Abstract
Background
Aerosols and droplets are produced during many dental procedures. With the advent of the droplet-spread disease severe acute respiratory syndrome, or SARS, a review of the infection control procedures for aerosols is warranted.
Types of Studies Reviewed
The authors reviewed representative medical and dental literature for studies and reports that documented the spread of disease through an airborne route. They also reviewed the dental literature for representative studies of contamination from various dental procedures and methods of reducing airborne contamination from those procedures.
Results
The airborne spread of measles, tuberculosis and SARS is well-documented in the medical literature. The dental literature shows that many dental procedures produce aerosols and droplets that are contaminated with bacteria and blood. These aerosols represent a potential route for disease transmission. The literature also documents that airborne contamination can be minimized easily and inexpensively by layering several infection control steps into the routine precautions used during all dental procedures.
Clinical Implications
In addition to the routine use of standard barriers such as masks and gloves, the universal use of pre-procedural rinses and high-volume evacuation is recommended.
The production of airborne material during dental procedures is obvious to the dentist, the dental team and the patient. An aerosol cloud of particulate matter and fluid often is clearly visible during dental procedures. This cloud is evident during tooth preparation with a rotary instrument or air abrasion, during the use of an air-water syringe, during the use of an ultrasonic scaler and during air polishing. This ubiquitous aerosolized cloud is a combination of materials originating from the treatment site and from the dental unit waterlines, or DUWLs. It is common for the patient to comment on this cloud of material. With the advent of severe acute respiratory syndrome, or SARS, questions concerning the potential for the spread of infections from this aerosol may arise.
In this article, we review relevant literature that has addressed the presence and makeup of dental aerosols and splatter. We also assess the threats that may be inherent in this airborne material, including risk potential to patients and the dental team. We make recommendations for the control of dental aerosols and splatter.
DISEASE TRANSMISSION THROUGH AN AIRBORNE ROUTE
The potential routes for the spread of infection in a dental office are direct contact with body fluids of an infected patient, contact with environmental surfaces or instruments that have been contaminated by the patient and contact with infectious particles from the patient that have become airborne.1 There is a long history of infections that have been transmitted by an airborne route. Even before the discovery of specific infectious agents such as bacteria and viruses, the potential of infection by the airborne route was recognized. In historical reports of the bubonic plague—the “black plague”—the pneumonic form of the disease was recognized as the most deadly. Historical accounts have noted that the pneumonic form of the plague, characterized by severe coughing, has been spread from patients who had the pneumonic form of plague to those who surrounded the patient but were not necessarily in direct contact. Apparently, because the bacteria that cause plague (Yersinia pestis) were inhaled, the pneumonic form of the disease was reported to progress more rapidly than other forms of plague, and historical reports indicate that it was almost universally fatal.2
There are more recent examples of the spread of disease by an airborne route. In one published report, a number of people were exposed to tuberculosis, or TB, while on a commercial airline flight. A patient with active TB boarded an airplane in Chicago en route to Honolulu. During the flight, the patient coughed repeatedly, aerosolizing the tubercle bacillus, which then entered the airplane’s ventilation system and subsequently spread to other parts of the airplane cabin. After it was confirmed that the patient had active TB, it was determined that 15 of the 55 passengers in the cabin who were tested had been exposed to TB, as confirmed by a positive tuberculin test. Passengers seated within two rows of the source patient had a higher probability of a positive skin test than did those seated elsewhere in the cabin.3
Another published example occurred in a medical office where the measles virus was spread through the ventilation system to multiple people. The source patient was a 12-year-old boy who was coughing. Of the seven people who had secondary cases of measles that were associated with him, three were never in the same room with the source patient and one entered the office an hour after he had left.4
More common is the apparent spread of cold and influenza viruses by airborne routes. However, the actual documentation of an airborne route for transmission of cold and influenza viruses is difficult to verify. Because cold and flu viruses can be transmitted by contact, contaminated objects and an airborne route, in a flu outbreak it often is difficult to know the exact route by which the virus is transferred.
