Abstract
Background
The authors conducted a study to compare the effectiveness of two dry-field isolation techniques with that of a control technique (no isolation) in reducing spatter from a dental operative site.
Methods
The authors designed a benchtop experiment to evaluate spatter patterns after performing simulated occlusal surface preparations on three typodont teeth in a dental manikin. Fluorescein dye served as the marker to enable visualization of the spatter distribution. The authors compared the effectiveness of a nonisolated control consisting of high-volume evacuation (HVE) alone with that of two dry-field isolation techniques: a dental dam with HVE and the Isolite system (Isolite Systems, Santa Barbara, Calif).
Results
The authors performed a two-way analysis of variance. Both the Isolite device and the dental dam with HVE exhibited a significant decrease in the number of contaminated squares (P < .001) compared with that for the nonisolated control. In addition, overall, the results showed no statistically significant difference between the Isolite system and the dental dam with HVE (P = .126).
Conclusions
The study results showed that use of a dental dam with HVE or the Isolite system significantly reduced spatter overall compared with use of HVE alone.
Clinical Implications
Isolation with a dental dam and HVE or with the Isolite system appears to aid in the reduction of spatter during operative dental procedures, potentially reducing exposure to oral pathogens.
Key Words: Dental dam, spatter, aerosol, fluorescence, isolation, high-volume evacuation
ABBREVIATION KEY: HVE: High-volume evacuator or evacuation
Dentists perform complex procedures routinely in the oral cavity. However, certain adverse conditions or potential complications are inherent to this part of the anatomy. They include continual salivary flow, a relatively dark environment in which shadowing is common, adjacent soft tissues in close proximity to the treatment site, open access to the patient's airway and the patient's difficulty in maintaining an open mouth. The use of a dental dam and rubber bite block is a common method of controlling some of these conditions.
Aerosol and spatter production during dental procedures in the oral cavity—including hard-tissue preparation with a high-speed dental handpiece and an ultrasonic scaler—has been well documented in the literature.1, 2, 3, 4, 5, 6 This aerosol and spatter might contain infectious agents originating from the patient or the dental unit waterlines that pose a health threat to the dentist, patient and staff members who are within the spray's pattern.7, 8, 9, 10, 11
Miller1 reported that aerosols generated from a patient's mouth can contain up to 100,000 bacteria per cubic foot of air. Although the aerosol (particles of respirable size < 10 micrometers) may remain airborne for extended periods, the large-particle spatter, which makes up the bulk of the spray from handpieces and ultrasonic scalers, settles quickly, landing on nearby surfaces. This pattern can encompass the area occupied by the dentist and dental team members during routine dental treatment.12, 13
In their review of the literature, Harrel and Molinari7 indicated that diseases such as tuberculosis, influenza, legionnaires' disease and severe acute respiratory syndrome are transmissible via droplets or aerosols. Therefore, a reduction of aerosol and spatter generated under normal dental operative conditions may lead to a decrease in the potential for transmission of communicable diseases from patient to dentist and dental staff members. Cochran and colleagues14 reported the effectiveness of a dental dam in reducing microbial contamination during dental procedures. In addition, several researchers have reported that use of a high-volume evacuator (HVE) can reduce the aerosol and spatter production arising from the dental procedural site by more than 90 percent.2, 15, 16, 17, 18
We conducted this study to compare the effectiveness of two dry-field isolation techniques—the Isolite system (Isolite Systems, Santa Barbara, Calif.) and a dental dam with bite block and concurrent use of an HVE—with that of HVE alone (control) to reduce spatter from a dental operative site. Our null hypothesis was that the dry-field techniques would not result in a significant reduction of spatter compared with the control technique.
