficiency, in keeping with their relative costs. These findings raise questions of cost-effectiveness that are outside the scope of this work.
Specific microbiological data also are outside the scope of our study. However, since powders are themselves vectors of infective pathogens, our data should provide a broad indication of the relative degrees of protection provided by the three masks. Furthermore, although the bicarbonate dust we used included particles of variable dimensions (< 1–300 μm) to mimic the clinical setting, we are unable to provide information about the relative penetration of different-sized particles, including the smallest ones (< 5 μm), which are thought to be particularly hazardous.10, 11 Future studies are needed to investigate these relevant considerations with other masks in current use.
CONCLUSION
This carefully designed simulation study comparing the filtering abilities—from the dentist's point of view—of two commonly used, conventional surgical masks with a modern, certified personal particulate respirator broadly confirms the manufacturer's claims regarding the products' relative characteristics. We thus provide independent confirmation that a certified personal device really is more effective in this setting. Our comparison, restricted to three masks made by a single manufacturer, indicates that a superior design can translate into significantly better filtering performance. To our knowledge, this is the first reported study on this topic for some years. In light of current concerns about transmission of airborne pathogens, we think that further studies are required to produce microbiological and other data on a wider variety of currently available masks.
Footnotes
3M ESPE SpA (Milan, Italy) had no role in the design or execution of the study described in this article, nor in the reporting of its results, and made no financial or commercial contribution toward it.
The authors are grateful to Irene Domenichini for statistical analysis and to Robin M.T. Cooke for scientific editing.
REFERENCES
- 1.Miller RL. Generation of airborne infection … by high speed dental equipment. J Am Soc Prev Dent. 1976;6(3):14–17. [PubMed] [Google Scholar]
- 2.Micik RE, Miller RL, Mazzarella MA, Ryge G. Studies on dental aerobiology, I: bacterial aerosols generated during dental procedures. J Dent Res. 1969;48(1):49–56. doi: 10.1177/00220345690480012401. [DOI] [PubMed] [Google Scholar]
- 3.Miller RL, Micik RE, Abel C, Ryge G. Studies on dental aerobiology, II: microbial splatter discharged from the oral cavity of dental patients. J Dent Res. 1971;50:621–625. doi: 10.1177/00220345710500031701. [DOI] [PubMed] [Google Scholar]
- 4.Larato DC, Ruskin PF, Martin A, Delanko R. Effect of a dental air turbine drill on the bacterial counts in air. J Prosthet Dent. 1966;16:758–765. [Google Scholar]
- 5.Holbrook WP, Muir KF, Macphee IT, Ross PW. Bacteriological investigation of the aerosol from ultrasonic scalers. Br Dent J. 1978;144:245–247. doi: 10.1038/sj.bdj.4804072. [DOI] [PubMed] [Google Scholar]
- 6.Gross KB, Overman PR, Cobb C, Brockmann S. Aerosol generation by two ultrasonic scalers and one sonic scaler: a comparative study. J Dent Hyg. 1992;66:314–318. [PubMed] [Google Scholar]
- 7.Eley BM. The future of dental amalgam: a review of the literature, II: mercury exposure in dental practice. Br Dent J. 1997;182:293–297. doi: 10.1038/sj.bdj.4809370. [DOI] [PubMed] [Google Scholar]
- 8.Shpuntoff H. High-speed dental handpieces and spread of airborne infections. N Y State Dent J. 1993;59(1):21–23. [PubMed] [Google Scholar]
- 9.Stewart FH, Stradling GN. Monitoring techniques for mercury and mercury vapour in dental surgeries: a preliminary report. Br Dent J. 1971;131:299–308. doi: 10.1038/sj.bdj.4802747. [DOI] [PubMed] [Google Scholar]
- 10.Bailey R, Giglio P, Blechman H, Nunez C. Effectiveness of disposable face masks in preventing cross contamination during dental procedures. J Dent Res. 1968;47:1062–1065. doi: 10.1177/00220345680470061001. [DOI] [PubMed] [Google Scholar]
- 11.Micik RE, Miller RL, Leong AC. Studies on dental aerobiology, III: efficacy of surgical masks in protecting dental personnel from airborne bacterial particles. J Dent Res. 1971;50:626–630. doi: 10.1177/00220345710500031801. [DOI] [PubMed] [Google Scholar]
- 12.Timbrell V, Eccles JD. The respirability of the aerosols produced in dentistry. J Dent. 1973;2(1):21–31. doi: 10.1016/s0300-5712(73)80006-5. [DOI] [PubMed] [Google Scholar]
- 13.Belting CM, Haberfelde GC, Juhl LK. Spread of organisms from dental air rotor. JADA. 1964;68:648–651. doi: 10.14219/jada.archive.1964.0145. [DOI] [PubMed] [Google Scholar]
- 14.Bentley CD, Burkhart NW, Crawford JJ. Evaluating spatter and aerosol contamination during dental procedures. JADA. 1994;125:579–584. doi: 10.14219/jada.archive.1994.0093. [DOI] [PubMed] [Google Scholar]
- 15.Ford CR, Peterson DE. The efficacy of surgical face masks. Am J Surg. 1963;106:954–957. doi: 10.1016/0002-9610(63)90163-6. [DOI] [PubMed] [Google Scholar]
- 16.Goldman HS, Hartman KS, Messite J. Occupational hazards in dentistry. Year Book Medical Publishers; Chicago: 1984. p. 21. [Google Scholar]
- 17.Craig DC, Quayle AA. The efficacy of face masks. Br Dent J. 1985;158(3):87–90. doi: 10.1038/sj.bdj.4805540. [DOI] [PubMed] [Google Scholar]
- 18.Pippin DJ, Verderame RA, Weber KK. Efficacy of face masks in preventing inhalation of airborne contaminants. J Maxillofac Surg. 1987;45:319–323. doi: 10.1016/0278-2391(87)90352-1. [DOI] [PubMed] [Google Scholar]
- 19.Del Piano M, Nicosia R, Sessa R, Lolli R, Creatura N, Venezia A. Azione filtrante antibatterica delle mascherine in chirurgia orale. Odontoiatria Oggi. 1991;8:19–26. [Google Scholar]
- 20.European Committee for Standardization EN 149:2001. Respiratory protective devices: filtering half masks to protect against particles—requirements, testing, marking. April 25, 2001. Available for purchase at. “www.cenorm.be/catweb/13.340.30.htm” Accessed July 10, 2003.