SARS recently has been reported in China, Canada and other countries. This severe flulike illness appears to be caused by a new form of coronavirus, a family of viruses usually associated with the common cold. The exact mechanisms by which SARS is spread remains uncertain, but it is clear that the primary method is through aerosolized droplets produced by coughing or other means. In a Hong Kong apartment complex outbreak, it appeared that the disease may have been spread through ventilation systems by airborne viruses that were independent of larger droplets.5 The Centers for Disease Control and Prevention, or CDC, and the ADA have recommended that aerosol-producing procedures should be avoided in patients with active SARS. The ADA has pointed out that it is unlikely that any dental treatment will be performed on a patient with active SARS, owing to the fact that these patients are extremely ill and should not undergo any elective procedures.6, 7
DENTAL AEROSOL AND SPLATTER
The terms “aerosol” and “splatter” in the dental environment were used by Micik and colleagues8, 9, 10, 11, 12 in their pioneering work on aerobiology. In these articles, aerosols were defined as particles less than 50 micrometers in diameter. Particles of this size are small enough to stay airborne for an extended period before they settle on environmental surfaces or enter the respiratory tract. The smaller particles of an aerosol (0.5 to 10 μm in diameter) have the potential to penetrate and lodge in the smaller passages of the lungs and are thought to carry the greatest potential for transmitting infections.
Splatter was defined by Micik and colleagues as airborne particles larger than 50 μm in diameter. Micik and colleagues stated that these particles behaved in a ballistic manner. This means that these particles or droplets are ejected forcibly from the operating site and arc in a trajectory similar to that of a bullet until they contact a surface or fall to the floor. These particles are too large to become suspended in the air and are airborne only briefly.
The consensus has been that the greatest airborne infection threat in dentistry comes from aerosols (particles less than 50 μm in diameter) due to their ability to stay airborne and potential to enter respiratory passages.13, 14 With the resurgence of TB, however, splatter droplets also must be considered a potential infection threat. The usual method for transmission of TB is through the formation of droplet nuclei.15 These form when a droplet of sputum or saliva containing Mycobacterium tuberculosis is projected from the patient by coughing or potentially by splatter from a dental procedure. As the droplet begins to evaporate, the size of the droplet becomes smaller, and it then has the potential to stay airborne or to become reairborne as a dust particle. Thus, splatter droplets also may be a potential source of infection in a dental treatment setting. Splatter and droplet nuclei also have been implicated in the transmission of diseases other than TB, such as SARS, measles and herpetic viruses. Some diseases known to be spread via an airborne route are listed in Table 1 .
TABLE 1.
DISEASES KNOWN TO BE SPREAD BY DROPLETS OR AEROSOLS.
| DISEASE | METHOD OF TRANSMISSION |
|---|---|
| Pneumonic Plague | Patient to patient without the usual insect vector (flea); apparently by inhalation of the causative bacteria |
| Tuberculosis | Droplet nuclei expelled from the patient by coughing; once considered an occupational disease for dentists |
| Influenza | Apparently associated with coughing but may require direct contact with the patient |
| Legionnaires’ Disease | Aerosolization of Legionella pneumophila has been associated with air conditioning systems and hot tub spas |
| Severe Acute Respiratory Syndrome | Spread by direct contact and aerosolized droplets |
SOURCES OF AIRBORNE CONTAMINATION DURING DENTAL TREATMENT
There are at least three potential sources of airborne contamination during dental treatment: dental instrumentation, saliva and respiratory sources, and the operative site. Contamination from dental instrumentation is the result of organisms on instruments and in DUWLs. Routine cleaning and sterilization procedures should eliminate contamination of all dental instruments except those being used with the current patient. The use of ADA-recommended methods to treat the DUWL also should minimize or eliminate airborne contamination from the DUWL. Because contamination from these sources is controlled relatively easily by following standard procedures, we do not discuss them in detail.16
SALIVA AND RESPIRATORY SOURCES OF CONTAMINATION
The oral environment is inherently wet with saliva that continuously replenishes the fluid in the mouth. The fluids in the mouth are grossly contaminated with bacteria and viruses. Dental plaque, both supragingival and in the periodontal pocket, is a major source of these organisms. It should not, however, be overlooked that the mouth also is part of the oronasal pharynx. As part of this complex, the mouth harbors bacteria and viruses from the nose, throat and respiratory tract. These may included various pathogenic viruses and bacteria that are present in the saliva and oral fluids. Any dental procedure that has the potential to aerosolize saliva will cause airborne contamination with organisms from some or all of these sources.
The most serious potential threat present in aerosols is M. tuberculosis, the organism that causes TB. In the past, TB was viewed as an occupational hazard of dentistry.17, 18 While the number of active TB cases in the United States is relatively small, certain populations such as the homeless, prisoners and recent immigrants have a higher percentage of TB infection.19 Patients known to have active TB should be treated using special respiratory precautions so that the aerosols produced during treatment can be controlled. Patients with undiagnosed, active, infectious TB, however, remain a risk for the dental team and other patients.