METHODS
In a dental operatory (with the door closed), we conducted a benchtop exercise to compare the spatter pattern obtained while performing a simulated tooth preparation procedure. We covered the air inlet vent to the operatory so that no airflow currents were present, as they could have affected the spatter pattern. We inserted a typodont manikin head (KaVo Dental, Charlotte, N.C.) into the headrest position of a dental chair. We constructed a 4 × 3-foot wooden platform to surround the manikin head as it was reclined into a usual position for operative dentistry so that the maxillary dental occlusal plane was perpendicular to the floor. We then inserted a typodont (D95SDP-200 32 Teeth Soft Gingivae Type, Kilgore International, Cold-water, Mich.) into the maxillary and mandibular positions of the manikin head. Royal blue fadeless bulletin board paper was trimmed to fit and placed on the wooden platform.
We placed two laboratory stands next to the manikin at the 2-o'clock and 12-o'clock positions. Each stand held a three-pronged clamp in which we placed a dental handpiece or the HVE and maintained it in a fixed position. We used vinyl polysiloxane (VP Mix regular set mint [102–8752], Henry Schein, Melville, N.Y.) to adapt the clamps closely to the handpiece and HVE. We oriented the dental handpiece and HVE in such a way as to simulate the position of a right-handed dentist during preparation of the occlusal surface of three posterior teeth (nos. 18, 19 and 20) (Figure 1 ). We placed a carbide 330 bur in the dental handpiece and oriented it into a small occlusal preparation in the tooth to act as an index for reproducibility.
Figure 1.

Overview of the experimental design setup.
To simulate the volumetric size of the oral cavity, we placed the vinyl polysiloxane putty in areas of the typodont in which water may flow. In a clinical situation, the Isolite system and a dental dam adapt closely to the oral soft tissues so that essentially no spaces exist through which water spray could flow into the oropharynx (Figure 2 ). In the typodont, various spaces exist that may skew the spatter pattern or volume of spray. Placement of the vinyl polysiloxane putty allowed for a closer approximation to in vivo conditions.
Figure 2.

Placement of the Isolite system (Isolite Systems, Santa Barbara, Calif.) in the mouth, showing close adaptation to the oral soft tissues. Image of the Isolite system reproduced with permission of Isolite Systems, Santa Barbara, Calif.
We oriented the orifice of the HVE to be parallel to and 1 centimeter from the buccal surface of the experimental tooth during the control and dental dam trials (Figure 3 ). We used water and air spray to approximate the aerosol plume produced during operative dental procedures, and we used one high-speed handpiece (KaVo INTRAmatic LUX 3 25LHA, KaVo Dental). The handpiece was operated at the maximum torque and rotation speed of 200,000 revolutions per minute for 10 seconds. We set the water flow through the handpiece at 25 milliliters/minute19, 20 and set the air pressure to achieve a normal aerosol plume. We measured the rate of suction of the HVE and the Isolite device by inserting each into a 2-liter graduated cylinder filled with 2,000 mL of water. The HVE cleared all water in the cylinder in 14 seconds, equating to a rate of 142.9 mL/second. The Isolite device cleared all water in the cylinder in 35 seconds, equating to a rate of 57.1 mL/second. We conducted all 72 trials (as described later) in one session and did not adjust any settings.
Figure 3.

Experimental setup for the dental dam with a high-volume evacuator. Note the proximity of the high-volume evacuator to the buccal surface of the tooth.
The control consisted of a simulated preparation on teeth nos. 18, 19 and 20, with a bite block in place and an HVE positioned adjacent to the operative site as described earlier. The first experimental condition consisted of a simulated tooth preparation with use of a bite block, a dental dam and the HVE. The second experimental condition consisted of a simulated tooth preparation and use of the Isolite system set at maximum strength. The Isolite system is designed to provide simultaneous isolation of the maxillary and mandibular quadrants with use of a mouthpiece that has flexible flanges. The system also provides illumination and is used to aspirate oral fluids. The dental dam trials involved the use of a standard 6-inch non-latex dental dam punched with three holes to isolate teeth nos. 18, 19 and 20 for each trial.