The saliva and nasopharyngeal secretions also may contain other pathogenic organisms. These may include common cold and influenza viruses, herpes viruses, pathogenic streptococci and staphylococci, and the SARS virus. The use of universal precautions with all patients initially was based on the assumption that all patients may have an infectious bloodborne infection, such as with hepatitis B virus, hepatitis C virus and HIV. It also should be assumed that all patients may have an infectious disease that has the potential to be spread by dental aerosols; thus, universal precautions to limit aerosols also should be in place.
CONTAMINATION FROM THE OPERATIVE SITE
Most dental procedures that use mechanical instrumentation will produce airborne particles from the site where the instrument is used. Dental handpieces, ultrasonic scalers, air polishers and air abrasion units produce the most visible aerosols. Each of these instruments removes material from the operative site that becomes aerosolized by the action of the rotary instrument, ultrasonic vibrations or the combined action of water sprays and compressed air. The water spray usually is the portion of the aerosol that is most visible to the naked eye and is noticed by the patient and dental personnel. Figure 1 and Figure 2 show the coolant water aerosol and splatter produced by an ultrasonic scaler and air polisher.
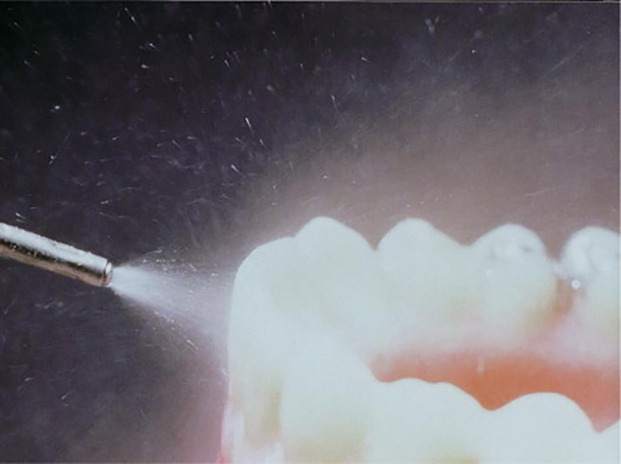
Figure 1.
The visible aerosol cloud produced by an ultrasonic scaler using a flow of 17 milliliters per minute of coolant water.
Figure 2.
The visible aerosol cloud, made up of water and abrasive at the levels recommended by the manufacturer, produced by an air polisher.
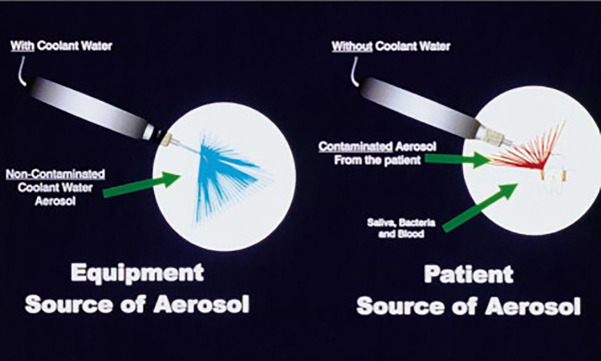
One study, however, showed that when an ultrasonic scaler was used in vitro without any coolant water, there still was a large amount of aerosol and splatter formed from small amounts of liquid placed at the operative site to simulate blood and saliva.20 This airborne material was spread for a distance of at least 18 inches from the operative site. Despite the amount of splatter and the distance it was spread, no visible aerosol was detected during the use of the ultrasonic scaler, and it could only be detected as settled droplets on the environmental surfaces. Figure 3 shows that aerosols and splatter from an ultrasonic scaler can arise both from a coolant water source and directly from the patient.
Figure 3.
The two sources of aerosols produced during dental treatment: coolant water and the patient.
COMPOSITION OF DENTAL AEROSOLS
Qualitative and quantitative analysis of the makeup of dental aerosols would be extremely difficult, and the composition of aerosols probably varies with each patient and operative site. However, it is reasonable to suppose that components of saliva, nasopharyngeal secretions, plaque, blood, tooth components and any material used in the dental procedure, such as abrasives for air polishing and air abrasion, all are present in dental aerosols. In the past, studies usually concentrated on the number of bacteria present in dental aerosols; several recent studies have analyzed the presence of blood components in dental aerosols.21, 22
Multiple studies have been conducted to determine which dental procedure produces the most airborne bacterial contamination.23, 24, 25, 26, 27, 28 In these studies, researchers have measured the number of bacteria that settle on growth media plates over a specific period. In almost all instances, a nonselective bacterial growth media such as blood agar has been used. When an aerobic bacterium settles on the plates and grows as a colony, it will be counted as a colony-forming unit, or CFU. Most results have been reported as the total CFUs produced during the various dental procedures. This method gives a good picture of the increase in total airborne bacterial CFUs from a particular procedure, but it does not provide any differentiation between whether the bacteria are relatively benign or a pathogenic species. Any bacteria that require special media or growth conditions, such as mycobacteria or strict anaerobes that are common in periodontal pockets, will not grow on media used in these tests and therefore are not counted. Also, because they do not grow on the type of media used for bacterial studies, no viral particles such as influenza, rhinoviruses and SARS coronovirus would be measured. Table 2 lists the dental instruments and procedures that produce the greatest amount of aerosols.
TABLE 2.
DENTAL DEVICES AND PROCEDURES KNOWN TO PRODUCE AIRBORNE CONTAMINATION.
| Ultrasonic and Sonic Scalers | Considered the greatest source of aerosol contamination; use of a high-volume evacuator will reduce the airborne contamination by more than 95 percent |
| Air Polishing | Bacterial counts indicate that airborne contamination is nearly equal to that of ultrasonic scalers; available suction devices will reduce airborne contamination by more than 95 percent |
| Air-Water Syringe | Bacterial counts indicate that airborne contamination is nearly equal to that of ultrasonic scalers; high-volume evacuator will reduce airborne bacteria by nearly 99 percent |
| Tooth Preparation With Air Turbine Handpiece | Minimal airborne contamination if a rubber dam is used |
| Tooth Preparation With Air Abrasion | Bacterial contamination is unknown; extensive contamination with abrasive particles has been shown |
Because of the methods used, bacterial growth studies give only a partial picture of the airborne contamination that occurs during dental procedures. However, in relative terms these studies can be viewed as providing a good comparative index of the amount of airborne material that is generated during various dental procedures. Using the bacterial growth method, the ultrasonic scaler has been shown to produce the greatest amount of airborne contamination, followed by the air-driven high-speed handpiece, the air polisher and various other instruments such as the air-water syringe and prophylaxis angles.12, 23, 24, 25, 26, 27, 28 To date, no studies have been performed on the bacterial contamination produced by air abrasion.
Investigations have evaluated the presence or absence of blood contamination in the aerosols produced during root planing when an ultrasonic scaler is used.21, 22 These studies have shown that blood is present universally in ultrasonic scaler aerosols during root planing. While the presence of blood has not been directly studied, it would seem logical that blood also would be present in any dental aerosol that is produced by an instrument in a blood-contaminated field. This would include restorative procedures that extend subgingivally, as well as periodontal and oral surgery procedures.
METHODS OF REDUCING AIRBORNE CONTAMINATION
As noted previously, if the ADA’s recommendations for sterilization of instruments and treatment of DUWLs are followed, these major sources of potentially contaminated dental aerosols can be controlled. However, it should be recognized that the aerosol created by the interaction of coolant water and ultrasonic vibrations or by compressed air and a rotary motion are visible to patients and dental personnel. It is important that this aerosol cloud be controlled to the greatest extent possible to reassure patients and dental personnel. It also should be recognized that contaminated aerosols are produced during dental procedures when there are little or no visible aerosols. As has been shown in the study of aerosol production by ultrasonic scalers when no coolant water was used, even in the complete absence of coolant water there is aerosolization of material from the operative site.20 During routine dental treatment, there is a strong likelihood that aerosolized material will include viruses, blood, and supra- and subgingival plaque organisms.
At this time, it is impossible to determine the exact infection risk represented by aerosolized material. The potential for the spread of infection via an almost invisible aerosol, however, must be recognized and minimized or eliminated to the greatest extent feasible within a clinical situation.
The use of personal barrier protection such as masks, gloves and eye protection will eliminate much of the danger inherent in splatter droplets arising from the operative site.29 However, any infectious material that is present in a true aerosol form (particles less than 50 μm in diameter) or splatter that becomes reairborne as droplet nuclei has the potential to enter the respiratory tract through leaks in masks30 and contact mucus membranes by going around protective devices such as safety glasses. A true aerosol or droplet nuclei may be present in the air of the operatory for up to 30 minutes after a procedure.13 This means that after a dental procedure, if the operator removes a protective barrier such as a face mask to talk to a patient when a procedure is completed, the potential for contact with airborne contaminated material remains. Also, there is a potential for an airborne contaminant to enter the ventilation system and spread to areas of the facility where barrier protection is not used.