We added a 0.1 percent fluorescein dye solution (Sigma-Aldrich, St. Louis) to the dental unit water supply. During the simulated tooth preparation procedure, the water spray aerosolized and scattered away from the test tooth; the resulting spatter settled outside of the typodont mouth and onto the paper-covered platform. We removed the bulletin board paper after each trial and allowed it to dry thoroughly. We then numbered each sheet of paper randomly so that scoring would be masked.
We constructed a 5–square centimeter overlay grid with the use of framer's string fixed tightly at 5-cm intervals. We placed the grid on each sheet of paper. We held a light-emitting diode dental curing light (Demi, Kerr, Orange, Calif.) (emitting blue light with a spectral range of between 425 and 500 nanometers) 8 cm from the surface of the paper and used it to fluoresce the spatter droplets that had collected. When viewed through amber-colored protective glasses, the fluorescence was visualized easily (Figure 4 ). If the operator (M.C.H., J.M.L.) found even one spot of fluorescence within a 5-cm2 grid, he scored the sample as being contaminated. The operator then counted the number of squares with contamination to determine the amount of spatter produced in each trial.
Figure 4.
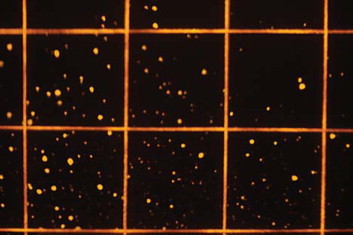
Fluorescent spatter with overlay grid. The image is from one of the control trials for tooth no. 18.
To achieve a power of 0.80 (effect size = 0.20; P < .05), 24 trials in each group were necessary. Therefore, we conducted eight trials for each of the three teeth tested in each group (that is, the control and two experimental groups). This resulted in a total of 72 trials for the experiment. Two graders (M.C.H., J.M.L.) each scored 36 trials. To analyze the data, we conducted a two-way analysis of variance (ANOVA) with the use of statistical software (PASW statistics 18.0.0, IBM, Armonk, N.Y.). The results of the ANOVA indicated both significant main effects and interaction effects. We subsequently conducted a post hoc Tukey honestly significant difference test for the main effects, and we used a Bonferroni correction to evaluate pairwise comparisons of the interaction effects.
RESULTS
To ensure interrater agreement, each grader scored four of the other grader's trials in a masked fashion, and we calculated a κ statistic (κ = 0.98). The dependent variable—amount of spatter—was normally distributed for the groups formed by the combination of tooth number and isolation method, as assessed by the Shapiro-Wilk test (P > .05). The results showed homogeneity of variance between groups, as assessed by Levene's test for equality of error variances (P = .273). Table 1 shows the descriptive statistics including mean (standard deviation) number of contaminated squares.
Table 1.
Descriptive statistics showing mean number of contaminated squares.
| TOOTHNUMBER | MEAN (SD*) NO.OF CONTAMINATED SQUARES |
||
|---|---|---|---|
| Control (HVE† Only) | Isolite System‡ | Dental Dam With HVE | |
| 18 (n = 8) | 87.50 (19.03) | 63.00 (9.12) | 69.13 (10.33) |
| 19 (n = 8) | 92.13 (11.03) | 77.13 (16.08) | 73.38 (12.05) |
| 20 (n = 8) | 118.75 (6.61) | 81.25 (10.05) | 57.63 (12.81) |
SD: Standard deviation.
HVE: High-volume evacuator.
Isolite system manufactured by Isolite Systems, Santa Barbara, Calif.
The two-way ANOVA showed statistically significant differences in the amount of spatter produced between the control, dental dam and Isolite groups (F 2,63 = 46.267, P < .001), in the amount of spatter produced between teeth nos. 18, 19 and 20 (F 2,63 = 6.343, P = .003) and in the interaction between the isolation method and the tooth number (F 4,63 = 8.230, P < .001).