One method of reducing overall bacterial counts produced during dental procedures is the use of a preprocedural rinse. The use of a .01 percent chlorhexidine or essential oil–containing mouthwash for one minute before a dental procedure has been shown to significantly reduce the bacterial count in the air of the operatory.31, 32 Chlorhexidine is an effective antiseptic for free-floating oral bacteria such as those found in the saliva and those loosely adhering to mucus membranes. Chlorhexidine, however, does not affect bacteria in a biofilm such as established dental plaque, does not penetrate subgingivally, will not affect blood coming directly from the operative site and is unlikely to affect viruses and bacteria harbored in the nasopharynx. While preprocedural rinses will reduce the extent of contamination within dental aerosols as routinely measured on agar plates, they do not eliminate the infectious potential of dental aerosols.
During many dental procedures, the use of a rubber dam will eliminate virtually all contamination arising from saliva or blood. If a rubber dam can be used, the only remaining source for airborne contamination is from the tooth that is undergoing treatment. This will be limited to airborne tooth material and any organisms contained within the tooth itself. In certain restorative procedures such as subgingival restorations and the final steps of crown preparation, it often is impossible to use a rubber dam. The use of a rubber dam also is not feasible for periodontal and hygiene procedures such as root planing, periodontal surgery and routine prophylaxis. This is of particular concern owing to the fact that periodontal procedures always are performed in the presence of blood and instruments such as the ultrasonic scaler, which has been shown to create the greatest amount of aerosol contamination, are used.
Two methods are available to reduce airborne contamination arising from the operative site. One method involves using devices that remove the contaminated material from the air of the treatment area after it has become airborne. The other is to remove the airborne contamination before it leaves the immediate area surrounding the operative site. The most frequently mentioned methods of removing airborne contamination from the air of the treatment room are the use of a high efficiency particulate air, or HEPA, filter and the use of ultraviolet, or UV, chambers in the ventilation system. While both of these systems appear to reduce airborne contamination, they are somewhat expensive; the UV system is cost-prohibitive for most dental offices at this time. Both approaches also have the problem that it takes an extended period for the air in the treatment room to cycle through the filter or UV treatment system.
From a practical point of view, it is easiest to remove as much airborne contamination as possible before it escapes the immediate treatment site. The use of a high-volume evacuator, or HVE, has been shown to reduce the contamination arising from the operative site by more than 90 percent.8, 23, 33, 34, 35 It should be emphasized that for a suction system to be classified as an HVE, it must remove a large volume of air within a short period. An evacuator that pulls a high vacuum but does not remove a large volume of air, such as is used routinely for hospital suction, is not considered an HVE. The usual HVE used in dentistry has a large opening (usually 8 millimeters or greater) and is attached to an evacuation system that will remove a large volume of air (up to 100 cubic feet of air per minute). The small opening of a saliva ejector does not remove a large enough volume of air to be classified as an HVE.
During restorative dentistry, the HVE often will be used by an assistant who is able to guide and aim the vacuum in a manner that eliminates or greatly reduces the visible water spray produced during dental procedures. It has been shown that the number of CFUs produced during dental procedures is reduced greatly when an assistant uses an HVE.8 A problem arises when the operator is working without an assistant. This often is the case during delivery of periodontal treatment by a dental hygienist. Several options are available to operators working without an assistant. They include using the operating instrument in one hand and the HVE in the other hand, HVE devices that attach to the operating instrument and various “dry field” devices that attach to an HVE. For air polishing and air abrasion, devices are available that combine a barrier device to help contain the abrasive material and a vacuum to remove the abrasive material and the airborne particles created by the procedures.28, 36 All of these instruments are available commercially from multiple sources.
It must be emphasized that no single approach or device can minimize the risk of infection to dental personnel and other patients completely. A single step will reduce the risk of infection by a certain percentage, another step added to the first step will reduce the remaining risk, until such time as the risk is minimal. This can be described as a layering of protective procedures. This layering of infection control steps needs to be followed in reducing the potential danger from dental aerosols.
The dental team should not rely on a single precautionary strategy. In the reduction of dental aerosols, the first layer of defense is personal protection barriers such as masks, gloves and safety glasses. The second layer of defense is the routine use of an antiseptic preprocedural rinse with a mouthwash such as chlorhexadine. The third layer of defense is the routine use of an HVE either by an assistant or attached to the instrument being used. An additional layer of defense may be the use of a device to reduce aerosol contamination that escapes the operating area, such as a HEPA filter. The first three layers of defense are found routinely in most dental operatories, are inexpensive and can be made part of routine infection control practices easily. Unfortunately, many operators appear to use only the first layer of defense (personal protection barriers) without following the other simple steps. All three simple and inexpensive steps should be followed routinely for adequate protection. Table 3 lists the available methods of reducing aerosols and splatter contamination, as well as their relative effectiveness and costs.
TABLE 3.
METHODS OF REDUCING AIRBORNE CONTAMINATION.
| DEVICE | ADVANTAGES | DISADVANTAGES |
|---|---|---|
| Barrier Protection—Masks, Gloves and Eye Protection | Part of “standard precautions,” inexpensive | Masks will only filter out 60 to 95 percent of aerosols, subject to leakage if not well-fitted, do not protect when mask is removed after the procedure |
| Preprocedural Rinse With Antiseptic Mouthwash Such as Chlorhexidine | Reduces the bacterial count in the mouth, saliva and air; inexpensive on a per-patient basis | Tends to be most effective on freefloating organisms; it will not affect biofilm organisms such as plaque, subgingival organisms, blood from the operative site or organisms from the nasopharynx |
| High-Volume Evacuator | Will reduce the number of bacteria in the air and remove most of the material generated at the operative site such as bacteria, blood and viruses; inexpensive on a per-patient basis | When an assistant is not available, it is necessary to use a high-volume evacuator attached to the instrument or a “dry field” device; a small-bore saliva ejector is not an adequate substitute |
| High-Efficiency Particulate Air Room Filters and Ultraviolet Treatment of Ventilation System | Effective in reducing numbers of airborne organisms | Only effective once the organisms are already in the room’s air, moderate to expensive, may require engineering changes to the ventilation system |
REGULATORY AND LEGAL CONCERNS
The ADA and CDC have recommended that all blood-contaminated aerosols and splatter should be minimized.29 Occupational Safety and Health Administration regulations state that “all procedures involving blood or other potentially infectious materials shall be performed in such a manner as to minimize splashing, spraying, spattering, and generation of droplets of the these substances.”37 In the guidelines for infection control in dental health-care settings that was published recently by the CDC, all of these recommendations were retained. The use of rubber dams and HVEs are considered to be “appropriate work practices”—precautions that always should be followed during dental procedures.38
By following the simple and inexpensive recom mendations for controlling aerosols and splatter outlined in this article, dental practitioners will be in compliance with these recommendations and will minimize any legal or regulatory risks that may exist.
CONCLUSIONS
The aerosols and splatter generated during dental procedures have the potential to spread infection to dental personnel and other people in the dental office. While, as with all infection control procedures, it is impossible to completely eliminate the risk posed by dental aerosols, it is possible to minimize the risk with relatively simple and inexpensive precautions. We feel that the following procedures are appropriate as universal precautions whenever an aerosol is produced:
-

universal barrier precautions should be followed;
-

a preprocedural rinse should be used before treatment;
-

a rubber dam should be used where possible;
-

an HVE should be used for all procedures. The use of these precautions should reduce the risk of an aerosolized spreading of infection to a minimal level. Further, the universal application of these infection control strategies will reduce the employer’s legal exposure to the lowest possible level.
Biographies
 Dr. Harrel is an associate clinical professor, Baylor College of Dentistry, Dallas. He also maintains a private practice at 10246 Midway Road, #101, Dallas, Texas 75229. Address reprint requests to Dr. Harrel.
Dr. Harrel is an associate clinical professor, Baylor College of Dentistry, Dallas. He also maintains a private practice at 10246 Midway Road, #101, Dallas, Texas 75229. Address reprint requests to Dr. Harrel.
 Dr. Molinari is a professor and the chairman, Biomedical Sciences, University of Detroit Mercy School of Dentistry, Detroit.
Dr. Molinari is a professor and the chairman, Biomedical Sciences, University of Detroit Mercy School of Dentistry, Detroit.