Overall, use of both the Isolite system and dental dam with HVE decreased spatter significantly compared with the control technique. In addition, the results showed no statistically significant differences between the two isolation methods. Pairwise comparisons demonstrate the performance of each treatment method, according to tooth number (Table 2 ). For tooth no. 18, both the dental dam and Isolite device reduced spatter by a statistically significant amount compared with results for the control technique (that is, no isolation), and there was no statistically significant difference between the two isolation methods. For tooth no. 19, the reduction in spatter with the use of the dental dam was significant, whereas use of the Isolite device did not result in a significant reduction in spatter (P = .056). Yet, there was no significant difference between the dental dam and the Isolite device for tooth no. 19. Finally, for tooth no. 20, the reduction in spatter was statistically significant with both the dental dam and the Isolite device. However, the reduction in spatter with the dental dam was significantly greater than that with the Isolite device (P = .001).
Table 2.
Pairwise comparisons (post hoc tests).
| MODEL EFFECT | MEANDIFFERENCE | STANDARDERROR | P VALUE |
|---|---|---|---|
| Isolation Method* | |||
| Isolite† versus control (HVE‡) | −25.7 | 3.6 | < .001 |
| Dental dam with HVE versus control | −32.8 | 3.6 | < .001 |
| Isolite versus dental dam | 7.1 | 3.6 | .126 |
| Tooth No.* | |||
| 18 versus 19 | −7.7 | 3.6 | .090 |
| 19 versus 20 | −5.0 | 3.6 | .349 |
| 18 versus 20 | −12.7 | 3.6 | .002 |
| Interaction,§ According to Tooth Number and Isolation Method | |||
| Tooth no. 18 | |||
| Isolite versus control (HVE) | −24.5 | 6.2 | .001 |
| Dental dam versus control | −18.4 | 6.2 | .013 |
| Isolite versus dental dam | −6.1 | 6.2 | .982 |
| Tooth no. 19 | |||
| Isolite versus control | −15.0 | 6.2 | .056 |
| Dental dam versus control | −18.8 | 6.2 | .011 |
| Isolite versus dental dam | 3.8 | 6.2 | − 1.000 |
| Tooth no. 20 | |||
| Isolite versus control | −37.5 | 6.2 | < .001 |
| Dental dam versus control | −61.1 | 6.2 | < .001 |
| Isolite versus dental dam | 23.6 | 6.2 | .001 |
Main effects determined by means of Tukey honestly significant difference test; α = .05.
Isolite system manufactured by Isolite Systems, Santa Barbara, Calif.
HVE: High-volume evacuator.
Interaction effects determined by means of Bonferroni adjustment; α = .05.
DISCUSSION
The standard protocol to limit water spray contamination from a high-speed dental handpiece has been use of a dental dam.14 However, the concurrent use of an HVE is required to reduce aerosol and spatter production.2, 15, 16, 17, 18
The Isolite system offers dentists the ability to control for several adverse factors in the oral cavity, such as continual salivary flow and a relatively dark environment in which shadowing is common. Specifically, the Isolite system allows for shadowless illumination, isolation, high-speed evacuation, protection of adjacent soft tissues, assistance in opening the mouth and protection from accidental ingestion or aspiration of foreign objects. In addition, in our experience, the device is easy to place and ideal for preparing teeth for fixed prosthodontics, as well as for other situations in which use of a dental dam would hinder access. To use the system, the dentist or a team member connects the HVE of the dental unit to the Isolite device itself. Generally, this results in no need for additional high-volume evacuation in the operative site.
We found that, overall, the Isolite device and the dental dam with HVE reduced the amount of spatter produced during the simulated tooth preparations on the left mandibular arch compared with use of the HVE alone. The study results also show that the two methods were not significantly different from each other. We also wanted to determine whether tooth position within the quadrant affected the amount of spatter that was produced. Our data show that the amount increased as we moved mesially from tooth no. 18 to 19 and then to 20. However, the only statistically significant increase occurred in moving from tooth no. 18 to tooth no. 20. This increase can be explained by the fact that the source of the water spray (that is, the hand-piece) is positioned closer to the oral aperture for tooth no. 20, and water would be more likely to escape from the mouth than to adhere to the adjacent oral tissue, the dental dam or the Isolite mouthpiece.