References
- 1.Garner JS. Guideline for isolation precautions in hospitals. The Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol. 1996;17(1):53–80. doi: 10.1086/647190. [DOI] [PubMed] [Google Scholar]
- 2.Gottfried RS. The black death: Natural and human disaster in medieval Europe. Free Press; New York: 1983. pp. 7–10. [Google Scholar]
- 3.Kenyon TA, Valway SE, Ihle WW, Onorato IM, Castro KG. Transmission of multidrug-resistant Mycobacterium tuberculosis during a long airplane flight. N Engl J Med. 1996;334(15):933–938. doi: 10.1056/NEJM199604113341501. [DOI] [PubMed] [Google Scholar]
- 4.Bloch AB, Orenstein WA, Ewing WM. Measles outbreak in a pediatric practice: airborne transmission in an office setting. Pediatrics. 1985;75:676–683. [PubMed] [Google Scholar]
- 5.World Health Organization Communicable disease surveillance and response (CSR): severe acute respiratory syndrome (SARS) Available at: “www.who.int/csr/sars/en/” Accessed June 14, 2003.
- 6.CDC Interim domestic infection control precautions for aerosol-generating procedures on patients with severe acute respiratory syndrome (SARS) Available at: “www.cdc.gov/ncidod/sars/aerosolinfectioncontrol.htm” Accessed June 14, 2003.
- 7.American Dental Association Severe acute respiratory syndrome (SARS). Available at. “www.ada.org/prof/resources/topics/sars.asp” Accessed June 14, 2003.
- 8.Micik RE, Miller RL, Mazzarella MA, Ryge G. Studies on dental aerobiology, I: bacterial aerosols generated during dental procedures. J Dent Res. 1969;48(1):49–56. doi: 10.1177/00220345690480012401. [DOI] [PubMed] [Google Scholar]
- 9.Miller RL, Micik RE, Abel C, Ryge G. Studies of dental aerobiology, II: microbial splatter discharged from the oral cavity of dental patients. J Dent Res. 1971;50:621–625. doi: 10.1177/00220345710500031701. [DOI] [PubMed] [Google Scholar]
- 10.Micik RE, Miller RL, Leong AC. Studies on dental aerobiology, 3: efficacy of surgical masks in protecting dental personnel from airborne bacterial particles. J Dent Res. 1971;50:626–630. doi: 10.1177/00220345710500031801. [DOI] [PubMed] [Google Scholar]
- 11.Abel LC, Miller RL, Micik RE, Ryge G. Studies on dental aerobiology, IV: bacterial contamination of water delivered by dental units. J Dent Res. 1971;50:1567–1569. doi: 10.1177/00220345710500063601. [DOI] [PubMed] [Google Scholar]
- 12.Miller RL, Micik RE. Air pollution and its control in the dental office. Dent Clin North Am. 1978;22:453–476. [PubMed] [Google Scholar]
- 13.Hinds WC. Aerosol technology: Properties, behavior, and measurement of airborne particles. Wiley; New York: 1982. pp. 6–8. [Google Scholar]
- 14.Cottone JA, Terezhalmy GT, Molinari JA. Practical infection control in dentistry. Williams & Wilkins; Baltimore: 1996. pp. 139–140. [Google Scholar]
- 15.Zinsser H, Joklik WK. Zinsser microbiology. 20th ed. Appleton & Lange; Norwalk, Conn.: 1992. pp. 497–525. [Google Scholar]
- 16.Murdoch-Kinch CA, Andrews NL, Atwan S, Jude R, Gleason MJ, Molinari JA. Comparison of dental water quality management procedures. JADA. 1997;128:1235–1243. doi: 10.14219/jada.archive.1997.0400. [DOI] [PubMed] [Google Scholar]
- 17.Smith WH, Davies D, Mason KD, Onions JP. Intraoral and pulmonary tuberculosis following dental treatment. Lancet. 1982;1:842–844. doi: 10.1016/s0140-6736(82)91886-4. [DOI] [PubMed] [Google Scholar]
- 18.Belting CM, Haberfelde GC, Juhl LK. Spread of organisms from dental air rotor. JADA. 1964;68:648–651. doi: 10.14219/jada.archive.1964.0145. [DOI] [PubMed] [Google Scholar]
- 19.Shearer BG. MDR-TB. Another challenge from the microbial world. JADA. 1994;125(1):42–49. doi: 10.14219/jada.archive.1994.0002. [DOI] [PubMed] [Google Scholar]