Pairwise comparisons enabled us to examine the various combinations of isolation method and tooth number. We found that both the Isolite device and the dental dam were significantly better than the control at reducing spatter for teeth nos. 18 and 20. For tooth no. 19, use of the dental dam resulted in a statistically significant reduction in spatter, but use of the Isolite device did not. The P value in that condition was not significant. However, we surmise that if the sample size had been larger, we might have seen a significant effect because the mean difference in spatter production between the Isolite system and the dental dam for tooth no. 19 was not statistically significantly different.
For the most anterior tooth in the study, no. 20, the dental dam with HVE performed better than did the Isolite system. We believe this is due to the design of the Isolite system. The unit has two suction ports whose orifices are located at the junction of the suction unit and the mouthpiece. Suction currents and pooled water suction are aided by perforations along the superior and inferior edges of the mouthpiece. It seems logical to us that the greatest evacuation strength would be toward the most posterior aspect of the unit. This is evidenced by the Isolite system's comparable performance for molars in this study. We should point out that although the dental dam with HVE performed better than did the Isolite device for tooth no. 20, use of the latter still resulted in a significant amount of spatter reduction.
The results of this study indicate that the Isolite system can aid in the reduction of spatter produced during operative dental procedures. The system provides the clinical benefits described earlier, and it reduces the amount of spatter comparable with that of the dental dam with HVE. However, the bacterial content of the spatter may be different for the two dry-field techniques. With the Isolite system, some gingival tissue remains exposed. A properly placed dental dam is inverted into the gingival sulcus. The bacterial content of the aerosol and spatter produced when using the Isolite device may be higher or more diverse than that produced when using the dental dam with HVE. Investigators in future studies should examine this issue.
CONCLUSIONS
Our study findings indicate that when preparing a posterior tooth in the left mandibular arch, dentists can use either a dental dam with HVE or the Isolite system, because both dry-field techniques reduced spatter significantly compared with use of an HVE alone. As a result, we can reject the null hypothesis that the dry-field techniques would not result in a significant reduction of spatter compared with the control. In addition, we found that, overall, there was no statistically significant difference between the two dry-field techniques in the amount of spatter reduction. The Isolite system appears to be comparable to the dental dam with HVE in its effectiveness in reducing spatter during procedures involving mandibular posterior permanent teeth. Investigators should conduct additional studies to compare these two techniques in different areas of the mouth and to extrapolate these results into an in vivo scenario in which the bacterial content of the spatter can be explored.
Footnotes
Disclosure. None of the authors reported any disclosures.
Isolite Systems, Santa Barbara, Calif., provided financial support for the research described in this article.
References
- 1.Miller RL. Generation of airborne infection by high speed dental equipment. J Am Soc Prev Dent. 1976;6(3):14–17. [PubMed] [Google Scholar]
- 2.Micik RE, Miller RL, Mazzarella MA, Ryge G. Studies on dental aerobiology, part I: bacterial aerosols generated during dental procedures. J Dent Res. 1969;48(1):49–56. doi: 10.1177/00220345690480012401. [DOI] [PubMed] [Google Scholar]
- 3.Miller RL, Micik RE, Abel C, Ryge G. Studies on dental aerobiology, part II: microbial splatter discharged from the oral cavity of dental patients. J Dent Res. 1971;50(3):621–625. doi: 10.1177/00220345710500031701. [DOI] [PubMed] [Google Scholar]
- 4.Holbrook WP, Muir KF, Macphee IT, Ross PW. Bacteriological investigation of the aerosol from ultrasonic scalers. Br Dent J. 1978;144(8):245–247. doi: 10.1038/sj.bdj.4804072. [DOI] [PubMed] [Google Scholar]
- 5.Larato DC, Ruskin PF, Martin A, Delanko R. Effect of a dental air turbine drill on the bacterial counts in air. J Prosthet Dent. 1966;16(4):758–765. [Google Scholar]
- 6.Gross KB, Overman PR, Cobb C, Brockmann S. Aerosol generation by two ultrasonic scalers and one sonic scaler: a comparative study. J Dent Hyg. 1992;66(7):314–318. [PubMed] [Google Scholar]
- 7.Harrel SK, Molinari J. Aerosols and splatter in dentistry: a brief review of the literature and infection control implications. JADA. 2004;135(4):429–437. doi: 10.14219/jada.archive.2004.0207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kumar S, Atray D, Paiwal D, Balasubramanyam G, Duraiswamy P, Kulkarni S. Dental unit waterlines: source of contamination and cross-infection. J Hosp Infect. 2010;74(2):99–111. doi: 10.1016/j.jhin.2009.03.027. [DOI] [PubMed] [Google Scholar]
- 9.Yamada H, Ishihama K, Yasuda K, Hasumi-Nakayama Y, Shimoji S, Furusawa K. Aerial dispersal of blood-contaminated aerosols during dental procedures. Quintessence Int. 2011;42(5):399–405. [PubMed] [Google Scholar]
- 10.O'Donnell MJ, Boyle MA, Russell RJ, Coleman DC. Management of dental unit waterline biofilms in the 21st century. Future Microbiol. 2011;6(10):1209–1226. doi: 10.2217/fmb.11.104. [DOI] [PubMed] [Google Scholar]
- 11.Syzmanska J, Sitkowska J, Dutkiewicz J. Microbial contamination of dental unit waterlines. Ann Agric Environ Med. 2008;15(2):173–179. [PubMed] [Google Scholar]
- 12.Kohn WG, Collins AS, Cleveland JL, Harte JA, Eklund KJ, Malvitz DM, Centers for Disease Control and Prevention Guidelines for infection control in dental health-care settings—2003. MMWR Recomm Rep. 2003;52(RR-17):1–61. [PubMed] [Google Scholar]
- 13.Syzmanska J. Dental bioaerosol as an occupational hazard in a dentist's workplace. Ann Agric Envion Med. 2007;14(2):203–207. [PubMed] [Google Scholar]
- 14.Cochran MA, Miller CH, Sheldrake MA. The efficacy of the rubber dam as a barrier to the spread of microorganisms during dental treatment. JADA. 1989;119(1):141–144. doi: 10.14219/jada.archive.1989.0131. [DOI] [PubMed] [Google Scholar]
- 15.Bentley CD, Burkhart NW, Crawford JJ. Evaluating spatter and aerosol contamination during dental procedures. JADA. 1994;125(5):579–584. doi: 10.14219/jada.archive.1994.0093. [DOI] [PubMed] [Google Scholar]
- 16.Harrel SK, Barnes JB, Rivera-Hidalgo F. Reduction of aerosols produced by ultrasonic scalers. J Periodontol. 1998;67(1):28–32. doi: 10.1902/jop.1996.67.1.28. [DOI] [PubMed] [Google Scholar]
- 17.Jacks ME. A laboratory comparison of evacuation devices on aerosol reduction. J Dent Hyg. 2002;76(3):202–206. [PubMed] [Google Scholar]
- 18.Klyn SL, Cummings DE, Richardson BW, Davis RD. Reduction of bacteria-containing spray produced during ultrasonic scaling. Gen Dent. 2001;49(6):648–652. [PubMed] [Google Scholar]
- 19.Siegel SC, von Fraunhofer JA. The effect of handpiece spray patterns on cutting efficiency. JADA. 2002;133(2):184–188. doi: 10.14219/jada.archive.2002.0142. [DOI] [PubMed] [Google Scholar]
- 20.Galindo DF, Ercoli C, Funkenbusch PD. Tooth preparation: a study on the effect of different variables and a comparison between conventional and channeled diamond burs. J Prosthodont. 2004;13(1):3–16. doi: 10.1111/j.1532-849X.2004.04003.x. [DOI] [PubMed] [Google Scholar]