- 20.Harrel SK, Barnes JB, Rivera-Hidalgo F. Aerosol and splatter contamination from the operative site during ultrasonic scaling. JADA. 1998;129:1241–1249. doi: 10.14219/jada.archive.1998.0421. [DOI] [PubMed] [Google Scholar]
- 21.King TB, Muzzin KB, Berry CW, Anders LM. The effectiveness of an aerosol reduction device for ultrasonic scalers. J Periodontol. 1997;68(1):45–49. doi: 10.1902/jop.1997.68.1.45. [DOI] [PubMed] [Google Scholar]
- 22.Logothetis DD, Gross KB, Eberhart A, Drisko C. Bacterial airborne contamination with an air-polishing device. Gen Den. 1988;36:496–499. [PubMed] [Google Scholar]
- 23.Bentley CD, Burkhart NW, Crawford JJ. Evaluating spatter and aerosol contamination during dental procedures. JADA. 1994;125:579–584. doi: 10.14219/jada.archive.1994.0093. [DOI] [PubMed] [Google Scholar]
- 24.Legnani P, Checchi L, Pelliccioni GA, D’Achille C. Atmospheric contamination during dental procedures. Quintessence Int 994;25:435–9. [PubMed]
- 25.Gross KB, Overman PR, Cobb C, Brockmann S. Aerosol generation by two ultrasonic scalers and one sonic scaler: a comparative study. J Dent Hyg. 1992;66:314–318. [PubMed] [Google Scholar]
- 26.Muzzin KB, King TB, Berry CW. Assessing the clinical effectiveness of an aerosol reduction device for the air polisher. JADA. 1999;130:1354–1359. doi: 10.14219/jada.archive.1999.0407. [DOI] [PubMed] [Google Scholar]
- 27.Harrel SK. Clinical use of an aerosol-reduction device with ultrasonic scaler. Compend Cont Educ Dent. 1996;17:1185–1193. [PubMed] [Google Scholar]
- 28.Barnes JB, Harrel SK, Rivera-Hidalgo F. Blood contamination of the aerosols produced by the in vivo use of ultrasonic scalers. J Periodontol. 1998;69:434–438. doi: 10.1902/jop.1998.69.4.434. [DOI] [PubMed] [Google Scholar]
- 29.Infection control recommendations for the dental office and the dental laboratory. ADA Council on Scientific Affairs and ADA Council on Dental Practice. JADA. 1996;127:672–680. doi: 10.14219/jada.archive.1996.0280. [DOI] [PubMed] [Google Scholar]
- 30.Pippen DJ, Verderame RA, Weber KK. Efficacy of face masks in preventing inhalation of airborne contaminants. J Oral Maxillofac Surg. 1987;45:319–323. doi: 10.1016/0278-2391(87)90352-1. [DOI] [PubMed] [Google Scholar]
- 31.Logothetis DD, Martinez-Welles JM. Reducing bacterial aerosol contamination with a chlorhexidine gluconate pre-rinse. JADA. 1995;126:1634–1639. doi: 10.14219/jada.archive.1995.0111. [DOI] [PubMed] [Google Scholar]
- 32.Fine DH, Korik I, Furgang D. Assessing pre-procedural subgingival irrigation and rinsing with an antiseptic mouthrinse to reduce bacteremia. JADA. 1996;127(5):641–642. doi: 10.14219/jada.archive.1996.0276. 645–6. [DOI] [PubMed] [Google Scholar]
- 33.Harrel SK, Barnes JB, Rivera-Hidalgo F. Reduction of aerosols produced by ultrasonic scalers. J Periodontol. 1996;67(1):28–32. doi: 10.1902/jop.1996.67.1.28. [DOI] [PubMed] [Google Scholar]
- 34.Jacks ME. A laboratory comparison of evacuation devices on aerosol reduction. J Dent Hyg. 2002;76(3):202–206. [PubMed] [Google Scholar]
- 35.Klyn SL, Cummings DE, Richardson BW, Davis RD. Reduction of bacteria-containing spray produced during ultrasonic scaling. Gen Dent. 2001;49(6):648–652. [PubMed] [Google Scholar]
- 36.Harrel SK, Barnes JB, Rivera-Hidalgo F. Aerosol reduction during air polishing. Quintessence Int. 1999;30:623–628. [PubMed] [Google Scholar]
- 37.Occupational exposure to bloodborne pathogens: OSHA—Final rule. Fed Regist. 1991;56(235):64004–64182. [PubMed] [Google Scholar]
- 38.Kohn WG, Collins AS, Cleveland JL, Harte JA, Eklund KJ, Malvitz DM, Centers for Disease Control and Prevention (CDC) Guidelines for infection control in dental health-care settings: 2003. MMWR Recomm Rep. 2003;52(RR-17):16–17. [PubMed] [Google Scholar]